Lucy Letby Innocence
-
Main Page
Lucy Letby - The Complete Trial
This page contains the complete day-by-day trial reporting by the Chester Standard and others.
The first week- Monday 10th October The charges - jury panel finalised - jury instructions - Prosecution Opening Statement begins
- Tuesday 11th October Prosecution Opening Statement day 2
- Wednesday 12th October Prosecution Opening Statement day 3
- Thursday 13th October Prosecution Opening Statement day 4 - Defence Opening Statement
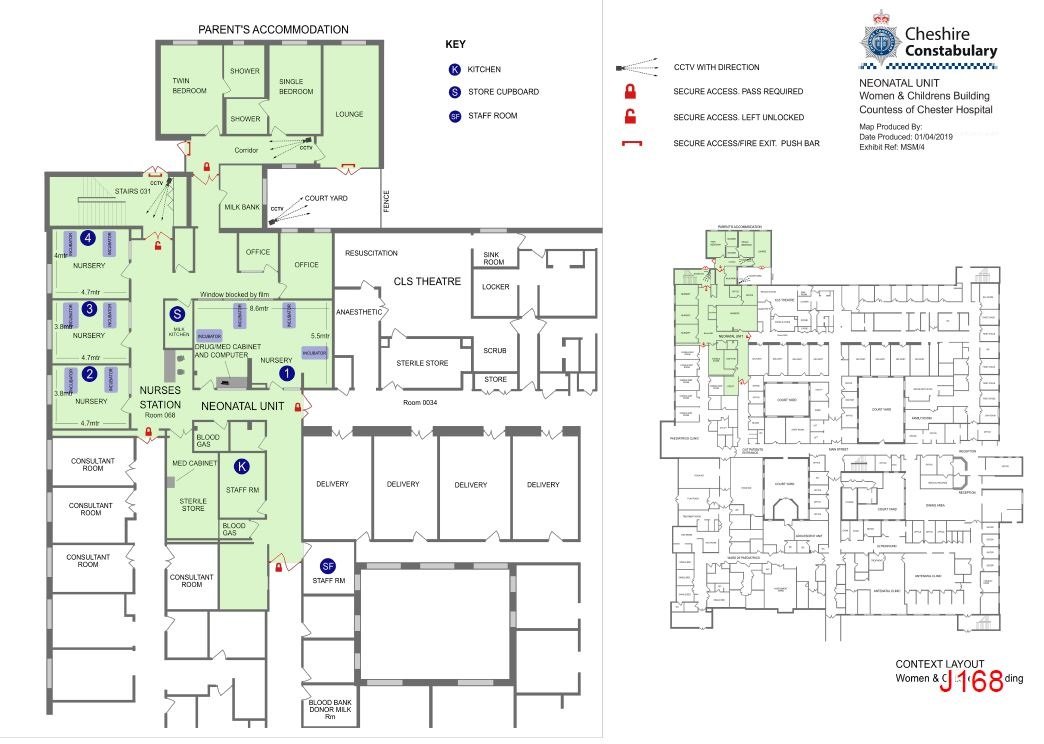
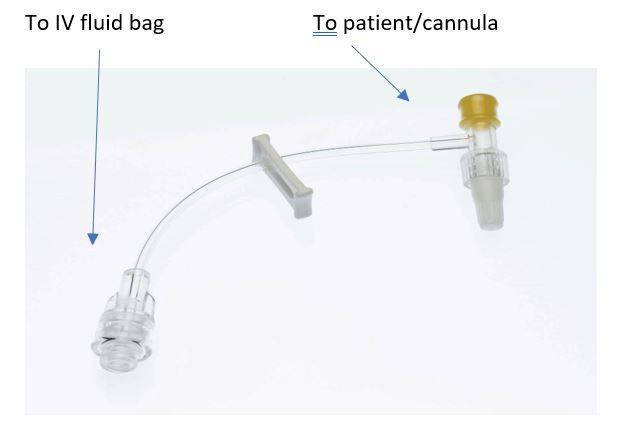
- Friday 14th October Hospital layout - Neonatology procedures & equipment - Dr Dewi Evans
- Monday 17th October Parents' statements - Grandmother's statement - Police analyst: Recorded events & messages
- Tuesday 18th October Police analyst: Recorded events & messages (Child A)
- Wednesday 19th October Police analyst: Recorded events & messages (Child B) - other agreed facts - Statements from: Midwife, Dr Gail Beech, Dr Andrew Brunton, Unnamed doctor (trainee) - Nurse Melanie Taylor
- Thursday 20th October Nurse Melanie Taylor - Dr David Harkness - Statements from: Dr Christopher Wood , Nurse assistant Lisa Walker, Nurse Joanne Williams
- Friday 21st October Dr Harkness - Professor Owen Arthurs (radiologist) - Senior neonatal Nurse Caroline Bennion - Nurse A (Shift leader)
- Monday 24th October Nurse A - Dr Rachel Lambie - Dr Ravi Jayaram
- Tuesday 25th October Dr B - Dr Dewi Evans - Dr Sandie Bohin
- Wednesday 26th October Dr Sandie Bohin - Summary of police interviews - Parents' statements - Police analyst: Recorded events & messages
- Thursday 27th October Police analyst: Recorded events & messages - Dr Sally Ogden - Dr Gail Beech - Yvonne Griffiths (senior nursing practitioner & neonatal unit deputy manager)
- Friday 28th October Nurse Joanne Williams - Nurse Sophie Ellis - Nurse Melanie Taylor
- Monday 31st October Nurse B (shift leader) - Dr Katherine Davis - Dr John Gibbs
- Tuesday 1st November Dr John Gibbs - Statements from: Dr Andrew Brunton (trainee paediatrician) & Nurse Bernadette Butterworth - Dr Dewi Evans - Dr Sandie Bohin
- Monday 2nd November Dr Sandie Bohin - Summary of police interviews
- Thursday 3rd November Family statements - Police analyst: Recorded events & messages
- Friday 4th November Police Analyst: Recorded events & charts - Nurse Caroline Oakley
- Monday 7th November Dr Andrew Brunton - Dr Joanne Davies (consultant in obstetrics and gynaecology) - Nurse Assistant Lisa Walker
- Tuesday 8th November Dr Sarah Rylance - Unnamed Nurse - Dr Emily Thomas - Nurse Elizabeth Marshall
- Wednesday 9th November Dr. Elizabeth Newby - Nurse Kathryn Percival-Calderbank - Dr Dewi Evans
- Friday 11th November Dr Sally Ogden - Professor Owen Arthurs (Child C & Child D) - Dr Sandie Bohin - Summary of police interviews
- Monday 14th November Parents' testimony - Police analyst: Recorded events & messages
- Tuesday 15th November Statement of Midwife Susan Brookes - Dr Christopher Wood - Nurse B - Statement of Nurse Caroline Oakley
- Wednesday 16th November Dr C - Unnamed nurse
- Thursday 17th November Dr David Harkness
- Friday 18th November Dr Dewi Evans - Dr Sandie Bohin
- Tuesday 22nd November Police analyst: Recorded events & messages - Dr Gail Beech
- Wednesday 23rd November Nurse Shelley Tomlins - Nurse Sophie Ellis - Nurse Belinda Williamson
- Thursday 24th November Dr C - Video demonstration of an Alaris Pump - Dr John Gibbs - Unnamed nurse
- Friday 25th November Dr Anna Milan (Clinical biochemist) - Professor Peter Hindmarsh - Dr David Harkness
- Monday 28th November Dr Satyanarayana Saladi (Consultant) - Dr Alison Ventress (Registrar) - Unnamed nurse
- Tuesday 29th November Professor Sally Kinsey (haematologist - evidence for Child A, B, E & F) - Ian Allen (Pharmacy)
- Wednesday 30th November Yvonne Griffiths - Nurse Kate Bramall - Unnamed nurse - Nurse Cheryl Cuthbertson-Taylor - Nurse Valerie Thomas, Statement of Dr Simon Woods(consultant obstetrician & gynaecologist) - Dr Sandie Bohin - Dr Dewi Evans
- Thursday 1st December Police analyst: Recorded events & messages - Parents' statements - Dr Alison Ventress.
- Friday 2nd December Unnamed nurse - Nurse Ailsa Simpson (shift leader)
- Tuesday 6th December Statement of Unnamed nurse, Instructional videos on ventilators, suction tubes & heart rate monitors
- Monday 12th December Dr Stephen Brearey - Dr David Harkness - Nurse Christopher Booth - Dr Dewi Evans - Dr Sandie Bohin
- Tuesday 13th December Dr Sandie Bohin - Statement of Medical engineer Steve Eccles - Police analyst: Recorded events & messages - Unnamed nurse
- Wednesday 14th December Unnamed nurse - Dr Peter Fielding (SHO) - Dr John Gibbs - Nurse Caroline Bennion - NNU Manager Eirian Powell - Expert witness statements from: Professor Simon Kenny, Dr Stavros Stivaros
- Thursday 15th December Dr David Harkness
- Wednesday 18th January Dr
Dewi Evans - Dr Sandie Bohin - Summary of police interviews
Child H: Parents' statements - Police analyst: Recorded events & messages
- Thursday 19th January Statement of Midwife Deborah Moore - Unnamed nurse - Dr Ventress
- Friday 20th January Dr Ravi Jayaram - Dr John Gibbs
- Monday 23rd January Dr Matthew Neame (Registrar) - Nurse Shelley Tomlins - Nurse Christopher Booth
- Tuesday 24th January Dr Sandie Bohin - Dr Dewi Evans
- Wednesday 25th January Mother’s statement - Police analyst: Recorded events & messages
- Thursday 26th January Unnamed nurses - Nurse Bernadette Butterworth
- Friday 27th January GP Dr Lucy Beebe - Nurse Ashleigh Hudson
- Wednesday 1st February Dr Matthew Neame - text messages
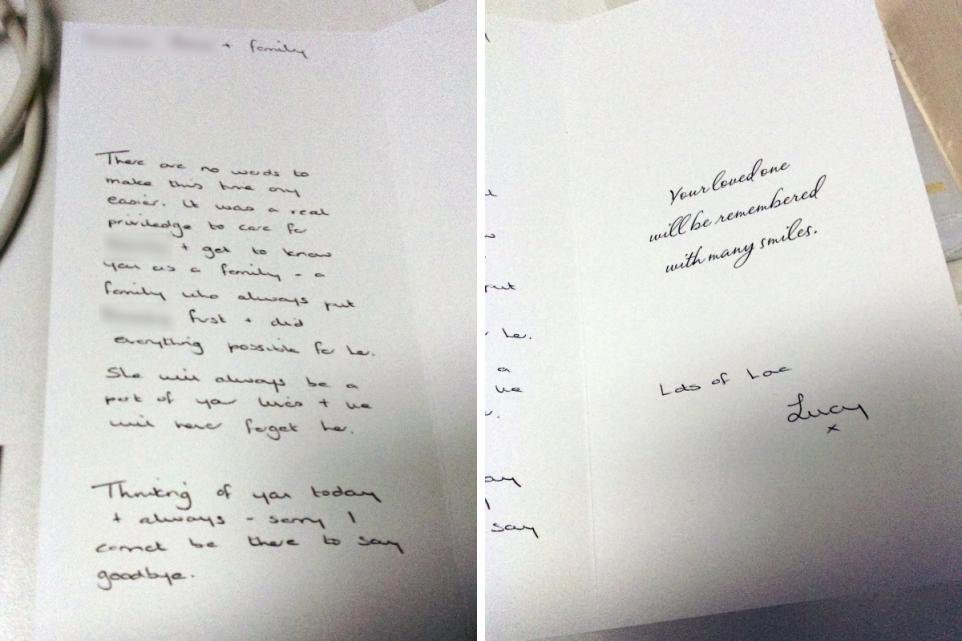
- Thursday 2nd February Statements from: Nurse Shelley Tomlins, Nurse Joanne Williams, Nurse Laura Eagles, Dr David Harkness, Consultant from Arrowe Park Hospital - Police analyst: Recorded events & messages, sympathy card - Nurse Ashleigh Hudson
- Friday 3rd February Professor Owen Arthurs (radiologist) - Dr Rachel Chang - Statements from: Nurse Christopher Booth, Nurse Melanie Taylor, Nursery nurse Valerie Thomas
- Thursday 9th February Dr John Gibbs - Dr Dewi Evans
- Friday 10th February Dr Sandie Bohin -
Summary of police interviews -
Child J: Mother - Police analyst: Recorded events & messages
- Monday 13th February Dr John Gibbs - Dr Stephen Brearey - Nurse Mary Griffith
- Tuesday 14th February Dr Dewi Evans - Dr Sandie Bohin
- Wednesday 15th February Police analyst: Recorded events & messages - Parents' statements - Midwife's statement, Dr Sudeshna Bhowmik (Paediatric trainee) - Nurse Amy Davies - Dr Anthony Ukoh
- Thursday 16th February Dr A - Dr John Gibbs
- Monday 20th February
Child L: Dr Anna Milan (Clinical biochemist) - Dr. Gwen Wark (Director of the Guildford RSCH Peptide Hormone Laboratory) - Summary of police interviews
Child M: Police analyst: Recorded events & messages - Tuesday 21st February Child M: Nurse Mary Griffith - Unnamed nurse - Dr Anthony Ukoh
- Wednesday 22nd February Child M: Nurse Belinda Williamson - statement of Nurse Ashleigh Hudson - Dr Ravi Jayaram
- Thursday 23rd February Child M: Dr John Gibbs - Statement of consultant paediatric cardiologist Dr. Arjamand - Dr Dewi Evans - Dr Sandi Bohin - Summary of police interviews
- Friday 24th February Child L: Dr Emma Lewis (Consultant clinical biochemist at the CoCH) - Professor Peter Hindmarsh
- Monday 27th February Mother's statement - Police analyst: Recorded events & messages - Dr Jonathan Ford - Dr James Smith - Nurse Joanne Williams
- Tuesday 28th February Nurse Joanne Williams - Dr Ravi Jayaram - Elizabeth Morgan (Cheshire Police Nursing Advisor)
- Wednesday 1st March Summary of Police Interviews
- Thursday 2nd March Parents' statements - Police analyst: Recorded events & messages - Dr. Jennifer Loughnane - Statements from Dr Sudeshna Bhowmik, Caroline Oakley, Melanie Taylor, Sophie Ellis, Christopher Booth, Valerie Thomas
- Friday 3rd March Police analyst: Recorded events & messages - Nurse Jennifer Jones-Key - Dr D (Registrar)
- Monday 6th March Dr Huw Mayberry - Dr A - Dr John Gibbs - Dr Stephen Brearey - Dr Francis Potter (Alder Hey)
- Tuesday 7th March Statements from doctors & nurses - Elizabeth Morgan (Cheshire Police Nursing Advisor) - Professor Sally Kinsey - Dr Dewi Evans - Dr Sandie Bohin
- Wednesday 8th March Children O & P: Statements from mother & grandmother, father's statement by video - Police Analyst: Recorded events & messages - Statements of Dr B & Nurse Kate Bissell - Nurse Sophie Ellis
- Thursday 9th March Dr Huw Mayberry - Dr. Kataryna Cooke (SHO) - Nurse Melanie Taylor
- Tuesday 14th March Statements of neonatal nurse practitioner Amy Davies - Unnamed nurse - Dr Stephen Brearey - Unnamed doctor
- Wednesday 15th March Dr Dewi Evans - Summary of police interviews
- Thursday 16th March Professor Owen Arthurs (Children O & P)
- Monday 20th March Police analyst: Recorded events & messages - Dr A - Dr Ukoh - Nurse Sophie Ellis
- Tuesday 21st March Senior nurse Kathryn Percival-Calderbank - Unnamed consultant
- Wednesday 22nd March Dr John Gibbs - Dr Stephen Brearey - Dr Oliver Rackham (Arrowe Park)- Dr Dewi Evans
- Thursday 23rd March Dr Dewi Evans - Dr Sandie Bohin
- Wednesday 29th March Pathologist Dr Andreas Marnerides (children A, C, D, I & O)
- Thursday 30th March Pathologist Dr Andreas Marnerides (children A, C, D, I & O)
- Friday 31st March Parents' statements - Police analyst: Recorded events & messages - Statements of Midwife & Nurse Christopher Booth - Nurse Tanya Downes
- Monday 3rd April Nurse Samantha O'Brien - Unnamed doctor - Nurse Mary Griffith - Nurse Minna Lappalainen (shift leader)
- Wednesday 5th April Dr A - Dr John Gibbs - Dr Dewi Evans
- Thursday 6th April Dr Sandie Bohin - Police analyst: Texts & messages
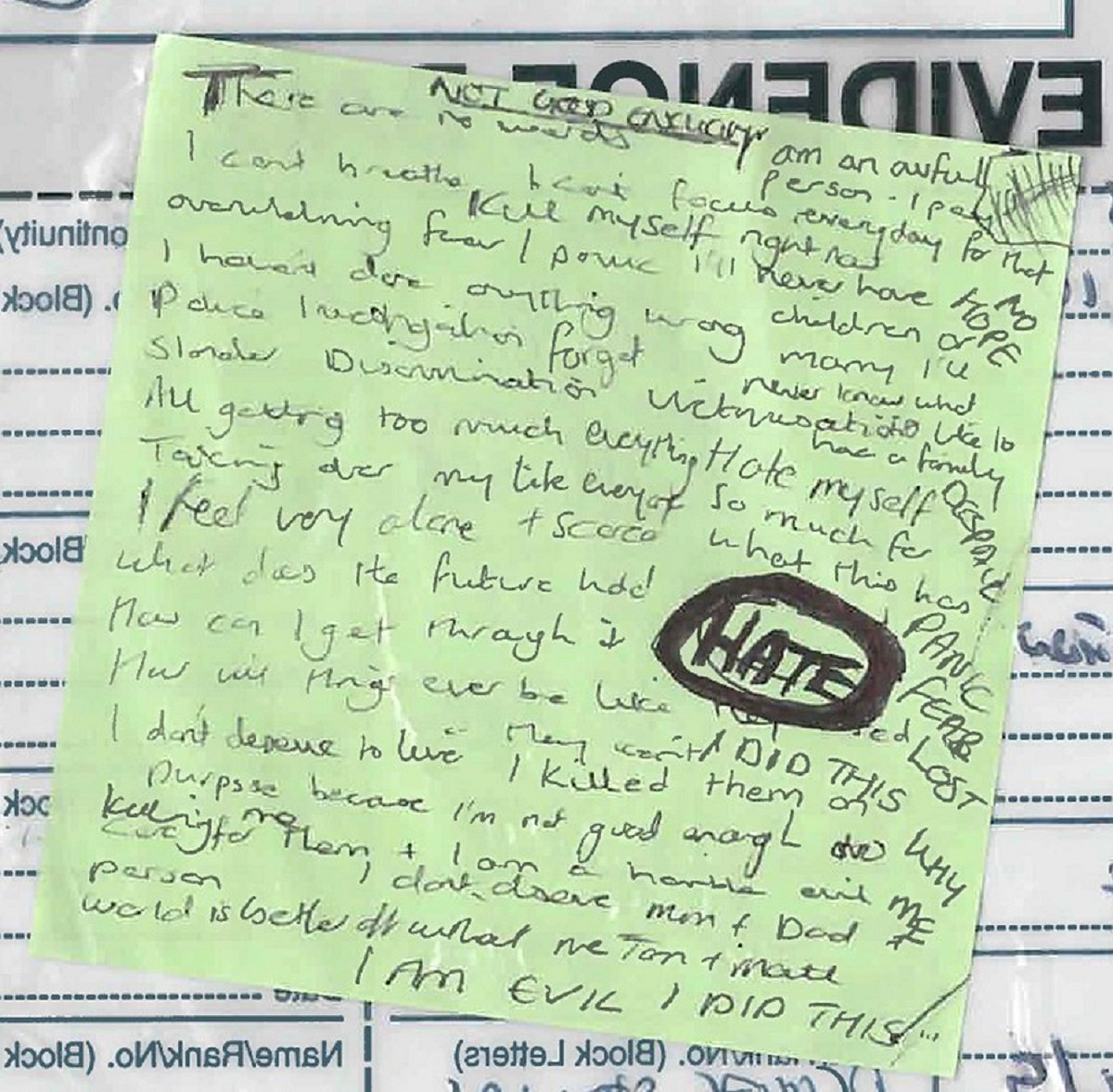
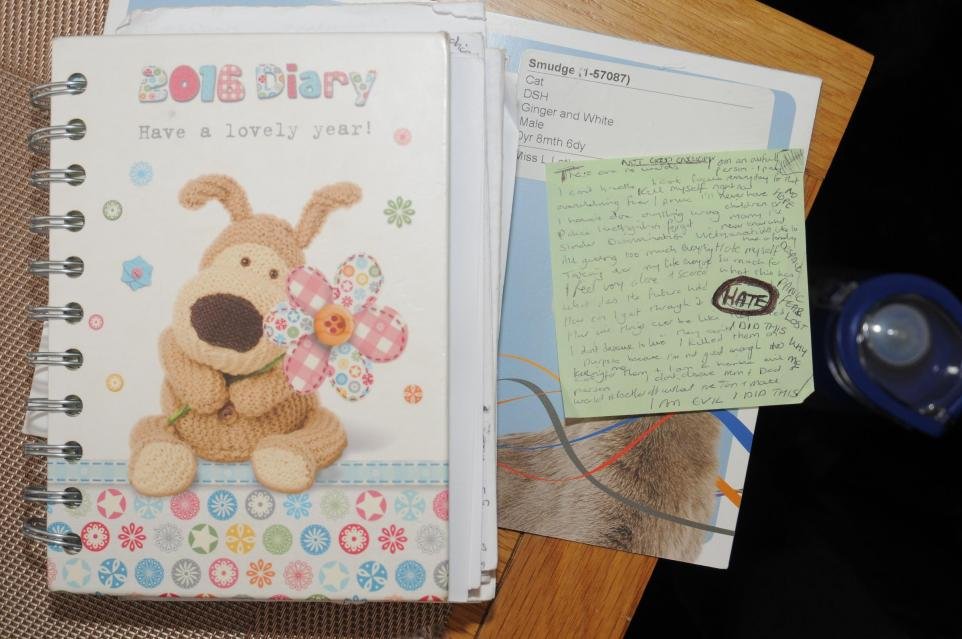
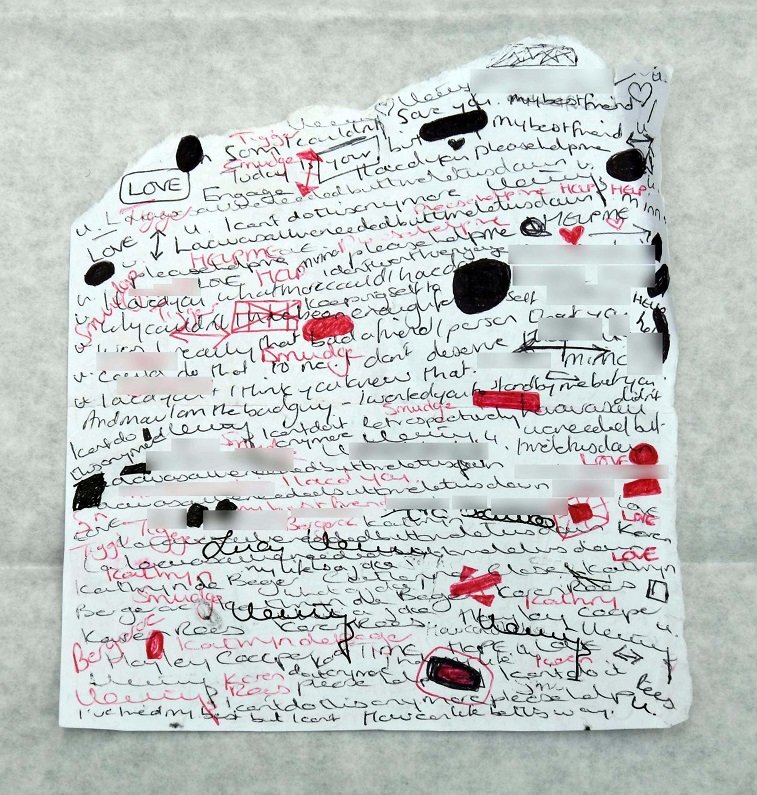
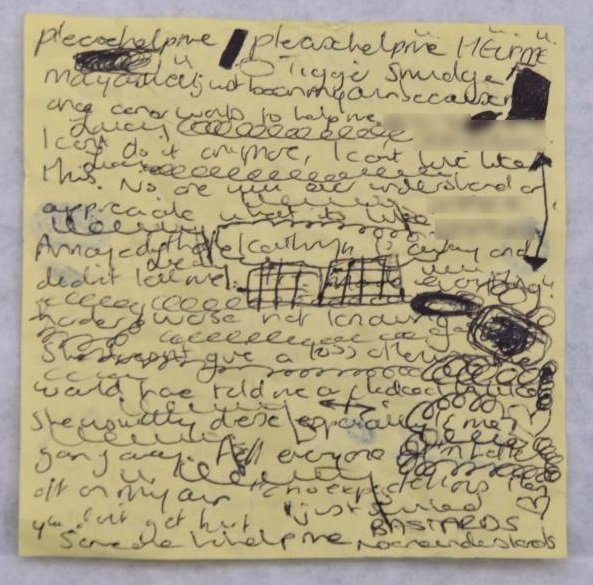
- Monday 17th April House search: post-it notes, diary, handover sheets - Police interviews re Child A
- Thursday 20th April Professor Arthurs (Child Q) - Police interviews re Children A-H
- Tuesday 25th April Police interviews re Children I-P
- Thursday 27th April Police interviews re Child Q - Police interviews on other matters e.g. the notes, competencies & staffing, handover sheets, training - Eirian Powell - Other agreed facts
- Thursday 2nd May Background and general topics
- Friday 5th May Children A, B, C, D & E
- Monday 15th May Children F, G, H & I
- Tuesday 16th May Children I, J, K, L & M
- Wednesday 17th May Children N, O, P & Q
Cross-examination by Nick Johnson KC for the Prosecution begins
- Thursday 18th May Day 2 - General topics - Children A, B & C
- Friday 19th May Day 3 - Children C & D
- Wednesday 24th May Day 4 - Children E, G, & H
- Thursday 25th May Day 5 - Children H & I
- Friday 2nd June Day 6 - Children I, J & K
- Monday 5th June Day 7 - Children K, F & L - (juror sent home unwell)
- Wednesday 7th June Day 8 - Children M & N
- Thursday 8th June Day 9 - Children O, P & Q
- Friday 9th June Day 10 - What happened next
- other matters (Facebook searches, Dr A, social life, notes etc) -
Re-examination by Ben Myers KC for the Defence
- Wednesday 14th June Defence witness: Plumber Lorenzo Mansutti
- Thursday 15th June Mr Justice Goss addresses the Jury
- Monday 19th June Day 1
- Tuesday 20th June Day 2
- Wednesday 21st June Day 3
- Thursday 22nd June Day 4
- Monday 26th June Day 1 & Contents Menu
- Tuesday 27th June Day 2
- Wednesday 28th June Day 3
- Thursday 29th June Day 4
- Friday 30th June Day 5
- Monday 3rd July 2023 Day 1: Background - Children A, B & C
- Tuesday 4th July 2023 Day 2: Children D, E, F & G
- Wednesday 5th July 2023 Day 3: Children H, I & J
- Thursday 6th July 2023 Day 4: Children K, L, M, N, O & P
- Monday 10th July 2023 Day 5: Child Q - Other topics (Notes, Handover sheets, Diaries etc.) - General Instructions
The complete text (transcript) of the Judge's summing up is here: Mr Justice Goss's Summing Up Of The Letby Case
Monday 10th October 2022
Chester Standard Live Reporting - Monday 10th to Wednesday 12th October AM
9:53am: The trial of former Countess of Chester Hospital nurse Lucy Letby, who is accused of multiple baby murders, is due to finalise its jury and hear from the prosecution today (Monday, October 10).
9:59am: It is anticipated that today will be the day the trial jury will be finalised, and following that, the prosecution will formally open the case. Due to the complexity of the case, it is anticipated the prosecution opening could last two days.
10:00am: Jurors will have been selected from a longlist of well over 100 people, and each member of the finalised jury will have to make themselves available until the end of April, to attend every day of the trial which is expected to last six months.
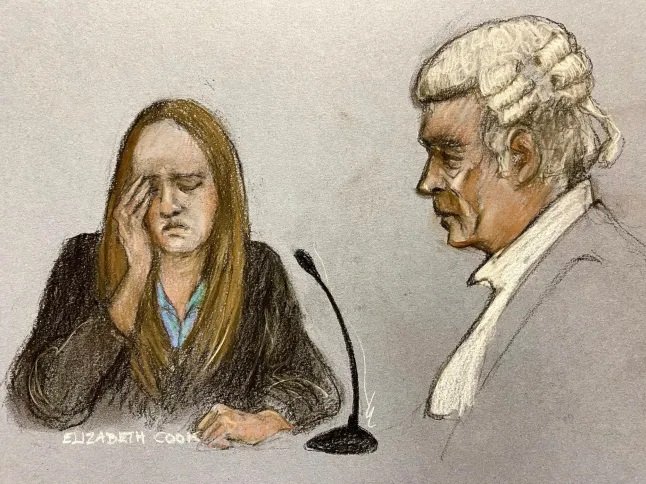
10:18am: Members of the press are attending the annexe courtroom provided for the media at Manchester Magistrates Court. The trial itself is taking place at the nearby Manchester Crown Court, with limited space for the media - the Press Association have allocated seats there, plus space for courtroom sketch artists. For the rest of the media, the trial is being broadcast on TV screens in the nearby magistrates courtroom, the only place outside of the crown court where the press can view proceedings. The magistrates courtroom has allocated spaces for up to 50 journalists from print, TV and radio publications.
10:20am: This is day four of the trial, which began on Tuesday, October 4, but did not sit the following day. The case resumed for court hearings last Thursday and Friday, where there were further legal discussions.
10:24am: Lawyers are now attending the courtroom at Manchester Crown Court, with the case due to resume at 10.30am.
10:40am: Lucy Letby has entered the courtroom, wearing dark clothing, as has the court judge.
10:42am: A number of amendments have been put to the charges. Letby now faces an increased number of charges - 22 in total.
10:47am: The number of alleged victims remains the same - 17. The five new charges are for repeat attempted murder charges.
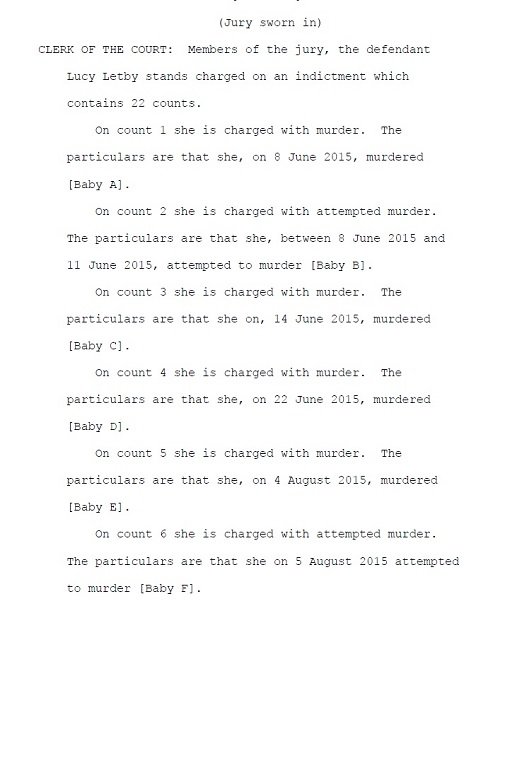
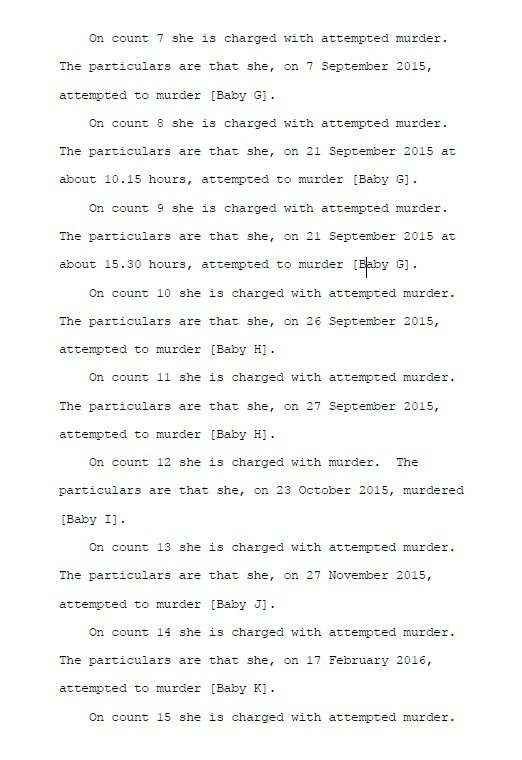
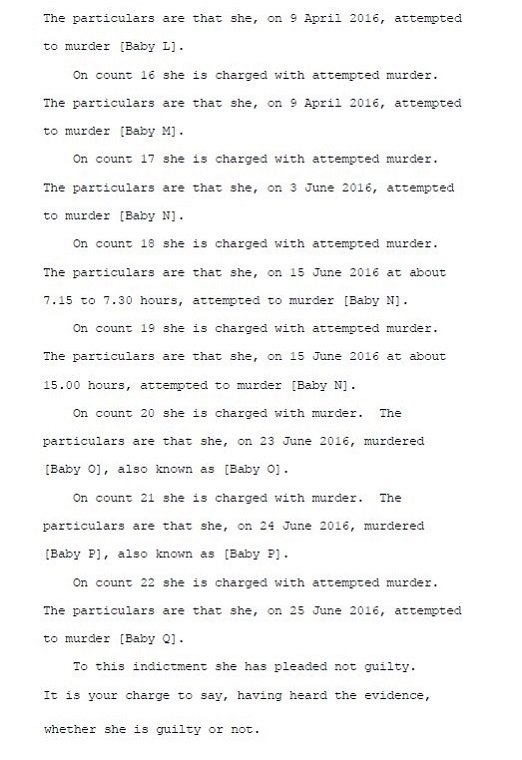
The charges:
Count 1: Murder of Baby A on 8 June 2015.
Count 2: Attempted murder of Baby B between 8 June 2015 and 11 June 2015.
Count 3: Murder of Baby C on 14 June 2015.
Count 4: Murder of Baby D on 22 June 2015.
Count 5: Murder of Baby E on 4 August 2015.
Count 6: Attempted murder of Baby F on 5 August 2015.
Count 7: Attempted murder of Baby G on 7 September 2015.
Count 8: Attempted murder of Baby G on 21 September 2015, at about 10.15 hours.
Count 9: Attempted murder of Baby G on 21 September 2015, at about 15.30 hours.
Count 10: Attempted murder of Baby H on 26 September 2015.
Count 11: Attempted murder of Baby H on 27 September 2015.
Count 12: Murder of Baby I on 23 October 2015.
Count 13: Attempted murder of Baby J on 27 November 2015.
Count 14: Attempted murder of Baby K on 17 February 2016.
Count 15: Attempted murder of Baby L on 9 April 2016.
Count 16: Attempted murder of Baby M on 9 April 2016.
Count 17: Attempted murder of Baby N on 3 June 2016.
Count 18: Attempted murder of Baby N on 15 June 2016, at about 7.15 to 7.30 hours.
Count 19: Attempted murder of Baby N on 15 June 2016, at about 15.00 hours.
Count 20: Murder of Baby O on 23 June 2016.
Count 21: Murder of Baby P on 24 June 2016.
Count 22: Attempted murder of Baby Q on 25 June 2016.
10:55am: Letby has pleaded not guilty to all 22 charges. For the sake of clarity, she was asked to re-enter a plea to all existing 17 charges - seven of murder, 10 of attempted murder. The five new charges were all of attempted murder.
11:24am: The court has had a short adjournment, and upon its return it is expected the trial jury will be finalised.
11:35am: Lucy Letby, 32, wearing a blue jacket over a black shirt, stood in the dock this morning and replied “not guilty” as each of the 22 charges were read out to her at Manchester Crown Court. Family members of some of her alleged child victims sat in the public gallery listening as the names of the children were read out during her not guilty pleas. On the other side of the public gallery sat the defendant’s parents, John, 76, and Susan, 62.
11:55am: The jury panel has now been finalised. Jury members are to appear in court, identify themselves, then will take their places in the jury box. It is expected the prosecution will then formally begin the opening.
11:58am: All potential jurors have declared they can make themselves available to attend the trial for up to the next six months.
12:06pm: Two potential jurors were recognised by members of the prosecution team, so have been taken out of the final jury. A final jury of 12 members, plus two in reserve, has now been selected.
12:08pm: The 12 jurors are now taking their allocated spaces in the courtroom.
12:14pm: The 12 (plus two in reserve) are now being formally sworn in as the jury for the Lucy Letby trial.
12:20pm: The jury is now being informed of the 22 charges Lucy Letby faces - seven of murder, 15 of attempted murder. All charges relate to offences alleged during her time at the Countess of Chester Hospital's neonatal unit between June 2015 and June 2016. Letby denies all 22 charges.
12:24pm: Addressing the jury, the judge, Mr Justice James Goss, is now explaining the role of the jurors for this trial, adding they will have noted the "common theme" of charges listed - those of murder and attempted murder.
12:28pm: The judge is asking the jurors not to be "anxious" during the course of this trial, explaining there are a number of serious cases being tried up and down the country, and to keep an open mind until they have heard all the evidence.
12:30pm: Mr Justice Goss adds the instinctive reaction to charges of this nature, of murdering and attempting to murder babies, is one of "horror". He says the jury must put emotions to one side and consider the evidence "calmly, rationally, fairly and dispassionately."
12:33pm: The jury are being advised they are not prohibited from using social media, but they should ignore comments made on there in relation to the trial, and to understand that media reports will be "selective" and focus on only parts of the trial. Jurors are also urged not to research additional evidence, outside of the courtroom, in relation to the case in any way.
12:35pm: The jury are also advised not to talk about the case to family or friends over the next six months, with Mr Justice Goss saying there will be "many opportunities" for members of the jury to mix with people they know during that time. The judge is reminding them that doing so would be an offence, for which they could be prosecuted, and the integrity of the trial could be at risk.
12:39pm: The jury is also being told that any deliberations they make at the conclusion of the trial have a "lifetime prohibition" from being revealed in public, and each juror takes the contents of what was discussed in the deliberation room in relation to the case as secret "for as long as they are alive".
12:43pm: Members of the jury are also being told that court days during the trial will typically last until about 4.15pm, but can go later in exceptional circumstances, and can sometimes finish earlier.
12:48pm: The jury will have their evidence available on iPads, rather than what would otherwise be a heavy bundle of paper documents for this trial.
12:49pm: The prosecution will now begin the opening.
12:51pm: Prosecuting, Nicholas Johnson KC said everyone should be aware of the city of Chester, and its busy general hospital. Said hospital includes a neonatal unit, caring for premature and sick babies. "It is a hospital like so many others in the UK," he added. "But unlike so many others, within the neonatal unit, a poisoner was at work."
12:52pm: The statistics of the mortality rate were comparable, prior to January 2015, but there was "a significant rise" in the number of babies dying or having "catastrophic collapses". This rise was "noticed" and the concern was the babies had died "unexpectedly", and when babies collapsed, they did not respond to sufficient resuscitation. The collapses "defied" the expectations of the treating doctors.
12:54pm: Usually, when an intervention is taken, a positive response can be expected, he told the jury. Babies "who had not been unstable at all" or "on the mend", "suddenly deteriorated", "for no reason at all". Consultants noted there was "one common denominator" - the presence of neonatal nurse Lucy Letby.
12:55pm: There were between 25-30 nurses and 15-20 nursery unit nurses in that part of the hospital, working day/night shifts. More would work on the day than the night shifts, typically. Parents tended to visit their sick children during the day, Mr Johnson added. Many of the events occurred "during the night shifts". When Letby was moved to the day shifts, the rate of collapses "shifted to the day shift pattern".
12:56pm: Police were then called in, and commissioned a "painstaking review" by "experienced doctors with no connection to the Countess of Chester Hospital". The review concluded that two children were "poisoned" with insulin. The prosecution say the "only reasonable conclusion" is the babies were poisoned "deliberately - these were no accidents".
12:58pm: The prosecution say other collapses could be due to "sabotaging". The prosecution adds these deaths and non-fatal collapses were deliberate, and Letby was the "constant malevolent presence" when things took a turn for the worse in these 17 children, Mr Johnson added.
12:59pm: Mr Johnson said there were "a very restrictive number of people" who could have entered the neonatal unit, due to the security arrangements in place at the hospital.
1:00pm: The prosecution has now stopped for the 1pm lunch break, and will resume later today.
2:08pm: The afternoon session in court is to begin shortly.
2:10pm: Prosecutor Nicholas Johnson KC will resume the opening to the case.
2:12pm: We will hear further details on the two babies the prosecution say were deliberately poisoned by Lucy Letby. One matter which was resolved during last week's legal discussions was on a matter of reporting restrictions. For this trial, nothing can be published that could identify any of the children listed in the charges. While normally the media would be able to report the names of people who have died in court reporting, for this case a crown court judge has imposed a reporting restriction preventing the publication of all children listed on the charges, including the babies who died. That means the press cannot report the names of the children or their parents, as well as witnesses connected with the children. As a result, it has been agreed among the media that each of the children has been named as a letter - ie, 'Baby/Child A, Baby/Child B, Baby/Child C', following the pattern to 'Baby/Child Q'. Each letter will refer to a child listed on the charges Letby faces. The media have been asked to stick with this system so all reports on the case will have a uniformed approach.
2:14pm: The babies, each a twin belonging to a separate family, were "poisoned with insulin", the prosecution said. Mr Johnson said: "Both boys’ blood sugar inexplicably dropped to dangerous levels – the sort of levels that can result in all sorts of medical problems and ultimately in death if not rapidly rectified. Both boys survived because of the skill of the medical staff."
2:16pm: The cause of 'poisoning' "simply did not occur to medical staff working at the Countess that someone in the neonatal unit "would have injected them with insulin", the court heard.
2:17pm: Both babies 'targeted' with insulin had brothers. The prosecution say they too were "attacked" by Letby. One of the brothers "was killed".
2:18pm: Mr Johnson: The method by which these two babies were "attacked" was "by having air injected into the bloodstream – what the doctors call an air embolus."
2:21pm: Mr Johnson: For other babies, some were "harmed and killed" by the 'injection of air' into the bloodstream or via a tube into the stomach."
"Sometimes they were injected with 'too much' milk or some other fluid, or air, that can have catastrophic effects on the baby... sometimes insulin."
"But the constant presence at all these events was Lucy Letby."2:25pm: There are "many events" that will mirror the counts in the indictment, that the jury will hear, the prosecution tells the court. A chart is displayed to the jury about the presence of staff on duty at the time the babies were "attacked", with Letby present for all 24 incidents listed between 2015 and 2016. The majority of incidents are at night-time. No other member of registered nurse and/or nursery nurse staff is present for more than a total of seven incidents.
2:27pm: "It is a process of elimination," Mr Johnson tells the court.
2:31pm: The case "concerns seven allegations of murder of seven babies and the attempted murder of 10 other babies." Mr Johnson tells the court: "Sometimes Lucy Letby tried to kill the same baby more than once – and sometimes a baby that she succeeded in managing to kill was not killed the first or second time, and in one case, even the third time."
2:43pm: Letby was "originally from Hereford" and studied nursing at the University of Chester. Mr Johnson tells the court: "At the time of the events leading to the charges against her she was a nurse at the Countess of Chester Hospital and had been so since she had qualified a few years earlier. "Throughout the period she had been working in the neonatal unit." Prior to her arrest, she had been living in Chester, the court hears.
2:45pm: Nurses worked on the children's ward as well as the neonatal unit, but "it was the general rule" they did not mix on a shift. A day shift would begin at 7.30am and the night shift would end at 8am, leaving a 30-minute handover period. A general briefing would occur during that time, before patient-specific handovers. There were two types of day shift - a short day and a long day. A short day would end in the afternoon, the long day shift would end at 8pm. When babies are handed over from one shift to the next, the system was that a sheet was produced, listing all the babies in the unit at the time and their corresponding designated nurses.
2:48pm: The hospital has - and had - band 6 nurses, band 5 nurses - ones who had done special training and ones who had not - and band 4 nurses (nursery nurses). Letby had done her special training, caring for intensive care unit babies, which permitted her to work in the neonatal unit.
2:51pm: On a specific shift, a senior nurse would be designated as a shift leader, responsible for assigning specific nurses to specific babies. They would be responsible for the administration of medicine. The neonatal unit had four rooms, split into the ICU (intensive care unit), the HDU (high dependency unit) and special care babies rooms. "With one or two exceptions", the cases in this trial, Mr Johnson explains, were dealt with in the ICU or HDU.
2:55pm: Doctors at the hospital would work different shifts from the nurses, and a shift would cover the children's ward and the neonatal unit. Paediatric consultants would be on duty from 9am-5pm, while at night there would be a paediatric consultant on call within 10 minutes of the department. Registrars would provide senior medical cover overnight.
2:57pm: All the children involved in the case were in the neonatal unit and, Mr Johnson said, Letby "was either responsible for their care or got involved with them." Witnesses will be called to give evidence from just before, at the time of, or just after the events of alleged criminality occurred.
3:00pm: The evidence given, Mr Johnson explains, will "put into context" into what was going on at the neonatal unit and how an individual child was being treated at the time.
3:03pm: The prosecution is now turning to the individual cases.
3:06pm: Count 1: Child A murder allegation Child A, a boy, was born premature in June 2015, the younger of a twin child (Child B).
3:11pm: Medical records for Child A's birth are shown to the jury, including the names of which medical staff were present at the birth, and the condition of Child A, plus medical observations. Child A was in "good condition" at birth, and taken to the neonatal unit ICU. 13 hours later, he was breathing "in air" without the requirement of extra, medically administered, oxygen.
3:18pm: A medical chart records the fluids going in and out of Child A. Child A was given 1ml of milk via a nasogastric tube at 4pm and 6pm. A nurse had looked after Child A that day. She handed over care to Letby at 8pm before she had been able to administer intravenous fluids. The fluids were started at the time of the handover - the nurse assisting Letby. Child A was stable at the time of the handover.
3:23pm: The connection of the fluids, Mr Johnson said, would have been after 8.10pm, and it was recorded on the infusion prescription chart at 8.05pm. At 8.20pm, Child A was reported to have white feet and hands, and Letby called a doctor to the incubator at 8.26pm, as child A was deteriorating. Resuscitation procedures began, with adrenaline administered to stimulate the heart. Doctors observed "an odd discolouration on Child A's abdominal skin - flitting patches of pink over blue skin that seemed to appear and disappear". Mr Johnson said: "This proved to be the first of a series of similar presentations on the skin of babies suddenly and catastrophically collapsing at the CoCH NNU over the succeeding months. "It is a hallmark of some of the cases in which Lucy Letby injected air into the blood streams of some of these small babies."
3:26pm: "All resuscitation techniques which would be expected to bring a baby back to life failed." Child A was pronounced dead at 8.58pm. He had died, Mr Johnson said, within 90 minutes of Lucy Letby coming on duty. She was recorded as being the only witness associated with Child A's collapse. The doctor noted, at 8.26pm, that Lety was showing an oxygen mask to Child A's face. The monitors showed Child A had a normal heart rate and good oxygen saturations, and a normal ECG, but was not breathing. The doctor noted: "an unusual blotchy pattern of well perfused pink skin over the whole of [Child A]'s body coupled with patches of white and blue skin … all over his body." The case was referred to the coroner and the cause of Child A's death was 'unascertained' at the time.
3:30pm: Medical expert Dr Dewi Evans suggested Child A's collapse was "consistent with a deliberate injection of air or something else into [Child A]'s circulation a minute or two prior to deterioration," Mr Johnson told the court. Only Letby was present. Another medical expert said the cause was "not some natural disease process, but a dose of air "deliberately administered". An independent pathologist described the cause of death was 'unascertained', in that there was nothing in the autopsy that pointed to why Child A had died, but the cause was most likely 'exogenous air administration through the longline or UVC'.
3:31pm: Said explanations are also backed up, the prosecution say, by an independent radiologist.
3:36pm: When interviewed by police regarding the circumstances over Child A's death, Letby said she had given fluids to Child A at the time of the change of shifts. She said within "maybe" five minutes, Child A developed 'almost a rash appearance, like a blotchy red marks on the skin'. She said she had wondered whether the bag of fluid "was not what we thought it was". In an interview in June 2019, Letby said she had asked for all fluids to be kept from the bag at the end to be checked, but the prosecution said there was was no record of her having made such a request. It was suggested by police that Letby had administered an air embolus. She replied it would have been very hard to push air through the line.
3:38pm: In a November 2020 police interview, police put to her that Letby had tracked the family of Child A on Facebook. She said she had no memory of doing so but accepted it if there was evidence on her computer doing so. The prosecution said there was evidence.
3:40pm: Count 2: Child B attempted murder Child B is the elder twin sister of Child A, born in June 2015. She required breathing support via a ventilator at birth. Attempts to fit an umbilical vein catheter (UVC) twice failed, so a long line (IV) was inserted for fluids to be administered successfully. Breathing support gradually lessened and Child B was stable.
3:44pm: A designated night-shift nurse was responsible for Child B. Shortly before midnight, the blood/oxygen levels had fallen to 75% and the Cpap nasal prongs were dislodged from Child B's nostrils. The nurse repositioned the prongs and the levels recovered. Just after midnight, Letby started a bag of liquid feed with Child B, with the nurse, through an IV line. At 12.16am Letby - while not Child B's designated nurse - took her blood gases. About 28 hours after her twin brother had died, at about 12.30am, Child B's alarm sounded and Letby had called the nurse to the child's incubator. Child B was not breathing.
3:47pm: A crash call was put out at 12.33am, and resuscitation began. The nurse noted purple blotches and white patches all over Child B's body, and the heart rate had dropped. In a witness statement three years later, Letby's colleague, the designated nurse for Child B, said she and Letby had been preparing antibiotics at the time of the collapse. After efforts to resuscitate Child B, Child B "recovered very quickly". A doctor subsequently found "loops of gas filled bowel". The prosecution say this was a finding replicated many times in the upcoming cases. Child B improved until being discharged the following month. Dr Dewi Evans concluded Child B was "subjected to form of sabotage" that night, the court hears.
3:49pm: Another medical expert said an airway obstruction would cause a "sudden desaturation and reduction in heart-rate", but would not account for the "florid change in skin colour and perfusion noted at the time". The medical expert said a "relatively quick recovery" would "only be explained by a dose of air...deliberately administered in the bloodstream".
3:51pm: A blood expert added "no blood disorder would account for the sudden deterioration suffered by [Child B]."
3:53pm: In police interview, Letby was asked about the circumstances regarding the connection of a liquid feed bag at 12.05am. She said she had looked at paperwork for the lipid syringe (an addition to the liquid feed bag to children not being given milk), and said the prescription was "not her writing" but "she had signed for it" and "ideally it should have been co-signed by somebody". The rules are that two nurses have to sign for things administered to a baby.
3:55pm: Letby told police she had conducted observations on Child B, but the other nurse was the allocated nurse. Letby also said it was the other nurse who had alerted her to the problem with Child B. In a June 2019 police interview, Letby said it was her signature on the blood gas record at 12.15am, just before Child B collapsed. The prosecution say this is an example of Lucy Letby signing the charts for a baby who was not her designated patient at a time just before the child collapsed.
3:59pm: In November 2020, Letby was asked by police about a handover sheet relating to Child B found at her home address in a search. The sheet showed she had been the designated nurse for two babies in a different room that night. Mr Johnson said: "Here you can see that we have twins who were born prematurely but in pretty good condition. "No one expected them to face grave problems, yet both suffered unusual symptoms within a short time of each other which in interview Lucy Letby said were similar. "The prosecution’s expert paediatricians say that the collapses and skin mottling were the result of air being injected into their bloodstream. "The first injection caused the death of [Child A], the second the dangerous collapse of his sister. "We say that there is no plausible alternative to an air injection [air embolus]. The fact that it happened in 2 cases just over 24 hours apart shows that these were no accidents. "Lucy Letby was the only person present [with Child A] at the time he collapsed...and was in the room when the same happened to [Child B]. "We also say that you are entitled to look at the evidence of what happened to [Child A and B] in the context of one, what Lucy Letby did to other children and two, most starkly, her having poisoned [two other children] with insulin."
4:00pm: The case is now being adjourned for Monday. The prosecution will continue outlining the case tomorrow.
Tuesday 11th October 2022
Chester Standard Live Reporting - Monday 10th to Wednesday 12th October AM
11:08am: We are hearing evidence on Child C's death. Dr Dewi Evans heard that infection was a "significant factor" in Child C's collapse, but could not adequately explain it. He had concerns about Child C's sudden deterioration. The cause of death was ‘widespread hypoxic/ischaemic damage to the heart/myocardium’ due to lung disease, with maternal vascular under perfusion as a contributary factor.
11:12am: As was the case with Child B, the prosecution say, Lucy Letby was not the designated nurse for Child C, a baby boy. Letby was assigned to look after a baby girl, and the leading nurse had to reinforce this assignment when, the prosecution say, Letby was 'ignoring her'.
11:13am: A medical expert concluded Child C was killed by air "deliberately put into the nasal gastric tube". The prosecution say this was a "variant or refinement of a theme Letby had started with the twins".
11:15am: The prosecution added an independent pathologist said the skin colour changes in Child C were likely caused by prolonged unsuccessful resuscitation. Child C had pneumonia, but the pathologist concluded Child C died as a result of having an excessive quantity of air injected into his stomach via the nasogastric tube (NGT).
11:19am: The court has heard Child C was being looked after by a nurse less qualified than Lucy Letby and had been given the responsibility as Child C was stable. That nurse had left to go to the nurses station in the hospital. While there, she heard Child C's monitor sound an alarm. Upon her return, Letby was already in the room, standing next to Child C's cot. It was the third baby to have suffered a serious deterioration in the matter of a few days, the court heard.
11:20am: Letby was the only nurse who had been on duty for all three collapse incidents for Child A, B and C.
11:22am: In police interview, Letby denied she had anything to do with Child C, other than with the resuscitation. She could not remember why she had ended up in nursery 1. In a second interview, asked about texts which had been found on her phone placing her in that room, Letby said that she might have been sending them from the nurses’ station and then gone into room 1 “to do something else”. She then agreed that she had been the only person in the room when Child C had collapsed.
11:24am: After finishing her shift, Letby searched on Facebook for Child C's parents. The prosecution say this would've been one of the first things she would have done after that night shift ended. Mr Johnson, for the prosecution, added Letby would have been the only adult in the room when Child C collapsed, as was the case with Child A, and was one of only two in the room when Child B collapsed.
11:25am: "What we are going to see as we progress is that Lucy Letby’s method of attacking the babies in the neonatal unit was beginning to develop," Mr Johnson tells the court.
11:27am: Child D - murder allegation from June 2015 Child D was a baby girl, born as 'full-term' (ie not premature). The court hears there is valid criticism for the hospital as the mother should have been given antibiotics to stave off infection, after her waters broke early, but she was not. Although born healthy, Child D "lost colour" and "became floppy" in her father's arms. She was put under observation as she was showing signs of respiratory distress, by grunting, and her temperature dropped.
11:29am: Child D was admitted to room 1 in the neonatal unit, placed into an incubator, and given oxygen therapy and antibiotics. She developed a very high temperature and a rise in her heart rate. She was intubated, and ventilated. She improved "significantly, but was still affected by her infection".
11:32am: Child D had catheters inserted and the levels of infection dropped. "All good signs," Mr Johnson tells the court. A designated nurse other than Letby was assigned care for Child D in room 1 on the night-shift, along with a different child in room 2. Letby was the designated nurse for the two other babies in room 1.
11:34am: On that night-shift, Child D collapsed three times. The first at about 1.30am, the second at 3am, and finally at 3.45am.
Mr Johnson: "On each occasion, those attending were struck by the sight of mottling, poor perfusion and brown/black discolouration to her skin, mainly over the trunk. "We've heard that sort of thing before, haven't we? "The prosecution say that this was another case of injecting a child via an IV air embolus."11:36am: At 1.15am, the designated nurse checked Child D, recording observations. At 1.25am, the designated nurse and Letby noted the starting of an infusion. An aspirate - drawing liquid through the nasogastric tube - is noted at 1.30am. At 1.29am a doctor noted "an unusual...spreading, non-blanching rash" on Child D.
11:41am: There is a note in Lucy Letby's records she was engaged in the care of a different baby at the time, but the prosecution say nursing notes suggest Letby and the designated nurse called the doctor to the room. The prosecution allege either the notes recorded were simply inaccurate, or Letby was setting herself up with an alibi in someone else's medical records. Child D was successfully resuscitated. At 2.40am, medication was administered by Letby and the designated nurse, who then left to another room. But Child D then collapsed at 3am. Letby was in the room, the designated nurse was not, and no-one else had a reason to be in the room.
11:43am: Child D was resuscitated again but, according to the prosecution, Letby "did not leave things there". At 3.20am, there is a record of Letby starting an infusion and Letby appears to have remained in the room, as a record shows her caring for another baby in the room at 3.30am. At 3.45am, Child D suffered her third and final collapse. CPR began and Child D was pronounced dead at 4.25am. The coroner gave the cause of death as "pneumonia with acute lung injury."
11:45am: Medical expert Dr Dewi Evans, the prosecution says, observed that a child "exhibiting a window of near recovery on two occasions followed by another collapse was not consistent with the fatal evolution of antenatal pneumonia." He added the "abdominal discolouration was indicative of air embolus".
11:48am: Another medical expert said the clinical status of Child D the previous night was not that of a deteriorating baby who would be dead a few hours later. She added the injection of '3-5ml per kilogram' of air would be sufficient to kill. Child D had been observed in distress prior to her death, and the medical expert added this would also be consistent with cases of air embolus (air injected into the system).
11:50am: The court is told none of the medical staff on duty that night had also been present for the collapses of Child A, B or C - other than Letby. For nursing staff, two of the nurses had been on duty for one each of the other collapses.
11:53am: Letby, in police interview, said she "cannot remember" how she got involved. She seemed to accept that she had administered medication with a syringe at 1.25am – 5 minutes before the first collapse. In a June 2019 police interview, she said she could not remember calling back the doctor when Child D collapsed, but it was possible she had. It was put to Letby, in November 2020, that she had searched for the parents of Child D on Facebook. She said that she could not recall but accepted she had done so. She said she could not explain why she had done it. The prosecution said: "We suggest that if you searched for that family of a baby who you had seen die you would know and remember why you had done it."
11:54am: Letby was asked about a text message in which she had referred to "an element of fate" being involved. She said that it was 'fate that babies get unwell sometimes' but that she would have to know the context. The prosecution say for Child D, her bad luck, or fate, was the fact Letby was working in the neonatal unit.
11:55am: The prosecution add all of Children A-D were not expected to have serious problems, but only one of them survived - and only Letby was "the constant presence".
11:59am: The court has adjourned for a short break. The prosecution will resume outline their case, talking about the circumstances of Child E's death, shortly.
12:14pm: The court is now resuming.
12:16pm: Child E - murder allegation Child E, a boy, was born premature in July 2015. The prosecution say this is the twin brother of the child poisoned with insulin. Child E was born, weighing less than 3lbs. He was given oxygen, then weaned to air, and transferred to nursery 1.
12:19pm: The court hears Child E was at risk of a serious gastro-intestinal disorder, NEC, and was started on antibiotics, IV fluids and caffeine. He had a nasogastric tube inserted. Fluids were inserted the following day via a long line. He had a "mild, transient high blood sugar" was was corrected with "a very low dose of insulin", then given tiny quantities of milk the following day, every two hours. The following day after that, he had two small vomits and air was aspirated, but otherwise the feeds were well tolerated and increased incrementally to 2ml every 2 hours. The nursing notes indicated he was stable, on a tiny dose of insulin to correct high blood sugar.
12:20pm: At 9pm on August 3, 2015, the mother decided to visit her twin sons, and "interrupted Lucy Letby who was in the process of attacking Child E", the prosecution say, although the mum "did not realise it at the time".
12:21pm: Child E was 'acutely distressed' and bleeding from the mouth. The mum said Letby attempted to reassure her the blood was due to the NGT irritating the throat. "Trust me, I'm a nurse," Mr Johnson told the court.
12:22pm: Letby said the registrar would be down to review Child E, and urged her to return to the postnatal ward. The mum called her husband when she got to the labour ward, in a call lasting four minutes and 25 seconds, at 9.11pm. Letby made a note in Child F's records (Child F being the twin of Child E), "after she had got rid of" the mum, Mr Johnson said. The next time the mum visited Child E, he was in terminal decline.
12:28pm: The prosecution say the mum was "fobbed off" by Lucy Letby. Two records are made at 4.51am, after Child E had died. The later note records: "Mummy was present at the start of shift attending to cares. Visited again approx. 22:00. Aware that we had obtained blood from his NG tube and were starting some different medications to treat this. She was updated by Reg xxxxx and contained [Child E]. Informed her that we would contact her if any changes. Once [Child E] began to deteriorate midwifery staff were contacted. Both parents present during resus." The prosecution say Letby's note suggests the mum was present at the start of the shift (7.30pm-8pm), and returned at 10pm, when "neither is true". The prosecution say 9pm was an important time, as it was the time Child E was due to be fed, by his mother's expressed breast milk. The mum said that is why she attended at 9pm. "She was bringing the milk". The phone call at 9.11pm to her husband also fits the mum's timing, the prosecution add.
12:29pm: Letby's notes also show: "prior to 21:00 feed, 16ml mucky slightly bile-stained aspirate obtained and discarded, abdo soft, not distended. SHO [Senior House Officer] informed, to omit feed." The prosecution say the nursing notes made are false, and fail to mention that Child E was bleeding at 9pm. They mention a meeting that neither the registrar or the mother remember.
12:35pm: A record of feeds - a feeding chart - is shown to the court. At 9pm, Letby has recorded information to detail the volume of fluids given via the IV line and a line in Child E's left leg, and the 9pm feed is 'omitted'. In the 10pm column is '15ml fresh blood'. The SHO said he had no recollection of giving advice to omit the 9pm feed. He was on the paediatric ward most of that night, until Child E entered a terminal decline. He believes the only time he had anything to do with Child E was in a secondary role to the registrar in an examination at 10.20pm.
12:37pm: The registrar recalled being told Child E had suffered a blood-flecked vomit. He does not recall seeing any blood on Child E's face, but regarded the presentation as undramatic. But "around half an hour to an hour later there was a large amount of fresh blood which had come up" Child E's tube.
The prosecution said: "This was the first indication of any serious problem so far as the medical staff were concerned.
"There was a further loss of 13 mls of blood at 23:00 hrs."
"13mls may not sound much, but [the doctor] had never seen a small baby bleed like this." This was the equivalent to 25 per cent of Child E's blood volume, a figure which the prosecution say is an under-estimate in context.12:41pm: The prosecution add that at 11.40pm, Child E suffered a sudden desaturation. His abdomen "developed a striking discolouration with flitting white and purple patches." CPR was started, but Child E "continued to bleed". Although Letby was participating in the resuscitation of Child E, she co-signed for medication given to another baby in room 4. Child E was pronounced at at 1.40am. The on-call consultant said Child E was a high-risk infant who had shown signs of NEC. The parents did not wish to have a post-mortem, the consultant did not deem one necessary, and the coroner's office agreed. The prosecution say: "As subsequent reviews have established – that was a big mistake."
12:42pm: Dr Dewi Evans said Child E's death "was the result of a combination of an air embolus and bleeding which was indicative of trauma". The air embolus was "intentionally introduced" into Child E's bloodstream via an IV line "to cause significant harm".
12:43pm: Medical expert Dr Sandie Bohin agreed the cause of death was air embolus and acute bleeding. She concluded that the cause of the bleeding was unknown but acknowledged “fleetingly rare” possible natural causes that could not be ruled out in the absence of a post-mortem. Dr Bohin concentrated on the abdominal discolouration and concluded that air was deliberately introduced via an intravenous line.
12:46pm: The court is reminded by the prosecution that, once again, only Lucy Letby was "the constant presence" for all of the collapses in Children A-E.
12:52pm: In police interview, Letby said he could remember Child E and he was "stable" at the time of the handover, with nothing of concern "before the large bile aspirate". She said she and another member of staff had disposed of the aspirate and the advice was to omit the feed. She said Child E's abdomen was becoming fuller and there was a purple discolouration, so had asked a doctor to review Child E. She said she had got blood from the NG tube. She was asked about the 10pm note and said if there had been any blood prior to the 9pm feed, "she would have noted it". She said it was after 9pm that the SHO had reviewed Child E but could not recall if it was face-to-face or over the phone. She said she could remember the mum leaving after 'the 10pm visit'.
In a June 2019 interview, she was pressed over a conversation with the SHO. She said she had no independent memory of it. She said she could not remember the mum coming into the room at 9pm with milk, nor Child E being upset, with blood coming from the mouth. She said she would not have told the mum to go back upstairs. "We have a stark contrast between what the mum says and what Lucy Letby says," Mr Johnson tells the court. "You know he was due to be fed...breastmilk. You know, we say, that is why [the mum] was there. "This has been wiped out of the records, by Lucy Letby, because she knows the consequences of [the mum] being right about this."
12:54pm: In a November 2020 interview, Letby is asked why she had sent a text referring to Child E had queried whether he had Down Syndrome. She said she could not remember whether there had ever been any mention of Downs in the medical notes. The prosecution say Lucy Letby "took an unusual interest" in the family of Child E. She did social media searches on the parents two days after Child E’s death, and on August 23, September 14, October 5, November 5, December 7, and even on December 25. The prosecution say there were further searches in January 2016.
12:55pm: The court is now adjourning for the lunch break. It will resume later this afternoon, discussing the circumstances surrounding the collapse of Child F - Child E's twin brother. The prosecution allege this was an attempted murder by insulin poisoning.
2:04pm: The court will shortly be resuming with its afternoon session.
2:20pm: Mr Johnson will now be giving details of the prosecution's case for Child F, the twin brother of Child E.
2:21pm: Child F - attempted murder allegation (by method of insulin poisoning) The prosecution say Child F was marginally the younger of the twins, and he required some resuscitation at birth and later intubated, ventilated and given a medicine to help his lungs.
2:22pm: He was recorded as having 'high blood sugar' so was prescribed 'a tiny dose of insulin'. He had his breathing tube removed and was given some breathing support. Child F had small amounts of breast milk and given fluid nutrients via a long line.
2:24pm: If it is known in advance that a baby cannot have milk and needs to be fed fluids then the TPN bag is prepared by the Aseptic Pharmacy Unit (APU) at the CoCH on receipt of a prescription. The pharmacy bag is delivered back to the ward and is bespoke, prepared for an individual patient. "If, for whatever reason, there is no need for a TPN bag, there are a couple of stock bags...kept in reserve."
2:27pm: "As a matter of practice", insulin is "never" added to a TPN bag. Insulin is "given via its own infusion, usually in a syringe which delivers an automatic dose over a period of time". The prosecution adds insulin is not added to a TPN bag as it would "stick to the plastic - or bind" to the bag, making it difficult to accurately give a reliable dose.
2:28pm: Early on August 4, Child E had died. Later that day, the pharmacy received a prescription for a TPN bag for Child F, the twin brother. A confirmation document was printed, at 12.32pm, for Child F. The pharmacist produced a handwritten correction to say it was to be used within 48 hours of 11.30pm that day.
2:30pm: The TPN bag was delivered up to the ward at 4pm that day. On that night shift, the designated nurse for Child F, in room 2, was not Letby. Letby had a single baby to look after that night, also in room 2. There were seven babies in the unit that night, with five nurses working.
2:33pm: Letby and the designated nurse signed the prescription chart to record the TPN bag was started and administered via a long line at 12.25am. A TPN chart is a written record for putting up the bags, and was used for Child F. It includes 'lipids' - nutrients for babies not being given milk. Letby signed for the TPN bag to be used for 48 hours.
2:40pm: There are two further prescriptions for TPN bags, to run for 48 hours. Following the conclusion of a Letby night-shift, after the administration of a TPN bag Letby had co-signed for, a doctor instructed the nursing staff to stop the TPN via the longline and provide dextrose (sugar to counteract the fall in blood sugar), and move the TPN to a peripheral line while a new long line was put in. All fluids were interrupted at 11am while a new long line was put in.
2:48pm: Child F's blood glucose increased, before falling back. A new bespoke TPN was made for Child F, delivered at 4pm. The prosecution say this could not have been the same one fitted to Child F at noon that day which would have been either a bespoke bag which Lucy Letby co-signed for, or a stock bag from the fridge. Mr Johnson said Child F's low blood sugar continued in the absence of Lucy Letby. Child F's blood sample at 5.56pm had a glucose level was very low, and after he was taken off the TPN and replaced with dextrose, his blood glucose levels returned to normal by 7.30pm. He had no further episodes of hypoglycaemia. "These episodes were sufficiently concerning" that medical staff checked Child F's blood plasma level. The 5.56pm sample recorded a "very high insulin measurement of 4,657". Child F's hormone level of C-peptide was very low - less than 169. The combination of the two levels, the prosecution say, means someone must have "been given or taken synthetic insulin" - "the only conclusion". "That, we say, means that somebody gave Child F synthetic insulin - somebody poisoned him."
2:49pm: "All experienced medical and nursing members of staff would know the dangers of introducing insulin into any individual whose glucose values were within the normal range and would know that extreme hypoglycaemia, over a prolonged period of time, carries life threatening risks. "No other baby on the neonatal unit was prescribed insulin at the time."
2:51pm: Mr Johnson: "To give Child F insulin someone would've had to access the locked fridge, use a needle and syringe to remove some insulin, or, if they didn't do it that way, go to the cotside and inject the insulin directly into the infant through the intravenous system, intramuscular injection, or - and this is what we say happened - via the TPN bag."
2:55pm: Medical experts Dr Dewi Evans and Dr Sandie Bohin said the hormone levels were consistent with insulin being put into the TPN bag prior to Child F's hypoglycaemic episode. "You know who was in the room, and you know who hung up the bag," Mr Johnson told the jury. Professor Peter Hindmarsh said the insulin "had to have gone in through the TPN bag" as the the hypoglycaemia "persisted for such a long time" despite five injections of 10% dextrose. Professor Hindmarsh said the following possibilities happened. That the same bag was transferred over the line, that the replacement stock bag was contaminated, or that some part of the 'giving set' was contaminated by insulin from the first TPN bag which had bound to the plastic, and therefore continued to flow through the hardware even after a non-contaminated bag was attached. "There can be no doubt that somebody contaminated that original bag with insulin. "Because of that...the problem continued through the day."
3:00pm: Letby was interviewed by police in July 2018 about that night shift. She remembered Child F, but had no recollection of the incident and "had not been involved in his care". She was asked about the TPN bags chart. She said the TPN was kept in a locked fridge and the insulin was kept in that same fridge. She confirmed her signature on the TPN form. She had no recollection of having had involvement with administering the TPN bag contents to Child F, but confirmed giving Child F glucose injections and taken observations. She also confirmed signing for a lipid syringe at 12.10am, the shift before. The prosecution say she should have had someone to co-sign for it.
"She accepted that the signature tended to suggest she had administered it."
"Interestingly, at the end of this part of the interview she asked whether the police had access to the TPN bag that she had connected," Mr Johnson added.3:02pm: In a June 2019 police interview, Letby agreed with the idea that insulin would not be administered accidentally. In November 2020, she was asked why she had searched for the parents of Child E and F. She said she thought it might be to see how Child F was doing. She was asked asked about texting Child F’s blood sugar levels to an off- duty colleague at 8am. She said she must have looked on his chart.
3:03pm: Mr Johnson: "The fact it was done through the TPN bag tells you it wasn't a mistake - whoever was doing it was to avoid detection. "Only a few people had the opportunity. "We suggest there is only one credible candidate for the poisoning. The one who was present for all the unexpected collapses and deaths at the neonatal unit."
3:06pm: Child G - attempted murder allegations (three attempts) Mr Johnson said Child G, born in May 2015 at Arrowe Park Hospital, was a baby girl and born very premature, weighing 1lb and 2oz.
3:07pm: Child G suffered bleeding on her lungs and had nine blood transfusions, with a number of 'septic' or 'suspected septic' episodes requiring antibiotics, but improved and was transferred to the Countess of Chester Hospital's neonatal unit in August, and was clinically stable, being fed expressed breast milk.
3:09pm: On the night in September, Child G was in nursery 2, with a designated nurse (not Letby). There were seven babies in the unit, with five nursing staff. Letby's assigned baby that night was in nursery 1.
3:10pm: It was a milestone night for Child G and nurses marked the occasion with a small celebration. Child G was being fed every three hours alternately by bottle and nasogastric tube.
3:11pm: At 2am, a feed had shown minimal aspirated of partially digested milk. The nurse took her scheduled one-hour break. "Nothing is recorded on who was asked to keep an eye on Child G," Mr Johnson said.
3:14pm: At 2.15am, the shift leader said she was sat with Lucy Leader when she heard Child G vomiting, along with Child G's monitor alarm going off. They ran into her nursery. Child G had vomited violently and suffered a collapse. The prosecution said medical records suggest the shift leader nurse's memory of being with Lucy Letby for a period of time before this event cannot be accurate.
3:17pm: The prosecution say despite Child G's stomach being 'pretty much empty' prior to her feed, 45mls of milk was aspirated from her NGT. But, the prosecution say, 45mls of milk had been administered for her feed, which then did not explain what accounted for the vomit. Subsequent x-rays showed air in the abdomen and intestines. Child G suffered further deteriorations. During intubation, a doctor noticed bloodstained fluid from the trachea - something the prosecution say was consistent with that seen in other collapses in the case so far.
3:19pm: At 6.05am, following a further desaturation, 100mls of air was aspirated from the NG tube. When the tube was removed, the registrar noted thick secretions in her mouth "and a blood clot at the end of her breathing tube". There were also signs of infection. Child G was transferred to Arrowe Park, before returning to the Countess neonatal unit just over a week later. During that time, Child G "recovered remarkably".
3:20pm: Five days after her return to the Countess, Child G was due to receive her immunisations, such was her improved condition. A team of nurses came on the day shift that day, Lucy Letby being among them. Letby was Child G's designated nurse that day.
3:23pm: Child G was fed with 40ml via a NG tube by Letby at 9.15am. At about 10.20am, Child G had projectile vomited twice and went apnoeic for several seconds, the court is told. Child G's blood saturations fell to 30%. The same problem she had faced two weeks prior. A nurse took over the care from Letby at 11.30am, as Letby was looking after two other children in room 4. The nurse took all the observations and noted Child G was connected to a 'Masimo monitor' - which measures oxygen saturations and heart rate levels. It is a device which stays on and cannot be turned off by a baby.
3:25pm: At 3.30pm a consultant doctor was called to cannulate Child G. Privacy screens were erected and Child G was on a trolley, with the monitor still attached. The nurse went to care for another baby. The consultant doctor said he "could not recall" if Child G's monitoring equipment was switched off during the cannula fitting, but "it is his practice to transfer the sensor from one limb to another or if temporary detachment is required to reattach the monitor as soon as possible." He added if Child G was not stable he would not have left her.
3:26pm: After the doctors had gone, the nurse responded to Lucy Letby's shout for help. When she attended, Child G's monitor had been switched off (power was off). Child G was struggling to breathe. Letby was giving ventilation breaths. Child G responded to treatment.
3:28pm: In a text sent by Letby to a colleague, she wrote Child G: "...looked rubbish when I took over this morning then she vomited at 9 and I got her screened … mum said she hasn’t been herself for a couple of days”. But the prosecution said Child G had been due to have her immunisations, something which would not have been contemplated if Child G had not been well. The prosecution say Child G had vomited because she had been given excessive milk and air. A subsequent MRI scan revealed neurological changes and, in August 2016, it was revealed Child G had suffered "irreversible brain damage".
3:29pm: The overfeeding "doesn't happen by accident," Mr Johnson told the court. He added similar cases will be heard with other babies.
3:30pm: Mr Johnson: "Someone had switched off the monitor when Child G collapsed, and she was 'discovered' by Lucy Letby".
3:35pm: In police interview, Letby said she remembered the nurse had been on her break when the incident happened with Child G in nursery 2. She could not remember who had been assigned to look after her. Letby suggested the excess air in Child G after the vomiting was the result of some sort of infection, or as a consequence of the vomiting. She said she had withdrawn the 45mls of milk after that episode, and air had come with it, and she had seen Child G vomiting. She said she did not know why she had gone into the room, but it was possible it was as a result of hearing Child G vomiting. Letby 'vaguely' recalled the day Child G vomited after her return to the hospital, accepting she had been the designated nurse. She had no recollection of Child G vomiting. In a subsequent interview, Letby accepted there were only two alternatives to the first vomiting incident - that Child G had been fed far more than should have been, or she had not digested her earlier feed. She accepted that the clear inference to be drawn was that Child G had been given excess milk and air via the NGT. She denied responsibility for either of those eventualities.
3:37pm: For the second incident, Letby denied either over-feeding or injecting air into Child G's stomach. In November 2020, Letby denied to police that she had switched off the Masimo monitor. She was asked about Facebook searches carried done on the day of the second vomiting incident that Letby looked up the parents of Child G. She said "she had no recollection of them".
3:39pm: The prosecution say that, within a minute or two of looking at the mother of Child G on Facebook, she then looked at the mums of two other babies listed in the charges. One was the mum who, the prosecution said, "interrupted the attack" by Letby on Child E.
3:41pm: Mr Johnson: "The practice of the nurses on the NNU was to use the NGT to check whether an infant had an empty stomach before feeding. That was done in Child G’s case – nothing came up which means there was nothing in her stomach. "She was then fed and her designated nurse went on a break. 15 minutes later Child G produced projectile vomits of such force that they left the cot and landed on the floor and nearby chair. "Child G collapsed and stopped breathing. An amount of feed was aspirated from her NGT equal to what she had been given about 15 minutes earlier together with lots of air. "There was a similar episode a few weeks later. "These were not naturally occurring, or random events; they were deliberate attempts to kill using a slightly different method by whilst Lucy Letby sought to give the appearance of chance events in the neonatal unit at the Countess of Chester Hospital." The court is now adjourning for today. The prosecution case will resume its opening tomorrow (Wednesday).
Wednesday 12th October 2022
Chester Standard Live Reporting - Monday 10th to Wednesday 12th October AM
Chester Standard Live Reporting - Wednesday 12th October PM
10:34am: We are into day three of the prosecution opening in the Lucy Letby trial. The court shall hear the prosecution's version of events which led to the collapses of Child H.
10:35am: Child H - attempted murder allegation (twice) Child H was born in September 2015 and had breathing difficulties shortly after birth. She was transferred to neonatal unit nursery room 1.
10:37am: Independent experts say there was an "unacceptable delay" in intubating her and administering a protein which helps the lungs, which the prosecution say means the case is complicated by "sub-optimal treatment" at the hospital. Additionally, Child H "was put on a ventilator she was not paralysed; she was also left with butterfly needles in her chest for prolonged periods which may have punctured her lung tissues and contributed to further punctured lungs."
10:44am: The prosecution say Letby attempted to kill Child H on September 26 at 3.24am, and on September 27 at 12.55am. Mr Johnson said Child H had previously deteriorated on the night of September 23 and required ventilator support and intubation, followed later by oxygen support. The court hears Child H responded to intervening treatment, but desaturations were "frequent" and "significant". Mr Johnson said all but two events could be explained medically and responded to with routine resuscitative measures. The two events - in the early hours of September 26 and 27, were "uncharacteristic" and required CPR.
10:49am: Letby was on duty for both those night shifts, and was the designated nurse for Child H. That night, Child H was given a blood transfusion. At 2.15am, medical notes by a doctor showed a re-accumulation of her left-sided pneumothorax. A further chest drain was inserted to relieve the pressure. The ICU chart shows that Letby recorded having given Child H a dose of morphine at 1.25am and a dose of saline at 2.50am. The saline bolus was set to run for 20 minutes and would therefore have ended at 3.10am. Lucy Letby would have had the cover of legitimacy for accessing Child H's lines just before she collapsed again. At 3.22am, Child H collapsed and required CPR. The attending doctor said the cause was unclear. He concluded the episode was 'hypoxia' (shortage of oxygen).
10:53am: Letby made notes at 4.14am, recording a lowering of the heart rate at 11.30pm which required treatment. She recorded the additional chest drain and a blood transfusion at 2am. Of the collapse at 3.22am, she recorded: "profound desaturation and colour loss to 30%, good chest movement and air entry, colour change on CO2 detector, Neopuff commenced in 100% oxygen and help requested. Serous fluid +++ from all 3 drains, became bradycardic. Drs crash called and resus commenced as documented" At 5.21am, Letby recorded a conversation between herself, the attending doctor, and Child H's parents.
10:54am: During the following day, Child H was relatively stable. A different nurse was the designated nurse for Child H, still in room 1, on the night of September 26. Letby was also on duty.
10:56am: The designated nurse 'could not recall' if she had taken a break during the shift, but there would have been times she would have gone out of the room to get a drink or retrieve something from a cupboard. Letby was looking after a child in room 2. Child H suffered "two sudden and unexpected episodes of profound desaturation at 12.55am and 3.30am."
10:58am: The registrar responded to the emergency calls and on one occasion, saw Letby administering treatment, and took the history from her, assuming she was the designated nurse. The nurse noted 'pink tinged secretions' around Child H's mouth. The prosecution say this was a similar finding to that found on three other babies in the case so far.
11:04am: The nurse noted a 'profound desaturation' - a "profound drop in Child H's blood", despite air going into the lungs and carbon dioxide coming out. Both collapses at 12.55am and 3.30am had "no known cause". Child H was transferred to Arrowe Park Hospital at 5.25am, and was stabilised en route in the ambulance. Her mother, who was with her spoke of a "dramatic improvement" as soon as Child H got to the hospital. Child H returned to the Countess of Chester Hospital and the rest of her time was uneventful before being discharged. The court hears she had not suffered any permanent consequences.
11:06am: The prosecution says medical expert Dr Dewi Evans said there was "no obvious explanation" for Child H's deterioration in those two early-morning collapses. Dr Sandie Bohin "expressed concern" at those events, and the collapses "were more significant than the others, for which there are obvious clear medical explanations". She was also "critical of the way the chest drains were inserted and managed".
11:09am: Letby was interviewed in 2018 by police. She confirmed she had remembered Child H because she had chest drains - which the court hears are a fairly rare thing these days. For the second incident, Letby said she had not been the designated nurse so assumed she had not been caring for Child H. She identified her signatures on two medicine administrations. In 2019, she identified her signature on more documents. In this interview, she told police she had not been the designated nurse but had been giving her treatment at the time Child H collapsed.
11:11am: On October 5, 2015, the prosecution say Letby searched for the mum of Child H, the father of Children E and F, and the mother of Child I. It was her day off. Mr Johnson said: "We say this has to be looked in the context of everything else. "We say it is more than an innocent coincidence that once Child H was moved out of the Countess of Chester Hospital she had no further problems."
11:12am: Child I - murder allegation Child I was born in Liverpool Women's Hospital, premature, on August 2015.
11:13am: The prosecution say Letby made four attempts to kill Child I, succeeding on the fourth attempt.
11:14am: Child I was born, weighing 2lbs 2oz, but in good condition. She was intubated and ventilated, then supported by CPAP, and fed through a nasogastric tube. In the first few weeks, she had "a few problems", but "all were resolved".
11:19am: Child I, by late September, had diminished clinical concerns, and no breathing problems. For what the prosecution say was the first attempt, Letby was on a 'long day' shift (8am-8pm) on September 30. She was Child I's designated nurse in room three. According to Child I's mum, Letby expressed concern about the child and indicated Child I would be reviewed by a doctor. When she made a nursing note, Letby "reversed the concern", and said it was the mum who had raised a concern about the abdomen, saying it was "more distended to yesterday" and Child I was "quiet...not on monitor but nil increased work of breathing”.
11:26am: A review took place at 3pm - over an hour after these notes. Child I appeared mottled in colour with a distended abdomen and prominent veins. A feeding chart showed 35mls was given to Child I when asleep, but Letby had recorded Child I as "handling well and waking for feeds". At 4pm, Letby recorded feeding Child I 35mls of expressed breast milk via the NGT. An emergency crash call was called at 4.30pm as Child I had vomited, desaturated, her heart-rate had dropped and she was struggling to breathe. Her airway had to be cleared and she was given breathing support, and Child I was transferred to room 1.
11:27am: An x-ray at 5.39pm revealed a "massive amount of gas in her stomach and bowels" and her lungs appeared "squashed" and "of small volume". The prosecution say air had been injected into the NGT to give a 'splinted diaphragm'.
11:29am: A doctor recorded Child I had suffered a 'respiratory arrest' at 4.30pm, struggling to breathe, she was pale and distressed, and the abdomen was 'distended and hard'. The NGT was aspirated and produced 'air+++ and 2mls of milk', after which Child I improved. The prosecution says this is at odds with the 35mls of milk Child I was fed with at 4pm.
11:30am: The prosecution say "removed from the orbit of Lucy Letby," Child I's condition improved.
11:32am: Child I continued to improve and was in nursery room 2 on the night of October 12 by a designated nurse different to Letby. Letby was looking after a baby in room 1. Child I was being bottle fed every 4 hours, and at 1.30am took a 55ml bottle of breast milk. At 3am, the designated nurse left the nursery temporarily and said she asked either Letby or another colleague to listen out for Child I.
11:36am: The designated nurse, records show, helped another colleague with something in room 1. The prosecution say it is more likely the nurse would have asked Letby to look out for Child I. Upon the designated nurse's return to room 2, Letby was "standing in the doorway of the room" and Letby said Child I "looked pale". The designated nurse switched on the light and saw Child I was "at the point of death". She later recalled the child was breathing about 'once every 20 seconds'. The prosecution says the jury should consider how Lucy Letby could see a child was looking pale when the room was darkened at 3.20am, with minimal lighting.
11:39am: The prosecution say the nurse's recollection is right, as Lucy Letby made a note at the end of her shift at 8.10am: '[Child I] noted to be pale in cot by myself at 03:20hrs … apnoea alarm in situ and had not sounded. On examination [Child I] centrally white, minimal shallow breaths followed by gasping observed.'
11:42am: The registrar was called to the unit at 3.23am. On arrival, he saw nurses giving Child I full CPR. The notes suggest he had to reposition the ETT. A consultant doctor administered adrenaline, intubated and ventilated Child I. An X-ray showed gross gaseous distention throughout the bowel and signs of chronic lung disease of prematurity (CLD). Child I, the prosecution say, had the same problem that she had when Letby had fed her on September 30. The medical team felt that the abdominal distention had affected her ability to expand the chest and in turn caused desaturation. Both nursing and medical staff commented on a bruised like discolouration to the right of the sternum. They assumed this was the result of chest compressions. The category of nursing care was raised a level. "Ironically," the prosecution say, Letby was made the designated nurse, as she was more qualified.
11:43am: Medical notes showed the ETT had been "displaced" and, at 4.25am, the NGT was "curled in the oesophagus", which the prosecution say would have prevented release of the pressure created by excess air in the stomach.
11:45am: For what the prosecution say was the third attempt, Letby had responsibility for Child I on the night of October 13. Both Letby and a doctor recorded Child I had increasing abdominal distension, discolouration to the right and sensitivity to touch between 5am and 5.55am. The X-ray taken at 6.05ams showed widespread gaseous distention sufficient to splint the diaphragm. This prevented her from breathing properly. Child I had the same problem as before.
11:47am: At 7am, CPR was required as Child I had a 'significant desaturation'. The doctor recorded, at 7.10am: "desaturating again despite good AE (air entry), chest wall movement and negative cold light (i.e. no pneumothorax) … at about 7.45am HR (heart rate) below 60. CPR initiated… [various boluses given] … capnography positive. Chest wall movement and equal AE noted…” The prosecution says Child I was "brought back from the brink of death right at the end of the shift, at 7.58am".
11:48am: Letby noted at 8.43am: "At 05:00hrs abdomen noted to be more distened (sic) and firmer in appearance with area of discolouration spreading on right hand side. Veins more prominent … gradually requiring 100% oxygen. Blood gases poor as charted …. nil obtained from NG tube throughout. Continued to decline. Re intubated at approx. 07:00 – initially responded well … resuscitation commenced as documented in medical notes. Night and day staff members present” That was, the prosecution say, the third attempt at murder.
11:49am: Child I was transferred to Arrowe Park Hospital. She had an episode of bradycardia and desaturations after which she quickly stabilised. The prosecution say once again, a child had recovered quickly out of the care of Letby. Child I was transferred back to the Countess of Chester Hospital on October 17.
11:51am: On the night of October 22, Letby was on a night shift, with a different nurse being the designated nurse for Child I. Between 8pm and Child I's collapse, the only entry Letby made in any child's records was those in her charge in room 3. The prosecution say it was, from her records, a slow night for her.
11:53am: Just before midnight, Child I became unsettled. Letby and another nurse attended to her but Child I collapsed and required CPR. The on-call registrar noted Child I had a mottled blue appearance of the trunk and peripheries. After 5 minutes of CPR, Child I's saturation rate returned to 100% and she recovered to the point of 'rooting' - ie a sign of hunger, and was 'fighting the ventilator' - ie trying to breathe independently. The ET tube was removed at 12.45am.
11:54am: At 1.06am a nurse, having left the nursery temporarily, responded to Child I's alarm and saw Lucy Letby at the incubator. Child I was very distressed and wanted to intervene, but Letby assured her that they would be able to settle the baby. "Don't worry - we will sort it out," Mr Johnson tells the jury. Child I then collapsed.
11:57am: The on-call doctor arrived and resuscitation attempts were made. Purple and white mottling were noted on Child I's skin. All resuscitative efforts were unsuccessful and treatment was withdrawn at 2.10am, and Child I was pronounced dead at 2.30am. In the immediate aftermath, Child I's parents were taken to a private room. As the mum bathed her recently deceased child, Lucy Letby came into the room and, in the words of the mum, "was smiling and kept going on about how she was present at [Child I']s first bath and how much [Child I] had loved it.”
11:58am: The cause of death was given by the coroner as Hypoxic ischaemic damage of brain and chronic lung due to prematurity and 1b. Extreme prematurity. All loops of bowel showed significantly dilated lumen due to increased air content – in layman’s terms they were expanded like a partially inflated balloon. There was no sign of NEC (bowel necrosis) or any other bowel problem. The prosecution say there were signs of "earlier hypoxic ischaemic damage – in other words, the earlier attempts to kill her had caused brain damage resulting from a shortage of oxygen."
12:03pm: Medical expert Dr Dewi Evans said he believed the apnoea monitor might have been switched off on October 13 for child I, and the deliberate administering of a large bolus of air into Child I's stomach via her NG tube on October 22/23. In police interview, Letby said she could not remember the circumstances of September 30, and had taken over the care of Child I after the child had an "episode". She said she had no recollection of the events surrounding Child I's death, and said the child had been returned from Arrowe Park Hospital too quickly. In June 2019, she was asked about a sympathy card she had sent to the child's parents. She said it was not normal to do so - and this was the only time she had done so. She accepted having an image of that card on her phone. She was asked about the October 13 incident and challenged the nurse's account, adding: "Maybe I spotted something that [the nurse] wasn't able to spot", as she was "more experienced". She was asked why she had searched for the parents' details on Facebook. She said she did not recall doing it.
12:04pm: The prosecution say Child I "was doing well by the time Lucy Letby got her hands on her. "What happened...followed the pattern of what happened to others before and what has yet to happen to others. "All of a sudden out of nowhere came vomiting, breathing problems and critical desaturations. "It was persistent, it was calculated, and it was cold-blooded."
12:06pm: The court is now adjourning for a short break, and will resume with the prosecution's version of events surrounding Child J, a baby girl they say was the victim of attempted murder.
12:24pm: Child J - attempted murder charge Child J, a girl, was initially stable but it was discovered she had a necrotic and perforated bowel. The prosecution say he really did have NEC. She was transferred to Alder Hey for surgery to fit her with a stoma bag.
12:27pm: Child J 'recovered well' and was taken to the Countess of Chester Hospital on November 10, 2015. She had a relatively rare type of intravenous line fitted, a 'Broviac line'. On November 16, medical notes referred to her as being well. But on November 27, she suffered an unexplained collapse in the early hours. Letby was on duty.
12:28pm: Before she went to work for that shift, Lucy Letby exchanged text messages with one of her colleagues. The prosecution say It seemed that she was not happy with working conditions and she referred to the difficulties of looking after the babies who just needed feeding support. Child J was one of those. The prosecution add that it appeared working in such nurseries was "not sufficiently stimulating for Lucy Letby".
12:33pm: Letby was in a different room to Child J, and was not the designated nurse, but 'got involved', by co-signing for medication at 12.02am. Letby's colleague was a band 4 nurse and not sufficiently qualified to give intravenous medication. After 4.40am, that nurse thought Child J became pale and mottled. She left the room for a short time, and upon her return another nurse was assisting Child J with breathing. The last thing Letby had recorded on notes was at 3am. There is data from the door system showing Letby coming in at 3.47am. The prosecution suggest Letby had been on a break during that time. Just after 5am, Child J suffered another desaturation and she was moved to the hugh dependency unit in room 2. The registrar was called and Child J was working hard to breathe, but had otherwise recovered well.
At 6.56am, Child J's alarm sounded and Letby was among those responding. A doctor attended and took control. He noted oxygen levels were 'unrecordable' and circulation 'poor'. There were symptoms of a seizure. Letby was in a different room to Child J, and was not the designated nurse, but 'got involved', by co-signing for medication at 12.02am. Letby's colleague was a band 4 nurse and not sufficiently qualified to give intravenous medication. After 4.40am, that nurse thought Child J became pale and mottled. She left the room for a short time, and upon her return another nurse was assisting Child J with breathing. The last thing Letby had recorded on notes was at 3am. There is data from the door system showing Letby coming in at 3.47am.
The prosecution suggest Letby had been on a break during that time. Just after 5am, Child J suffered another desaturation and she was moved to the hugh dependency unit in room 2. The registrar was called and Child J was working hard to breathe, but had otherwise recovered well. At 6.56am, Child J's alarm sounded and Letby was among those responding. A doctor attended and took control. He noted oxygen levels were 'unrecordable' and circulation 'poor'. There were symptoms of a seizure.
12:35pm: At 7.20am, Letby co-signed a chart for a 10% glucose infusion. At 7.24am, Child J collapsed again. The doctor assisted in resuscitating her. Child J recovered and the doctor could not explain what happened from the results of various tests taken. He considered the events unexplained.
12:37pm: Medical expert Dr Dewi Evans described the collapse at 7.11am as unexpected without any straightforward explanation. He said that it was “of concern and consistent with some form of obstruction of her airways, such as smothering”. The symptoms of a seizure suggested oxygen deprived to the brain. Child J has not suffered a seizure since.
Dr Evans added: "Whilst I have concerns...one cannot rule out the presence of infection, despite the normal inflammatory markers… at the time of the two collapse episodes…I note also the presence of the stoma which could be the source of the organism(s) that caused her systemic infections.”12:38pm: Dr Evans, in a follow-up statement, maintained 'airway obstruction' was the most likely cause of Child J's collapse. Dr Sandie Bohin concluded that the issue was not infection because there were no “soft signs” and the gradual deterioration which might be expected, but the collapse was "sudden" and had caused seizures.
12:39pm: In interview, Letby said she had little recollection of Child J, but remembered the Broviac line. She confirmed contact with Child J, but denied doing anything to cause her harm. In 2020, she was asked why she had searched Facebook for Child J's parents. She replied: "I don't remember doing that."
12:40pm: The prosecution said: "It is remarkable that on many occasions, when children who had suffered unexpected spectacular and life-threatening collapses were removed from her [Lucy Letby's] orbit, they had exceptional recoveries."
12:42pm: Child K - murder allegation Child K was born at the Countess of Chester Hospital in February 2016, very premature, and weighing only 692g. There was not time to deliver at a hospital for this type of maternity delivery care. Dr Ravi Jayaram, paediatric consultant, was present at her birth as a result.
12:45pm: Lucy Letby booked Child K on to the neonatal unit. Child had required help with breathing, but was stable and in as good a condition as a baby of that prematurity could be. Arrangements were made for Child K to transfer her to Arrowe Park Hospital. At 3.50am, Dr Jayaram was standing at the nurses’ station compiling his notes. Although he did not have a view into Nursery 1, Dr Jayaram was aware the designated nurse was not there, a fact backed up by door swipe data. Lucy Letby was the only nurse in room 1, alone with Child K. "Feeling uncomfortable with this because he was beginning to notice the coincidence between the unexplained deaths and serious collapses and the presence of Lucy Letby, Dr Jayaram decided to check on where Lucy Letby was and where Child K was."
12:46pm: "As he walked in, he could see Letby standing over Child K's incubator. He could see Child K's oxygen levels were falling. However, the alarm was not sounding and Lucy Letby was making no effort to help. "Dr Jayaram went straight to treat Child K and found her chest was not moving, he asked Letby if anything had happened to which she replied, “she’s just started deteriorating now”.
12:48pm: Dr Jayaram found Child K's breathing tube had been dislodged. Child K was very premature, and had been sedated and inactive. The tube had been secured by tape and attached to Child K's headgear.
Mr Johnson: "It's well recognised if you handle a child you can dislodge the tube accidentally, but any experienced staff member would recognise that. "Dr Jayaram was troubled as the levels were falling and Nurse Letby had been the only person in the room."12:52pm: The prosecution added: "On these monitors, all readings are set to default values in the neonatal unit. "Saturation levels falling to the 80s, is a serious issue and if the machine is working properly, it would have an alarm if the saturation levels fell to the 80s, as Dr Jayaram noticed. "There is an alarm pause button on the screen of the monitor - if you want to treat the child, you don't want the alarm going away. It will pause for one minute. "Bearing in mind the rate displayed on the monitor, Dr Jayaram estimates the tube would have been dislodged between 30-60 seconds, and that is on the assumption the alarm had been cancelled once." The court hears Dr Jayaram did not make a contemporaneous note of his suspicions or the alarm failing to activate.
12:56pm: Child K remained unwell and later died. Medical expert Dr Dewi Evans viewed Lucy Letby’s failure to summon help as soon as possible was unusual.
12:57pm: The prosecution allege that Lucy letby was trying to kill Child K when Dr Jayaram walked in.
1:00pm: In police interview, when Dr Jayaram's account was put to her, she said no concerns had been raised at the time. She said the alarm had not sounded. She said Child K was sedated and had not been moving around. She also did not recall either any significant fall in saturations or there being no alarm. She accepted that in the circumstances described by Dr Jayaram she would have expected the alarm to have sounded. she denied dislodging the tube and said she would have summoned help had Dr Jayaram not arrived, saying she was "possibly waiting to see if she self-corrected, we don’t normally intervene straight away if they weren’t dangerously low".
After the interviews - that suggestion made by Lucy Letby was referred to a nursing expert. Her view was that it was very unlikely that a nurse would leave the bedside of an intubated neonate unless they were very confident that the ET tube was correctly located and secure, the baby was inactive and then they would be away only briefly. The nurse dismissed the idea that a competent nurse would have delayed intervention if there had been a desaturation. Letby was found to have researched Child K's parents on Facebook in April 2018 - two years and two months after Child K had died. When asked about this, she said she did not recall doing so.
1:01pm: The court is now adjourning for the lunch break.
1:55pm: The trial of Lucy Letby is continuing this afternoon at Manchester Crown Court.
2:01pm: The trial is due to hear the prosecution's version of events surrounding the circumstances of Child L this afternoon.
2:15pm: The next case concerns twin brothers. Mr Johnson refers to Child L first. Child L - attempted murder (by insulin)
2:16pm: Child L was born in April 2016. It is the prosecution case Letby poisoned Child L, while also attacking Child M - the twin.
2:19pm: Child L's blood glucose level was noted to be low and he was treated with a dextrose infusion. His condition improved and he was stable by the day-time shift of April 9. Letby came on duty that day at 7.30am. By this time, the prosecution say, Letby was supposed only to be working day shifts because the consultants were concerned about the correlation between her presence and unexpected deaths and life-threatening episodes on the night-shifts.
2:21pm: In the hours that followed, Child L's glucose levels fell abnormally low. He was given additional doses of glucose, but they proved ineffective. The answers to these levels were found after a lab sample sent to the Royal Liverpool Teaching Hospital laboratory came back with results some time later. The results of the test were "grossly abnormal", but nothing was done about it as Child L had, by the time the results came back, returned to normal.
2:22pm: The reading was "at the very top of the scale" the equipment could measure, the court hears. There was no correspondingly high level of C-peptide: it was within the normal range. The only explanation for this anomaly is that what was being measured was synthetic insulin, which had not been prescribed to Child L but was stored and readily available in the neonatal unit.
2:25pm: The court is shown an 'infusion therapy prescription sheet', a written record of the dextrose bag fed to Child L. The bag was running from noon on April 8, when it had been set up an hour earlier by Letby and another nurse. Prosecutor Nicholas Johnson KC: "We say Lucy Letby added insulin to that bag of dextrose. She did it deliberately to kill [Child L]. "She had failed to kill [Child F] so gave an increased dose."
2:26pm: Letby had been present for the birth of Child L. She cared for him on his first day and the prosecution say would have been aware of his mild hypoglycaemia. Child L's blood sugar level remained "dangerously low" through the day. At 4.30pm, a new infusion bag was required and this was being applied when Child L, the twin brother, was being taken ill.
2:29pm: The prosecution says medical expert evidence is this was a case of insulin poisoning, administered intravenously via Child L's liquid feed. In police interview, Letby said she was aware of Child L's low blood sugar levels and knew the insulin was kept in a locked fridge, with a variety of other drugs. Keys were passed around nursing staff and there was no record of who held the keys at any time. She agreed the insulin could not have been administered accidentally, but denied being responsible. Her explanation was it must have been in one of the bags already being received. The prosecution say that is not a credible possibility.
2:32pm: Child M was born in good condition and was assessed as requiring 'special care'. He had an unexpected life-threatening event at about 4pm on April 9, at the same time his twin's blood sugar was dangerously low. The prosecution say "he came close to death", but "within four hours he was able to breathe unsupported in air."
2:37pm: At 3.30pm, a fluid bag was attached to Child M. At 3.45pm, he received intravenous antibiotics. The notes showed Letby was one of two to administer the medicine. Digital records show Letby's colleague was using the computer at 3.45pm. At 4pm, Child M's monitor alarmed and Letby was first to the cot. The emergency was such that doctors were called urgently. The consultant, Dr Ravi Jayaram attended and noticed unusual patches of discolouration on Child M’s skin which he thought particularly noticeable because of Child M’s skin tone. He thought the patches unusual because normally, if a baby arrests and there is not enough oxygen moving round the body, the baby is uniformly pale, grey or blue. What he saw he thought similar to what he had seen during the resuscitations of Children A and B.
2:38pm: Child M did not respond well to resuscitation. Six doses of adrenaline followed in 25 minutes and treatment was "about to be withdrawn", when Child M "suddenly improved". Dr Jayaram could not find any cause for the sudden collapse, but the discolouration he saw caused him to suspect an air embolism.
2:39pm: At 9.14pm, Letby noted Child M was tensing his limbs, curling fingers and toes and rotating hands and feet inwards - signs of brain damage. On the following night-shift, Child M had what the prosecution called a 'speedy recovery', although he did suffer further desaturations.
2:41pm: Medical expert Dr Dewi Evans said the rapid recovery would not have meant infection or a lung problem was likely. His conclusion was airway obstruction or air embolus. A paediatric neuroradiologist reviewed a brain scan on May 2016 and found brain damage for Child M, likely caused by the cardio-respiratory collapse on April 9.
2:44pm: Mr Johnson says when Letby's home was searched in 2018, a handwritten log of drugs administered during Child M's collapse was found, and she had made a note of the collapse in her diary. LD [Long day] - twin resus'. In police interview, Letby agreed she had connected a fluid bag to Child M and had co-signed for medication at 3.45pm but could not be sure if she had administered it. She thought she must have taken the notes home 'by accident', and had simply noted what had happened in her diary. She denied that the notes were a "souvenir" and denied deliberately trying to harm Child M. She could think of no reason how he would have suffered an air embolism.
2:45pm: The prosecution says the cases of Child E-F and Child L-M are similar, in that one suffered an insulin overdose and the other an IV air embolism.
Mr Johnson: "We suggest that coincidences like that simply do not happen innocently. Someone was responsible and the only credible candidate is Lucy Letby."2:46pm: Child N - attempted murder (three allegations) Child N, a boy, was born in June 2016. He was a couple of weeks premature and he was admitted to the neonatal unit. His clinical condition was "excellent". The prosecution say there are three separate occasions on which Lucy Letby tried to kill him.
2:48pm: Child N had haemophilia. Subsequent investigation found him to have a mild version of the disease, and children of his age do not bleed for no reason, particularly in the throat, the prosecution say. The prosecution said Lucy Letby used Child N's haemophilia as a "cover" to attack him.
2:50pm: On the night of June 2, Letby was on the shift and not the designated nurse for Child N. She had earlier texted friends and sent a message to a colleague saying “we’ve got a baby with haemophilia”. She sent a further text saying, “everyone bit panicked by seems of things although baby appears fine”. At 8.04pm she sent a text saying that she was going to “Google” haemophilia. 7 minutes later Letby texted her colleague: “complex condition, yeah 50:50 chance antenatally”.
2:54pm: The designated nurse said Child N was stable and left for a break at about 1am. He would have asked a colleague to look after Child N, but he could not recall which one. Letby had two babies to care for, in room 4. At 1.05am, Child N's oxygen saturation levels fell from 99% to 40%. "Unusually", for a baby, he was described as crying and "screaming". Child N recovered quickly, while the doctor was then called to another emergency. Medical expert Dr Dewi Evans said he believed the deterioration of Child N "was consistent with some kind of inflicted injury which caused severe pain". Dr Sandie Bohin said such a profound desaturation followed by a rapid recovery, in the absence of any painful or uncomfortable procedure, suggested an inflicted painful stimulus. She said – “this is life threatening. He was also noted to be … ‘screaming’ and apparently cried for 30 minutes. This is most unusual. I have never observed a premature neonate to scream.” The designated nurse said Child N was stable and left for a break at about 1am. He would have asked a colleague to look after Child N, but he could not recall which one.
Letby had two babies to care for, in room 4. At 1.05am, Child N's oxygen saturation levels fell from 99% to 40%. "Unusually", for a baby, he was described as crying and "screaming". Child N recovered quickly, while the doctor was then called to another emergency. Medical expert Dr Dewi Evans said he believed the deterioration of Child N "was consistent with some kind of inflicted injury which caused severe pain". Dr Sandie Bohin said such a profound desaturation followed by a rapid recovery, in the absence of any painful or uncomfortable procedure, suggested an inflicted painful stimulus. She said – “this is life threatening. He was also noted to be … ‘screaming’ and apparently cried for 30 minutes. This is most unusual. I have never observed a premature neonate to scream.”
2:57pm: 12 days later, there were two separate incidents on June 15 for Child N. Letby had been the designated nurse for the previous day. Overnight he was in nursery 3. At the beginning of the night shift, Child N was 'very unsettled'. Letby was to be the designated nurse for June 15. The use of her phone appeared to show she was awake by 5.10am and in for her shift at 7.12am. She had texted a colleague that she had “escaped [room] 1 [and was] back in 3”.
2:59pm: A colleague said Lucy Letby same into the room to say hello, but when the nurse's back was turned, Letby told her Child N had desaturated before assisting with the breathing. There was no evidence of an alarm sounding or if Letby waited to see if he self-corrected. Doctors were called and an attempt was made to intubate Child N. He was “surprised by his anatomy more than anything else … I could not visualise parts of the back of his throat because of swelling”.
3:01pm: The doctor saw "fresh blood" in Child N's throat, which the prosecution say was the same seen in Childs C, E and G. The doctor was unable to get the breathing tube down the throat of Child N as he was unable to visualise the child's tracheal inlet. He attempted to intubate Child N on three occasions.
3:07pm: An intensive care chart is presented to the court, which records the amount of dextrose going into Child N. The bleeding record, of 10am '1ml fresh blood', recording aspirates from the NG tube. Said bleeding, the prosecution say, is not recorded anywhere in the medical notes. It was more than 2 hours after the attempts to intubate. At 11.29am Letby sent a Facebook message to the doctor telling him “small amounts of blood from mouth and 1ml from ng. Looks like pulmonary bleed on x ray [i.e. a bleed from the lungs]. Given factor 8 – wait and see”. Other than that phone message, there is no evidence that Lucy Letby brought the bleeding to the attention of any of the medical staff. The prosecution said this is surprising given the problems Child N had suffered. In an update recorded on the computer notes by Lucy Letby at 1.53pm she wrote that Child N was “stiff” on handling and extending upper limbs, back arching … settled in between episodes. The prosecution say this is similar to that found in other cases heard so far. At 3pm there is a further entry in Letby's writing of '3ml blood', initialled not by Letby and coincides with a second collapse that day.
3:10pm: Child N collapsed just before 3pm and a consultant was called at 2.59pm. While awaiting a consultant, a junior doctor looked into the airway of Child N and saw a “large swelling at the end of his epiglottis” he could only just see the bottom of the vocal cords. He had never seen anything like this before in a newborn baby. The junior doctor's notes made at 4.30pm recorded: "desaturated this afternoon at 2:50pm with blood in the oropharynx + blood in the NG tube. Improved with bagging. Elective intubation planned following ??? unsuccessful attempts with 2 registrars and 2 consultants cords difficult to visualise …” Letby recorded at 6.30pm: "approx. 14:50 infant became apnoeic, with desaturation to 44%, heart rate 90 bpm. Fresh blood noted from mouth and 3mls blood aspirated from NG tube. … Drs crash called”. The prosecution said Child N was "so unwell" that attempts were made to reintubate him, but the doctor could not see down Child N's throat as the view was obscured by fresh blood. A more specialist team was called to carry out the intubation.
3:11pm: Child N continued to be unwell on June 15 and difficulties with ventilation persisted. Eventually he was transferred to Alder Hey, where the prosecution say he recovered quickly.
3:13pm: Medical expert Dr Dewi Evans said the blood seen in Child N's stomach had originated there, caused not from intubation attempts but "instead some preceding trauma". He suggested that “thrusting” a NG tube into the back of the throat might be the mechanism used to inflict the injury. Dr Sandie Bohin suggested only two possible explanations; either inflicted trauma or a spontaneous bleed. She considers the latter less likely as the haemophilia was 'only moderate'. Dr Bohin’s view was that the likely cause of the bleeding was trauma to the mouth, to the throat or to the oropharynx, most likely from a NGT or suction catheter.
3:14pm: Professor Sally Kinsey describes the collapse on June 3 as dramatic with no recognised medical cause. She excluded the possibility of a pulmonary haemorrhage - in other words, bleeding in the lungs, causing the collapse on June 15. In her opinion such bleeding would not have occurred spontaneously in a child with Child N's degree of haemophilia. It follows, the prosecution say, the bleeding was caused by trauma. Professor Kinsey also ruled out heavy-handed intubation as a cause.
3:15pm: In police interview, Letby had difficulty remembering Child N. She did recall an occasion when doctors had difficulty intubating him. She agreed that she had seen blood but denied being responsible for causing him harm. She could not explain the entry in her notes timed at 10am on June 15 in which she recorded aspirating more fresh blood which she had not apparently brought to the attention of anyone else.
3:16pm: Child O - murder allegation Child O and Child P were two of three triplet brothers, the court hears.
3:17pm: Child O weighed 2.02kgs, which was good for a premature triplet. He was in good condition and made good progress. He was stable up to June 23, when he suffered what Dr Evans said was a “remarkable deterioration” and died.
3:18pm: Between June 15 and June 23, Lucy Letby had been on holiday in Ibiza.
3:21pm: Child O's body was examined after his death and an injury to his liver was found. Letby was working the day shift on June 23 and was the designated nurse for Child O and P, in room 2, with another child. The prosecution say this "gave her an open opportunity to sabotage the babies". The third of the triplets was in room 1, the doctors believing he was the most needy of the triplets.
3:28pm: Letby also had the responsibility of supervising a student nurse that day. The designated nurse recorded 'no nursing concern - observations normal' for Child O. There are three records of feeds by Letby, at 8.30am, 10.30am, and 12.30pm - the earliest signed by the student nurse, the latter two signed by Letby. In a note made by the doctor at 1.15pm, there was '1x vomit post feed' with 'abdomen distended'. Child O was put on to IV fluids as a precaution. Child O's heart rate was 160-170, blood gases were low, and raised CO2 level. The doctor recorded the results as 'not normal' for a child breathing on their own and treated for suspected 'NEC'. It was thought down to Child O's swallowing of air or the passing of a stool earlier. An x-ray taken at the time showed a moderate amount of gas in the bowel loops throughout the abdomen
3:29pm: Letby noted at 8.35pm - 'reviewed by registrar at 1.15pm - [Child O] had vomited (undigested milk) tachycardic and abdomen distended. NG tube placed on free drainage … 10ml/kg saline bolus given as prescribed along with antibiotics. Placed nil by mouth and abdominal x ray performed. Observations returned to normal”.
3:31pm: Prior to Child O's collapse, a colleague said of Child O: "“he doesn’t look as well now as he did earlier. Do you think we should move him back to [room] 1 to be safe?" Letby did not agree. The prosecution say this echoes the final, fatal collapse of Child I.
3:33pm: Letby had taken Child O's observations at 2.30pm as 100% oxygen saturations and normal breathing rates. From her phone, she was on Facebook Messenger at the time, and at 2.39pm, the door entry system recorded her coming into the neonatal unit. Within a few minutes of that, Child O suffered his first collapse. Letby called for help, having been alone with Child O in room 2 at the time. Child O's heart rate and saturations had dropped to dangerously low levels. A breathing tube was inserted by the medical staff and he was successfully resuscitated. He was kept on a ventilator.
3:35pm: At 3.49pm, Child O desaturated again. doctors removed the ET and replaced it "as a precaution". Letby's written notes suggest she was the one who called for help. Child O suffered a further collapse at 4.15pm which required CPR. Those efforts were unsuccessful and Child O died soon after treatment was withdrawn at 5.47pm. A consultant doctor noted Child O had an area of discoloured skin on the right side of his chest wall which was purpuric. He noted a rash at 4.30pm, which had gone by 5.15pm, and did not consider it purpura, but unsure what it was or what had caused it. The doctor was particularly concerned about Child O's death as he was clinically stable before these events, his collapse was so sudden and he did not respond to resuscitation as he should have.
3:37pm: After the shift, Letby sent a series of messages to the doctor on Facebook, and to her colleague. She suggested Child O "had a big tummy overnight but just ballooned after lunch and went from there." A post-mortem examination found free un-clotted blood in the peritoneal (abdominal)space from a liver injury. There was damage in multiple locations on and in the liver. The blood was found in the peritoneal cavity. He certified death on the basis of natural causes and intra-abdominal bleeding. He observed that the cause of this bleeding could have been asphyxia, trauma or vigorous resuscitation. The prosecution say no-one would have thought a nurse would have assaulted a child in the neonatal unit.
3:38pm: Dr Dewi Evans concluded Child O's death was the result of a combination of intravenous air embolus and trauma. The liver injury was not in his view consistent with vigorous CPR. His view was that the liver damage would have occurred before the collapse and contributed to it and was probably the reason for his symptoms through the morning. As for the air in the bowel loops, Dr Evans concluded that that was consistent with excessive air going down via the NGT. Dr Bohin concluded concluded that together with the chest wall discolouration seen by the doctor that was indicative of air having been injected into Child O's circulation. She agreed that the abdominal distension was due to excess gas via the NGT.
3:39pm: Dr Andreas Marnerides, the reviewing pathologist, thought that the liver injuries were most likely the result of impact type trauma and not the result of CPR. He thought that the excess air via the NGT was likely to have led to stimulation of the vagal nerve which has an effect on heart rate and would have compromised Child O's breathing. He could not say whether it was either of these factors in isolation or in combination which caused Child O's death. He certified the cause of death to be “Inflicted traumatic injury to the liver and profound gastric and intestinal distension following acute excessive injection or infusion of air via a nasogastric tube” and air embolus.
3:41pm: In police interview, Letby said she had responded to child O's alarm at 1.15pm and found he had vomited. She responded first at 2.40pm and discovered mottling all over with purple blotches and red rash. She said that his abdomen just kept swelling and suggested that sometimes babies can gulp air when they are receiving assistance from Optiflo, as Child O was. A year later, on the anniversary of Child O's death, Letby carried out a search on Facebook on the surname of the child.
3:43pm: The court is now adjourning for today. Tomorrow (Thursday), the prosecution is expected to conclude its opening. The defence is also expected to give its opening statement.
Thursday 13th October 2022
Chester Standard Live Reporting
9:26am: Manchester Crown Court is today expected to hear the final part of the prosecution's outline of its case against Lucy Letby.
9:30am: Prosecutor Nicholas Johnson KC is expected to give the prosecution's version of events surrounding Child P, one of three triplet brothers, and Child Q. A reminder that reporting restrictions are in place preventing the naming of any of the children in the case. The media have been advised to use, for this trial, the names 'Child/Baby A-Q' for the babies allegedly attacked by Lucy Letby.
10:25am: People have filed into the Manchester Crown Court room, where the Lucy Letby trial continues. The judge, Mr Justice Goss, is expected to appear shortly for the resumption of the case at about 10.30am.
10:34am: The judge has arrived in court. Proseuctor Nicholas Johnson KC will resume the prosecution case outline shortly. Firstly, discussions on the use of iPads that the jury will use are taking place. The iPads will not have internet access, and have bespoke passwords for each juror, and will only store the evidence in the case for them to access.
10:38am: Child P - murder allegation The prosecution allege Child P was murdered the following day from brother Child O.
10:39am: Letby was the designated nurse for Child P. Letby fed Child P donor expressed breast milk at 8am, 10am, noon, 2pm and 6pm. The final feed, if accurately recorded, was about 13 minutes after Child O had died.
10:45am: A feeding chart is presented to the court. All the feeds from 8am-4pm are signed by a student nurse and co-signed by Letby. The 6pm feed is signed only by Letby. The court hears on the day shift feeds there is nothing more than a 'trace' aspirate (checking if there is anything in the stomach before the baby is fed), apart from a small amount of vomit at noon. The 8pm feed - the first after Letby's shift, produced a 14ml milk acidic (pH3) aspirate.
10:47am: The court hears because Child O had died in unusual circumstances, Child P was reviewed by Dr Gibbs at 6pm. The abdomen was “full … mildly distended”. There was no tenderness and he had active bowel sounds – good signs. He was screened for infection. An x-ray taken at 8pm showed striking gaseous distension throughout the stomach and whole bowel. Lucy Letby made her nursing notes at 8.24pm - therefore she was still in the neonatal at this time, Mr Johnson tells the court. The allegation is Letby "deliberately caused the problems" as she was ending her day shift, so she would not be detected, Mr Johnson tells the court.
10:49am: On that night shift, milk feeds were stopped for Child P on the grounds that a further large part-digested aspirate was drawn up the NGT at feeding time. At 6.39am, a nurse recorded the abdomen was "soft and non distended." 25ml of air had been aspirated by one of the nurses, and the NGT had been placed on "free drainage". Mr Johnson said the "problem" Child P had when Letby handed over to the night shift had been resolved. The problem appeared to be air.
10:51am: When the next day shift happened, Letby was Child P's designated nurse again. He was with his other brother - the third of the triplets - in room 2. The court hears as events unfolded, while Letby was the designated nurse for the other triplet, care was transferred to another nurse. Text messages Letby sent to a doctor at just after 8.30am suggest she had sent, or was sending, her student with a baby who needed an MRI scan.
10:54am: A registrar noted Child P, at 9.35am, had “desat + bradys” and had a moderately distended / bloated abdomen and slightly mottled skin. Letby's nursing notes from that night (9.18pm-10pm) recorded: "Written in retrospect...NG tube on free drainage - trace amount in tube. Abdomen full – loops visible, soft to touch … Reg...arrived to carry out ward round – [Child P] had apnoea, brady, desat with mottled appearance requiring facial oxygen and Neopuff for approx. 1 min. Abdomen becoming distended. Decision made to carry out bloods and gas (approx. 09:30)”
10:55am: The prosecution says it follows the problem with which Child P had been handed over by Letby to the night shift, but then apparently reappeared within 90 minutes of Letby taking over again. 15 minutes later, Child P had an acute deterioration. A crash call went out. Child P was intubated and improved, and efforts were made to transfer him to Arrowe Park Hospital
10:57am: Child P desaturated again at 11.30am. He was given adrenaline. His spontaneous circulation improved but he continued to deteriorate through the day. A punctured lung was identified from an x-ray taken at 11.57am, treatment started at 12.40pm. The transport team arrived at 3pm. Just before they arrived, Child P's blood gases were taken and were satisfactory. A doctor was hopeful of Child P's prospects. The court hears Letby said to her something like: "he’s not leaving here alive is he?"
10:59am: Child P's final collapse came at 3.14pm and, despite resuscitative efforts, he died at 4pm. A post-mortem examination had the coroner concluding Child P died from Sudden Unexpected Postnatal Collapse but he was unable to identify the underlying cause. He certified the cause of death as “prematurity”. Medical expert Dr Dewi Evans initially suggested the cause of death was complications from his pneumothorax. He was, however, suspicious of the large volume of air in the stomach and intestines evident on x-ray. In his subsequent reports Dr Evans concluded that excess air in the stomach could have “splinted” Child P's diaphragm compromising his breathing.
11:00am: Dr Sandie Bohin also concluded that the abdominal distension splinted Child P's diaphragm resulting in an inability fully to expand his lungs and causing his collapse. Subsequent resuscitation and intubation involved high ventilatory pressures, which together with vigorous resuscitation, can cause pneumothorax. She described the abnormal gas pattern seen in Child P's stomach through to his rectum which she concluded it was caused by the exogenous injection of air via the NGT – describing that as “the only plausible explanation”. This excess gas splinted the diaphragm, compromised breathing and it caused Child P's collapse.
11:01am: Mr Johnson tells the court: "As with all these cases – it is the coincidence of problems happening when Lucy Letby was about and the coincidence of the same problems happening with different babies at different times, which we suggest is so telling and indicates that it was her malign hand at work."
11:04am: In police interviews, Letby said the student nurse fed Child P at two-hourly intervals on June 23, and she had fed Child P alone at 6pm. She said she had agreed to be Child P's designated nurse because the parents had asked for some continuity. Early in the shift, around 8am, she said could see “loops” in his tummy and brought these to the attention of the doctor, and notes were made later that day. If what she noted was true, the prosecution say, it would say when she took over the care from the previous night, he had a developing problem, but the prosecution says we know that was not the case. A note by a nurse at 6.39am 'ran contrary' to Letby's note, as the problem 'had been resolved' during the night.
Mr Johnson: "This is another example of Lucy Letby making factually false entries in the notes to cover herself." Letby denied deliberately causing Child P any harm.11:06am: Child Q - attempted murder allegation Child Q was born on June 22 - the day after Child O and P. He was premature but a good weight, and on CPAP for the first 20 hours. He was admitted to the neonatal unit as he needed breathing support, but was initially stable. He had a catheter in place via his umbilicus for nutrition, however he was well enough to commence feeding via his NGT. Initially he was put into room 1.
11:08am: Nursing staff noted small amounts of bile when they checked his NGT on June 23-24. These were not of sufficient concern to stop him being fed milk. A different nurse was Child Q's designated nurse on the night shift for June 24. She monitored him through the night, and fed him 0.5ml of milk every 2 hours at 3am, 5am and 7am. The nurse was content with the condition, although the blood gases deteriorated slightly, so she referred the results to a doctor. The doctor reviewed them and was not concerned. The day shift on June 25, Letby was on duty and was Child Q's designated nurse. Child Q had been moved into room 2.
11:10am: Letby made notes on Child Q's fluid/feeding chart at 8am. Child Q was receiving nutrition Babiven via a UVC. Just after 9am, Letby and the nurse were together in nursery 2, and it was feeding time. The other nurse attended to another child in the room.
11:14am: According to the record, Child Q's heart and respiratory rates both increased for a short period of time. But, the prosecution say, the feeding chart shows something 'unusual'. That chart is shown to the court. The 9am fluid chart, in Letby's handwriting, appears unfinished, with numbers noted for fluids, but no record for the feed or Letby's signature initials at the bottom of the 9am column. The prosecution suggests something caused Letby to leave halfway through doing this.
11:16am: Letby signed for medication for another baby at 9.04am. The other nurse agreed to keep an eye on Child Q at 9am. A few minutes later, Child Q's monitor alarms activated to alert staff to a deterioration in his condition.
Mr Johnson: "We say that Lucy Letby had sabotaged [Child Q] and had injected him with air and a clear fluid into his stomach via the NGT. She was trying to kill him."11:19am: The nurse called for help and was joined by another nurse. Child Q had been sick and nurses used a suction catheter while respiratory support was given. Lucy Letby appeared soon afterwards together with doctors who were responding to the call for help. Medical notes indicates doctors were called to the unit at 9.17am as Child Q had "just vomited" and oxygen saturation levels were in the "low 60s". The prosecution say medical staff gave him assistance with breathing using a Neopuff device and applied suction to clear his airways. The records indicate not only had his oxygen dropped but also his heart rate. He is described as “mottled” in appearance and, most significantly, a substantial amount of air was aspirated from his stomach via the NGT. Mr Johnson tells the court the air had been put in there by Letby, as if the feeding chart had been followed correctly at 9am, the person feeding - Letby - would have aspirated Child Q's stomach to check there was nothing there before administering the 0.5ml milk feed.
11:22am: Another nurse's medical note on an 'apnoea/brady/fit chart' notes: "09:10; brady 98; desat 68; fit ?; baby found to be very mucousy, clear mucous from nasopharynx oropharynx removed clear fluid +++. "O2 via Neopuff given post suctioning. Dr... emergency called to attend. "NGT used to aspirate stomach by Nurse L Letby” The prosecution say given that Letby was Child Q's designated nurse and she performed the aspiration of air, it might be thought surprising that she did not make the note – yet she did make notes in records of other babies’ notes at about the same time.
Mr Johnson: "We question whether this is an attempt by her to create a documentary alibi."11:27am: Computerised nursing notes made by Letby for that morning: "“09:10hrs [Child Q] attended to by SN... – he had vomited clear fluid nasally and from mouth, desaturation and bradycardia, mottled ++. Neopuff and suction applied. [Registrar] attended. Air ++ aspirated from NG tube”. Following the collapse, blood was taken to test for infection and other parameters. A venous blood gas test showed results suggesting that he was unwell but this had resolved by 11.12am. He was started on a course of antibiotics as a precaution. The doctor's view recorded at the time said Child Q's collapse was a result of “presumed sepsis with jaundice”. At that stage a chest x ray was taken which showed nothing untoward. The more detailed blood tests were recorded at 1.50pm and showed slightly abnormal results which were treated.
Child Q had made a reasonable recovery through the day and at 7.20pm was "looking tired". Doctors took the decision to intubate him because his respiratory rate was down to 19 (low)and his heart rate was between 160-200 bpm (high). At that stage his blood gas readings were good. The prosecution say Lucy Letby was "worried" when she got home that night. She texted a doctor at 10.46pm and asked "do I need to be worried about what Dr G was asking?" The doctor sought to put her mind at rest and told her that Dr G was only asking to make sure that the normal procedures were carried out. She replied that after Child Q had collapsed she (LL) had walked into the equipment room and Dr G had been asking the other nurse who was present in the room (when Child Q had collapsed) and how quickly someone had gone to him because she (LL) had not been there. She continued her texts to the doctor, telling him that she had needed to go to her designated baby in room 1.
11:29am: The following day, Child Q's gases were unsatisfactory, but he had been extubated 4 hours earlier and was in air with high saturations. Medical staff noted a 'mildly dilated loop of bowel' on Child Q's left side and raised the possibility of NEC and surgery. Child Q was transferred to Alder Hey, where he quickly stabilised and no surgery was required. The prosecution say this was "another child who had suffered life-threatening problems and...when out of the orbit of Lucy Letby, he made a rapid recovery." Other than three days the following week, that was the last time Lucy Letby worked in the neonatal unit at the Countess of Chester Hospital, the court is told.
11:33am: Medical expert Dr Dewi Evans said Child Q's collapse was due to 'inappropriate care', and he had been injected with air via the NGT. The significant amount of air aspirated from his stomach 'could not have arisen in any other way'. Dr Sandie Bohin noted Child Q was well up until June 25 and believed something happened between 9am and his collapse. He was only being fed what Dr Bohin describes as “tiny” amounts of milk yet he had taken in “copious amounts of air” from the NGT. This was abnormal. The effect of a large volume of air in the stomach would “squash” the lungs leading to desaturation and instability. Although a baby may recover quickly after such an event, he may remain unstable for some time thereafter. She agreed with Dr Evans’ conclusion that events were consistent with the introduction of a large amount of air via the NGT. A professor reviewed brain imaging of Child Q taken in November 2019 - more than three years later. He found evidence of abnormalities which whilst they were not diagnostic of him having suffered a brain injury as a result of being given excessive air and liquid via his NGT, they could be explained.
11:34am: In Letby's home search, officers recovered the handover sheet from the morning of June 25 which included Child Q's name. This was a document which should not have left the hospital. When interviewed by police, Letby agreed Child Q had been well enough for her to leave him on the morning of June 25. When asked about the excess air aspirated from his stomach, she suggested babies sometimes gulp air when they vomit. She denied putting excess air down the NGT.
11:37am: Mr Johnson: "Following those events, the consultants suspected that the deaths and life-threatening collapses of these 17 children were not medically explicable and were the result of the actions of Lucy Letby. "No doubt they were acutely aware that making such an allegation against a nurse was as serious as it gets. "They, at the time, did not have the benefit of the evidence that you will hear and the decision was taken by the hospital took the decision to remove Lucy Letby from a hands-on role. She was moved to clerical duties where she would not come into contact with children. "The police were contacted and began a very lengthy and complex enquiry. "This involved the police contacting independent paediatricians and other specialists to review many cases which had passed through the NNU at the CoCH. Following that review, the decision was taken to arrest Lucy Letby – the first arrest came in July 2018. "On July 3 she was arrested at her home, where the house was searched. "In addition to some of the paperwork, they found some other interesting items. "There were some Post-it notes with closely written words on them, some of which included the names of some of her colleagues.
"On some of the notes were phrases such as “Why/how has this happened – what process has led to this current situation. What allegations have been made and by who? Do they have written evidence to support their comments?"
"In her writings, she expressed frustration at the fact that she was not being allowed back on the neonatal unit and wrote 'I haven’t done anything wrong and they have no evidence so why have I had to hide away?'
"Her notes also expressed concern for the long-term effects of what she feared was being alleged against her and there are also many protestations of innocence."11:39am: "On another piece of paper, she wrote: 'I don’t deserve to live. I killed them on purpose because I’m not good enough”. “'I am a horrible evil person' and in capital letters, 'I AM EVIL I DID THIS'. "That, in a nutshell," Mr Johnson tells the court, "is your case."
11:40am: That is the conclusion of the prosecution opening. The defence, led by Benjamin Myers KC, will give a defence statement after a short adjournment.
12:13pm:
Mr Myers: "It is difficult to think of allegations that may be harder to stand back and look fairly and look at the actual evidence. "The sympathy of everyone will rightly be with families of the children...involved in this case. We all share the same feelings and experiences."12:15pm: "It is natural to sympathise - we all do it. We recognise the sadness, distress and anger that come with allegations like these. "We acknowledge the great loss suffered by all families. "Nothing I can say in this trial is intended to diminish that in any way. "It is obvious...where we have such terrible allegations, it would be terribly easy for emotion to overcome reason, and convict without hearing a word of evidence."
12:16pm: "There is a real danger people will simply accept the prosecution 'theory' of guilt. "It is a theory built 'firmly' on coincidence."
12:18pm: "What we are left with is coincidence. "In the events that happened. Sometimes what happened was the result of deterioration in a baby. "Sometimes, no-one can say what caused a deterioration. "Sometimes, things have gone wrong, or the necessary standards of care have not been met, irrespective of anything to do with Lucy Letby. For that, she should not get the blame."
12:19pm: The assumption is "The worse it sounds, the more guilty she must be."
12:22pm: Mr Myers outlines the 'key issues' for the defence, in what he says will assist the jury and will place everything into context. He said his speech, at this stage, will take about a couple of hours, and will break down the defence into three general areas: Letby and the general area of her defence, coincidence, and the medical evidence.
12:23pm: He tells the court the medical evidence is a key area, and there are 'key issues' for each count.
12:24pm: Letby was a "dedicated nurse" "who did her best" to care for infants and did not intentionally cause "any harm" to any baby, My Myers said.
"She loved her job...and cared for the babies' families."12:26pm: "You won't get your answers [to what Letby is like] through seeing her in the dock.
"This is what she is like six years after the allegations started. That, as you can imagine, is gruelling for anyone.
"You may want to keep that in mind as we go through the evidence in this case."12:27pm: "A young woman who trained hard to be a nurse...and looked after many vulnerable babies for years. "A young woman who loved what she did, and found she was being blamed for the deaths of the babies she cared for. "We are dealing with a real person dealing with...a litany of allegations...not one of which has been proved."
12:32pm: Mr Myers refers back to the note shown to the court just before the break. He said it is a note written in anguish and despair. She was "going through a grievance procedure" with the NHS at the time, the court hears, and knew what was being said about her before her arrest. The allegations were "destructive", the court hears. The note is headed 'not good enough'. The defence notes it does not say 'guilty'. The note adds: "I will never have children or marry". Another part of the note says "I haven't done anything wrong".
Mr Myers: "We say people can pour feelings on to paper. "This [paper] represents the anguished state of mind Letby felt when accused of killing children she had cared for. "We say this paper represents 'anguish' and not 'guilt'."12:33pm: There was further paperwork the police took from Letby's address at the time of her arrest. The defence say the paperwork was "nothing more extraordinary" that Letby being someone who scribbles a lot of work down, and keeps hold of it.
12:34pm: The defence say the prosecution case is "driven by the assumption of someone doing deliberate harm combined by the coincidence of Letby's presence."
12:37pm: That is, Mr Myers said, combined with Letby "not doing" what is alleged against her. "You will find, from what we have heard, no evidence of her actually doing harm to a child. "These allegations are of attacks. You will have heard words of poisoning, sabotage - words likely to have had an emotional impact on you. "You will have to refer to whether Letby is engaged in any of the attacks alleged. "Using syringes to inject air? No. Tampering with bags of fluid - or poisoning them? No. Physically assaulting children? Smothering them? "We are dealing with 24 events and we say there is nothing [to suggest that]."
12:39pm: "The time of Letby's presence has itself become an explanation for the deterioration."
12:43pm: The list of nursing staff on duty for all the fatal and non-fatal collapses, with Letby on duty for all events, is shown again to the court.
"This table exists because the prosecution created it, and was put together for the purpose of the prosecution. “It was to show what were declared to be key events. "This is a self-serving document. What we have here is because the prosecution have chosen to present it this way." The defence says it does not show the 'individual health of the children concerned, or any problems they had from birth, or the risks, or the course of treatment and/or problems encountered by said treatment'. The chart does not show 'other collapses or desaturations' for the children when Letby is not present.
12:44pm: The table does not show 'shortcomings in care' which 'could have impacted the health of the baby', or 'how busy the unit was', or 'what Letby was actually doing at the time of the event', My Myers tells the court. It doesn't show 'whether Lucy Letby was anywhere near to a child at the time of the event' or if there was 'a problem which could be traced before Letby's arrival'.
12:45pm: Regarding the explanations for what happened, My Myers said: "This is something which is quite a difficult question, even for experts to look at."
12:46pm: "What the case will come down to is the medical evidence, on what can be safely proved and what it can't."
12:49pm: Regarding the medical evidence, Mr Myers said: "The cause of the deteriorations, or deaths, is not clear and have a number of possibilities. "Generally, we are dealing with babies who are fragile, and their condition can change and deteriorate very rapidly." Mr Myers adds the premature and vulnerable babies can come with developmental conditions that require extra treatment, and are prone to infections. "It is crucial to consider the starting point in these cases. "There is a question to whether this hospital should have been caring for this number of children."
12:50pm:
Mr Myers: "We suggest whether an event that clearly fits an ongoing and difficult condition has been converted into an event of deep suspicion that harm is being done."12:52pm: For a nurse standing in the neonatal unit next to an infant is "unremarkable", without a "suspicion of guilt", Mr Myers tells the court. "When we come to the experts, you will need to consider their evidence and how strong it is."
12:55pm: The defence say there are five 'important' considerations for the evidence: The birth condition of the infant. If there were any problems in the care leading up to the event - events 'can come up from nowhere' Whether the prosecution expert evidence concludes there was deliberate harm done Whether Lucy Letby was present at the relevant time, and what she was doing Whether there were failings in care by other people or the neonatal unit as a whole
12:57pm: The birth condition of the infant Mr Myers tells the court: "We are dealing with some of the most medically fragile babies under the most intense medical care. "All of them, bar one, are premature to varying degrees. Some had considerable problems. "These babies are already at risk of deterioration and this can happen unexpectedly and it can be rapid."
12:58pm: The court is adjourning for the lunch break. The defence will resume giving its outline statement after the adjournment.
2:14pm: The jury is now coming back in to hear the rest of the defence case outline.
2:16pm: The matters leading up up to the event Mr Myers refers to the medical situation and condition of the children involved. Sometimes that includes 'the ability of doctors and nurses to spot' signs of problems in the build-up to the event.
2:17pm: Sometimes that would be a problem if the unit was "understaffed and overstretched," Mr Myers said.
2:19pm: The defence say in relation to the evidence, "we have to be careful of the assumption or theory of guilt," and the "dangers of opinion" in relation to the conclusions of "deliberate harm". "We say that if an expert sets out within expectation a suspicion of harm being done, that may make it more likely they will reach conclusions which are harm based...rather than innocent explanations. "When there is no explanation, there is a danger of the expert filling the absence of an explanation with one...by the prosecution."
2:20pm: "If someone looks for something, and has something in mind, they will look for that."
"Confirmation bias," added Mr Myers.2:21pm: "There is plenty of disagreement" between the prosecution expert evidence and the defence.
2:24pm: Medical evidence Mr Myers tells the court that sometimes deteriorations are unexplained, and if Lucy Letby cannot provide an explanation, that does not make her responsible. For every count, Letby is "adamant" she has "done nothing wrong" to cause any deliberate harm to any of the babies in the case, Mr Myers adds.
2:27pm: Regarding the point of air embolus cases The defence "accept it is a theoretical possibility", but that "does not establish very much". The defence do not accept, for Child A, an air embolus was the cause, but one of "sub-optimal care", as a result of either "lack of fluids" or "various lines put into him, with potential to interfere with his heart rate".
2:28pm: "You will hear in this case, that the air present after death does not indicate an air embolus." Mr Myers said air present in the abdomen "can happen post-mortem".
2:29pm: For Child B, the defence say she had been born in a "precarious condition" and there were no signs of diagnosing an "air embolus". The defence say prosecution experts had been "influenced" into believing harm was done. The defence say Child B had other episodes where she struggled to breathe, after the indictment.
2:34pm: For Child C, the defence say it is accepted that someone had injected air as a "theoretical possibility", but that is "a very long way from proving what has taken place". Mr Myers said the jury would have to look at the practicalities of that, and consider alternative explanations. Child C was "subject to a variety of complications" due to being born premature, the jury is told. "We say, for a starting point, he should have been at a unit providing more specialist care." The defence say pathology identified acute pneumonia in Child C. The defence suggest a structural blockage could have caused distention.
2:36pm: For Child D, the defence say the hospital "failed to provide appropriate care", and this was "beyond dispute" as the prosecution accepted care was sub-optimal. Child D "was never able to breathe unaided" and there was a "strong" possibility of infection, and evidence of pneumonia after death.
2:38pm: For Child E, the defence say there is "no evidence of an air embolus", or of "direct trauma" that led to blood loss. There was "no clear explanation" on the cause of death, but that was not a presumption of guilt. The defence say the absence of a post-mortem meant the prosecution could "float suggestions of deliberate harm".
2:43pm: For Child F and Child L, the children allegedly poisoned with insulin, the defence "cannot say what has happened". "It is difficult to say if you don't know," Mr Myers said. "So much has been said about these. These are not simple allegations which can automatically lead to a conviction." The defence say Child E's TPN bag was put up by Letby in August 2015 and hours later there were blood sugar problems. That bag was replaced, in the absence of Letby, but the problems continued. The sample taken came from "the second bag", the defence say. A professor had given "three possible explanations", none of which identified Letby as a culprit. For Child L, there were issues with the documentation provided, so those are challenged, the defence say. There is "nothing to say" Letby was directly involved in the acts.
2:45pm: For Child G, the defence say the child was extremely premature, "on the margins of viability" - "there will be problems," Mr Myers said. Child G was a "high risk baby", "irrespective of anything to do with Lucy Letby". Child G also displayed "signs of infection".
2:48pm: For Child H, the defence say she was treated with three chest drains and her case, as said by the prosecution, was complicated by "sub-optimal treatment". Butterfly needles were left in for hours "which may have punctured her lung". The prosecution experts "appear to have no explanation" for what happened. The harm "was nothing to do with Lucy Letby" and a cause of Child H's deterioration included "infection".
2:50pm: For Child I, the defence say her death was a result of "ongoing clinical problems caused by her extreme prematurity". The air embolus is "not accepted" as a cause by the defence.
2:51pm: The defence say CPAP treatment may have caused 'CPAP belly' in Child I, causing a distended abdomen.
2:53pm: For Child J, the defence say "there is not a great deal of explanation" for what caused the deterioration from the prosecution experts. The defence say there is "an assumption of deliberate harm being used to blame her" when it was actually "inadequate care" at the hospital.
2:55pm: For Child K, the defence say the tube was dislodged, and the prosecution say that was Letby's doing. "Letby does not agree she did that, nor is she seen to have done that." The prosecution say Child K had been sedated. The defence say it is disputed, that Child K was able to move, and there would be evidence to follow on that. The defence say there was "sub-optimal care" and Child K "should not have been at the Countess of Chester Hospital in the first place", but in a hospital providing tertiary care.
2:57pm: For Child M, the defence say "there is no obvious cause of collapse" in this case, but it is not established the "obvious" one is an air embolus. "We are back in the territory of blaming Lucy Letby because there is no other cause. "The mere fact she is there is being used as an explanation."
3:00pm: For Child N, the defence say there are "many reasons" why a baby would shout or scream. "It was far more likely to be hunger" - "you certainly won't find evidence of anything else". Regarding the allegation Letby did something to cause Child N to bleed, the prosecution say the intubating doctor already saw blood, because Letby harmed him. The defence disagree and say blood was "not identified until intubation had already happened, or was in the process of happening". There were three attempts to intubate him. The defence say, again, there was "sub-optimal care" for Child N.
3:02pm: For Child O, the allegations are "various". An air embolus is "not accepted" and the defence point towards an infection, along with "CPAP belly".
3:03pm: The "liver injury" was "caused during resuscitation", the defence say. The prosecution "do not accept that", Mr Myers tells the court.
3:06pm: For Child P, the defence agree the collapse could have occurred by a splintered diaphragm, but do not agree with how it was caused. The defence say Optiflo is a cause. The defence agree once Child P collapsed, it was unclear why he did not respond to resuscitation, but that did not point to deliberate harm.
3:07pm: For Child Q, the defence say there was viral-drawn aspirates, indicating a bowel problem, supported by a diagnosis of NEC. "A poorly funcitioning bowel" had led to Child Q vomiting.
3:11pm: Mr Myers added there are two further areas to consider.
"It is important not to guess, or proceed on a presumption of guilt."
"Even when we have timings...some will be more precise than others."
There were many occasions when "Lucy Letby was simply not there" when harm was being alleged.3:14pm: "Lucy Letby was a young nurse with no family commitment, who had built her life around the neonatal unit. "She was often called in to help babies with severe health issues...she was more likely to be there to cover for clinically difficult babies."
3:15pm: The defence say Letby's lack of recollecting details in police interviews should be put into context, like other witnesses, who may not be able to recall anything beyond the notes they made at the time. "Goodness knows how many babies she will have cared for over the years," Mr Myers said.
3:17pm: Other staff Mr Myers said this is important - it would be "unbalanced and unfair" if the focus was on Lucy Letby without focusing on problems with other staff, or how the unit was run. "We do not suggest for one moment the doctors and nurses did anything other than the best they could. "What they do is admirable and crucial."
3:18pm: "We say there were problems with the way the unit performed which had nothing to do with Lucy Letby." Examples of sub-optimal care for babies previously mentioned and conceded by the prosecution are relayed to the jury. "There are many other examples of sub-optimal care of babies in this unit," Mr Myers.
3:19pm: The defence say the prosecutino have referred how babies improved rapidly when moved to a tertiary unit - "when moved away from Lucy Letby" The defence says the improvement could be because they had been "moved away from the Countess of Chester Hospital". It is evidence that the unit "did not always deliver the level of care that it should have provided" and to blame Letby "is unfair and inaccurate".
3:23pm: Mr Myers explains the neonatal unit is a level 2 unit, with level 3 offering the highest specialist care for new-borns, such as in Arrowe Park. Either 'through lack of technical level of skill among the staff, or because it was too busy and could not deliver with the level of staff it had available.' The Countess of Chester Hospital neonatal unit was subsequently 'resdesignated' as a level 1 unit after Letby was redeployed in July 2016, Mr Myers said. "You can imagine in a situation like that, there is bound to be concern."
3:26pm: The defence also refer to Dr Ravi Jayaram, and his 'concern' about Letby's behaviour as detailed by the prosecution in the opening. "You may wonder what on earth that is all about. "If Dr Jayaram had these suspicions, when did that start? "You may think that if consultants had suspicions, then why did Letby continue? "You may wonder if there was any basis for suspicion at all. "You may think that suspicions by one or more consultants like that, if Letby is to blame, then that is fertile self-serving territory for an assumption of guilt to take hold." Mr Myers said Letby became a "target" for blame.
3:30pm: "It would be very unfair to judge Lucy Letby by standards or expectations different to other staff in the unit," Mr Myers said. The defence say if it can be interpreted the unit is understaffed, treatment is "hurried," "mistakes made" and records "not kept". Mistakes may "not be immediate".
Mr Myers: If the unit has "failed" in its care which has led to this "uncharateristic spike in deaths", you can imagine "pressures" which call for an explanation, 'distancing the blame from those running the hospital' through "confirmation bias". "The blame is far too great for just one person," Mr Myers added. "In that dock is a woman who says this is not her fault."3:34pm: That concludes the defence outline case. It is also the end that the jury sits as 14 members, as one juror has indicated they can no longer serve on the jury. The reserve juror has taken their place. The second reserve juror has also been discharged. The jury will now sit as 12.
Friday 14th October 2022
Chester Standard Live Reporting
10:32am: The case is now resuming. The jury of 12 is now filing into court.
10:35am: Slightly unusually, the jury are now being shown how to use iPads for the purpose of this trial. Unlike traditional trials of the past, where juries would be handed large paper bundles in files, this one will have the evidence stored on electronic devices. Given the amount of evidence expected to be handed to the jury members, the court is told this will save on the amount of paperwork, and if additional evidence is produced in court, that will be added to the jury members' electronic files.
10:36am: The judge, Mr Justice Goss, has already said the jury members will not be able to use the iPads to access the internet, so culd not, for example, do any independent research in connection with the case.
10:41am: Each iPad is tailored to each juror with a bespoke, unique password, allowing the jurors to make notes without anyone else in court seeing them.
11:08am: The judge, Mr Justice Goss, says he is a 'first-timer' for using an iPad for a trial himself, adding it will save a lot of paperwork for the jury.
11:25am: We have had a short adjournment while the prosecution readies some paperwork it shall present shortly.
11:38am: The trial is now resuming.
11:42am: Having been shown how to use iPads for electronic evidence, new documents are now being presented to jurors 'the old fashioned way' by way of paperwork, to add to their files.
11:45am: Medical expert Dr Dewi Evans is now being called to give evidence. He has been named several times during the prosecution opening.
11:49am: Dr Dewi Evans is a consultant paediatrician. He is giving his background and experience. The court hears he has specialist knowledge of new-born babies, in providing healthcare, including intensive care, in the 1980s and 1990s in Swansea.
11:54am: Dr Evans confirms he has never been employed at the Countess of Chester Hospital, nor has he had any involvement with the care of babies involved in this case. He said he was involved in the development of neonatal care. "It was an essential and important part of our generation that we provided good services for these ill babies. "A lot of my experience was not about reading books, but was hands-on. You were there, with a sick baby in the incubator. You support the monitoring - nothing as good as it is now. A lot of it was 'touch and go', really. It could be quite fraught as there were ther demands on children's services. "We were passionate about these babies to get money for developments...and...publicity for baby care. "In 1980 in Swansea, the health board built a brand new children's department with a new neonatal unit that I had designed. "Life became easier as...we had some superb nursing staff and by that time there were far more junior doctors developing an interest in baby care."
11:55am: "Babies arrived in all sorts of conditions. The most common were associated with prematurity. One would have to see them through the first few days of life - giving them oxygen...CPAP - which has saved thousands of lives over the past few decades. "If not CPAP, it would be intubation - a breathing tube into the lungs and put them on...a breathing machine. "The initial machines were primitive...but they worked. "In addition to giving babies ventilation support, we would give them IV fluids to help them absorb milk."
11:56am: Cannulas would also be used to help babies get adequate fluid, such as glucose and amino acids. Sometimes a 'cocktail' of nutrition would be required for each baby.
11:58am: "All the neonatal units are dedicated units. They are responsible only for new-born babies. "Usually they are next door to the maternity unit. They tend to be divided into sections - the sickest in the intensive care area, babies who are recovering are in a high dependency area, and babies who are recovering but too sick to go home are in the 'ordinary' area."
12:02pm: Dr Evans said he gave up his full-time medical practice in 2009 after 30 years. He has done a few short-term locums since then, but has since dedicated his time to the courts, providing reports for baby care. He had done reports involving clinical negligence - the first in 1988. He said he does not take on new cases involving that now. He now says he takes time in family courts and crown court, involving serious cases of babies having died suspiciously or being injured. He has prepared reports for police authorities, such as the National Crime Agency. He has also prepared reports on behalf of defendants.
12:09pm: The court is being reminded of the 'tiered' hospital structure locally, with Arrowe Park and Liverpool Women's Hospital designated as 'level three' units, able to provide the most complex neonatal care. The Countess of Chester Hospital was designated as a 'level two' unit, able to provide intensive care for vulnerable babies up to 48 hours, after which they would be transferred to a level three unit. Other hospitals in Cheshire, such as Leighton, were designated as 'level one'. Alder Hey was the designated surgical hospital unit.
12:15pm: The court hears the Countess of Chester Hospital neonatal unit has four rooms - room 1 the ICU, room 2 the HDU, and rooms 3 and 4 the special care rooms. Babies would be moved between the rooms as their condition changed, with transitional care cots available. Entry to the neonatal unit was controlled through locked doors. One from the public entrance side, the other from the maternity/labour side. Swipe cars would be used by staff to gain access to the neonatal unit, and their dates and times would be recorded.
12:17pm: Times when this would not record someone would be: a) when person A swipes to open the door, and person B also enters at the same time b) from inside the hospital via a push-button to open the door c) via the buzz system of gaining entry - pressing a buzzer and a member of staff would provide entry for individuals The system of entry is 'commonplace', the court hears.
12:20pm: The court is now being shown a walk-through of the neonatal unit at the Countess of Chester Hospital, dated September 2021 - which has changed following hospital upgrades since 2016.
12:26pm: The 10-minute video is being played to the jury, showing all the rooms in the neonatal unit, and what purpose the rooms served back in 2016.
12:30pm: The court is hearing from a list of agreed facts - ie, evidence agreed by the prosecution and defence. The hierarchy of the Countess of Chester Hospital staff is being explained to the court.
12:33pm: Doctors would be alerted by two forms of 'bleep' - one non-urgent, the other 'urgent' - the latter being labelled a 'crash call'.
12:37pm: The neonatal unit baby monitors, used to monitor vulnerable/unwell babies, are now being explained to the court. Dr Evans says if levels fall below specified values, or if monitoring equipment falls off the baby, an alarm will go off to alert medical staff.
12:39pm: A video explaining the technicalities of the Phillips IntelliVue monitors is played to the court. They are similar to monitors found for hospital patients, but the values are set to a 'neonatal profile', and cannot be changed. Dr Evans explains the values for neonatal babies are different to children, and to adults. Values for neonatal babies would be "far too fast" for children.
12:41pm: A heart-rate of 140 is "fine" for a neonatal baby, but a sign of sickness for an adult. Over oxygenation "can lead to blindness" so greater care should be taken for such babies.
12:44pm: Alarm parameter settings can be adjusted by a nurse, but must be in 'clinically safe' settings, the video explains. For example, a heart rate range can be between 50bpm and 165bpm, with the alarm sounding if the heart rate goes outside that range.
12:46pm: Dr Evans explains the monitor also shows wavy lines which show how regular the heart rate is, and the pattern of breathing.
12:51pm: The video, played to the jury, demonstrates what alarms sound when a 'yellow alarm' goes off, and a 'red alarm'. The red alarm is for more immediate emergencies, and has a different tone to the yellow alarm sound.
12:53pm: The alarms can be 'paused', via the 'pause' button, which turns the alarm off for one minute. A light will continue to show on the monitor, either yellow or red, depending on the type of alarm that sounded, even when paused.
12:58pm: The alarms can be manually turned off, the video explains, for each parameter. If done so, a display on the monitor would show the alarm for that parameter had been turned off. "This would not be standard practice," the court is told. If the monitor numbers then headed outside the alarm parameters, the numbers on display would then start flashing.
1:02pm: The court is now adjourning for the lunch break. It will resume this afternoon, with Dr Evans due to give further evidence.
2:10pm: The afternoon session is about to begin in the Lucy Letby trial.
2:14pm: Dr Dewi Evans is being asked about medical terms, such as 'air embolism', apnoea, blood gases, capillary, and medical equipment.
2:16pm: A video is now being presented to the court showing what a cannula is, and a demonstration of how it is administered to a patient.
2:22pm: A video is now explaining what happens in 'Neopuffing', more crudely known as 'bagging' of patients, "one of the most important pieces of equipment" in a neonatal unit, which can give artificial breaths to a baby.
2:23pm: There is a dial which can deliver varying amounts of oxygen, from 21% (air) to 100%. The pressure can also be altered depending on the prematurity of the babies, "to help open their lungs".
2:24pm: The Neopuff machines are checked "once each shift" by neonatal staff.
2:26pm: The video played to the court shows a demonstration of a Neopuff machine, with the mask being attached to a dummy baby's nose and mouth.
2:27pm: Five inflation breaths', each for three seconds at a time, are given to babies with breathing difficulties or for babies who have collapsed.
2:30pm: The Neopuff machine can also be applied to intubated babies, as the video demonstrates. A second video, titled 'Neopuff consumables', is played to the court demonstrating additional equipment.
2:35pm: The process of getting 'aspirates' from the stomach, via a nasogastric tube, is also explained to the court. Dr Dewi Evans says it is important for the stomach to be empty, prior to a next feed for a baby, as the presence of milk aspirate could suggest problems with that child.
2:39pm: The video demonstrates that any aspirate found has a 0.5ml sample checked for pH levels. Dr Evans explains the syringe used is purple in colour - it is a syringe only used for nasogastric tube, and cannot be used for IV feeds - you cannot be used to inject milk into a vein, for example, as the shape is different.
2:44pm: The video played to the court says action can be taken by medical staff to withdraw air from the baby's tummy if the abdomen becomes distended. Dr Evans says 'free drainage' means the nasogastric tube (NGT) is left in the stomach, the other end is left open, so if any air is in the stomach, it can escape through the NGT.
2:52pm: The court is now hearing the definition of the term 'NEC', pronounced as 'neck' "in the business", a gastro-intestinal disease in the small intestine. Dr Evans says the causes can be poor blood flow, as a result of infection. Sometimes it can appear "without being sure why". "The sicker the baby, the greater the risk," Mr Evans tells the court. Other symptoms are 'a bit' of abdominal distension, bile aspirates and blood in the stool. Early diagnosis is important to lower the need for surgery. The prosecution says NEC will be referred to a lot in the course of the trial.
2:53pm: "Doctors, if they suspect NEC, start treatment immediately" - even if they are not 100 per cent sure of a diagnosis, Dr Evans adds.
2:55pm: One of the reasons for this is some of the babies may not "tolerate" surgery. The court hears NEC is a "serious" medical emergency. The prosecution says if symptoms are detected, they treat swiftly. "And properly," Dr Evans adds.
2:58pm: Different types of rashes are discussed, in particular a purpuric rash where if you press on the skin, the rash does not fade. It is associated with sepsis, or blood clotting, and is a "serious medical problem".
3:01pm: The process of intubation is demonstrated on a video presented to the court.
3:15pm: CPAP is the "least invasive form" of giving breathing support to babies, the court hears. BiPAP is the next stage, and 'full ventilation' "requires a very sophisticated ventilator" and is the most invasive form. A positive sign of "returning to normal" is for the oxygen saturation levels return to over 90%. The respiratory rate is then controlled via the ventilator setting. If the baby 'fights' against that, by trying to breathe independently, that baby is sedated so it can benefit the most from the ventilator.
3:22pm: A video is presented to the court displaying the process of CPAP, and what responsibilities nurses and doctors have while the equipment is attached. The video says it is "inevitable" air will pass into the stomach and intestines, and with time, can lead to "distension of the stomach and intestines". To avoid this, an NGT is inserted into the stomach to help ventilate excess gases. The video says "Despite this, some babies on CPAP will still develop some degree of CPAP belly." Dr Evans says CPAP is the "safest method" as it is the "least invasive".
3:23pm: The video explains there are "other important causes of abdominal distension and it is the doctor's responsibility to distinguish CPAP belly from other conditions, particularly...NEC."
3:25pm: Dr Evans will shortly be cross-examined by the defence's Ben Myers KC on the medical matters raised so far.
3:37pm: We've had a short adjournment. Mr Myers KC is going to discuss some general points raised today with Dr Evans.
3:39pm: Mr Myers asks if the procedure for intubation would be different in a neonatal unit at 3am, compared to that in a lecture on a training dummy.
Dr Evans: "The procedure for intubating a baby would be the same."
"The atmosphere would be quite different?"
"No."
He adds the atmosphere might be different in an ambulance, for example. Dr Evans says there is a "limit" to what you can learn from the videos.3:40pm:
Dr Evans: "What you have is, if you have a baby that requires resuscitation, by definition that is the sickest baby in the unit and requires treatment by the most experienced doctors and nurses."
Mr Myers: "I am talking generally. Would the atmosphere in a generally functioning unit, such as fitting a cannula, be different?"
Dr Evans: "Well of course it would."3:41pm: Dr Evans adds the size of premature babies would vary, from about 600g to over 2kg, and would generally be smaller than that of the mannequin seen in the video.
3:43pm: Dr Evans explains how intubations may not be possible, generally due to "swelling in the surrounding area", in the cords and epiglottis area.
3:46pm: Mr Myers explains the role and clinical experience gained by a neonatologist by working in the unit, which can include "discussions with colleagues" and "variations in different patients and conditions". Dr Evans agrees. Sometime the differences can be "subtle", Mr Myers says. Dr Evans says: "It can depend on each case."
3:47pm: Mr Myers says Dr Evans is not a consultant neonatologist. "I'm a consultant paediatrician," Dr Evans responds.
3:48pm: "The bulk" of Dr Evans' experience is via the unit he set up in the 1980s-2007/8, Mr Myers says, with much of that in the 1980s, alongside other paediatric duties. "In that sense, you were not working exclusively in neonatology," Mr Myers says. "That is correct," replies Dr Evans.
3:56pm: Mr Myers details Dr Evans' CV and says his duties are shared between neonatology and paediatrician.
Mr Myers: "Would you agree you didn't have day-to-day sole experience [of neonatology] over a period of years?"
Dr Evans: "I don't really agree - I'll tell you why. We were where we were in the 1980s as neonatology, which was relatively new. Our generation was inspired to improve the services. "Because there were so few consultants around, you had greater contact with babies than with 10 neonatologists. "The other consultants deferred to my interests in neonatology development. "My experience was huge. "Our on-call system was one in four. I was on call every one in four weekends. "In the 80s and 90s I was looking after neonatals in Swansea and Neath. "My hands-on experience of developing neonatal experience is, I am more than happy to say, is as extensive as anybody's. "I attended neonatal courses...You can attach labels all you want, but in terms of the neonatal experience is...extensive. "I reckon I could intubate a baby today. It's like riding a bicycle. "I am very happy with my neonatal experience, expertise and background."3:57pm: Mr Myers says Dr Evans had not seen a Phillips machine monitor. Dr Evans said a Hewlett-Packard machine was used in his experience, and had introduced them to the hospital.
3:59pm: Mr Myers said Dr Evans retired from clinical practice in 2009, and was not working in neonatology in 2015/6. Dr Evans agrees. Dr Evans says his interest has been in child safeguarding since.
Mr Myers: "This case has involved you in a great deal of neonatology. "That hasn't been the case before, has it?"
Dr Evans: "It has, actually. In clinical negligence, a lot of the cases involved babies. "I have kept fully up to speed with neonatal practice."4:03pm:
Mr Myers: "Would you agree the optimal position would be current clinical practice?"
Dr Evans: "I think the important thing is clinical experience. "You develop your professionalism through the whole of your career. You do not spend the whole of your 40 years attached to an exclusive clinical scenario." Myers: "Clinical practice evolves over years."
Dr Evans: "It does."
M: "If you are not in practice, you are at a disadvantage?"
DrE: "No - you don't simply forget, the day you finish."
M: "I am not suggesting you have forgotten, but if new approaches are made -"
DrE: "If you can tell me of any new approach, then do so, but babies...do not change in the approach of their conditions, and that has not changed in the past 10 years."4:06pm: "I have not retired, I should remind everybody," Dr Evans adds, as he reiterates his experience, adding it would be difficult for him to be present in court if he was working five days a week in a neonatal unit in Swansea. He is able to give an "objective and clear" opinion on the evidence presented.
Mr Myers: "Being an expert witness has been your chief activity [since 2009]?"
Dr Evans: "Yes, I suppose it has."4:09pm: Mr Myers adds one of the training courses is in expert witnesses and 'how to avoid pitfalls'.
Dr Evans: "It's to help prepare for court." Dr Evans is asked about being 'an expert' in being 'an expert witness'.
Dr Evans: "I think that's far too flash for me. My role is to assist the court on some extremely challenging issues. "I call myself an independent medical witness, not an expert."4:11pm: That concludes the trial for today. The case will resume on Monday, expected to open at the slightly later time of 11am.
Monday 17th October 2022
Children A & B (twins)
Parents' statements - Grandmother's statement - Police analyst: Recorded events & messagesChester Standard Live Reporting
10:49am: The trial is due to resume at 11am, but there may be a small delay due to technical difficulties with the court videolink system. The Lucy Letby trial is being heard in quite a small courtroom in Manchester Crown Court, so consequently there are videolink facilities for the press and public, who are watching in separate rooms. For the press, the majority are watching proceedings from the nearby Manchester Magistrates Court (the remainder are at the press bench at the Manchester Crown Court room).
11:09am: Lucy Letby is in court as we await the resumption of her trial.
11:18am: The judge, Mr Justice Goss, has now entered court.
11:21am: Members of the jury are now also filing into court, and the trial will resume imminently.
11:24am: The prosecution will now focus on the cases of Childs A and B, having outlined their cases last week.
11:29am: Letby is charged with the murder of Child A on June 8, 2015, and the attempted murder of Child B, between June 8-11, 2015. Child A, a boy, was born premature in June 2015, the younger of a twin sister (Child B). A reminder that reporting restrictions mean none of the children can be named in this case, and a naming convention of 'Baby/Child A-Q' is being used by the media.
11:30am: Agreed facts are now being read out to the court. 'Agreed facts' are evidence which is agreed by both the prosecution and the defence - ie, the defence does not challenge them.
11:38am: The first witness statement is dated from 2017 and is from the mother of Child A and B. She confirms she had been diagnosed, prior to her pregnancy, with a blood disorder, and had been given medication to treat it. She discovered she was pregnant and it was decided the blood condition would be monitored and managed throughout. It was planned for the babies to be delivered at a medical centre outside of Chester, at full term.
11:41am: The mother was admitted to the Countess of Chester Hospital, and was "very upset", as there had been medical issues diagnosed, and she had been only a week away from moving to the area where the specialist outside of Chester would have delivered the babies.
11:45am: The mother had an emergency caesarean section as her blood pressure levels were high, and the twins were delivered. Afterwards the doctor was "surprised" at how well she was doing, and the mother asked if she could see her children. She was told once she was well enough to sit in a chair, she would be taken to see them. As time passed, she said: "I was getting a little anxious as I just wanted to see my children". It was about 12-1pm on June 8 when she went to see Child A and B, who were both in incubators.
11:48am: She stayed with the twins for about an hour, and was told to rest on advice of the nursing staff back in her room. At about 8pm, a male member of staff came into the room.
"You need to come in quickly, there is something wrong with twin 2."
"All I can remember is coming in and seeing what felt like hundreds of people trying to resuscitate [Child A]."
The mum was asked for permission by medical staff to stop resuscitative attempts.
"I couldn't bring myself to say stop.
"The only thing I could bring myself to do was nod my head.
"One of the things that upsets me the most is I never had the chance to hold him in my arms."11:51am: The mum said, following the death of Child A: "I was frantic, anxious and extremely upset." Afterwards, the mum said she wanted a member of the family to keep an eye on Child B at all times. After saying goodbyes to Child A, upon her return, she was asked if she wanted to hold Child B, who couldn't be out of the incubator for a prolonged period of time. "I felt joy and sadness at the same time."
11:55am: The couple were woken up by a female member of staff to come quickly to see Child B. She said: "My heart sank - not my baby, not again." They were told Child B had suffered a similar situation to Child A, but had stabilised. Blotches and mottling had been on Child B. "[The consultant said] she had never seen this before - I remember being surprised by this." Said consultant had asked to take photos of the blotches, but by the time a camera was arranged, the blotches had disappeared. The mum did take a photo the following day, noticing the hands and feet were still "a little discoloured". The photo, dated June 10 in the morning, is presented to the court.
11:57am: The mum said she would always go to see Child B at the neonatal unit each day from 9am, until the start of the night shift, and would set an alarm to call the designated parent line every 2 hours during the night.
"I was, and still am, extremely protective of her."
"I couldn't help myself."12:00pm: It was said to the mum from a member of the Countess staff that Child A's death, if 'unascertained' from the coroner, could have come from her blood condition. She was "furious" upon being told this, and sought answers. That concludes her statement.
12:06pm: The father of Child A and B has also provided a statement. He said everything was "fine" with the pregnancy up to the 28-week check-up appointment, when concerns were raised over the mum's medical symptom. The mum had contacted the specialist doctor based outside of Chester to see if it was possible for the babies to be delivered as planned, but the couple were told it was "too risky".
12:11pm: The father said the mum did not have the opportunity to see the children that first night, having had general anaesthetic for the birth. He said he took several photos of Child A and B in the neonatal unit that night, and showed them to the mum. The mum had said no-one else in the family was allowed to see the children before she had the opportunity to do so.
12:17pm: The father said the mum was getting increasingly anxious to see the children, and with assistance, was able to get in a wheelchair to the neonatal unit. The father remembered "a nurse called Lucy" explained the baby monitor machines to him, as he was nervous about them. The parents returned to the delivery room after about an hour. Later, they were told by a nurse to come to the neonatal unit:
"There's something wrong."
"You need to come quick, it's twin 2."
I can only remember seeing 'hundreds' of people trying resuscitate.
"We were asked if we were religious, and if we would like to say a prayer."
The parents were told resuscitative attempts had failed.
"Neither one of us wanted to say stop. "
[The mum] was hysterical.
"I said something along the lines of 'you have to let him go, he's not there anymore, you have to let him go'.
"She nodded her head and that gave permission.
"One thing that upsets us both is we never had the chance to hold [Child A] when he was alive.
"We were told he was doing fine, breathing by himself, and doing well."12:20pm: While the mum rested, the father stayed with other family members and Child B. The father said Child A was brought to them by Lucy Letby, prior to the child's transfer to Alder Hey for a post-mortem examination. Upon their return, they were asked if they wanted to hold Child B. The father said he was too scared to, because of Child B's tiny size, and the child needed to be kept in an incubator or her body temperature would drop.
12:23pm: It was 'shortly after shift change-over' at 8pm when the parents returned to the neonatal unit and had had very little sleep. The other family members had left the unit for rest. This was the first time since that none of the family members were by Child B. It was shortly afterwards when a nurse came in to say: "You need to come now" The father said: "I didn't know what to think. My heart sank." They found Child B had stabilised, after the oxygen saturation levels had fallen sharply. The father had said the consultant nurse had given a 'crossed-fingers' to the nurse on duty when she left, as a 'good luck - I hope the child survives]'.
12:25pm: Child B was in the neonatal unit for a further 4 weeks, and the mum went to hospital on a daily basis, including after she had been discharged as a patient herself, arriving at 9am. The father said they had wanted to be kept updated on Child B, day and night, 'no matter what'.
12:30pm: The third 'agreed fact' statement is from the grandmother of Child A and B. She recalls the whole family was "thrilled" at the news of the pregnancy, and were aware of her daughter's blood condition, and arrangements had been made for her treatment prior to, and for the delivery itself.
12:31pm: The grandmother recalls a "commotion" in the operating theatre, and incubators being brought in. The mum was "quite poorly" afterwards.
12:32pm: Nursing staff had told the mum the babies were "doing well" and "both fine", the grandmother recalled.
12:35pm: The grandmother had popped in to the neonatal unit to see the babies "very briefly", noting they were "very small and fragile" before returning to see her daughter in the labour ward, as she was still poorly. It was 'about 8.30-9pm' on Monday, June 8, when one of the nurses ran past the door, saying "It's one of the twins". "I could tell there was a problem, my heart sank. I just immediately thought she was referring to [my daughter's] babies."
12:37pm: "Your baby is very poorly, or has collapsed - it was something along those lines. "We went into the neonatal unit room 1. A member of staff held the doors open for us. "The minute I went into that room and saw that baby boy, I knew he was gone. "Everybody was desperately trying to help him. "The room seemed full of medical staff. "[My daughter] was sobbing uncontrollably at this point - 'please don't let my baby die, please don't let my baby die'." The family were told the situation was not good for Child A.
12:39pm: The grandmother said a doctor had come over to say, three or four times during the resuscitation attempts, saying the situation did not look good and if Child A survived, he would likely be left with brain damage and other complications. Eventually the mum nodded her head silently to indicate to staff to stop.
12:42pm: The grandmother recalled that the following, Child A was placed into a cot, adjacent to Child B's incubator. A nurse had placed a comfortable chair for the mum to sit in, next to the babies. She said the mum would not leave the children unsupervised.
12:45pm: Later, the grandmother was awoken by a mobile phone call from the father. "The only words I could remember him saying were 'the baby's collapsed, she's really poorly." The family members made their way to the neonatal unit. She said: "I was having chest pains, thinking I was going to have a heart attack. I was struggling to breathe, I couldn’t think anything other than I hope [Child B] is OK. "Once we got in, she was not looking good. There was mottling." Child B later stabilised.
12:46pm: The court hears medical records are now going to be looked at.
12:51pm: The court is hearing from Claire Hocknell, intelligence analyst employed by Cheshire Police. She explains data has been obtained from medical records, Lucy Letby's mobile phone, and door swipe data showing access/exits by medical staff at the Countess of Chester Hospital's neonatal unit. Nicholas Johnson KC says if that includes social media searches carried out by Letby. Ms Hocknell confirms that is correct.
12:57pm: Ms Hocknell confirms all the evidence collated for the data records has been served upon the defence in advance of the trial. After the defence had sight of the evidence, additional data record material was sought and added, and any mistakes made in its compilation were corrected.
1:00pm: The court is now adjourning for the lunch break, and will resume later, where it will discuss the medical records further.
2:12pm: The judge, Mr Justice Goss, has returned to the courtroom. The trial shall resume shortly.
2:14pm: The sequence of events, packaged in an electronic display, is presented to the courtroom and on jurors' iPads. The first slides are the original, scanned, neonatal admission for Child A, and a typed up transcription of the doctor's notes.
2:25pm: The package records Child A was transferred to the neonatal unit at 2.41am on June 8, as a note written retrospectively recorded. A 24-hour observation chart records Child A's heart rate, respirations and body temperature. Clinical notes are also shown, along with Ms Hocknell's transcription.
2:43pm: Further medical charts are shown as part of the electronic evidence package, along with the intelligence analyst's transcribed summary. At this stage, the full details of these charts will not be analysed. The prosecutor, Nicholas Johnson KC, explains doctors and nurses will be called into court later to provide more context on these notes.
2:47pm: One of the clinical notes includes a very basic sketch of lungs and the abdomen, to describe Child A's condition, which noted the child looked stable.
2:51pm: The medical records also show an x-ray was taken on Child A, using a portable x-ray machine.
3:02pm: A record labelled 'family update' is made at 7.12am about how 'dad had visited [the neonatal unit] multiple times throughout the night', with the mum not being well enough to visit the twins as she was still in recovery. Another note, made for 7.30am, describes who was working in what role for the following shift, such as the paediatrician of the week, the on-call consultant, the registrar and other clinical staff, registered nursing staff including the shift leader, the designated nurse, and other nurses. Other staff listed for this shift are a nursery nurse and a student placement.
3:07pm: The evidence also shows text messages sent between Letby and colleagues. At 9.21am, a message is sent to Letby asking her to split her shifts.
She replies: "Yes that's fine...is it busy?"
The reply: "We have 3 on CPAP...twins last night...wanted six staff on."
Letby replies: "No problem." At 9.25am, an outgoing WhatsApp message from Letby to a friend says: "...I'm working tonight and tomorrow now as busy."3:12pm: Letby sends another WhatsApp message: "Will just have a quiet one today. Slept well. They have 3 30wkers on CPAP." Her colleague replies: "It will calm down again soon then." Further WhatsApp messages are exchanged, which go into 'a social nature', up until 10.10am.
3:18pm: A message from another colleague of Letby's is sent to Letby.
She replies: "I've been moved forward as busy. Doing tonight and tom." After friendly messages are exchanged, the conversation then turned to work, and how busy work had been.3:21pm: The evidence records an x-ray taken of Child A's chest and abdomen taken, along with notes at 1.53pm indicating no concerns with the child at that time.
3:22pm: Letby's colleague sends a WhatsApp at 2.11pm to Letby: "Oh well, you'll just have to kick me if I start nodding off."
3:27pm: The medical charts show hourly observations are made of Child A.
3:30pm: At 4pm, a cannula is tissued and Child A begins to be fed expressed breast milk for the first time. The note for fluids also shows 10% glucose is provided at 8pm by Lucy Letby.
3:34pm: Swipe data shows the nurses coming on for their night shift. They include, at 7.22pm, Lucy Letby.
3:37pm: Child A was said to be 'stable' in a nursing note, which concludes 'Care handed over to Lucy Letby at 8pm'.
3:39pm: Letby's nursing note is written in retrospect at 7.56am the following day, after Child A had died. Part of the note was 'care taken over at 8pm, emergency equipment checked, fluids calculated. [Child A] nursed on CPAP, peep 5-6cm in air. Observations stable.'
3:41pm: A medical note shows there is no record on the 8pm time slot of Child A's temperature - but there are other hours on the chart prior to that where the temperature is not recorded either, the court hears.
3:47pm: A chart shows any 'major events' that took place for Child A. One was UVC lines at 1pm. The prosecution point out the '10% glucose commenced at 8.05pm', signed by Lucy Letby, as a 'major event' on the chart for the 8pm timeslot.
3:51pm: A further retrospective nursing note, by Letby, refers to the administration of 10% glucose via a long line. Child A was noted by Letby, to be 'jittery'.
3:57pm: Records show a nurse other than Letby is 'using the computer' at 8.14-8.15pm, where she is referring to the family of Child A and B being updated on the condition of Child B. Lucy Letby's retrospective note recorded: 'At 8.20pm Child A's hands and feet noted to be white. Centrally pale and poor perfusion.'
3:59pm: Further nursing notes are shown to the court showing the registrar was called for, as Child A had become apnoeic. He was then 'making nil respiratory effort' and, later, no heart rate was detected. The nursing notes record that, despite 'full resuscitation efforts', Child A 'passed away at 8.58pm'.
4:07pm: The doctor who recorded notes dealing with the efforts to resuscitate Child A, and the time of death recorded, will be coming to court to give evidence, Mr Johnson tells the court.
4:11pm: A minor technical difficulty has curtailed events at court for the day by a few minutes. The trial will resume tomorrow morning (Tuesday, October 18).
Tuesday 18th October 2022
Children A & B (twins)
Police analyst: Recorded events & messages (Child A)Chester Standard Live Reporting
10:33am: The trial is now resuming, with members of the jury filing into court.
10:37am: The prosecution is continuing its examination of the medical notes evidence, collated into an electronic bundle, for Child A. Claire Hocknell, intelligence analyst, is talking through the various electronic slides. The first is a slide showing which nurses were the designated nurses for the children in the neonatal unit on June 8 for the night-shift. Letby was the designated nurse for Child A.
10:52am: The court is shown a series of doctors' clinical notes, written in retrospect on the collapse of Child A before 8.30pm on June 8, and the failed attempts to resuscitate him. The court hears the doctors, including consultant Dr Ravi Jayaram, will provide further explanations and context for their notes when they are called to give evidence in court later.
11:06am: Letby's notes, written in retrospect, record the time of death for Child A, at 8.58pm, that Child A and B were baptised together, and a lock of hair and hand/footprints taken for Child A in accordance with the parents' wishes.
11:09am: Letby searched on Facebook for Child A's mum's name at 9.58am on June 9. A message to Letby from a colleague, shortly afterwards on June 9, following the death of Child A, began: "Luckily it doesn't happen very often here, not that that's any consolation at all."
11:13am: A nurse's note on June 9 records that the family of Child A were offered support throughout the day, and declined to receive a memory box for Child A and photographs at that time as they were too upset and bereaved. The note concludes that the parents were made aware the mementos were there for the family to keep, when they were ready to receive them.
11:17am: Letby sent a WhatsApp message to a colleague saying she "didn't want to see" Child A's parents. A colleague responds: "That's understandable." Letby says: "Don't mind being in [nursery room] 1 but don't want to have [Child B]." The colleague offers to look after Child B, with Letby also present in the room. Letby agrees and says: "I think it'd be good for you."
11:19am: Letby messages another colleague: "I think we did everything we could under very difficult circumstances." She added, in another message: "...I can't look after [Child B] because I just don't know how to feel seeing parents..."
11:21am: Letby responds, in regards to her previous night-shift: "It was the hardest thing I've ever had to do."
11:23am: Letby WhatsApped a colleague, after her night shift started on June 9, to say: "Hard coming back in tonight."
11:29am: The evidence documents move to the non-fatal collapse of Child B. A nurse records Child B's CPAP prongs were found to have been pushed out at midnight, and Child B collapsed at 12.30am.
11:40am: Letby is recorded making another search on Facebook for the mum of Child A and B at 11.31pm on June 10.
11:42am: A further search is made on June 25 at 9.50pm.
11:50am: The court has also been shown a series of messages sent between Letby and nursing colleagues in relation to the death of Child A and the non-fatal collapse of Child B. On June 30, following the deaths of Child A, C and D, and the non-fatal collapse of Child B, Letby's colleague messaged her there was something 'odd' about that night.
Letby replies: 'What do you mean? Odd that we lost three and in different circumstances?' Letby's colleague responds: "I don't know, were they that different?" The colleague added: "Ignore me, I'm speculating."12:03pm: The court had earlier heard messages sent between Letby and colleagues. Letby said in one message to a colleague, regarding the death of Child A: "Think we all need answers." She later messaged to say she had been watching 'An Hour to Save Your Life', about a life working in a neonatal unit. Letby's colleague responded: "...don't really watch things like that...get enough in work". Letby responded: "I just find it interesting, to see how our work is portrayed to the public."
12:07pm: Letby later messaged another colleague, who had been off work after looking after Child A, to say: "Hi [nurse] - you may have heard by now but wanted to let you know that we lost little [Child A] on Monday. Knew you looked after him." The colleague responded: "I didn't know actually, thanks for letting me know. That's terrible!"
Letby: "It was awful...he died very suddenly and unexpectedly just after handover. Not sure why. It's gone to the coroner." The colleague: "Oh god, he was doing really well when I left."12:08pm: Letby had made a further search on Facebook for the mum of Child A on September 2, 2015.
12:10pm: In the same conversation between Letby and her colleague, Letby said: "I was not supposed to be in either - [boss] swapped my nights as unit busy - but these things happen unfortunately." Letby's colleague: "Yeah it's the business we are in unfortunately...hopefully [Child B] will be ok in the end."
12:21pm: Intelligence analyst Claire Hocknell is continuing the walkthrough of electronic evidence to help jurors navigating through it.
12:24pm: Ms Hocknell confirms to the court that not all messages found on Letby's phone are in the evidence bundle; some messages are ones which the prosecution and defence are aware of, but do not deem that relevant for the case.
12:31pm: Kate Tyndall, intelligence analyst employed by Cheshire Police, is now giving evidence.
12:40pm: Ms Tyndall is showing the jury a walkthrough of the 'neonatal unit review schedule' electronic documents, which are to be presented to the court. The talking through of this set of evidence is for Child A. It is a seven-page document showing a timeline of data for all babies being treated in the neonatal unit around the time of Child A's collapse. It is split into the date and time, the baby's name, what type of record is made, a summary of that activity, the member of staff administering that activity (if known), and a cross-reference to where further details of this activity can be found in the electronic evidence bundle.
12:50pm: The timeline highlights events for Child A and recorded activity for Lucy Letby.
1:03pm: Ms Tyndall has finished giving her evidence. The court is now adjourning for the lunch break, and will resume later today.
1:20pm: A small clarification for the 11.50am entry - the messages between Letby and her colleague, written on June 30, initially talk about 'that night' as the night Child A collapsed. The conversation then moved on to the wider topic of Child A, Child C and Child D having collapsed and died in the same month (June). Letby's messages from and to her colleagues will be revisited by the prosecution later in the trial.
2:10pm: The trial has now resumed. The next electronic evidence bundle is being shown, for Child B. Intelligence analyst Claire Hocknell has returned to give evidence.
2:34pm: The medical notes presented to the court are in the same format as for Child A.
2:45pm: Child B's lungs were examined to be "clear" and the child was "very alert" and "active", on the morning of June 9. A 'weaning programme' note is made at 11am, which is for the weaning of Child B off breathing support.
2:49pm: A further nursing note showed Child B was 'very stable' after being weaned off CPAP and allowed time to be with Child B's mum, before returning to CPAP with a view to further weaning off.
3:00pm: A nursing note recorded in the afternoon of June 9 said "maximum support" was being offered to the family of Child A and B, who were still "understandably" very upset.
3:07pm: A diagram of the neonatal unit, showing which nurses were designated to which rooms during the relevant shift on the night of June 9, is presented to the court. Child B is in room 1, while Letby is assigned to look after two babies in room 3. The court hears one of Letby's colleagues is the designated nurse for Child B and another baby in room 1. Following Child B's collapse, another nurse took over looking after the other baby in room 1.
3:19pm: Nursing notes written by the designated nurse, written in retrospect, found Child B's CPAP prongs had been pushed out of the nose, and oxygen saturation levels had fallen to 75%, before midnight. The prongs were repositioned, and after "a little while", the oxygen levels recovered. The heart rate was stable and there was "good respiratory effort throughout". Child B was observed to be "stable" prior to midnight. Letby is then involved with administering nutrition at 12.05am.
3:23pm: Letby is a co-signer for the nutrition prescription at 12.05am on June 10.
3:30pm: A blood gases record by Letby of Child B is made at 12.16am and another at what appears to be 12.51am, the latter "during Neopuffing".
3:33pm: The designated nurse's record for the desaturation and collapse event at 12.30am, written retrospectively, includes the notes: "Sudden desaturation to 50%. "Colour changed rapidly to purple blotchiness with white patches. "Emergency call for doctors put out." A 'fast bleep' alert for a nurse to attend the neonatal unit as soon as they can is made at 12.33am. The court hears this is a 'crash call'.
3:40pm: Following emergency treatment, Child B was placed on a ventilator and 'good air entry' was noted. A doctor entered the neonatal unit at 12.34am and the on-call consultant was called at home at 12.36am. Child B's "colour started to improve almost as quickly as it had deteriorated", and morphine treatment began, while the parents were called to the unit and kept informed at cotside.
3:43pm: Clinical notes recorded by the consultant recorded for 12.50am: "Suddenly purple blotching of body all over with slowing of heart rate. "Bagged and then tubed by registrar. Heart rate came up. Adrenaline not required."
3:45pm: Letby is recorded taking the hourly observations at 1am for Child B in room 1. The prosecution reminds the court Letby was the designated nurse for two babies in room 3 at the start of her shift.
3:48pm: A note timed at 1.09am from an x-ray said Child B's lungs were "mildly hyperinflated" and "clear".
3:52pm: Child B was also noted, from a note at 12.45am, to have a "full/mildly distended" abdomen.
4:02pm: Further medication is administered to Child B during the night, with Letby again listed as a co-signer.
4:06pm: At 2.40am, the 'purple discolouration' had been 'almost resolved'. The cause was '??', and Child B had been 'stabilised at present'.
Wednesday 19th October 2022
Children A & B (twins)
Police analyst: Recorded events & messages (Child B) - other agreed facts - Statements from: Midwife, Dr Gail Beech, Dr Andrew Brunton, Unnamed doctor (trainee) - Nurse Melanie TaylorChester Standard Live Reporting
9:25am: This will be the eighth day the jury will have been in Manchester Crown Court for the trial. A reminder that the case is expected to last six months. The 12 jurors have to make themselves available for every day the trial will be taking place.
10:35am: The trial is now resuming, with Nicholas Johnson KC prosecuting.
10:36am: Claire Hocknell, intelligence analyst employed by Cheshire Police, is continuing to provide the jury with a walkthrough of the electronic evidence bundle in relation to Child B.
10:39am: A nursing note made by one of Letby's colleagues on Wednesday, June 10 at 8.09am recorded that the family were "very upset" after the non-fatal collapse of Child B at 12.30am the previous night. Child A, the twin brother, had earlier died on the evening of June 8.
10:45am: A message sent from Lucy Letby on WhatsApp to a colleague at 12.04pm included the request: "Will you let me know if any change with [Child B]."
10:53am: The colleague's response said the shift had been "manic", and there had been "no change" with Child B. Letby enquired again about Child B that night, at 10.08pm, and was informed Child B was "looking really good".
10:58am: A text message at the end of June, from Letby, said: "I had a mini meltdown last night about what's happened at work... "I just need some time off with mum and dad." The message was sent following the deaths of Child A, C and D and the non-fatal collapse of Child B.
11:10am: Ms Hocknell is asked by the defence about Letby's Facebook searches. She is asked whether Letby searched on Facebook for the parents of children other than those listed in the charges. Ms Hocknell confirms that is the case. "There are a lot of searches for different people."
11:12am: Further agreed evidence is now being read out to the court.
11:16am: The consultant doctor who looked after the mum of Child A and Child B said he had no recollection of the delivery, but could recall the pre-existing conditions the mum had and the "intensive input of care" she received as a result. He said the mum was classed as a "high risk" pregnancy.
11:19am: The consultant recalls in his statement he first met the mum on June 7. "An extensive plan" of care had in place for her by other consultants. He was later informed of a "deterioration" in her blood results and a rise in her blood pressure. The decision was made to transfer the mum to a labour ward to stabilise the pressure.
11:23am: The consultant added further medication was administered to try and stabilise the blood pressure, and the decision was taken to deliver with the permission of the mum. The mum was transferred into the theatre for delivery.
11:25am: Further medication was administered in the theatre as the mum's blood pressure remained high, the consultant adds. The consultant said the priority was to stabilise the mum's blood pressure before general anaesthetic was administered.
11:27am: There were "no complications" and "minimal blood loss" in what was described as a "routine Caesarean section operation".
11:30am: The court is now hearing a statement from a midwife at the Countess of Chester Hospital, which again is 'agreed evidence', in that neither the prosecution or the defence dispute its contents.
11:38am: The midwife recalled her memory of that night shift, and had recorded that following the birth, she told the parents the babies were "doing well".
11:54am: The next 'agreed evidence' statement is from Dr Gail Beech, who worked at the Countess of Chester Hospital at the time. She recalls, in a statement, the care she provided to Child A in the minutes after he was born, including breathing support via a Neopuff device to inflate the lungs, to get the required heart rate. Child A then cried. Further ventilation support was given to Child A with the Neopuff device "for a short time" to reduce the pauses in between breathing. He was then recorded as having "very good" oxygen levels, so the use of the Neopuff device was reduced and Dr Beech noted Child A was "fully breathing by himself". Administering breathing support was "not unexpected" for a pre-term baby. The decision was then taken to transfer him to a neonatal unit. Dr Beech recalls showing Child A briefly to his family en route to the unit. * A previous version of this entry said Dr Beech's statement said 'administering breathing support was 'not expected' for a pre-term baby. We would like to clarify that it the words used in the statement were 'not unexpected'.
11:57am: She recalls 'chest compressions' were seen on Child B, which she interpreted as "a bad sign". "It was difficult to know which baby to assist," Dr Beech recalled, as Child A was still not yet stable. Another doctor entered and Dr Beech said for that doctor to look after Child B. Dr Beech said she did not have any direct care for Child B that night shift.
12:17pm: We've had a short adjournment - and the prosecution will now continue giving agreed evidence.
12:21pm: Dr Beech's recorded observations at the time (June 9) for Child B are shown to the court. There was 'suspected sepsis' and 'jaundice'. A management plan to 'start allowing time off CPAP', among other treatments, is noted.
12:26pm: Dr Beech's note at 2.50pm asked for an "urgent post-mortem" for Child A to look for signs of thrombosis, "as this may have implications for [Child B]".
12:33pm: A video is now played to the court of what the interior of the Countess of Chester Hospital neonatal unit nursery room 1 looked like.
12:36pm: An agreed evidence statement by Dr Andrew Brunton is read out to the court. He records that at 11.50pm on June 7, he carried out observations for Child A, who "appeared well" and was "clinically stable on CPAP".
12:42pm: An x-ray review had shown Child A had a symptom of newborn respiratory distress syndrome, but this was "nothing unusual" for a pre-term baby. The review was recorded during the night of June 7.
12:52pm: The next agreed evidence comes from someone who was a trainee doctor at the time, who is explaining how certain medical procedures were carried out for Child A.
12:59pm: The trainee doctor was called to insert a UVC (a catheter) into Child A on the afternoon of June 8. Following an X-ray, the catheter was "not ideally placed". The trainee doctor then removed and re-sited the UVC, following discussion with more senior doctors.
1:20pm: The court has adjourned for the lunch break. It will resume with further prosecution evidence later this afternoon.
2:09pm: The trial will resume shortly at Manchester Crown Court.
2:13pm: The prosecution is now giving an agreed evidence statement from Dr Sally Ogden, who looked after Child A.
2:31pm: A short adjournment is now being made for preparations to be made for the next witness due to give evidence in court.
2:38pm: The next witness to give evidence is Melanie Taylor, who is in court. She was employed as a nurse at the Countess of Chester Hospital in the neonatal unit in 2015.
2:52pm: The court hears she came on duty at about 7.30am on June 8, the twins having been born the previous night shift. A computerised record shows she was the designated nurse for that day shift for Child A. Miss Taylor explains records of the various medical charts would be cotside, including hourly observations. "The observation charts would be written as we were doing them," Miss Taylor explains.
3:02pm: Miss Taylor confirms she had recently become a band 6 nurse in 2015, having worked at the hospital for several years. She tells the court Child A and B were in neighbouring incubators in the neonatal unit. Child A was "stable", on nasal CPAP.
3:10pm: Miss Taylor explains the medical observations made for Child A during the day shift, via retrospective notes. The respiratory rate was 'slightly raised at times', but Miss Taylor said this was not unusual.
3:21pm: Miss Taylor: "I had no concerns with him, he was stable - on CPAP, but stable. "One thing was he didn't have fluids for a couple of hours because of issues with lines. "The cannula - that 'tissued' at some point during the shift [the vein has 'gone' and it cannot be suitable for a cannula to be used there]. "A UVC was attempted to be put in - but it has to be x-rayed and under sterile conditions and in the right position before we can use that line." The UVC was in the 'wrong position' twice - it had been taken out and re-inserted, but was still in the wrong place. Another option was sought. "They attempted to...[use a] long line, which again has to be done under sterile conditions by a doctor, and again x-rays have to be used." Miss Taylor said Child A would not have had fluids for 'about a couple of hours'. A reading on the chart to say 'cannula tissued' is made by Miss Taylor in the 4pm row. A small amount of expressed breast milk is administered at 4pm and 6pm via the nasogastric tube.
3:26pm: Miss Taylor said she had "no concerns" from the neonatal intensive care unit observation chart measuring Child A's heart rate, respiratory rate and body temperature each hour.
3:31pm: An addendum by Miss Taylor just after 7pm recorded the UVC was in the wrong position, and was reinserted, but was still in the wrong position. Notes shown on the screen record: "Aware no fluids running for a couple of hours," adding a long line was inserted by the registrar.
3:41pm: Miss Taylor said she would have relayed the observations to Lucy Letby at the hand-over, and there were no concerns other than the lack of fluids Child A had had for a couple of hours. The 10% dextrose IV fluid is prescribed, via long line, prescribed by a doctor. A prescription form is shown the court and Miss Taylor explains the various columns and signatures. Miss Taylor: "All fluids will be checked by two nurses - it is signed [on the prescription form] that I have checked it with Lucy Letby." The time and date the medication is started is June 8 at 8.05pm.
3:46pm: Miss Taylor explains emergency equipment checks are made at the time of the hand-over - in this case, 8pm.
3:54pm: Miss Taylor said she would have started writing up a nursing note, but Child A then started deteriorating, so the note would not have been saved on the computer. She said she would have been able to see Child A's incubator when sat at the computer. She said: "Lucy Letby was standing by the incubator. Initially I stayed there [when Child A started deteriorating] as he was fairly stable and Lucy Letby was there, but when I realised he was not recovering from deterioration I got up to help Lucy Letby." She said the baby monitor would have alarmed. Miss Taylor said she is unable to say how long she had been away from the incubator, and thinks it was after the dextrose was administered. Miss Taylor said she thought Child A was going to recover "quite quickly" as such desaturations were not that uncommon, but when it became clear he was not going to recover she went to help. "I kept thinking he was going to recover, but he didn't." Miss Taylor said she was not directly involved in the resuscitation, but involved in getting adrenaline medication. The following day Miss Taylor was called back to the hospital to finish the notes which had not been completed at the time, 'due to the trauma of what had gone on'.
3:55pm: Ben Myers KC, for the defence, is now questioning Miss Taylor.
3:57pm:
Mr Myers: "Do you find that even with the notes, it can be difficult to recall what happened?" Miss Taylor: "It is, but...in my witness statement, if I was not sure, I said I was not sure."4:02pm: Mr Myers examines the staffing levels at the Countess of Chester Hospital neonatal unit. For babies in intensive care, it should be one nurse to one baby', he tells the court, and 'one nurse to two babies' for high-dependency babies, and 'one nurse to four babies' in the special care nursery room, he tells the court. Rotas would be relayed to staff "a month in advance", Miss Taylor says. "If they [the neonatal unit] were busy", then some nurses would be asked to come in "at short notice".
4:06pm: Miss Taylor explains the shift leader gives the hand-over to the new nurses coming in for the following shift in a 'huddle', lasting '10-15 minutes'. The shift leader would be a 'band 6 nurse'. The shift leader is "usually pre-allocated", but could change. There would be a 'handover sheet' with babies' names and an outline of care provided the previous shift.
4:07pm:
Mr Myers: "And that handover sheet would be kept by him or her throughout the shift?" Miss Taylor: "Yes, that's correct."4:08pm: "Generally," that handover would last until about 8pm, the court hears.
4:13pm: Mr Myers explains that some duties "require two nurses", such as administering medication and checking it is correct. Mr Myers points to a section of the intensive care unit chart for Child A, where a different nurse to the designated nurse has signed for the observations at 4am on June 8. The designated nurse has signed for other hours including 2am, 3am and 5am. He asked Miss Taylor: "There is absolutely nothing unusual about that, is there?" Miss Taylor responds: "No."
4:18pm: The court is now adjourning for today. Mr Myers will continue to ask Miss Taylor to give evidence tomorrow (Thursday, October 20). We will provide updates throughout the day.
Thursday 20th October 2022
Children A & B (twins)
Nurse Melanie Taylor - Dr David Harkness - Statements from: Dr Christopher Wood , Nurse assistant Lisa Walker, Nurse Joanne WilliamsChester Standard Live Reporting
10:00am: When the trial resumes this morning, Letby's defence, led by Ben Myers KC, is expected to continue to question nurse Melanie Taylor about the night Child A died on June 8, 2015.
10:33am: The trial has now resumed. Mr Myers asks Miss Taylor about the layout of the Countess of Chester Hospital neonatal unit.
10:38am: Mr Myers said Child A would have required "constant observation" despite being deemed "stable" in the neonatal unit. Miss Taylor agrees. He added that pre-term babies would also be "prone to infection". Miss Taylor agrees.
Mr Myers: "They can be prone to collapses, can't they?" Miss Taylor: "I don't know if I would agree with that, exactly."10:44am: Mr Myers said a baby fitted with a UVC would be 'intensive care'. Miss Taylor agrees. Child A had become an 'intensive care baby' during the day shift as he had required. Mr Myers said Miss Taylor would have been looking after an intensive care baby (ITU), as well as another baby which required a lot of care - which falls outside the guidelines. "In terms of ITU, they technically are intensive care, but not as intensive - some babies require a lot of hands-on, one-to-one care. Some technically become ITU, but in terms of care, they are more like HDU."
Mr Myers: "Were there, at the time, a lot of poorly babies?" Miss Taylor said that particular shift was a busy one, she recalls. She accepts that an increased number of poorly babies coming into the unit would create an increased demand on nursing staff.10:45am: Mr Myers asks why a baby's temperature would not necessarily be recorded every hour on the chart. Miss Taylor says the temperature records involve putting a thermometer under the baby's arm, which the "babies don't like", while a heart rate is done on the monitor, while the respiratory rate would be manually counted through observation.
10:49am: Mr Myers asks if handling babies (for example, to take their temperature) could led to an increase in the baby's stress, which would lead to an increased risk of deterioration. Miss Taylor: "...to a certain degree, yes." She adds if a temperature is recorded for one hour in a stable reading, the baby's temperature would not necessarily be taken on the following hourly check.
10:55am: Melanie Taylor's nursing note for June 8 is shown to the court, at 1pm. It documents the insertion of the UVC for Child A. Miss Taylor said she cannot remember the two attempts of insertion of the UVC, but sees it is made on her notes. The note, written at 7.05pm, says: "UVC in wrong position, reinserted...again in wrong position. Cannula tissued. Doctors busy on ward 30. Aware no fluids running for a couple of hours. Long line inserted by Reg Harkness. awaiting X-ray. Remains settled on NCPAP. Enteral feeds of donor expressed breast milk started at 1ml/2hourly."
10:59am: The intensive care chart is shown to the court, showing 'cannula tissued' at 4pm. Miss Taylor explains she might have written 'cannula tissued' retrospectively, so it could be before or after 4pm when that was noted. Mr Myers said Miss Taylor would have had to wait for a doctor to put a long line in.
Mr Myers: "You said it was very busy - and that caused a delay, didn't it?" Miss Taylor: "Yes."11:05am:
Mr Myers: "It's important to make sure the tip of the long line is in the right position, isn't it?"
Miss Taylor: "Yes."
"It's a sterilised procedure? It's very thin."
"Yes."
Miss Taylor says she's not too familiar with the long lines as she is not involved with the procedure. The judge clarifies Mr Myers' question, asking if it is important to get fluid in once the long line is in place. Miss Taylor agrees.11:08am: Miss Taylor says she is not aware of anything that might have been running through the long line prior to the 8pm 10% dextrose administration. Mr Myers adds "the conventional practice" is for fluids to be administered immediately in the long line after it is inserted. "Yes. Ideally we would get an x-ray first." Mr Myers says there was a delay because the doctor was delayed elsewhere. Miss Taylor: "I think so."
11:12am: Miss Taylor is asked about the retrospectively written note at 9.28pm on June 8, which begins. "Observations stable, pink, well perfused. UVC still insitu, but in wrong position, to be used if no other access available. "Long line inserted by reg Dr Harkness, secured, x-rayed. 10% dextrose run through and connected to long line."
11:17am: An observation chart showing the respiration rate is 'elevating', Mr Myers says, throughout the day is shown to the court. "Yes, a little," replies Miss Taylor. A blood gas record chart shows the lactate levels had increased on the records of 12.13am, 6.37am and after 2pm, with levels at 1.6, 2.6 and 2.7. The latter two readings are, Mr Myers says, outside of the desired area. No other records are given.
11:21am: Miss Taylor says she does not know what time the long line was inserted. Mr Myers says there was a delay in getting the x-ray. Miss Taylor: "From memory, I cannot remember the timings, but possibly." Letby's notes, written retrospectively at 7.56am on June 9, are shown to the court. They begin: "Glucose commenced via long line...UVC remained in situ from day shift, instructed line not to be used by registrar. "[Child A] noted to be jittery, was due to have blood gas and blood sugar taken. "At 8.20pm [Child A] hands and feet noted to be white. Centrally pale and poor perfusion..."
Mr Myers: "He should have been getting fluids during this four-hour period, shouldn't he? Miss Taylor: "Yes."11:24am: Miss Taylor says she cannot remember whether it was herself or Lucy Letby who administered the fluids. Mr Myers said "two nurses" are involved in the process, and one has to be in sterile conditions. Miss Taylor: "I honestly don't know whether it was me or Lucy [who was in sterile clothing]."
11:26am: The defence say it was Miss Taylor who was the one in sterile clothing for the fluid administration, with Lucy Letby assisting. Miss Taylor says it could have been that, or the other way around.
11:30am:
Mr Myers: "When the deterioration commenced, you were at your computer making notes?"
"Yes."
A note by Miss Taylor is made at 8.18pm for Child B.
"It shows you were at the computer at 8.18pm?"
"Yes."
"Was Dr Harkness also in that room?"
"I don't remember."
"You could see where [Child A] incubator was, and the alarm sounded."
"Yes."
"When you went over to Child A, could you recall whether he was breathing or not?"
"I don't recall."
"Would it be fair to say that what followed makes it difficult to recall - that there is a lot of activity surrounding the cot?"
"When you realise that extra support is needed, yes."11:31am:
Mr Myers: "Lucy Letby went to support the family at one point, do you recall that?" Miss Taylor: "I don't remember that." Miss Taylor says if Letby was the designated nurse, she would be involved with assisting the resuscitation attempts. She adds that designated nurses would often be the one to provide support to the family afterwards.11:32am: Memory boxes, Miss Taylor says, are collated with permission of the family.
Mr Myers: "Do you recall about whether there was any discussion about whether the fluid bag should be kept?" Miss Taylor: "I don't recall that, no."11:39am: Miss Taylor is presented with an interview transcript, dated February 7, 2018, one of a series of interviews she had involving babies in her care at the Countess of Chester Hospital. The interview says Miss Taylor believed that sometimes, babies collapsed with no explanation. Miss Taylor: "When I said that, that is what I believed to be true - whether that's my rational brain, trying to rationalise what happened." Mr Myers reads from the statement: "It's a shock to us, because we have such a low rate." Miss Taylor: "That is what I believed, that was my opinion at the time. I tried to rationalise what happened at the time. Whether that's true - I'm not medical - but that was my opinion at the time." The prosecution say this interview concerned a different set of twins. Miss Taylor: "I feel like I shouldn't have said that - I tried to rationalise that, because as a nurse, that is what I tried to do."
11:43am: The prosecution shows the intensive care chart to the court again, focusing on the feeding records between 4pm-8pm. The feeding of expressed breast milk at 4pm and 6pm were "trophy feeds". Miss Taylor explains small amounts of food are for the stomach to be lined so it could help get the stomach used to future feeds. A 6pm 'output' of 25mls of urine is noted. Miss Taylor says that is weighed via the nappy - a "tried and trusted method", the prosecution say. "Does that show fluids were passing through [Child A]?"
"That does."
"Does it follow that fluids that go out must have gone in?"
"It does that fluids that have gone in through the day, yes."11:48am: Blood gases records were noted by the defence as "being outside the optimum range". The prosecution say with those records in mind, was Child A still 'stable'? Miss Taylor: "Yes." She explains the elevated respiratory rate was not uncommon, and other symptoms, such as the baby grunting, would be noted as part of a bigger picture. The elevated respiratory rate and blood gas level would not be, in isolation, uncommon, but still "relevant". Miss Taylor says she does not remember Child A being "jittery", and had not documented it in her notes. She says if she had seen Child A being jittery, she would have noted it. She adds it would be considered as part of a bigger picture. "It does not necessarily [mean] a concerning cause, but it is something to consider."
11:49am: That concludes Miss Taylor's evidence for Child A and B. The court hears she will be asked to return to court to give evidence on other babies.
12:00pm: The court has had a short adjournment while the next witness comes in to give evidence.
12:07pm: The next witness to give evidence is Dr David Harkness. The court hears that in 2015 he was a paediatric registrar, sometimes based at the Countess of Chester Hospital. He confirms he has, since then, been interviewed by police, and made witness statements about more than one baby which was a patients at the neonatal unit. He is being asked about the case of Child A.
12:12pm: He confirms that at the time, he was a registrar and was on duty on the evening of June 8. His clinical notes, written in retrospect at 9.30pm, record for 5pm: "UVC in situ on my arrival on NICU at 5pm. No definitive access at this point, so I've left in situ with plan to remove if long line sited or pull back to low position is long line not successful." He said he was looking after children outside of the neonatal unit prior to 5pm, and on his arrival, his "first port of call" was seeing Child A.
12:15pm: He says the UVC is preferred as a feeding method to the long line, and can be moved to a low position as a short-term measure until something better is in place. The prosecution say a UVC was in place, an x-ray was taken before it was used for purpose of administering fluids. If it is "imperfect" in position, the options are withdrawing, or adjusting it. The latter would be on a short-term basis. The doctor agrees.
12:19pm: A note by Dr Harkness at 7pm: "Long line inserted at 1st attempt." A sticker confirming the insertion of the long line is placed. An x-ray review sticker is also placed, timed 7.09pm. Dr Harkness said he was junior at the time, so would have recommended the long line be moved back slightly, as outlined in his recorded note, but now he would say the long line was in the right position.
12:24pm: Dr Harkness said because the night of June 8 was a "traumatic event", his memory of entering the unit room was "quite fresh" and he explains there were three babies in the nursery room 1 - the intensive care unit, at the time, and two of them would have been Child A and Child B. He describes which incubators they would have been in, which are adjacent to each other. A video of the layout of the nursery room one is played to the court and Dr Harkness confirms where Child A and Child B would have been located.
12:31pm: Dr Harkness's x-ray review said at the time the x-ray was available to review, he was "scrubbed inserting a line into another patient", which meant he had to adhere to sterilised conditions, he explains. The doctor's opinion at the time was the position of the long line was "less than perfect", the prosecution said. Dr Harkness said that following consultation and in accordance with guidelines, the position of the longline was "actually correct".
12:35pm: He said he was "just about finished with [another baby]" when he was called to Child A at 8.26pm. Bagging was started "via Neopuff immediately". The saturations, which "should be in the 90%'s", were in the '70s-80%'s'. The heart rate was "slightly on the lower side", Dr Harkness records. He said he can remember the events.
12:37pm: He said he was called "by nursing staff" over problems with Child A's breathing. A junior doctor took on the responsibility of making contemporaneous notes for Dr Harkness during the event, the court hears.
12:39pm: He said it was "most likely nursing staff" who started the Neopuff bagging process by the time he arrived. "Good chest movement seen" meant there was not a blockage, Dr Harkness explains.
12:44pm: Dr Harkness said as far as he was concerned the longline was the last thing which was inserted, so he removed it at 8.27pm. He said: "That was my immediate thought. In hindsight...there was no possible link [between its insertion and the collapse]." He said if the long line had been moved further in, towards the heart, it could have caused a significant increase in the heart rate, or other heart complications. There was no evidence then, or since, which had supported that, he explains. Help was called at 8.27pm. Child A was "intubated at the first attempt".
12:56pm: The note records intubation was at 8.28pm. Child A's heart rate fell to 60-70 the same minute, it was noted. Dr Harkness had said ideally the heart rate should be above 100, and chest compressions are started when the heart rate is at 60. Chest compressions were started and fluids including adrenaline are administered. The court hears while air was still getting into the lungs, "unfortunately" there was no heart rate detected at about 8.33pm. Further chest compressions and medicinal doses are given up to 8.49pm. A heart rate of 50-60 is noted at 8.50pm, and a further adrenaline dose is given, but then there is no heart rate again, and CPR continues until 8.57pm. At that point a review was carried out by Dr Ravi Jayaram in attendance, and no heart rate was present. Dr Harkness says: "It was felt the kindest thing to do was to stop resuscitation."
1:17pm: Dr Harkness said the circumstances of Child A's death were "very unusual and very unexpected." He said: "It was very surprising to be called back [to Child A] at this time [as he had been stable]. "It was very unusual - the skin [patterns] I had never seen before, and I have only seen again at the Countess of Chester Hospital. "I was faced with a baby unexpectedly deteriorating." Dr Harkness noted there was "unusual skin colouring."
1:20pm: Dr Harkness said he had only ever seen this "patchy" skin colouring and pattern in one other baby at the Countess of Chester Hospital, when dealing with the case of Child E and F.
1:56pm: Dr Harkness said he could not remember the exact pattern of the skin at the time as he was "busy trying to save [Child A's] life" at the time, but "it was unusual enough for me to make notes and document it." He added he had, with his experience of being a doctor, "unfortunately" seen dying or dead children patients and the type of skin blotching and patterns that would be found, "but not a pattern like this".
2:11pm: The court has had its lunch break, and the trial is ready to resume with Dr Harkness giving further evidence.
2:16pm: Dr Harkness is asked to examine a clinical note. During the time he was looking at a third baby in the room, he was scrubbed up and sterilised for a procedure which "takes a lot of concentration."
"Typically, you are left to your own devices." He said it was shortly after that (about 1-2 minutes), he was urgently called to Child A.2:35pm: Dr Harkness is now being asked questions by the defence. Mr Myers says what happened was "a tragic event". He said "You have given us a description of skin evidence which was unusual." Dr Harkness agrees the skin patches of purple, blue, red and white were "very striking", but adds he was not forensically analysing the skin at the time. Mr Myers refers to notes retrospectively written at 9.20pm-9.30pm and attributed to Dr Harkness, which does not refer to skin condition. "You could have put anything you wanted in these notes? "Nowhere do you make reference to skin colour." Dr Harkness said the "significance" of the skin colour changes was noted later, following conversations and the non-fatal collapse of Child B.
The defence asks Dr Harkness if he had been "influenced" in his recollections, that had led him to form the impression of the skin pattern in Child A. He said at the time it was an "emotional" time, as it was "one of the first" neonatal deaths he had seen in his experience, and he had found it "greatly upsetting". He added that at that time his documentation may not have been as detailed. The defence say the skin patterns are also not referenced in Child A's inquest report from October 2016, but "pale and poor peripheral perfusion". Dr Harkness admits it's "not clearly documented" but he would still have been in an emotional state. Mr Myers asks that by the time of the police statement, his impression had been formed. Dr Harkness says his statement of observations in the cases of Child E and F had jogged his memory for Child A's skin patterns.2:39pm: Dr Harkness says "there was no evidence" for the long line to have moved in Child A. "This has been proved on the post-mortem." Mr Myers says would the long line have still been in there at the time of the post-mortem?
Dr Harkness: "No, and there was no damage [found] there [where the long line had been]." Dr Harkness said the long line was removed at 8.27pm as a "theoretical" concern "based on no evidence at the time". He said the last new thing, as far as he could know, was the addition of the long line at the time of the collapse. He adds: "The logical thing was to remove it."2:41pm:
Mr Myers: "There are dangers with a long line too close to the heart?"
Dr Harkness: "Yes...that was my concern at the time. There was no evidence at the time or subsequently that that long line did any damage."2:45pm: Mr Myers refers to the x-ray review from 7.09pm, and the position of the long line at that point. Dr Harkness noted it was "to be pulled back." He explained the review took place at 7.10pm - it would have been reviewed during the procedure I was doing." He said his view the long line was to be pulled back was made 'with his experience and knowledge at the time'. "It was not a danger then and it's not a danger now. With my experience and knowledge then, that was my assumption. The guidelines and subsequent experience say...it was fine. It's ideal." Dr Harkness said he likely inserted the long line 'between 6pm and 7pm'.
2:48pm: Dr Harkness explains the x-ray dept takes 15-30 minutes to come to the department with a portable x-ray. "You wouldn't expect to report these in 30 minutes. An hour would be more likely."
Mr Myers: "Surely if the long line was in the wrong position, you would want to know immediately?" Dr Harkness says "In an ideal world" the x-ray would have been made available immediately, but "in reality" it was "impossible". He agrees the x-ray result could have been available more quickly with extra staff and if he had not been treating another patient at the time. The decision to administer the 10% dextrose was because it was "safe" for all over the body.2:53pm: Dr Harkness said he was able to review the x-ray as soon as the image was made available from radiology, and fluids were able to be administered at that point, as he wanted to check for the x-ray first. He says there would be "reluctance" from nurses to administer fluids without having seen an x-ray first. He says, from his experience, medical staff are "much more keen" to administer the fluids, while nurses would want to see the x-ray result first. Dr Harkness says the long line was in the right position, and the use of it was appropriate. The prosecution ask one more question about the "striking discolouration".
Dr Harkness: "Categorically, yes, there was discolouration." That concludes Dr Harkness giving evidence for Child A.3:07pm: More 'agreed evidence' - evidence which is agreed by both the prosecution and defence - is being read out, via a statement. The next statement is from a junior doctor, Dr Christopher Wood, who assisted Dr Harkness in the long line procedure by preparing sterile equipment.
3:12pm: He said he did not remember hearing a 'crash bleep' at the time of Child A's collapse, but he was very close by at the time. Swipe data suggests Dr Wood had previously entered the neonatal unit at 7.40pm.
3:16pm: He said that he was "the least experienced person there", so "took a step back" and began scribing. All the times on the record had come from a fob watch Dr Wood had, and said scribing was "an important role". He documented what fluids were administered, as said by Dr Harkness, and which staff members were present, and the events which followed.
3:21pm: He added he left the room at the conclusion of the resuscitation attempts to give the family of Child A some space and privacy. He added it was "only natural" doctors would look back and wonder if they could have done anything differently. He added: "The death came as a shock," saying there had been no concerns "flagged" at the start of the shift for Child A.
3:35pm: Countess of Chester Hospital neonatal nurse assistant Lisa Walker said, in her agreed evidence statement, she was not working in the neonatal room 1, but knew it was "very busy" that night. She said she could "recall the sadness in the atmosphere in the unit" that night. She added she could recall an increase in the number of neonatal unit deaths at the time, and prior to that, in her 10 years, "there was only news of a couple of deaths". She added: "I remember thinking, 'what on earth is happening?'" in relation to the increased number of neonatal unit deaths. The witness concludes, in her statement, that she had a lot of interaction with Child B as she recovered in the weeks following her non-fatal collapse and subsequent relocation to nursery room 4, and was in contact with the mother.
3:42pm: Further 'agreed evidence' statements are being read out by the prosecution, made by Countess of Chester Hospital staff.
3:53pm: Joanne Williams explains she was the designated neonatal unit nurse for Child B, who was in room 1. The shift on June 9 was not "unusually busy", but they were "always busy". The screens were put up for the family following the loss of Child A the previous night. She assisted the mum with skin-to-skin contact, and taking "lots of photos". Child B became tired so was placed back in the incubator. Throughout the shift, Child B was "stable" and "nothing significant happened". She was "breathing for herself".
Ms Williams said she tried to keep the atmosphere "calm and relaxed" for the family. "Although I had no dealing with [Child A], [the death] had come as a shock." She adds: "Throughout the shift, [Child B] was progressing well," with a slight rise in her breathing rate, which she put down to Child B being tied after being taken out of the incubator. Child B was "doing relatively well". Although she said nurses "can never become complacent", there were "no obvious signs that caused any concern" when she went off the shift that night. When she arrived for her next shift, the reventilation of Child B "came as a bit of a shock". She added that babies "can deteriorate quickly".3:55pm: That concludes the evidence for today. The trial will resume tomorrow (Friday, October 21). We will continue to bring updates throughout the day.
Friday 21st October 2022
Children A & B (twins)
Dr Harkness - Professor Owen Arthurs (radiologist) - Senior neonatal Nurse Caroline Bennion - Nurse A (Shift leader)Chester Standard Live Reporting
8:29am: One of the doctors giving evidence on Thursday told of the 'striking' discolouration found on Child A's skin following his collapse, which he had 'never seen before'.
10:07am: The trial is due to resume at 10.30am, with the prosecution calling further witnesses to give evidence in the cases of Child A and B.
10:35am: There has been a short delay in starting, but the trial is expected to resume imminently.
10:42am: A legal discussion has resulted in a delay to the start of today's hearing. The trial is now expected to start at 11.15am.
11:34am: The trial is now resuming, with the next witness, Prof Owen Arthurs, consultant paediatric radiologist at Great Ormond Street Hospital, giving evidence. The court hears he has reviewed "many of the children in this case", and will be asked questions about Child A and Child B.
11:43am: Prof Arthurs is asked about a post-mortem x-ray for Child A. He comments "unusual findings" in gas and air found in the baby boy, including "a line of gas just in front of the spine".
11:44am: He said such a finding is not found in cases of 'natural causes' death in babies.
11:47am: Trapped air such as this, Prof Arthurs explains, could be found in cases such as road traffic accidents, or infection such as sepsis - overwhelming infection in the organs of the body, or "very occasionally" outside of hospital in 'sudden unexpected death in infants'.
11:52am: Prosecution: Have you seen this much gas in a baby before?
Prof Arthurs: "Only in one other case, which I think we'll explain later on [another of the children in the Letby case]." Prosecution: "What was your final opinion?"
Prof Arthurs: "This was an unusual appearance. In the absence of any other explanation...this is consistent with...air being administered."11:57am: Ben Myers KC is now questioning Dr Arthurs. He asks questions about 'air in the body' and analysis of them.
Mr Myers: "Radiographic evidence of air embolus is rare, isn't it?"
Prof Arthurs: "Yes."
"On post-mortem imaging, the presence of air may also be the result of medical procedures or placement?"
"Yes."12:00pm: Mr Myers asks if the presence of a UVC or long line for some time could lead to air in the system. Dr Arthurs agrees. Prof Arthurs says the "assumption that an image is needed to prove an air embolus is wrong".
12:05pm: Prof Arthurs says his review of the cases involved him, to give a conclusion of 'unusual', having to look through a number of past cases. Mr Myers says that translated to similar findings in 25% of the total number of past cases he had gone through.
12:14pm: Mr Myers says Prof Arthurs looked at 500 cases at Great Ormond Street Hospital, which after narrowing down the criteria, amounted to 38 babies aged under two months, and of those, eight had gases in the greater vessels. Prof Arthurs said there were "no unexplained cases" of gases in that location. The causes found included trauma, a road traffic accident, sudden unexpected death in infants or congenital heart disease. Mr Myers said that does not include many cases of babies in similar circumstances of death of babies aged under four days old. He says there are "many variables" in such a study.
12:17pm: Prof Arthurs says air can be 'distributed' in the system during CPR.
12:20pm: For Child A, Mr Myers says "one possibility" of the air seen on the image is air administration. He says others can be through resuscitation or post-mortem changes.
Prof Arthurs: "Yes."12:28pm: For Child B, the radiograph image shown from June 10, about 40 minutes after the time of the non-fatal collapse.
Mr Myers: "On that image, there are no features which support an air embolus diagnosis?"
Prof Arthurs: "Yes." He clarifies from a question by the prosecution that it could not be concluded either way. Prof Arthurs says his observational study was from "a large body of evidence". The judge, Mr Justice Goss, asks about the study as the jury has not seen it. Prof Arthurs said the study was carried out for children (up to 18 years old) in 2015 and looked at 35 cases, with 10 having some gas in the larger vessels. The study was published, peer-reviewed and available in literature. He tells the court "probably none" were of premature babies. The study was performed independently of the trial, the court hears, and was prior to Prof Arthurs' own review, for babies, carried out later at Great Ormond Street Hospital, involving hundreds of cases.12:32pm: The court is now adjourning for an early lunch break.
1:29pm: Due to the early lunch break, the trial is expected to resume earlier, for 1.40pm.
1:43pm: The trial is now resuming.
1:47pm: The next witness to give evidence is senior neonatal practitioner Caroline Bennion, who was present for the delivery of Child A and Child B in June 2015.
1:49pm: She recalls that Child B required assistance at birth, and that support was given for her. She explains more support was required for her than Child A.
1:53pm: Child B "recovered well" and, after review, she was tried off the ventilator as she was "vigorous" and was breathing by herself.
2:04pm: She is now being asked about "the significant event" for Child A on the evening of June 8. Child A suffered a collapse and died during that evening. She says she was in the room when that collapse happened. She knew that she had taken the handover - a "comprehensive update" from the day-time shift staff - from 7.30pm, and carried out equipment checks.
2:07pm: She said, from reading her statement, she was "next to [Child B]" and "still doing" her checks and completing observations and safety checks at the time. She said she "wouldn't have left" Child B. She said she remembered Lucy Letby asking for help on Child A. "When it became more obvious she needed assistance and [Child B] was safe, I went over to help." She said she did not have a recollection whether the alarm went off.
2:08pm: She said it was a "busy evening" with babies having long lines put in, and the nursery was "quite full" with the cross-over of day and night staff. She also said Dr Harkness was in at the time.
2:09pm: She recalled she helped Lucy Letby give some ventilation breaths via the Neopuff device.
2:10pm: She said there was no crash call put out as the doctors were already in attendance.
2:12pm: The nurse recalls drawing up the emergency drugs required during Child A's emergency treatment. Child A passed away following a series of resuscitation attempts. The nurse said she then returned to treatment of Child B.
2:17pm: The court is shown the nurse continued to take hourly observations for Child B. She confirms "nothing unusual" was noted during the rest of that night shift for her.
2:21pm: Questioned by the defence's Ben Myers KC, the nurse says she had many years of experience in neonatal care. She is asked about if there were challenges in staffing levels. The nurse replies: "We were always very fortunate to have a lot of senior staff."
"There were occasions where we had busier periods, but that is the nature of a neonatal unit."2:24pm: The nurse agrees the babies were "vulnerable" and "could deteriorate very rapidly". She agrees 'it was known' a deterioration could happen when a baby was almost ready to go home.
2:28pm: Ms Bennion is asked about medication that is given to babies who would 'otherwise be at risk of infection'. For Child A, she is asked about such a prescription, and a 'clinical indication' is for 'suspected sepsis' on June 7 at 10pm. The administration of the dose is dated at June 7, 10.46pm.
2:38pm: Ms Bennion is being asked about blood gas records for Child A. The blood gas machine was "on the unit" in the next room, taking about 3-4 minutes, providing an automatic read-out to be attached to the chart.
2:47pm: Ms Bennion is shown a copy of the neonatal record chart, about how some of the tasks and times are shown taking place on the hour, when they might be around that time. My Myers says that as some tasks take some time, it could give the impression a member of staff was 'in two places at once'. The nurse agrees.
2:52pm: Ms Bennion is now being asked about Child A's collapse, and that Lucy Letby had called for assistance. She said: "We have an emergency buzzer which could be pulled, but there were so many staff that a nurse can call for assistance.
Mr Myers: "That would be appropriate?"
"Yes."2:54pm: Ms Bennion is asked if there was any 'formal support' for nurses, particularly for dealing with incidents such as when an infant died. She said there was no formal support, but said of the nursing team: "We were very supportive of each other."
2:56pm: She said there was "no formal procedure or form for everyone to fill in." She added: "Under the direction of the medical staff, a debrief would always be offered. We have a supportive management team and...in the network of our close unit [if a nurse did not want to return to room 1 for the following shift following a traumatic event the previous shift], that can be provided."
"Even after a tragic event, you have to remain professional in the care you give."3:00pm: Ms Bennion adds, from a follow-up question from the prosecution, that simultaneous observation of two babies would not happen, even if the documentation would appear as simultaneous on the records. She is asked about the "speed of the deterioration" of Child A. Ms Bennion said it was "very rapid, very sudden". "It's like a jigsaw, you're putting in observations, but there was nothing to say [Child A was going to collapse]. "However it has happened, and it can happen."
3:17pm: The next witness [Nurse A] is someone who was also working at the Countess of Chester Hospital, as a neonatal nurse in June 2015. She describes, on staffing levels: "There were definitely periods when we were short-staffed, periods when we were ok." For shifts when they were 'short on numbers', they would look to bring staff and swap on the rota, or if anyone could do an extra shift. Agency or bank nurses were a possibility, but didn't happen very often.
3:28pm: The nurse [Nurse A] was the shift leader at the neonatal unit on the night-shift for June 8. Lucy Letby was one of the designated nurses.
3:35pm: The nurse remembers walking by the neonatal unit room 1 and seeing Dr Harkness in there at the incubator for Child A. Swipe data showed her coming into the neonatal unit at 8.20pm. She said: "I was like, something has happened. "With my experience, I was thinking he was having a sort of 'episode' that babies can have." She believed it was down to one of a number of medical conditions. She recalls seeing who else was in the room.
3:37pm: She recalls the Neopuff device was being used to give Child A breaths, as he had "stopped breathing". She recalled being told it had happened "suddenly".
3:40pm: She recalled being involved in the resuscitation attempts, and was physically holding Child A at the time.
3:43pm: She recalled she had "never seen a baby look that way before", with a skin discolouration on a pattern she had "never seen before". Asked to describe the discolouration, she said he was "white with purple blotches", with a bit of "blue", and it had "come on very suddenly". "Just very unusual, it was," she added.
3:54pm: The nurse will continue to give evidence next Monday. The court is now adjourning for today. We will continue to provide live updates next week.
Monday 24th October 2022
Children A & B (twins)
Nurse A - Dr Rachel Lambie - Dr Ravi Jayaram10:40am: I'm back at Manchester Crown Court this morning for the trial of Lucy Letby. Jurors currently hearing from a nurse, who cannot be named for legal reasons, who was on shift the evening Child B fell ill. She recalls that there was no concerns for her health when she began her shift
11:12am: The nurse is telling the jury how Child B stopped breathing around 12.30am on a night in June 2015. The baby, which survived, broke out in similar 'whitey purple blotchy' patches to Child A. 'I just thought no, not again', the nurse told the jury
11:22am: Notes from that night show how an emergency call went out to doctors. Child B was placed on an infant resuscitator and medicines administered. Within about 10/15mins Child B began to 'improve almost as quickly as she had deteriorated'
11:29am: Lucy Letby's defence barrister Ben Myers KC is now questioning the witness. He asks her if there were times when the Countess of Chester, during the period June 2015-June 2016, was 'just too short staffed' 'Yes', the nurse replies.
11:44am: Mr Myers is now asking the nurse about the circumstances of Child A's death. He asks whether she had been made aware, when starting her shift, that Child A had been without fluids and medicines for several hours due to various tubes being out of position. 'Possibly', she said
12:18pm: Circling back to the nurse's description of 'white and purple' patches, Mr Myers points the jury to past statements made by the witness - to police in 2018 - which make no mention of such patches. Asked to explain why they're mentioned now, but not then the nurse cannot explain. Mr Myers puts it to the witness that these descriptions of patches have come from subsequent discussions with other staff, rather than what was actually seen on Child A
2:06pm: We're back after a break. Jury is now hearing evidence from paediatric registrar Dr Rachel Lambie, who was on duty the night Child A died. Dr Lambie is talking the court through the emergency 'crash' call she got after Child A fell ill
2:12pm: Dr Lambie recalls arriving in the neonatal intensive care unit as medics were attempting to resuscitate Child A. After 30-40mintutes the decision was taken to stop.
2:16pm: Dr Lambie was also on shift the evening Child B fell ill, she recalls 'patches of purple and red flitting around her body...they lasted 10 seconds, disappeared and moved…as we treated her, they subsided and went away'
3:30pm: Paediatric consultant Dr Ravi Jayaram is now giving evidence. He is taking the jury through his recollection of the evening Child A died...he says the baby's deterioration 'didn't fit to me with any disease process that I have seen, learned or read about'
4:41pm: Dr Jayaram told the court that when he raised initial concerns about Ms Letby he was told 'not to make a fuss' by senior managers, he said he 'wished' he had been 'more courageous' in reporting his concerns. The case has been adjourned until tomorrow
Chester Standard article 24-10-2022
Giving evidence at Manchester Crown Court on Monday, October 24, a nursing colleague of Letby recalled she was preparing medicines when the monitor alarm sounded at Child B's incubator.
The nurse – who cannot be identified for legal reasons – said Letby was the first to go to the cot and she called her for help.
Asked about Child B's appearance, she said: "She looked very ill. She looked very like her brother did the night before. Pale, white, with this purple blotchy discolouration. It was all over her body.
"I just remember thinking 'not again' – to see his sister with the same appearance."
A breathing tube was inserted and Child B "started to stabilise quite quickly", said the witness, giving evidence screened from the public gallery and the defendant.
The nurse added: "(Child A's) deterioration was very sudden and to an unusual degree. Babies can be very poorly quickly but there is usually some indication that is happening. We had no undue concerns.
"To go from that is very unusual and then (Child B) had been good throughout the evening for me… then she became ill very quickly. She deteriorated very quickly and then this discolouration.
"You never want any baby to die. You want to help them go home to their families. That's always been my goal."
Child B recovered and was eventually discharged a month later, the court has heard.
The witness could not explain why, when interviewed by police in 2018, she had not mentioned an unusual discolouration in Child A's appearance, but when later questioned about Child B she said her discoloured skin was similar to her brother.
She told Ben Myers KC, defending, that people on the unit were talking at the time about rashes but she was not influenced by anything somebody said.
The nurse told the jury she could not remember who administered intravenous fluids to Child A shortly before his collapse but accepted she told police that another nursing colleague had "pressed start" in the process and Letby assisted with checks.
She said she acted as "mentor" to Letby, who first came to the unit as a trainee around 2010/11 while studying at the University of Chester.
They became "good friends", she said, as Letby went on to join the unit after she qualified.
Mr Myers said: "We know the allegations but your experience when working with her was she was highly professional?
"Yes," replied the witness.
Mr Myers said: "And dedicated to the work she was doing?"
"Yes," agreed the witness.
Tuesday 25th October 2022
Children A & B (twins)
Dr B - Dr Dewi Evans - Dr Sandie BohinChester Standard Live Reporting
10:34am: The trial is now resuming, with someone who was a consultant paediatrician at the time of June 2015, giving evidence in court in relation to Child A and Child B.
10:37am: She said she "cannot recall" the events for Child B's collapse at 12.30am on June 10, as it was seven years ago, and her recollection would be based on the statement she had given to police.
10:40am: The court is shown clinical notes made by her, written retrospectively at 2.40am on June 10, 2015. She was called at home at 12.36am, and arrived at the neonatal unit at 12.50am. She recorded Child B "went apnoeic [stopped breathing]", followed by "suddenly purple blotching of body all over, with slowing of heart rate."
10:41am: The consultant says the 'purple blotching' would have been the registrar's account of events, relayed to her.
10:44am: The registrar also relayed Child B was bagged and tubed, and the heart rate went up, with adrenaline "not required". The consultant noted, for her observation: "Upon my arrival purple blotching right mid-abdomen and right hand." The baby was "pink and active". The prosecution asks: "Do you have any independent recollection of that now?" The consultant replies: "No."
10:51am: The consultant relays the various medical observations that were recorded at the time, including blood gases, protein levels, and heart rate.
10:57am: The consultant tells the court discussions had been ongoing since the evening of June 9, in light of Child B's twin brother dying, on whether Child A and/or Child B had been affected by the mum's blood condition. Consultants at Great Ormond Street Hospital had said they "did not feel" the mother's condition would affect the baby "in any way", while consultants at Alder Hey Hospital suggested further blood tests being carried. Following Child B's collapse, the blood observations taken were 'good', the court heard, and meant the requested extra tests were "held off".
10:58am: Child B was restarted on antibiotics "as a precaution". There was still concern her circulation had to return to normal, so the consultant noted more fluid was administered to help with that.
11:04am: The consultant's notes add: "Spoke to parents. "Purple discolouration almost resolved. "?? cause." The consultant says, from looking at her notes, she was "quite puzzled" by that as there were two question marks. The notes add: "Stabilised at present. "[Continued antibiotics]. "[Nil by mouth]. "Repeat gas and wean as tolerated."
11:05am: The notes conclude for further tests to be repeated at 7.30am, at the end of the night shift.
11:06am: Ben Myers KC, for Letby's defence, asks about "one area" on the clinical notes talked about.
11:14am: Mr Myers asks about the purple discolouration, and that by the time the consultant had arrived, she had noted what she had seen at 12.50am, and had 'almost resolved' by the time of the note at 2.40am. She tells the court: "I think this was something I was puzzled about, and wondering what it would be." She says other causes were ruled out as such a rash had "come out of nowhere" and had "almost completely gone" a couple of hours later. She added she was "a little bit confused" and was "trying to put in place all the safe things" she could do to treat Child B.
11:25am: Independent medical expert Dr Dewi Evans has returned to give evidence in respect of Child A. He confirms he has written four separate statements in respect of Child A, the latter two being clarification on technicalities. The first report was written in November 2017, the second in May 2018.
11:31am: Dr Evans said he became involved in the case in July 2017 by the National Crime Agency. He visited Cheshire Police where they had concerns about a number of deaths in the Countess of Chester Hospital which were "unusual" and "far more deaths than they would expect".
11:33am: The deaths had "followed collapses in babies" which were "otherwise quite stable" and involved collapses where resuscitation attempts were not successful. He said: "I thought I could help, advise review case notes and form an opinion that led to the collapses of [Child A and Child B]."
11:35am: He said "despite the prompt resuscitation in [A's] case", Child A had died despite doing "very well". He said his job was to look at the "clinical evidence". He added that Child A was the first case he looked at, and subsequent reviews of other children had reinforced his opinions for the conclusions of Child A and B.
11:37am: He said "a pattern became apparent in the cases", which he described as "quite disturbing and quite unusual."
11:39am: For Child A, Dr Evans confirms he had received clinical records for the baby boy to review, and had received statements from Countess of Chester Hospital medical staff for the case.
11:47am: Dr Evans explains to the court certain medical procedures such as cannulas, UVC and long lines.
11:53am: Dr Evans said there is a connection between the insertion of a long line and 'cardiac tamponade', where fluid obstructs the heart and is a "deadly serious condition". He added that, "sadly", he was aware of a case which happened in Swansea where a baby had died as a result of that. He said such cases are where a long line has been in place "for several days". Diagnosing such a condition post-mortem would also be "relatively straightforward" as fluid would be detected outside the heart. For Child A, he had not come to the conclusion that cardiac tamponade was the likely cause of death.
11:54am: Dr Evans says, from looking at Dr Harkness's clinical notes at the time, the efforts to save Child A were "very good standard resuscitation procedures." He added: "[It is] what you would expect in any neonatal unit in 2015."
12:01pm: Dr Evans said, just before Child A's collapse, he was "in a stable condition". In his report he had described his condition as "perfectly satisfactory." He added: "He was as well as could be expected. All the markers of well-being were very satisfactory. He was in air, not needing additional oxygen, heart rate in normal limits, oxygen saturation normal - it had been in the 90s...respiratory rate slightly above normal rate but that was the only marker outside normal rate."
12:06pm: He said Child A "had survived the most dangerous journey of his life" and, although he needed care for feeding himself, he "was doing really, really well" and "everyone one the unit would have been really pleased with how he was."
12:17pm: Dr Evans said he had not been presented with evidence of the discolouration, as the court has heard through this trial, for Child A. He said it was not noted in the evidence he had received. He adds: "I think the rash in [Child A's] collapse fits together and fits a significant diagnosis...of air embolus [injection of air into the circulation]."
12:18pm: "Somehow air had got into the circulation...I found this opinion without knowing about the rash and without anybody suggesting expressing concern of air embolus."
12:21pm: He rules out other conditions such as sepsis, a lack of fluids or hypoxia as causes, or contributing factors to the collapse. He said he had "only one" conclusion, that Child A had received an air embolus, "through an IV line". He said with the systems in place, and the medical equipment, and medical staff being "obsessive" about making sure patients are not injected with air, "there was no way this could have been done by accident".
12:24pm: Dr Evans will be cross-examined by the defence after giving evidence for Child B. Before that, independent medical expert Dr Sandie Bohin has now been called in to give evidence for Child A. She is detailing to the court her medical and professional background.
12:27pm: Dr Bohin says she was asked to peer review Dr Evans's reports and was to find whether she agreed with them, disagreed with them, or had additional findings to present. She has also considered other findings from other independent experts in the case.
12:28pm: The prosecution ask Dr Bohin to clarify whether she had also seen a post-mortem report for Child A, and the reports of Countess medical staff. She confirms that was the case.
12:31pm: Dr Bohin explains Child A was, for a baby born 10 weeks premature, a "stable baby", on breathing support via CPAP but not requiring oxygen ventilation, and was doing "so well" that medical staff decided to start giving him some feeds. "If he was unstable in any way they would have done so," she tells the court.
12:33pm: The UVC placement and long line placement did not have any contribution to Child A's death, Dr Bohin tells the court.
12:39pm: Was the stopping of breathing for Child A caused by his prematurity, the prosecution asks. Dr Bohin said it could be ruled out as there were no previous episodes, and caffeine had already been administered to counteract it as a precaution.
12:45pm: The discolouration seen, while seen in collapses in other infants, "did not explain" the pink blotching that came and went in Child A, Dr Bohin tells the court. She says the "only plausible explanation" for Child A's collapse is an air embolus.
12:48pm: Dr Bohin said doctors and nurses are "absolutely meticulous" in making sure even "the tiniest air bubble" is not injected by accident into a patient's circulation. She adds that even if air was accidentally administered, there is an electronic pump system which would detect the air and stop the administration. Dr Bohin explains to the court that could be bypassed further down the line by administering the air embolus via a connector normally used for administering drugs.
1:02pm: Dr Bohin is asked how much of an air embolus would be considered fatal to a child of Child A's size? She says that 3-5ml of air per kilogram of body weight "could be fatal". She explains Child A weighed 1.6kg [about 3.5lb]. "A teaspoon of air?" Nicholas Johnson KC, prosecuting, asks. "Well, that is 5ml of air, so yes," replies Dr Bohin.
Mr Johnson: "What, in your opinion, killed [Child A]?"
Dr Bohin: "[Child A] was killed by an air embolus."1:08pm: Dr Evans is recalled to give evidence for Child B's non-fatal collapse. He said the collapse was "not really" likely as "all the markers were satisfactory" and the medical staff had felt comfortable enough to allow the baby girl to be out of the incubator for a short time so she could be handled by the mum. He said that was "not something you would do" if the child was not stable.
1:10pm: He said the two conclusions he had for Child B's collapse were "smothering" or an "air embolus". He said the discolouration was a "striking feature" which had been seen in Child A arrived and went "very quick". He said if the rash was associated with other conditions, it "tends to stay".
1:17pm: Dr Evans tells the court the collapse was "very similar" to that of Child A, but what happened was "less severe". He said "either the volume of air [injected] was less, or the volume of air in the circulation got there more slowly, or a combination of the two." Asked by Mr Johnson if there were any other possibilities to the cause of the collapse, Dr Evans replies: "I could not think of anything else. "The doctors did a really good job in saving her. "There was no evidence of sepsis, problems with the lungs, nothing unusual about the chest x-rays, lungs were full of air...nothing else to explain this collapse which again was sudden and unexpected." He added: "We have heard numerous doctors saying they have never seen this before. I feel I can say the same. It's very unusual."
1:54pm: The court has adjourned for the lunch break, with the trial resuming at 2.10pm. Dr Evans will be cross-examined by the defence this afternoon in relation to the collapses of Child A and Child B.
2:16pm: The trial has resumed. Ben Myers KC, defending, says Dr Evans has prepared a "large number of reports" over the years, and air emboluses feature in "a number of them" - "literally dozens". Dr Evans agrees. Dr Evans is asked to explain the features of an air embolus. He adds: "An air embolus will lead to a sudden and unexpected collapse. A patient, otherwise stable, collapses. And by collapse, I mean change of colour, stops breathing...reduced heart rate, and death. This occurs all of a sudden. "There are additional features - you don't get all the features in all the cases. The two main associated features are unusual skin discolouration and the presence of air in 'great vessels' - various parts of the body. Those are the compounding features which lead to a diagnosis of air embolus. "This occurs when there is no other explanation...which fits the collapse, and when resuscitation is unsuccessful. "Resuscitating patients [for doctors] is part of our bread and butter, so resuscitating is well known. When that is unsuccessful, it adds to the confirmation [of an air embolus diagnosis]."
2:20pm: Dr Evans relays one case of a baby who had died in Swansea from an air embolus, from what "should have been a regular surgical procedure", when recalling it was "absolutely awful" and led to a criminal trial. He said he had not been involved in the report so was unaware of any discolouration in that baby. He says he has never come across such skin discolouration in a collapse in 'hands-on experience'. "That is something I am relieved and pleased about, actually."
2:21pm: Mr Myers said the diagnosis is 'one of exclusion' - ruling out alternatives until there is one explanation left. Dr Evans said there is more to the case than that. He said his original conclusion was without knowing about the skin discolouration in Child A. He adds that if you discover additional information, that "simply firms up your diagnosis".
2:26pm: Dr Evans states that air embolus cases are difficult as there are "isolated" case reports, and the systems are put in place in modern times so the conditions are not repeated - "that is not a criticism, that is a compliment", hence there is "very little new research". He adds that doctors may be reluctant to "spread news" of mistakes in cases where there may have been an air embolus.
2:40pm: Dr Evans said he was tasked with investigating a "clinical condition", not a "crime", when he became aware of the Countess of Chester Hospital case, when tasked by the National Crime Agency. He said the scenarios added up to a "constellation of worries" on what went on between June 2015 and June 2016. He adds that in past cases, he has been brought in by police and the conclusion was accidental, so the case was closed with no further police involvement.
He is asked about his 'state of mind' in his approach to the cases. "My state of mind was very clear - let's find a diagnosis. Nothing to do with crime. Let's identify any specific collapse, and see if I can explain it. "There were occasions where I couldn't explain it, and occasions where I found something deeply suspicious. "There were incidents I found disturbing." He was asked to investigate 33 cases in total, with two insulin cases later. He said there were two babies were born in unsurvivable conditions, with obvious medical diagnoses. He said: "The name Lucy Letby meant nothing to me. I didn't know the staff. "I was the easiest physician and the most difficult. I was a blank sheet of paper. I had no idea and relied entirely on the evidence I could see from the clinical notes and applying my clinical experience and forming an opinion to the cause."2:42pm: He said he asked to have one case file to have "an idea" of what he was dealing with.
Mr Myers: "Was the phrase 'air embolus' used at all?"
Dr Evans: "No. The first person to use air embolus, as far as I was concerned, was me. "I need to give the NCA a compliment, they never gave me a steer. They are good, professional people."2:48pm: Mr Myers turns to the case of Child A. He asks that pre-term babies such as Child A are 'prone to complications'?
Dr Evans: "That is why we have neonatal units." He adds that the care he received meant he had overcome the most difficult parts of his life and was "stable" prior to his deterioration.2:50pm: Mr Myers asks if Child A was "perfectly satisfactory" prior to the collapse, as according to Dr Evans's notes. Dr Evans says he does not want to engage in semantics, but adds that, for a pre-term baby in the position he was in, Child A was "satisfactory" and "really good".
2:53pm: A clinical note is presented to the court, with a number of 'problems' listed.
Dr Evans: "I would call them issues, not problems. "This is what any competent junior doctor would list as the issues present. "We have got to deal with the fact he is pre-term, he has breathing support, we need to establish feeds, there are concerns over suspected sepsis. "Any doctor would write this things down."2:55pm: An x-ray review is presented, with the note 'RDS [respiratory distress syndrome] type picture'. Dr Evans is asked about that comment. He says: "I have seen the report, it's not too bad actually. This is why we put babies on CPAP."
2:59pm: A blood gas record showing a 'high' number for lactate (2.6 - outside the range up to 2) is shown. Dr Evans explains he wouldn't be "particularly" concerned at such a reading, in the "whole picture", as he says one or two readings would be outside the normal range. He describes the reading as "marginal", with all the other readings "normal", and Child A was "handling well". He said he would not interpret an oxygen reading from a capillary sample from a 'heel prick'. He says if he saw such readings, knowing if the baby was "in air", he would not be "rushing to stick needles in him" unless there was a change in condition in the baby.
3:07pm: A NICU observation chart is presented for Child A, including the respiratory rate. Mr Myers says the readings are "not stable." Dr Evans disagrees, saying the readings are "within range". The 'increase' in the respiratory rate readings were down to the insertion of the long line and UVC, handling of the baby and a heel price procedure which caused the baby discomfort. Dr Evans said he would expect the heart rate to go up with an increased respiratory rate, which would be a concern. But as the heart rate had remained stable, he said he would "not be concerned" and Child A "was not even requiring oxygen", with saturation levels at about 97-99 per cent, "was about as good as it gets".
3:10pm: Dr Evans says "it happens" that children on neonatal units can go without fluids for four hours. He said it was not ideal, and "unfortunate", but it did not make a "clinical difference" in this case. He said a child which had missed out on that level of fluids for that time would not have subsequently collapsed and died.
3:12pm: Dr Evans reiterates that the context of other readings had "all the markers" of a stable baby. "This was a baby who was stable prior to him collapsing," he said, referring to the words other doctors had made in evidence.
3:18pm: Dr Evans dismisses alternatives put forward by the defence, including 'infection', saying such evidence would appear on a post-mortem examination. He dismisses a suggestion of a 'rapidly spreading infection' in the baby as "ridiculous", as he said such evidence would again be found post-mortem by a pathologist.
3:22pm: Dr Evans said his conclusion of an air embolus was based on a baby "suddenly crashing" and, "more significantly", followed by "resuscitation which was unsuccessful". He adds the subsequent x-ray and skin discolouration reports had firmed his opinion.
3:24pm: "A collapse of this speed in a baby unit, with full medical care, is very unusual these days."
3:27pm: He adds that Child A, given all the factors, is normal, and in "the safest place on the planet" for their needs. "Neonatal unit care is as good as it gets. "It has come on leaps and bounds [over the years]."
3:29pm: Mr Myers says skin discolouration can be a sign of illness, or due to underlying circulation problems, or infection, or blood pressure issues (secondary to something else). Dr Evans agrees. Mr Myers asks if it would be "flawed" to diagnose skin discolouration as an air embolus.
Dr Evans: "Discolouration is a general term, noting there is something present on the skin, as noted by a doctor or nurse. You can't say it is due to a specific condition."3:34pm: Mr Myers refers to a 1989 study which showed, following 50 cases involving an air embolism, only '11 per cent' involved skin discolouration. Dr Evans said he had come to his initial conclusion of an air embolus for Child A before becoming aware of the skin discolouration.
3:41pm: The judge rephrases a question of Mr Myers to ask that "failure of resuscitation", of itself and in isolation, is not a consequence of an air embolus. Dr Evans agrees. He says in combination with all factors already presented - including air in the great vessels, sudden collapse and skin discolouration, the conclusion is that of an air embolus. He says an air embolus is not "common", but is rare and unusual.
3:48pm: Dr Evans said in 14 of the 17 cases he had completed his preliminary reports by November 2017, and was unaware of any medical staff member being a suspect. He became aware of the name 'Lucy Letby' for the first time upon her arrest in July 2018 when he read her name in the press. He said he was the first to come up with a diagnosis of an air embolus, and this had been agreed by a peer review by Dr Sandie Bohin, plus by a medical expert who began to peer review his reports but sadly, before completing the review, became seriously unwell and died.
3:54pm: Mr Myers asks about the non-fatal collapse of Child B, who needed breathing support at birth, as a clinical note shown to the court shows. An x-ray review has the note 'RDS type picture', as also shown for Child A. Dr Evans agrees with Mr Myers that a child such as Child B is 'prone to desaturations'.
4:03pm: Mr Myers presents a clinical note to the court from June 19, 12 days after Child B was born, noting there were desaturations recorded - if not on the same scale as those recorded during the non-fatal the collapse - and on June 20 when "the apnoea alarm went off" on three occasions, with oxygen saturation "down to 70-80% each occasion". A paediatric assessment dated July 14 for Child B is presented to the court, in which 'breathing problems' are noted along with 'mottling'.
Mr Myers: "There are some respiratory issues associated with her health?"
Dr Evans: "Nothing compared to what we would call the 'index event' (the collapse). She needed resuscitating."4:07pm: Mr Myers asks about the differential diagnosis for Child B, concluding there was either an air embolus, suffocation, or someone had removed the prongs on purpose. Dr Evans said, in his opinion, he was "on the ball from the start" in considering an air embolus. He said his opinion was reinforced by colour changes "every 10 seconds" as mentioned by a Countess staff member in court.
4:09pm: The theory of removing the CPAP prongs on purpose is discussed. He says it's possible for a baby to move them by accident. He is asked if smothering is a possibility, to which Dr Evans says he has since discounted.
4:16pm: Mr Myers said it is a 'key aspect' that the inability to successfully resuscitate Child A had led to an air embolus. He adds that child B recovered, and that is "inconsistent" and "contradicts the air embolus theory".
Dr Evans: "No it does not. We cannot do studies where we inject air into babies and see what happens." He adds that the volume and speed at which air is injected, along with the skill of the resuscitation attempts, can make a difference as to whether the baby survives or dies.4:19pm: Dr Evans says, under questioning by Mr Myers, he would be happy to hear of an alternative explanation from a medical perspective for Child B, but he is happy with the conclusion he has made for Child B, that she had had an air embolus.
4:24pm: The prosecution refers to the clinical note from June 20, following the desaturations recorded. The note adds Child B 'self-corrected'.
Dr Evans: "It's a bit frightening, but she self-corrected. These things happen in babies." He reiterates that those events noted on June 20 are a long way from what happened when Child B suffered a non-fatal collapse.5:02pm: The trial has been adjourned for today. Our live coverage will continue tomorrow (Wednesday, October 26), with updates throughout the day.
Wednesday 26th October 2022
Children A & B (twins)
Dr Sandie Bohin - Summary of police interviews - Parents' statements - Police analyst: Recorded events & messagesChester Standard Live Reporting
9:27am: One of the medical experts giving evidence on Tuesday said a "teaspoon" amount of air - about 5ml - would have been enough to kill one of the babies in the neonatal unit. The court heard that amount of air was, in the medical experts' opinion, injected into the blood circulation and resulted in the fatal collapse of Child A and the non-fatal collapse of Child B.
10:12am: The trial is expected to resume at 10.30am.
10:32am: Dr Sandie Bohin is now giving evidence in respect of Child B.
10:34am: She confirms she has examined medical records, case notes and photographs for Child B, and peer-reviewed Dr Dewi Evans's report for her non-fatal collapse in June 2015. Medical experts giving evidence in cases of Child A and B
10:36am: Child B collapsed at 12.33am on June 10, 2015, at the neonatal unit. She later recovered and, four weeks later, was discharged from the Countess of Chester Hospital.
10:38am: Dr Bohin says Child B was "compromised" at birth, and required respiratory support, which was "not that unusual" for someone of her prematurity. "She stabilised very quickly," Dr Bohin added, and was "in air" with "normal" blood gases, and "stable enough" to have skin to skin contact with her mother and for feeds to be started.
10:41am: Dr Bohin said the circumstances of Child B's collapse were not normal, but "very concerning". She said: "Despite being on CPAP, she was otherwise normal." If such babies deteriorate, there is normally "prior warning", but there was "nothing to suggest she was going to collapse in this way".
10:43am: The prosecution refer to an event where the nasal prongs were dislodged, prior to the collapse. Dr Bohin said the prongs can be "misplaced", and the babies are "probably quite uncomfortable", and if left for a prolonged period of time, there would be a desaturation, with prior warning. She added: "It was noted, the prongs were replaced, and everything went back to normal". Dr Bohin replies to the question if the misplaced prongs had anything to do with the subsequent collapse: "No, none at all".
10:44am: Dr Bohin said other factors, such as infection or cardiac arrhythmia, could be discounted, and the only conclusion left was "air embolus".
10:45am: She refers to the skin colour changes seen on Child B, and how "florid and different it was from anything they had seen before". "It just didn't fit with any other potential different causes". Dr Bohin said she looked at Child B's case "on its own merit", as with any other, when coming to a conclusion.
10:52am: Ben Myers KC, for Letby's defence, is now asking questions to Dr Bohin. Mr Myers asks if it is important that medical experts have current day-to-day experience in a medical environment.
Dr Bohin: "Not necessarily no - what you can't do is dispel the experience they have had over many years." She adds it is not "crucial" they have on-the-job current day-to-day experience. After further questions, she said such experience would be "advantageous".10:56am: Mr Myers refers to GMC guidance in giving evidence as an expert witness, and asks if someone who retired from clinical practice is still in the same position to give evidence for events which happened in 2015. Dr Bohin says someone does not lose their knowledge after retiring from on-the-job clinical practice, but if they keep up to date with clinical practice, they are not at a disadvantage.
10:58am: Dr Bohin said the first time she had contact with other medical expert Dr Evans was earlier this year, to discuss one of the cases in the trial, via a telephone conversation, as there had been a difference of opinion.
11:01am: Dr Bohin said she had previously seen one example of an air embolus, and it was in a neonatal case, but was "very long ago". She said she could not recall the specifics of the case, but the air bubbles seen in the imagery were "very striking". She said she had formed her views after excluding other possibilities.
11:04am: Dr Bohin said she is unaware of any genetic condition which would cause a baby to collapse and die within 24 hours. She said genetic screening would only be done if staff had a suspicion the baby had a genetic condition.
11:07am: Mr Myers says Dr Bohin said Child A was "extremely stable" prior to collapse. She said there was "nothing which was cause for concern".
11:09am: The blood gas record for Child A is shown, and Dr Bohin says the lactate number of 2.6-2.7 is 'slightly elevated' (a normal reading at the Countess was '2'), but has to be taken in context with other parameters which were normal.
11:11am: The NICU Observation Chart is shown to the court for Child A. Mr Myers says the respiration rate is "not stable". Dr Bohin says it's above the normal rate, but "is stable". She said the range is 60-80 breaths, which is outside the normal range, but with CPAP breathing support, and 'in air'. She said during the afternoon there would have been interventions which would have caused the respiration rate to rise.
11:13am: She said the respiratory rate, in conjunction with other factors, would have been something staff "would have been aware of".
Mr Myers: "Would you say this was an alert?"
Dr Bohin: "Yes, but there was nothing else that needed to be done. He wasn't having a lot of desaturations. "The next step would have been to ventilate him...and he didn't require that."11:15am: Dr Bohin: "Handling in a baby with respiration support can make the respiration go up." Mr Myers asks if the heart rate would also go up.
Dr Bohin: "It can do...but not necessarily."11:22am: Mr Myers refers to the insertion of the UVC and long lines. Dr Bohin said the long line was not in the "best" position, but was in a "fine" position that was "safe" and would not cause problems with the heart.
11:27am: Dr Bohin said a long line can move if left in "for two weeks or more". She said the long line would not have moved in the space of a day, and the recommendation is not to x-ray every day.
11:28am: Mr Myers refers to Child A's lack of fluids for four hours. Dr Bohin says it was "not ok", and "would not be optimal care", but he had "no IV access" and the doctors had to prioritise other matters on duty, and adds "it wouldn't cause a sudden collapse like with [Child A]."
"The only deterioration he could possibly have would be to drop his blood sugar."11:31am:
Mr Myers: "Would you agree the whole situation is sub-optimal at that moment?"
Dr Bohin: "No." Mr Myers asks if the lack of fluids means the whole situation is sub-optimal for Child A.
Dr Bohin: "No."11:32am: Mr Myers refers to the skin discolouration. Dr Bohin explains there is a difference between a rash, such as chickenpox, and changes to colour in the skin, where it can go blue, or pale, or mottled.
11:38am: Mr Myers refers to a paper published by the International Journal of Critical Illness and Injury Services on air embolisms, which reports air can enter via the UVC during negative pressure in the vessel systems. Dr Bohin says she knows this sort of thing can happen, but in adults, and is not aware of any neonatal cases.
11:42am: Mr Myers now refers to the case of Child B. He says the UVC procedure had to be repeated with her. He asks if that was "sub-optimal". Dr Bohin replies: "No. Ideally you would want it in first time."
11:44am: A clinical note refers to Child B not getting fluids "for a couple of hours". He asks if that was "sub-optimal". Dr Bohin agrees.
11:49am: Mr Myers refers to a clinical note showing it took five attempts to insert a long line for Child B, and asks if that was sub-optimal.
Dr Bohin: "Five attempts is what it took - it's incredibly difficult to site these - they are a millimetre wide. At times it just won't thread for you. "If it won't thread for you...you are very aware you are handling this baby and the easier thing is to take it out and reinsert it," she adds, rather than "fiddling about with it" in the baby's body.11:50am:
Mr Myers: "[Five attempts to insert the long line] This is standard, is it, in practice?"
Dr Bohin: "Yes, it is."11:53am: Referring to treatment, Dr Bohin said "nothing can ever be done immediately" in the hospital, but the size of the neonatal unit care was standard for a unit of that size.
12:02pm: Dr Bohin agrees there were breathing problems for Child B at birth.
Mr Myers: "Do you agree that Child B could deteriorate without deliberate harm?"
Dr Bohin: "It is a possibility."
Mr Myers: "Air embolus is usually fatal, isn't it?" Dr Bohin agrees there is a risk. Dr Bohin says a small quantity of air could create an air embolus. She said it is the volume and speed which are the factors. Mr Myers says it is "almost always" fatal. Dr Bohin replies that can be the case with adults [to which there have been medical reports published].12:08pm: A clinical note refers to the "purple blotching...pink and active" for Child B, and is shown to the court. Mr Myers asks if 'pink and active' refers to the baby.
Dr Bohin: "Yes."12:13pm: We are having a short adjournment in court. The trial will resume in a few minutes.
12:23pm: The prosecution, led by Nicholas Johnson KC, is clarifying a few matters from Dr Bohin's evidence. Dr Bohin said she needs to be "completely independent" and base her conclusion on the evidence presented to her.
12:30pm: The blood gas record is shown to the court. One of the parameters from a blood capillary reading, a 'PO2' recording, is typically "disregarded" as it is not reliable, Dr Bohin says.
12:32pm: Dr Bohin presents a UVC to the court, and explains how it is administered and left so there is no air left in the tube. She explains a long line looks similar, but has a wire inside it.
12:39pm: Dr Bohin clarifies she has never heard of a case, in clinical experience or in educational courses, or in published literature, of a neonatal having an air embolus as a result of negative air pressure, as described in the medical paper concerning air embolisms in adults.
12:41pm: Dr Bohin is asked if there is any link between Child B not getting fluids and the collapse which happened 28-30 hours later.
Dr Bohin: "No."12:45pm: A note, dated July 14, relays a progress report for Child B. Mr Johnson asks if there is any evidence of breathing problems in that note. Dr Bohin says there isn't.
12:47pm: Dr Bohin says the colour change 'on its own' is not diagnostic of an air embolus, but needs to be taken into context with the sudden and unexpected collapse.
12:52pm: Intelligence analyst Claire Hocknell is now being brought back into court to point out a few corrections made in the bundle of evidence for Child A and Child B. The corrections are largely typos and names for text messages being the wrong way around. All such evidence was corrected during the course over the past few days and has been automatically updated on the jurors' electronic bundles.
2:02pm: We have had an adjournment for lunch. Court is resuming in the next few minutes.
2:11pm: The jury is now coming back in. Nicholas Johnson KC, for the prosecution, explains to the jurors he will now read a summary of the police interview Lucy Letby had in respect of Child A and Child B. The wording of the summary has been agreed between the prosecution and defence.
2:14pm: For the case of Child A - the first interview took place in July 2018. Letby was allowed to look through the case notes, and was asked if she remembered the specific shift. She replied: "Yes." Letby gave details of the handover and the long line administration. She said she checked the fluids and a nurse colleague "had the bag out". She said they noticed Child A was "pale and mottled", and a crash call was put out. She said full resuscitation attempts followed. She said Child A had been "a little bit jittery in appearance" and believed that was due to low blood sugar levels. She said a colleague was there with the fluids at the handover.
2:15pm: She was asked why the fluids were a priority, and Letby explains Child A had gone 'a few hours' with a lack of fluids. She said that "wasn't ideal". She said Child A went pale after a colleague had connected the fluids. She said Child A had "gone pale" 'about five minutes' after the fluids were administered.
2:17pm: She said Child A had a rash-like appearance, which Letby put as being the result of an infection, or being cold. "He was more pale than the areas of the mottling." She was asked if anyone had seen the mottling.
Letby replies: "Yes." She said they were advised to stop administration of the fluids. Child A was then not breathing, and Dr Harkness was called over.2:20pm: Letby said she could not recall Child A's resuscitation, but recalled Dr Jayaram had entered the room. She said the death of Child A "had been difficult" for her, and said there was a support network among the nursing team. She said she could not recall who attached the fluids line, but believed it was her nursing colleague Melanie Taylor who had connected the fluids. She said photos were taken of Child A in accordance with the parents' wishes on their phone, along with a lock of hair and hand/footprints.
2:23pm: She agreed she had been taught to prime lines so air could not get in them. She denied having done so via Child A's long line or UVC. She said she didn't know exactly what an air embolism was. She said her relationship with the child's parents was "strictly professional" and could not explain or remember why she had searched the mum's name on Facebook several times in the following weeks. She explained, for a later search, she may have been searching for their names for an update on Child B.
2:27pm: For Child B, Letby explained the discolouration was a different appearance to that of Child A. Child B's appearance was observed before resuscitation attempts began. She did not recall having had any concerns for Child B, or any alarm going off for her. She confirmed she would have handled Child B to an extent for medication and to attach lines. She said she did not recall how upset Child A and B's parents were at the time.
2:28pm: The court is now being told about the case of Child C - a murder allegation for a baby boy who died on June 14, 2015.
2:29pm: The first 'agreed evidence' statement comes from Child C's mother, dated January 2019.
2:30pm: The mum said she had gone for an anatomy scan at the Countess of Chester Hospital. She was informed, while everything was 'normal', the baby 'looked very small'. It was recommended a test was to be taken for any genetic conditions that may be present.
2:33pm: The results of the scan showed there were 'no genetic problems'. The baby was small, 'but it was not known why'. Further scans were held, along with blood flow checks. Child C's growth then 'began to falter' later on, and it became delivery would take place 'quite soon'. She was being monitored 'twice weekly'. In June, the mother had raised blood pressure in a test, and she was admitted to the Countess of Chester Hospital as a precaution. That night, it was found Child C's heart rate had dropped, and she was moved to the labour ward as concerns had grown. On this occasion, nothing happened, so she was moved back to the antenatal ward.
2:35pm: The following Monday, the dedicated consultant said it would be best to closely monitor the situation. On June 10, the mother had a scan, and found there was a risk of a still-born birth. The mum was taken to the labour ward and given various drugs to support the baby. The mum was then taken to theatre and a Caesarean section took place. "The birth was extremely stressful," the mother recalls.
2:37pm: Child C was intubated and put on a ventilator, but the mum was told the nursing staff "weren't particularly concerned" for his immediate condition. The mum was unable to see Child C for several hours afterwards. She said she was able to see Child C - "tiny", weighing "800 grammes", that night. Child C was given CPAP and had been taken off ventilator support. On June 11, the mum and dad had "small periods of time" where they could hold Child C. The nurse Joanne Williams there was "very supportive".
2:42pm: In the following days, Child C was taken off CPAP and was "calmer" on June 13. He had a gastric tube fitted. When fluid came out, it was a black colour and staff could not explain what that was. The family had "a cautious positivity" for Child C. His oxygen levels were being weaned down "as he was doing so well". She was woken up at 11.20pm by one of the nurses, having been contacted by one of the neonatal nurses to go there "immediately". She arrived to see CPR being performed on Child C. "He had stopped breathing without any warning. "This was sudden and unexpected." The mum told her husband to come to the neonatal unit. She recalls not being able to take everything in, and was asked by a nurse if she wanted to get in contact with a priest. The mum was shocked and asked if Child C was going to die. The nurse replied in the affirmative.
2:46pm: The mum said while waiting for a priest, her husband arrived. They had to wait for 50 minutes until the priest arrived. She was told Child C, after being baptised, had passed away. Although there was a pulse, there was no brain activity. The mum said: "It was awful." After Child C passed away, the mum handled him. She was asked by a nurse if they wanted a lock of his hair. On June 15, she was contacted by the coroner's office at Alder Hey, for the post-mortem. She was advised the conclusion was "natural causes".
2:49pm: The father's 'agreed evidence' statement is read out to the court. He said the mum's pregnancy was "highly stressful", and recalls she had elevated blood pressure, requiring a trip to hospital. He recalls being present for Child C's birth, where the child was placed into an incubator. He said medical staff were "really pleased" with him, and he followed Child C into the neonatal unit.
2:51pm: He said Child C "was still doing well" in the first few hours, and needed respiratory support, but was "capable of breathing independently". "At no point did the staff express concern of him not surviving."
2:59pm: He said Child C had continued to do well, and was at home when he was called by the mum to come to the hospital "right away". When he arrived, the mum was waiting for her and he was informed Child C had collapsed and stopped breathing. "She didn't think she could do any more", but they continued trying, until a priest arrived. Child C then began breathing by himself. The family were taken into a room, where there were two nurses there, one of whom the father has since been able to identify as Lucy Letby. The father and mother took turns holding Child C, "as we knew he wasn't going to make it".
He remembers one of the nurses administering morphine to Child C. At regular intervals, the nurses came in to check on their welfare. A hand and footprint were taken of Child C, along with toys that were cotside. The father said he and the mum looked after Child C in that room: "We just wanted to cuddle him and make sure he was pain free." One of the nurses came in and said something along the lines of 'you've said your goodbyes, now do you want me to put him in here [a basket]?' The mum said 'he's not dying yet', and the nurse backtracked. "We remember being really shocked by this."3:02pm: The jury is now being waked through the sequence of events for Child C, with the evidence, as was the case for Child A and B, being shown on an interactive display to the court. The electronically stored evidence is also available to view on the juror's iPads. The jury is informed that, as they are increasingly used to the system and the descriptions of types of medical records, this process will go quicker than that for Child A and B.
3:07pm: Text messages exchanged following the deaths of Child A and B show Lucy Letby asking if there were spare shifts going, adding: "Think I need to throw myself back in on Saturday." The response: "Hopefully it might settle down by then."
Letby: "I think from a confidence point of view I need to take an ITU [intensive treatment unit] baby soon." The response: "It does knock you a bit when things like that happen, but it's ok to have time out as well. Enjoy the sun"3:16pm: The court is shown the nursing night shift for June 13, with a different nurse identified as the designated nurse for Child C, and Letby being a nurse for two other babies.
3:29pm: A message sent to Letby on June 13, at 9.48pm, says: "You ok? x"
Letby replies: "I just keep thinking about Mon. Feel like I need to be in [neonatal unit room] 1 to overcome it, but [nursing colleague] said no x" The colleague responds: "I agree with her, don't think it will help. You need a break from full-on ITU, you need to let it go or it will eat you up..." Letby responds: "Not the vented baby necessarily, I just feel I need to be in 1, to get the image out of my head."3:35pm: Letby adds: "It probably sounds odd but it's how I feel x" The colleague responds: "Well it's up to you but I don't think it's going to help." After further messages are exchanged, the colleague suggests: "Why don't you go in 1 for a bit?" Letby responds: "Yeah, I have done a couple of meds in 1." Letby later adds: "Forget I said anything, I will be fine, it's part of the job. Just don't feel like there is much team spirit tonight x" The colleague replies: "I am not going to forget but think you're way too hard on yourself..." Letby referred to previous events she had seen in a women's hospital, and the support available following such events.
3:36pm: The text message conversation, on WhatsApp, concludes at about 11pm. Child C collapsed 20 minutes later.
4:48pm: The trial has now concluded for today. We will be back with further live coverage tomorrow (Thursday, October 27).
5:01pm: The trial has now concluded for today. We will be back with further live coverage tomorrow (Thursday, October 27).
Thursday 27th October 2022
Child C
Police analyst: Recorded events & messages - Dr Sally Ogden - Dr Gail Beech - Yvonne Griffiths (senior nursing practitioner & neonatal unit deputy manager)Chester Standard Live Reporting
9:25am: The prosecution began giving evidence for Child C on Wednesday. Child C was a premature baby boy who died at the Countess of Chester Hospital neonatal unit in June 2015. The prosecution say he was murdered by Lucy Letby. On Wednesday, statements from Child C's parents were read out to the court.
10:34am: The trial is now resuming.
10:37am: Intelligence analyst Kate Tyndall is continuing to give evidence, providing a walkthrough of the clinical notes and other documents, presented in electronic form, to the jury.
10:58am: Text messages and WhatsApp messages sent to and from Letby's phone the morning after Child C died are shown to the court. Letby messages a colleague: "Sorry I was just off [last night], was not a great start to shift but sadly it got worse." The colleague responds: "You weren't off, you just were not happy and there is nothing I could say that was going to make it any better."
11:04am:
Letby: "I was struggling to accept what happened to [Child A], now we have lost [Child C] overnight and it's all a bit much." The colleague replies: "It will be but it does happen to these babies unfortunately."
"It's a very sad part of our job." The colleague recalls a baby who had previously died in the neonatal unit, but had "overwhelming sepsis" so "nothing would have saved that baby".
Letby: "[C] is the little 800g baby...went off very suddenly. I know it happens but it's so sudden..." Messages are relayed detailing how nursing staff on the night were upset by what happened. Letby's colleague messages: "This is where we have to pull together and look after each other."
Letby: "Think we support each other brilliantly...just such a shock especially after Monday." Letby is advised to "switch off for a bit".11:05am: Letby messaged her mum that morning to say: "We lost a little one overnight. Very unexpected and sad xx"
11:10am: Letby added, in the message to her mum: "He only weighted 800g...new girl was looking after him, she is devastated." Letby's colleague, in a message to Letby, said: "Hoping you are going to ok, this is not like you. Sending the biggest hugs." Letby, in her reply, says: "It's heartbreaking but it's not about me." Letby's colleague, in her reply, says to use a 'northern phrase': "Chin up chuck we will get through it together."
Letby: "It's not about me or anybody else, it's those poor parents who have to walk away without their baby."11:12am: Letby messages another colleague asking when she is next work, before adding: "We lost little [Child C] overnight, everyone's devastated." The colleague responds: "Damn. Infection? Crap week. How is [Child B]?" Letby gives an update and says, for Child C, "it happened very quickly." The colleague responds: "Damn. As quick as [Child A]? Yeah, s*** week."
11:15am: Letby messaged the colleague: "Parents sat with [Child C] in the family room...persuaded them to have hand and footprints but they just wanted to go home." The colleague responds: "That is so sad, don't know what to say."
Letby: "There are no words, it's been awful." The colleague: "It's a really tough week, especially for you." The conversation ends at 10.12am. Letby searched for both the parents of Child C on Facebook later that day, at 3.32pm.11:18am: A conversation Letby has with a third colleague, later that day, is shown to the court.
Letby: "I don't really want to go in tonight." The colleague responds: "I don't particularly but we will get each other through it."
Letby: "We are a good team and we will get through. You did so so well." The colleague: "We all did - so lucky to work with such an amazing and supportive team."11:26am: The court is now hearing evidence from Dr Sally Ogden, who in 2015 was a paediatric registrar at the Countess of Chester Hospital. Child C was born at 3.31pm on June 10, 2015, with Dr Ogden confirming she was present at the birth and facilitated the baby boy's transfer to the neonatal unit. Child C was "smaller than expected for that gestation", with a C-section made necessary.
11:29am: The birth weight of 800g was within the range for Child C to be allowed to be treated at a Level 2 neonatal facility - the one at the Countess of Chester Hospital. An 'Apgar score', recording how well the new-born is doing immediately after birth, is noted, rising from 7, to 9 out of 10.
11:33am: A clinical note showed there were 'no RF [risk factors] for sepsis', and Child C was "born in good condition", "came out crying, good resp[iratory] effort...no resus[citation] needed...pink...well perfused." The heart rate was ">100", the saturation was "95% air". Dr Ogden said those latter two readings were what would have been expected.
11:36am: Upon arrival to the neonatal unit, Dr Ogden noted symptoms Child C was starting to struggle breathing, including grunting and subcostal recessions. The note added: "Decision to intubate", which Dr Ogden said would have been her decision. The respiratory signs "can change quite quickly after birth", Dr Ogden says, so such support for babies of Child C's pre-term "would not be unusual".
11:39am: Ventilator support was set up for Child C, with "standard settings...for the context" set up on the machine.
11:46am: A note of medical communication with the parents is shown to the court. Dr Ogden's colleague recorded observations taken by her, relaying to the parents that Child C was born in a good condition with good breathing. Another clinical note showed a 10% dextrose solution would be administered via a TPN bag, through a UVC. A note on a discussion between the hospital and the Liverpool Women's Hospital was made - due to Child C's weight. The discussion would have raised the possibility of Child C being transferred to Liverpool.
12:00pm: The trial is now resuming following a short break. Dr Ogden will continue to give evidence.
12:04pm: The clinical note, regarding a possible transfer for Child C, concludes: "Happy for patient to remain @ CoCH [Countess of Chester Hospital] at present. If clinical concern overnight for rediscussion with [Liverpool Women's Hospital]."
12:10pm: A clinical note, dated June 11, 2015 at 11am, is made by Dr Ogden, with a number of medical observations. They include details of the respiratory support and feeds. Dr Ogden says Child C was on CPAP support by this time, on 41% oxygen - a "moderate" amount for a pre-term baby, with other readings being normal. There was an increased breathing rate noted. A high lactate reading was noted, "which needed to be noted in context" with other readings. It was a "sign of multiple different conditions" and, Dr Ogden says, was a sign to look out for such conditions.
12:20pm: Child C's blood sugar levels were stable. Child C was screened for sepsis, and placed on antibiotics "as a precautionary measure". There were "no concerns" on the cardiovascular system. Child C was observed to be "active, pink, well perfused", with "chest clear, slight increase in work of breathing". Other observations were recorded as normal. The overall picture was Child C was "responding as to be expected". The prosecution say a 'generic plan' of next steps was put forward for Child C, to which Dr Ogden agrees.
12:28pm: Another note by Dr Ogden at June 13, 9.30am is made for Child C. The list of 'problems' is noted, including 'RDS' and 'suspected sepsis'. Dr Ogden says the oxygen levels had gone down on CPAP to 26%, as had the lactate reading. Child C's breathing was "stable and possibly improved". "Very dark bilious aspirates" are noted from the feeding section. This was "not normal" and "suggested a problem with his abdomen", or a sign of how Child C's bowels were responding to being pre-term. "That would have been a concern," Dr Ogden said.
12:40pm: Child C had a long line put in place by this time. Other observations made included that chest was clear with no increased work of breath. The abdomen was "soft, not distended", which Dr Ogden said was a "reassuring sign", amid a concern from Child C's aspirates that the gastro-intestinal disease NEC was a possibility.
12:43pm: The reviewing doctor suggested to "hold off feeds" for now and review in the afternoon if the aspirates did not get any worse.
12:45pm: Ben Myers KC, for Letby's defence, is now asking questions to Dr Ogden. He refers to the decision about which hospital Child C should have been placed in. Liverpool Women's Hospital offered Level 3 neonatal care, with the Countess of Chester Hospital offering Level 2 care at the time.
12:46pm: Dr Ogden said she "believed" the minimum weight for Level 2 care centres to treat babies was 800g - the birth weight of Child C.
Mr Myers: "He was right on the borderline of what could be accepted at the Countess?"
Dr Ogden: "Yes."12:49pm: Mr Myers refers to the conditions detected that led to the C-section. He asks if one of the conditions that could follow would be NEC. Dr Ogden agrees. Mr Myers said for such babies, there would be an increased risk of infant mortality. Dr Ogden agrees. She also agrees that Child C would be a "high risk" baby. She says that for the context, and taking the considerations for those conditions into account, Child C was in a good condition.
12:51pm: Mr Myers refers to the Apgar score for Child C at birth, with readings at one minute, five minutes and 10 minutes. Child C scored 7/10, 9/10 and 9/10 respectively. The scores are "subjective" and based on observations.
12:54pm: Mr Myers asks about the clinical note which refers to the discussion between the Countess and the Level 3 Liverpool Women's Hospital.
Mr Myers: "At this early point, your view was that Liverpool Women's Hospital needed some communication [in relation to whether Child C would need to be transferred]?"
Dr Ogden: "Yes, that's right." Mr Myers says if Child C had other problems, along with a 'borderline' weight, then that may affect the decision to transfer a baby to a tertiary centre.
Dr Ogden: "Potentially, it would depend on the circumstances." Dr Ogden said the decision to transfer would be a joint one made between the hospitals and made via consultants.12:56pm: Dr Ogden said if Liverpool Women's Hospital could not accommodate a baby, there would have been other tertiary centres available if necessary. Mr Myers says the Countess would have required sufficient numbers of staff to care for Child C. He asks if June 2015 "was a particularly busy time for [the neonatal unit in] Chester?"
Dr Ogden: "Yes."12:58pm: Mr Myers said with the number of babies, another factor would be the individual care required for each baby, which included a number of pre-term babies in June 2015.
2:03pm: The trial has adjourned for a lunch break, and is due to resume at about 2.10pm. Ben Myers KC will continue to ask Dr Sally Ogden questions on behalf of the defence.
2:15pm: Mr Myers now refers to the case of Child C. He asks about the risk of infection, which Dr Ogden was "not immediately a concern" at the time of his birth. Mr Myers says infection "is always a potential risk". He asks about the breathing issues Child C had at birth, and asks whether such issues could be a "sign of infection". Dr Ogden agrees.
2:20pm: The court is shown an x-ray review in which a staff member had noted "hazy left lung field". Dr Ogden said she hadn't seen the x-ray, but agrees the note in the review means there could be a sign of infection. The list of 'problems' in a clinical note is raised, including 'suspected sepsis'. Dr Ogden says there was a treatment plan in place for 'suspected sepsis'. The 'high lactate' noted is an indicator of a potential, non-specific issue with the baby, the court hears.
2:25pm: The clinical note from June 13 is raised. Mr Myers suggests there are 'increased issues' for Child C.
Dr Ogden: "It's hard to say." Mr Myers refers to the 'very dark...black aspirates', and Dr Ogden agrees they are "a cause for concern".2:27pm: Mr Myers asks if the aspirates are a 'red flag' warning sign.
Dr Ogden: "It's certainly a worrying sign which would need more investigation."2:30pm: A nursing note is presented which showed Child C's weight, by June 13, had dropped to 717g. The note adds: "Doctors aware." Mr Myers says if that was the weight of Child C at birth, he would not have been card for at the Countess.
Dr Ogden: "I don't think so, no."2:31pm: Dr Ogden agrees at this point, there would have been some concerns with Child C, and he would've needed close monitoring care.
2:34pm: That concludes Dr Ogden's evidence. Dr Gail Beech is now being called to give evidence.
2:43pm: In June 2015, Dr Beech was working at the Countess of Chester Hospital as a registrar. She confirms working day shifts on June 11-12 and had involvement with Child C and his parents. She confirms she carried out an ultrasound scan for child C on June 11, and the reviewing doctor recorded 'NAD' - no abnormalities detected.
2:53pm: Dr Beech's note made on June 12, 10.15am is shown to the court. She recorded, from data, Child C was on CPAP, 30-40% oxygen assistance from CPAP, the saturation levels for Child C were '91-98%', with 'no documented desaturations'. Gases were 'satisfactory'. "It looks like he was pretty stable on those CPAP settings," Dr Beech tells the court. The gases refer to the blood gases. The urine levels were "slightly high, but not concerning yet". Under the heading 'sepsis', a CRP reading going up was "something to be aware of" but "not a huge rise", according to Dr Beech, and a note 'awaiting lumbar puncture' was made.
2:57pm: The lactate reading recorded is 1.8-2.8. Dr Beech says 2.8 is "high" but had been falling from a higher number.
2:59pm: Dr Beech said there was "nothing there" on the clinical chart numbers which was "worrying", with a few readings being "something to be mindful of". He was a "nice stable baby" as he had been allowed out of his incubator to be allowed skin-to-skin contact with his mum, Dr Beech added.
3:01pm: Dr Beech said the UVC had come out of Child C during a previous shift, and a note was made for a long line to be inserted later.
3:06pm: The follow-up note showed Dr Beech had inserted the long line under sterile conditions, and was secured in at the third attempt, with the note 'happy with position', adding 'patient left comfortable'. An x-ray of Child C, timed 12.36pm on June 12, shows the long line having been inserted.
3:12pm: An x-ray review recorded, in the comments, 'large stomach bubble, gaseous bowel'. Dr Beech said this "wouldn't be a huge concern" given Child C was on CPAP.
3:16pm: Dr Beech reiterates there were no significant concerns for Child C at that point, but there were "matters to be mindful of".
3:19pm: Mr Myers now asks Dr Beech questions on behalf of Lucy Letby. The three attempts to insert a long line, from a clinical note, are shown to the court again. Mr Myers asks if there is a guide to the number of attempts, or who should administer them. Dr Beech said it would be a procedure by a doctor, not a nurse, and would be done by the most junior doctor present, to get them experience, subject to availability and the complexity of the procedure. Dr Beech said there was "an unwritten rule" a registrar would have two or three attempts before escalating the procedure to someone more senior.
3:21pm: Dr Beech explains the note 'flushed' is made as confirmation the long line has been 'flushed' to ensure there is no air in it.
3:28pm: The x-ray of Child C with the long line in is presented to the court again. The dark areas in the stomach and bowel areas refer to air inside the body, the court hears. It is compared to an x-ray taken of Child C at birth, where there was also a pocket of air in the stomach. Dr Beech noted, from the June 12 x-ray, it was "very gaseous", and the result of CPAP. Mr Myers asks if that could also be termed 'CPAP belly'. Dr Beech says it could.
3:30pm: Dr Beech has concluded giving evidence. There will be a short break in court of about 10-15 minutes.
3:59pm: The court is now hearing evidence from Yvonne Griffiths, who was the Countess of Chester Hospital neonatal unit deputy manager in June 2015 and a senior nursing practitioner. An 'admin error' had resulted in Ms Griffiths' notes for child C being written in the file for a different child, but the error was spotted and rectified quickly. The note is written on June 14 on reflection notes from June 12, with care from 8am that day. The notes record "assistance with ventilation by NCPAP", with oxygen levels varying from 37% to 25%. Child C was "unsettled at times".
Ms Griffiths said he "only loved to be held by parents in a kangaroo style". The long line was administered, and at 6.30pm, 'bile noted on blanket'. Ms Griffiths said with any baby there is a worry with introducing feeds too early. On this occasion bile came out "spontaneously". Ms Griffiths said the nasogastric tube was aspirated as a matter of procedure and 2mls of black stained fluid appeared. Child C was "too unsettled" for a lumbar puncture - plan to reassess later". Ms Griffiths said they would not want to take the risk if the baby was too active, as a lumbar puncture would involve a needle. Ms Griffiths added she came in the morning after Child C had died, to assist staff.4:01pm: Mr Myers says Child C was "at the limit" [for weight] for being accepted into care at the Countess of Chester Hospital. Ms Griffiths had said, in a police statement, the hospital did not often care for babies of that weight. She tells the court there is a decision to be made whether the baby is suitable to be cared for at the Countess, or risking transfer to a tertiary centre, and that is made following consultation.
4:12pm: Ms Griffiths said, in the police statement, "it was very uncertain" what the outcome would be for Child C. She confirms she was the designated nurse for Child C on June 12. She also confirms Letby was not in the unit that day. Mr Myers talks through the nursing notes from the previous night shift, for June 11-12. At that point no bile aspirates had been recorded. He refers to a note about Child C requiring an increase in oxygen when handling as Child C was desaturating. Ms Griffiths says, in relation to the air in the stomach, the nurses "did everything" they could through the nasogastric tube to aspirate air.
4:18pm: The note referring to bile found on the blanket and 2mls of black stained fluid being aspirated from June 12 at 6.30pm is referred to. Mr Myers asks if dark bile is a matter for concern. "Any bile is a matter of caution," Ms Griffiths replies, and feeds would be stopped as a precaution. She added Child C did not desaturate when vomiting a small amount of fluid. She agrees it was important for close monitoring on Child C.
Mr Myers: "It is a potentially serious issue, isn't it?" Ms Griffiths: "Yes - and I did get the doctor to review."4:24pm: Ms Griffiths has finished giving evidence. The court has now adjourned for today. The trial will resume at the earlier time of 10am on Friday, October 28. We will be continue to provide live coverage throughout the day.
Friday 28th October 2022
Child C
Nurse Joanne Williams - Nurse Sophie Ellis - Nurse Melanie TaylorChester Standard Live Reporting
10:04am: The trial has now resumed, with evidence being heard in the case of Child C. The first witness to give evidence today is Joanne Williams, who previously gave evidence, in an agreed evidence statement, for the case of Child A and Child B. The court is reminded she was a neonatal unit nurse in June 2015.
10:10am: Mrs Williams recalls she was the designated nurse for Child C on June 13, and had cared for him prior to that day. She said that particular day shift was 'not too busy'. She recalls Child C was small and premature, and weighed 800g at birth.
10:14am: A nursing note by Mrs Williams is presented to the court, written retrospectively at 4.19pm on June 13, shows Child C was on NCPAP with 23-26% oxygen - "a minimal amount of oxygen". Mrs Williams said that was "a good sign". A blood gas reading was "very good" at 9am, but Child C was noted to be "very unsettled and fractious", which Ms Williams tells the court was not that uncommon for a baby of his size. The note adds Child C was allowed to be taken off CPAP to have skin-to-skin contact with mum. Mrs Williams says such contact is "extremely powerful" for a new-born baby and is "really beneficial" for them. The note adds Child C "calmed down straight away while on mummy, just required some facial [oxygen] while out. No signs of increased work of breathing".
10:17am: Child C was weaned off CPAP for two hours and placed on Optiflo at 1pm as, it was noted, the baby boy was "so unsettled on NCPAP". The court hears Optiflo is a less invasive form of breathing support than CPAP. Child C was "very settled this afternoon" with a "slight increase in respiratory rate". A further blood gas reading was taken later in the afternoon with readings "not quite as good", which Mrs Williams was "something to be taken into consideration" and had followed Child C being placed on Optiflo. The note adds: "Clinically remain stable but aware do not want to push [Child C]."
10:21am: Mrs Williams said fluids were increased, with 10% dextrose discontinued as it was day 4, and the dextrose would not have been needed with lipids [fats] increased to support nutrition. The note adds: "Continues to have dark bile aspirates, frequently this morning". Mrs Williams says it's "not reassuring" as it could be a sign of NEC [a gastro-intestinal disease]. Philip Astbury, prosecuting: "Was it of concern?"
Mrs Williams: "Yes." It was escalated to an on-duty doctor that day. Mrs Williams says Child C was on nil-by-mouth and a cautious feeding regime.10:28am: The court hears Child C had pulled out two oral gastric tubes during the morning due to being "feisty" and unsettled. A nasogastric tube was "on free drainage" to drain air from Child C, reducing air build-up in the stomach, and check for any aspirates. The notes adds: "Abdo[men] full but soft". The court hears that was "quite normal for a baby...for [Child C]." The abdomen had a "slight shine but not veiny or distended". The court hears a distended abdomen would be a symptom of NEC.
10:30am: The note adds: "If aspirates improve can start [trophic] feeds this evening". Ranitidine was administered via an IV to counteract the bile aspirates. The weight of 717g was noted, which Mrs Williams says is not unusual as all babies lose weight in the first few days. She said doctors were aware of the weight update. A cranial ultrasound scan was carried out, with 'no abnormalities detected'.
10:39am: An intensive care unit chart for Child C is now presented to the court, which details the various readings and notes corresponding to Mrs Williams's nursing note. The aspirates of dark bile are recorded at 9am and 1pm. 0.5ml dark bile is recorded at the latter, which was a "small" amount, but any dark bile was a "concern", Mrs Williams says. A further 0.5ml of dark bile is aspirated at 4pm.
10:43am: A nursing note of 'family communications', from June 13, is shown to the court, written by Mrs Williams. She records: "Mummy and daddy on the unit during the day, both have had skin-to-skin with [Child C]. Pleased to see him more settled this afternoon. "Appear happy with plan of care."
10:45am: A further nursing note showed a blood gas reading at 6pm was "improvement from previous CBG", but lactate levels had increased. Child C remained on Optiflo and was "stable". The aspirates were "reduced this evening". The note adds: "?? Commence enteral feed tonight" Mrs Williams clarifies: "Query query."
10:46am: Mrs Williams said you would "always be cautious of a baby that size", referring to Child C. Mr Astbury: "How was the progress during that shift?"
"He had done well, weaned off to Optiflo, he had benefitted from time with mum and dad."10:51am: Ben Myers KC, for Letby's defence, is now asking Mrs Williams questions. She agrees that "you can never be complacent" with a child like Child C, and however stable he is, he would require close monitoring. She said it was important to carry out observations, and look for "subtle signs".
10:54am: Mr Myers says the observations for Child C need to be taken into context for a baby the size of Child C. Mrs Williams says that could "potentially" be the case. She adds she was aware of pre-existing concerns raised at Child C's birth.
10:57am: Mr Myers asks if Child C still needed breathing support with Optiflo, and would not have been switched if he had been settled on NCPAP. Mrs Williams says he had good blood gases so was able to "step down" respiratory support to Optiflo.
11:00am:
Mr Myers: "You are documenting all the little changes made [on the nursing notes], because he is such a little baby?"
Mrs Williams: "It is important to be thorough."11:03am: The note of 'aware do not want to push [Child C]' is raised.
Mrs Williams: "It's making sure we are doing individual care and very aware of what's happening with [Child C] and what he needs." Not wanting to push Child C was not to tire him, and/or administer procedures such as a lumbar puncture. Mrs Williams said not wanting to push Child C, in this context, was in relation to breathing.
Mr Myers: "Could that apply to feeding as well?"
Mrs Williams: "Yes." The matter of dark bile aspirates is mentioned.
Mr Myers: "We have seen from the chart, that aspirates have been taken throughout the day, and they have been there the day before?"
Mrs Williams: "Yes."11:05am: A distended abdomen could be a symptom of other conditions, Mrs Williams adds, but NEC would be one which would be of concern.
11:07am: The 'trophic feeds', as mentioned on the nursing note, would be via expressed breast milk if the aspirates improved, along with the "overall clinical picture", Mrs Williams tells the court.
11:09am: The weight of 717g is "a significant reduction, isn't it?" Mr Myers asks. Mrs Williams says it would need to be taken into context, and it was important to administer feeds safely. The plan to do so would be, following a discussion, to commence enteral feeds that night.
11:12am: Mr Astbury rises to ask one more question on CPAP: "Would you ever take a baby off CPAP just if they were unsettled?"
Mrs Williams: "No." The court hears the step down to Optiflo would be done in consideration with other factors. Mrs Williams has now finished giving evidence for Child C. There will now be a short break in court before the trial resumes.11:32am: The trial is now resuming.
11:34am: The next witness to give evidence in court is Sophie Ellis, who was working as a neonatal unit nurse in June 2015. She recalls Child C, and first saw him first when he was delivered, as an observer, learning in the nursing role.
11:36am: She said she was on duty for the night-shift of June 13, starting at 7.30am, ending at 8am the following day. She said she was allocated to look after Child C for that shift, on her own, with support from another staff member as she was junior in her role.
11:38am: The nursing staff roles for that shift are presented to the court, with Ms Ellis the designated nurse for Child C, and Lucy Letby looking after two other babies in the neonatal unit.
11:45am: She said she was aware Child C had been moved to Optiflo, and knew the subject of feeds was a topic being discussed, that they were "hopefully" going to start feeds. Her nursing note is shown to the court, showing care taken over at 8pm. "Safety checks completed and fluid requirements calculated...Optiflo...in 25% [oxygen]. Observations satisfactory...[respiratory rate]...elevated at times as previously been for past few days. "Pink and well perfused. Active and alert." The fluids dose is stated "due to birth weight of below 1000g". The long line site was "satisfactory". A blood gas reading was to be taken at 2am. Trophic feeds were agreed to be started.
11:46am: Ms Ellis said she was not present for the first desaturation as she had left the room.
11:48am: A discussion on trophic feeds was had "before 11pm", with the feed administered at 11pm. Ms Ellis said "there was nothing particularly striking" about the care for Child C between 8-11pm, he was "doing well" and was "feisty" at that time.
11:53am: A retrospective note written by Ms Ellis says: "Had 2x fleeting [Bradycardia]s - self correcting not needing any intervention shortly before prolonged [Bradycardia] and apnoea requiring resus[citation]. She said she had left the room "just around the corner", then the alarm went off. She said she could not recall which type of alarm it was - a lower-level yellow or a more frequent [urgent] red alarm. She said she went into the nursery, having been out for "not a long" time. She recalls, upon entering: "I saw Lucy standing at [Child C's] incubator. She said he had just had a Brady and a desaturation. I can't remember what she was doing at the time."
11:57am: "After that, the 'brady' and the desat resolved quite quickly." Ms Ellis said she didn't do or see anything being done to correct the desat and bradycardia, as Child C self corrected. She added she then sat at a computer which faced a wall, with Child C behind, out of view. She explains Lucy Letby was still in there, but not sure about anybody else. Child C, Ms Ellis tells the court, had a further 'brady' and desaturation which did not resolve and required resuscitation. She said when she turned around, Lucy Letby was stood at the incubator. A nursing colleague had asked her to put out a crash call.
11:58am: Prior to administering the 11pm feed, Miss Ellis said she had aspirated a tiny amount of 'light green bile' from Child C.
12:00pm: A nursing colleague who was in the room said to put out a crash call, and Miss Ellis left the room, she tells the court. She said she left the room "not long". She said when she returned, a nursing colleague was getting ready to administer drugs, and for her to continue chest compressions. She said Lucy Letby was at the side of the incubator, but cannot recall what she was doing. Miss Ellis said the medical team of registrars arrived along with a doctor to the unit at some point.
12:03pm: Miss Ellis adds the parents were then informed. She said she became upset herself as this was "the first time" something like this had happened in her experience, and she found it "overwhelming". Lucy Letby said to her: "Do you want me to take over?" to which she said: "Yes." Miss Ellis said she then left the room, taking a minute to compose herself, before returning to the unit to look after other babies.
12:05pm: The nursing note says care for Child C was handed over to senior nurse Melanie Taylor following the collapse. Miss Ellis reiterates that, from memory, there was nothing that concerned her about Child C's condition between 8pm-11pm.
12:06pm: Mr Myers asks how long Miss Ellis had been working at the Countess - she replied it was since January 2015.
12:08pm: Miss Ellis she had not previously cared for a baby as small as Child C. Mr Myers asks: "How is it that someone as inexperienced as you [was given the responsibility of looking after Child C]?"
"Child C was very stable and I was being supported by Mel[anie Taylor]. "You were very well supported at the Countess of Chester Hospital."12:09pm: Miss Ellis said there was "always a nurse" in the room looking after Child C, even when she left the room briefly. She said Lucy Letby was in there, and cannot recall if Melanie Taylor was also in there.
12:12pm: Miss Ellis says Child C "could have had" two bradys, as they are quite common. She said she did not know whether Melanie Taylor was in the room at the time of the collapse.
12:13pm: Miss Ellis tells the court for one of the two bradys, Lucy Letby was in the room for the second one, but not the first.
12:18pm: Mr Myers refers to the 8.46am, June 14 nursing note and said there was nothing prior to the 11.15pm collapse. He asks why the first bradys are not mentioned.
Miss Ellis: "I would have forgotten to write it - it was a traumatic shift". Miss Ellis says she would have added the detail of that on her subsequent nursing note. She says she does not remember if Melanie Taylor was in the room at the start of the collapse. Mr Myers puts it to Miss Ellis that Lucy Letby was not in there at the time of the collapse, and only arrived later [during the resuscitation efforts].
Miss Ellis: "I don't agree with that."
Mr Myers: "You have placed her there when you spoke to the police several years later."
Miss Ellis: "I don't agree with that."12:21pm: Miss Ellis has finished giving evidence for Child C.
12:39pm: The next witness to give evidence in the case of Child C is Melanie Taylor, who has previously given evidence for Child A and Child B. The court is shown Melanie Taylor's observation chart for Child C on the night shift from June 12-13, where "normal" readings are made for the heart and respiration rate. Two of the readings were "slightly elevated" but were normal given the context Child C was on CPAP at the time. Temperature readings were "stable and in normal limits - what you would expect". Other readings were considered to be normal.
12:45pm: Other CPAP readings were "normal". Fluid readings are recorded on a fluid chart, including the "dark bile aspirate". Ms Taylor says: "We would be concerned about NEC [with those aspirates]."
12:52pm: Ms Taylor concludes Child C was a "stable baby". There were concerns over bile aspirates but they were not uncommon in neonatal babies. She adds the aspirates found were: "Not a major cause for concern"
12:56pm: Ms Taylor says further observations were made to check for symptoms of NEC, but the 'tummy soft, not distended' was a good sign. The registrar was made aware of the dark bile aspirates.
Ms Taylor: "From what I've written, he was a stable baby."12:59pm: The court is now adjourning for a shorter than usual lunch break. The trial will resume later this afternoon, with Ms Taylor giving further evidence.
1:43pm: The trial is now resuming.
1:47pm: The handover note for the June 13 night shift is presented to the court, showing Melanie Taylor is one of the nurses on duty that night, and a designated nurse for one of the babies (not Child C) that night. She confirms she was present in room 1 that night, in the same room as colleague Sophie Ellis. "Sophie was a very competent nurse. She was completely able to look after [Child C]. I had no concerns [with her], he had been stable. I was there for support if she needed it."
1:50pm: Ms Taylor said her memory of the collapse was that she did not know where she was at the time Child C deteriorated, but when she arrived at the incubator, Lucy Letby "was already there". She did not know if anybody else was in the room at that point. She recalls: "I think also Sophie was there - as she was caring for him." Ventilation support was provided via a Neopuff device, and Ms Taylor struggled to get any chest movement for Child C.
1:51pm: Ms Taylor said Lucy Letby suggested using a type of ventilation support - a Guedel device - to aid Child C.
1:54pm: The Guedel device was followed by use of the Neopuff. Ms Taylor said a crash call was put out. She added, from her statement, chest compressions began before the first doctors arrived in the unit. The on-call registrar was first to arrive, Ms Taylor said.
1:57pm: Ms Taylor recalled the chest compressions and resuscitation attempts went on for some time. Child C later died, the time of death recorded as 5.58am on June 14. A retrospective nursing note by Ms Taylor, written a couple of hours later, said: "Called to help as baby had brady desat, when arrived to baby, baby apnoiec..."
2:01pm: The notes describe the resuscitation attempts made. An addendum made at 8.14am said: "Parents stated with [Child C], they took him round to quiet room...registrar went round to quiet room, as mum concerned he is still gasping and has pulse. Doctor explained that it is a brainstem response following resuscitation, further discussion with parents, parents happy for [Child C] to have IV morphine for comfort. "Maternal and paternal grandparents present, discussed with parents what they would like to do, and offered that we can do it at their pace when they are ready." The note concludes that a camera was left with the parents if they wished to take photos of Child C. They declined, and had taken some photos on their phone. Child C's hand and footprints were made for the parents.
2:02pm: Mr Myers is now asking Ms Taylor questions about dark bile aspirates. He said Child C was "a stable baby", with the aspirates not being "a major cause for concern". Ms Taylor said: “It’s not something we would initially be very worried about, but would take into consideration...and act very cautiously when we find bile. "I was not necessarily concerned he was unstable."
2:03pm: Ms Taylor: "You have to look at the bigger picture and see what it could possibly be, and see if it could be NEC, and act on that and take it as a consideration."
2:05pm: "We do encounter it [bile] in premature babies. We would have to act appropriately and if there are no other signs of NEC then we would treat accordingly." Mr Myers asks if there could be other, more immediate problems associated with dark bile. Ms Taylor said that would be a matter for doctors to examine if there was a possibility of that. "There is no room for error with a baby like [Child C] is there?" Ms Taylor agrees, and agrees there are "inherent risks" with treating such a baby.
2:06pm: Mr Myers asks about the experience of colleague Sophie Ellis.
Ms Taylor: "You do have a foundation training in neonatal care and you would look after a baby on CPAP. New nurses have to get experience and I was supervising and she was very competent. "She would not have been left alone."2:10pm:
Mr Myers: "It was a very busy shift, wasn't it?"
Ms Taylor: "Yes." Mr Myers says Ms Taylor was not sure she was in the room when the collapse happened. "The only person you remember [being there] was Lucy?" Ms Taylor agrees. She adds she assumed Sophie Ellis was also present.
Mr Myers: "It is from your account, Lucy is there, no-one else is present, maybe Sophie?"
Ms Taylor: "Yes."
Mr Myers: "I am going to suggest, you were in the nursery when this happened?" Ms Taylor says she doesn't believe so.
Mr Myers: "That it was Sophie Ellis who called you?"
Ms Taylor: "It might have been."
Mr Myers: "That Lucy Letby was not there at the start of this?"
Ms Taylor: "I disagree."2:14pm: Mr Myers says Ms Taylor, in her police statement, said she was "pretty sure" she was "already in nursery room 1", feeding another baby, at the time of the collapse. Ms Taylor says her memory has deteriorated since then, and what is in her police statement is correct. Mr Myers says Ms Taylor's police statement said she was called over by Sophie Ellis, and there is no mention of Lucy Letby.
Ms Taylor: "No, but she was there."2:19pm: Ms Taylor said she read her police statement for the first time this morning and had not memorised everything from it. She added: "I didn't say Lucy Letby called me over. "I likely wasn't asked [by police] if Lucy Letby was there. "Now I have been shown that [statement], I can remember Sophie called me over. "Years have passed since this has happened." Ms Taylor said she has not changed her mind about who was present there. "I tell you now, when I approached the incubator, she [Lucy Letby] was there on the other side." She added she remembered how "cool and calm" Lucy Letby looked at the time. Ms Taylor said she hadn't said Lucy Letby was not in room 1 at the time of the collapse.
2:20pm: Ms Taylor tells the court said she didn't think it was necessary at the time to include that information [of Letby's presence] to police.
3:20pm: The trial has been adjourned for today - the jury had been made aware there would be an early finish for this day.
Monday 31st October 2022
Child C
Nurse B (shift leader) - Dr Katherine Davis - Dr John GibbsChester Standard Live Reporting
9:29am: A reminder that the Lucy Letby trial is due to last six months, so although the court case is now entering the fourth week before a jury, there is still a long way to go before its scheduled conclusion.
10:44am: There has been a delay to the start of today's trial.
11:23am: The current estimated time for the trial to resume today is 11.30am.
11:33am: The trial is now resuming. The judge, Mr Justice James Goss, apologises for the delayed start, which he said was due to a cancelled Northern Rail train.
11:34am: The first witness to give evidence to day is from a nurse, who cannot be named due to reporting restrictions, who explains she was a shift leader at the Countess of Chester Hospital neonatal unit in June 2015.
11:40am: The nurse explains to the court the types of different care that would be provided to babies arriving in the neonatal unit.
11:43am: The nurse is now being asked questions on Child C. A reminder that none of the children listed in the charges can be identified, so a naming system of 'Baby/Child A' to 'Baby/Child Q' is being used by the press.
11:47am: The nurse said back in 2015, she was not sure she was the one allocating the designated nurses to the babies for that shift, as the allocation system was in the process of changing. She said she remembers Sophie Ellis was the designated nurse for Child C that evening. She says Sophie was a "very competent nurse", having come through the neonatal unit as a student nurse.
11:49am: The nurse remembers there being 'no clinical concerns' for Child C at the start of the shift.
11:50am: The nurse says she remembers Melanie Taylor also being assigned to room 1, with Sophie Ellis who was looking after Child C. Melanie Taylor "would be there for support, for Sophie".
11:54am: The nurse also recalls Lucy Letby was on duty that night, looking after 'at least' one different baby, in room 3. The nurse said she had 'concerns over respiratory distress' for that baby at the start of that night shift. He was 'grunting', and such symptoms had not been present prior to that. The nurse asked Lucy Letby to increase the observations for that baby from two-hourly to one-hourly and call the registrar in.
12:00pm: The prosecution asks the nurse about Child C's collapse at 11.15pm. "I do not remember where, but I was not in nursery room 1." She recalls "a shout for help", but does not remember who called it. She entered room 1 and saw Melanie Taylor and Sophie Ellis, and a Neopuff device was being administered. She noticed Child C was not breathing and the heart rate was very low. The Neopuff gave Child C chest movement, but he did not breathe himself. Child C had a "mottled" skin appearance, the nurse recalled. She remembers a crash call being put out, and recalls Lucy Letby being present, but does not recall when Letby entered the room. She recalled Sophie Ellis "becoming emotionally upset" and the nurse said she advised her to step outside.
12:02pm: The nurse remembers resuscitation efforts were made, and Child C was baptised, and overseeing palliative care to make the baby boy more comfortable before he died.
12:05pm: The prosecution asks: "Whose responsibility is it to ensure the memory box is made and who takes care of it?" The nurse: "The designated nurse at the time, if they're able." The nurse said Melanie Taylor took over as designated nurse and "partly" arranged the memory box. The nurse explains she asked Lucy Letby to focus back on a baby in nursery room 3, but Letby went into the family room "a few times". The nurse recalled asking Lucy Letby to leave the family to Melanie Taylor. The nurse tells the court Letby did not have any designated duties to be in the family room, and told her "more than once" not to be in the family room. Ben Myers KC, for the defence, is now asking the nurse questions.
12:12pm: Mr Myers asks the nurse how busy the unit had been between 2015 and 2016, and from a statement she had made, there were more babies arriving into the unit, and more "intensive unit" babies arriving. Mr Myers said the number of intensive unit babies arriving seemed more than what Arrowe Park, a tertiary centre, had. Mr Myers says the nurse, in her 2018 statement, said a ward manager was "fighting" for more nursing staff for the Countess of Chester Hospital neonatal unit. "She still is."
"We sometimes weren't meeting staff guidelines for ratios." The nurse replies that was the case across the nursing network. The nurse agrees it was "not an ideal experience for staff."
Mr Myers: "And not an ideal experience for babies? There will be a danger of a knock-on effect." The nurse replies: "Just because the amount of babies increased does not mean we were not compliant on any shift." The nurse says she did not say staff were "struggling to cope", after being asked about her statement saying staff were missing breaks during "busy" shifts.12:17pm: Mr Myers asks about Child C, asking if he was in a "potentially fragile condition". The nurse agrees. Mr Myers says that due to his size and prematurity, there was a risk he could die. The nurse agrees.
12:21pm: The nurse says she could have changed the staffing allocation for designated nurses for that night shift, had she wanted to. She says she does not know whether Sophie Ellis had looked after a baby as premature as Child C before, but had confidence in her as Melanie Taylor was there for support. She says she does not recall if Lucy Letby had asked her to spend some time in that room 1.
12:30pm: Mr Myers asks about Child C's collapse. The nurse says she was not in room 1 at the time, but saw Sophie Ellis and Melanie Taylor in that room, attempting to assist Child C's breathing with the Neopuff device when she arrived. The nurse says an initial crash call was put out, followed by one for a consultant. Mr Myers says the police statement refers to "I think Lucy Letby was in the room by now". The nurse said she made the statement three years after the incident, and could not recall precisely when Letby had entered. Mr Myers asks the nurse if she was the one to take an upset Sophie Ellis aside and get her to step down from duty for that time. The nurse agrees. The nurse said Lucy Letby returned to looking after the other babies "after a number of askings" not to be in the family room, as the nurse and Melanie Taylor were looking after Child C and his parents following the collapse.
12:34pm: Simon Driver, for the prosecution, rises to ask the nurse more questions. The nurse is asked if, given the busy shift, the quality of care was in any way "diminished" for Child C. The nurse says "no". The nurse adds she would have allocated Sophie Ellis to look after Child C as the designated nurse, with Melanie Taylor supervising, as she believed her to be competent. The nurse said she believed another baby on the neonatal unit - the one Lucy Letby was designated to look after that night - should have had more care, including a septic screening, as the nurse believed that child was the most concerning to her that night.
12:38pm: The nurse says, from her police interview, she "believed" Sophie Ellis and Melanie Taylor were in room 1 with the Neopuff device when she arrived. The court hears the response from police was "ok", followed by the nurse saying: "But I...100 per cent couldn't tell you", which the prosecution say meant she was not 100 per cent sure.
12:49pm: The next witness to give evidence is Dr Katherine Davis, who in June 2015 was a paediatric registrar at the Countess of Chester Hospital. The court hears she had been working night shifts for the night Child C collapsed, and the previous night.
12:52pm: Dr Davis says she does not recall the previous night shift, but from her nursing notes on the night shift of June 12-13 she recalls the observations for Child C at 9.20pm on June 12, 2015. The notes include "suspected sepsis" and "jaundice" on a list of ongoing problems. The latter is, the court hears, "very common" in premature babies.
12:54pm: Dr Davis added that, at that point, there had been 'no desaturations' or 'bradys' (bradycardia). Child C was 'NBM' (nil by mouth) due to "bilious aspirates".
1:02pm: Dr Davis's notes include simple drawings of the lungs and abdomen. The lungs had "good air entry", with the abdomen 'soft' and 'not discoloured'. Dr Davis says there was "nothing worrying" about Child C's tummy at the time, noting that there would likely be air in the stomach due to him being on CPAP.
2:02pm: The court has been adjourned for the lunch break, and is expected to resume from 2.05pm.
2:08pm: Dr Katherine Davis is continuing to give evidence, with prosecutor Philip Astbury asking questions in relation to the collapse of Child C. She said she would have received a 'crash call' bleep, and was "relatively close" to the unit when it happened. She remembers "a lot of activity" when she went into room 1. She remembers there being a senior nurse present, but beyond that, is not sure of who was there.
2:12pm: Dr Davis's note is presented to the court, written at 1.30am on June 14 and timed retrospectively. The note said she was arrived at the unit in "less than one minute" after the crash bleep went off. A 'Guedel airway in situ' was noted, with chest compressions in progress. Dr Davis noted 'occasional intermittent gasps noted'. Dr Davis said she believed Child C "looked pale" when she arrived. Dr Davis explains chest compressions would stop "briefly" to detect if Child C had a heart rate, and if there was no heart rate, which Dr Davis said "was unusual" from her experience.
2:18pm: Chest compressions were restarted and the on-call consultant was called "urgently". Dr Davis attempted to intubate Child C, but was unable to do so as Child C's vocal cords were swollen. Dr David tried again with a smaller tube, twice, but was again unable to intubate. A list of drugs was administered, including several doses of adrenaline.
2:20pm: The next note was at 2am, following a "prolonged attempt" at resuscitation.
Dr Davis: "It became obvious that we were not winning, we hadn't got a heart rate". The failure to resuscitate was "very unusual" as premature babies usually had some response to resuscitation efforts, even if it was temporary, Dr Davis tells the court. Child C had no response.2:29pm: Dr Davis said baptism of Child C took place, and it was noted during the resuscitation attempts that a capnograph on Child C had detected carbon dioxide coming out of the baby boy. The on-call consultant was called. The baptism and blessing were completed. "Unexpectedly," Dr Davis said, Child C was gasping and had a heart rate at this time. A discussion was had at the "appropriate way forward", and "unfortunately", it was concluded Child C would have had a lack of oxygen to the brain for a "prolonged time" which would have left him with significant damage to the brain and potential other issues, such as kidney damage. Morphine was administered to Child C for pain relief, following a discussion with Child C's parents, as Child C was "unlikely to survive".
2:31pm: Dr Davis said she was later called by a family member of Child C to be informed they had believed Child C had died, and she explains she would have carried out the necessary observations, and verified the baby boy had passed away.
2:32pm: Ben Myers KC, for Letby's defence, is now asking Dr Davis questions. He says that Child C "was on the limit" of what the Countess of Chester Hospital could treat, being at 800g birth weight. Dr Davis agrees.
2:34pm: Mr Myers is referring to Dr Davis's notes on June 12, where a "raised CRP" reading is noted, which he says is "a potential marker for infection". Dr Davis agrees. She also agrees Child C is at increased risk of abdominal problems due to his prematurity.
2:36pm: Mr Myers asks about the bilious aspirates. Dr Davis says any such aspirates, of any colour, are a cause of concern.
Mr Myers: "It's a red flag for a problem, isn't it?"
Dr Davis: "Yes."2:40pm: Dr Davis said she would have examined the "bigger picture", in that Child C handled well, had a soft abdomen, and there were bowel sounds. "There was no suggestion we should do anything different." Dr Davis said there were no other signs of NEC. Mr Myers said the bile aspirates could be a symptom of something else. Dr Davis says Child C was examined for other symptoms, but was still "well", and his bowels were not yet open. Dr Davis adds: "He had a lot of challenges, but he was doing well."
Mr Myers: "He had the potential, as a small baby, to deteriorate rather rapidly?"
Dr Davis: "Yes.2:44pm: Dr Davis said Child C "was not getting sick" despite the readings of dark bile aspirates. "It is not something we should ignore, it's something we would keep an eye on...but I don't think there was anything else we should have done." She adds that dark bile is "not normal", but "not uncommon" in premature babies. Mr Myers said Child C was not seen by a consultant until three days after he was born, on June 13, and "the appropriate step" would have been for Child C to see him before then. Dr Davis said such a step would have been discussed prior to June 13.
2:50pm: Mr Myers said the collapse of Child C happened before Dr Davis had a chance to review him. Dr Davis agrees. Mr Myers refers to the circumstances of Child C's collapse. He asks if a tertiary unit would have had advanced practitioners capable of intubating a baby. Dr Davis said they would have had more staff available, but cannot comment on Arrowe Park. She says from her experience in a tertiary centre, there would be advanced nursing practitioners, but they would not work night shifts.
2:53pm: Dr Davis said there would be a risk-benefit discussion for whether a baby would be in a level 2 unit at the Countess of Chester Hospital, or a level 3 unit such as Arrowe Park. She said there would be risks in transporting a baby in an ambulance to that tertiary centre. She adds bed availability would not be an issue as they could always transport out of the region if necessary.
2:58pm: Dr Davis said at the time she arrived in room 1, the nursing staff were doing everything they could do. She says that the decision to intubate was not necessarily the right or wrong thing to do, but had its advantages. The intubation period would have lasted about 30 seconds, as during that time Child C would not have had Neopuff bag support. Dr Davis said after those 30 seconds, efforts to resuscitate using the Neopuff would resume.
3:02pm: Dr Davis said despite the resuscitation attempts, Child C would have had a "huge amount of time" without a heart rate.
Mr Myers: "Did the delay in intubation cause any difficulties down the line?"
Dr Davis: "No."3:04pm: Philip Astbury rises to ask if Dr Davis had seen a collapse that sudden or unexpected in a child like Child C before.
Dr Davis: "Absolutely not." She adds that from her experience, she had seen a lot of babies with significant abdominal issues, and had dealt with babies with NEC, but they didn't "behave or die in the way that [Child C] did."3:17pm: We have had a short adjournment while the next witness comes to give evidence. The next witness is Dr John Gibbs, who in June 2015 was working at the Countess of Chester Hospital as a consultant paediatrician, and had been working at the hospital for over 20 years.
3:26pm: He says he had seen Child C a few times during the first few days of his life, and had carried out a review. "There was no particular concern" about Child C, despite there being gastric aspirates, and while being "small" even for being premature, he was at risk of conditions such as NEC. He said such aspirates were "not uncommon" as gastric acid could accumulate in the stomach, and Dr Gibbs recommended an antacid be given for the stomach. He says Dr Ogden's note of the abdomen being "soft, not distended" is a "very reassuring sign". Dr Gibbs said if the aspirates "got steadily larger" that would be a concerning sign, and a symptom of NEC. It was decided, Dr Gibbs said, to monitor the aspirates and hold off giving feeds at that time. He said if the aspirates got larger, or came with vomiting, then an abdominal x-ray would be carried out.
3:32pm: Dr Gibbs said he carried out an ultrasound scan of Child C's head, which was recorded as 'normal', a 3.55pm on June 13. He was next involved with Child C as the on-call consultant, having received an emergency call at about 11.28pm. A note is written, retrospectively, by Dr Gibbs at 12.30am. He said then when he arrived, efforts were being made by staff to resuscitate Child C. He said Child C looked "pale and mottled", which he said was "not uncommon" in babies in cardiac arrest.
3:40pm: The notes show Dr Gibbs intubated Child C to provide more effective ventilation. He adds that ventilation can also be obtained through the Neopuff device.
3:43pm: Dr Gibbs says that babies experiencing a sudden and unexpected collapse would normally be expected to show some signs of responding to resuscitation efforts, and it was "unusual" Child C did not.
3:52pm: The resuscitation attempts were said to have "failed" after 40 minutes. Dr Gibbs said it was "standard practice" for attempts to cease after 20 minutes, but staff would carry on for a little longer "in the hope" of the baby responding. Resuscitation efforts continued after the 40-minute point while the priest arrived to baptise Child C. He said, "surprisingly", there were some "minimal" signs of life in Child C, and he was "not sure what to do" as it was "unexpected". He was "not sure" why a feeble heart rate, and breathing gasps, were being recorded for Child C. He relayed to the parents that, due to the prolonged time without oxygen, the chances of Child C being brought back without "profound" brain damage were "extremely remote".
3:53pm: Dr Gibbs said it was planned to offer Child C palliative care for his final hours.
3:55pm: Dr Gibbs said he could not provide a cause of death, so subsequently contacted the coroner's office.
4:01pm: Dr Gibbs said a debrief was carried out for Child C's fatal collapse on July 2, in which the circumstances were discussed. It was noted, in a summary of the debrief, Child C 'did not seem unwell', was 'active (kept pulling out NG tubes)', an infection was 'suggested' but Child C was on antibiotics. Dr Gibbs noted in the debrief the collapse was not related to the feed, which was administered shortly before the collapse, as he said he could not see how the administration of a 0.5ml feed could lead to a cardiac arrest. The resuscitation was performed "technically well", and the "team worked well together". Dr Gibbs explains the context from the notes, was that the staff had done everything they could to save Child C.
4:04pm: Dr Gibbs said it was not possible to rule out a pulmonary embolus - a blood clot which breaks off from another part in the body, blocking lung circulation. Another theory was toxins from medicine administered. The post-mortem had been held at this point, but the results were not available.
4:08pm: The debrief noted that Child C's parents were advised that "further life support measures" were "futile". Dr Gibbs said the notes said for future situations, rather than prolonging a baby's life with 'token resuscitation efforts' for a priest/vicar to arrive, it would be better for a nursing member of staff to carry out the baptism duties themselves. This would be in the event of following prolonged, and ultimately failed, resuscitation efforts which left a baby with no realistic prospect of survival. Dr Gibbs said he would have discussed this with the rest of his consultant colleagues.
4:13pm: Dr Gibbs said he wants to clarify that he is not blaming the parents for requesting to allow Child C to be baptised, and the wait that followed for a priest and vicar to arrive. He said the problem was that Child C's heart and lungs restarted following the token efforts to resuscitate, and he could not think why that was the case. "Whatever catastrophic event that had happened [to Child C] had reversed, or begun to reverse. "I don't understand that from a natural disease process." He said it was right the parents requested for a priest to arrive for baptism. He adds the difficulty was that Child C's heart and breathing restarted following that.
Tuesday 1st November 2022
Child C
Dr John Gibbs - Statements from Dr Andrew Brunton (trainee paediatrician) & Nurse Bernadette Butterworth - Dr Dewi Evans - Dr Sandie BohinChester Standard Live Reporting
10:34am: The trial is now resuming, with Dr John Gibbs giving evidence.
10:39am: Philip Astbury has one more question to ask for the prosecution, about monitors in place at the neonatal unit in June 2015. He asks Dr Gibbs if such monitors record the displayed readings, for people to look up a potential archive of readings. Dr Gibbs says he isn't sure, but doesn't think they did. He adds he hasn't done so, in his practice.
10:43am: Ben Myers KC, for Letby's defence, is now asking Dr Gibbs questions. He asks about the staffing arrangements in place at the hospital at the time. Dr Gibbs says at the time, he is fairly sure the paediatrician of the week on a rota would cover the children's ward and the neonatal ward. They would not have any planned clinics for that week. Other consultants would cover during the night, as that paediatrician could not cover a 24/7 week, the court hears.
10:47am: Dr Gibbs said the workload would depend on need, and consultants would spend more time on the paediatric ward as there would be much more turnover there than the neonatal unit. Mr Myers asks if Dr Gibbs would agree consultant cover was stretched during 2015-2016 Dr Gibbs said more consultants arrived after June 2016, but they had been requested for several years. The consultant cover at the time was "fairly typical" for a level 2 unit, the court hears.
10:51am: Dr Gibbs said the addition of two consultants "had been planned" for many years. He said "every speciality wants more staff", as did a lot of hospitals, given the context of the staffing pressures of the NHS overall. "We wanted to increase the number of staff so we could reduce the number of hours". Mr Myers says the two consultants arrived after the Countess of Chester Hospital was reduced to a level 1 neonatal unit in June 2016. Dr Gibbs says that is the case, but the two were not linked.
10:54am: Mr Myers asks about Child C being 'on the limit' with birth weight. He asks whether it would be "almost inevitable" Child C would have faced complications, and asks if in hindsight, Child C should have been cared for at a tertiary unit.
Dr Gibbs: "That depends on what causes sudden and unexpected collapses [leading to his death]." Mr Myers asks, taking that aside, should Child C have been cared for at a tertiary centre.
Dr Gibbs: "No."10:58am: Mr Myers asks about the bilious aspirates found. He says if a baby is producing dark bile, if that is a concern.
Dr Gibbs: "It raises some concern, yes."
Mr Myers: "It's potentially serious, is it not?"
Dr Gibbs: "No - it comes from acid reflux...some normal premature babies [produce bile aspirates]." He adds that is why an antacid was administered to Child C.11:08am: Mr Myers produces a nursing note from Yvonne Griffiths, which refers to, on June 12, 2mls of 'black stained fluid', plus 'bile on blanket'. Dr Gibbs says he would have been concerned if Child C had continued to vomit bile, and there was a lot of it. Mr Myers produces the intensive care unit chart for June 12, showing 'vomit dark bile' at midnight. He asks if it is a matter for concern. Dr Gibbs says there is one note of vomit, and says that is a worry, but would be more concerning if it was repeated. The intensive care unit for June 13 is presented, showing more dark bile readings. Dr Gibbs says there are no more vomit readings, and the June 13 readings are from aspirates, which can be common in premature babies.
11:12am: Dr Gibbs says the aspirates were not increasing from 0.5ml on June 13. He said the baby would be examined first, with an examination of the abdomen. Mr Myers asks if there was a possibility of something other than NEC Child C could have had. Dr Gibbs says NEC was "a particular risk", but there could have been an obstruction in the body, and medical staff would not have just been focusing on looking for symptoms of NEC.
11:26am: A diagram of the small and large intestine is presented to the court. Mr Myers asks about the passage of air, and refers to radiograph images for Child C, one taken on June 12, and the accompanying note refers to 'marked gaseous distension of the stomach and proximal small bowel'. Dr Gibbs says there is 'not much air in the large intestine' shown. Mr Myers asks if there is an obstruction. Dr Gibbs says it is a possibility, and the air seen is common for babies on CPAP ventilation. Mr Myers asks if there is an intestinal blockage. Dr Gibbs says it is a possibility. Mr Myers says a symptom of intestinal blockage is vomiting dark bile. Dr Gibbs says there is only one recorded instance of that, and the symptom would be 'repeated vomiting'. He says a sign of an intestinal blockage would be a 'very distended abdomen', and when he examined him on June 13, Child C had a 'soft, not distended abdomen'.
11:27am: Dr Gibbs adds the amount of dark bile aspirates, in the case of an intestinal blockage, would increase, and that was not the case with Child C.
11:35am: Dr Gibbs says an obstruction is "a possibility", but "not the explanation". Mr Myers asks if not looking to see whether Child C had a potential obstruction, in view of vomiting dark bile, was "a potential mistake". Dr Gibbs repeats there was not repeated vomiting, and dark bile aspirates would be found in normal babies. The court hears Child C did not have his bowels open during his life. Dr Gibbs says that was not surprising as he had not been fed. Mr Myers asks if that was unusual, after three days, for the bowels not to open. Dr Gibbs said it could be unusual, but Child C had not been fed, so there were not going to be bowel motions.
11:39am: Mr Myers asks if it would have been preferable for Child C to have been examined by a senior consultant prior to June 13.
Dr Gibbs: "It would have been preferable if there had been significant concerns about him, and he had not already been reviewed by the registrar and junior doctor." Dr Gibbs said he would have carried out daily reviews, without a full examination, of neonatal unit babies.11:42am: Mr Myers asks about Child C's collapse. He says Dr Gibbs intubated Child C at the first attempt, and said Dr Gibbs had told the court intubation was more effective than Neopuff. Dr Gibbs said it was more effective during prolonged resuscitation attempts, and Neopuff by itself was effective too. Dr Gibbs said even if he was unable to intubate Child C, Neopuff administration could have continued.
11:48am: Mr Myers asks about the debriefing notes written by Dr Gibbs on July 2, 2015. He says no mention is made about the dark bile aspirates. Dr Gibbs says that is correct. Mr Myers asks if it is a consideration on the notes that could later be seen as part of legal action, and would that be something Dr Gibbs would be aware of. Dr Gibbs said the purpose of the debriefings was for the benefit of future patients, not for lawyers.
11:50am: Philip Astbury asks about hours worked by Countess staff. Dr Gibbs said the long hours worked were a "widespread problem" in the paediatric network, but the quality of care for patients was not diminished. He added: "It would be better for a consultant to be available every day to carry out comprehensive reviews." He said that was the case in most units in the UK.
11:52am: Asked about the dark bilious aspirates and the one case of vomiting, Dr Gibbs said Child C was not a cause for concern as the abdomen was soft and the other observations were normal.
12:16pm: We have had a short adjournment. The prosecution is now reading out agreed evidence statements. The first is from Dr Andrew Brunton, a specialist trainee in paediatrics at the Countess of Chester Hospital at the time of June 2015. He discussed Child C's clinical situation at birth (weighing 800g) with a consultant, who was happy for Child C to be treated at the Countess of Chester Hospital, but that situation would be kept under review. He noted inserting a UVC into Child C. He was not on duty at the time of Child C's collapse.
12:24pm: An agreed evidence statement from nurse Bernadette Butterworth is read out. She recalls seeing the UVC had come out of Child C, which was not a usual sight, and his blanket was wet. She was designated nurse for Child C for the night shifts of June 10-11 and June 11-12. On the first shift, she recalled recording readings which included rapid breathing, and the incubator temperature was reduced. Child C was 'unsettled at times', and oxygen of 'up to 37%' was required to maintain saturation levels. A further note was made to say the UVC 'continued to ooze'. The note concludes 'will discuss increasing feeds due to large urine output, continue to observe oozing'. The nurse said she noted Child C was 'unsettled' and 'poorly' at that time, and on antibiotics. Child C 'was the same at the end of the shift' as he had been when the nurse began the shift at 1am.
12:30pm: The nurse's notes from the following night are presented to the court. Child C required varying oxygen support, and continued to breathe at an increased respiratory rate. The UVC was found, at one point, to be 'out and damp', so had not been out for long. She noted the abdomen appeared distended, 'soft to firm, not hard, bowels not opened, minimal aspirates'. Child C was "unsettled at times" and required increased oxygen support after handling.
12:39pm: The nurse says, for the abdomen readings, they were 'distended but soft to firm', and nurses always check for symptoms of NEC. The distended abdomen can be a sign of the consequences of using CPAP - 'CPAP belly'. The nurse said from her notes on her night shifts, Child C had minimal, clear aspirates.
12:49pm: Dr Dewi Evans, independent medical expert, has now returned to court to give evidence in relation to Child C.
12:52pm: Nicholas Johnson KC, for the prosecution, asks Dr Evans to confirm he has made a number of reports for Child C, made between 2017 and September 2022. Dr Evans confirms that is the case. Dr Evans confirms he was sent records from Alder Hey and the Countess of Chester Hospitals, including images and records taken, after Child C had died.
12:56pm: Dr Evans says Child C was a vulnerable, pre-term baby, with restricted growth meaning he was 800g at birth. "He had two significant risk factors" that meant admission to a neonatal unit with "careful management" that would have been required of several weeks. He said Child C would have been at risk of a number of conditions during that time. The commonest risk would have been to his respiratory system, the second would have related to feeding, as premature babies are not necessarily adapted to receive milk. He would also have been at risk of NEC. The third would have related to infection. The fourth complication would have been metabolic, and it was important to maintain glucose levels and be aware of the risk of jaundice.
12:58pm: In relation to the breathing problems, Dr Evans says from the records, Child C's breathing stabilised over the days, with CPAP and oxygen support decreasing. Child C had been taken off CPAP on placed on Optiflo, which as "a very encouraging sign" that Child C could begin breathing on his own. The percentage of oxygen support had decreased from a 'common' support of 40% to 25%, the latter which was 'very low' for breathing support. "They were good markers of progress," Dr Evans says.
12:59pm: Mr Johnson says Child C also had periods of skin-to-skin contact with his mum without breathing support required. Dr Evans you "wouldn't dream of doing that" if Child C was unstable on breathing support.
2:05pm: The trial is now resuming after the court adjourned for a lunch break. Dr Dewi Evans will continue to give evidence.
2:07pm: Dr Evans continues to discuss the 'realistic risks' Child C could have faced. One was feeding; Dr Evans says all premature babies require nasogastric feeding. If the babies cannot tolerate that, then it is clinical practice to administer nutrition via TPNs, via IV. Child C was fed via the latter method, which was "the right thing to do".
2:09pm: Dr Evans said aspirates would be taken from the stomach prior to feeding. He said dark bile aspirates could be a symptom of NEC or an obstruction, but it would need to be taken in context with other signs such as the baby's abdomen condition, and the general condition of the baby - and signs of a problem would be whether the heart rate would increase, the breathing rate would increase, and/or whether the oxygen would need to be increased.
2:15pm: Dr Evans said medical staff were aware to monitor Child C's abdomen and make regular notes. He says there is one entry made in the nursing notes of 'black fluid' - not necessarily bile, but discoloured blood. That was to be 'monitored' and to 'keep an eye' on the baby's condition. It would not, in itself, be a concern. For the 'one-off' vomit reading, Dr Evans says if there was something 'serious' going on, it would happen more often than once. The four dark bile aspirate readings, each 0.5ml, are 'a tiny amount', Dr Evans tells the court. "The good news is it's only 0.5ml. The other good news is the bile aspirate is not increasing [per reading]. "That is an indication the baby is not getting worse." He said increasing readings would point to an obstruction, as would a distended abdomen. Dr Evans says Child C's status was "under control".
2:18pm: Dr Evans says Child C was well for a '30-weeker' (in terms of gestational age). A blood test for CRP had increased from 1 to 22-23 - 'not particularly high', the clinical was 'aware of this' and Child C was placed on antibiotics. Child C's platelet count had fallen - which 'on their own don't tell you very much', but in combination with an x-ray was a 'non-specific marker pointing to an infection'.
2:21pm: Blood gas readings taken were 'within acceptable values', Dr Evans tells the court, and in terms of metabolic readings, Child C was a 'stable little baby'. Dr Evans said all premature babies develop symptoms of jaundice. "The good news with [Child C] is the jaundice levels were very satisfactory". If Child C had signs of severe jaundice, he would have required phototherapy, Dr Evans explains.
2:25pm: Dr Evans says Child C had a lung infection, of pneumonia, which was "very common" in premature babies, and he was placed on antibiotics in advance of any test results.
Mr Johnson: "Did breathing issues have any direct cause for [Child C's] death?"
Dr Evans: "No."
Mr Johnson: "Did any feeding issues cause his collapse?"
Dr Evans: "No, that cannot explain his collapse either."
Mr Johnson: "Did the infection of pneumonia cause it?"
Dr Evans: "No - the infection was under control and being treated." Dr Evans explains if the pneumonia treatment was not working, a number of markers would be shown. There would be an increase in heart rate (which did not occur, he says), an increase in respiratory rate - but that stayed the same. Oxygen saturation levels stayed "absolutely where they should be", whereas in worsening pneumonia conditions those levels would fall.2:28pm: Mr Johnson: "Did the jaundice/glucose issues cause his collapse?"
Dr Evans: "None at all." Dr Evans says there were "no worrying trends" recorded in the notes. "What was the cause of [Child C's] catastrophic collapse and death?" Dr Evans says, initially, he did not have a conclusion to Child C's death. He adds one complication is if the abdomen is filled with air.
Dr Evans: "If you get a significant injection of air into the stomach, it can cause splintering of the diaphragm." As a result, a baby could collapse pretty quickly as they would suffocate. Dr Evans says that was his conclusion for Child C.2:31pm: Dr Evans says if the diaphragm is unable to move effectively, the lungs are unable to get fresh oxygen, and that causes the collapse.
2:48pm: After a short adjournment, Ben Myers KC, for Letby's defence, is now asking Dr Dewi Evans questions in relation to Child C.
2:53pm: Mr Myers says Dr Evans has had the case material for Child C for about four and a half years, and has provided such conclusions. "Before today, you have never suggested that [the collapse on] June 13, the splintering of the diaphragm, is the cause of the death, have you?"
"That is correct." Mr Myers suggests that Dr Evans's opinion alone would not have reached this conclusion. Dr Evans said the death could not be explained from the usual causes babies get. He said, taking into account all the other evidence and information from experienced medical people's reports, and reading the pathology report, the splintering of the diaphragm was now his conclusion. He said he was functioning as a clinician. "The fact is this baby has collapsed having previously been stable, and one has to explain that." Mr Myers suggests Dr Evans had been influenced into supporting this conclusion. He says Dr Evans had not provided this 'splintering of the diaphragm' conclusion in his eight previous reports.2:54pm: Dr Evans says while Child C was at 'constant' risk of a number of conditions, he was under continual observation and was in a neonatal unit. He confirms his initial conclusion from 2017 was 'one may never identify the cause of his collapse'.
2:58pm: Mr Myers said Dr Evans 'could not rule out infection' in his 2017 conclusion. Dr Evans said infection was "a factor" in Child C's short life. "It is possible to suggest that...his pneumonia was under control, he was requiring hardly any oxygen. It was my role, investigating this unexpected collapse, to give an impartial view of all the issues. I don't prepare partisan reports." He says infection was a part of Child C's status. He adds it did not cause Child C's death.
3:04pm: Dr Evans tells the court the process in accumulating information in reaching his conclusions. He says while Child C had an infection, he was recovering from it, as he had gone off CPAP support, on to Optiflo. "Respiratory wise, he didn't stay the same, he was improving." Mr Myers says up until the evidence of today, he had not provided in his reports an allegation of harm.
Mr Myers: "You are coming up with things to support an allegation of harm."
Dr Evans: "I am coming up with clinical evidence." Dr Evans says he has read varying reports, but had not read a single medical report that said "I'm wrong, [Child C] died of something else." Dr Evans says this case "will always be a challenging case" for any clinician as it is difficult to separate the pathological problems from an event where Child C "was placed in harm's way by some kind of deliberate act."3:09pm:
Dr Evans: "You can't exclude infection from [Child C]'s general status. "He's got an infection, but it's under control." Mr Myers refers to another of Dr Evans's reports, from 2019, referring to infection being 'probable' as a significant cause in Child C's collapse. Dr Evans says if he receives additional evidence, then he will change his mind. Mr Myers says Dr Evans has not received any new evidence on Child C's infection since.3:17pm: Mr Myers says the 2019 report said Dr Evans raised a possibility of deliberate injection of air from June 12 via the nasogastric tube. Dr Evans, reflecting on that report, said: "Can't rule it out". Mr Myers refers to a 'massive gastric dilation' was 'most likely' due to an injection of air on June 12.
Dr Evans: "That was a possibility, yes." Mr Myers says in that report, there was no suggestion the diaphragm had been splintered since, and if he wanted to say so in that report, he could have done so. "If it wasn't said, it wasn't said." Dr Evans said what was being discussed, on June 12, there was a "distinct possibility" Child C had excess air in the stomach from CPAP belly. He was "still stable" from a respiratory point of view. He tell the court: "However the air went in, it would have been insufficient to splinter the diaphragm on the 12th, as he would've collapsed and died on the 12th." The air which had gone in was 'insufficient' to cause a collapse. There was 'nothing to suggest' the excess air was enough on June 12. He says the two events on June 12 and 13 "are quite different" in the way they happened. Mr Myers said that it was Dr Evans's view, a couple of months ago, there was deliberate harm on June 12. "That was a possibility, yes it was."3:19pm:
Mr Myers: "What you have done today in your evidence is introduce something supporting the allegation."
Dr Evans: "That is incorrect." He adds that in coming to his conclusion for this case he is not relying solely on his opinions, but taking in other clinical evidence and reports. "That is what doctors do, we do it all the time." in what Dr Evans says is a "complicated case".3:28pm: Mr Myers has gone back to the case of Child B to discuss the legibility of a nursing note concerning blotchiness of Child B's skin. The discussion goes on for several minutes. Dr Evans adds: "This is just making a meal out of something."
Mr Myers: "You're not independent, as a witness, are you, Dr Evans?"
Dr Evans: "I am completely independent. I am not here for the prosecution, I am not here for the defence, I am here...to assist the jury." The judge interjects to clarify the meaning of the note, before the case resumes on Child C.3:31pm: Mr Myers asks about the bile aspirates, and asks if the dark colour was additional concern. Dr Evans says it could be discoloured blood, and the presence of vomit once would be a concern, but would need to be put in context of the baby's condition. "You can't choose out something that supports your case - you need to look at the big picture."
3:38pm: Mr Myers says the x-ray from June 12 had helped form Dr Evans's initial view that there had been an air injection into the stomach. "That was an opinion I have expressed, yes." Mr Myers asks Dr Evans what evidence there is to support that air had been injected into the stomach on June 13.
Dr Evans: "The baby collapsed and died." Asked to explain further, Dr Evans says it was part of a differential diagnosis. He said there were three clinical scenarios - injecting air into the stomach that interfered with his breathing, or that air was injected intravenously, or from a combination of the two, which Dr Evans says "sounds awful". Dr Evans says, from his perspective, from an academic point of view, he would not be able to rule out any one of those three scenarios.3:42pm: Dr Evans says none of the normal processes described why a baby collapsed. He adds, for further medical information, he would prefer to defer the matter to the radiologist and pathologist. He said he objects to being accused by Mr Myers of making things up, and says he is putting forward the information in this case as a result of his own opinion and that of other people's reports.
3:46pm: Mr Myers says 'never once' is an air embolus mentioned in Dr Evans's reports. Dr Evans agrees. Mr Myers suggests that Dr Evans has just made up information as he has gone along. "You keep saying that, and I keep disagreeing."
"And you're not an independent witness at all, are you?"
"And again, that is just being insulting."3:50pm: Independent medical expert Dr Sandie Bohin has returned to court to give evidence, this time for Child C.
3:52pm: Dr Bohin confirms, after being asked by Mr Johnson, she has received and reviewed all the case evidence, including from doctors' witness statements.
3:55pm: Dr Bohin says her role was not to 'rubber-stamp' anything, but to come to her own conclusions and see whether they agreed with that of Dr Evans. She said she set out what she thought were the important facts for Child C. They include an x-ray taken on June 12 following the insertion of a long line. She noted the long line was in a "low position", but in a "usable position". The stomach looked swollen and had a distended bowel. She said initially she could not see a nasogastric tube on the x-ray image on her laptop, but from viewing the x-ray image shown in court in higher resolution, she could detect it was present, 'very high', in 'not an ideal position'.
4:01pm: Dr Bohin is asked about her conclusions regarding Child C. She said it was known Child C was premature, growth restricted at birth, and 'potentially at risk of complications', but 'managed very well indeed' in his early days, improving to being put on Optiflo. He had 'clearly not liked' being on CPAP, and had been put on skin-to-skin contact with his parents, without CPAP for a couple of hours, and had done well during those times. "This was not a baby who was ill, this was a baby who was improving." Dr Bohin noted Child C "clearly" had an infection, which was "an alerting feature" and for which the medical team treated him with antibiotics and did an x-ray confirming left lung pneumonia. Despite that, Child C had appeared to respond to treatment due to the lessening of respiratory support.
4:03pm: Dr Bohin said it was "very clear" Child C had pneumonia, but a baby with pneumonia will "often survive", but a sign of that will be that they would slowly deteriorate, going from CPAP to ventilator support, increased heart and breathing rate. Child C's breathing rate was "very stable", despite "effectively breathing with one lung". Dr Bohin's conclusion was that he had pneumonia, but that did not cause the collapse or kill him.
4:04pm: Dr Bohin said pneumonia would be a factor in the difficulties in response to resuscitation. She tells the court there would be a sign something was "amiss" prior to the collapse, and a sudden unexpected collapse would be uncommon in babies.
4:09pm: Dr Bohin says babies on CPAP can have CPAP belly, and in order to minimise that, they would aspirate the NGT. "It is usual practice to note down the volumes of air aspirated to give colleagues an idea [of how much air is coming out of the baby]."
"I couldn't find any evidence of that [in the notes]." She adds that, for babies not fed, the nursing staff would put the tube on free drainage so air could come out on its own, as well as actively aspirate every four hours or so. She says there was only 'fleeting mention' of free drainage. If neither of those things happen, Dr Bohin said that would lead to gas accumulation in the stomach.4:11pm: Dr Bohin said it was not clear from the notes how long the 'free drainage' was in place. She said one conclusion for Child C's collapse was CPAP accumulation of air, the other being deliberate injection of air. She said the doctors did not appear to have a concern as they had noted the abdomen to be "soft".
4:14pm: Dr Bohin said Child C died "with his pneumonia, not because of his pneumonia." She added babies such as Child C do not collapse suddenly and without warning. She said an infection would not be the cause as that would lead to a gradual deterioration in the baby, not a sudden collapse and no response to resuscitation.
Wednesday 2nd November 2022
Child C
Dr Sandie Bohin - Summary of police interviewsChester Standard article 2-11-2022
A NURSE accused of multiple baby murders at the Countess of Chester Hospital told police she found it "quite hard" when one of her alleged victims lived for several hours after his catastrophic collapse.
The newborn boy stopped breathing without warning just days after his premature birth, weighing just 800 grammes, at the hospital's neonatal unit in June 2015.
The infant, referred to as child C, is one of seven babies allegedly killed by the 32-year-old who is also said to have attempted to murder 10 others.
Letby, who denies the charges, is said to have caused the collapse of child C at about 11.15pm on June 13 by inserting air into the boy's stomach via a nasogastric tube.
Jurors at Manchester Crown Court have heard medics failed to revive him and that "token resuscitation" took place until the arrival of a Church of England vicar to baptise the boy and a Catholic priest to perform a blessing.
However, signs of life reappeared during the wait for the ministers with "occasional gasps of breathing" and "feeble heart beats" noted as the parents cuddled their son.
An on-call consultant could not explain the "fairly minimal" signs of life but explained to child C's parents the chance of him recovering was "remote" and the prospect of him not suffering profound brain damage was "extremely remote".
Palliative care was provided and no further gasps or heartbeat were heard some five hours after the christening and child C was pronounced dead at 5.58am on June 14, the court heard.
When interviewed about child C, the defendant said she remembered him because he was a small baby.
Letby recalled he deteriorated not long after his first feed by one of the nurses but said she had no involvement in that.
Her only involvement with child C was when she was asked to help with the resuscitation attempt, she told police.
She added she had a "vague recollection" of taking child C's hand and foot prints for a memory box while the infant was sat with his parents but "couldn't be certain".
Letby went on to say she found the boy's death "quite hard because he lived several hours (after the collapse)" and she had "not seen that before".
Detectives also asked her about a conversation in which a nurse was said to have asked child C's parents if they wanted him to be taken away in a ventilator basket while he was still alive.
She replied she had no recollection of making that comment and questioned whether the parents had said she was the nurse who said that, the court heard.
She said it was "very sad" for the parents.
Letby, originally from Hereford, denies administering air to child C.
She accepted she made Facebook searches for his parents about 10 hours after their son died but could not remember doing the searches or why.
The court has previously heard Letby messaged a colleague during the night-shift of June 13 that it was "eating her up" she was not allocated to work in the intensive care unit (ICU) room just days after the fatal collapse of another baby.
Letby told police she agreed she wanted to go the room "as it can be hard to go back into an ICU environment after having a sick baby so she preferred to go straight back in".
Giving evidence, expert medical witness Dr Sandie Bohin said Child C was "potentially at risk of complications" after birth.
But she told the court: "Actually, in his early days he managed very well indeed. A couple of times he had skin-to-skin contact with his parents and that is something you would not do if you had concerns.
"He was not only doing well but was actually improving. This was not a baby who was ill."
She agreed Child C developed pneumonia but said he received the standard treatment of antibiotics.
Dr Bohin said: "My conclusion was, yes, he had pneumonia, but that was not what caused him to collapse.
"I think the pneumonia contributed to not surviving the resuscitation."
Asked to explain a build-up of gas in Child C's abdomen detected on a X-ray on June 12 – the day before his fatal collapse – Dr Bohin said air could have accumulated via respiratory support he was receiving. The alternative explanation is a deliberate introduction of air down a fitted nasogastric tube, she said.
Prosecutor Nick Johnson KC asked: "When you looked for a reason for (Child C's) collapse on June 13, can you find an explanation?"
Dr Bohin replied: "No. Babies like this should not collapse. You get prior warning that something is amiss.
"They don't go from being stable into a cardiorespiratory situation within minutes. They rarely collapse in this way but they are usually responsive to resuscitation and he was not."
Mr Johnson said: "In your view, did the infection that (Child C) had, was that the cause of his catastrophic collapse?"
Dr Bohin said: "I think he died with his pneumonia, not because of his pneumonia."
Ben Myers KC, defending, noted Child C's markers for infection rose in the last 24 hours of his life.
His blood platelet count fell below acceptable levels, his weight was low and he had not been fed, he said.
Notes were also recorded of dark bile being produced and an incident of vomit with bile, he added.
Mr Myers asked: "If you put things together they might be a matter for concern?"
Dr Bohin said: "I say there was not."
Mr Myers said: "It's not a question of you minimising the seriousness of (Child C's) condition, is it?"
"Absolutely not," said Dr Bohin.
Mr Myers previously told the jury Child C was vulnerable, especially to infection, and should have been at a specialist children's hospital rather than the Countess of Chester.
Thursday 3rd November 2022
Child D
Family statements - Police analyst: Recorded events & messagesChester Standard Live Reporting
9:40am: In the past week, members of the jury have been hearing evidence in relation to the fatal collapse of Child C at the neonatal unit in the Countess of Chester Hospital. It is expected that today the case will turn to the fatal collapse of Child D in June 2015. The prosecution say that Lucy Letby, as in the case of Child A, B and C, administered a fatal air injection. The defence deny this.
9:45am: During the prosecution opening statement, the jury has heard Child D, a baby girl, died following three collapses in the early hours of June 22, 2015. As has been the case for the other children in the case so far, the court will hear evidence of the circumstances which happened in the days leading up to Child D's collapse.
10:10am: As ever, the case is being heard in Manchester Crown Court, in front of a jury of eight women and four men, and the trial is expected to last six months. This is the fourth week of the trial being heard before a jury.
10:15am: The trial is expected to resume at 10.30am.
10:36am: Members of the jury are arriving in court now.
10:37am: Child D's mother is now being called to give evidence.
10:38am: A reminder that the family members of any children involved in the case cannot be identified, due to reporting restrictions.
10:43am: The prosecution, led by Nicholas Johnson KC, ask Child D's mother to confirm details. Child D's mother tells the court she developed a concern about her waters breaking, which the court hears was "well founded" as her waters broke when she woke up on June 18. The hospital told her to "monitor the situation". She waited, and rang the hospital again, and was then told to go to hospital. At 11.30am, she arrived at hospital, and staff confirmed her waters had broken, but did not test. They then checked her and her baby, "not for very long".
10:45am: "Were you, in effect, sent home after being examined?"
"Yes." The following day, the mother returned to the hospital, and saw a midwife. "Were you examined and various checks performed on you?"
"Yes...not straight away. I had to wait."
"Did you express concern to staff at the Countess." The mum said her waters had broken over 24 hours before, she didn't "feel right" and the baby "didn't seem to move as well" and she was concerned about infection as she hadn't been given any antibiotics.10:46am: The decision was then taken to induce. She said staff were "very busy", and she was not placed on an IV but not for "many hours". It was "very delayed", the mother tells the court.
10:47am: The mother said she was "very worried and scared", "unwell" and "not in control" and "forgotten by the staff", as it was nearly 48 hours after her waters had broken. On a trip to the bathroom, she noted blood had come out. She asked someone to do something.
10:49am: She said she remembered seeing a doctor, and recalled a description for her. It was the first time she had seen a doctor since her admission. She was told that essentially both her and her baby girl were ok, and that a natural birth would be considered, and that would be reviewed 4 hours later at 11am.
10:53am: At 11am, the mother was assessed again, by a different doctor. She recalls a description for the male doctor. She was told there had been "little progress" and she said he was the "first professional who spoke to me and addressed my concerns". The mother said it had been about 50 hours since the waters had broken and a C-section was considered, as there had been no dilation. The mother was informed a natural birth would be the preferred option to a C-section. By 3pm, the mother had discussed the situation with her husband and concluded she would be 'less patient' and call for a C-section if there had been no progress.
10:55am: At 3pm, the mother was reviewed by the same male doctor, and he was "more concerned" about the situation, as she appeared more tense. The doctor then confirmed she would receive a C-section as he said it was "not a good idea to wait any longer" as the baby appeared 'distressed'. Events then moved on "a lot more quickly" after staff had initially appeared "chilled". After the C-section decision was made, matters "moved a lot more quickly".
10:57am: Child D was delivered and lifted over the screen for the mother to see. The mother recalls seeing "no life - lifeless - she did not scream, everything was quiet in the room." Mr Johnson asks if there was a nurse in the theatre room at this stage. The mother does not recall. The mother was taken to a ward, while medical professionals dealt with Child D.
10:59am: The mother recalls seeing Child D very briefly, in the operating theatre, before they [the staff] took her away as they had "concerns". The mother said she was "very aware" of things going on, despite having received anaesthetic. She did not have physical contact with Child D, but her husband did. The mother was taken to a ward.
11:03am: The mother was taken to a further room, and it was there where she had physical contact with Child D. Her impression of Child D condition at that point was "really worried as she [was brought to my chest] but she didn't have any movement, she looked limp and pale - struggled to breathe and was making a groaning noise. "She wasn't really responsive. There was a split-second where she opened her eyes and looked at me, and then no response. "I tried to breastfeed her, but she was completely limp, so I was worried." A male paediatrician informed the mother 'not to worry' as the delivery had been through C-section so the breathing wasn't as clear. The mother said she didn't believe what he said. His attitude seemed "too careless".
11:04am: The mother said she thought something was wrong with Child D and one of the midwives would assess her in 'a couple of hours'. She said she did not want to wait that long and wanted another doctor's opinion. The same doctor came back, but he had spoken to a consultant. The mother said she was "not reassured" but "was glad someone took me seriously". She was then worried as Child D was taken straight to neonatal unit intensive care.
11:06am: The mother said she felt "rubbish...drained" and didn't feel any relief. She was "in pain" and "knackered". The mother said it was around 7-8pm when she was separated from Child D.
11:08am: The following day was Father's Day. The mother was given news that Child D had been "up and down" all night, struggling with feeding, and staff "didn't seem too concerned then", but Child D "wasn't great". The mother believed she had been spoken to by a female consultant doctor that morning.
11:10am: The mother said she recalled Child D needed to be on a CPAP machine and every time they tried to take her off she would crash. She said staff did not seem overly concerned as Child D was a good-size baby and making progress, despite being 'poorly'. Other tests showed she seemed 'fine'. The mother said she was able to see Child D at about 7pm that day.
11:14am: The mother said she had spoken to a doctor before heading to the neonatal unit. A drawing that the mother had made, showing a plan of the neonatal unit room, is shown to the court, showing the positioning of Child D's cot, other cots, and crosses identifying a number of medical machinery.
11:16am: Child D's mother said she had spoken to Dr Andrew Brunton at 9-9.30pm, and was told he was "very happy" with Child D's test results. They had "done more scans" and she was "well" and promised her she would be able to hold and cuddle her the following day. The mother said she was not in a good condition herself, being moved in a wheelchair and '10/10 pain', on morphine, but was happy with Child D. Child D looked like "a good pink baby", "tiny but chubby", and looked "healthy".
11:18am: The next time she saw Dr Brunton was the following night. She and her husband were woken up 'about 4am' by a nurse to 'come quickly' as Child D was poorly. They "rushed downstairs" and Dr Brunton was "holding her" and trying "really hard" to resuscitate her.
11:19am: "We were just standing there looking at [Child D] dying." The doctor was "quite agitated" and the couple heard they "had to let [Child D] go." The mother said she could not stay there anymore and asked to be taken away.
11:22am: A nurse, who the mother believed to be Lucy Letby, was holding a phone to Dr Brunton's ear, she recalled. The mother said she had seen Lucy Letby before, when she went to see Child D in the neonatal unit at about 7pm. The mother recalls as she was wheeled into the room, Lucy Letby was "hovering around, not doing much" with Child D, and had a clipboard, and was looking at the machinery. "I didn't understand what she was doing", and the mother asked if Child D was fine, to which Lucy Letby said she was. Lucy Letby "just stuck around" and was "just watching, looking over us". The mother said she asked for Lucy Letby to "just go away and leave us [in privacy]."
11:25am: Mr Johnson asks if Lucy Letby was in the neonatal unit room at the time Child D died. The mother agrees, and says other doctors were in that room. The mother says she did not stay in that room. The mother recalls she was taken to a private room, where Child D was, along with her husband and another family member, and a nurse she had not seen before. The mother said she did not see Lucy Letby again. Ben Myers KC, for the defence, is now asking the mother questions.
11:28am: Mr Myers says it is an "awful experience" what the mother went through, and says he has one or two questions to ask. He asks about the 7pm neonatal unit visit on June 21. The mother says she went there with her husband. She recalls 7pm as she 'must have looked at the clock'. She said there was "an exchange of few words" between her and Lucy Letby. Mr Myers asks if that was possibly another nurse. The mother replies: "I don't think so." The judge, Mr Justice Goss, asks for clarification. The mother said she would not have known the name of Lucy Letby at the time, but would after seeing her picture after she had been arrested.
11:31am: The court is now hearing an agreed evidence statement from the father of Child D. The court hears, from the statement, Child D died at 4.25am on Monday, June 22. He said he does not remember any specific problems from the mother's pregnancy, but had "immediate concerns" when she was born, as she "appeared grey" and was not crying. "Initially, we were reassured by the staff" - and he said he believed them, and never thought Child D would die in the circumstances she did.
11:34am: The father recalls the circumstances leading up to the birth, as recalled by the mother. He recalled the mother did not respond to inducement measures, and had mild contractions between 2am-3am on June 20, but had not dilated. She was "encouraged to wait" for inducement methods, but she "did not want to" as she had been in labour for some time. They were told medical staff were "monitoring the situation" and were told antibiotics were "not necessary" at this stage. They said they agreed on a C-section, and at about 4pm, the mother went for an emergency C-section.
11:39am: Child D was held above the sheet, momentarily, and wrapped up, taken to the scales. "We weren't informed of any issues" - "I was led to believe everything was ok". He said Child D was very quiet, which was unexpected, and held her in his arms. He said he was not sure if Child D was given any breathing support at this stage. He went back to the ward with Child D for a brief time, and he and the mother put pyjamas on her. However "she didn't seem interested in feeding at all". They said they were told Child D was doing well. "We repeatedly asked if she was ok. We just weren't comfortable with how she was." Medical staff kept telling her Child D was ok. A few hours later, a different paediatrician came and Child D was taken to the neonatal unit. The parents were later told Child D was not well. "It was a bit of a shock" when the father saw Child D in the neonatal unit, as she was "very poorly...wasn't feeding...and had lots of tubes in her mouth". Nursing staff "always made" the father feel welcome when he arrived.
11:41am: On June 21, the father went to see Child D and was "almost certain" he saw she had been taken off CPAP. He said he frequently visited the neonatal unit, and asked staff "It was Father's Day, and I was given a handmade father's Day card. "The staff had put it together, and it had a message from [Child D] - with a photo stuck inside. "On the first photo, she has CPAP. I took that with me. "Later that day, I was given a welcome card, and a photo which showed her looking better, and not on CPAP."
11:46am: In the early hours of June 22, he was woken by a nurse and to go to the neonatal unit as Child D was "poorly", and they were taken there quickly. "When we walked in, we understood immediately it was a very serious situation. "Andrew, the senior doctor, seemed to be in charge. "I remember someone mentioning adrenaline, and there was a sense of urgency. "Andrew had a phone held up to him, and he was discussing the situation with someone on the other end. "There seemed to be some confusion over what baby they were talking about. "The person on the other end seemed to be referring to a different child. "They were unsuccessful in resuscitating [Child D]. they said they had been trying to resuscitate [Child D] for over 20 minutes. "I couldn't tell you which staff were in...as I wasn't paying much attention. I didn't want to look." He added the parents weren't in the room for too long, about five minutes. He said he does not recall seeing Lucy Letby at this time. He went back to the ward and informed another family member of the news.
11:47am: A statement from another family member of Child D is read out to the court. They said they had visited Child D in the neonatal unit: "It didn't even cross my mind that she was in danger of dying. "When she died, we just weren't prepared for it. "Nothing I saw appeared out of the ordinary...but I didn't have anything to compare their actions to."
12:05pm: The court has had a short adjournment. It will next hear, from the prosecution, the sequence of events. As has been the case for Child A, Child B and Child C, the evidence has been presented to the jury electronically on iPads.
12:06pm: Intelligence analyst Kate Tyndall has returned to give evidence and give a walkthrough to the jury on the evidence 'tiles' in the electronic bundle.
12:10pm: The first evidence shown to the court is Lucy Letby's shift patterns for June 2015. It shows which days Letby was on 'long day' shifts, and 'night' shifts. She worked long day shifts on June 2, 4, 17, 19, 27 and 28. She worked night shifts on June 8, 9, 13, 14, 21, 22 and 23. Child A died on the night of June 8-9, and Child B had a non-fatal collapse on June 9-10. Child C died on the night of June 13-14. Child D died on the night of June 21-22.
12:12pm: The evidence shown to the court shows Child D was born at 4.01pm on June 20, weighing 3.13kg [6lb 14oz], and required breathing support at birth. The Apgar scores were 8 [out of 10] at 1 minute after birth, and 9 at 5 minutes.
12:14pm: Child D was admitted to the neonatal unit at 7.30pm on June 20 'for respiratory support requiring ventilation'. Child D was 'grunting' and her colour was 'dusky', it was observed.
12:21pm: Child D was placed on CPAP, with 40% oxygen support, and placed on 'double phototherapy'. Doctor Ahmed Chowdhury noted discussing Child D with the parents, saying 'on moving baby to labour ward baby became blue/dusky. Sats 47% on arrival NNU - had bagging, sats picked up. Given antibiotics, baby put on CPAP. Not explained to parents yet'.
12:24pm: Notes record the administration of antibiotics and sodium chloride to Child D. The court hears phototherapy was carried out to treat Child D's jaundice.
12:31pm: Child D was administered with an endotracheal tube on the second attempt. The nursing notes record Child D was 'starting to out a few breaths in for herself now'.
12:33pm: An x-ray reading for Child D showed 'shadowing consistent with transient tachypnoea of the newborn [TTN, a respiratory disorder]'.
12:34pm: A nurse's note recorded meeting the father, who had visited the neonatal unit, and it was explained to him that Child D would be on the neonatal unit for "at least 48 hours", and the dad was "visibly upset", so "lots of reassurance" was given to him.
12:42pm: A further nursing note at 4.30am on June 21 showed Child D was making 'good respiratory effort', and blood gas readings were 'good', so ventilation support was reduced.
12:45pm: Another nursing note at 7.21am recalls the father's visit to the neonatal unit. It includes: "[Father] appeared overwhelmed so lots of reassurance given."
12:53pm: A note from nurse Kate Bissell reads, at 9am on June 21, that Child D was 'extubated...following satisfactory blood gas'. Child D was 'initially apnoeic and required stimulation...via Neopuff/CPAP', but the breathing became more regular after a couple of minutes. Kate Bissell, in a subsequent nursing note, said a blood gas reading at 10.15am was subsequently taken and the results showed signs of respiratory acidosis, so Child D was put back on CPAP. The blood gas was repeated two hours later and 'showed further deterioration with increasing metabolic acidosis'. Child D's perfusion was 'poor' and a doctor approved a decision to administer medication. Dr Ahmed Chowdhury recorded a UVC and a UAC were inserted.
2:08pm: The trial is now resuming.
2:10pm: The court is continuing to go through the sequence of events, which is up to the afternoon of Sunday, June 21, 2015.
2:13pm: A 'family communication' note is made at 5.53pm - "Dad visiting most of the day, he is up to date with the plan of care. Mum has visited this evening." Both parents were 'anxious' about the levels of care provided.
2:18pm: A nursing note at 7.15pm said attempts were made to get Child D off CPAP, but breathing was still 'shallow' off that, so CPAP resumed. Swipe data showed Lucy Letby arrived at the neonatal unit at 7.26pm. The handover note showed Letby was one of the nurses on duty that night, with a different nurse being the designated nurse for Child D, in room 1. Letby was the designated nurse for two other babies in room 1.
2:19pm: At this time, another nurse was looking after Child B in room 3 for that night. The court had previously heard Child B had suffered a non-fatal collapse earlier that month.
2:28pm: Further observations for Child D are documented throughout that night shift, until after 1am.
2:31pm: A neonatal infusion prescription chart at 1.25am, for Child D, is shown to the court. Lucy Letby is one of the two nurses to provide a signature for a saline dose prescription at that time.
2:32pm: Child D then first collapsed at 1.30am.
Mr Johnson: "This is within a very short time of the document with Lucy Letby's signature on, isn't it?" Kate Tyndall: "Yes."2:34pm: A nursing note, timestamped for 1.30am but written retrospectively, recalls: "Called to nursery ward...[Child D] had desaturated to 70s, required oral suction as was bubbly and had lost colour. Discolourations to skin observed, trunk/legs/arm/chin."
2:39pm: Notes of medication are made. At 2.40am, a neonatal infusion prescription chart is recorded for a sodium chloride dose with 10% dextrose. Letby is one of the two nurses signing for it.
2:41pm: The medication administration update is made on the computer at 2.44am. At 3am, Child D collapsed for the second time. The nursing note recorded for 3am: '[Child D] crying and desaturated again to 70s, commenced on 100% O2 via CPAP and picked up well but skin discoloured again..."
2:44pm: At 3.20am, a further neonatal infusion prescription is made, with Lucy Letby being one of the signatories. At 3.45am, Child D collapses for the third and final time. The nursing note recalled the alarm went off and Child D 'desaturated and then became apnoeic. Called Letby...' Resuscitation efforts began but to 'no effect'. A bleep alarm went off and doctors were called to the neonatal unit.
2:47pm: The court is shown a number of clinical notes are made by doctors for this time. These clinical notes will be discussed further when the doctors involved in them come to court to give evidence in the coming days. They include the resuscitation efforts, administration of adrenaline doses and the decision, ultimately, to discontinue CPR. Child D died at 4.25am.
3:11pm: A text message sent from Lucy Letby to a colleague said, at 8.36am: "We had such a rubbish night. "Our job is just far too sad sometimes."
The colleague replied: "No what happened?"
Letby: "We lost [Child D]."
The colleague: "What!!!! But she was improving. What happened? "Wanna chat? I can't believe you were on again. You are having such a tough time."3:15pm: Letby refers to Child D being "messed about a couple of times" and refers to a rash that "looked like overwhelming sepsis". She adds that two members of staff said the circumstances "would be investigated". The colleague replies: "Dad was very anxious all day." and adds, in relation to the investigation, "What the delay in treatment?"
Letby replies: "Just overall looking into the case. "And reviewing what antibiotics she was on if sepsis."3:31pm: The colleague says Child D "was behaving septic". She adds, to Letby: "Oh hun, you need a break." Letby said, in her response: "But it's part of the job and it's hard for everyone." The colleague responds: "Yes but you have had it all recently." Letby, in her response, says: "Hmm well it's happened and that is it, got to carry on..." before referring to her planned time off. The conversation then discusses staffing arrangements, and the difficulties of the job, before noting an instance of a happier occasion on the unit. Letby says: "How do such sick babies get through and others get to [die] so unexpectedly?" Her colleague, in her response, says: "We just don't have magic wands..." The colleague refers to what Child D looked like in their care.
Letby replies: "I think there is an element of fate involved. There is a reason for everything."3:38pm: The colleague adds: "It's important to remember that a death is not a failure," and says Letby is "an excellent nurse." Letby, in her response, accepts the need to take positives from the job, but it's "just so sad to watch what families go through."
4:13pm: A nursing note by Yvonne Farmer recorded that Child D was blessed by a reverend with the family present, with hand and footprints obtained. The note added: "Parents had lots of cuddles and said goodbye to [Child D]." The parents were also given a bereavement box with mementoes and information on the Sands charity.
4:20pm: Further messages are exchanged between Letby and her colleague the following evening. The colleague asks: "How you doing?"
Letby replies: "I'm ok - trying not to think about it. Work busy but at least we have 6 tonight." The colleague enquires about Child D and whether anything had been said about not "bringing her through sooner on Saturday".
Letby replies: "I don't think so", before adding there was a theory Child D may have had meningitis. The colleague responds: "I'm worried I missed something."
Letby: "I don't think any of us did and she [Child D] was on the right antibiotics."4:24pm: The colleague replies: "Yeah, just would treatment sooner have made a difference." Letby asks her colleague if Child D had a lumbar puncture. The colleague replies she was not sure it ever got done, given that the baby girl was ill and had been on CPAP. She adds her gas reading was "appalling" when she first came through to the unit.
4:25pm: Letby, in her response, says: "I think we did what we could." She then refers to the condition of the mother of Child D. The court hears at 9.51pm on June 25, Letby searched for both the parents' names of Child D on Facebook.
4:36pm: Towards the end of June, Letby sent a message to a colleague: "Work has been awful." The colleague responds: "Oh dear. Staffing probe?" Letby, in her response, says: "We have had three unexpected deaths," adding the unit is "full". She adds: "What I have seen has really hit me tonight." The colleague asks: "Have you worked today?"
Letby: "No, been off since Wednesday morning and now it has all hit me." The colleague asks if Letby tries "talking to a proper counsellor". Letby replies that she does not think she can. The colleague: "Why not?"
Letby: "I can't talk about it now...I can't stop crying...I just need to get it out of my system." The colleague advises Letby to think carefully what to do, before adding: "Maybe you need to take time off."
Letby: "Work is always my priority," adding she had not cried about the incidents until then.
Friday 4th November 2022
Child D
Police Analyst: Recorded events & charts - Nurse Caroline OakleyChester Standard Live Reporting
10:35am: The trial is now resuming, with intelligence analyst Claire Hocknell returning to provide a walkthrough for the jury on neonatal unit evidence.
10:46am: The chart being shown to the court is the neonatal review schedule, showing when electronic records are made, including e-prescriptions, with Lucy Letby's name highlighted on the chart. Nicholas Johnson KC, for the prosecution, highlights the three 'infusion started' notes, each one of them happening before Child D's collapses. Lucy Letby and Caroline Oakley are the two nurses to sign for the medication and administering the infusion.
10:48am: The neonatal unit review chart also shows a long list of clinical notes made following the final collapse, made by doctors, regarding the efforts to try and save Child D's life, before ultimately the decision is made to discontinue resuscitation efforts and record the time of death at 4.25am on June 22, 2015.
10:58am: Ben Myers KC, for Letby's defence, asks about a note which said Letby administered to a baby 'whose location is unconfirmed [as recorded on a map of the neonatal unit for that night]' on the night of June 21. Letby was a designated nurse for that baby, and two babies in room 1, that night. Mr Myers asks about Lucy Letby and Caroline Oakley administering medication to a number of different of babies that night. Claire Hocknell confirms the records.
11:00am: Mr Johnson asks to clarify the map which includes the detail about the baby 'whose location is unconfirmed' - he tells the court Letby was initially the designated nurse for that baby until 10.45pm that night on June 21, and then care was passed to a different nurse.
11:17am: Caroline Oakley is now being called to give evidence. In June 2015, she was employed as a senior neonatal unit nurse at the Countess of Chester Hospital. Mrs Oakley confirms she would at times be a shift leader, and would look after the people on that shift, not necessarily working with managers.
11:18am: She confirms she had direct involvement with Child D on the night shift from June 21-22, and was her designated nurse during that shift.
11:25am: Mrs Oakley says she does not recall which nurses were designated nurses for which babies that night. Her nursing note, written retrospectively at 4.46am on June 22 for the night shift, is presented to the court. The note records, at the handover, 'lower limbs dusky and feet bruised. Doctors aware. Feet cool to slightly warm. Observations satisfactory.' Mrs Oakley added Child D was 'nursed on CPAP in air. antibiotics given as prescribed.'
11:26am: Mrs Oakley tells the court Child D was not pink yet, and might have been sampled with heel pricks, which could make the feet bruised. She said it was something to monitor, but was not a concern at that stage, and those observations had been relayed to doctors.
11:28am: The nurse said Child D's circulation was not "100 per cent brilliant" at that point, but this was common in newborn babies. The note records Child D was reviewed by Dr Andrew Brunton. The decision was made to 'commence feeds and increase as tolerated', with expressed breast milk. Blood gas readings taken at 11.52pm and 1.14am were 'satisfactory'.
11:31am: Mrs Oakley said she remembered "being very happy with her" at that point of the night shift. While Child D was an intensive care patient in the neonatal unit, she was 'only requiring a little assistance' with breathing, and she was "stable".
11:35am: The observation chart for Child D for that night shift is shown to the court, which shows Caroline Oakley's initials signing hourly observation readings. The heart rate, respiration rate and temperature are recorded. Child D's heart rate says for the first few hours, the heart rate was "completely normal" up to 12.30am. It had peaked at 1.15am, but could have been after handling and/or a nappy change, Mrs Oakley tells the court. She said that reading was "still within normal parameters".
11:36am: The respiration rate was at the "upper end of what would be considered ideal", but was still within normal parameters, Mrs Oakley adds. The temperature readings are also "completely normal" with "no high temperature".
11:43am: A further observation chart records the readings made for Child D being on CPAP. The chart recorded Child D did not require oxygen support at this stage, having been taken off that in the early hours of June 21. The oxygen saturation levels were '100', which meant Child D was "breathing beautifully".
11:51am: Another intensive care chart is shown to the court, showing fluids administered during the evening and night of June 21. A 'minimal' amount of 'acidic' aspirates is recorded from the stomach in the evening. It was followed by 'mostly clear' aspirates, with occasional darker bits. Mrs Oakley says there was "nothing" she was "worried about" from those readings.
11:54am: The neonatal infusion prescription chart at 1.25am is shown to the court. It is signed by Caroline Oakley and Lucy Letby. Mrs Oakley says usually the nurse looking after the baby will administer it. She confirms the two signatures made, showing they had checked the fluid. Mrs Oakley adds: "I would presume that I connected the fluid".
11:58am: At 1.30am, nurse Oakley's notes record: 'called to nursery by senior nurse...and senior nurse Letby; [Child D] had desaturated to 70s, required oral suction as was bubbly and had lost colour. Discolourations to skin observed; trunk/legs/arm/chin. Dr Brunton called to review'. Mrs Oakley says she remembers being on her break at 1am-2am, so was in the resuscitation room where staff had their breaks. She said she had been gone because Child D was poorly. The prosecution ask about the timing of the 1.25am medication, and if the nurse can account for that. Mrs Oakley says she cannot. She says: "To the best of my knowledge, I remember going on my break, and remember being called back. "I had only been gone half an hour, and had been happy with her before I left. "I remember saying: 'What's happening?'"
12:00pm: Asked about the note, Mrs Oakley said the 'bubbly' bit is for bubbly saliva. She says she does not remember specifically the exact rash discolouration, but "hadn't seen it before - it was dark, it was unusual, and the rash struck me." Asked to expand on that, she says: "I haven't seen that rash before on a baby I have looked after. To the best of my knowledge, in my years of neonates (over 20), no."
12:01pm: Mrs Oakley adds: "It was unusual, I had not seen it before, and probably struggled to describe it. It was a deep red-brown...different from mottling, different from what I'd seen before." She says sometimes babies can look 'generally white' with a 'mottled all over' appearance, whereas this was a rash 'in specific places'.
12:02pm: She says: "It was just different from what I'd seen before, that's what stayed with me."
12:03pm: The nursing note adds: 'Saturations to 100% and O2 weaned to air. Observations satisfactory." Mrs Oakley said she couldn't recall who was doing what, but the oxygen was turned up on the CPAP machine, and Child D responded.
12:09pm: The note adds: "Dr Newby called in to review; fluids increased..." and a number of drugs and solutions were administered and prescribed. The note adds: "Discolourations resolved. [Abdominal x-ray] taken satisfactory. Continue supportive treatment [ie antibiotics]. Maintain UVC [ie don't take it out]. Decision to speak to parents later as [Child D] stable and doctors required on paediatrics. Repeat gas good." Mrs Oakley confirms the rash-like appearance had 'resolved' between 1.30am and after the doctor's review. She says Child D had had an episode but had responded "quickly" and "normal parameters" had resumed within an hour. As Child D was "very stable again", and the doctors were "busy", the decision was made to let the parents rest and inform them in the morning.
12:15pm: Mrs Oakley is asked to put into context further observation readings at 2.30am for Child D, which had "returned to normal". She says they would be considered "stable".
12:21pm: A 1.30am fluids reading records 'nil by mouth' at the time for Child D, along with 'oral secretion ++' for aspirates.
12:24pm: The fluids chart also notes what Mrs Oakley believes is a task carried out for Child D by Lucy Letby at 1.05am, which she said would have been noted retrospectively, as Mrs Oakley would have started her break at this time.
12:28pm: Nurse Oakley's nursing note adds: "[3am Child D] crying and desaturated again to 70s. Commenced on 100% O2 via CPAP and picked up well but skin discoloured again but less than previously. Dr Brunton called to review; take off NCPAP, further fluid bolus and gas 1 hour cares attended to; [passed urine] +++ and passed meconium." Mrs Oakley says she cannot recall the events around this collapse, and says her memory of it is limited to that of her notes.
12:35pm: A nursing note of drug infusion, which Mrs Oakley says the doctors believed Child D would need more fluid on board, is noted at 3.20am. The fluid chart records for 3.30am 'restart expressed breast milk (1ml).' The prosecution say the collapses had been of concern to nurses, and why the doctors were called. Mrs Oakley said after the review, the doctors were "happy with her" and for fluids to continue to be administered. She added Child D had passed urine and had a wet nappy, and so she was comfortable in changing her nappy. "If I thought she was unstable, I would not have chosen to change her nappy. If the baby's unstable, they do not tolerate handling. Even cleaning them could cause them to be unsettled, with their heart rate going up."
12:37pm: The nurse added 'observations satisfactory' and Child D was 'handling well'. The final observation readings were all in normal parameters at 3.30am.
12:42pm: At 3.45am, the nurse noted: "Monitor alarming, [Child D] desaturated again and [stopped breathing]. Called senior nurse Letby to help. Stimulation given." Use of Neopuff was given at 3.52pm. A senior house officer was called to help. Dr Brunton called to help, resuscitation efforts began. The prosecution asks if Mrs Oakley has a memory of this. She says she does note, it was "just a blur, just very busy. She 'misbehaved' [had gone poorly again]. I don't remember specifically." She does not recall if an alarm went off. From her notes, she called Letby to assist. The initial 'stimulation' effort was, the court hears, to tickle the feet, trunk, ears, which can in itself get a baby stimulated enough to start breathing. Mrs Oakley says she played a part in the resuscitation efforts.
12:47pm: Ben Myers KC, for Letby's defence, is now asking Caroline Oakley questions. He asks if she was aware of the 'increased mortality rate' between June 2015 and July 2016, and in a police statement, said it was a 'busy and stressful time'. Mrs Oakley agrees. He asks whether that was from increased admissions to the neonatal unit. "There were a lot of babies." She said she couldn't say if that was an increase, and would have to see the statistics. Asked if there were an increased number of acutely poorly babies, Mrs Oakley replies: "I'm not sure, I worked there a long time. We used to take a lot of 24-weekers when I started [over 20 years prior]. "I remember midwives bringing babies in when we were busy."
12:49pm: She says she does not remember the unit being "unduly short-staffed". Mr Myers suggests that at times of crisis, they had the staff they required. Nurse Oakley: "Yes, as they would be called from other patients."
Mr Myers: "But maybe at other times, you didn't have as many staff as you needed?" Nurse Oakley: "I'm not sure."12:52pm: He refers to Child D as an intensive care baby. Mrs Oakley says she wasn't a 'poorly' intensive care baby as she wasn't on ventilator support. She says Child D was classified as an intensive care baby. The chart showing Mrs Oakley looking after Child D in room 1 and a baby in room 2. He says intensive care babies require one-to-one support. "Ideally yes" He says the fact Mrs Oakley was looking after another baby too that night fell outside the guidelines. "That isn't in the guidelines, is it?" Mrs Oakley: "Strictly speaking no, but it does happen."
12:59pm:
Mr Myers: "It's important that with babies like [Child D] you remain vigilant, as they can deteriorate quite suddenly, can't they?" Mrs Oakley: "They can, yes." Mr Myers asks if Mrs Oakley was aware Child D had been on a ventilator until the early hours of June 21. She says she only knows that from the medical notes.1:45pm: We've had an adjournment for a shorter-than-usual lunch break. The trial is now resuming.
1:48pm: Ben Myers KC is continuing to ask nurse Caroline Oakley questions. He asks if she knew there had been a delay in giving Child D antibiotics after birth. She says she cannot remember, but can see from the notes. Mr Myers refers to a nursing note from June 21, during the day, that there were signs of respiratory acidosis after extubation. Mrs Oakley says she cannot remember that note, but she would have been told about it during the shift handover.
1:49pm: Mr Myers refers to the note continuing with 'blood gas repeated 2 hours later showed a further deterioration 'with increasing metabolic acidosis'. He asks whether she would have been informed of this. Mrs Oakley: "I'm sure it would've been mentioned [at the handover], yes."
1:51pm: Mr Myers asks about the attempt to take Child D off CPAP at 7.15pm, but Child began shallow breathing again, so was put back on CPAP. "What we have is a baby who has been struggling to breathe unaided [throughout the day]?"
"Yes." Mr Myers says there are warning signs she was not in an optimal state, and an indication she was "unwell". "If she needs help with her breathing, yes."1:58pm: The observation chart is shown for Child D for the night shift is shown again to the court. Mr Myers then refers, for context, to the previous 24 hours, showing Child D's observations were in 'the warning zone' for heart rate and breathing rate on several hourly observation readings from late on June 20 throughout the day of June 21.
2:06pm: A blood gas readings chart is shown to the court. The PH readings recorded at 10.14am and 12.10pm on June 21, of 7.194 and 7.173 are 'acidic'. Mrs Oakley agrees. She adds that doctors would have a better idea of the parameters of what would be normal readings for babies. Mr Myers, referring to other readings, says the situation is 'not as good' at 11.52pm as it was at a reading from 6.44pm. Mrs Oakley agrees. Mr Myers says the blood gas readings are worse at 1.14am, and point to a deterioration. Mrs Oakley says the readings to her are not as good as earlier, and says the doctors would take action based on them.
2:08pm: Mr Myers refers to the break Mrs Oakley took between 1-2am. Mes Oakley says she is not sure the 1.14am blood gas reading notes are in her handwriting. Mr Myers refers to the 1.15am observation chart reading note, which has Mrs Oakley's signature initials. Mrs Oakley says she would have usually expected to write those observations at 1.30am [prior readings are 11.30pm and 12.30am, with subsequent readings at 2.30am and 3.30am], and may have written them retrospectively - "it does happen".
2:12pm: An IV prescription chart, with Mrs Oakley's signature initials at 1.25am, is presented to the court. Mrs Oakley said the prescription is not in her handwriting. Mr Myers says it's not unusual for nurses to help each other out, particularly for procedures which could involve two nurses. Mrs Oakley agrees.
2:15pm: A fluids chart is presented, showing the gastric tube change recording '0105 - suction pp ll, AXR, bolus'. Mrs Oakley says she believes she has written that retrospectively, and has summarised what was told for that 1.05am. She has summarised that they wanted a bolus and an abdominal x-ray. She says she would have been told all this by Lucy Letby, by another nurse Kate Percival-Ward, or a combination of both.
2:19pm: Mr Myers refers to the 1.30am collapse of Child D. Mrs Oakley says it was a short distance from the resuscitation room to room 1, and does not recall who came to get her. Mr Myers said Child D responded well to the oxygen, and no resuscitation was required. Mrs Oakley agrees.
2:22pm: Mr Myers refers to the skin discolouration of Child D at the time of the first collapse.
Mr Myers: "Does that suggest the skin discolouration was all over her body?" Mrs Oakley: "The front of it yes, but I don't know if it was all the trunk. I don't think it was all the trunk, all the legs." Mr Myers refers to her finding the rash-like appearance being 'unusual', and a 'struggle to describe it'. "You said you couldn't remember it - was a deep red-brown what you saw?"
"I just remember the rash, I don't remember the specifics of it, I just remember it was an unusual rash."
"Would it be fair to say the fact it was unusual that stuck in your mind?"
"It always has, yes."2:24pm: Mr Myers refers to the 3am collapse of Child D. He suggests that Mrs Oakley was present at the time of the collapse. Mrs Oakley says she would have been in the vicinity at the time, and does not remember what she was doing.
2:28pm: Mr Myers says it was an episode which resolved 'quickly' and resulted in a decision to take Child D off CPAP. He asks whether there had been a discussion about Child D's breathing support difficulties earlier that day. Mrs Oakley says she does not remember. She says she believes if the desaturations had gone to the 70s, the alarms would have gone off and she would have been alerted to Child D. The 3.45am collapse is now being referred to. Mr Myers says at that point, Child D had been taken off CPAP. Mrs Oakley replies: "Honestly, you would have to check the times for me."
"She was stable in between these two times?"
"Definitely." Mr Myers says there is then a more marked deterioration, as Child D stopped breathing, and nurse Oakley called for help. Mrs Oakley agrees.2:31pm: The prosecution rise once more, led by Simon Driver, to ask about the discolouration of Child D's skin at 1.30am. He asks what it was that struck her about the rash appearance that was unusual at 1.30am. "I'd not seen it before." He asks how it had changed by 3am. She replies the rash wasn't as pronounced, not "as bad", but she was not expecting Child D to deteriorate again. She says she had previously experienced 'mottled' appearance in babies - 'newborn spots', or 'mottled', but "we don't specifically get rashes, in my experience".
2:34pm: The judge, Mr Justice James Goss, asks to clarify one matter from the 1.30am collapse. "You said some of that was what you had been told had happened." Mrs Oakley says the 'oral suctions' referred to what was being done to Child D before she arrived back in room 1. The part of the note from 'discolourations to skin observed' were her own observations.
Monday 7th November 2022
Child D
Dr Andrew Brunton - Dr Joanne Davies (consultant in obstetrics and gynaecology) - Nurse Assistant Lisa Walker10:12am: This morning we're expecting to hear evidence from former colleagues in regards to the death of Child D in June 2015.
10:44am: Dr Andrew Brunton, who is now a consultant neonatologist but was a trainee doctor in 2015, is in the witness box. He is running the jury through is notes from June 20. He notes at the start of his shift that Child D was in 'respiratory distress' His notes from around 21:45 that evening state: 'Explained (to father) that safest option at present would be to intubate and ventilate her now with the hope of weaning her off the ventilator quickly'
10:54am: Child D was deemed 'clinically stable' at around 23:15 after being placed on a ventilator. At that time, parents were told 'if prolonged ventilation is required or a deterioration, we may have to think of transferring to Arrowe Park Hospital or Liverpool Women's Hospital'
10:59am: Another note from 01:50 on 21 June, 2015 shows an improvement in Child D's condition. Dr Brunton took the decision around this time to wean her off the ventilator.
11:11am: Later that day, Child D was taken off a ventilator and placed back on a less invasive form of respiratory support (continuous positive airway pressure or CPAP therapy). Dr Brunton's notes from that night state that she was 'clinically improving' and 'well enough' to take milk
11:16am: Four hours later at around 01:40 on June 22, Dr Brunton was called 'urgently' to attend to Child D. His note from that morning states: ‘Called urgently to review baby. Nurses noted that became extremely mottled also noted to have tracking lesions dark brown/black across trunk'
11:22am: Dr Brunton tells the court that a consultant was called as 'this was a completely unusual situation that I hadn’t seen before', he said he 'couldn’t explain' the discolouration of Child D's skin
11:34am: After treatment, an hour later notes show Child D's condition had 'improved' and areas of discolouration had 'completely disappeared'
11:38am: Dr Brunton was 'urgently' called back to attend Child D again at 03:15. His notes from that morning show that the rash had reappeared. It is the Crown's case that the rash was a result of Ms Letby injecting air into the bloodstream
11:53am: At around 03:55, emergency treatment commenced. Dr Brunton recalls running from another area of the hospital after receiving a crash call. He along with other medics began chest compressions after Child D stopped breathing. Adrenaline was administered shortly after 04:00
12:01pm: Dr Brunton's notes show that five adrenaline doses were administered over the next 10minutes. 'This was necessary because (Child D) was in effect dying in front of us', he told the court. After a conversation with Child D's parents, CPR was stopped after 28 minutes. Asked to summarise the events of that evening, he said: 'From when I came in on my night shift there weren't any particular worries or concerns regarding (Child D). He added: 'By 01:40 to her death (Child D) had dramatic deteriorations at different points. It was completely unclear to me why that was occurring 'I've never seen a baby behave in that matter prior to this or after this'
12:47pm: Ben Myers KC, defending Ms Letby, is now taking jurors back through Dr Brunton's notes. Mr Myers has said it is important to look at the 'whole clinical picture' when assessing Child D's health He has previously told the jury there was more evidence that infection played a part in Child D's death and the hospital failed to provide adequate care
12:57pm: Mr Myers is putting it to Dr Brunton that there was nothing to support (in terms of Child D's condition) his decision to move her off CPAP. Dr Brunton rejects this, he says her clinical readings were moving in the right direction He added that is was a 'natural process' on a neonatal unit to try and move a baby off CPAP. Court has now adjourned, back in an hour.
2:17pm: We're back. Dr Joanne Davies, who is a consultant in obstetrics and gynaecology at the Countess of Chester, is now giving evidence. She's discussing the health of Child D's mother. She says that it was a 'low risk' pregnancy.
2:51pm: The court previously heard that Child D's mother was left waiting more than 50 hours for treatment after her waters broke early. Last week the mother told the court: 'I felt very worried and scared, I felt unwell and not in control. I felt I was being forgotten by the staff' Dr Davies tells the court that the mother's 'care followed the guidelines'. She said the guidance is to 'leave someone for 24 hours to see if they labour by themselves', they are then offered inducement - but it is 'not unusual' for this to take another 24 hours hours
2:53pm: When pressed by Ms Letby's defence barrister, Dr Davies does however acknowledge that there was a shortfall in the care of Child D's mother as an oral antibiotic was not initially provided after her waters broke
2:55pm: Dr Davies says she doubts whether the antibiotic 'would have had any effect in this case'. Mr Myers responds saying, 'you may doubt, but you don't know do you?' 'I don’t know', Dr Davies says
3:15pm: Dr Davies told the court that the mother did not present with any signs of infection prior to the birth, but accepted the findings of a pathologist's report into the death of Child D which deemed the cause of death was pneumonia. Mr Myers described this as a 'conundrum'
3:31pm: Junior nurse Lisa Walker is now in the witness box. She is describing seeing Child D in the moments after her birth. 'She looked very blue in colour. I immediately shouted for help', she said
3:33pm: She said a doctor that was present 'looked shocked I shouted for help'. She said he 'wondered why I shouted for help...he didn’t know what was going on' Ms Walker said following the incident she filled out an internal form to express concern over his (lack of) action
3:57pm: Court has now adjourned for today, back tomorrow.
Chester Standard article 7-11-2022
A DOCTOR has told a jury it was "completely unclear" why a baby allegedly murdered by Countess of Chester Hospital nurse Lucy Letby had "dramatic deteriorations" before her death.
The baby girl, referred to as child D, is said to be the third child murdered by the defendant in a two-week period, with another suffering a life-threatening collapse during the same time.
Registrar Andrew Brunton was called three times by concerned nurses during a night shift at the Countess of Chester Hospital's neonatal unit in June 2015.
Child D was receiving respiratory support after she was earlier taken off a ventilator on June 21 - a day after her birth, soon after which she lost colour and became floppy in her father's arms.
Dr Brunton told jurors at Manchester Crown Court that child D was "clinically improving" on the evening of June 21, but he was called to urgently review her at 1.40am the next day.
He said there was a concern her oxygen levels had dropped and she had developed a rash.
In his notes, Dr Brunton put: "Skin brown. Areas of discolouration – light brown across trunk (stomach)."
Child D quickly recovered and the rash vanished, the court heard, but Dr Brunton contacted the on-call consultant to review the infant.
Giving evidence on Monday, November 7, he said: "This was a completely unusual situation that I had never seen. The changes in the skin – I couldn't explain it."
He was called again at 3am as he was informed Child D was upset and crying, her oxygen requirements had risen again and the rash had reappeared.
Dr Brunton said: "I can't remember the specifics but I remember her being quite agitated and upset. This stuck in my mind as she had not been like that when I examined her before."
Child D recovered and he said he decided to withdraw CPAP (continuous positive airway pressure) respiratory support, as he thought at the time it may be the source of her agitation.
Dr Brunton noted skin discolouration again on the abdomen but not as pronounced as the first occasion, the court was told.
At 3.45am he was asked again to attend the neo-natal unit and said he ran when the request was followed by the sound of a "crash bleep".
Child D had stopped breathing and chest compressions had started by the time he arrived, he said.
She was given a number of adrenaline doses in a bid to stimulate her heart, as well as fluids and sodium bicarbonate.
Dr Brunton said: "All of that was necessary because (Child D) was, in effect, dying in front of us."
A discussion with her parents followed and it was agreed to stop CPR. Child D was pronounced dead at 4.25am.
Prosecutor Simon Driver asked Dr Brunton: " Having made repeated observations and examinations on (Child D) during the course of the shift which culminated in her death, how would you summarise the evolution of her condition that night?"
He replied: "From when I came in on my night shift there were no particular worries or concerns identified, but by 1.40am to the time of her death she had dramatic deteriorations over different points.
"It was completely unclear to me why that was occurring."
Mr Driver said: "Why was it unclear?"
Dr Brunton said: "Because I had never seen a baby behave in that manner prior to this and I have never seen a baby behave in that manner after this."
Ben Myers, defending, said Child D had breathing problems from birth, had previously needed to go on a ventilator and "nothing indicated" she would do well if taken off CPAP.
He asked the witness: "When you took the decision that she should come off CPAP, did it cross your mind it may lead to a deterioration?"
Dr Brunton replied: "Absolutely not.
"If we are trialling a baby off CPAP they can go back on it if we think they are not able to cope with it."
The Crown say Letby injected a fatal amount of air into Child D's bloodstream.
Letby, 32, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others at the Countess of Chester Hospital between June 2015 and June 2016.
Tuesday 8th November 2022
Child D
Dr Sarah Rylance - Unnamed Nurse - Dr Emily Thomas - Nurse Elizabeth MarshallChester Standard Live Reporting
10:30am: The trial will resume shortly. Letby has arrived in court with a custody officer, as has been the case for each day of the trial.
10:41am: An interpreter will be required in court today, for an unusual reason. The next doctor witness will be giving evidence from Switzerland, via videolink. Under Swiss law, the doctor's evidence will be coming from a court in Switzerland, and a French-speaking Swiss prosecutor will be present. What is said in Manchester, and the doctor's evidence, will be translated into French by the interpreter in the Swiss court for the benefit of the Swiss prosecutor.
10:46am: Through discussions between the two courts, it is now understood everyone in the Swiss court can understand English. The judge in Manchester, Mr Justice Goss, has said the proceedings will carry on in English, and translation will only be required if there are either technical difficulties or the odd word which will require interpreting into French.
10:49am: Members of the jury have now come into court, and matters have been explained to them about the international videolink arrangement. The next witness to give evidence is Dr Sarah Rylance.
10:54am: Dr Rylance confirms she was employed at the Countess at Chester Hospital as a registrar in June 2015, and worked a long day shift on June 20 that day. She confirms she has the clinical notes for Child D to hand. A reminder that, due to reporting restrictions, none of the children in this case can be identified.
11:03am: Dr Rylance says she does not believe she was present at the birth of Child D. The details are recorded retrospectively, that Child D was born at 4.01pm on June 20. The note includes: 'Bleeped again as midwife not happy with her colour' - she is not able to say whether that was her being bleeped again. Child D 'looked dusky' and had 'poor respiratory [efforts]', with initial oxygen saturations at 48%, poor respiratory effort at 7.30pm. The note adds 'transferred into incubator'. After being given breathing assistance via Neopuff, Child D 'pinked up quickly and started regular resps'.
11:05am: The prosecution ask for what Child D would have been assessed as. Dr Rylance: "She responded well to the ventilation support she has been given."
"In relation to the blood gases, it's difficult to assess how that reflects on her clinical condition." The blood gases suggest Child D had difficulties with breathing and metabolism, but Dr Rylance said she would not use the blood gases alone to make a diagnosis, but take it into context with other readings and observations.11:07am: Child D was 'transferred on to CPAP', and an IV saline solution was administered. Child D was also started on 'triple lights' as part of phototherapy to treat her jaundice symptoms. That was the "maximum treatment" level, Dr Rylance, tells the court.
11:09am: Dr Rylance's notes, also record, for Child D at 8pm, the baby girl was on CPAP, 40% oxygen, and '[saturations] 100%'. Child D's heart sounds were "normal", with an "ok" pulse rate, and it was noted there were regular breathing efforts, "but fairly shallow" and the abdomen was not distended. The plan was to continue CPAP and administer dextrose, and repeat a blood gas test at 8.45pm.
11:12am: Dr Rylance's notes at 8.20pm record the parents were updated on Child D's condition, with "likely sepsis" and she was receiving antibiotics "to treat infection". The doctor tells the court Child D's condition was, at this point, "responding well to interventions" and "appeared to be stabilised on the CPAP and making respiratory efforts."
"Overall I was happy with the the progress she had made, but she needed to be closely monitored and assessed."11:18am: A further entry is made at June 21, 2pm, in the clinical notes. The entry records the insertion of a UAC and UVC into Child D. The UVC was removed as it was 'only able to advance to 5cm'. Dr Rylance says usually "you are expected to advance it much further. "It can be difficult and fiddly to do this procedure in new-born babies." The UAC was inserted to 20.5cm, but did not get a blood sample back. An x-ray review found it was advanced 'way too far', and the route was 'not typical of a UAC'. The UAC "should follow a typical route", the court hears, and the line was pulled back to 9cm. A blood gas reading was taken and the readings were 'much improved'. A second x-ray showed the UAC position was 'better', but the route was 'still not typical'.
11:23am: The 'much improved' blood gas reading was, Dr Rylance believes, a comparison with the previous blood gas reading. The UAC was 'actually a UVC' and adjusted to be used as a UVC. The plan was to continue CPAP for Child D and repeat a blood gas reading, and 'try to sample UVC' for various readings. A review is carried out at 7pm on June 21, with 'presumed sepsis' noted. A CRP reading of 1 is recorded, having previously been 6. Dr Rylance, commenting on those readings: "I wouldn't attach particular significance to it," as both readings were "low", and would need to be taken in context with the baby's clinical condition and observations.
11:25am: Child D had been on CPAP all day, but 'in air' and 'saturating well', with 'no desat[urations].' The initial blood gases post-extubation at 9am were 'not good', so Child D was put back on to CPAP at 10.30am. Dr Rylance said Child D had made good progress, and her ventilation status was "very satisfactory" at the time she reviewed her.
11:32am: Under the heading 'sepsis', the CRP reading was '1', and Child D had 'not had [lumbar puncture] yet.' Such a test is done in clinically stable babies to test infection has not spread, the court hears, but Child D was 'not stable enough' for that to be carried out. Other observations were noted by Dr Rylance that Child D was 'responsive on handling', with 'chest clear, regular resp effort, minimal recession', abdomen 'soft, not distended'. The feet were 'quite purple', but Dr Rylance says that would be as a result of frequent tests carried out. The court has previously heard heel prick tests would be done to get results such as blood gas readings. Dr Rylance added: "Overall my observations were that she was stable and handling well...and responding well to treatment she had received throughout the course of the day." Under 'impressions', Dr Rylance noted: 'stable on CPAP, tried taking her off but resp effort became irregular and desaturated a few times so put back on'. Dr Rylance said she would not have attached a lot of significance to this, as "it takes babies some time to settle. She was obviously unwell when she came to the neonatal unit the previous evening. "She needed a bit more time from the CPAP...allow us to transition having been ventilated and moving to breathing. "If they don't seem to tolerate it well, you can just put them back on [CPAP]. "She was heading in the right direction, she just needed a little support from the [CPAP] machine without added oxygen."
11:34am: The note added, as part of the plan, 'leave on CPAP, await CRP...leave UVC for now to allow sampling for gases, continue [antibiotics].' Dr Rylance says she was "happy" with Child D's clinical condition, having had "a very satisfactory day" and was improving, in good colour, not needing oxygen support. "She has shown good improvement from the condition when I first saw her on the neonatal unit the previous evening."
11:37am: Ben Myers KC, for Letby's defence, is now asking Dr Sarah Rylance questions. He says there were two instances of her examining Child D. He said that at the end of the June 20 examination, she was "happy with [Child D's] progress". "Would you agree she was at risk of complications?" Dr Rylance says Child D had responded well to treatment, but the blood gases were not in the normal range, and that would require close observation.
11:41am: Mr Myers points to Child D having 'lost colour' and 'floppy' when in her father's arms moments after birth. "Do you agree that is worrying at that stage?" Dr Rylance agrees the Apgar scores of 8/10 and 9/10 aren't relevant for 12 minutes later. Mr Myers asks if the progress of Child D is based on the reference point from the worrying signs just after birth. Dr Rylance: "My opinion of her at the end of the shift, my reference point is from when I first had contact with her on the neonatal unit, from when she required ventilation support. "I wasn't involved at her birth...I can't comment on her condition at the time. My writing [on the clinical notes] is based on what I had been told. "It's my summary, but not my observations, if that makes sense."
11:42am:
Mr Myers: "You will have known...she started grunting in theatre...reviewed after 1.5 hours, 'grunting but otherwise observations ok'." Mr Myers asks if grunting can refer to respiratory effort difficulties. Dr Rylance: "Yes it can."11:45am: Dr Rylance says she is unable to recollect whether she saw Child D prior to her neonatal unit admission, but does not believe she was involved in the review to bring her to the unit. She said: "From the point she came to the unit, these were my direct observations." Mr Myers asks if Dr Rylance reviewed Child D at about 7.30pm.
Mr Myers: "She presents as a baby who is seriously ill?" Dr Rylance: "Yes...at that point she was an unwell baby."11:48am: Dr Rylance says she believes the first time she reviewed Child D was in the neonatal unit. Had she done so before, she would have noted that from a ward observation. The venous gases taken at that time show 'marked acidosis', Mr Myers asks. Dr Rylance agrees.
Mr Myers: "You explained to us these were abnormal and indicate difficulty with the respiratory system and metabolic components?" Dr Rylance: "Yes, that's correct." Mr Myers says those readings are taking into account the clinical condition for Child D. Dr Rylance: "Yes."
Mr Myers: "But at this stage, weighing up the clinical picture, it was not a good picture, was it?" Dr Rylance: "No."11:52am: Mr Myers said at one point, Dr Rylance had referred to the examination as being 'normal', but there was quite a lot of Child D being 'abnormal'. Dr Rylance says Child D was "not a healthy baby at this point in time". She says she is aware Child D was later put on to a ventilator.
Mr Myers says infection is a 'leading cause' in neonatal deaths and can 'develop very quickly'. Dr Rylance: "It can."
"As a rule, antibiotics should be given to a neonatal baby... "There are different guidelines on whether babies should receive antibiotics, with clinical risk factors. "When you have concerns...then you want the antibiotics as soon as possible." Mr Myers says Child D's mother had her waters break many hours before giving birth, and that Child D was, at birth, 'floppy' and at risk of collapse. Dr Rylance agrees Child D should have received antibiotics at this stage. She adds this is reliant on someone else's documentation, and it is difficult to say precisely how Child D was responding at that time. She says it would have been a good idea to start antibiotics as quickly as could be done, and that was done upon her arrival at the neonatal unit.11:55am:
Mr Myers: "The reality is, from the point of collapse at 12 minutes...given everything we know, [the plan] would have been to give antibiotics rapidly?"
"Yes, I think so." Mr Myers says Child D was not given antibiotics until nearly four hours after birth, at the neonatal unit. Dr Rylance agrees that would be the case. "There was a four-hour delay in the delivery of antibiotics after birth?"
"Yes."
"You may not be responsible, but that falls below the standard of care for a new-born baby, doesn't it?"
"Yes."
"The purpose of antibiotics is to treat and reduce the risk of infection?"
"Yes."12:00pm: Mr Myers refers to the blood gas readings on the afternoon of June 21. Dr Rylance says there would have been a blood gas chart and the readings were presumably an improvement on what was previously taken. Dr Rylance tells the court the intention was to insert a UVC and a UAC, "if it's possible to do so." The court hears the 'UAC' inserted acted as a suitable UVC instead.
12:08pm: Mr Myers refers to the 'presumed sepsis CRP 1'. He says the CRP reading increases from CRP 1 to CRP 6 later that night. He says from those readings, they cannot diagnose infection on their own. Dr Rylance: "Yes." Mr Myers refers to an attempt to take Child D off CPAP by Dr Rylance, as noted, and an accompanying nursing note referring to the oxygen levels desaturating to the 80s.
He says "that is not a healthy state to be in, is it?"
"It reflects she needed more respiratory support, but the fact she had moved on from ventilator support, and needed no oxygen support, suggested it was improving.
"By trying to take her off CPAP, we wouldn't have done that if she wasn't stable.
"She didn't tolerate it, so we put her back on."
The improving clinical condition, Dr Rylance says, was from Child D arriving at the neonatal unit to her observation the following day. Mr Myers says the 'satisfactory examination' of Child D was carried out while she was on CPAP. Dr Rylance says a lumbar puncture is "quite an invasive" procedure and there is a risk of that being carried out if a baby is still on breathing support. In Child D's case, it was "weighed up" and it was felt it was not needed to be done at that time.12:09pm: Mr Myers said Dr Rylance had identified sepsis and acidosis "at various points" and during the time she was cared for, Child D required breathing support. He says that when Child D was taken off CPAP, she began deteriorating. Dr Rylance agrees.
12:13pm: The prosecution, led by Simon Driver, rises to clarify about the notes made for Child D following birth. "As of your last review on 7pm on June 21, what was your assessment of her at that stage?"
"From what I documented, [Child D] was stable...with minimal respiratory support and no additional oxygen support. "In handling, she was responsive and making good progress and making good response to treatments over the previous 24 hours. "She was not a healthy baby at that time [due to still requiring CPAP], but...clinically she was stable and making a lot of progress."12:30pm: The next witness, who cannot be named due to reporting restrictions, confirms she was a neonatal unit nurse at the Countess of Chester Hospital in June 2015. She tells the court night shifts would be "generally quieter" in terms of staffing numbers, and there were no set rules on when they would take breaks, and would depend on workloads. When they were on breaks, another member of staff would be directed to cover for the designated baby. That role could be done by the shift leader.
12:34pm: The nurse confirms she was the designated nurse for two babies in room 2 on the night shift of June 21. She said she cannot remember having any cause to be involved with Child D on the early part of that night. A medicine chart is presented to the court showing the nurse was a co-signer for doses of medication for Child D at 9.23pm.
12:38pm: The nurse says her memory of Child D's collapse at 1.30am is "vague", but remembers her being "stiff" and having a "rash" on her abdomen. She says she does not remember whether she was in the room at the time of the collapse. She says, from her statement, colleague Caroline Oakley (the designated nurse) was not present in the room at that time. She recalls Child D's appearance - the baby girl was 'discoloured' and "stiff". The discolouration "was like a mottled appearance", it was "an odd rash, it was unusual". She said mottling would be blue and grey, whereas this was "not that colour". She said it was a "reddy brown" colour, which was "unusual", and this was found on Child D's abdomen.
12:41pm: The nurse says she wants to say she had seen this discoloured appearance again, but could not say whether that was before or after June 2015. Asked by the prosecution to clarify, she tells the court she had not seen that discoloured skin appearance in the years prior to that. The nurse remembers Child D recovered quickly and was examined by Dr Andrew Brunton. She says, from her notes, the rash had 'resolved' by that point.
12:42pm: The nurse added a similar event happened for Child D where she desaturated. She does not remember the circumstances but believed it was similar where she was given treatment, reviewed, and recovered. She said she didn't remember seeing Child D, but would have done so as part of her shift. She said she didn't remember anything about the child's appearance or recovery.
12:46pm: The nurse tells the court there was further desaturating for Child D, she would have been notified to the room - but does not recall how - and there was a call for a medical review. Full CPR was being carried out on Child D by the time Dr Brunton arrived in the room, the nurse tells the court.
12:52pm: The nurse recalls the efforts made to resuscitate Child D, which were made in established guidelines, and ultimately efforts were not successful. She recalls the parents were there at the time. After Child D had died, she recalls having a conversation with Lucy Letby on the resuscitation drugs used. A chart advising dose levels for the drugs would usually be kept by the child, but this A4 chart, a laminated piece of paper, was missing. The nurse said that chart was missing, and the resuscitation drugs were administered by calculating the doses with Child D's weight, and using her years of experience. The chart "eventually turned up", the court hears, as "it must have gone missing in the stress of everything". Lucy Letby asked the nurse how she knew what dose levels to give, and the nurse explained how she had done so.
12:57pm: Mr Myers, for Letby's defence, asks the nurse about workloads between June 2015-June 2016. The nurse agrees there was a higher workload during that time, with an increased acuity overall in the patients arriving in the unit. Mr Myers asks about the 14 babies being on the unit on the night of June 21. He says "ideally", the shift leader (which the nurse was working that night) would not be looking after babies on the unit for that shift. The nurse agrees. Mr Myers said Child D was being looked after by Caroline Oakley, who was in room 1 (the intensive unit room), and another baby in room 2 (a high-dependency unit room), and that goes against the guidelines. The nurse says: "It's not what the guidelines say, however, the ITU guidelines are quite specific." The nurse says some babies in intensive care require different levels of care. Mr Myers says, ideally, Child D would have 1-2-1 care that night. "Ideally, yes."
12:59pm: Mr Myers asks about Child D's collapses that night. The nurse confirms resuscitation attempts were only required on the third collapse. Mr Myers asks about the rash - which the nurse described as 'mottled, white circles, with a reddy-brown colour'. He asks if that is what the nurse remembers from telling the police, or from discussing it with colleagues. The nurse: "No, that is how I remember the rash." Mr Myers asks if that is how she remembers the rash, as 'reddy-brown' was not in the police statement. The nurse agrees. She also says she cannot remember how long the rash lasted.
1:05pm: The court is now hearing from Dr Emily Thomas, who in June 2015 was working at the Countess of Chester Hospital. She remembers the night shift being busy on the children's ward, and her colleague Dr Andrew Brunton being called out to assist Child D. She recalls an unusual rash appearance at the 1.30am collapse, with purple colouring around the abdomen. Dr Thomas said she was in the middle of a septic screening in room 2 or 3 at the time of the third collapse. She said she believed Lucy Letby was the one who had called for help, and recalled her being upset, saying what she recalled was: "This is my second baby that this has happened to".
1:06pm: She did not recall seeing a rash on Child D during the resuscitation attempts.
1:14pm: The next witness, Elizabeth Marsh, was working a night shift on June 21. She said on this shift, she was looking after babies on the post-natal ward and babies on the neonatal unit. She said she saw Lucy Letby giving chest compressions to Child D at the time of her third collapse. She said she was not directly involved in the resuscitation attempts, and was involved in the transcribing of the efforts, writing the notes on a paper towel. She said there was a short debrief at the end of that, but nothing more formal at that time.
1:24pm: The court also heard, from Dr Thomas's statement, there was a communication mix-up when Dr Brunton was on the telephone to what he thought was an on-call consultant, but was actually one of the parents of Child A and B. By this time, Child A had died and Child B was being treated in the neonatal unit following a non-fatal collapse. Previously, the court heard the parents of Child A and B would be in very regular contact with the hospital throughout the nights for an update on Child B's condition. Dr Brunton was "mortified" when he realised the communications error had been made.
5:09pm: The trial finished early on Tuesday as it had been anticipated Dr Sarah Rylance's evidence was to be translated into French for the benefit of the Swiss prosecutor in the Swiss court she was giving evidence from. However, once it transpired all parties were able to speak English, that meant the evidence was able to be given much quicker, without a need for an interpreter. The trial will continue on Wednesday.
Wednesday 9th November 2022
Child D
Dr. Elizabeth Newby - Nurse Kathryn Percival-Calderbank - Dr Dewi Evans10:40am: I’m at Manchester Crown Court for the continuing trial of the nurse Lucy Letby.
10:54am: Consultant paediatrician Dr Elizabeth Newby is describing how she treated an alleged victim, Child D. She says D as born in good condition but needed help with breathing shortly afterwards. By the evening she needed to have a tube in her windpipe to help….
10:57am: …but by the next morning D was well enough for the breathing tube to be removed. D was able to breathe on her own in air. Dr Newby “felt it was likely that there was an element of infection” as D’s mothers waters broke early and there was a delay in her having a C section birth
11:10am: Dr Newby was called in to see D at 2am the following day as D had had a “profound desaturation”. [very sudden loss of oxygen levels in blood]. She was called in because D had been so stable and then had deteriorated.
11:18am: Dr Newby describes unusual discolourations (“bruised areas”) on D’s abdomen. “We didn’t know what to make of them, to be honest. It was quite unusual. We felt it must be related to infection.”
11:22am: She says the discolouration might be related to meningococcal disease in older children, but “I know that couldn’t apply to neonates because you don’t see meningococcal disease babies.”
11:24am: Cross examined by Ben Myers KC, defending Ms Letby, Dr Newby agrees that after birth D’s “condition was consistent with an infection of some sort.”
11:40am: Mr Myers asks Dr Newby about notes relating to D the night before she collapsed showing that efforts to take her off CPAP (continuous positive airway pressure) were unsuccessful because D deteriorated when this happened.
11:49am: Dr Newby agrees with Mr Myers that “ a baby who is unwell can have resistance to infection - to keep running at a certain level and then deteriorate very rapidly.”
2:25pm: Court now hearing from Dr Dewi Evans, a paediatric expert instructed by the prosecution. Nicholas Johnson KC is asking him what he says about his review of the medical notes relating to Child D.
2:27pm: Asked about “mottling” seen on Child D’s body the first time she collapsed, Dr Evans says “it’s very significant and extraordinarily unusual. This is not something that happens out of the blue.”
2:36pm: Asked about D’s condition immediately before her collapse, Dr Evans says “Her condition could not have been better. Her condition was entirely consistent with a baby recovering from early onset pneumonia. She was doing exceptionally well and was clinically very satisfactory.”
2:37pm: But Dr Evans says D was “recovering” from early onset pneumonia, not that she had “recovered” from it.
2:53pm: Dr Evans asked what would have happened if pneumonia had caused D’s death. “You find increased amounts of clinical input would not lead to improvement.. in D’s case none of this happened. She got better.”
2:54pm: Dr Evans says his conclusion in Child D’s case is that death was caused by an injection of air into her bloodstream.
2:58pm: Ben Myers KC, defending, asks Dr Evans why he thinks this. Dr Evans gives 5 reasons. 1. D’s collapse was rapid and v striking. 2. The presence of discolouration on D’s body “a pattern experienced [nurses and doctors] had never seen before and never since and it came and went..
3:01pm: 3. Attempts to resuscitate D were unsuccessful. 4. The presence [at post mortem] of air in D’s blood vessels and 5. None of the other issues, eg pneumonia were relevant.
3:03pm: “What we have in [D’s] case is a full house of clinical characteristics consistent with her having suffered an air embolism, ie air has been injected into her.” says Dr Evans.
3:07pm: Dr Evans agrees with the defence that D was in a state of very poor health when she went to the neonatal unit.
3:10pm: Mr Myers refers to Dr Evans saying D was “recovering” from pneumonia, and suggests that she still had the “potential to become quite unwell.” Dr Evans says “She was in a neonatal unit , the best place on the planet for her.”
3:12pm: When asked by Mr Myers again about her potential to become unwell, Dr Evans says “The potential is there, which is why she was on a neonatal unit.”
3:21pm: Mr Myers suggests Dr Evans doesn’t want to accept problems with [D’s] respiration because that would “undermine” his conclusion that D died from an air embolus. Dr Evans says “No.”
Chester Standard article 9-11-2022
A SENIOR nurse had "sleepless nights" over incidents at the Countess of Chester Hospital neo-natal unit where her colleague Lucy Letby is accused of murdering seven babies and attempting to kill 10 others.
Kathryn Percival-Calderbank recalled a night shift in which Letby, 32 is said to have administered a fatal amount of air into the bloodstream of a baby girl.
The infant, referred to as Child D, suffered three collapses at the Countess of Chester Hospital in the early hours of June 22, 2015.
On the first occasion, Mrs Percival-Calderbank told Manchester Crown Court on Wednesday, November 9, she noticed an "unusual, mosaic-type" rash on the youngster's torso and arms which was "reddy-brown" in colour.
Child D is alleged to be the third infant murdered by the defendant in a two-week period in June 2015, with another suffering a life-threatening collapse during the same time.
Giving evidence behind a screen, Mrs Percival-Calderbank said she had worked at the unit for newborn infants since 1993.
She recalled checking in on Child D while the infant's designated nurse, Caroline Oakley, was on a break.
"I remember looking in," she said. "She was nice and stable, the baby seemed quite settled.
"I popped in another time about 10 minutes later. She was OK."
Some time later, the witness said she returned to the intensive care room when alarms sounded.
Mrs Percival-Calderbank added: "The baby's monitor was showing she was desaturating and her heart rate had dropped.
"I don't know whether there was anyone else around at the time but I think there may have been."
She said she checked Child D's head position, gave "gentle stimulations" with her hand and then used a facemask to provide oxygen.
She went on: "I was assisted by someone. I can't clearly remember who it was. I have a feeling it might have been Lucy, but I can't categorically say."
Asked by prosecutor Philip Astbury if she noticed anything while assisting Child D, Mrs Percival-Calderbank said: "There was a rash on her trunk and arms. It was on her body from the chest downwards.
"It was not like a normal rash that you would know if a baby was becoming septic. The blood vessels tend to more bluey.
"This seemed to be a largely mosaic-type rash and it was a reddy brown colouring.
"It was not like a spotty rash. It was oval-type markings on the skin. The vessels of the blood seemed to be meeting up with each other.
"She was quite a pale-skinned baby, so they seemed to be pronounced browny/red."
The witness said the discolouring "seemed to disappear and dissipate after a while" and that Child D settled back into a normal pattern of breathing after doctors assisted in the intervention.
Ben Myers, KC, defending, asked if the "extra detail" she had provided about the rash, compared to her police statement, was something she may have picked up in conversation at work.
Mrs Percival-Calderbank replied: "I might have done, but it's also my recollections which have come back. It was an odd rash. It wasn't like a normal septic rash, it was a different type of rash."
Mr Myers said: "Can you help us with how you got the extra details?"
The witness said: "Because I started thinking about the events. As I was getting sleepless nights I was thinking about the events that happened."
On-call consultant paediatrician Dr Elizabeth Newby told the court she was asked to attend the first collapse of Child D but was "very surprised" when later asked to return.
Child D had recovered by the time she arrived at the unit, she said, but she stayed for "about an hour or so" to check if she remained stable and await blood test results.
Dr Newby said: "So I left and then not long after I was called back urgently as (Child D) had a further episode of collapse. When I arrived there was a full resuscitation in process.
"I was very surprised to hear a crash call because although I was concerned after the first episode she didn't appear to be a baby in extremis.
"Yes I admit these things can happen but that was not what I was expecting to happen that night."
Letby, originally from Hereford, denies the offences, said to have been committed between June 2015 and June 2016.
Thursday 10th November 2022 - no court (juror ill)
Friday 11th November 2022
Child D
Dr Sally Ogden - Professor Owen Arthurs (Child C & Child D) - Dr Sandie Bohin - Summary of police interviewsChester Standard Live Reporting
10:31am: The trial is now resuming.
10:36am: An additional agreed evidence statement is being read out for Dr Sally Ogden in respect of Child C, in relation to a clinical note. She refers to the clinical note from June 13, which include "bowel sounds heard". She said she heard Child C's bowel sounds as part of a routine examination, and documented that bowel sounds were heard. She said each individual finding forms part of the overall condition. She couldn't recall any more information about the bowel sounds, but if they had sounded 'abnormal', then that would have been documented as an 'important' finding. She said Child C's abdominal condition, from her observation, was 'normal'.
10:37am: Professor Owen Arthurs has been recalled to give evidence in respect of Child C and Child D.
10:43am: Professor Arthurs, a medical expert witness, confirms he has compiled reports for Child C and Child D. Nicholas Johnson KC, for the prosecution, asks about Child C specifically. Pictures are shown to the court, the first are radiograph images for Child C taken on June 10. He points out Child C is small and can almost fit entirely on the one x-ray image. The x-rays were taken to check for positioning of the UVC. He says the tube has been brought in a little too far and should be brought back a little. He says the problem with x-rays is they are 2D images of a 3D person, so there is difficulty with interpreting the picture 'without the baby in front of you'.
10:46am: Another x-ray of Child C is shown, taken at 10.38pm, showing the line had been withdrawn. There was 'normal gas' in the stomach and bowel. He says the most striking abnormality is the right lung on the image (the left lung from the child's perspective) is 'white', meaning there is 'something in the lung' preventing the x-ray light passing through, which would indicate an infection.
10:48am: A further x-ray image is shown for Child C at June 12 at 12.36pm, which is centred at the child's abdomen. He says the most striking feature about this image is the dilatation of the stomach, which is 'full of gas'.
10:49am: He says this is more gas in the stomach 'than you would expect for a child of this age'. There was a 'small tube' in the stomach taking out air. The left lung cannot be seen on this x-ray image.
10:51am: Professor Arthurs says, for his conclusion for Child C, that the 'marked gas dilatation' in the stomach noted at June 12 had several potential causes, including CPAP belly, sepsis, NEC or exogenous administration of air by someone.
10:53am: An observation was made there was no gas in the rectum area for Child C.
10:56am: Professor Arthurs is now giving evidence for Child D, and has examined radiograph images as part of his report. The first one, at June 20, 10.22pm, is presented to the court, in which there are no abnormalities seen.
10:59am: A second x-ray image of 'effectively the whole body' is shown the court at June 21, 1.32pm. Professor Arthurs notes two features - the 'obvious one' being the UVC going up towards the heart, which has been pushed in too far. The 'subtle' observation was a sign of infection in the child's right lung, but the magnitude was 'nothing like' that seen in Child C's case. The third x-ray image was taken at June 22, 1.51am, after Child D's first collapse. The UVC line has been 'withdrawn slightly'. The two-minute Remembrance Day silence is observed in court.
11:02am: Professor Arthurs resumes giving evidence.
11:05am: He explains the UVC is 'in a loop', and is 'almost certain to be outside the body'. He says there is 'nothing unusual' in the appearance, and the diaphragm 'looks pretty clear', indicating a potential infection looks like it had improved. Professor Arthurs says it is difficult to gauge between one x-ray and the other, but it would be consistent with an improving picture for a baby in air throughout that time.
11:07am: A further x-ray image, taken at Alder Hey Hospital after Child D had died, is shown to the court. The UVC is still in, and a 'black line' just in front of the spine is a 'striking feature'. Professor Arthurs says "air is present" on what the court hears is the 'main highway' of the circulation.
11:10am: Professor Arthurs says the significance of that is that it is an "unusual feature in babies who have died without an explanation". He adds that amount of gas is consistent in babies who have died of sepsis, sudden unexpected death in infants, a road traffic collision, and two other babies in the trial. Another was Child A. He says one of the other explanations which needs to be considered is deliberate air injection. He says the most plausible conclusion was, in the absence of any other explanations, he considered they were 'consistent with, but [not] diagnostic of, deliberate air administration'. He confirms he has never seen this before in his experience.
11:12am: Ben Myers KC, for Letby's defence, is going to ask questions on the baby girl, Child D, first. He asks if it was correct that, at post-mortem stage, there were normal amounts of gas found in the normal areas, including in the bowel. Professor Arthurs agrees.
11:18am: Mr Myers asks about how often gases are found, post-mortem. Professor Arthurs says for a quarter of those cases of gases found in the post-mortem examinations at Great Ormond Street Hospital, there were gases found in the great vessels areas, for which there was an explanation of post-mortem gases. He adds if there is 'overwhelming evidence' of infection, that can lead to gases appearing there, or potentially gas being redistributed in the body during prolonged resuscitation efforts. He says administration of air is one of the explanations.
11:22am: Professor Arthurs is being asked about Child C. He agrees the left lung infection is a 'significant factor' from the first radiograph image. He says the second image has a possibility of gas in the bowel wall, which is a possibility of NEC. He says, as far as he knows, no NEC was found in Child C.
11:26am: Mr Myers says Child C, at four days old, did not have his bowels open, and a bowel obstruction could be considered.
11:30am: Professor Arthurs, asked by the prosecution about a bowel obstruction, says if the bowel was blocked at a particular point, it would give a 'marker' of where the obstruction was. He says the image shows no such marker, and as bowel obstructions are a 'common clinical occurrence', it would be diagnosed and babies would go to theatre for an operation. He says there is no evidence of a bowel obstruction on the imaging, on the clinical notes, or in an autopsy. Referring to the possibility of a twisted bowel, which he says 'can happen in small babies' and result in a blockage. He says that is often a surgical emergency, and would be documented as such, and found post-mortem if there is such a finding.
11:33am: That concludes Professor Arthurs's evidence at this stage.
11:50am: After a short break, the trial is now resuming with Dr Sandie Bohin being recalled to give evidence.
11:52am: Medical expert witness Dr Bohin is giving evidence on Child D, and confirms she has made a report on her, having had access to relevant medical reports and images from the Countess of Chester Hospital and Alder Hey, plus other medical experts. She confirms her role was to peer-review Dr Dewi Evans's conclusions from his report.
11:55am: Dr Bohin says there is now an advantage in delaying the cutting of the umbilical cord by two minutes, if the baby is in good condition, which is true in premature babies. However, if the baby is 'in extremis', the priority is on saving the life and cutting the umbilical cord immediately is the priority. Dr Bohin said the cord was cut for Child D after two minutes.
11:58am: She says Child D was in some respiratory distress due to 'grunting', which started when she was taken to the post-natal ward. It had been noted by the parents Child D was floppy and dusky in colour. Upon similar observations by medical staff, Child D was taken to the neonatal unit. Dr Bohin noted Child D was put on to CPAP with 40% oxygen, and during the night she had improved but was 'still not normal'. She tells the court there were still signs of respiratory distress for Child D.
12:03pm: Dr Bohin confirms she has noted what medical staff noted during their observations and records. She noted the skin discolouration observations for Child D at the time of the first collapse at 1.30am on June 22.
12:04pm: Dr Bohin says she would have been 'surprised' if an infection was the sole cause behind Child D's 'catastrophic collapse'.
12:11pm: The original cause of death, post-mortem, was 'pneumonia with acute lung injury', Mr Johnson tells the court. Dr Bohin explains, in her opinion, Child D's condition at birth was 'good', with good APGAR scores, and delayed cord clamping which would not have been done if Child D was not in a good condition. She says, upon the observation of Child D becoming 'floppy in her father's arms', she has had "First-time parents are desperately keen to have their baby with them - with skin-to-skin, which has a number of benefits." Dr Bohin says she means "no disrespect" to Child D's parents, who were first-time parents, that the father could have held Child D in such a way as the baby put their head on to the father's chest, "and that can collapse slightly, their windpipe."
"I see this fairly regularly...and with inflation breaths, the baby seems fine. "I cannot tell whether this was a clinical collapse, or [simply] an unusual position of the head."12:12pm: Dr Bohin notes the inconsistent temperatures for Child D showed sign of an infection, and Child D should have been screened at that point. It was when Child D refused to feed, that she was then, later, transferred to the neonatal unit.
12:16pm: Dr Bohin says newborn babies usually maintain their temperature quite well, but premature babies require more monitoring. Child D's temperature was low on arrival to the neonatal unit, but says the nursing staff 'probably overdid it' in increasing the incubator temperature, as Child D's temperature and heart rate rose to levels outside normal readings. Dr Bohin says the breathing rate was "high" and she required oxygen support. "Breathing at that rate is hard work for babies - rather than wait for them to be tired...it's much safer for the baby to intervene rather than wait for them to collapse."
12:17pm: The clinical picture for Child D was 'consistent with infection', Dr Bohin says, even if the x-ray image did not show that.
12:19pm: The second x-ray image showed 'a small patch of' infection in the lung. Dr Bohin says Child D, throughout June 21, was "well and stable". She required CPAP, but in air, and was "improving" despite having pneumonia as an infection, but was "getting better" with treatment.
12:20pm: Dr Bohin says, regarding the decision to begin feeds for Child D, indicates the baby girl was "stable" as feeds would not be administered if the child was not stable. She says all three collapses for Child D were "sudden" and "unexpected". "They came out of the blue...she recovered very quickly with the first two, and two of the episodes were associated with an unusual mottling of the skin. "They didn't have any clear cause."
12:21pm: Dr Bohin: "She seemed to recover very quickly after the medical team's intervention and she was well again."
12:24pm: Dr Bohin notes, for babies on CPAP, they will often find it uncomfortable as they will try fighting it. A baby who is "relatively well" will fight it. However, Dr Bohin said, in relation to one of the nursing notes: "The fact she [Child D] became upset then was a concern to me, as she had tolerated it well up to then." Dr Bohin says she believes the infection was acquired prior to birth, adding the initial administration of antibiotics was "late". Dr Bohin said the medical team knew Child D had an infection, but there was nothing to indicate she was at imminent risk of dying.
12:28pm: For pneumonia, Dr Bohin said babies would show a gradual deterioration, with declining blood gases, increased respiration rate, increasing ventilation support, abnormal blood parameters, and additional medication doses. "Taking into account the sudden nature of the collapses and the very quick recovery...I was very clear it wasn't infection, so the conclusion had to be something unusual and odd." Dr Bohin refers to the unusual skin condition medical staff observed. Other conditions were crossed off as they 'didn't fit'. She concludes the collapses were caused by intravenous air administration either through the UVC or the cannula. Dr Bohin says with air embolus, the speed and quantity of the air administered depends on whether it is fatal. She says the first two administrations of air would have been small, but the third would have been larger to cause circulation to stop.
12:29pm: Dr Bohin says the suddenness of the collapse, with skin discolouration, fitted with cases of air embolus, as did the presence of air found in the 'great vessels' on post-mortem x-rays.
12:31pm: Ben Myers KC, for Letby's defence, is now asking Dr Bohin questions. He says that 'in the absence of infection', there had to be 'something unusual and odd' found. Dr Bohin said she had looked at the clinical picture and had excluded the explanations more commonly found, which left the only conclusion as 'something unusual and odd'.
12:38pm: Mr Myers asks about the relevance for Child D being in distress. Dr Bohin said it was a possible explanation for that seen in adults, they can "be in distress after an air embolus." She adds there is very poor literature on this for neonatal babies, as there are few cases and little evidence of this. Mr Myers says Dr Bohin cannot apply to neonatal babies what has been seen in adults. Dr Bohin says neonatal babies don't have different biological systems, and a lot of the medicine relates to what has previously been done in adults. She adds Child D had been content with CPAP before, and her being in distress was a sign of concern.
12:46pm: Dr Bohin said Child D was taken off CPAP, following the second collapse, in case she was being distressed.
Mr Myers: "Are you just trying to find any evidence to support your air embolus conclusion?"
Dr Bohin: "No, absolutely not."
Mr Myers: "You just take any bits that you can find to support your diagnosis?"
Dr Bohin: "No, absolutely not." Dr Bohin adds, in relation to the skin discolouration, the rash observations noted by medical staff were like nothing she has observed for any neonate. She adds she was not there, but those observations by doctors and nurses were not ones she had found in neonates before. She adds she is not using skin discolouration alone as her diagnosis, but fits as part of a 'constellation of features'. She says such discolouration would be 'circular, with reddy-brown marks, which came and went', and not 'mottling'. She adds: "There is no single distinguishing feature of an air embolus."12:49pm: The 1989 medical journal review into air embolus is presented to the court, mentioning a particular case - 'blanching and migrating areas of cutaneous pallor were noted in several cases and, in one of our own cases, we noted bright pink vessels against a generally cyanosed...background."
"We have had many particular descriptions - they do not all conform to this, do they?"
"I think they're pretty similar."
"Nowhere in the clinical notes for any of the children in this, have we had [this description]?"
"We have seen reddy-brown patches on a background that is cyanosed, so yes, we have."12:51pm: Mr Myers says there is 'no uniform presentation' of the skin discolouration to mark it against. Dr Bohin says it is rare, so there isn't, and agrees that the 1989 medical journal is a reference to such evidence. She repeats the skin discolouration observations are "remarkably similar".
12:53pm: Mr Myers says there is no discolouration or distress in the third collapse.
Dr Bohin: "Discolouration doesn't [present itself] but there are other features which do." Dr Bohin says there was a catastrophic collapse and air present in the great vessels post-mortem. She says it was not just the rapidity of the collapse but the severity of it, and that she could not be resuscitated.12:59pm: Mr Myers says Child D recovered twice, which, in principle, is inconsistent with an air embolus. Dr Bohin disagrees, saying it depends on the speed and volume of the air administered. She said there is a treatment for air embolus. Mr Myers refers to air embolus experiments in animal testing, and asks how that can compare between animals and neonates. Dr Bohin said experiments are not done on monkeys any more, they aren't done on rats, but they are done on piglets as the biology is similar. Mr Myers says Dr Bohin refers to a medical paper in which testing is done on dogs and rabbits. "What basis do you have?"
"I have the basis in literature."
"Which is based on dogs and rabbits?"
"Yes." Dr Bohin adds it is not ethical to do such testing in humans.2:00pm: The court is now resuming the case following a lunch break.
2:01pm: Mr Myers resumes questioning Dr Bohin. He suggests Dr Bohin has disregarded or minimised 'certain facts that show how unwell [Child D] was'. Dr Bohin disagrees.
2:06pm: A nursing chart from June 20 is presented to the court at birth. Mr Myers says Child D was 'very unwell' at birth. Dr Bohin says she disagrees. Mr Myers refers to the note at 12 minutes, she was 'very unwell indeed'. Dr Bohin said she had 'an event' which required intervention, but it was not clear what her overall condition was. Mr Myers says she had referred to the father's handling of the baby as the cause of the event. Dr Bohin said that was one possibility, but not the only one. She said she was "very clear" the father was not responsible for the collapse, as new fathers are nervous with holding babies, and you cannot tell whether it was an obstruction or part of a clinical condition. Mr Myers says the mother had noted Child D 'looked lifeless' when the baby was presented to her. Dr Bohin said Child D had just been delivered, and the cord had not been cut. If a baby was 'in extremis', the baby would not have been presented to the mother, she tells the court.
2:10pm: Mr Myers refers to the nursing notes made in the hours following Child D's birth. Dr Bohin said it was clear, by the time of the neonatal unit admission, Child D had signs of an infection and was unwell. Mr Myers said the mother had referred to being "really worried" about Child D, being 'limp' and 'without colour - a bit grey, purple', making 'grunting noises', not 'responsive'. "That's a really poorly baby, isn't it, Dr Bohin?"
"That's the mother's interpretation, but I can't believe [the midwifery team] would have allowed...the baby to be fed or stay on the post-natal ward in that condition." Mr Myers says the midwife team did not administer antibiotics to Child D at this stage. Dr Bohin said that would have been a medical staff decision, not a midwifery decision, to administer antibiotics. She agrees antibiotics were not administered at that point.2:16pm: Dr Bohin says the low blood gas reading would be a concern, but would need to be put in a clinical context as part of a trend as part of the overall clinical picture. Mr Myers refers to a table of blood gas readings, and Dr Bohin says they have deteriorated as Child D was being moved off ventilator support on to CPAP. Mr Myers says Child D had an infection on June 21, and that was not a sign of a well baby. Dr Bohin said she was very clear Child D had pneumonia, but was on antibiotics and improving, and 'coping on CPAP' without needing to go on a ventilator. She agrees Child D did not manage well with being taken off CPAP, and was put back on. Mr Myers says 'the fact a baby desaturates like that...is a sign of poor health, isn't it?' Dr Bohin said the clinical team made a 'good judgment call' in attempting to take Child D off CPAP, as they cannot stay on CPAP forever, but it was 'perfectly acceptable' for her to be on CPAP and she was quickly put back on it.
2:18pm: Mr Myers refers to a blood gas reading at 1.14am on June 22 which he says is 'not normal' and a 'deterioration' on the one before. Dr Bohin says it is not as good as the one before, but is marginal, and needs to be taken in the overall clinical context. Mr Myers asks if Dr Bohin is sure she isn't trying to minimise such evidence as this in her overall findings.
Dr Bohin: "I'd like to make it clear my duty is to the court, to present my findings in an impartial way."2:26pm: Dr Bohin says the lack of antibiotics at one stage was a 'blip' in the care Child D had received, but she presented as a 'well' baby throughout June 21. Mr Myers says about the decision to take Child D off CPAP, after the second collapse, there would be a 'low threshold to intervene' if there were further desaturations. He says Child D desaturated again, and says that would have been a moment to increase ventilation support.
Dr Bohin: "Not necessarily." She said the doctor would have noted the overall clinical picture for Child D. Dr Bohin is asked if the decision to feed Child D was a 'bad decision'. She replies it was not a bad decision as the clinical position was stable. Mr Myers says the decision to take Child D off CPAP was a bad one. Dr Bohin says, given the clinical parameters, the decision to take Child D off CPAP was a right one to make.2:31pm: Mr Myers asks if Child D had respiratory difficulties throughout her life. Dr Bohin disagrees.
Mr Myers: "But she was on CPAP." Dr Bohin said Child D was stable on CPAP, and it was not possible to see how Child D was breathing unaided unless she was taken off CPAP. Dr Bohin adds she believed Child D died with pneumonia, not because of pneumonia. Mr Myers concludes by asking if Dr Bohin has been 'influenced' in making her conclusions rather than looking at all the facts. Dr Bohin disagrees.2:38pm: Intelligence analyst Kate Tyndall has now been recalled to court to provide the jury with a few corrections on their electronic bundle of evidence. A reminder that members of the jury are accessing the evidence for this case on iPads which contain evidence such as nursing notes, 'swipe data' for Countess of Chester Hospital staff entering and exiting the neonatal at certain times, details of medication, x-ray results and relevant text messages recovered from Lucy Letby's phone.
2:47pm: The court is now hearing evidence of police interviews conducted with Lucy Letby in relation to Child D. Nicholas Johnson KC says he is relaying a summary of the interviews. Letby, in her July 2018 interview, said she did not remember Child D. Looking through notes, she accepted she was in her care, but could not remember her. She said when administering medicine, two nurses would sign for medication, but it was not necessary for both of them to be present. In 2019, she denied administering Child D with an injection of air, and "didn't do anything" to Child D. Asked about the Facebook searches for Child D's parents, she said she could not recall making those searches. Asked about messages exchanged between Letby and a nursing colleague, she was asked why she had said Child D had 'overwhelming sepsis'. Letby says she could not recall, but thought from the context of the text, she thought Child D had been rescreened for infection. She was asked why, later that day, someone had said it could have been meningitis. She said she could not remember that being said to her.
2:48pm: That concludes the evidence for Child D at this stage, the court hears. The court hears the cases of Child E and Child F, twin babies, will be heard on the morning of Monday, November 14.
Monday 14th November 2022
Child E
Parents' testimony - Police analyst: Recorded events & messagesChester Standard Live Reporting
10:33am: The judge, Mr Justice James Goss, has entered the court. Members of the jury have now arrived in court, and the trial will resume.
10:34am: The mother of Child E and F is now giving evidence.
10:37am: She confirms she gave birth to identical twins in July 29, 2015 at the Countess of Chester Hospital. She had been expected to give birth in Liverpool Women's Hospital, but due to capacity reasons she was taken to the Countess of Chester Hospital. She believed the twins were in 'good condition for the gestation they were in' at birth.
10:38am: She said she had physical contact with the twins a few hours after giving birth to them, in the neonatal unit. She says she was only able to spend "a few minutes" with them due to their respective conditions.
10:41am: On July 30, she tells the court she was able to visit the twins in the neonatal unit, from upstairs in the post-natal wards. She said that would take about 5-10 minutes to get from one place to the other, due to having had a C-section, which made the journey time longer. She said she was able to cuddle Child E as he wasn't on CPAP, while Child F was on CPAP.
10:44am: She says she had decided she wanted to feed the twins her breast milk, and was helped to express that, and in the meantime had agreed to donor milk, but was able to provide her breast milk in due course as, she said: "That was very important to me."
10:45am: She confirms she expressed breast milk and dropped that off at the neonatal unit that day. She said: "It was the only thing I could do for them at that point. It was important to me. It was non-negotiable." She confirms she was given support by nursing staff to do this.
10:48am: She said Child E was progressing better, of the two twins, over July 30-31, but both were doing "really well" by August 1. She says she was keen to get home and was keen to transport both babies to a hospital closer to home, and was waiting for two ambulances to be provided. She said she and her partner were under the impression both babies were well enough to travel. By that stage, she had had skin-to-skin contact with both twins, and both were managing "fine". "We were never informed about anything to say they weren't fine."
10:49am: By August 2, the couple were still waiting for transport. She said on that day, the twins were both out of their incubators by this stage. Child E was breathing "easily" and Child F was "great". She says she does not remember any specific conversation about insulin production for the twins, but remembers it being mentioned, and that it was 'normal' for premature babies.
10:50am: By August 3, she said the twins were "great - doing really well". "We were absolutely thrilled that both boys were doing so well and we couldn't have asked for any more than that. They were both progressing."
10:53am: The father was commuting to and from the hospital at this time, and on August 3 he had gone home to "prepare the house" as it was "imminent" that the babies were going to be transferred to another hospital and she would be able to go home. She said he left the hospital at about 5pm. At that time, she was "having skin-to-skin contact" with Child E, which ended at "half past 6ish". She changed his nappy and had cleaned him, around the eyes and neck. She said she was still "sore and sensitive" but "over the moon" as her two boys were "perfect".
10:55am: She said she went up to the post-natal ward to express breast milk and have something to eat, 'between 7pm and 8.30pm'. She then took the expressed breast milk "straight down" to the neonatal unit where her twins were. She said she arrived there "a touch before nine o'clock."
10:58am: The mother had drawn a plan of the neonatal unit layout, as she remembered it, to police. That is now shown to the court.
11:00am: She tells the court she had gone into room 1, where the twins were, as was Lucy Letby, the only other adult in the room beside the mum. She said she could her her son crying and it was "like nothing I'd ever heard before". The mum walked to the incubator, to see blood coming out of Child E's mouth, and panicked as she "believed that something was wrong".
11:09am: Lucy Letby was at the workstation at the time, the mum tells the court. A video of the neonatal unit room one is shown to the court. The mum, fighting back tears, tells the court which incubators her twins were located in - both in adjoining ones. She said she heard "crying" - a sound which "shouldn't have come from a tiny baby. I can't explain what that sound was...horrendous. It was screaming more than crying." She said she heard it in the corridor in the unit itself, and entered the unit through the door where the twins were. Lucy Letby was "busy doing something, but she wasn't near [Child E]." She said she immediately went to Child E and used a 'containment technique' which she had been taught, to make him feel calmer, but "it didn't work". Child E "continued to make the same noise". She said she was there for "about 10 minutes" in that room. She said: "There was blood on his face, around his mouth."
11:11am: She tells the court she was asked by police to draw, on a drawing of a child's face, where the blood was coming from. She tells the court the blood was coming "around the mouth" Nicholas Johnson KC says it is 'almost like a goatee beard'. The judge asks for clarification, and the mum says the blood was 'a little above the lips, but mostly below'.
11:14am: The mum said she asked Lucy Letby why Child E was bleeding and what was wrong. She said Letby replied the feeding tube was rubbing the back of the throat and that would have caused the blood. The mum said she accepted that explanation, but was concerned about it. The mum said Letby "told her to go back to the ward", and she did what she was told as Letby "was in authority and knew better than me and I trusted her - completely."
"She said the registrar was on his way and if there was a problem, someone would ring up to the post-natal ward." She said she accepted that explanation and returned to the post-natal ward. Upon her return, she rang her husband as "she knew there was something very wrong".11:18am: "I knew I needed to speak to him, and tell him." The court hears the telephone records, including timings, were obtained. The call to her husband was made at 9.11pm, and lasted 4 minutes and 25 seconds. She said she rang her husband about her concerns, and remained on the post-natal ward. She returned to the neo-natal ward "later on that evening", sat in the corridor, watching a team of people around Child E's incubator. Mr Johnson clarifies this was at the time Child E was being resuscitated.
11:21am: In the time before that, the mum said she was "panicking", having conversations with the midwife, and was "panicking and waiting, waiting, following the rules". She said Letby had told her the rules to go back to the post-natal ward and wait for anything further. She was later told by the midwife and to ring her husband. The midwife called the husband at 10.52pm, telling him to come to the hospital, after the neo-natal rang the maternity ward. She said she does not know why the midwife rang, but assumed it was because she was "very upset" and "knew there was something wrong".
11:23am: The mum was taken to the neo-natal ward and the medical team were 'working on Child E' and were unsuccessful in their resuscitation attempts. She had contact with Lucy Letby after Child E had died. She tells the court she was asked if she wanted to bath Child E, but at that moment she did not feel able to. Fighting back tears, the mum says: "I was just...broken, and I couldn't. Lucy Letby bathed him in front of me in the neo-natal unit. "After he was bathed, he was placed in a white gown. "I just remember being thankful as we had no clothes for him as he was so little. "He was given back to us, and put in his incubator, and that is where he stayed."
11:28am: Mr Johnson asks if there was a potential post-mortem raised by one of the doctors. The mum says the husband asked a few questions and they were told by the doctor a post-mortem "wouldn't tell them much" more than what they had already been told by the doctor, and it would delay the transfer back home. "We just wanted to take him home." The mum adds they were given a "memory box" by Lucy Letby which "totally surprised" her and included a memory card, a lock of his hair, a teddy, hand/footprints. The mum said she was "so overcome with emotion" by that, as she had no other memories for Child E. Another teddy was provided, and the teddies were swapped, so Child F had Child E's teddy bear, and vice versa. Lucy Letby also presented a picture of Child F, having 'rolled over and cuddled the [Child E] bear', which she said was 'so amazing' so she had taken a picture to give to them.
11:29am: The mum tells the court she had written a card, with a picture of Child E and Child F on the front, expressing the parents' thanks for staff on the neo-natal unit.
11:31am: The mum tells the court, for Child F, he has never had any bleeding issues in his life.
11:32am: Ben Myers KC, for Letby's defence, expresses his sympathy for what the mum has gone through, and says that nothing he says will seek to minimise anything the mum did in caring for her twins. The mum confirms these were her first babies.
11:34am: The mum is asked if any of the times she said to the court were not correct, on her recollection, given she made a statement to police two years after the events. The mum confirms the time she went to the neo-natal unit on August 3, 2015 was correct.
11:35am: Mr Myers suggests the mum went down at about 8pm, at the time of the hand-over, and went down at about 10pm with the breast milk, and went again when Child E was being resuscitated. The mum says she "absolutely" disagrees with that.
11:37am: Mr Myers says, for that supposed 9pm time, the observations were the screaming and the blood coming out of Child E's mouth. The mum agrees. Mr Myers asks, for the crying, there were other staff about at the time. "At no other time did any other staff come into the room, did they?"
"No."11:39am: Mr Myers suggests the screaming was "not as bad as that [horrendous]." The mum says it was horrendous. Mr Myers asks about the blood seen. The mum says, other than around the chin, the other blood seen was above the lip, and no blood anywhere else, and the blood was "not coming out" or "going on the bedding".
11:42am: The mum agrees with her statement the blood was "not fresh". The mum says, and nods, it was blood. Mr Myers asks about the midwife seen. The mum says this was the first time she had seen this midwife, as there had been others seen, and she was "distraught". She said she was "distraught" and "knew there was something very wrong". She confirms the first name of the midwife, when asked by Mr Myers if the midwife was "Susan Brooks".
11:45am: The mum said she told her husband "there was something very wrong", cannot remember telling the midwife that, but said she was very upset at the time. Mr Myers says, for the 10.52pm phone call, she mentioned to her husband about the blood coming out of Child E. The mum says she does not remember the 10.52pm phone call as the midwife got in contact with the husband. Mr Myers suggests the mum was not as worried at the 9.11pm phone call as she was at 10.52pm. The mum says she disagrees with that.
11:48am: Mr Myers says he suggests the mum went with the breast milk as 'late as 10pm', that Lucy Letby never mentioned the tube was 'irritating Child E'. The mum disagrees with both those suggestions. The mum says she did not see anyone else at 9pm when she went to the unit. Mr Myers asks if there was a conversation between Letby, a doctor, and her, regarding medication. The mum says she disagrees, and said she was told by Letby the registrar 'would be down [to the neonatal unit room]', but did not make an appearance.
11:49am: Mr Myers asks about the resuscitation attempt. The mum says she could not see what was going on, other than several medical staff being present at the time. The mum says she is now aware there are bereavement procedures, such as memory boxes.
11:50am: Mr Myers asks about the discussion with the post-mortem was with a female doctor. He asks if it was because there was 'little point' in having one, according to the doctor. The mum says she felt 'persuaded' not to have one in that case.
11:54am: The mum is asked, by Nicholas Johnson KC, about the appearance of the blood on Child E. It was "stained - not dripping, smudged. It didn't look completely dry, but it was darker." She says it is "really hard to explain" the colour. It was "not bright red, it was darker than that. I don't know how else to explain that." That completes the mum's evidence. The father will give evidence shortly.
12:09pm: The father of Child E and Child F is now giving evidence.
12:14pm: He confirms the birth date for Child E and Child F. Mr Johnson asks about the progress on their twins. The father says he was "very happy" with the twins' progress before the phone call on August 3, they were doing "good". He confirms he had gone home on the evening of August 3, and then received a phone call from his wife that night. He tells the court the phone call he received from his wife at 9.11pm, wo was "upset and very worried" about the bleeding from the baby's mouth. He said he was sure the medical staff knew what they were doing, and she was panicking over nothing. The second phone call was split between the midwife and his wife. He was told: "Don't panic, but get over here now." Mr Myers asks if the bleeding was referred to at the 10.52pm phone call, rather than 9.11pm. The father replies it was not; that was referred to in the 9.11pm phone call.
12:16pm: That completes the father's evidence. Nicholas Johnson KC says the court will now go through the sequence of events, with intelligence analyst Claire Hocknell directing the jury through the electronic evidence bundle for Child E and Child F. A reminder the jury have access to the evidence in this case on iPads, rather than the traditional paper bundles.
12:19pm: The first evidence refers to text messages sent to and from Lucy Letby's phone on July 27, asking if Letby, on her time off, will be back in time for a debrief regarding the death of Child A. Letby says she will be looking to get back in time for that.
12:21pm: Child E was 1.327kg at birth (2lb 14oz), with APGAR scores of 7/10 at 1 minute and 9/10 at five minutes (APGAR scores recording how well a baby is presenting in the minutes after birth). Clinical notes refer to the admission of the twins to the neonatal unit.
12:27pm: The debrief for Child A takes place on July 30, with Letby having confirmed her attendance in a text message prior. Letby is then the designated nurse for Child F on the night shift of August 1 and August 2. Melanie Taylor was the designated nurse for Child E on the night of August 2. Melanie Taylor's notes record for Child E for that night shift: "Self ventilating in 24% oxygen, resps 6-70, minimal recession evident."
12:31pm: A message sent from nursing colleague Jennifer Jones-Key to Lucy Letby at 10.34pm on August 2 says: "Hope work ok".
Letby replies: "...yeah it's fine, bit too Q word really."
The reply: "Don't complain as Wed and Thurs horrible lol! It will pick up again."12:37pm: The court is shown further nursing notes by Melanie Taylor recording two Brady desats (slow heart rate) at the early hours of August 3, requiring 'gentle stimulation' to correct. One of the Bradys is recorded as lasting 45 seconds. Child E's tummy was 'soft, not distended', had satisfactory blood gas readings and heart/respiratory rate, and fluids were being administered. The bowels were not yet opened.
12:40pm: Melanie Taylor's notes at the end of the night shift said 'feeds tolerated, tummy remains soft'. A family communication note is also made by the nurse. "Mum and dad visiting at start of shift, mum has been 2x with [expressed breast milk] overnight."
12:43pm: A 'Kangaroo care record' is presented to the court, documenting the times when the parents were able to have physical contact for Child E, and how long it lasted, and how well it was tolerated. A nurse's record notes for that day that mum 'had long periods of skin to skin [contact]'.
12:48pm: The note records, at 10.44am, Child E was 'self ventilating in 25% ambient oxygen. No signs of respiratory distress...pink and well perfused....handles well. Caffeine given as prescribed.' A doctor's note at 11.45am on August 3 records Child E has 'suspected sepsis', 'hyperglycaemia', and was 'off lights' for jaundice, with 'good gases'. Child E was 'tolerating well' expressed breast milk. The baby boy was 'not examined at present as having cuddles with mum'. The plan was to 'examine later' and increase feeds. Aspirates were 'ok'.
12:50pm: Dr Emily Thomas made clinical notes at 2.10pm on August 3, noting: 'examination of [Child E] as having skin to skin on [ward round earlier that day]. Good tone and movements, handling appropriately throughout the day.'
12:56pm: Child E was placed on a small dose of insulin, given via infusion.
12:58pm: A nursing note at 5.24pm said Child E was 'self ventilating in air', blood gas reading was 'satisfactory', and feeds were increased.
1:00pm: At 7.30pm, Dr Emily Thomas made clinical notes, with a CRP reading less than 1, Child E was on 23% oxygen, and antibiotics were 'likely to stop at 36 hours as improving'. A series of other observations are made.
2:07pm: The trial is now resuming, following a lunch break.
2:10pm: A shift handover for August 3, 2015, the night shift, is shown to the court. Letby is named as a designated nurse. Letby is the designated nurse for both Child E and Child F in nursery room 1 that night. The list shows three babies in room 2, one in room 3, and four in room 4. There is also a baby in the transitional care unit.
2:12pm: Letby's note for 8pm at August 3 is written, written at 4.51am retrospectively, to say: "Mummy was present at start of shift attending to cares."
2:16pm: A further Letby note reads: 'Prior to 9pm feed, 16ml 'mucky' slightly bile stained aspirate' recorded for Child E. The neonatal fluid chart for the 9pm column records, under milk feeds, 'omitted', and the word 'discarded' is in a non-specific line. For aspirates, the note '16ml mucky' is made. To the right of that, at the 10pm column, is '15ml fresh blood' on aspirates. The two columns for that chart are signed by Lucy Letby's initials.
2:17pm: The phone records showing the calls made from Child E and Child F's mum to the father are also shown, including calls at 9.11pm and 10.52pm.
2:19pm: An observation chart is shown for Child E. The 'cares' row has one tick, recorded at 7pm, signed by Letby's colleague from the day shift.
2:25pm: Dr David Harkness records readings from 9.40pm, written at 10.10pm, 'asked to see patient re: gastric bleed'. Large, very slightly bile-stained aspirate 30 mins ago.' 14ml of blood vomit is also recorded. Letby records: "At 10pm large vomit of fresh blood. 14ml fresh blood aspirate obtained from NG tube. Reg Harkness attended. Blood gas satisfactory..." Child E was 'handling well'. Letby's further note: 'Mum visited again approx 10pm. Aware that we had obtained blood from his NG tube and were starting [treatment]...' Dr Harkness noted Child E was 'alert, pink, well perfused', with an abdomen which was 'soft, not distended' and no bowel sounds. The note adds 'G I [gastrointestinal] bleed ? Cause'
2:28pm: A neonatal fluid balance chart is shown to the court, with no name or notes for the 11pm column. Letby's retrospective nursing notes said: 'NG tube on free drainage. Further 13mls blood obtained by 11pm. Beginning to desaturate and perfusion poor. Oxygen given via Neopuff'. Child E was said by Letby to be 'cold to the touch' and was beginning to 'decline'. Dr Harkness noted '13ml blood-stained fluid from NGT on free drainage.' Child E's blood pressure was 'stable' and saturates' remained 60-70%', and 'making good respiratory effort', and was 'crying'. A plan of action, including x-rays and medication, was made.
2:30pm: A note for 11.30pm on the observation chart has no record of a heart rate made, and blank readings for cot temperature, and no initials recorded. Blood pressure and respiratory rate are recorded.
2:33pm: Child E then collapsed at about 11.40pm. Letby recorded, retrospectively: "11.40pm became Bradycardic, purple band of discolouration over abdomen, perfusion poor, CRT 3secs. "Emergency intubation successful and placed on ventilator..." Dr Harkness records, in clinical notes at this time, written retrospectively, 'Sudden deterioration at 11.40pm, brady 80-90bpm, sats 60%, poor perfusion, colour change over abdomen purple discoloured patches'. The note adds, after an improvement in sats, 'purple discolouration in abdomen remained', and a plan of action noted for Child E.
2:35pm: Further notes by
Letby: 'Required 100% oxygen, saturations 80%, SIMV 22/5 rate 60. Further saline bolus and morphine bolus given. 2nd peripheral line sited..."
"Once [Child E] began to deteriorate, midwifery staff were contacted." The latter note is written, retrospectively, at 4.51am.2:41pm: A further observation reading for Child E, made by Letby, is taken at 12.15am, with a heart rate 'down from where it had been earlier', and a drop in temperature, recording he was on 100% oxygen. A consultant paediatrician arrives at the neonatal unit at 12.25am. An x-ray is taken at 12.27am, relating to the chest and abdomen. A further, 'acute deterioration' for Child E, is noted by Letby at 12.36am. 'Resus commenced as documented'. The consultant paediatrician noted CPR commenced, along with ventilations, and medications.
2:48pm: A blood transfusion is started for Child E at 12.50am, and several adrenaline doses are administered. Letby's note, for 1.01am, reads 'chest compressions no longer required'. For 1.15am, Letby notes 'further decline, resus recommenced'. CPR was discontinued at 1.23am - 'resus discontinued when [Child E] was given to parents. [Child E] was actively bleeding...' The time of death was recorded as 1.40am on August 4.
2:50pm: Letby's note: 'both parents present during the resus. Fully updated by nursing and medical team throughout. Parents wished for [Child E] to be baptised.... Child E was bathed by myself and photographs taken as requested, both were present during this. Consent obtained for [hair] and hand/footprints... Both distraught...'
2:52pm: The official documented report for the incident is made by Letby - 'unexpected death following gastrointestinal bleed. Full resus unsuccessful'.
2:54pm: A 'checklist for staff following neonatal death' is presented to the court, for Child E. It records what levels of 'emotional support' were offered to the parents. Letby noted at 8.21am 'Parents resident on unit overnight. Wish to be left alone'.
3:14pm: A series of text messages to and from Letby's phone are shown to the court.
3:17pm: Ben Myers KC asks to clarify that the nursing notes made, which have been gone through in 'broken up parts' in the sequence of events, are actually made of larger notes. The intelligence analyst agrees. Mr Myers also refers to the sequence of events showing Letby searched for the mum of Child E and Child F several times on Facebook in the weeks and months after Child E died. He asks if it is correct Letby also searched for the names of parents who are not part of this case. The intelligence analyst agrees.
3:31pm: The text message sent from a colleague of Letby to Letby's phone at 8.58am on August 4 says: "You ok? Just heard about [Child E]. Did you have him? Sending hugs xx" Letby responds: "News travels fast - who told you? Yeah I had them both, was horrible." The colleague responded that she had been informed by someone at the handover 'told me just now'. 'Had he been getting poorly or was it sudden?' Letby responds Child E had a 'massive gastrointestinal haemorrhage'. The colleague said Child E 'had always struggled feeding'. Letby responds that Child E was 'IUGR [Intrauterine growth restriction] and REDF [Reversal of umbilical artery end-diastolic flow]' and believed Child E was 'high risk'. She added: "I feel numb".
3:38pm: At 7.55pm, Jennifer Jones-Key messaged Lucy Letby: "Hey how's you?" Letby responds: "Not so good, we lost [Child E] overnight." The response: "That is sad. You are on a terrible run at the moment. Were you in [room] 1?"
Letby: "I had him and [Child F]"
Ms Jones-Key: "That is not good, you need a break..."
Letby: "It's the luck of the draw...unfortunately."
Ms Jones-Key: "You do seem to be having some very bad luck..."
Letby: "Not a lot I can do really - he had a massive haemorrhage, could have happened to any baby really." Ms Jones-Key says Letby "did everything you could", adding she had seen a haemorrhage in babies before, and was 'horrible' to see.
Letby replies: "This was abdominal", and she had previously only seen pulmonary.3:44pm: On August 9, at 10.17pm, Letby messages a colleague saying she had said goodbye to the parents of Child E and Child F, and said they had cried and both hugged her, saying they would never forget the care the staff provided. The colleague responds: "It's heartbreaking, but you have done your job to the highest standard with compassion and professionalism." The colleague added: "You should feel very proud of yourself." Letby responded she felt sad after what had happened. The colleague adds: "They know everything possible was done" and was in Child E's "best interests".
3:50pm: The court is shown evidence that Letby searched for the mum and dad of Child E and Child F on Facebook nine times in the following months, the vast majority for the mother. The first of the searches was on August 6 at 7.58pm, and one of the searches is at 11.26pm on December 25. The final two searches were made in January 2016, the last on January 10 at 11.03pm.
Tuesday 15th November 2022
Child E
Statement of Midwife Susan Brookes - Dr Christopher Wood - Nurse B - Statement of Nurse Caroline OakleyChester Standard Live Reporting
10:38am: There has been a slight delay in resuming the trial today. It is currently expected for the case to resume at 10.45am.
10:52am: Members of the jury are now coming into court, and the trial will resume.
10:53am: The judge, Mr Justice James Goss, says "travel difficulties" have caused the delay this morning for the court.
11:01am: Agreed evidence is now being read out by prosecutor Simon Driver. A statement by Susan Brookes is read out, dated April 2, 2019. She was a registered midwife at the Countess of Chester Hospital in August 2015. She said there would have been two midwives working that night shift. She said her responsibilities included making sure the mother was well and providing emotional support when needed. Her 'midwife notes' are presented to the court, showing the mum of Child E was 'post-natal well', and one of the twins had 'deteriorated slightly'. At 11.30pm on August 3 she had a call from the neonatal unit to ask Child E's mother to go down in 30 minutes as Child E had a bleed and required intubating - 'very poorly'. She said the mum was very upset and she thought the 30-minute was 'unreasonable' and asked to go sooner. At midnight, the midwife stayed with Child E's mother for 10 minutes in the corridor outside the neonatal nursery room where Child E and Child F were, and the mum was eventually allowed in once medical staff had stabilised Child E.
11:05am: Dr Christopher Wood has now been called to give evidence. He confirms that in August 2015, he was on a four-month trainee placement at the Countess of Chester Hospital, as part of his GP training, and was present at the birth of Child E and Child F. After assisting with the delivery, he did not have contact with the twin boys until the night of August 3-4. He said he was on call, primarily on the paediatric unit as it was an area where he was "more comfortable", but would be called to the neonatal unit if needed. He was the more junior doctor to the other one present that night, Dr David Harkness.
11:07am: He said he was called to the neonatal unit as part of a crash call, having been in the doctors room in the paediatric unit, writing up notes.
11:13am: He says he didn't recall being on the neonatal unit that night, prior to the crash call at 11.40pm. He confirms signing for a prescription of morphine bolus for Child E. Dr Wood says he would have had very little experience of intubating babies, so he would have done the prescription as a formality. The accompanying medical note by Dr Wood says 'Sats 60-70% Morphine bolus - sats improved to 80%'. He recalls he immediately attended upon notification of the crash call. He said a number of people were ready, and resuscitation attempts had already begun upon his arrival. He said the best thing to do was do other jobs while more experienced members of the team did more specialised aspects of the resuscitation. He recorded notes and made sure things weren't missed.
11:20am: Dr Wood had made a note of staff present during the resuscitation - a team of six, including himself, Dr Harkness, a further doctor, and three senior nurses including Lucy Letby. Clinical notes made by Dr Wood record the efforts to resuscitate Child E from 12.37am. Five doses of adrenaline are administered during the efforts. While chest compressions stop at 1.01am, with ventilations continuing, Child E's heart rate fell again at 1.15am and CPR recommenced. At 1.23am, CPR stopped and Child E was cleaned. At 1.24am, ventilation [efforts] stopped and Child E was given to the parents.
11:24am: A pathology report is shown to the court, showing Child E with 'relevant clinical details: GI bleed'. Dr Wood says he cannot recall details surrounding this. Ben Myers KC, for Letby's defence, says Dr Wood was split between the paediatric and neonatal wards. He says Dr Wood had 'very little experience with neonates'. Dr Wood agrees. Mr Myers asks if this was Dr Wood's last night shift with the Countess. Dr Wood says he believes the following night was his last one.
11:27am: Mr Myers says if you lose a significant quantity of blood from a neonate, that would be different from an adult losing a significant quantity of blood, as there could be time to 'seal a gastric bleed' in an adult. Dr Wood agrees. A clinical note is shown with 'plan - discuss with surgeons, with x-rays'. Mr Myers asks if Dr Wood was aware surgeons were at the Countess of Chester Hospital who were capable of performing gastric surgery on neonates of the size of Child E. Dr Wood: "I'm not aware of that. I would imagine most [likely] this would be Alder Hey [Hospital in Liverpool]."
11:28am: Mr Myers says, for the birth, there were 'potential complications' for the twins. Dr Wood agrees. Mr Myers says the doctors for the neonatal unit were shared with the maternity and paediatric units, and their duties were split. Dr Wood says that was the case, but the doctors would normally be assigned a specific unit per shift.
11:31am: Mr Myers refers to the night of August 3. Dr Wood confirms he was the only senior health officer covering paediatrics and the neonatal unit, with Dr Harkness the only registrar covering those units that night. Mr Myers asks if Dr Wood recalls at 9-10pm, receiving a report of a bile-stained aspiration on the neonatal unit. Dr Wood says he doesn't recall - he doesn't remember. Mr Myers asks if doctors would receive news of such reports from the neonatal unit. Dr Wood says he probably would not have received a call from the registrar to him about it. He adds he was on the paediatric unit by himself, and it was his understanding that, therefore, Dr Harkness would have been on the neonatal unit 'at some point during the evening'.
11:34am: Mr Driver rises to ask about the bile-stained aspirate via a phone call. He asks in Dr Wood's capacity as a GP trainee, if he had received any data/information about a neonatal unit patient, what he would have done. He replies if he had received a call from a nurse, he would have taken action, and if it was from a registrar, it would have most likely been out of courtesy. In the former case, he would have recorded it in his notes and would have sought advice from the registrar.
11:59am: The trial has had a short adjournment, and is now resuming. The next witness to give evidence is a nurse who cannot be named due to reporting restrictions.
12:01pm: The Countess of Chester Hospital neonatal nurse has previously given evidence earlier in the trial. She has returned to give evidence in the case of Child E.
12:08pm: She confirms she was the designated nurse for Child E during the day of August 3 (8am-8pm), as well as the designated nurse for Child F. She made a note at 10.42am, regarding family communication: 'mum on unit from 9am onwards, fully updated by myself and reg. Had long periods of skin-to-skin.' The nurse said she recalled the skin-to-skin contact, and during this shift, Child F was unable to have a 'cuddle', but 'containment holding' instead. Child F remained on CPAP (a level of respiratory support), and was not as stable. Child E was breathing by himself, requiring a little supplementary oxygen, and therefore 'could have as many cuddles as they [the mum and Child E] wanted'.
12:15pm: Child E was, in the nurse's 10.50am 'top to toe' clinical note: 'self ventilating in 25% ambient oxygen, no signs of respiratory distress. Heart rate and temperature stable. Pink and well perfused. Cap refill 1 second'. The observations were 'normal'. The nurse added the fluids which were being provided, via a longline infusion. Child E was on a 'cautious feeding regime', based on guidelines in the neonatal unit. Child E, it was also noted, 'handles well'.
12:17pm: A 'minimal to 1ml partially digested milk' was obtained from the NGT aspirates, which the nurse says was normal, and was a sign Child E was digesting the milk being fed.
12:24pm: The nurse's addendum is made, retrospectively, at 5.24pm that day. A CRP reading was 'less than 1', which the nurse explains any reading of less than 10 is 'a good sign'. The antibiotics would 'be reviewed at 36 hours [treatment]'. The blood cultures were 'currently negative' - in absence of bacteria. Child E remained self ventilating in air, with 'satisfactory' blood gas readings. The nurse says Child E had a blood sugar reading of 18.5mmols, which was "too high". A doctor was informed and insulin was 're-commenced at a rate of 0.02/units/kg/hr'. Feeds were increased as Child E was 'tolerating his feeds'. The court hears a 'PKU' was taken with parental consent, which was a neonatal blood screening taken from every baby at about Child E's age [if the parents agree], looking for various potential [inherited] conditions, with results to follow.
12:29pm: An observation chart is shown for Child E, from 6pm on August 2 to 5pm on August 3. The respiratory rate, the court hears, is 'normal', and the baby boy was said to be stable. A second observation chart is shown with the nurse signing for readings at 6pm and 7pm. The nurse agrees with Mr Driver the observations show "stable trends" for Child E.
12:32pm: Mr Driver asks about the blood sugar readings. The nurse says she found that level in a blood gas reading, which was 'outside the parameter' so consulted a doctor, and action was taken following guidelines for insulin to be commenced.
12:37pm: The blood gas reading chart is shown to the court, which shows the nurse took the sample for Child E at 2.38pm on August 3. The glucose reading of 18.4 was the only 'abnormal' reading recorded, the court hears.
12:41pm: The neonatal fluid balance chart for Child E on August 3 is shown to the court. The nurse explains the milk levels given to Child E that day. The aspirates recorded 1ml partially digested milk at 9am, which was 'replaced [in the NG tube] as [Child E] had worked hard to digest that milk', as 'normal practice'. The nurse explains the 1ml milk was taken out, put back in, and a 1ml additional milk feed was administered.
12:44pm: Minimal aspirates' are recorded for 11am and 1pm, with a 'moderately high' level of urine recorded at 1pm. Minimal aspirates are recorded at 3pm, with 1ml aspirate at 5pm. That was a 'normal finding' and was replaced. At 7pm, another 'minimal aspirate' is recorded. At 7pm, there was also urine recorded, and a sign Child E's bowels had opened by this time. Asked for the assessment of Child E, the nurse says: "[He] was doing well on that shift, apart from the high blood sugars. It can be a worrying factor, it could be a stress response."
12:48pm: Ben Myers KC, for Letby's defence, asks about Child E's condition on August 3, that he was 'doing well for a baby of that gestation', except for the blood sugar reading. He asks if the nurse was aware of a number of risk factors associated with him. The nurse agrees, and agrees Child E was premature, and there were risks associated with that. She says she would have also been aware of risks of twin births, and agrees with Mr Myers Child E 'could be vulnerable to health complications'.
1:00pm: Mr Myers asks about Child E's first shift involving Child E on the night of July 29-30, referring to the nurse's note at 12.17am: 'NCPAP commenced at 10.50pm as oxygen requirement increased to 30% and required Neopuff x2 for apnoea.' A chart is also shown of Apnoea/Bradys, recording five such incidents for Child E between August 1-3. Mr Myers says, talking through the chart with the nurse, one Brady happened at August 1, no apnoea is identified, but heart rate dropped to 79bpm and desat reading was '84', and the duration was 45 seconds. That is confirmed by a separate doctor's note, which required 'gentle stimulation' to resolve. The second desat happens on August 2 at 6.20am, with a reading of '83-88', lasting two minutes. The nurse says gentle stimulation is putting a hand on the abdomen gently, or very carefully giving the baby a light tickle. She says if the situation does not improve, the baby's chin would be placed into a neutral position to help the airway, and/or administer oxygen. This episode required, according to a nurse's note, 'facial oxygen was required for a short period - had hiccups at the time'. The third was a brady and a desat for 30 seconds, which was 'self-correcting'. The fourth was a Brady and desat at 11.50pm on August 2, lasting 45 seconds, requiring gentle stimulation to resolve. The fifth and final episode was at 1am on August 3, with brady and desat in the '70s', lasting 45 seconds, requiring gentle stimulation to resolve.
2:04pm: The trial is now resuming following a lunch break.
2:09pm: Ben Myers KC is continuing to ask the nurse questions. The fluid chart is shown to the court once more for Child E on August 3. Mr Myers asks about the blood glucose readings, and what the parameters should be. The nurse says the readings should be above 2.6, and the upper limit is not defined in pre-term babies (Mr Myers says the upper limit is 6 for full-term babies). The nurse says it would be a worrying sign. Mr Myers asks if the reading of 18.4 is 'worryingly high'. The nurse agrees. She says the cut-off point for insulin to be prescribed would either be '12 or 14'. She agrees the blood sugar readings of 12.8, 18.4, 13.5, 12.9 are 'at the higher end of normal', with '18.4' being 'particularly high'.
2:15pm: A chart showing a form of insulin - Actrapid - is administered on several occasions to Child E. The first is on July 31 at 6.45am, and the rate of insulin administration lowers at 2pm on August 1 and is increased slightly again at 2.10am on August 2. A prescription for 3pm on August 3 is made, but then crossed out, then redone with 'a correct dose'. The nurse says the previous, crossed out one, was 'an incorrect dose' of 0.05units/kg/hr. The second is the 'correct dose' of 0.02units/kg/hr. Insulin of a neonatal is a "continual infusion", the nurse tells the court.
2:18pm: Mr Myers says the insulin administration is 'a feature' of Child E's treatment during his time at the neonatal unit. The nurse agrees. The blood gas chart for August 3 is shown, with the nurse having signed a blood gas reading taken at 2.38pm. Mr Myers suggests the pH reading of 7.293 is outside the normal range of being under 7.3, by being slightly acidic. The nurse says she was trained that anything above 7.25 was normal.
2:19pm: Mr Myers suggests that the blood gas readings suggest a case of acidosis. The nurse says the readings taken are within the parameters, and the doctor would, in any case, make the decision.
2:22pm: Mr Driver, for the prosecution, rises to ask a matter of the brady and apnoea chart, which recorded five episodes with Bradys and desats. The nurse did not record any of these episodes. He asks if the episodes recorded on August 1-3 would lead the nurse to adjust her opinion of Child E's stability/well-being. The nurse says the chart is "not a worrying trend of information".
2:30pm: Mr Driver asks if the insulin prescription are four separate doses, or one continuous administration. The nurse says the first dose is administered at July 31, 6.45am, and that dose remains unchanged until 2pm at August 1, and the dose is reduced. It would be the same infusion, via a syringe of diluted sodium chloride, administered via a computer. The court hears the insulin would be paused in the event of the syringe being emptied or the insulin expiring, and a replacement dose would have been prescribed prior to that.
2:44pm: Mr Myers asks further about the insulin dose. The nurse says, for the dose she administered, that was a fresh solution. The previous one, the notes the previous dose was administered from 2.10am on August 2. The judge asks if that dose of insulin would have ended after 12 hours, as the insulin would expire thereafter. The nurse says you would have to check the relevant nursing notes for that. She can only say to the court the insulin dose she administered at 3pm on August 3 was a fresh dose, and Child E had not been on insulin.
2:45pm: The next evidence is an agreed evidence statement from nurse Caroline Oakley, who was shift leader on August 3, and was involved in the resuscitation efforts for Child E, but does not recall who was doing what, as it was a team process. She adds she does not recall attending a debrief for Child E following his death.
Wednesday 16th November 2022
Child E
Dr C - Unnamed nurse10:35am: I’m in Manchester for the continuing trial of nurse Lucy Letby.
10:43am: The court is hearing from a consultant paediatrician [Dr C] who was on duty when Babies E and F were on the neonatal unit. Court orders mean we can’t name the alleged victims or this doctor. Nurse Letby allegedly murdered Child E and allegedly attempted to murder his twin F.
10:53am: [Dr C] was on call in hospital accommodation on the night Baby E became ill. She’s recalling telephone discussions with a junior colleague who was treating E. The junior doctor’s notes concern 2 incidents when E had blood loss from his mouth and had a fall in blood oxygen.
10:58am: [Dr C] says the notes show on the 2nd occasion Baby E’s blood oxygen level stayed at 60-70% despite being given 100% oxygen. “This suggests something dramatic has changed in their clinical condition.” 1/2
10:59am: “It suggests there’s not a problem with his breathing effort that’s making his oxygen saturation low.” 2/2
11:06am: It’s alleged that Nurse #Letby murdered Baby E by injecting air into his blood. She denies this, as she denies all the charges she faces.
11:09am: When the consultant [Dr C] got to the neonatal unit E’s blood oxygen level was 80% in 100% oxygen. “They’ve improved since ventilation but they’re still not as good as we would like them to be.”
11:12am: An x ray showed E’s heart size was normal and his lungs were clear. “There’s no indication from the X ray why E’s saturation was low” says the consultant.
11:19am: 11 minutes after [Dr C] arrived at the neonatal unit her notes say E’s blood oxygen had fallen to 50-60% in 100% oxygen and he had “no detectable [heart rate]”, so CPR was started.
11:23am: The consultant was the team leader for resuscitation efforts for Baby E. She says she wouldn’t get involved in the physical tasks because you “lose awareness of the overall situation.”
11:36am: [Dr C] says her notes “[don’t] tell me anything about what caused the collapse, just that [E] is extremely poorly.”
11:38am: Resuscitation efforts for E were not successful and CPR was stopped. The notes say he was “transferred to Mum and Dad for cuddles”.
11:43am: [Dr C] says at the time she thought E’s cause of death was necrotising enterocolitis (NEC), where part of the bowel becomes inflamed and may die. It occurs in newborns who are premature or otherwise unwell.
11:49am: She thought this because E was an at risk baby, he had gastro-intestinal bleeding and he had skin discolouration. She agreed with the coroner that that she be put as his cause of death. But she now says she doubts he had NEC because …
11:53am: …”[E’s] observations were stable right up to the point of collapse” and that’s not what happens with NEC, where deterioration is normally slower. There was also no sign of NEC on the X ray….
11:56am: “I don’t think I gave that enough weight at the time, that the X ray was normal.” [Dr C] says she didn’t push the idea of E having a post mortem because his parents were so upset, “which is now something I regret.”
11:59am: [Dr C] is now being cross examined by Ben Myers KC who’s defending Nurse #Letby. She agrees with him that as a premature baby E faced specific problems.
12:02pm: She also agrees with Mr Myers that a condition E and his twin F had where they shared a placenta can increase risks for them. Those risks can include NEC. Dr agrees E was at high risk for a number of conditions.
12:04pm: In a police statement in Nov 2018 [Dr C] said she discussed with a colleague that E had “an unusual deterioration but in a high risk baby that was not entirely unexpected.”
12:09pm: Mr Myers says E’s blood glucose levels were high during his time in hospital were high and this can mean baby is labouring under stress. The doctor agrees but says they’re not unusual in babies like E.
12:14pm: When Mr Myers suggest again suggests that Baby E was at risk because he was less robust physically, the doctor says “His deterioration was well outside what we would expect.”
12:24pm: Mr Myers suggests that the notes show that although E lost blood and fluid there was no discussion, as there should have been, of replacing fluid or transfusing blood. [Dr C] says though it’s not in the notes, blood transfusion was discussed.
12:30pm: Mr Myers suggests [Dr C] (who was on call) should have gone to the neonatal unit sooner than she did to treat E. “With hindsight I should have attended but I don’t think I would have made any different decisions [from the doctors who were at the unit]”.
12:31pm: Mr Myers: “You should have been there.” [Dr C] “Yes.”
12:35pm: The consultant disagrees with Mr Myers when he suggests the Countess of Chester neonatal unit was “too slow” to intubate* E. (* where a tube is inserted into the windpipe to aid breathing).
12:47pm: Mr Myers suggests the consultant is “minimising the impact of a late blood transfusion” for E. [Dr C]: “I am minimising it as I don’t think a late blood transfusion led to [E’s] collapse and death.”
12:56pm: Mr Myers says [Dr C] should have ensured that Baby E had a post mortem. She says “I apologise to them [E’s parents] that I didn’t push for that.”
3:08pm: Court now hearing from a nurse who worked on the neonatal unit at the Countess of Chester in 2015. She’s telling the jury about how nurses administered various drugs and treatments to the babies on the unit.
3:32pm: The nurse agrees with Ben Myers KC, defending, that neonates can sometimes deteriorate rapidly, and that sometimes they can deteriorate when they’d appeared quite stable. When asked if it follows that such babies can die she says “sometimes”.
3:37pm: Nurse agrees with Mr Myers that at the time some aspects of the neonatal unit at Chester were “quite old”. “Plumbing and drainage would not function as you would have expected.” The nurse says “correct”. Also agrees “at times” it was difficult to get hold of doctors when needed.
3:49pm: Court has ended for the day and will resume tomorrow. I don’t think I’ll be here, but my colleague @Tom_Mullen will keep you up to date. I’ll have a report on today’s proceedings in @bbcmerseyside at 1720 and on at 1830.
Chester Standard article 16-11-2022
A DOCTOR [Dr C] has apologised in court for not "pushing" for a post-mortem examination of a baby boy allegedly murdered by Countess of Chester Hospital neonatal nurse Lucy Letby.
Letby, 32, is said to have administered a fatal amount of air into the bloodstream of the infant while he was being cared for in the neonatal unit.
The death of the premature-born twin, referred to as Child E, was the fourth baby murdered by the defendant in a six-week period, according to the prosecution.
During her evidence on Wednesday, November 16, a consultant paediatrician – who cannot be identified for legal reasons – turned from the witness box to Child E's parents sitting in the public gallery and made her apology.
The doctor was the on-call consultant when Child E deteriorated rapidly late on the evening of August 3, 2015 and died in the early hours of the next day.
Jurors heard that necrotising enterocolitis (NEC) – a serious gastro-intestinal disorder – was entered as the cause of death on Child E's death certificate.
The doctor told the court: "At the time I felt (Child E) had NEC which had led to his collapse and deterioration so I discussed that with the coroner and we agreed for that to be put as (Child E's) cause of death."
She said the infant was a "high-risk baby" and also took into account a colleague's observations of gastro-intestinal bleeding and abdominal discolouration.
Prosecutor Simon Driver asked: "Any clinical factors that militated against that conclusion?"
The consultant replied: "I considered them fully at the time but the fact that (Child E's) observations were very stable up to the point of collapse does not normally fit with NEC.
"And the abdominal X-ray not showing any signs of NEC over an hour before he died – I don't think I gave that enough weight at the time; that the X-ray had been normal."
She told the court she now did not think NEC was the cause of death.
The doctor went on: "A post-mortem would take place if we didn't feel we had a cause of death. It can be requested for any baby who dies if the parents want that investigation.
"The parents were understandably devastated that Child E had died and were not keen on a post-mortem and I didn't want to make a terrible situation any worse so I didn't push, which is something I now regret."
Ben Myers KC, defending, said: "This is precisely the type of situation where a post-mortem would have been very helpful, isn't it?"
The witness said: "And I regret for not pushing for a post-mortem at that time."
Mr Myers said: "But at the time you were questioning NEC and at the time you didn't have an obvious explanation?"
The doctor replied: "I completely agree with hindsight. I should have requested a post-mortem. I was keen to avoid that, to avoid any distress."
She turned to Child E's parents and said: "I apologise to them that I didn't push for that."
Mr Myers suggested: "You, in effect, steered them away from a post-mortem?"
The witness said: "I don't believe that was the case."
On Monday, Child E's mother told jurors the doctor told them a post-mortem "would not tell us very much".
She said she and her husband decided not to ask for one "largely" because it was explained to them there was "little point".
Letby, originally from Hereford, is also accused of attempting to murder Child E's twin brother, Child F, by poisoning him with insulin.
She denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
A DOCTOR has apologised in court for not "pushing" for a post-mortem examination of a baby boy allegedly murdered by Countess of Chester Hospital neonatal nurse Lucy Letby.
Letby, 32, is said to have administered a fatal amount of air into the bloodstream of the infant while he was being cared for in the neonatal unit.
The death of the premature-born twin, referred to as Child E, was the fourth baby murdered by the defendant in a six-week period, according to the prosecution.
During her evidence on Wednesday, November 16, a consultant paediatrician – who cannot be identified for legal reasons – turned from the witness box to Child E's parents sitting in the public gallery and made her apology.
The doctor was the on-call consultant when Child E deteriorated rapidly late on the evening of August 3, 2015 and died in the early hours of the next day.
Jurors heard that necrotising enterocolitis (NEC) – a serious gastro-intestinal disorder – was entered as the cause of death on Child E's death certificate.
The doctor told the court: "At the time I felt (Child E) had NEC which had led to his collapse and deterioration so I discussed that with the coroner and we agreed for that to be put as (Child E's) cause of death."
She said the infant was a "high-risk baby" and also took into account a colleague's observations of gastro-intestinal bleeding and abdominal discolouration.
Prosecutor Simon Driver asked: "Any clinical factors that militated against that conclusion?"
The consultant replied: "I considered them fully at the time but the fact that (Child E's) observations were very stable up to the point of collapse does not normally fit with NEC.
"And the abdominal X-ray not showing any signs of NEC over an hour before he died – I don't think I gave that enough weight at the time; that the X-ray had been normal."
She told the court she now did not think NEC was the cause of death.
The doctor went on: "A post-mortem would take place if we didn't feel we had a cause of death. It can be requested for any baby who dies if the parents want that investigation.
"The parents were understandably devastated that Child E had died and were not keen on a post-mortem and I didn't want to make a terrible situation any worse so I didn't push, which is something I now regret."
Ben Myers KC, defending, said: "This is precisely the type of situation where a post-mortem would have been very helpful, isn't it?"
The witness said: "And I regret for not pushing for a post-mortem at that time."
Mr Myers said: "But at the time you were questioning NEC and at the time you didn't have an obvious explanation?"
The doctor replied: "I completely agree with hindsight. I should have requested a post-mortem. I was keen to avoid that, to avoid any distress."
She turned to Child E's parents and said: "I apologise to them that I didn't push for that."
Mr Myers suggested: "You, in effect, steered them away from a post-mortem?"
The witness said: "I don't believe that was the case."
On Monday, Child E's mother told jurors the doctor told them a post-mortem "would not tell us very much".
She said she and her husband decided not to ask for one "largely" because it was explained to them there was "little point".
Letby, originally from Hereford, is also accused of attempting to murder Child E's twin brother, Child F, by poisoning him with insulin.
She denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Thursday 17th November 2022
Child E
Dr David HarknessChester Standard Live Reporting
10:39am: The trial is expected to resume at about 10.45am, with 'traffic difficulties' understood to be the cause of the slight delay. Lucy Letby has already arrived and is, as ever, accompanied by a dock officer.
10:48am: The traffic delays may include the collision on the M56 motorway this morning, which the Highways Agency says has led to 60-minute travel delays between Chester and Manchester.
11:18am: After a delay, the court is now ready to resume the trial.
11:23am: The judge, Mr Justice James Goss, explains that travel difficulties have led to the court's delayed start. Philip Astbury, for the prosecution, is calling Dr David Harkness to give evidence.
11:26am: Dr Harkness, a paediatric registrar at the Countess of Chester Hospital in summer 2015, is being asked about Child E on the night shift of August 3. He says they started that shift at about 8.30-9pm. He explains, with working in different hospitals, it is difficult to remember the shift patterns. He explains there would have been a handover period, where he would have read a handover sheet for the various patients and any outstanding conditions those patients had. There would be one sheet for the paediatric ward and one for the neonatal ward. If there were any sick children in A&E, the doctors would have been responsible in attending to them too. He says the handover period would have lasted about 30 minutes.
11:29am: He says some tasks would have required him to work with Dr Christopher Wood, his colleague on the night, and some would have been done solo. He says his tasks would have included speaking to nurses and seeing the neonatal unit babies. He says if there was nothing outstanding happening on the neonatal unit, he would be there at 10-10.30pm. He says for this night he was called over at 10pm, having been called over because Child E had blood in his vomit. Small amounts of blood' - minuscule blood flecks - were spotted when the NG Tube was brought out of Child E, he recalls.
11:42am: The court is shown Dr Harkness's note from 10.10pm on August 3, which says 'asked to see patient [Child E] regarding gastric bleed. Large, very slightly bile-stained aspirate 30mins ago.' The note adds: 'Sudden large vomit of fresh blood and 14ml aspirate.' The doctor is given the opportunity to look through his clinical notes, and Lucy Letby's nursing notes from that shift, to see the chronology of events that night.
11:47am: The court is now shown the 10.10pm note. He says it is not clear, from his note, how much of the 14ml aspirate contained 'fresh blood'. He says the fresh blood was what he had witnessed, having been called over to see it. The court hears he did not see the child vomit, but saw the fresh blood as a product of it.
11:51am: He notes Child E's blood pressure was 'very good', a CRT reading was good, the heart rate was 'normal' and saturation rates were good, with minimal oxygen support. "At that point in time, everything is fine, except for the blood in the aspirate," he tells the court. Child E was also 'pink, well perfused', the lungs were 'clear', the abdomen was 'soft, not distended'.
11:54am: Dr Harkness notes 'GI bleed ? Cause', and tells the court that is a possible diagnosis for the bleeding, and a plan of action with administration of antibiotics is made. The note 'close observation' is made, emphasising the designated nurse - Lucy Letby - was to monitor Child E closely in room 1.
11:59am: Dr Harkness says, from his recollection, he does not believe he left the unit as the bleed was 'something unusual' in Child E so he does not believe he went very far. For the 11pm note, he says Letby called him into room 1, where 'Further GI blood loss and desaturation to 70%' is noted. A '13ml blood-stained fluid from NGT on free drainage' is noted. He says he remembers seeing 'fresh, red blood in the tube', with the contents of the stomach. He says the free drainage setup would have allowed the vomit to come out rather than go into the baby's lungs. He says the origin of the blood must have come from somewhere in the oesophageal tract, down to the stomach. It rules out blood coming from the lungs.
12:01pm: The saturates 'remained 60-70% in 100% O2', with Dr Harkness said 'because of Child E's condition', the oxygen requirement had gone up from 'minimal support'. He says Child E was still trying to breathe at this time. The comment 'crying' is added in the note. Dr Harkness says the child is still well enough to be awake enough and conscious to cry. He said just the note 'crying' would suggest it was a 'typical cry'.
12:03pm: Dr Harkness says the fact Child E was crying would mean he would have had to have been taking deep breaths to do so. The plan of action was 'replace losses' - getting fluid back in. Strict fluid balance' - the court hears, 'knowing how much to put back in'. Dr Harkness says he is planning to intubate Child E and do an x-ray to check Child E's lungs and abdomen to try and explain why the baby was deteriorating.
12:05pm: The type of intubation was 'elective', which was not on the level of 'an emergency situation', the court hears. Dr Harkness says he would discuss the result of the x-ray with surgeons at Alder Hey and seek advice from them.
12:10pm: Dr Harkness said he would then have been preparing to intubate and get the equipment ready. Prescriptions are made from 11.28pm-11.30pm for a number of drugs.
12:17pm: A further note, written in retrospect, is made at 1.45am. He records 'sudden deterioration at 11.40pm' Prior to that, Child E was still to be 'under close observation' by Lucy Letby. Dr Harkness tells the court he was in the room when the 'sudden deterioration' happened, and was there with Lucy Letby and another nurse. Those nurses would have been gathering the drugs to be administered. The notes record 'brady 80-90bpm, sats 60%, poor perfusion, colour change over abdomen, purple discoloured patches'. He says: "This was a strange pattern over the tummy and abdomen, which didn't fit with the poor perfusion - the rest was still pink, but there were these strange purple patches." He says some of the patches were still pink, but others were purple-blue, were unusual. He likens the purple-blue colour to be what you would see after going for a swim in cold water and coming out, with 'purple-blue' colour on the lips. The rest of the skin was 'normal colour'. The abdomen had 'purple patches', which didn't fit with an anatomical part of the body. He says it is difficult to describe in any detail, without a photo. He says he has seen this in Child A before and had not seen it on any other baby, outside of the babies in the case.
12:20pm: The patches were 'different sizes' and in the region of 1-2cm big - 'not dots'. The areas were 'on the abdomen - not above the chest or below the groin - in the middle section'. The patches 'did not fit with the perfusion' seen. He tells the court if the abdomen was dusky or white, then the whole of the body would gradually take that colour too. He says in the case of an affected blood supply, the blood would be lost from the legs first and the body would pull the blood 'into the middle of the body'. "But on this occasion, it is the middle where you are seeing these discolourations?"
"Yes."12:21pm: Dr Harkness confirms he has never seen these discolourations before or since, outside of the babies in this case.
12:22pm: Dr Harkness's notes record 'intubated as an emergency at 11.45pm' He says although there were risks associated with this, the 'safer option' for Child E was to do things as an emergency.
12:25pm: An ET tube was inserted, with 'good air and chest movement' recorded, and the tube was recorded to be in the correct place. Child E was also 'put on ventilator', with 100% oxygen. The saturation readings were '60-70%', and after a morphine bolus was administered, those improved to 80%.
12:31pm: The 'purple discolouration of abdomen remained', it is noted. Child E's blood pressure had dropped but was still in the normal range. The plan was to administer further medication, but there was a concern that administering a drug to make the heart beat faster would lead to 'worse bleeding'. Dr Harkness says 'from his recollection' the blood had settled and there was no further substantial amount of blood recorded.
12:32pm: Dr Harkness said he and a colleague were stood at the end of the incubator, discussing what medication and plans were being put in place for Child E, when Child E collapsed "in front of our face when we were stood there".
12:37pm: Dr Harkness recalls the resuscitation efforts began, and Child E's heart rate recovered at 1.01am, and the parents had arrived by that time. He tells the court the blood supply was 'very poor'. He says during CPR, blood was coming out of Child E's nose and mouth, suggesting the blood pressure was low. He says the sight was "not very nice, particularly".
12:40pm: Dr Harkness is asked about the bleeding seen on Child E. He says: "I have never seen it in a baby, to this extent." He says he had seen the level of blood in a teenager, but not, relatively, in a baby as small as Child E.
12:44pm: Dr Harkness is asked about Letby's nursing note made on the night shift of August 3, which refer to Child E's mum visiting at 10pm and she was informed by Letby and Dr Harkness about blood coming from the NG Tube. It refers to 'she was updated by Reg Harkness and contained [Child E]'. The note is shown to the court. Dr Harkness confirms it was the note shown to him. He does not know what 'contained' meant in the context. He says he does not remember if the mum was present at that time.
12:47pm: A pathology report for Child E is shown, with 'PT and APTT' readings. Those are two tests for blood clotting measurements. They were 'high, but not enough to be shocked by'. The readings were 19.5 and 53.6, compared to the normal ranges of '12.5-15' and '26-35' respectively.
1:22pm: After a short lunch break, the trial is now resuming.
1:23pm: Ben Myers KC, for Letby's defence, opens by mentioning about Letby's note made. Mr Myers says a 'containment technique' was used, as described by Child E's mother, to clarify the 'contained' comment. It was a technique used to calm a baby.
1:28pm: Mr Myers asks about the sequence of events. He refers to a police statement Dr Harkness made, where the doctor says: "I was asked to review [Child E] by Letby [following the finding of a dirty aspirate]. Looking at the notes it was 10pm-10.30pm...I only came on at 9pm'. He described, in the statement, the aspirate which was largely mucus-y. He said he could not be sure if there was a fleck of blood around Child E's face [on examination]. [Child E] looked relatively settled and there was nothing to suggest that was ging to change'.
1:30pm: The statement adds: 'However, around half an hour to an hour later there was a large amount of fluid which came up the tube. From memory it was 12-14ml of blood which for a baby was a substantial amount'. Child D brought up further 'fresh blood' in quantities which he had 'not seen [in sudden cases] since'.
1:38pm: Mr Myers asks about the initial stages from the first clinical note, at 10.10pm. Dr Harkness confirms he has been asked to review Child E, following the bile-stained aspirate '30 mins ago'. Mr Myers said all of what had happened in the 10.10pm note, had happened by 10.10pm. Dr Harkness says this was a 40-minute period of several year ago. He said this was potentially a period of 9.30-10.10pm. He said it would 'match up' with the note. In the police statement, Dr Harkness said he would have been 'bleeped' by Lucy Letby. He says that would have been the most common approach to be alerted to the nursery room 1. He said he had seen 'a dirty aspirate which may have contained blood flecks and bile'. Mr Myers says the police statement said Child E had 'nothing dramatic' around the baby's face, and could not be sure if there were any blood flecks. Child E was 'not in distress' and 'appeared fine'. Dr Harkness says he does not know if he saw Child E's mother, and does not have a clear recollection. He says it could be the case, looking at the notes provided.
1:39pm: Mr Myers asks if Dr Harkness had 'any particular concerns' from the first reading. Dr Harkness says there wasn't. He agrees the second note, with blood vomit, was 'more concerning' and suggested a gastrointestinal bleed. Mr Myers asks if such a bleed was 'serious'. "Potentially," Dr Harkness replies.
1:41pm: Mr Myers suggests that a GI bleed should have led to a blood transfusion. Dr Harkness says if there were other observations which collated that, he would have done so, but at this point, he would not have done so, as the blood vomit could have had other causes. He said a blood transfusion 'may have come up in a conversation' with a fellow doctor. Mr Myers asks why that wasn't documented. Dr Harkness says he cannot answer that.
1:47pm: The clinical note for 11pm is shown to the court, which the court hears refers to the 'large amount of fresh blood'. Dr Harkness was called into the unit. The '13ml blood-stained fluid' is a 'significant quantity', Dr Harkness confirms. Mr Myers said this follows other blood which came out earlier, and a typical baby would have had something 'in the region of 120ml' in him at that time. Dr Harkness agrees. Mr Myers said there had been 27mls of blood and aspirate taken from him in that time, which was 'up to a quarter' of Child E's blood. Dr Harkness agrees. Mr Myers says the heart rate is 'normal', but the saturation rate is 'low'. He says the heart rate 'should be higher'. Dr Harkness says: "Not necessary - there are multi factors to that. It's part of a separate conversation with expert witnesses." He says it is not as simple as saying one reading should go up in line with others. He says blood pressure was normal, and there were other factors to consider. Mr Myers says the pairing of heart rate and saturations is 'not normal'. Dr Harkness says it is abnormal, in the sense that the heart rate is normal and the saturations rate is abnormal.
1:51pm: Mr Myers asks why a consultation with surgeons was required following x-rays. Dr Harkness says advice would have been taken from them once the extra results would have been acquired from the x-rays. Mr Myers says he could have been dealing with a 'very serious situation indeed'.
Dr Harkness: "Potentially." Dr Harkness says things were "changing" but Child E was still "stable".
Mr Myers: "Are you suggesting that a baby who has lost a quarter of its blood is not an emergency situation?" Dr Harkness "What I'm suggesting is there are things to do and there is time to do it." Mr Myers says transfusion was not being considered at this point, and one of the 'obvious things' to consider. "It is something you had failed to consider, isn't it?" Dr Harkness says it was likely considered, but accepts it was not documented at the 11pm note. Mr Myers suggests it was a "serious mistake" not to consider blood transfusion.
Dr Harkness: "I disagree."1:55pm: Mr Myers asks about the staffing levels that night, and asks what would have happened if he had been called to the A&E department. Dr Harkness said he would have contacted the on-call consultant at that time to come over in that instance.
Mr Myers: "I would suggest you were out of your depth at this point."
"I disagree." He adds that is "wrong and disrespectful to my ability." Mr Myers says blood transfusion is not considered. "But we do have a plan, and we do have a discussion with a consultant." Mr Myers says the intubation should have happened earlier. Dr Harkness says there are benefits to an elective intubation compared to an emergency intubation, as the latter could cause stress and complications to the baby. He said that 'now' this would still have been the course to take in that situation.1:57pm: The court hears the preparations are made for the intubation during a half hour. Dr Harkness disagrees with Mr Myers that it was a "delay" and was using his time "appropriately". "You make more mistakes when you are not taking your time."
1:59pm: Mr Myers says the blood transfusion is mentioned for the first time at a later note, after 11.40pm. Dr Harkness says it would not have been appropriate to give more saline boluses without administrating fresh blood. He disagrees a blood transfusion was not considered earlier. He says his documentation is not as thorough as it would be now, and agrees in hindsight, it should have been documented more clearly.
2:04pm: The 'skin discolouration' observation is noted, and that it later 'remained' on the abdomen. A nursing colleague had referred to 'discoloured abdomen' in a retrospectively written note at 1.30am. Mr Myers said Dr Harkness had referred to the discolouration being 'strange' and 'unusual', and 'appearing and disappearing'. That does not appear in the medical note, Mr Myers says. Dr Harkness says that observation had "stayed with him" and the clinical note he made at the time was not 'forensic'.
2:10pm: Mr Myers reads out part of Dr Harkness's statement to the police, referring to the discolouration being on the abdomen. Dr Harkness says he does not recall the part of the statement of the discolourations' 'path to the body', and said he would not agree with the wording of that. He says he has not been in discussions with anyone in relation to these observations. Mr Myers said by October 2018 (by the time of his police statement), there had been discussions in the hospital about the skin discolourations. Dr Harkness said there were discussions to say it was unusual, but refutes any of the details of the discolourations had been discussed. Mr Myers says Dr Harkness is 'putting details together' from various observations.
Dr Harkness: "No." Mr Myers says Child A's skin discolouration, as referred to by Dr Harkness in court earlier in the trial, were not mentioned in the clinical note at the time or the note to the coroner. Mr Myers says 'red patches' found on Child A were not mentioned for Child E. Dr Harkness said the overall discolouration observations were 'similar enough'.2:11pm: Mr Myers refers to Child E's collapse 'in front of the medical staff'. He says by this point, "there had still been no transfusion". Dr Harkness said there was no further evidence of bleeding after the second bleed.
Mr Myers: "The reaction to the second haemorrhage was far too slow wasn't it?"
Dr Harkness: "I disagree."2:13pm: Mr Myers says a blood transfusion, for O-negative blood, is noted at 12.50am on the medical notes. Dr Harkness says the O-negative blood [a type which can be suitable for all blood transfusions] would be used in this instance as seeking a specifically matched blood type at this stage would take too long in acquiring it from the donor fridge.
2:19pm: The note of 12.36am - CPR commenced, is mentioned. The transfusion would have followed. Mr Myers says, in 'distressing detail' relayed by Dr Harkness earlier in court, it had been discussed about blood coming from Child E's mouth and nose during CPR. Dr Harkness said blood would 'keep coming out' until the cause of it is found. Mr Myers says the cause of death would be 'acute blood loss'. Dr Harkness said that cannot be known without a post-mortem examination. He says the blood loss could be a factor, but it is not 'black and white'. He said it was 'not his place' to call for a post-mortem examination. Mr Myers says the blood loss seen would normally be 'fatal'. Dr Harkness said it could be 'linked'. Mr Myers asks if the actions taken were 'far too slow'.
Dr Harkness: "No."
"Would you have admitted it if it was?"
"Yes."2:21pm: The prosecution rise to ask about the timing of Dr Harkness 'meeting the mother of Child E'. Dr Harkness said that would have been the case, based on a nursing note. The prosecution ask if that was from looking at Letby's note. Dr Harkness agrees. The prosecution say Dr Harkness's clinical note does not refer to meeting the family. Dr Harkness said it could be documented, but would depend on the level of detail of the discussion.
2:27pm: Dr Harkness's interview with police from September 2018 is relayed to the court. Dr Harkness is asked about the skin discolouration, and says it is 'similar [between Child A and Child E]' and is not a rash. The interview transcript says Child E's discolouration was 'around the abdomen and chest', with 'purple patches' that 'suddenly come on'. "It came so quickly - not affected by the monitors or anything". "It was just this purple and pale patches". He was asked in the police interview if that was symptomatic of other cases, and Dr Harkness said that was not.
Friday 18th November 2022
Child E
Dr Dewi Evans - Dr Sandie Bohin10:32am: I'm back at Manchester Crown Court for the trial of nurse Lucy Letby. We're expecting to hear expert medical evidence from Dr Dewi Evans today
10:39am: Dr Dewi Evans was approached by the National Crime Agency to review the case in 2017. In a report he produced in 2018, Dr Evans set out that a number of babies in this case died as a result of an intentional injection of air into the bloodstream
10:43am: Dr Evans is talking the jury through his assessment of Child E's condition in the days before his death. He says that the infant's bloods, white blood cell levels, saturation were as 'stable as you can get'....'he was active and pink, all was satisfactory'
10:48am: Dr Evans is summarising that for the first five days of Child E's life he was 'stable' and that there was nothing to suggest there was 'something wrong' with him
10:54am: The court is being shown heartrate and respiratory charts from the day before Child E's death, again Dr Evans says these show he was a 'stable' and 'well little baby'
10:59am: Asked if it was a point of concern that the baby needed insulin, Dr Evans says 'no', he explains 'he needed insulin to control his glucose values, that’s fine, that’s what neonatal units are for'
11:05am: We're now looking at medical notes and charts from the evening before Child E's collapse and death. Between 18:00 and 21:00, Dr Evans says everything was 'normal' and 'stable'
11:19am: Dr Evans is now giving his overall observations of Child E. He explains the reason for the need for insulin was that as a premature baby, his own insulin production had not yet kicked in. He notes that the baby was at risk of necrotising enterocolitis (NEC) This is a condition that can affect newborn babies, where tissue in the bowel (small and large intestines) becomes inflamed - doctors were aware of this at the time and held off with oral feeds for the first few days of his life
11:20am: Dr Evans is asked if NEC is a 'viable' explanation for what happened to Child E, he says 'no'
11:26am: Earlier this week, Child E's mother told the court that the evening before her infant son died, she found him with "blood on his face" and making "horrendous" sounds. Dr Evans said this is 'difficult to explain' He adds: 'This is not something I've seen other than in this case'
11:30am: Asked for his reasoning behind Child E's death, he said there are 'two major' factors - he says the baby suffered some kind of 'trauma' which caused gastric bleeding. He says there is no innocent explanation for this and says it could have been caused with a 'stiff' implement The second reasoning is air embolism - the intentional injection of air into the bloodstream
12:11pm: On the intentional trauma that Dr Evans cites, Ben Myers KC, defending, put it to the medic that he was "looking for possible items just to support the allegation, than simply looking at all the available facts". Dr Evans repeated that he believed Child E was subjected to a trauma that did not result from a 'natural phenomenon'. He earlier suggested this could have been caused by the inappropriate use of a surgical tool known as an introducer (a thin piece of wire covered in plastic)
12:12pm: Another medical expert Dr Sandie Bohin, who reviewed Dr Evans' reports on this case, is now in the witness box.
12:32pm: Dr Bohin is now going back over Child E's medical notes and the chronology of his collapse.
12:36pm: Dr Bohin said it was 'a poor decision' not to carry out a post-mortem on Child E. The senior paediatric consultant responsible, who cannot be named for legal reasons, told the court earlier this week that they "now regret" not recommending a post-mortem
12:47pm: Dr Bohin is asked about Child E's gastric bleed. She says she has 'never' seen a nasogastric (feeding) tube causing that damage - she says the infant lost 25% of his blood volume as a result
12:49pm: She says she was left 'clutching at straws' to explain such a haemorrhage. One explanation she found was an extremely rare condition (only six cases globally recorded since 1968) called Dieulafoy's lesion She said this condition is where an artery within the stomach wall spontaneously haemorrhages as a result of some inflammatory process in the gut wall
1:09pm: Court is now taking a short break.
2:06pm: Dr Sandie Bohin is being cross examined by Ms Letby's defence lawyer Ben Myers KC - she agrees that Child E was at 'higher risk' than other newborns, given his premature birth - but does not accept he was at a higher risk of death
2:31pm: Prosecution have just read a summary of Ms Letby's police interviews in 2018 and 2019 in relation to the death of Child E. Ms Letby denied causing any intentional harm to the infant.
2:39pm: Court has now adjourned, back Monday
Chester Standard article 18-11-2022
A RIGID wire or tube may have been used to cause "extraordinary bleeding" in a baby boy allegedly murdered by nurse Lucy Letby, a court has heard.
Jurors at Manchester Crown Court heard the infant lost a quarter of his blood volume before he collapsed and died in the Countess of Chester Hospital's neo-natal unit.
The blood loss took place during a night shift on August 3 2015 in which Letby was the designated nurse for the premature-born twin boy, referred to as Child E.
The Crown says Letby, 32, injected a fatal amount of air into the bloodstream of the youngster.
Giving evidence on Friday, expert medical witness Dr Dewi Evans said he thought Child E had suffered a fatal air embolism - a blockage of the blood supply - after a treating medic noticed "unusual" purple patches on the child's abdomen.
He said a second "major" issue was "significant haemorrhaging from the upper gastrointestinal tract, somewhere between the mouth and the stomach".
Dr Evans said: "I think he (Child E) suffered trauma from some other form of injury and there were a number of bits of equipment on a neo-natal unit that are relatively rigid.
"Plastic tubes used for suction, for instance, so it could have been interference with that."
He said another medical instrument known as an introducer - a thin wire surrounded by plastic which can be used to intubate a baby - would be "more than sufficient to cause trauma if used inappropriately".
Dr Evans said: "I cannot be 100 per cent certain what caused the trauma to the gastrointestinal system but it had to be some kind of relatively stiff (equipment) which was sufficient to cause this extraordinary bleeding."
Prosecutor Nick Johnson KC asked the consultant paediatrician if there could be an "innocent explanation" for the level of bleeding.
Dr Evans replied: "No. The other explanation for this is a bleeding ulcer. I have never seen a bleeding ulcer cause this sort of presentation."
In his initial reports Dr Evans said he was "at a loss" to explain the haemorrhaging and it was not possible to say if any deliberate harm took place because of an absence of a post-mortem.
In a further report - after he reviewed a statement from Child E's mother who described "horrendous crying" from her son and blood around his mouth - he suggested something "had been done or used" to cause trauma.
Dr Evans suggested that a nasogastric tube could have been thrust into the baby's stomach with inappropriate force.
However, he told the court he later saw the type of tube used by the hospital at the time and ruled out it could be capable of causing such damage.
Child E suffered a sudden deterioration from 11.40pm on August 3, the court has heard, and later died early the next morning after staff were unable to resuscitate him.
Dr Evans said, in his opinion, Child E was "stable" leading up to the beginning of the "massive" haemorrhaging during the night-shift.
Cross-examining, Ben Myers KC, defending, said: "The haemorrhaging that Child E experienced on August 3 and 4 could be due to some form of ulceration or bleeding from the stomach from natural causes, albeit not normal?"
Dr Evans replied: "I don't think so."
On the expert's initial belief a nasogastric tube could have been used to harm the child, Mr Myers said: "You were looking for something that could possibly support an allegation of deliberate harm that you must have known was not realistic?"
Dr Evans said: "I disagree."
Mr Myers went on: "You are actively trying to find things that would support this allegation even when there is no evidential basis?"
The witness replied: "Child E had massive haemorrhaging from his upper gastrointestinal system and that is not something that occurs as a result of some kind of natural phenomenon."
Fellow expert medical witness Dr Sandie Bohin agreed with Dr Evans that an air embolism was the cause of death.
She added: "I have never seen a baby have a gastrointestinal haemorrhage in this way.
"I think the bleeding may have made him unstable but I don't think that is what caused his death. I don't think that is what caused him to collapse and need CPR."
Mr Myers said: "He died because of a catastrophic bleed, didn't he?"
Dr Bohin replied: "I don't believe that is so."
On Thursday Mr Myers suggested that medics were too slow during the night-shift to order an emergency blood transfusion for Child E.
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Monday 21st November 2022 - no court (juror ill)
Tuesday 22nd November 2022
Child F
Police analyst: Recorded events & messages - Dr Gail BeechChester Standard Live Reporting
11:05am: The trial has now resumed. The jury is being shown the sequence of events for Child F, the twin boy of Child E.
11:08am: Child F was born on July 29, 2015, at the Countess of Chester Hospital, and had required some resuscitation at birth and was later intubated, ventilated and given medicine to help his lungs. On July 31, a high blood sugar reading was recorded for him, and he was prescribed a tiny dose of insulin to correct it. At this time his breathing tube was removed and he was given breathing support.
11:12am: In the early hours of August 4, Child E had died. Later that day, just before 5pm, a nursing note records family communication in which Child F's parents wish to transfer care to another hospital in the North West, but transport was unavailable due to an emergency. The note adds 'sincere apologies given to parents'.
11:14am: The court is now focusing on the night shift of August 4-5, in which the prosecution allege Child F was poisoned on this night. A staff shift rota shows Belinda Simcock was the shift leader, with one nurse being the designated nurse for Child F in nursery room 2, and Lucy Letby being a designated nurse for the other baby in room 2 that night.
11:16am: The court is shown a plan of the neonatal unit and the designated nurses for the babies on the unit that night.
That night, there was one baby being cared for in room 3, twins being cared for in room 4, and two other babies in the unit whose location cannot be established from the records, the court hears. There were a total of seven babies in the unit and five nurses on duty that night.
11:17am: During the handover period at 7.30-8pm, a message from Letby's colleague Jennifer Jones-Key is sent to Letby's phone, saying: "Hey how's you? x"
11:21am: Letby responds at 8.01pm: "Not so good. We lost [Child E] overnight. x" [8.02pm]
Ms Jones-Key: "That's sad. We're on a terrible run at moment. We're you in 1? X" [8.02pm]
Letby: "Yes. I had him & [another child]
Jones-Key: "That's not good. You need a break from it being on your shift."
Letby replied it was the "luck of the drawer [sic]".
Jones-Key: "You seem to be having some very bad luck though"11:22am:
Letby: "Not a lot I can do really. He had massive haemorrhage which could have happened to any baby x"11:23am: Jones-Key: "...Oh yeah I know that and it can happen to any baby. Very scary and I have seen one"
Jones-Key: "Hope your [sic] be ok. Chin up"
Letby: "I'm ok. Went to [colleague] for a chat earlier on [and with] nice people tonight."11:24am:
Letby: "This was abdominal [bleed in Child E]. I've seen pulmonary before"
Jones-Key: "That's not good. It's horrible seeing it. "Hope your night goes ok"11:28am: The court is shown medication is being administered to Child F at this time, between 9-10pm. A blood gas record result at 11.32pm shows a blood glucose level of 5.5.
11:33am: A 48-hour bag prescription of nutrition is signed, solely, by Lucy Letby, recording it ending at 12.25am on August 5. Two records are shown for the next administration, the first being crossed out. The second nutrition bag has a higher level of Babiven, along with quantities of lipid and 10% dextrose that weren't on the first, crossed out, administration. The Babiven is stated to start at 12.25am, and the lipid administration is signed to begin at 3am. Letby is a co-signer for both the Babiven prescriptions, but not the lipid administration.
11:37am: The 12.25am prescription for the TPN bag starts to be administered at 12.25am. Child F then suffered a deterioration, the court hears. A fluid chart shows Child F, for 1am in the 'NGT aspirate/vomit' column, four '+' signs.
11:41am: The nursing note, written retrospectively and timed for 1am, records: "large milky vomit. Heart rate increased to 200-210. [respiration rate] increased to 65-80. [Oxygen saturation levels] >96%. Became quieter than usual. Abdomen soft and not distended. Slightly jaundiced in appearance but no loss of colour. Dr Harkness R/V."
11:44am: An observation chart for Child F is timed at 1.15am. The heart rate is shown having increased, along with the respiration rate, at this time, into the 'yellow area', which the court has previously heard is something medical staff would note and raise concerns if necessary. Prosecutor Nicholas Johnson KC says the relevant nurse will be asked to give further details on this in due course. A blood gas reading for Child F at 1.54am has his blood glucose level as 0.8.
11:48am: Medication of 10% dextrose is administered intravenously at 2.05am, along with various other medications. Blood tests are ordered for Child F by doctors at 2.15am and 2.17am. They are collected between 2.33am and 2.45am. Child F's blood glucose level is recorded as 2.3 at 2.55am. This is still "below where it should safely have been", Mr Johnson tells the court.
12:04pm: The trial is now resuming after a short break. Intelligence analyst Claire Hocknell is continuing to talk through the sequence of events for Child F in court.
12:07pm: The lipid prescription is administered at 3.10am on August 5, with 0.9% saline administered at 3.35am. A 10% dextrose infusion is recorded at 3.50am. At 4.02am, Child F's blood glucose reading is 1.9. Further saline and 10% dextrose medications are administered at 4.25am. The blood glucose level is recorded as 2.9 at 5am.
12:11pm: The shift handover is carried out at 7.30am, with day shift nurse Shelley Tomlins recording a blood glucose level for Child F as 1.7 for 8am. Prosecutor Mr Johnson says this is a "dangerously low level". The subsequent reading, recorded at 11.46am, is 1.4.
12:16pm: Dr Ogden records a blood glucose level at 10am for Child F as '1.3'.
12:21pm: Prior to this reading, Letby has been messaging the night-shift designated nurse for Child F, saying: "Did you hear what [Child F]'s sugar was at 8[am]?" The nurse replies: "No?"
Letby: "1.8" The nurse replies: "[S***]!!!!", adding she felt "awful" for her care of Child F that night.
Letby: "Something isn't right if he is dropping like that," adding that Child F's heel has to be taken into consideration [as blood gas tests are taken via heel pricks, and cannot be done too regularly]. The nurse responds: "Exactly, he had so much handling. No something not right. Heart rate and sugars."
Letby: "Dr Gibbs came so hopefully they will get him sorted. "He is a worry [though]." The nurse replies: "Hpe so. He is a worry." Letby responds: "Hope you sleep well...let me know how [Child F] is tonight please." The nurse replies: "I will hun".12:22pm: Child F's blood glucose level is recorded by a doctor as 2.4 at 12pm. Further medication administrations are made throughout the morning. A new long line is also inserted at this time.
12:27pm: Child F's blood glucose level is recorded as being 2.4 at noon, 1.9 at 2pm and 1.3 at 3.01pm. More dextrose is administered. The blood glucose level is still "very low", the court hears, at 1.9 at 4pm.
12:28pm: At that time (4pm), Letby's phone receives an invitation from an estate agency firm confirming a viewing for a property in Chester, near the hospital. This home would be the address where Letby stayed until her 2018 arrest.
12:31pm: Child F's blood glucose level is recorded as being 1.3 at 5.56pm. A blood test is recorded for insulin to the Royal Liverpool Hospital at 5.56pm. The court hears those results did not come back for a week. Child F's blood glucose level is recorded as 1.9 at 6pm.
12:36pm: Letby messages a colleague at 6pm to ask: "Hi! Are you going to salsa tonite?" The colleague responds: "Should do really as I haven't been for ages." After confirming she will, Letby responds with an 'ok' emoji. Letby adds: "Need to try and find some sort of nites energy", before clarifying "post nites" She adds, to conclude the conversation: "Hasta luego".
12:39pm: A nursing note records there was a change from the TPN/lipid and 10% dextrose administration to 'just 15% dextrose with sodium chloride added'. The new fluids were commenced at 7pm.
1:02pm: The designated nurse for the previous night shift returns to care for Child F on the night shift for August 5-6. She messages Letby to say: "He is a bit more stable, heart rate 160-170." The long line had "tissued" and Child F's thigh was "swollen". It was thought the tissued long line "may be" the cause of the hypoglycaemia.
1:04pm: The colleague added: "Changed long line but sugars still 1.9 all afternoon. Seems like long line tissued was not cause of sugar problem, doing various tests [to find the source of the problem]. Letby responds: "Oh dear, thanks for letting me know" The nurse colleague replies: "He is def better though. Looks well. Handles fine."
1:16pm:
Letby replies: "Good." At 9.17pm, Child F's blood glucose level is recorded as being 4.1. Letby later adds, at 11.58pm: "Wonder if he has an endocrine problem then. Hope they can get to bottom of it. "On way home from salsa feel better now I have been out." The colleague replies: "Good, glad you feel better. Maybe re endocrine. Maybe just prematurity."
Letby replies: "How are parents?" Colleague: "OK. Tired. They've just gone to bed."
Letby: "Glad they feel able to leave him." Colleague: "Yes. they know we'll get them so good they trust us."
Letby: "Yes. "Hope you have a good night."1:40pm: Child F's blood glucose levels rose to 9.9 at 1.30am on August 6, a repeat 9.9 reading being made at 2am. Letby made the first of nine Facebook searches for the mum of Child E and F at 7.58pm on August 6. The searches were carried out between August 2015 and January 2016, and included a search on Christmas Day. One other search was carried out for the father of Child E and F on Facebook at 1.17am on October 5.
1:52pm: Letby sent a message to the designated nurse for Child F from those two night shifts, on August 9 at 10.17pm, saying: "I said goodbye to [Child E and F's parents] as [Child F] might go tomorrow. They both cried and hugged me saying they will never be able to thank me for the love and care I gave to [Child E] and for the precious memories I've given them. It's heartbreaking."
1:53pm: The nurse colleague replies: "It is heartbreaking but you've done your job to the highest standard with compassion and professionalism. When we can't save a baby we can try to make sure that the loss of their child is the one regret the parents have. It sounds like that's exactly what you have done. You should feel very proud of yourself esp[ecially] as you've done so well in such tough heartbreaking circumstances. Xxxx"
1:56pm:
Letby: "I just feel sad that they are thanking me when they have lost him and for something that any of us would have done. But it's really nice to know that I got it right for them. That's all I want." The colleague replies: "It has been tough. You've handled it all really well."
"They know everything possible was done and that no-one gave up on [Child E] till it was in his best interest. As a parent you want the best for your child and sometimes that isn't what you'd choose. Doesn't mean that your [sic] not grateful to those that helped your child and you tho xxx"
Letby: "Thank you xx"1:58pm: On November 12, another colleague messages Lucy Letby at 8.32pm, saying: "[Child E and Child F]'s parents brought a gorgeous huge hamper in today. Felt awful as couldn't remember who they were till opened the card. Was very nice to them though n [Child F] looks fab x" Letby responds: "Oh gosh did they, awe wish I could have seen them. That'll stay with me forever. Lovely family x"
2:12pm: The trial is now resuming after a lunch break. The court hears there is being some slight 'rejigging' of witnesses coming into court this week, after the trial heard no evidence on Monday due to juror illness. That has meant the witnesses are being called into court in a slightly different order than originally planned for the week, due to their respective availability.
2:16pm: Intelligence analyst Claire Hocknell is now talking through the neonatal review for Child F. This sort of review has been shown to the court for previous babies in the case.
2:25pm: Philip Astbury, prosecuting, is now calling Dr Gail Beech to give evidence. She was employed at the Countess of Chester Hospital as a paediatric registrar in summer 2015. She was present at the birth of Child E and Child F, and looked after the former. Her first involvement with Child F was during the day shift on August 4.
2:28pm: She says it would have been "usual practice" that she would have been told about the death of Child E as part of her hand-over for that day shift. A 'ward round-up' is presented to the court, filled in, in preparation for the weekly consultant 'grand round' ward round-up on a Wednesday. The list of problems, readings and observations for each child is noted, concluding with a management plan.
2:32pm: Dr Beech explains Child F was born premature, and the note recorded Child E had died aged six days. Child F was on Optiflo, with 'suspected sepsis' noted, a raised urea and creatinine, 'jaundice' but not on phototherapy at this stage. Child F was also 'establishing feeds' and awaiting genetics test for Down's, but Child F was not showing any clinical features, and 'hyperglycaemia - resolved'. Mr Astbury says the genetic test results were received on August 7. Dr Beech said they confirmed there wasn't a presence of Down's. Dr Beech confirms she was satisfied the hyperglycaemia [high blood sugar] level had been resolved.
2:34pm: Dr Beech said a standard list of medication was prescribed. The Optiflo reading was not supplemented with oxygen - Child F had been 'in air since 3.30am'. Oxygen saturation levels were 92-97%, which were 'satisfactory'.
2:37pm: Dr Beech says there 'weren't any concerns' on the cardiovascular system. Child F weighed 1.296kg [2lb 13oz], from a birth weight of 1.434kg [3lb 2oz]. Dr Beech said this was not a concern as babies, particularly neonates, lose weight in the first days following birth.
2:39pm: Dr Beech confirms Child F was receiving nutrition via a TPN bag. Child F was 'active, moving all 4 limbs'.
2:44pm: Child F was 'active and pink', with a 'clear' chest, no increased rate of breathing. A note saying Child F required further tests on 'mouth and palate', and 'eyes', as part of a 'top to toe examination'.
2:45pm: The management plan says, for Child F, 'wean Optiflo flow when in air.' Complete 7 days of antibiotics' "Continue increasing feeds as tolerated'. Chase genetics [for results]'. Complete examination and baby check later (parents arrived, upset about twin 1)'.
2:53pm: Dr Beech is now asked to look at a chart for a prescription for Babiven, which she has dated, but does not recall writing it. She had signed for a rate of lipid, but that was zero as it wasn't required. Babiven is a "standard bag" which would be given at a bespoke rate for Child F. Dr Beech says the second prescription, with different Babiven levels and a new lipid level, was made as Child F had been made 'nil by mouth' and the increased levels were so Child F could acquire the same level of nutrients in his body.
2:57pm: Dr Beech is asked if there was anything notable from previous clinical records that she could recall in respect of Child F. She says there was not. Her note at 5.40pm on August 5 documented 'asked to prescribe 150ml/kg/day 15% dextrose over 24hr at handover with 5ml/kg/day in it. "Also to stop TPN, check urinary [sodium], cortisol and insulin." Dr Beech says she cannot remember if Child F had been prescribed additional dextrose doses. She says the 15% dextrose - a "high amount" - would normally be due to low blood sugar levels.
3:01pm: An intensive care chart is shown to the court, showing blood sugar levels which are "all low". "2.9 [the 5am reading] isn't bad for a neonate - anything less than 2.6 is considered low" Readings of 1.8 and 1.9 are shown for much of the day, up to 6pm. 10% dextrose solutions are administered at 3pm and 4pm.
3:04pm: A blood test is recorded at 5.56pm, sent to a laboratory, with 'relevant clinical details: preterm neonate, hypoglycaemia, on 10% dextrose'. The blood glucose levels recorded are 1.3. The 'lab sample' "tends to be more accurate" than one on a blood gas machine, Dr Beech tells the court.
3:06pm: The cortisol reading is 364, which is within the range of 155 to 607. The insulin reading is 4,657. The insulin c-pep reading is less than 169. Dr Beech says the insulin reading is "very high" - while there is no 'normal upper limit', that reading could be considered high, the court hears. The insulin c-pep reading is the lowest reading the machine can record. The two readings [insulin and insulin c-pep] are "expected to be similar," Dr Beech tells the court.
3:09pm: A urine sample sent at 6.43pm had 'no unusual readings', but Dr Beech tells the court she cannot think, off the top of her head, how to interpret those results recorded. A chart showing a 7pm prescription of 15% dextrose, with sodium chloride, is administered intravenously. Dr Beech has signed that.
3:12pm: Ben Myers KC, for Letby's defence, asks about the review she completed for Child F. She clarifies she was waiting genetic test results for Child F for the presence of Down's Syndrome. Those results came back on August 7, with no evidence of Down's Syndrome. Mr Myers asks if a further, microarray genetics test can be conducted to show for further potential genetic disorders. Dr Beech confirms that is the case.
3:14pm: Mr Myers says on August 4, the fluids were being administered via TPN, and milk coming in via the NGT [nasogastric tube], with no lipid required as Child F was getting milk in.
3:17pm: Mr Myers asks about the management plan - 'continue increasing feeds as tolerated'. He then refers to the two August 4 prescriptions of fluids [the first being crossed out], and if Dr Beech had completed the figures. Dr Beech confirms that was the case, and that she signed for them. At the first one, there is no component of lipid. Dr Beech says she would have written these figures after the ward round, so the TPN could be made up.
3:22pm: Dr Beech says it would take some time from prescribing the TPN bag to it then being administered. Mr Myers asks for clarity on how the second prescription comes to be made, with a different rate of administration of Babiven and a new lipid and new 10% dextrose doses. Dr Beech confirms she did not prescribe these additional nutritions, as they are signed by a colleague. The total nutrition administration is now 165ml and the rate is slightly increased from the first, crossed-out prescription of total 150ml fluid. Dr Beech says the additional nutrition would come on separate infusions. That concludes Dr Beech's evidence.
Wednesday 23rd November 2022
Child F
Nurse Shelley Tomlins - Nurse Sophie Ellis - Nurse Belinda WilliamsonChester Standard article 23-11-2022
THREE nurses have denied they gave insulin to a baby boy allegedly poisoned by their colleague Lucy Letby, a court has heard.
Each gave evidence on Wednesday, November 23 about their involvement in the care of the premature-born twin at the Countess of Chester Hospital's neo-natal unit.
Nurses Shelley Tomlins, Sophie Ellis and Belinda Williamson were on duty in August 2015 in the days that followed the infant's birth.
It is the Crown's case that Letby, 32, attempted to murder the youngster, referred to as Child F, by intentionally administering insulin shortly after midnight on August 4, 2015.
Jurors at Manchester Crown Court have heard Child F's heart rate surged and his blood glucose levels dropped dangerously low after he received a new intravenous feed including nutrients and sugar.
His glucose levels remained low on the day shift of August 5 even after the intravenous line, and a connected bag containing nutrients, needed to be replaced after swelling to Child F's leg.
Child F's blood glucose rose to safe levels later that evening after the nutrients were stopped and extra sugar was given independently, the court was told.
He went on to make a full recovery and was later discharged.
Ms Tomlins, who worked on the day shifts of August 4 and 5, said stock nutrient bags would be kept in a padlocked fridge in the neo-natal unit.
The nursing shift leader would hold a bunch of keys for the fridge and for locked cupboards containing medication but they would be passed around the nurses with no log of access, she said.
At the end of his questioning Philip Astbury asked her: "Did you at any point in time administer insulin to (Child F)?"
Giving evidence from Australia via videolink, the witness replied: "No."
Mr Astbury repeated the question to Ms Ellis, giving evidence from behind a screen, who worked with Letby on the night shift of August 4.
Ms Ellis replied: "Absolutely not."
Finally Mr Astbury asked Ms Williamson, the shift leader on the night of August 4: "Did you during the course of the shift, at any stage, administer (Child F) any insulin?"
"No," said Ms Williamson.
Letby is accused of attempting to murder Child F less than 24 hours after she allegedly murdered his twin brother, Child E, by injecting air into his bloodstream.
The defendant, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Thursday 24th November 2022
Child F
Dr C - Video demonstration of an Alaris Pump - Dr John Gibbs - Unnamed nurseChester Standard Live Reporting
10:31am: The trial is now resuming.
10:34am: The first witness is a doctor who has previously given evidence in the trial, but cannot be named due to reporting restrictions. She says she didn't have any direct treating care role for Child F.
10:38am: The court is shown clinical notes on August 13 from a junior doctor colleague, in which she received genetic test results from Liverpool Women's Hospital. The test had been conducted to check for signs of Down's Syndrome. The doctor says Child F did not show any clinical signs of Down's at birth, and the test result showed no signs that was the case either. The 'hypo screen results' were from a series of blood tests done when a baby has a "persistent" low blood sugar score. Some tests are conducted in the Countess of Chester hospital, some are taken to a laboratory in Liverpool, the court hears.
10:42am: The doctor says the cortisol reading was 'normal', the insulin at a reading of 4,657 was "too high for a baby who has a low blood sugar". The doctor says it would be expected, with a baby in low blood sugar, for insulin to stop being produced, so that would also be low. The insulin c-peptide reading of 'less than 169' does not correlate with the insulin reading. The insulin and insulin-cpep readings would be 'proportionate' with each other. The doctor says it was likely insulin was given as a drug or medicine, rather than being produced by Child F, to account for this insulin reading. "This is something we found very confusing at the time," the doctor says, and said there weren't any other babies in the unit being prescribed insulin at that time, which would rule out "accidental administration".
10:43am: The doctor says there are "some medical conditions" where a low blood sugar reading would also see a high insulin reading, but the low insulin c-peptide reading meant those conditions would be ruled out. The insulin reading was "physiologically inappropriate", the court hears.
10:45am: The doctor said those readings would be repeated, but as Child F's blood sugar levels had returned to normal by the time the test results came back several days later, there would be "no way" to repeat the test and expect similar results.
10:46am: The doctor tells the court that Child F had received 'rapid acting insulin' on July 31, but the effect of that insulin would have "long gone" by the time the hypoglycaemia episode was recorded on August 5.
10:47am: The clinical note added 'as now well and sugars stable, for no further [investigations]. "If hypoglycaemia again at any point for repeat screen." The doctor says if Child F had any further episodes of low blood sugar, then the blood test would be carried out again.
10:50am: The prosecution ask if anything was done with this data. The doctor says it was looked to see if anyone else at the time was prescribed insulin in the whole neonatal unit, for a possible 'accidental administration', but there were no other babies at that time. No further action was taken. Ben Myers KC, for Letby's defence, asks to clarify that Child F's blood sugar had stabilised at that time. The doctor agrees. The doctor clarifies, on a question from the judge Mr Justice James Goss, that the scope of the 'insulin prescription' checks were made for August 4 and August 5.
10:55am: A video is now shown to the court demonstrating how an Alaris pump, for infusions, is used at the Countess of Chester Hospital. The pump has an air sensor at the machine part, and the video explains there is no real way air could be added at any point in the infusion line. The machine can be set to administer an infusion from a TPN bag, down a line, at variable rates per 24 hour periods.
10:57am: The machine gives off an alarm if there is an 'occlusion' - or blockage - along the line. The alarm can be silenced for two minutes by pressing a button. While that alarm is silenced, a red button would flash on the top of the machine.
11:03am: An event log is displayed on the machine showing when the infusion starts/stops, if the rate is changed, and if it is primed. The machine can store 100 events, and the log cannot be deleted by staff while it is on. If the pump is switched off, and on restarting the option 'clear setup' is made, the event log is wiped. The video explains that typically the events on there are not logged by Countess staff unless they are in relation to a serious health issue with the patient.
11:07am: The video demonstrates what happens when an 'air bolus' - or air down the line - is in place when the machine is active. The machine displays an 'occlusion' text warning and an alarm goes off. A harsher sounding alarm then sounds, with 'air-in-line' displayed on the screen. The machine can infuse at a maximum rate of 100ml/hr, the court hears.
11:14am: The next witness to give evidence is Dr John Gibbs, who was a consultant paediatrician in August 2015. He was the 'consultant of the week' the week when Child E and Child F were born, and the clinical responsibility meant he would go around the neonatal unit for a full examination, in addition to going around the unit every other day for observations, but not a full examination. He said that was 'standard practice' for consultants in hospitals across the nation, as had been the case for many years. He adds the number of neonatal unit deaths up to 2015 were within the normal range or lower than the average, up to 2015-2016. He said the practice has since changed in 2016, in many hospitals, for there to be a 'consultant of the week' in the neonatal unit, and a separate 'consultant of the week' in the paediatric ward. He said, for the Countess of Chester Hospital, it had followed the higher than expected mortality rate in the neonatal unit in 2015-16.
11:17am: Dr Gibbs says the blood glucose levels for Child F, as noted by a colleague, soon after birth were 'satisfactory' at 2.7, as it should ideally be 'above 2.6'. He said the following reading was '1.9', and that can be a 'natural consequence of the separation of baby from mother', so was not unusual in itself, and was more commonly seen in premature babies, the court is told. Child F was "struggling with his breathing", so was started with an infusion with glucose.
11:21am: The blood gas readings for Child F are shown for July 30-31, Child F having been born on July 29. The glucose reading at 9.57pm for July 30 is '15.1' - an 'abnormally high' amount. Dr Gibbs says the reading shouldn't go above 7. He says that could be an indication for infection, and Child F was on antibiotics. A single high blood sugar level reading would be monitored, and repeat high readings would lead to action taken, Dr Gibbs tells the court. Because the blood sugar level reading on July 31 at 12.22am was 13.9, Child F was administered with insulin, "in a very small dose, carefully controlled", Dr Gibbs says.
11:22am: Dr Gibbs says the administration of insulin at 3.40am meant the junior doctors had waited until a couple of high blood glucose readings had been recorded. At 4.41am, the blood glucose level was 8.7, and Dr Gibbs says that meant Child F was "responding well" to the insulin infusion.
11:24am: Dr Gibbs says the insulin infusion progress is "fairly predictable" and "you would expect" the blood sugar levels to decrease gradually. He said: "It remained lower," so the insulin infusion was stopped at 6.20am.
11:30am: Dr Gibbs' notes from August 2 are shown to the court, for his examination of Child F, a 'routine ward round'. Dr Gibbs said he had seen Child F's twin brother, Child E, just before. Child F was recovering from 'respiratory distress syndrome', was being treated for suspected sepsis, and had lost weight from birth, which was normal in newborn babies, the court hears. The blood sugar levels were still 'moderately high', between 5-10. He had 'some jaundice, which is common in premature babies', and a note for a heart murmur is made, but Dr Gibbs said he had not heard that upon examination of Child F. Child F was on 'standardised' TPN fluid nutrition administration, plus nasal gastric feeds with expressed breast milk. Dr Gibbs said 'standard' TPN bags would continue to be administered with newborn babies, with any tailored additives for babies, depending on their requirements, administered via a separate infusion method.
11:33am: Child F had 'intermittent desaturations', which were not a cause for concern, the court hears. Dr Gibbs said he couldn't hear a heart murmur, but the CPAP machine was on, so that may explain why he could not have heard any heart murmur - "or there may have been no heart murmur there". Nurses had tried Child F off CPAP [breathing support] earlier that morning, which had led to oxygen desaturations, so he was put back on CPAP. Dr Gibbs said Child F was likely recovering from respiratory distress syndrome. The plan was to increase Child F's nasogastric milk 'as tolerated'.
11:38am: Dr Gibbs says the milk feeds were subsequently increased in the following days. At August 5, at 1.30am, Dr Gibbs was on call when Dr Harkness reviewed Child F, following concerns over vomit and heart rate. Dr Gibbs was telephoned at 3.30am. Dr Gibbs was told about the 'multiple small milky vomits and 9ml milky aspirate', and a heart rate above 200bpm, which he says was "high even for a premature baby". Dr Gibbs said otherwise, Child F presented as a healthy baby. The "sudden" increase of heart rate to over 200bpm was "very unusual". Dr Harkness had 'assumed' the change in observations was down to an infection, and Dr Gibbs agreed, but Dr Gibbs said it was "a very rapid change, even for infection", and there would normally be signs of Child F deteriorating beforehand. The plan was to rescreen for infection and start a new line for different, second-stage antibiotics.
11:43am: The August 5 intensive care chart for Child F is shown to the court. Dr Gibbs said as the nasogastric feed tube was stopped [nil by mouth], that meant the TPN bag had to be changed to account for the administration of new medication, via a long line. The blood glucose reading for Child F is 0.8 - "abnormally low" at 1.54am. The August 3-4 readings shown are between 3.8 and 5.4, which Dr Gibbs says were normal.
11:47am: Dr Gibbs says 0.8 is a "worryingly low reading for a baby". A bolus of glucose was administered, with Dr Harkness giving an additional administration of glucose and sodium chloride, to 'keep the blood sugar level up'. The following blood glucose reading of 2.3 at 2.55am was "much improved" but still low, so the plan for that would have been to continue to monitor the readings "carefully", Dr Gibbs says.
11:52am: The additional provision was administered at 4am. A reading of 2.9 was subsequently recorded. Dr Gibbs said Dr Harkness likely had concerns over the heart rate raising suddenly, wondering if Child F had an "inherent problem" with the heart rate - [Supraventricular tachycardia (SVT)]. However, those readings would see a heart rate of over 300bpm, so was recorded as "unlikely" on Dr Harkness's clinical note. The consultation on the phone concluded infection as a possible cause, but the readings were "unusual to have such a sudden change in his observations". Dehydration was also a possible cause. Fluids and saline were administered to treat the possible causes.
11:56am: Dr Gibbs said that Child F had an "extremely high" level of insulin in his body later that day, as revealed by a subsequent test result. He added: "It makes it likely that his symptoms were related to very low blood sugar, [and can only be explained] by him receiving a high dose of insulin." He said this was something he had concluded in hindsight. He had not come to this conclusion at 3.30am [during the telephone consultation], as he would not have had any reason to believe insulin had been administered.
12:01pm: Dr Gibbs' notes from 8.30am on August 5 recorded a 'natural increase in heart rate' due to Child F's stress. The blood glucose reading was '1.7' despite administrations of glucose. He also had signs of decreased circulation - a sign that he was "stressed, dehydrated, or had an infection". While the blood sugar levels had risen to the '2's during the night, the latest reading of 1.7 was unusual and "unexpected" as Child F had had glucose administered, but did not seem to be responding.
Dr Gibbs: "At the time we didn't know this was because he had a large dose of insulin inside him". Query marks were put on the note for sepsis - but the blood gas reading showed no sign of this, and for gastro-intestinal disease NEC, which had 'no clinical signs', as Dr Gibbs notes. A plan was to give a 'further glucose bolus'. The 'query query' was to consult the new 'consultant of the week' for a possible abdominal x-ray to look for signs of NEC, but Dr Gibbs tells the court this was not likely.12:08pm: At 11am, the TPN, which includes 10% dextrose, was 'off' as the line had "tissued", and it was restarted at noon. That TPN was stopped at 7pm, and replaced with a 15% dextrose infusion, Dr Gibbs tells the court. Dr Gibbs says the blood sugar levels remained "low, sometimes worryingly low" throughout the day. The reading was 1.9 for much of the afternoon, despite three 10% dextrose boluses being administered during the day. He adds after 7pm, the blood sugar readings, "at last", go to a "normal reading" of 4.1 by 9pm. Dr Gibbs says the dextrose administrations had some minor effect at times, other times no effect. He tells the court the assumption was infection, but it was "unusual" to have the blood sugar level remain so low, even with administration of 10% dextrose boluses, and that was what led to the call for a blood test to be carried out at the laboratory in the Royal Liverpool Hospital.
12:13pm: The blood sugar reading at 5.56pm on August 5 was "abnormally low" at 1.3, and the test was sent out to another laboratory as testing for insulin levels was a relatively "unusual" test. The test result is shown to the court. Dr Gibbs explains the readings. He says the cortisol reading is 'satisfactory', but the "more relevant" reading was insulin. "There should be virtually no insulin detected in the body...rather than that, there is a very high reading of 4,657". The insulin C-peptide reading should, for natural insulin, should be even higher [than 4,657] in this context, Dr Gibbs explains, but it is "very low" The ratio of C-peptide/insulin is marked as '0.0', when it should be '5.0-10.0' Dr Gibbs says the insulin c-peptide reading should be at 20,000-40,000 to correlate with the insulin reading in this test. The doctor says this insulin result showed Child F had been given a pharmaceutical form of insulin administered, and he "should have never received it".
12:32pm: The court is resuming after a short adjournment. Ben Myers KC, for Letby's defence, explains on this count [for Child F], Dr Gibbs will not be asked any questions on his evidence. He adds that Dr Gibbs will be cross-examined on a future occasion in the trial on evidence that has been raised.
12:33pm: The video showing the Alaris pump demonstration is shown to the court once more. Technical difficulties meant the final 90 seconds of the video were not replayed first time round.
1:55pm: The trial will resume shortly following its lunch break.
1:58pm: Members of the jury are now coming into court. The next witness to give evidence is a nurse who cannot be named due to reporting restrictions. She has previously given evidence in the trial, and is now giving evidence in the case of Child F.
2:01pm: The nurse confirms she had some involvement in the care of Child F, but was not the designated nurse. She confirms she administered an infusion of glucose to Child F on August 5 at 8.30am. She says it would have been a bolus of glucose given as a "push" response to low blood sugar.
2:11pm: An Alaris syringe driver video is displayed to the court, showing how a syringe dose can be electronically administered via infusion, at various rates. These rates can be locked. It is similar to the Alaris pump, and has alarms if the syringe is not loaded properly, if the infusion has been placed 'on hold' for a certain length of time, if the rate has been changed but has not been confirmed, if the infusion is complete, if there is a power failure or low on battery, if there is an error message. The alarm colour would be amber on the machine, and can be paused for two minutes. An event log would be available on the machine for 24 hours. The nurse confirms it was a standard machine used at the Countess of Chester Hospital, and was standard practice. The nurse said the event log wouldn't be looked at routinely by staff.
2:16pm: An 'occlusion' alarm would be a red alarm light, with an alarm sound. The syringe would be primed beforehand with the fluid, attaching the syringe to a line, and would be 'flushed' so no air would be present. The nurse says a different piece of equipment would be used for TPN bags, and this equipment would be used for the lipid [fats] element administered via syringe. The nurse says this equipment would be used to administer smaller amounts of fluids, such as 10% dextrose, or a saline bolus, or antibiotics.
2:20pm: The video demonstrates an 'accelerated rate' of a drug could be administered via infusion via a 'purge' function on the machine, which would be used as a possible bolus administration. The nurse says that 'purge' button would not be used at the Countess of Chester Hospital, and was not standard practice.
2:22pm: The video adds the 'purge' function would not add to the total millilitres of infusion administered on the machine's display - ie, any fluids administered during that 'purge' time would not be added to the total the machine had calculated so far. The machine also does not have the ability to detect air, the video presented to the court concludes.
2:31pm: An IV administration chart for August 5 is shown to the court, with four 10% dextrose infusions focused on. The nurse has co-signed for two of the four administrations, both boluses at 8.30am and 3.15pm. One more would have been through a bolus and another via an infusion at a certain rate, which would require mechanical assistance. The nurse said she would have delivered the two boluses she signed for as a 'push' infusion (ie, push the fluid manually via syringe attached to a clean, 'flushed' infusion line), and the process would be 'straightforward'.
2:40pm: The nurse is shown a note from the 'grand round', which the court heard was carried out by the on-call consultant each Wednesday. The note 'new long line' was made, and the nurse says that was because the existing long line had tissued. The new long line was made at noon on August 5.
2:44pm: The nurse says her normal practice would have been for putting a new bag of fluids on the long line.
2:45pm: The Alaris pump video is shown once again to the court, for the nurse to provide potential further context on what is demonstrated in the video.
2:48pm: The Alaris pump would be used in connection with TPN bags. The nurse says while there is an input port on the TPN bag, she would not input anything manually in conjunction with the machine. The output port would be used for 'giving' the infusion to the patient.
2:54pm: The nurse confirms a 10% dextrose administration was given to Child F at 3.30pm via an infusion. She tells the court the 10% dextrose infusion would have been administered, in addition to the existing dose from the new bag at noon, as the blood glucose level was still low for Child F. The nurse says the 3.30pm dose would have been administered via a syringe. Lipids would have been administered via a syringe driver.
3:01pm: The court is shown a 15% dextrose dose, plus sodium chloride, is administered for 7pm on August 5. The nurse has signed for that medication administration. The nurse is also a co-signer for medication at 2am on Thursday, August 6. The nurse explains the practice was someone from the day shift (in this case, herself) would co-sign for the drug during the day, then she would in practice text the person who was administering it to confirm it had been administered, and that the scheduled dose could be taken 'off the system' and wasn't at risk of being administered twice.
3:07pm: Ben Myers KC, for Letby's defence, asks about the administration of the drugs, and how they are administered. The nurse says the 10% dextrose would come in 500ml bags, and can be divided up on the unit for infusions, or come available via the pharmacy in 50ml pre-made doses. The nurse says she does not have an independent recollection of the event. She confirms if the long line is tissued, it cannot be used again. Mr Myers says if the long line is changed, then everything else is changed to avoid infection, including the TPN bag. The nurse confirms that would be the case.
Mr Myers: "You wouldn't put up an old [TPN] bag, would you?" The nurse: "I wouldn't, no. And we wouldn't have put it up as we would have documented that."3:08pm: Mr Myers says as a general rule, TPN bags would run for 48 hours unless there was a problem, and there would be a stock of maintenance bags in the fridge. Mr Myers says one of those would have been used in the course of this. The nurse agrees. The nurse says such bags are checked every night and if any were being used or out of date, then the stock would be replenished.
3:10pm: Simon Driver, for the prosecution, asks about the stock bags in the refrigerator. He says every night, a check would be undertaken to see if any had been used. He asks how the checker would know if they had been used. The nurse says if there weren't the stock five TPN bags in the fridge, new ones would be ordered. The refrigerator would have 'start-up' TPN bags and 'maintenance' TPN bags of nutrition. The nurse says there may be fewer 'target stock' of the 'start-up' TPN bags.
3:11pm: Each of the bags would have a dated 'shelf life' the court hears. The nurse says the bags would not be ordered in any particular fashion in the fridge.
3:15pm: A video of glucose/dextrose administration is played to the court. The procedure is described as a 'two-person procedure'.
3:23pm: A question from a juror asks if the syringe driver could administer an infusion if the line has not been primed (ie if the line still has air in it). The nurse confirms that would be the case. The equipment could have a filter connected, but it was the practice that the line would be primed before use.
Friday 25th November 2022
Child F
Dr Anna Milan (Clinical biochemist) - Professor Peter Hindmarsh - Dr David HarknessChester Standard Live Reporting
10:36am: The trial has now resumed. The court is hearing from Anna Milan, a clinical biochemist, how insulin and insulin c-peptide tests were taken for analysis.
10:47am: Child F's blood sample, which was dated August 5, 2015, was taken at 5.56pm. The court is shown a screenshot of Child F's blood sample results. Child F is referred to as 'twin 2' - Child E, the other twin boy, had died at the Countess of Chester Hospital on August 4. Dr Milan says Child F's insulin c-peptide level reading of 'less than 169' means it was not accurately detectable by the system. The insulin reading of '4,657' is recorded. A call log information is made noting the logged telephone call made by the biochemist to the Countess of Chester Hospital, with a comment made - 'low C-Peptide to insulin'
10:55am: The note adds '?Exogenous' - ie query whether it was insulin administered. The note added 'Suggest send sample to Guildford for exogenous insulin.' The court hears Guildford has a specialist, separate laboratory for such analysis in insulin, although the advice given to send the sample is not usually taken up by hospitals. Dr Milan said that advice would be there as an option for the Countess of Chester Hospital to take up. Dr Milan said she was 'very confident' in the accuracy of the blood test analysis produced for Child F's sample. Ben Myers, for Letby's defence, asks about the risk of the sample deteriorating if it is not frozen. Dr Milan said the sample arrived frozen. If it wasn't frozen, it would be accepted in 12-24 hours. She said the laboratory knew it arrived within 24 hours, and adds Chester has its own system in place to store the blood sample before transport.
10:57am: Mr Myers said the Child F blood sample would have been stored for seven days [in Liverpool], then disposed of. Dr Milan agrees.
10:58am: On a query from the judge, Mr Justice James Goss, Dr Milan explains how the blood sample is frozen and kept frozen for transport. She said the sample would not have been taken out of the freezer in Chester until it was ready to be transported.
11:02am: The next witness to give evidence is Professor Peter Hindmarsh, an expert witness. He explains to the court he is professor of paediatric endocrinology at University College London and consultant in paediatric endocrinology and diabetes at University College London Hospitals. Nicholas Johnson KC, for the prosecution, asks whether Professor Hindmarsh was contacted by Cheshire Police in connection with the case of Child F. Professor Hindmarsh confirms he was.
11:04am: Professor Hindmarsh confirms he had been told there was a suspicion Child F had received insulin in an 'exogenous' way - ie the insulin was not produced within the body.
11:06am: He said he concluded the cause of the hypoglycaemia was exogenous, and the chemical findings were compatible with the administration of exogenous insulin.
11:13am: The court hears about Child F's blood sugar being slightly below normal, just after birth, and he was given 10% dextrose, and that resolved the blood sugar level to a normal rate. There was also a point around July 30-31 when Child F's blood sugar level rose to a higher than normal rate, and he was given a tiny amount of insulin to lower the rate. Subsequent blood sugar readings returned to normal. The court is now shown Child F's observation chart for the night of August 4-5. Child F's heart rate rose from around 150bpm to 200-210bpm between 1.15am-4am. Child F had received a TPN bag of nutrition at 12.25am on August 5. Child F's blood sugar reading at 1.54am was 0.8. Professor Hindmarsh says it is a "significant" difference and "extremely low".
Mr Johnson: "Was it a cause for concern?"
Professor Hindmarsh: "Absolutely."11:16am: A table, created by Professor Hindmarsh, records all of Child F's blood sugar readings from 11.32pm on August 4 to 9.17pm on August 5.
They are:
5.5 (August 4, 11.32pm)
0.8 (August 5, 1.54am)
2.3 (2.55am)
1.9 (4.02am)
2.9 (5am)
1.7 (8.09am)
1.3 (10am)
1.4 (11.46am)
2.4 (noon)
1.9 (2pm)
1.9 (4pm)
1.9 (6pm)
2.5 (7pm)
4.1 (9.17pm)A reading of 'above 2.6' is considered 'normal'. Professor Hindmarsh says the hypoglycaemia is "persistent" right through the day until the conclusion of the TPN bag at 6.55pm.
11:19am: The 5am reading of 2.9, which the court hears is considered a 'normal' blood sugar reading, is gone into further detail. Mr Johnson asks the court to show the intensive care chart for Child F for August 5. For the 5am reading, the blood sugar reading signature has the initials 'LL'.
11:24am: The chart also shows Professor Hindmarsh's notes to provide context for the blood sugar readings throughout the day, when changes are made to the infusions for Child F. Professor Hindmarsh says the hypoglycaemia continues "despite" five boluses of 10% dextrose and "ongoing" glucose delivery from the 10% dextrose infusion, and the glucose contained within the TPN bag. He says that would, in total, give a glucose infusion which would be, at minimum, "twice the normal [daily] requirements of a baby". He said it is likely more glucose was being delivered from the bolus injections.
11:26am: Professor Hindmarsh had noted three events during August 5, after 1.54am, when the TPN bag was administered. At 10am, there were problems with the cannula infusion which meant the line had to be resited, and fluids were discontinued. The two further glucose readings after are '1.4' and '2.4', "implying" that the blood glucose level had started to rise "spontaneously" as there was "no contribution from the intravenous route".
11:28am: Mr Johnson said after Child F was taken off the 'double' dose of dextrose during that time, his blood sugar levels "actually rose".
Professor Hindmarsh: "That's how I see it, and I believe that is correct".11:30am: The reading was "heading in the wrong direction" down to 1.9 by 2pm, the court hears. The infusions stopped at 6.55pm.
Mr Johnson: "Is there a paradox between a child receiving glucose and their blood sugar falling?"
Prof Hindmarsh: "Correct."11:34am: The 5.56pm blood sample for Child F is referred to, which has a blood sugar reading of 1.3. Mr Johnson asks about the apparent disparity. Prof Hindmarsh says the laboratory reading of blood plasma of '1.3' differs from the neopatient reading of '1.9' (taken at 6pm). He explains a discrepancy of up to 0.8 between the two is considered acceptable. He says whichever the more accurate reading is 1.3 or 1.9, it is still "very low".
11:37am: Child F's blood test result from the laboratory, as shown earlier to the court today, is presented to Professor Hindmarsh. The sample was taken at 5.56pm on August 5 and collected at the Liverpool laboratory at 4.15pm on August 6. He says the insulin reading should be in proportion to the insulin C-Peptide reading, and should be several times higher in this context.
11:41am: Prof Hindmarsh explains to the court the dangers of prolonged low blood sugar in the body, which can lead to damage to the brain. Breakdown of fats can be used as a temporary measure, as a substitute. The problem, he says, is if the low blood sugar is caused by excess insulin. The insulin will 'switch off' key body formation. He says the brain would be in a "very, very susceptible state to receiving damage". That depends on the depth and length of the hypoglycaemia episode. An equivalent reading of 2.3 or so would lead to 'confusion' and difficulties reading/writing. Professor Hindmarsh says lower readings than that could lead to seizures, death of brain cells, coma, and in some cases, death.
11:47am: Professor Hindmarsh added, in his report, the insulin used in the hospital, has been used in the past 20-25 years, and is synthetic insulin. Stocks of pig/cow insulin would not be held as regular stock or in a pharmacy. They would have to be requested. The two types of synthetic insulin are fast-acting - ones that work within 30 minutes, applied via an injection, the effectiveness lasting 4-6 hours. The other type is long-acting, which lasts up to 12-24 hours. The second type of insulin, he explains, is not generally used for intravenous infusions, and he has never seen any evidence of that having been done.
11:50am: Professor Hindmarsh is shown a 10ml bottle of insulin, which normally comes with an orange, self-sealing cap. To extract the liquid from the bottle, to administer 'therapeutically', a medical professional would have to use a syringe, the court hears. Mr Johnson says by 'therapeutically', Professor Hindmarsh means 'legitimately'. Professor Hindmarsh agrees, and says the dose would have to be measured out carefully.
11:52am: The insulin bottle exhibit is shown to members of the jury and the defence.
12:00pm: Once a syringe is put into the bottle, the bottle self seals after the syringe is removed, the court hears. Professor Hindmarsh says it is not possible to give insulin by mouth as it is a large molecule, so cannot be absorbed easily and the protein would be broken down by the acid in the stomach. It could not have been administered via the nasogastric tube for the same reason. The only ways would have been through a skin injection or intravenously, he says. For a skin injection, he says the duration of action [for the insulin] of 4-6 hours would not fit with the 17 hours of hypoglycaemia. It would require multiple injections. He says an intravenous route "would be the most likely explanation". The way to do so would be a bolus of insulin - from testing in endocrinology, the blood sugar level would fall within 90 minutes, then rise back to normal. To maintain hypoglycaemia "over a protracted period of time" would require multiple insulin boluses "roughly every two hours". The second route would be via infusion - "probably the most likely way of achieving the blood glucose effect that we have observed". The infusion would be "continuous", using the bags available, and "fit nicely" with the time course of events. It would "also be consistent" with the measurements that took place during and after the TPN bag was replaced.
12:03pm: Professor Hindmarsh says the exogenous insulin, if the fast-acting type, would have reduced from the '4,657' reading to 'almost none' after a couple of hours after the TPN bag was removed. The rise of the blood glucose level in Child F to 4.1 by 9pm was "entirely consistent" with that.
12:16pm: Professor Hindmarsh says a rate of about 0.56ml/hr of insulin would have been required to lower Child F's blood sugar levels on the TPN bag. This was calculated given the insulin level administered to lower Child F's blood sugar levels on July 31.
Mr Johnson: "Would that level have been visible to the naked eye?"
Prof Hindmarsh: "No." Mr Johnson asks if the stock TPN bag was contaminated to the same degree as the bespoke bag. Prof Hindmarsh says the glucose concentrations are not much different from 1.54am-10am, when the bag is changed, and after then. "The contents [and contamination] are probably about the same." Mr Johnson asks about Professor Hindmarsh's conclusion, that the fluid he was receiving could only have been contaminated with insulin. "Yes I do."12:45pm: The trial is now resuming after a short lunch break.
12:50pm: Ben Myers KC, for Letby's defence, is now asking Professor Hindmarsh questions. He said the fast-acting insulin would not be visible. Professor Hindmarsh confirms that type of insulin would have a "distinctive smell" about it. Mr Myers says the concentration of insulin administered could, over time, could lead to complications for the patient.
Prof Hindmarsh: "That is correct."12:57pm: Mr Myers said it would be about 25 minutes before the insulin administered would have its effect. Prof Hindmarsh said it would take about 25 minutes for it to have its biggest effect. Mr Myers says other than the heart rate and vomiting, Child F did not appear to suffer any other physical symptoms than the low blood sugar levels. He asks, given the high level of insulin seen, would there be "more powerful, physical consequences?" Prof Hindmarsh says vomiting is not an unusual feature. In the magnitude of features, he says, the effects would be on brain function rather than any other peripheral manifestations. He said physical features of hypoglycaemia would "not be easy to pick up in a newborn, or a premature" baby. "Neurologically, that's different." The features would also be "extremely variable". The first symptom "could, and would often be, collapse and seizure". Mr Myers says it is an alleged 17-hour period of exposure of high levels of insulin, and if the effects would have been more apparent. Prof Hindmarsh says high levels of insulin have been recorded in babies with underlying conditions, and they present well up to the point of collapse.
1:03pm: The intensive care chart for Child F is presented to the court again. The blood sugar reading of 2.9 is recorded for 5am. "2.9 would present in the normal range wouldn't it?" A normal range would be 3.5 or above, Professor Hindmarsh says. A reading of 0.8 is at 1.54am, and 2.3 at 2.55am. Mr Myers says, while low, that is a "significant increase". He shows an IV chart, in the intervening period at 2.05am, an administration of 10% dextrose for Child F.
1:05pm: Mr Myers says the infusion chart, shown to the court, has a 10% dextrose bolus at 4.20am. Mr Myers adds between 4.02am and 5am, the blood glucose reading for Child F rises from 1.9 to 2.9.
1:12pm: Mr Myers refers to the level of contamination in the TPN bags. He refers to the blood sample taken at 5.56pm on August 5, nearly 17 hours after the first TPN bag was put up for Child F. He says that reading "only applies to the second [TPN] bag."
Professor Hindmarsh: "It did, yes."
Mr Myers: "That won't tell us what the insulin level was at 12.25am, would it?"
Prof Hindmarsh: "No, it won't. we haven't measured that." Mr Johnson, for the prosecution, rises to clarify insulin levels. He asks would it be reasonable to infer that if Child F has similar blood glucose levels throughout the day, he had had similar insulin levels inside him during that day. Professor Hindmarsh says there is a caveat in that there had been efforts to raise Child F's blood sugar during the day through 10% dextrose boluses. "Overall, the infusion [rate] has essentially stayed the same. "I can't be absolutely sure...but it's safe to assume that the glucose infusion rate did not change, which would imply that the amount of insulin around would be similar throughout the 17-hour period - allowing for the breaks when the infusion was discontinued." He adds that would be his conclusion.1:14pm: Mr Myers has one more query, to which Professor Hindmarsh clarifies that a measurement of blood glucose is not a measurement of insulin or insulin C-Peptide, but there are 'clear relationships' between the two, and what they would be expected to be.
1:16pm: He adds the blood glucose level, via infusion, was consistent, and "it would be reasonable to assume" the insulin infusion would also be at the same rate was it was at 5.56pm as it would be as earlier in the day.
1:18pm: Dr David Harkness is being recalled to give evidence. He has previously given evidence in the trial, and was employed at the Countess of Chester Hospital in summer 2015 as a paediatric registrar. He is being asked about the night shift of August 4-5, and confirms he was accompanied by Dr Christopher Wood. Notes showed he saw Child F on three occasions during that night shift.
1:23pm: He is asked about the 1.30am observations for Child F on August 5, of milky vomit and high heart rate. He confirms the observations were made by himself. He noted a 'soft continuous murmur' which is 'very common in babies'. The plan was to rescreen, and use a second line for antibiotics. There were "concerns" for Child F's heart rate, and that Child E, the twin baby boy, had passed away the previous night.
1:29pm: Dr Harkness's notes are shown to the court from 2.30am. He noted Child F had 'large milky aspirate' and was 'quieter than usual'. He said, from the heart rate observations being 'higher than normal', he was troubled by the possibility of infection, stress and pain, but those heart rates would go to 180bpm, not 200-210bpm, and come back down after a few seconds/minutes, not remain constantly high. A septic screen and a number of blood tests were called for. The blood sugar level of 0.8 [underlined on the note] was "very low". Child F was "handling well" and pink and well perfused, indicating good circulation, Dr Harkness says, with heart sounds 'normal', but with a very quiet murmur.
1:32pm: The two problems were hypoglycaemia and tachycardia. Dr Harkness's plan was for a dextrose bolus, a saline bolus, antibiotics, an ECG, and to consider medicine to slow the heart rate down - but that medicine had its risks and would only be used in the event of supraventricular tachycardia.
1:36pm: Dr Harkness's note at 3.30am for Child F showed a heart rate of 204. A discussion with the on-call consultant Dr John Gibbs, in which it was decided it was unlikely Child F had supraventricular tachycardia as the heart rate would be closer to 300bpm. Dr Gibbs suggested repeating the fluid bolus, continue to monitor Child F, and only to consider the heart-slowing medicine if the heart rate rose to near 300. A blood gas reading suggested Child F was dehydrated at this time. The plan was to continue to monitor Child F's sugar levels.
1:41pm: A 10% dextrose infusion is administered for Child F at 3.50am, plus a 10% dextrose bolus at 4.20am. Dr Harkness said the administrations had "an effect", but the blood sugar levels "kept drifting up and down". Mr Myers, for Letby's defence, says there will be no questions asked for Dr Harkness at this time.
Monday 28th November 2022
Child F
Dr Satyanarayana Saladi (Consultant) - Dr Alison Ventress (Registrar) - Unnamed nurse10:12am: I'm back at Manchester Crown Court for the murder trial of nurse Lucy Letby. Jurors will continue to hear evidence in relation to Child F this morning, who survived after allegedly being poisoned with insulin by Ms Letby, who denies all charges against her
10:33am: Consultant paediatrician Dr Satyanarayana Saladi is in the witness box. He is taking the court through his notes from August 2015 when Child F was at the Countess of Chester
10:47am: Dr Saladi is taking jurors through clinical notes from early August 2015 which show Child F's blood sugar levels were low. Other measures such as white blood cell levels were in the 'normal range' and the baby was 'handling well'
10:50am: The medic says that there was no abnormal breathing or heartrate and no abnormal bowl sounds. He assessed the baby's condition as 'satisfactory' on the morning of August 5
11:06am: Dr Alison Ventress, who was a registrar at the Countess of Chester in 2015, is now in the witness box. She's taking the court through medicine charts recorded in the days following Child F's birth
11:27am: She explains that a dose of insulin would always be prescribed by a doctor and it would always be administered as a separate infusion, never added to another fluid
11:50am: A nurse, who cannot be named for legal reasons, is now giving evidence. She is going over her notes from the morning of 3 August 2015, which show that Child F was in some respiratory distress, but was coping well. By the end of her shift that day he was 'satisfactory' showing 'no signs of any issues'
12:03pm: The nurse's notes show that in the hours before Child F's heart rate surged to over 200bmp and his blood sugars dropped, he was stable and handling well Her notes also show that Child F was, at the request of his parents, due to be moved from the Countess of Chester to another hospital, but the transport team was unavailable due to another unrelated emergency
12:42pm: Another nurse, who also cannot be named for legal reasons, is now in the witness box. Again she is taking the court through Child F's breathing/heart rate charts from her night shift - all showing the infant was 'stable'
12:54pm: The nurse said she had 'no concerns' about Child F on the evening of August 4
2:03pm: We're back after a short break. A former nursing colleague of Ms Letby, who cannot be named for legal reasons, is continuing to give evidence. She's talking the jury through Child F's medical charts in the days after his birth
2:15pm: The nurse is talking the court through the process of fitting a new babiven bag (used to supply fluids/medicines). She says the bags are checked by two nurses and says nothing new would be added to the bag once it was made up
2:33pm: Her note from the early hours of August 5 show that Child F 'became quieter' and was 'slightly jaundiced'....doctors administered fluids and medicines and he became 'more lively' as a result. She said that during this period his blood sugar levels were 'dangerously low'
2:48pm: The nurse observed that Child F had been 'nice and stable' but in the hours between midnight and 1am his heart/breathing rates 'suddenly' rose to a 'concerning level'
3:29pm: The jury are now being shown a 22minute instructional video on how intravenous bags are manufactured and prepared (this is to aid with understanding of evidence due to be given tomorrow, which the prosecution say is fairly technical)
4:06pm: Court has now adjourned for the day, back tomorrow.
Chester Standard article 28-11-2022
A NURSE who was working with Lucy Letby when a baby was allegedly poisoned has denied adding anything to his feed bag.
Letby, 32, is said to have tried to murder the premature twin by intentionally giving him insulin on the Countess of Chester Hospital's neonatal unit.
The prosecution say she struck after midnight on a night shift starting on August 4, 2015 as the youngster, referred to as Child F, received a new feed of nutrients via a bag connected to an intravenous line.
On Monday, November 28, the jury at Manchester Crown Court was shown a form signed by Letby and her colleague confirming the nutrient bag was changed at 12.25am on August 5.
The colleague, who cannot be named for legal reasons, said she had no recollection of the specific event and could not be sure whether it was Letby or her who put up the bag.
Philip Astbury, prosecuting, asked the nurse if she had put anything in the nutrient bag.
She replied: "Absolutely not."
She also answered "no" when asked if she gave Child F any insulin at any stage during that shift, in any way.
The court was shown messages sent between the witness and Letby after their night shift, in which they agreed Child F was a "worry" and Letby said: "Something isn't right if he's dropping like that."
The nurse said Child F's observations had been "within normal limits" before midnight.
She said: "I was really happy with him."
She told the court tests from the earlier part of her shift showed he had a "good blood sugar level" and no concerns were raised when she had a handover at the start of her night shift.
She said: "He'd been nice and stable for me in the evening and, in fact, in the earlier part of the evening when I wasn't there you can see the recordings are all within a similar level that we were happy with."
At a point between midnight and 1am, the child's heart rate and breathing rate "suddenly" went up to concerning levels, the court heard.
She agreed the change was worrying, and added: "Especially in the context that you can see from above they (his levels) have been nice and steady and stable for a while."
The nurse said she asked a doctor to review the baby and tests showed his glucose level was "dangerously low".
The court has heard his glucose levels remained low on the day shift of August 5 even after the intravenous line, and a connected bag containing nutrients, needed to be replaced after swelling to Child F's leg.
Child F's blood glucose rose to safe levels later that evening after the nutrients were stopped and extra sugar was given independently, the court was told.
He went on to make a full recovery and was later discharged.
Last week, three other colleagues – Shelley Tomlins, Sophie Ellis and Belinda Williamson – also denied giving insulin to the baby.
Letby is accused of trying to kill Child F less than 24 hours after she allegedly murdered his twin brother, Child E, by injecting air into his bloodstream.
The defendant, originally from Hereford, denies murdering seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Tuesday 29th November 2022
Child F
Professor Sally Kinsey (haematologist - evidence for Child A, B, E & F) - Ian Allen (Pharmacy)Chester Standard Live Reporting
10:42am: There is a delayed start to today's trial, and it is currently scheduled to begin at 11am.
11:13am: The legal teams have now arrived in court, but there will be a little further delay before the case is expected to resume.
11:26am: The judge, Mr Justice James Goss, and Lucy Letby are in the courtroom, with members of the public also now filing in. The trial will resume shortly.
11:29am: The trial has now resumed. Professor Sally Kinsey, a blood expert, is going to give evidence in relation to a number of the cases so far in the trial.
11:32am: Professor Kinsey confirms she was approached by Cheshire Police to look at several cases in the course of this trial. One is yet to come, while the other three are the cases of Child A and Child B (both twins) and Child F. She also confirms she has looked at the records of Child F's twin brother, Child E, for the purpose of her investigation. She has written reports for each case and set out the relevant backgrounds for each child, the court hears.
11:45am: Her first report is dated March 4, 2020, relating to Child A. The court hears the conditions that Child A and Child B's mother had before her birth, and the decision to deliver the twins by C-section in June 2015. The events of Child A's treatment at the Countess of Chester Hospital neonatal unit, subsequent collapse and death, are relayed in court.
11:57am: Child A's blood count was considered 'normal' for his age. She said she had considered whether Child A's mother's auto-immune disease could have been a significant factor in the death of Child A. Said auto-immune disease was a rare condition (affecting about 50 in 100,000 people) which affected the mother, which can cause increased blood clotting. It is "well recognised" that pregnancy can cause issues, which can cause nutritional problems for babies in the womb, and a C-section can be required "to save the life of the mother and the child". The court hears it can cause premature birth and blood clotting for the mother. Nicholas Johnson KC, for the prosecution, asks: "Did the...syndrome pass on to [Child A or Child B]?" Professor Kinsey: "No, that is not the case."
11:58am: Mr Johnson says there was concern the condition had passed from mother to son, but says Professor Kinsey is sure it did not. "It didn't," Professor Kinsey replies.
12:02pm: Prof Kinsey says, for the conclusion of air embolus for Child A, the doctors' descriptions of skin discolourations on the baby had "cemented" her concerns. She adds it is very "rare" and has not seen it in her experience, but she says she has read it from literature, and the skin discolorations are a "stark" feature. Prof Kinsey says she is sure the cause of Child A's death does not have a haematological origin.
12:16pm: The case of Child B, a baby girl, is now being discussed. The events of Child B's treatment at the neonatal unit and her collapse are relayed to the court. The jury is being shown clinical records which have previously been shown as part of the sequence of events and from doctor/nurse witnesses. Prof Kinsey confirms she had noted what was written for Child B's skin discolouration on June 10 - the 'purple blotching'. For all the blood results Prof Kinsey had seen, she said they were 'normal' for her age and the time the tests were taken. There was, like Child A, no passing on of the mother's auto-immune disease to Child B, she adds. The question of air embolus is raised. She said she had made similar observations to Child A. The professor says there was no haematological evidence that could have caused Child B's collapse, and wanted to draw attention to the skin discolouration in the area around the chin, which she said was most likely a 'rash' caused when medical staff were trying to administer air.
12:24pm: The case now turns to Child E and Child F, and the sequence of events is relayed to the court. Prof Kinsey says to determine whether Child E had a hereditary blood condition, the records of surviving twin brother Child F were examined. The sequence of events is now relayed for Child E.
12:36pm: Prof Kinsey noted she had observed from the nursing notes, a nasogastric tube had been present for Child E, and the aspirates were 'unremarkable'. The abdomen was 'soft, not distended' and Child E's bowels opened. At August 3, 10.44am, Child E was 'pink and well perfused'. The professor confirms she had recorded Lucy Letby's nursing note for August 4, 2015, an observation chart for Child E on August 4, and blood gas record for Child E recording a decline for the baby boy.
12:40pm: Prof Kinsey said the "striking thing" was there had been a big change [a drop] in the haemoglobin levels for Child E from 10.21pm at August 3 to 1.05am on August 4. It was significant in that Child E had lost blood in the aspirates, and would only have had a calculated total blood volume of 142ml in his system at that time.
12:41pm: Prof Kinsey said, for her conclusion for Child E, the haemoglobin count had been normal, as had the platelet count, prior to the deterioration. "This was spontaneous bleeding, with no clear explanation."
12:46pm: The case now turns to Child F. Mr Johnson says the significance of Child F is on a comparative basis to identical twin brother Child E. Prof Kinsey confirms she has had access to Child F's medical records, which was for the context of Child E on a haematological level. She said she looked at the history of Child F, and 'one or two things happened' which helped her in her investigation. She said there were three blood investigations for Child F, over the space of two and a half years, which showed 'normal results'. Child F had had a physical accident when a small child, and there were no haematological-related problems when he was checked, the court hears. Child F was said to be 'slightly iron deficient' when tested at the age of two years old, but that was 'normal for infants'. The blood results were "completely normal" for Child F. The bleeding for Child E in August 2015, based on that medical history, was "not spontaneous", Professor Kinsey tells the court.
12:50pm: Skin discolourations were noted for Child E, the court is told. Mr Johnson asks about the issue of air embolus as a cause for Child E's death. Prof Kinsey has produced diagrams to display how an air embolus in the body can present itself externally. These diagrams are shown to the court.
12:52pm: Haemoglobin is found in red blood cells. Deoxygenated haemoglobin is blue in colour, while oxygenated haemoglobin is bright red. A diagram is shown on how part of the air/blood circulation system works in a body.
1:07pm: Further diagrams explaining the circulation system are presented to the court.
2:16pm: The trial is now resuming following a lunch break. Professor Kinsey is explaining, via diagrams, how the blood is pumped through the heart. She is now explaining an embolus, which is something which "shouldn't be there" in the body. It is most commonly found from a blood clot which has broken off, and an embolus gets stuck in the blood vessel, causing damage. She adds there are other types of emboli, such as a fat embolus, or embolic conditions which can cause a stroke or heart attack.
2:20pm: Mr Johnson asks if air is injected into the system via a syringe, what would happen. Prof Kinsey explains the heart would be pumping, and the air bubbles would be broken into larger and tiny bubbles. The lungs would be able to cope with the smaller air bubbles, but the lungs would struggle with the larger air bubbles. In babies, air bubbles would be going in the arterial circulation - blood returning to the heart passing straight out again without being oxygenated through the lungs. This would lead to the changes in skin colour - a 'fluctuating' colour pattern, and would, the court hears, lead to the types of sin discolourations as described by doctors and nurses so far in the trial.
2:23pm: The court hears, in adults, the air bubbles would go to the lungs, if not blocked. If the bubbles are blocked, it could cause a pulmonary embolism. In babies, there is a section of the heart, called the oval foramen, which would still be open, meaning the air bubbles would go to the arterial circulation. The air bubbles would be absorbed by the haemoglobin, causing skin discolourations which move around the body and a mixture of blue, pink and purple discolouration, Mr Johnson summarises. Professor Kinsey agrees.
2:26pm: Ben Myers KC, for Letby's defence, is now asking Prof Kinsey questions. He says his questions are more concerned on the nature of an air embolus. For the haematology, he asks for Child E, whether it is a general point that such a child would not develop the levels of blood clotting as you would see in a more developed child or adult. Prof Kinsey agrees. Asked about the 'no explanation for spontaneous bleeding', Mr Myers says if that is from a haematological reason. Prof Kinsey agrees. Mr Myers says that does not rule out the possibility Child E had a gastro-intestinal haemorrhage. Prof Kinsey agrees.
2:29pm: Mr Myers asks about the principle of experts giving evidence, and their areas of expertise. He refers to Prof Kinsey's expertise in haematology and certain paediatric specialisms, and her reports. They include focus on cancers and blood disorders.
Mr Myers: "Air embolus does not feature in your expertise, does it?" Prof Kinsey: "No."2:33pm: Mr Myers refers to the diagrams of gas exchange, which are 'standard images' in the way gas exchange works in the body.
Mr Myers: "In no way are they designed to explain an air embolus." Prof Kinsey: "They were produced to explain the gas exchange and circulation."
Mr Myers: "What you are doing in your evidence is to take that understanding of circulation and gas exchange and use it to explain how an air embolus is displayed." Prof Kinsey: "Yes."2:42pm: Mr Myers says Prof Kinsey has, at times, commented on the issue of air embolus in her reports for Childs A, B and E. Prof Kinsey: "Only in the changes to the colour of the skin, very impactful." Mr Myers refers to the summary/opinion for Child A, and whether there was any haematological significance for Child A. He says that is not in dispute. He refers to the conclusion, which he says relies on comment from [medical experts] Dr Dewi Evans and Dr Sandie Bohin, and the description from [Countess of Chester Hospital consultant] Dr Ravi Jayaram of the skin discolouration for Child A. Mr Myers refers to the 1989 medical journal review: "mentioning a particular case - 'blanching and migrating areas of cutaneous pallor were noted in several cases and, in one of our own cases, we noted bright pink vessels against a generally cyanosed...background." Prof Kinsey confirms she is drawing a parallel between the 1989 journal review and what had been observed by doctors and nurses. She tells the court she was "shocked" by Dr Jayaram's description of skin discolouration for Child A, which she said came before she had considered the possibility of air embolus. She said she knew this is what air embolus was like, and knew from her own education, before seeing that description matched what was said in the 1989 medical journal review.
2:45pm: Mr Myers says Dr Jayaram's clinical note - 'legs noted to look very white and pale before cardiac arrest' does not contain the full details from her report. Dr Jayaram did not add anything further to the skin discolouration observation in the report to the coroner, Mr Myers adds.
Mr Myers: "The description you read came from his statement [to police] two and a half years later." Prof Kinsey agrees.2:53pm: Mr Myers refers to the case of Child B, and the summary/opinion Prof Kinsey made in her report. He says, for air embolus, Prof Kinsey again draws parallels between the 1989 medical journal and the skin discoloration observations seen for Child B. The clinical note of 'widespread purple discolouration with white patches' for Child B, made at the time, is shown to the court, along with a subsequent 'improvement in skin perfusion'. A doctor's note on June 10, shown to the court: 'suddenly purple blotching of body all over...upon my arrival purple blotching...[later] purple discolouration almost resolved'. Lucy Letby's note on June 10 is also shown to the court: 'Cyanosed in appearance...colour changed rapidly to purple blotchiness with white patches'.
Mr Myers: "In none of those is there any description of a bright pink or red feature?" Prof Kinsey: "No."2:59pm: Prof Kinsey's report, dated November 1, 2022, is referred to. Mr Myers says Prof Kinsey was asked to give further consideration as to how an air embolism worked. She says she was asked to give further explanation on the features of an air embolism. She said she was not an expert in such mechanisms, but has provided an explanation. Mr Myers says the report notes there is very little medical literature in relation to air emboli.
Mr Myers: "You have used your knowledge of blood and circulation to assist this?" Prof Kinsey: "Yes." Mr Myers says part of the limited medical literature relates to decompression in deep-sea divers, colloquially known as 'the bends', and that in those circumstances, nitrogen bubbles would be in the circulation longer than oxygen bubbles. He asks Prof Kinsey if that is the case. Prof Kinsey: "I don't know the answer to that question."3:04pm: Mr Myers says the research paper in question [for 'the bends'] dealt with four overweight deep-sea diving adults. Prof Kinsey: "Yes, there were many limitations to their findings." Mr Myers said the results were "very specific based to the people [in that study]." Mr Myers asks if the symptoms of decompression sickness would always result in skin discolouration. Prof Kinsey said it would not. Mr Myers asks if that can be applied to babies - if an air embolus could always lead to skin discolouration observations. Prof Kinsey said it would not.
3:07pm: Prof Kinsey says the problem with decompression syndrome, in comparison to air embolus in infants, is the bubbles get larger as the deep-sea diver returns to the surface. Mr Myers says that is another limitation of the available medical literature for air emboli. Prof Kinsey says the reason that study was used in her report was that skin discolouration had been an observation in that study, as it had been in cases of air embolus.
3:08pm: Prof Kinsey says the scale of the air embolus problem would depend on the size of the air bubble and the type of vessel that it is in.
3:10pm: Upon a question from the judge, Prof Kinsey says she has never encountered any discussion about nitrogen bubbles in the system, other than in deep-sea divers. She says the biggest factors for any air embolus would be the size of the air bubble and the vessel that it is in. What was not a factor in her discussions was the quantities that made up the air [ie what amount was nitrogen, what amount was oxygen, carbon dioxide, etc].
3:14pm: The next witness to give evidence is Ian Allen, who worked in the Countess of Chester Hospital's pharmacy department in summer 2015. Simon Driver, prosecuting, asks about the responsibilities Mr Allen had, which involved quality assurance and production of TPN bags for the neonatal unit.
3:16pm: Mr Driver focuses on the TPN bags, and a video which has been produced for the benefit of the court showing how a TPN bag is made. Mr Allen confirms he has seen the video. He describes the types of TPN nutrition bags - one would be used for the baby's first two days of life, and the other would be a maintenance 'stock' bag, supplied to the unit through the department.
3:20pm: Mr Allen says the initial order would be faxed down to the pharmacy from the neonatal unit. It would be handed to a pharmacist, reviewed by them, processed into a worksheet [a set of instructions on how to make the bag and the ingredients needed to make it]. A label would be generated. A member of the pharmacy team would gather the ingredients/quantities required. Every medicine would come with a batch sheet number as part of the 'assembly'. "Every step in the process has a standard operating procedure" Staff would be trained in the process through nationally recognised quality assurance, he tells the court.
3:25pm: The items would be sprayed and wiped to sterilise them, and then made in a controlled environment. Two operators would make the bag, with checks in place confirming the identity and quantity of the ingredients.
3:28pm: A pharmacist would check what has been used, looking at empty vials and ampoules to confirm what has been used. The pharmacist would be ultimately responsible for the product. The unit would be subject to regulatory monitoring to ensure the safety, quality and effectiveness of the products.
3:31pm: The video explaining how a TPN bag is made at the pharmacy department is played to the court for the second time - it was first shown on Monday. The prosecution say they may intervene at various points in the video to ask Mr Allen questions about what is shown to the court.
4:00pm: Mr Allen is now demonstrating how a TPN bag and its connectors work - which does have a connector which can be opened.
4:02pm: The empty TPN bag and its connectors are now being passed around members of the jury and the defence for examination.
4:06pm: Mr Driver is asking Mr Allen about how a quantity of liquid could be added to one of the ports, which is shown to be possible.
4:10pm: The court is shown a nutrition prescription for Child F for August 4. Mr Allen confirms he is familiar with the type of prescription shown, and the worksheet which is also shown to the court. He said this particular TPN would have followed the standard protocols in the pharmacy, and was reflective of the prescription. He said the bag would have been transferred from the pharmacy to the neonatal unit fridge.
4:14pm: A copy of the label for that TPN bag on August 4 would have been made for the pharmacy's records. The label has a use-by date of August 11, to be stored between 2-8 degrees C.
4:18pm: The August 4 TPN bag did not have lipids prescribed on the prescription. Mr Allen said such lipids would have been prescribed separately. Mr Driver asks 'Would there be insulin?' for the TPN bags. Mr Allen: "No, there would never be insulin prescribed in these bags." Mr Driver asks how would that [insulin prescription for a baby] be done? Mr Allen: "...by separate syringes."
4:25pm: Ben Myers KC, for Letby's defence, rises to clarify one matter on the TPN bag, which had an expiration date of seven days. He says normally, TPN bags could last for up to two months, but once the extra items are added to the prescription, the expiration would be reduced. Mr Allen: "That's correct." The court hears the stability of the bag is reduced. Mr Allen explains, upon questions from the judge, there would be nothing added by a pharmacist other than trace vitamins. The TPN bag would contain components such as 10% dextrose. The judge asks about the storage of the TPN bags. Mr Allen says there would be a stock level of TPN bags - they would be 'off-the-shelf' bags and a number would be stored in the pharmacy, and a smaller number would be stored in the unit's refrigeration area.
4:28pm: Members of the jury are reminded by the judge, having heard a lot of expert evidence in the case today, not to conduct any independent research.
Wednesday 30th November 2022
Child F
Yvonne Griffiths - Nurse Kate Bramall - Unnamed nurse - Nurse Cheryl Cuthbertson-Taylor - Nurse Valerie Thomas, Statement of Dr Simon Woods(consultant obstetrician & gynaecologist) - Dr Sandie Bohin - Dr Dewi Evans10:19am: I'm at Manchester Crown Court again today covering the murder trial of nurse Lucy Letby. We're expecting to hear from medical experts this morning in relation to Child F, who the Crown say was poisoned with insulin by Ms Letby in August 2015
10:40am: Yvonne Griffiths, who is a neonatal unit manager at the Countess of Chester, is first in the witness box today. She's giving evidence on Total Parenteral Nutrition (TPN) bags and how they are stored at the hospital
10:44am: The jury are being shown a photo of the treatment room at the Countess of Chester where medicines and kit was stored. Ms Griffiths is explaining that there was one set of keys for a refrigerator that stored controlled drugs
10:47am: She says that there wasn't a system for accessing the fridge, if a nurse needed anything they would just ask for the key
10:52am: Jury is now being shown images of the inside of the fridge, Ms Griffiths says insulin was stored in there
11:12am: A medicines requisition booklet from summer 2015 is now being shown to the court - this was used by nurses to request more stock. We're being shown an entry from June which shows there was a request for a babiven maintenance bag
11:22am: Ms Letby's defence lawyer Ben Myers KC is now questioning the witness. It's clarified that the treatment room wasn't locked and was open to doctors and nurses 24/7
11:51am: Neonatal nurse Kate Bramall has just been in the witness box. She was on shift when a TPN bag was delivered to the unit for Child F. She was asked if she had ever added anything to a bag. 'No, it's not something we do', she said. Asked if she had ever added insulin to a bag, she said :'No never' She explained insulin is administered through a separate syringe
12:03pm: Another nurse, who was also on shift, has just been asked the same questions. She again said she had never added anything to a TPN bag
12:17pm: Another nurse, Cheryl Cuthbertson-Taylor, has just been asked the same questions. Again she told the court she had never added anything to a TPN bag
12:26pm: Another nurse, Valerie Thomas, is in the witness box and is again being asked the same questions. She says she has never administered a TPN bag to a child or added anything to a bag
12:34pm: A statement from Consultant Obstetrician & Gynaecologist Simon Wood is now being read to the court. He helped to carry out the C-Section on the mother of Child E and F. He said the twins were 'born in good condition'
12:46pm: Expert medical witness Dr Dewi Evans returns to the witness box. He was asked to review the case by Cheshire Police and produced a number of reports on the events at the Countess of Chester
1:56pm: Dr Evans said there was 'only one explanation' for the 'astonishing' levels of insulin found in Child F's blood. 'These were very, very striking results. There's only one explanation for this, (Child F) had received insulin from some outside source', he said.
1:57pm: Dr Evans said he had concluded the drug had most likely been added to the baby's Total Parenteral Nutrition (TPN) bag, which is used to intravenously provide feeds to infants.
2:05pm: Ben Myers KC, defending, has no questions for Dr Evans on his evidence
2:09pm: Medical expert Dr Sandie Bohin, who reviewed Dr Evans' findings, is now in the witness box. She's asked if she agrees with Dr Evans that this was a case of insulin poisoning via TPN bag. 'Yes', she says
2:13pm: Again, Mr Myers has no questions for the witness. That concludes her evidence. Police intelligence analyst Claire Hocknell is now in the witness box, she is taking the jury through sequencing evidence
2:24pm: A summary of Ms Letby's police interview, carried out in 2019, in relation to Child F is read to the court. In that interview Ms Letby denied adding insulin to a TPN bag
2:32pm: That's it for today and that concludes evidence related to Child F. Tomorrow the court will move on to Child G.
Chester Standard article 30-11-2022
A BABY boy allegedly poisoned by Lucy Letby received two bags of intravenous feed contaminated with insulin, a court heard.
The 32-year-old nurse is accused of attempting to murder the infant by injecting synthetic insulin into his nutrition during a night shift at the Countess of Chester Hospital's neo-natal unit.
The heart rate of the youngster – referred to as Child F – soared and his blood sugar dropped to a dangerously low level after the prescribed bag containing nutrients was connected to an intravenous line after midnight on August 5, 2015.
His blood sugar levels remained low throughout the following day shift even after the intravenous long line, and the connected bag, had to be replaced after swelling to the infant's leg.
Child F eventually made a full recovery after a decision to stop giving the nutrients from the second stock bag in the early evening, Manchester Crown Court has heard.
On Wednesday, November 30, prosecutor Nick Johnson KC asked expert witness Dr Sandie Bohin: "Did you conduct a careful review of the medical notes and identified the fact that there was material… to suggest that the TPN ( Total Parenteral Nutrition) bag had been changed?"
"Yes," replied the consultant neonatologist.
Mr Johnson said: "And secondly, it followed, given the blood sugar readings, that two bags must have been contaminated with insulin?"
Dr Bohin said: "Yes, if a new long line is inserted it would be usual practice to throw away the old bag of TPN, change the long line and put up a new bag which would mean insulin would need to have been in two bags."
Jurors have heard the TPN bags – both prescribed and stock – were kept in a locked fridge in a store room at the unit, along with insulin.
The nursing shift leader would hold a set of keys to the fridge but they would be passed around colleagues as and when they needed access with no log taken.
Dr Bohin told the court that neonatal hypoglycaemia – persistent low blood sugar levels – could be "absolutely devastating".
She said: "'Initially babies may become a little unwell, but if left untreated they could go on to have seizures, fall into a coma and subsequently die.
"Neo-natal fits as a result of very low blood sugar are associated with significant brain damage, those children are not normal and go on to have long-term neuro-developmental problems."
Mr Johnson asked another expert witness, consultant paediatrician Dr Dewi Evans: "Have you ever heard of the legitimate administration of insulin by somebody putting it into a bag of feed?"
Dr Evans replied: "No. never happens. Insulin is always given in a 50ml syringe driver."
Jurors were told that Child F was the only baby who was receiving TPN on the night shift on which he was allegedly poisoned.
Letby is said to have tried to kill Child F less than 24 hours after she allegedly murdered his twin brother, Child E, by injecting air into his bloodstream.
The defendant, originally from Hereford, denies murdering seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Thursday 1st December 2022
Child G
Police analyst: Recorded events & messages - Parents' statements - Dr Alison Ventress.Chester Standard Live Reporting
10:18am: The trial is expected to resume at 10.30am.
10:33am: The trial has now resumed, and the jury will be hearing the case of Child G, a baby girl. Nicholas Johnson KC, for the prosecution, says intelligence analyst Kate Tyndall will first talk through the sequence of events, before a statement from the parents of Child G will be read out to the court.
10:38am: The court is first shown Lucy Letby's shift patterns for June 2015. Mr Johnson says, for the indictment, the charges of murder and attempted murder for Childs A-F, Letby was on night shifts. Letby was also on a night shift for September 6-7, the night Child G suffered a collapse. The prosecution say this was one of three murder attempts by Letby on Child G; the defence deny this.
10:41am: Child G was born on May 31, 2015, at Liverpool's Arrowe Park Hospital, at a gestational age of 23 weeks and six days. She weighed 535g - 1lb 2oz. Previously, the court heard this baby was the most premature birth of all the babies in the trial. She was in a poor condition at birth, requiring ventilation.
10:45am: She was cared for at Arrowe Park, a tertiary centre, until being transferred to the Countess of Chester Hospital on the night of August 13. At this stage she would have been a gestational age of 34 weeks plus 3 days. Nursing notes for Child G on Friday, August 14, recorded by Caroline Bennion, note: 'Currently [Child G] is on CPAP Peep of 4 in 29-40% of oxygen...has been since 17/7/15 and has occasional desaturations. [Child G] is trialling off CPAP in ambient oxygen and manages 1 hour in 2 episodes daily. May be eligible to trial Optiflo. Fluids are all enteral feed.' A further note: 'Mum intends to breast feed and is expressing well...first immunisations have been given on August 1. [Child G] has had metabolic bone disease but is not currently treated. Mum and dad have been shown around the unit and have been given contact numbers'.
10:48am: The court hears, from August 14 to September 6, Child G was treated at the Countess of Chester Hospital neonatal unit. The next evidence presented to the jury will be from September 6 onwards. At 2am on that day - when Child G was 99 days old - a feeding chart shows she was being fed with expressed breast milk, Gaviscon and a fortifier.
10:53am: The court is also shown a range of medications which were administered by Lucy Letby and another nurse, during that night, to Child G, before the handover at 7.30am. For the day shift, the designated nurse for Child G was Vicky Blamire, who recorded hourly observations and was a co-signer for some of Child G's medication. Consultant Dr Stephen Brearey records observations in an 11am clinical note. It was noted that Child G's weight had increased, by this point, to 1.985kg (4lb 6oz).
10:56am: Vicky Blamire's note at 3.37pm records 'all safety equipment present and correct', and Child G continued to receive regular feeds. Further prescribed medication is administered to Child G throughout the day. Her note at 6.44pm records, for Child G, 'Another bottle completed this evening. Bowels now open'.
11:00am: The handover takes place for the night shift team at 7.30pm. A different nurse to Lucy Letby - who cannot be named due to reporting restrictions - was the designated nurse for Child G this night. Letby was the designated nurse for one baby in room 1. The other nurse was the designated nurse for Child G in room 2, and another baby in a room whose location is unconfirmed on the chart. There were a total of seven babies in the neonatal unit that night, being looked after by a total of five nurses.
11:03am: Lucy Letby was the co-signer for medication administrations for Child G, along with the designated nurse. An observation chart for August 6 shows Child G's observations are made every three hours, with a heart rate in the 'normal' range at that stage.
11:07am: Letby had messaged colleague Kate Bissell at about 8.30pm enquiring about expressed breast milk for the baby she was the designated nurse for that night. The matter is clarified in the text conversation.
11:10am: Further medication is administered to Child G at 1.46am, signed by the designated nurse and Alisa Simpson. At 2am, the designated nurse records observations for Child G and a neonatal feeding chart records this is Child G's 100th day since birth. She received 45mls of milk via the nasogastric tube, with 'ph4' aspirates recorded. Child G was noted to be 'asleep' at this stage. The milk was expressed breast milk, plus fortifier and Gaviscon.
11:13am: Lucy Letby writes a note, written in retrospect at 8.57am, where care of Child G was transferred to her following an 'event'. The note says "written in retrospect for care given from 2am to present. [Child G] had large projectile milky vomit at 2.15am. Continued to vomit++. 45mls of milk obtained from NG tube with air++. Abdomen noted to be distended and discoloured. Colour improved few minutes after aspirating tube, remained distended but soft. Reg[istrar] Ventress asked to review. To go nil by mouth with IV fluids. Dr called to theatre."
11:15am: The designated nurse from the start of the shift records a note: 'nurse L Letby taken over care [of Child G] following vomit/apnoeic episode after 2am feed'.
11:16am: Dr Alison Ventress writes clinical notes, timed at 2.35am and written retrospectively at 4.40am. They record: 'Called to r/v [Child G] urgently at 2.35am. Had very large projectile vomit (reaching chair next to cot + canopy). Abdo appeared discoloured purple and distended. [Child G] distressed and uncomfortable. Red in face and purple all over. [Oxygen] to 1L via nasal cannula...'
11:17am: Letby's note at 3am for Child G - 'bowels opened large green watery stool at 0300'.
11:19am: At 3.15am, Letby's note adds: 'Approx 0315 [Child G] had profound desaturation to 20%, marked colour loss with apnoea. Brady to 50s. Neopuffed in 100% oxygen, observations improved but [Child G] remained apnoeic. Drs arrived. Intermittently breathing/apnoea. Decision made to intubate. Moved to nursery 1...'
11:25am: Dr Ventress also noted Child G was planned to cannulate, with plan to administer fluids, but this was delayed due to the need to deliver another baby in the delivery room. Later, she noted: 'called out of theatre to say [Child G] had gone apnoeic and dusky. Dr called in... On arrival sats 50% in oxygen. Receiving IPPV from nurse. Heart rate ok. Pink and well perfused with mask CPAP....[Child G] then had another profound apnoea and heart rate down to 70, sats 40%.' The doctor adds Child G was then intubated, and 'IV vitamin K given due to blood from trachea'. Mr Johnson says this is another case where a baby is cleeding at the mouth. Dr Stephen Brearey noted: 'Called in at 0330...large vomit and loose watery stool earlier followed by desat and brady. Intubated by Dr Ventress on my arrival. A small amount of blood visible on intubation. Blood samples taken and sent...'good gas post intubation'. At 3.45am, Child G's parents were notified by the former designated nurse.
11:27am: The blood sample for Child G is taken at 3.59am. Lucy Letby records observations, a fluid balance and an intensive care chart for Child G at 4am. The observations have gone, the the court hears, from every three hours, to every one hour.
11:30am: A blood gas record is shown for Child G, from August 14 to September 7. Lucy Letby has signed for the last of those records. An x-ray of Child G is taken at 4.49am. Consultant radiologist Dr Amer Rehman records, for the abdomen, 'generally slightly distended bowel loops, but gas noted in rectum, no transition point, mural or free gas detected on balance'.
11:34am: Lucy Letby and Alisa Simpson are co-signers for medications for Child G at 5.15am, and for a neonatal infusion prescription at 5.30am. Dr Alison Ventress notes, for 5.30am, 'approx 0530 had another profound desat, hr down ton 60 and sats to 40%. Taken off vent and IPPV Neopuff via ETT. Recovered slowly but desat when back on vent ? ventilator problem so flow sensor changed + then whole ventilator changed'. Dr Brearey also records Dr Ventress changed the ETT with 'less leak'. Child G had 'one further brady and poor perfusion.' Child G was sedated and 'will need discussion with Arrowe Park Hospital/Liverpool Women's Hospital'. The parents were kept informed, the note adds.
11:37am: Dr Ventress notes, from 6.05am - 'profound desat to 40% + HR down to 80. Decision to reintubate. IPPV given via ETT initially. Heart rate 120 but sats remained 50% [despite increase in oxygen] ETT removed at 6.10am. Thick secretions ++ in mouth. Blood clot at end of ETT. IPPV via facemask given NG aspirated as abdo appeared v large ~100mls aspirated. Reintubated 0615 ETT with intubation drugs. Blood-stained fluid in oropharynx. Capnograph positive.' The plan was to continue a series of medication, plus morphine, and keep parents updated.
11:39am: Lucy Letby noted: 'Reintubated at 0615 with intubation drugs...clear air entry and bilateral chest movement. Blood gases as charted...10% glucose commenced. Morphine running...[Child G] agitated and fighting ventilator. [Medication given]. Now synchronising well.'
11:40am: Medication is administered, with Lucy Letby being a co-signer along with Alisa Simpson. Dr Rehman has a further x-ray report at 6.36am, comparing observations with the previous x-ray. Among his observations, he notes: 'Lungs with slightly improved appearances, probably reflecting improved inspiration.'
11:46am: The former designated nurse are written retrospectively at 7.49am. For the night '[Child G] was being nursed in a Kanbed with monitoring... Feeds 180ml/kg 3x8 ebm with fortifier and Gaviscon via alternate bottle/NGT. Abdomen full but soft with no discolouration. Aspirates minimal, partial digested milk. Passed urine and bowels open++. Short period of straining/uncomfortable at start of night when having cuddles with dad. Dr Ventress aware.' The note adds care was transferred to Lucy Letby following Child G's large milky vomit just after 2am. The nurse adds, for family communication 'dad present for early part of night shift, had cuddles with [Child G]. Parents called by me approx 3.45am...arrived shortly after'.
11:57am: The trial is now resuming after a short break.
12:01pm: The care of Child G was then handed over to another designated nurse for the day shift on September 7. Letby had written a note, retrospectively at 8.57am, recording what happened during the night shift: 'Abdomen appears less distended and soft. Bowels opened large green watery stool at 0300. Urine output...NG tube on free drainage... Blood noted beyond vocal cords during intubation. [Child G] having frequent profound desaturations on ventilator, requiring Neopuff with high pressures and 100% oxygen, takes several minutes to recover.'
12:04pm: Dr David Harkness, in a clinical note at 9am, records Child G was 'paralysed and sedated, well perfused. [Abdomen] soft... Plan...discuss with tertiary centre [ie Arrowe Park/Liverpool Women's]' Letby, at 9.15am: 'Parents attended the unit and have been fully updated...by myself, Reg Ventress and consultant Brearey. Anxious but understand need for ventilation.' At 10am, Dr Harkness noted Child G's colour had 'improved'.
12:07pm: Lucy Letby sends a text message to a colleague in relation to the care of a different child on the neonatal unit from the previous night at 10.46am.
12:17pm: A longline is inserted into Child G at 3pm.
12:24pm: Dr Ravi Jayaram's clinical note at 3.30pm - 'spoke with consultant neonatologist at Arrowe. Agrees current management plan.' Child G's observations are noted, with 'cool hands and feet', 'abdomen - distended but soft'. The blood gases had raised metabolic acidosis.
12:36pm: A doctor's note at 4.30pm says Child G required a 2nd longline, and Child G 'remained unwell'.
12:46pm: The day-shift designated nurse's notes, at 8.13pm, include 'during [morning] handover required x2 episodes of Neopuff. Ventilation increased... BP deteriorated and cannula site became white. Moved to another cannula. BP again improved. Drs trying to obtain longline for better access... Chest clear and [blood gases] continue to be metabolic acidosis... Minimal urine output all day.' The family communication says, for 8.51pm: 'Parents on unit throughout day and updated. Aware that BP is too low and IV access difficult. Understandable very upset and struggling to see her this poorly again. Have looked at 100-day cake, are trying to remain positive at this time...'
12:49pm: Medication for Child G continues into the night of September 7. A consultant paediatrician said at 9.45pm, '[Arrowe Park Hospital consultant says] they are happy to accept [Child G there] - he will discuss with transport team.' The call to the Arrowe Park transport team is made at 10.08pm.
12:56pm: The ambulance is booked at 10.43pm. At 11pm, further observations are made for Child G. Nurse Belinda Simcock records, at 11.35pm, a series of observations for child G, which include longlines, morphine administered and antibiotics. The note adds 'infant to be transferred to Arrowe awaiting transport team'.
1:00pm: The transfer team arrived at the Countess of Chester Hospital at midnight. A consultant paediatrician's clinical notes record Child G was still 'very sick', the court hears, despite the series of medications throughout the day. More observations are made for Child G at 1am. At 1.05am on September 8, the transfer team noted Child G's abdomen was 'full and veiny'.
1:42pm: During the course of September 7, a number of text messages were exchanged between Lucy Letby and her colleagues. One conversation began at 1.33pm from Jennifer Jones-Key, who messaged Letby: "How you doing x"
Letby replied: "Had rubbish nights. x"
Jones-Key: "Yeah gathered. x"
Letby: "Thought someone would have told you x "Nothing else to say really, just hope they are both ok"
Jones-Key: "Don't know ins and outs as tried to avoid it, needed a break. Found Thursday horrendous, not really slept since then. Hope you're ok"
Letby: "That is understandable, won't tell you anything." The conversation then turned to Letby asking which of the team had informed Jennifer Jones-Key about the events of the night-shift for September 6-7. After a few guesses, the name 'Ali', in the messages, is said to be correct.
Jones-Key: "Ali. She not having a good time x"
Letby: "No, I know. It's been awful for her but she's coped with it brilliantly and got back-up when needed etc x"
Jones-Key: "Yeah I don't know how she's done it. She was fab on Thursday..."1:48pm: The daytime designated nurse for Child G is in a text conversation with Lucy Letby for much of the afternoon on September 7, the court is told. Much of the conversation relates to the condition of Child G, although messages are also exchanged in which the designated nurse is 'venting' about a number of colleagues, adding she was going to buy some sweets and eat them all to herself. Letby responded: "Absolutely, don't share", followed by an emoji of a face with its tongue sticking out. The nurse added Child G's parents were "devastated but determined...thought that if she got to 100 [days] they could feel confident she would be fine."
1:50pm: Letby responded that, at the start of that night shift, the team had been sat at a desk "preparing a banner [for Child G's 100-day milestone]." The nurse responded: "Yep. [Colleague] brought her cake in."
1:55pm: Later in the afternoon, the nurse messaged Letby that Child G's condition was still very poor. Letby responds: "any idea what's caused in [sic]?" The nurse responds, at 6.06pm, "Nope. Just seems to be a circulation collapse. Chest sounds clear."
Letby: "Hmm, what can cause that. "Is it that she is an extreme premature who had long-term inotrope and vent dependency and now she is older and doing more for herself...it just takes a little...something to tip her over." The nurse responds: "We are going with sepsis..." Child G was noted to be looking "grim".2:00pm: Letby had seen Child G that night on September 7, messaging the nurse at 10.56pm to say the baby girl "looks awful, doesn't she". The nurse responds: "Yeah, going to APH [Arrowe Park Hospital]. On triple antibiotics." Letby relays a blood gas reading for Child G to the nurse. The nurse responds: "So no better. Damn" adding: "I have a bad feeling." Letby messaged: "But at least going to where she is known."
"Just hope they get her there." The nurse replies: "Hmmmmm not sure they will."
Letby: "On today of all days." Letby added Child G was "declining bit by bit".2:06pm: The trial is now resuming following the lunch break.
2:17pm: The sequence of events continues to be talked through. Belinda Simcock records nursing notes for 1.30am and 1.40am on September 8, written in retrospect at 5.19am. The 1.40am note reads - 'Suctioned-nil from ETT, moderate amount thick white secretions obtained orally.' An increase in the dose of adrenaline is made for Child G. The transport team handover is formally made at 2.35am. Child G leaves the Countess of Chester Hospital in an ambulance at 3am, to be transferred to Arrowe Park Hospital. Belinda Simcock's note records that the parents were kept informed of the developments. Alisa Simpson later messages Lucy Letby to say: "Hi Lucy. Just to let you know that [Child G] has successfully been transferred out at 3am this morning to APH. She is stable and latest CBG [capillary blood gas] has improved! Fingers crossed for her!" Letby responds: "That is good news. Thanks for letting me know" Child G was then treated at Arrowe Park Hospital between September 8 and September 16, 2015, before returning to the Countess of Chester Hospital.
2:22pm: The court is now shown a chart illustrating the neonatal unit's staff duties and who recorded/administrated what for September 6-7, 2015. At a point between 2am and 3.30am, a different nurse takes over the care for what had been Lucy Letby's designated baby for that night shift.
2:27pm: The final chart shows Child G was moved from nursery room 2 to room 1 at 3.15am. One other baby was moved from room 1 to room 2 at 3.30am.
2:31pm: Philip Astbury is now reading the relevant parts of Child G's parents. The court hears this agreed evidence, and is not contested. The first statement is Child G's mother. "Things went ok" with the pregnancy until week 22, when she started bleeding. She was taken to hospital for checks. At week 23, she was taken to Arrowe Park, as her waters had broken and she was having stomach aches. She said she was struggling to sleep and went to the bathroom - she then gave birth to Child G. She said she rang for the emergency, but it wasn't working. Someone in the next door heard, and went for help. She said to medical staff: "Save [Child G]."
"She was only 1lb 2oz, a tiny little fighter. "During our time at Arrowe Park, she showed doctors she was a fighter. She made good progress." After a change of several cots, and at seven weeks, Child G was moved to the high-dependency unit and available for skin-to-skin contact. By 12 weeks old - she was 'so well' she could go to Chester.2:53pm: Child G turned 100 days old and Lucy Letby was looking after her that day. "When we got to the hospital, she was in intensive care...it was such a shock and it looked like she was going to die." Child G was taken back to Arrowe Park for nine days, before returning to Chester in the HDU. Child G got sick again, and had to return to the intensive care unit. She "looked different" - and after brain scans, it was said she would just be 'a little clumsy'.
3:00pm: The mum adds she had gone to get a coffee and when she went back to the high-dependency unit, Child G was "freaking out". Lucy Letby was there with another nurse. She said she told them she wanted to hold Child G as that would calm her down, and did so. Child G went to the intensive treatment unit that day. There were three times, she said, Child G was transferred to the ITU. She said she would always ring the hospital twice a day - once at 6am and one at 7-8pm; the latter to find out who would be looking after the baby girl that night. During the day, she would stay with Child G at the hospital. When Child G came home in November 2015, at 156 days old, she had been left with quadriplegic cerebral palsy and was visually impaired, and was being fed by stomach, and nil by mouth.
3:04pm: In a second statement, she said she was asked about the feeding of Child G, and how she had been taught to feed her baby daughter via a syringe, in a way she did not receive too much milk too quickly. She said sometimes she would be allowed to feed via the syringe, but Lucy Letby "always held the syringe" during feeding time.
3:08pm: A statement from Child G's father is read out to the court. He said there had been concerns at week 9 of the pregnancy when the mother began bleeding, and they feared there might be a miscarriage. The mother was taken to the Countess of Chester Hospital where the baby was seen to be doing fine in a scan, and the mother stayed there until the bleeding stopped. The mother began bleeding again later in the pregnancy and was transferred to Arrowe Park Hospital by ambulance. The father drove himself to the hospital. He left the mother at the hospital at 8-9pm, and later received a phone call to say the mother had gone into labour and given birth. He said he jumped into the car and drove to the hospital. Child G was 'stable' and the parents went to see her in the ITU. The mother had to be wheeled in. The father says Child G was not due to give birth until September 21 and had "only a 5% chance of survival".
3:10pm: The father said Child G was "no bigger than your hand..[she] looked like a tiny person." Child G was kept in for 11 weeks at Arrowe Park and although "they thought she was going to die", with her having "ups and downs" and underdeveloped lungs, she was "much more stable after a couple of weeks". He said he only picked her up for the first time when she weighed 2lb, "as she was so small".
3:18pm: Child G had 'regular ultrasounds' to check for brain development, which showed no brain bleeds, and all scans showed "she was normal". She was "stable enough" to be transferred to the Countess of Chester Hospital, in the HDU. When there, the mother would ring twice a day, and stay at the neonatal unit during the day. The father said he would collect the mother at 5.30pm, they would go home for tea, then he would go back to the hospital until about 10-11pm. He says he never saw anything in that time where a doctor or nurse was acting unprofessionally, nor did he have any concerns. There were "no problems" until Child G was 100 days old.
3:25pm: The father said on day 99, Child G required a low amount of oxygen for breathing assistance, had been fed and was "settled; she was fine when I left". The parents got a phone call in the early hours of September 7 from a nurse to say Child G had vomited and aspirated. The nurse said there was "no need to rush", but the parents went to hospital "immediately".
3:29pm: When the parents arrived, they found a banner to celebrate Child G's 100 days had been made, and Child G was onto a ventilator in the ITU. Child G was "just about stable", and they were told she had "projectile vomited". This, the father said, Child G had "never done before", although she has done since, "several times". Child G was transferred to Arrowe Park Hospital in the early hours of September 8, and due to the time of admission, the parents stayed in the parents room.
3:32pm: After a couple of days at Arrowe Park Hospital, Child G was weaned off oxygen completely, which exceeded the expectations of the parents. However, the father said, he "noticed something had changed about [Child G]."
3:45pm: He said while, prior to Child G's projectile vomiting incident, he would speak to her and she would smile in response. After the incident, he would speak to her, but she would not smile in response. Child G was transferred back to the Countess of Chester Hospital and the father asked if there was a virus at the hospital, as another baby in the unit [Child I] was also poorly. He said a consultant assured him "there was no virus" and "nothing wrong with the ward".
3:47pm: On a few occasions, Child G had to go back to the HDU, having appeared as if she was almost ready to leave when placed in nursery room 4. On one occasion, he recalled the nursing staff were trying to recannulate Child G to give antibiotics, and the mum said to them "Let me hold her", and after she did, Child g calmed down. "It seemed that every time she moved [to nursery room 4], something happened and she would be moved back to the HDU."
3:56pm: When Child G came home in November 2015, she weighed 5lb. She remained stable at 18 months and 24 months, but "missed milestones". At the age of two-and-a-half, she had an MRI, and it was only then that the parents "realised the true extent of her brain damage". Child G required treatment at Alder hey Hospital and required numerous ventilations throughout 2018. She was, at the time of the father's statement to police, 'nil by mouth', but was less prone to chest infections. The Countess of Chester Hospital continued to treat Child G, who had quadriplegic cerebral palsy, Level 5 cerebral palsy which meant she would go "really stiff" and stop breathing. The first time it happened, the parents believed she was having a tantrum, until they realised the lack of breathing was involuntary. Child G was visually impaired and also being treated for microcephaly, where the head is smaller than it should usually be. "We don't know what her life expectancy is," the father added.
3:59pm: Dr Alison Ventress is now recalled to give evidence. She said she recalls "very little" from the night shift at September 6-7. She says she did not see Child G vomiting that night. She tells the court Child G 'looked better' and appeared more stable, so did not refer the matter to consultants, and was called away for the delivery of another pre-term baby. She says she did not believe she would have been away from the neonatal unit for too long. If she believed so, she would have notified a consultant. The court believes she was away from the room for about half an hour.
Dr Ventress was then called back to the neonatal unit, and observed the saturation levels were 50%, which were 'low - they should be above 90%'. Child G was 'pink and well perfused' following efforts to assist her breathing, and moving her to room 1. Her saturation levels took 5 minutes to move up, but this was not seen as unusual. Child G then had 'another profound apnoea', which Dr Ventress said would '99% sure' have happened in her presence. The heart rate had dropped to 70, saturation levels to 40%, perfusion had dropped. Breathing assistance was administered and there was a 'gradual improvement'. Saturations increased and perfusion improved, according to Dr Ventress's notes.
She tells the court "We can't carry on in this situation" as Child G had suffered two profound desaturations in a short period of time, so it was necessary to intervene via intubation. Dr Ventress noted 'blood-stained fluid noted coming up from trachea/between cords' during intubation. Child G had 'good air entry'. There was a 'large leak' on the tube, but this was "not a concern" at this stage as there was good air entry. Vitamin K was administered to help with blood clotting, as blood had been seen. Dr Ventress tells the court: "She responded well to the treatment we had given her" at that stage.
At 5.30am Child G had another profound desaturation, with heart rate down to 60bpm and saturation levels down to 40%. Child G would "recover slowly" each time from the desaturations. After being put on the ventilator, Child G desaturated once more, so Dr Ventress said she was wondering if the problem was with the ventilation equipment. The equipment is changed, but Child G has another desaturation event at 6.05am, with the heart rate falling to 80bpm and saturations to 40%. Dr Ventress said, following reintubation, the heart rate went up to 120 but the saturation levels remained at 50% despite increased oxygen support. The doctor said she would "probably" have been cotside for most of this time.
The ETT is removed at 6.10am, with "thick secretions++ in mouth" and a blood clot at the end of the tube. Dr Ventress says breathing support is given via the mask and jaw support, but the saturations fell to 17%. Dr Brearey was called in "urgently". The nasogastric tube was aspirated as the abdomen "appeared very large", with about 100mls aspirated. The saturations gradually improved after this. Dr Ventress says it is "quite common" for the tummy to get bigger with breathing support administered, and it was likely it was air was removed. Child G was reintubated with a mild anaesthetic at 6.15am, with 'blood-stained fluid in oropharynx' noted. Dr Ventress says the first observation of blood was in the windpipe, whereas this was more in the throat. Child G "responded well" to being intubated. X-rays at 4.48am and 6.36am had the comment for abdomen: 'generalised gaseous distention'.
4:03pm: Ben Myers KC, for Letby's defence, is now asking Dr Ventress questions. Dr Ventress confirms she met Child G's parents when she was first admitted to the Countess of Chester Hospital. Mr Myers presents a 'neonatal discharge summary' for when Child G was discharged from Arrowe Park, with a summary of Child G's condition and problems. The main problems, Mr Myers, include 'chronic lung disease', 'extreme prematurity', 'sepsis suspected', and active problems include 'chronic lung disease - on CPAP' and 'establishing feeds'. He said chronic lung disease would be a 'persistent issue' for Child G. Dr Ventress said it would require breathing support such as CPAP.
4:07pm: Mr Myers says a baby like Child G requires constant medical care and was at risk of infection. Dr Ventress agrees. He says that by the time Child G went back to Arrowe Park on September 8, it was believed it was "linked to infection". Dr Ventress agrees. Mr Myers asks if this was something which did not appear out of the ordinary. Dr Ventress agrees.
4:10pm: Mr Myers shows blood gas readings for Child G for September 4-5, with pH readings that are 'normal', but the carbon dioxide and bicarbonate readings are 'elevated'. Dr Ventress says that is common in premature babies with chronic lung disease.
4:14pm: Dr Ventress confirms she would have been, for the night shift of September 6-7, her duties would involve patients at the children's ward and neonatal unit. She says it would be "rare" if she would have to cover A&E as well. She would also be tasked with the post-natal unit as well. At the time of the 'urgent review' at 2.35am on September 7, she said she would have been at the children's ward. She said, from her statement to police, she would have gone "straight away" to review Child G.
4:17pm: Mr Myers asks that upon attending the unit, and informing the plan of action for Child G, was Dr Ventress then called away before she could carry out anything herself? Dr Ventress agrees. Mr Myers says it was for delivery of another pre-term baby.
4:20pm: Dr Ventress's clinical note says Dr Ventress was called out of theatre to say [Child G] had gone apnoeic and dusky. Mr Myers refers to the note about 'blood-stained fluid noted coming up from trachea/between cords'. He asks if that was noted after intubation. Dr Ventress said it was during intubation. Mr Myers asks if it would be unusual to see that.
Dr Ventress: "It's not uncommon for the baby to [have bleeding during intubation] - it is unusual to have blood coming up from beneath the vocal cords."4:22pm: Mr Myers says would the blood-stained fluid be blood mixed with some secretion? Dr Ventress says she cannot quantify what the fluid was, but it was "not pure blood". Mr Myers says if there was any issue with blood intervening with the procedure. Dr Ventress says there was not.
Friday 2nd December 2022
Child G
Unnamed nurse - Nurse Ailsa Simpson (shift leader)Chester Standard article 2-12-2022
A NURSE was surprised to return from her break to find a baby in her care was unwell, the Lucy Letby murder trial has been told.
Letby, 32, allegedly tried to murder the youngster hours after she helped put up a party banner at the Countess of Chester Hospital's neonatal unit to celebrate the girl turning 100 days old.
The defendant is accused of overfeeding the baby with milk through a nasogastric tube (NGT) and/or injecting air into the tube.
Prosecutors say she struck after 2am on September 7 2015 while a colleague designated to look after the infant, referred to as Child G, was on an hour-long break.
The colleague, who cannot be named for legal reasons, said the baby's observations were stable when she left the high dependency unit after feeding her 45ml breast milk via the NGT.
On her return, the youngster was not in the room and had been moved to the intensive care unit as fellow staff gathered around her cot, she said.
She told Manchester Crown Court: "If I was concerned, I wouldn't have gone on my break. For example, if she looked unwell, or her monitor was alarming, or if she hadn't tolerated her feed, or woke up upset.
"I was told she had been unwell while I had gone on my break."
Simon Driver, prosecuting, asked: "Was that development expected or unexpected?"
She replied: "It was unexpected."
Mr Driver asked: "Why?"
The witness said: "Because she was fed and settled when I left her and there had not been any observations on her chart which caused me any concern."
Jurors have been told Letby went on to take over the care of Child G, who deteriorated later in the shift as her oxygen levels dipped and her breathing stopped periodically.
The witness told Ben Myers KC, defending, she was not trained in intensive care so her duties on the night would have been appropriately passed to Letby.
Shift leader Ailsa Simpson said she was with Letby at the nursing station - directly opposite the high dependency unit - when she heard a projectile vomit at 2.15am.
Both rushed into the room where Miss Simpson said she was greeted by alarms sounding from the monitor connected to Child G's cot.
She said she "sat up" the youngster and that either she or Letby then used a facemask to assist with Child G's breathing.
She said: "It was a large, milky digested vomit. It had gone from over the cot and on to a chair next to her."
Prosecutors say the defendant made two more attempts to murder Child G on September 21.
Letby, originally from Hereford, denies murdering seven babies and trying to murder 10 others between June 2015 and June 2016.
Monday 5th December 2022 - no court (juror ill)
Tuesday 6th December 2022
Child G
Statement of Unnamed nurse, Instructional videos on ventilators, suction tubes & heart rate monitors10:25am: Back at Manchester Crown Court for the murder trial of nurse Lucy Letby today. We're expecting to hear more evidence in relation to the collapse of Child G. Ms Letby is accused of attempting to murder the girl three times at the Countess of Chester Hospital in 2015
10:38am: Defence counsel Ben Myers KC cannot make today's sitting, therefore the court is hearing statements of agreed evidence from various former colleagues of Ms Letby being read by the prosecution
10:50am: A former colleague of Ms Letby, who cannot be named for legal reasons, said in her statement that she and staff on the neonatal unit had been 'surprised' by how 'very poorly' Child G became in early September as she had previously been 'stable'
11:14am: Jury are now being shown an instructional video of how a ventilator works
12:01pm: Further instructional videos showing how suction tubes/heart rate monitors work are being shown to the court
2:10pm: Court adjourned till tomorrow. Not many updates today as Ms Letby’s leading defence counsel could not be present. Back tomorrow
Chester Standard article 6-12-2022
A BABY girl allegedly attacked by nurse Lucy Letby as she turned 100 days old was "very poorly" after her sudden deterioration, a court has heard.
Day shift staff on the Countess of Chester Hospital's neo-natal unit were said to be "surprised" the infant had to be moved to intensive care overnight.
The Crown says Letby, 32, attempted to murder the youngster from 2am on September 7, 2015 while a colleague looking after the child was on a hour-long break.
Hours earlier, the defendant had helped make a party banner for the premature-born baby, known as Child G.
On Tuesday, jurors at Manchester Crown Court were read a statement from a nurse who took over Child G's care at the end of Letby's night shift.
The nurse, who cannot be identified for legal reasons, stated: "I remember (Child G) being very poorly that day which surprised me and the staff because prior to September 7 (Child G) was very stable."
She said Child G had been "feeding and growing" in the outside nursery rooms of the unit following her transfer from Wirral's Arrowe Park Hospital.
The nurse said she remembered September 7 because Child G was 100 days old and that was a regular milestone marked in which a staff member would bake a cake for a child, with balloons placed around the bedside.
She went on: "Lucy told me (Child G) had vomited while under the care of (another nurse) and then became unwell.
"She told me she had taken over as designated nurse because (the other nurse) did not have her intensive care course qualification."
Referring to her medical notes, she said Child G had "blood pressure issues" throughout the day and required several infusions plus more antibiotics.
Her observations showed a raised heart rate, the court heard, and the nurse also noted Child G was pale and cold.
The nurse described Child G's parents as a "loving, caring couple" who were "committed" to the wellbeing of their daughter.
Noting both had been on the unit all day, she wrote: "Understandable very upset and struggling to see her this poorly again. Have looked at 100 day cake and trying to remain positive at this stage."
In the early hours of September 8, Child G was moved to Arrowe Park, where she had been born weighing 1lb 2oz.
Medics suspected sepsis as Child G required ventilation support with 100% oxygen but gradually she improved and was breathing for herself a week later.
Her markers for infection also fell as doctors ruled she was clinically stable and no longer needed specialist care as she was returned to the Countess of Chester on September 16.
Letby is accused of overfeeding Child G with milk through a nasogastric tube (NGT) and/or injecting air into the tube.
The prosecution says she made two more attempts to murder Child G on September 21.
In his opening statement to the jury, Ben Myers KC, defending, said Letby did not do anything to contribute to the health problems of Child G, who he said was "extremely premature" and "high risk".
Letby, originally from Hereford, denies murdering seven babies and trying to murder 10 others between June 2015 and June 2016.
Wednesday 7th December to Friday 9th December 2022 - no court (juror ill)
Monday 12th December 2022
Child G
Dr Stephen Brearey - Dr David Harkness - Nurse Christopher Booth - Dr Dewi Evans - Dr Sandie BohinChester Standard Live Reporting
10:29am: The judge, Mr Justice James Goss, has entered the courtroom. The trial will resume shortly.
10:32am: Dr Stephen Brearey is being called to give evidence in the case of Child G.
10:33am: A reminder that none of the children can be identified in this case due to reporting restrictions. A naming system is in place, for Child A-Q.
10:36am: Dr Brearey confirms he has reviewed his clinical notes from the time of the care for Child G, from August-September 2015. He said by the time of the ward round, Child G was improving, having been at the Countess of Chester Hospital for a week [having been transferred from Arrowe Park Hospital], with main concerns being respiratory support. He recalls prescribing medication to help with Child G's bowels. On September 2, on the second ward round, there was a "pattern of improvement" and "everything was moving in the right direction".
10:40am: Dr Brearey's clinical note for 11am at Sunday, September 6, 2015, is presented to the court. He was the consultant for that weekend and carried out a check of Child G as part of a routine ward round. Child G was 97 days old at this point. she had been born at a gestational term of 23 weeks and six days. She was receiving feeds, including expressed breast milk, via the nasogastric tube and bottles. "Clearly she was making progress with that...and her oxygen requirement was coming down." The court hears Child G was 'quite stable' at this point.
10:46am: Child G was 'still a little under' her target weight by this stage, at 1.985kg, but this was "normal" for pre-term babies. Child G was on Gaviscon medication to help with the stomach lining, and other medication to help lower oxygen support requirements. Child G's gut was "clearly working normal", the chest was 'clear' and the abdomen 'soft'. Child G was considered to be at high risk of a chronic lung condition, as would be the case with many pre-term babies, and the plan would have been for monthly check-ups and a vaccine to help treat this.
10:51am: Dr Brearey then confirms he was called in, as the on-call consultant, at about 3.30am on September 7. Dr Alison Ventress had called him in, and was in the process of intubating Child G upon Dr Brearey's arrival. Dr Ventress noted Child G: "Had very large projectile vomit (reaching chair next to cot and canopy). Abdo[men] appeared discoloured purple and distended." Dr Brearey said he had not witnessed this sort of projectile vomiting before, in a pre-term baby "who has been stable for so long", without a suitable diagnosis of a condition which could cause projectile vomiting. Child G deteriorated and Dr Ventress intubated the baby girl. Dr Brearey confirms he was called in from home.
10:54am: He said Child G initially appeared she had stabilised after intubation, with 'normal' gas reading. He was then called to the pre-term delivery that Dr Ventress had been called away to, for a delivery at 4am. He said he was satisfied Dr Ventress had the situation under control, and there were satisfactory readings, so was called over to the delivery. The blood gas reading was, on Dr Ventress's note, 'good', 30 minutes after intubation. The ventilation status was also 'satisfactory'.
10:59am: At 5.30am, Child G had a profound desaturation. "Her heart rate dropped to 60[bpm] and her oxygen [saturation] to 40% - which is unusual" when Child G was on a ventilator. Dr Ventress wondered if the problem was the ventilation equipment, so moved to manual breathing support via a Neopuff device. Child G was then reattached to a ventilator, before the ventilator was changed. A 'large leak' remained, which meant the issue was unlikely to be with the ventilator. The 'large leak', Dr Brearey says, he cannot explain, for a pre-term baby. He says Dr Ventress was getting chest movement from Child G on the Neopuff device. "It's perplexing and I can't think of a natural cause why that would happen."
11:05am: Child G had another profound desaturation at 6.05am and the decision was made to reintubate her. The heart rate increased but the oxygen saturation levels remained low, despite further breathing support, with 100% oxygen ventilation and increased respiratory pressure. Those levels were "low" in the context of those support measures being applied, Dr Brearey says. Thick secretions ++ in mouth' were noted, with a blood clot at the end of the ETT. The oxygen saturation levels fell to 17%, with the heart rate down to 70bpm, and 'poor chest movement'. Dr Brearey tells the court a heart rate under 100bpm was cause for concern. He was called in urgently, the clinical note adds. The nasogastric tube was aspirated and 100mls was aspirated from Child G. "This seemed surprising" as Child G had been fed 45mls every three hours, and Child G "had already had a large vomit which covered the cot and the area around the cot". "It seems abnormal and I can't explain where that [aspirate] would have come from."
11:11am: The plan was to paralyse Child G, via a medication bolus, to allow for better ventilation, and to repeat a blood gas reading, and continue with morphine for sedation. Child G was 'nil by mouth' and IV fluids were to be given. Standard medicine to treat neonatal sepsis was also to be administered. The parents were 'about to be updated'. Dr Brearey said at the time they were not sure whether there was a problem with Child G's gut, given the large aspirate and large vomit, which was why the baby girl was 'nil by mouth'. An x-ray taken showed lungs of 'chronic lung disease', which was "known previously" and would not explain what had happened that night. The abdomen had 'generalised gaseous distention' - "but nothing which would indicate obstruction", and nothing which would indicate NEC, a gastro-intestinal disease.
11:17am: A note from Dr Brearey recorded, for the abdomen x-ray - 'gaseous abdomen, no perforation'. Dr Brearey's note adds, at 5.30am, 'compensated metabolic acidosis'. Dr Brearey says this is an 'error on my part', given the pH readings, from a 'long night'. The note concludes Child G's case 'will need discussion with Arrowe Park Hospital/Liverpool Women's Hospital' if her condition continued as it was.
11:21am: Dr Brearey tells the court Child G had an MRI scan following these events which "looked worse than previous scans". It was "still uncertain" what the long-term prognosis would have been since then, but since then Child G had developed dystonia, quadriplegic cerebral palsy, "as a result of brain damage in early life", which causes the muscles in the body to be stiff and have limited function. Child G required further feeding support mechanisms, so the food Child G has is less likely to aspirate [into other parts of the body] and be prone to chest infections. Child G was greatly dependent on the care of her parents. Dr Brearey adds: "I have great respect for everything they [the parents] have done for the last six/seven years."
11:23am: Ben Myers KC, for Letby's defence, is now asking Dr Brearey questions. Dr Brearey confirms he was the neonatal lead at the Countess of Chester Hospital for 2015-2016, and continued to hold that position until 2020. He said he would spend more time dealing with neonatal issues. Some of it would involve administration and management, but also development. Mr Myers says at the time of Child G's events, Dr Brearey believed infection was the most likely cause. Dr Brearey says his initial impression was that it was infection.
11:35am: Mr Myers says one of the problems was with oxygenation, and the ventilator was changed, but that did not resolve the problem with oxygenation. Dr Brearey agrees. Mr Myers refers to the ETT being removed at 6.10am, which was 'the same tube' being used for both ventilators. When the tube was removed, the blood clot was found, and that could have had an impact on oxygen saturation levels. Dr Brearey said it would not block it completely. He adds the blood gas results prior to that would not show that to be the case. "It might have a small degree of influence," but he said it would not have a huge impact, and in his experience he had not come across such an event, given that pressures are involved in the tube.
Mr Myers refers to the aspirates found - he asks if there is any reference to milk/fluid aspirates on the note. Dr Brearey confirms the type of aspirate is not shown. Mr Myers asks if Dr Brearey knew what the contents of that 100mls was. "The only other possibility if it is not stomach contents is if it's blood, and I certainly don't recall 100mls of blood." He said it would not be air, it would be recorded as fluid. He says the process of aspirating from the NGT, if it's just air, then that would be 'not significant and not recorded'. Mr Myers refers to Dr Ventress's recollection to court, that the '100mls' aspirated could have been air, although she was not 100 per cent sure, and if it was fluid, she would have recorded that. Dr Brearey said he wouldn't be 100 per cent, but if it was not air, that would be recorded. Mr Myers says the 100mls aspiration is not documented on Dr Brearey's note. Dr Brearey says in retrospect, he was concentrating on Child G's care, and it would have been easier, if knowing what was to come, to have recorded it on his notes. The prosecution rise to clarify about the blood clot, saying if that blood clot had blocked the tube, would the equipment have detected that. Dr Brearey said the equipment would have given off an alarm.
11:41am: Dr David Harkness, who has previously given evidence during the trial, is being recalled to give evidence in the case of Child G.
11:43am: He "vaguely" recalls the care of Child G, mainly from refreshing his memory by looking at clinical notes taken at the time. He tells the court Child G was "quite stable" with a small amount of oxygen support, and the most amount of support was via feeding, but she was not far off going on to bottle feeds each time. The feeds were 'greater than normal' to help Child G gain weight, as she was, at 1.985kg, a little underweight, and it was so Child G could go home without requiring nasogastric tube feeds. Dr Harkness confirms 'things were going in the right direction, generally', for Child G.
11:47am: For September 7, 2015, Dr Harkness notes the observations at the time of the event. He said he was on a day shift and was informed of the 'sudden desaturation' during the handover. He said sepsis 'was the most common' thing to think about whenever a baby has a desaturation, so Child G would have been treated for that. Chest x-rays were also a common test to carry out.
11:56am: The oxygen levels for Child G were "still dropping every now and then", with the heart dropping also, and she was "not doing particularly well with her breathing, despite being ventilated". During the daytime observation, the mean blood pressure for Child G was "low", despite being on medication to increase that, which Dr Harkness says was "worrying". Child G's heart rate was 200bpm, which was high, and the urine output was very low. The blood test taken for sepsis "was not an exact science"; the readings were "not alarming" but "difficult to take in isolation", the court hears.
12:02pm: Among the 9am plan for Dr Harkness on his notes, was 'discuss with tertiary centre' - as Child G was "so unwell". A follow-up note from 10am showed Child G's blood pressure had risen to a normal level, a low carbon dioxide level, and the blood gas reading showed a high pH number of 7.646 and a high lactate number. The plan was to decrease the ventilation support and repeat the blood gas in 30 minutes. Dr Harkness says Child g was "incredibly sick", had stabilised by 10am, but still "incredibly sick and we were worried about her at that time". He says the situation had improved but Child G needed a lot of support and was "not out of the woods at that point". He said the blood test was inconclusive, and could not recall why aspirations was on his list, and there was nothing on his record that could 'conclusively' say it was sepsis or some other diagnosis.
12:08pm: Mr Myers, for Letby's defence, asks Dr Harkness if he agrees that a sudden deterioration for Child G is 'not uncommon'. Dr Harkness says it is "very rare" in a stable, term baby. Mr Myers refers to Dr Harkness's statement to police in 2018, in which he said for September 7, 2015, at 9am: [Child G] had a deterioration - which is not uncommon' Dr Harkness says in his years of subsequent experience, he has seen considerably fewer sudden collapses. At the time of the statement in 2018, he had had seven years experience. He says as a point of generalisation, it was "not uncommon", but in term babies, it was 'uncommon', now he has had further years of experience and context. Mr Myers says in Dr Harkness's statement to police, the deterioration 'was no surprise to him' as it was relatively common, as there was a risk of infection in such babies. Dr Harkness says with further years, he has seen it "less and less", and would no longer hold that view. He says at the time, he felt it was relatively common, from his time in Chester.
12:25pm: The court is resuming after a short break. Senior nurse Christopher Booth is now being called to give evidence. He was employed at the Countess of Chester Hospital in 2015, and would sometimes be employed as a shift leader in the neonatal unit. He confirms he recalls Child G was an "extremely premature baby" who was approaching her 100th day milestone. He said: "We knew her well, we knew her family well." He says Child G was making good progress and establishing feeds, sometimes via a nasogastric tube and sometimes by bottle. Philip Astbury asks if there was anything Mr Booth can recall about the time approaching Child G's 100th day. He says it is a big milestone for babies on the unit. He tells the court: "We do make a big thing about it - it's an important event, we make banners for the family, one of the staff members brings in a cake for the family to celebrate."
12:30pm: Mr Booth is shown the shift layout for the September 6-7 night shift, in which he was looking after a baby in one of the neonatal unit rooms that night. He recalls, from his memory and what he has read from his statement, a call being put out when Child G had a "sudden deterioration", and her "colour was poor", at 3-3.15am. He said he was not aware of the projectile vomiting incident earlier that night, and that was ascertained later. He said he was there to help in the resuscitation efforts, having been 'quite peripheral' in the incident.
12:32pm: "A verbal call to seek assistance" was made at 3-3.15am. Mr Booth entered the nursery and saw Child G was being given breaths via a Neopuff device and oxygen support. He says Lucy Letby was there along with another nurse, and a senior house officer, and an urgent call for the consultant Alison Ventress was put out. Rescue breaths' were being given to Child G. Mr Booth says he cannot recall who was administering these. He recalls after 10 minutes, it was "prudent" to move Child G into nursery room 1, which had more suitable equipment and was "more suitable" to treat "sicker babies".
12:34pm: He tells the court he assisted in the transfer of Child G to room 1. He recalls he was aware of more apnoea episodes for Child G that night, but as he was happy with who was looking after Child G, he 'took a step back' from personal involvement. He says Lucy Letby was among the dedicated nursing staff for Child G.
12:37pm: Mr Myers KC, for Letby's defence, says he has no questions to ask of Christopher Booth.
12:43pm: Nicholas Johnson KC, for the prosecution, recalls medical expert Dr Dewi Evans to give evidence, for Child G. Mr Johnson reminds the jury this part of the case is for the first attempted murder charge on Child G (of three; the other two allegedly taking place on September 21, 2015).
12:47pm: The court hears Dr Evans has written several reports in respect of this case, the most recent being in September 14, 2022. Mr Johnson refers to a report Dr Evans made in May 2018. Child G was born at Arrowe Park Hospital on May 31, 2015, and two weeks later was examined via a cranial ultrasound to identify if there was any bleeding on the brain. Dr Evans says this is carried out routinely, and the absence of any bleeding on the brain was a very encouraging sign. The court hears Child G had been born "exceptionally early". Dr Evans said in his report that gestational age of 23 weeks and six days was "at the limits of viability".
12:50pm: Dr Evans explains the type of IV access that was given to very premature babies such as Child G. A follow-up ultrasound on June 30 showed no bleeding on the brain for child G, and was "very satisfactory", Dr Evans explains. Child G was transferred to the Countess of Chester Hospital in August 2015. At the time of her discharge, Dr Evans said she was "stable", with known chronic lung disease which required oxygen breathing support, and CPAP.
Dr Evans: "It was the standard management of babies when they have chronic lung disease."12:52pm: For the first couple of weeks at the Countess, Child G required 28-31% oxygen. A follow-up ultrasound showed "nothing concerning", and Child G had normal observations, requiring medicines which were common for premature babies, such as Gaviscon and supplemental sodium and iron. "All was well and her oxygen saturation was 95% which was very satisfactory".
12:58pm: Dr Evans says Child G's observations were "very satisfactory" at the Countess of Chester Hospital in early September 2015. Child G's condition was getting "even better" with oxygen breathing support being weaned off.
1:02pm: The observation for the shift of September 6-7 is shown to the court. The respiration rate is 'normal', with readings normally marked, in the three-hourly observations up to 2am. He says he is not sure why the individual readings have a cross and circle marked for the hourly observations afterwards, but suspects that is because Child G was on ventilation support. The oxygen saturation readings are "very stable" up to 2am, with the baby girl's readings "as stable" as they were in previous days. A mixture of medications is recorded on the intensive care chart for 4am onwards.
2:06pm: The trial is now resuming following a lunch break. Dr Dewi Evans will continue to give evidence.
2:12pm: Dr Evans agrees that Child G was in a satisfactory condition, prior to the events of September 7, 2015. Dr Alison Ventress's notes from the early hours of September 7 are shown to the court, describing Child G's projectile vomit at 2.35am, purple and distended abdomen, and increased oxygen requirement. 'Red in face and purple all over'. Dr Ventress noted Child G had 'gone apnoeic and dusky', and upon additional breathing support, the oxygen saturation levels went up and the baby girl was taken to nursery room 1.
2:18pm: A photo is shown to the court with black circles indicating where Child G's projectile vomit patches went. One patch is in the cot, another patch is on the floor, and another is on the seat of an adjacent chair. Mr Johnson continues to talk through the sequence of events, which Dr Evans confirms he has noted throughout his report.
2:19pm: Dr Evans said in his report, for the 100mls aspirate taken from Child G, "It is not clear how much of the 100mls was milk, and how much was air".
2:25pm: Mr Johnson asks about what happens if a baby's stomach is full. Dr Evans says if you give milk gravitationally, no more milk will go in, as the stomach is full. He says the baby is unlikely to absorb the final few millilitres of milk if the stomach capacity is, for example, 45ml, and the milk portion is 55ml. While the stomach could expand a little, the likelihood is the milk would drip out. Dr Evans describes there is a way of "forcing" more milk into the stomach via a syringe, which "you would never do" as it would forcibly distend the stomach.
2:30pm: Dr Evans says he was looking for signs of an infection in the records, as it is one of the most common findings on a neonatal unit, so one is "always alert" to that possibility. From Child G's blood test at 3.59am on September 7, the findings were all considered "normal" and did not point to a sign of infection, the court hears. A subsequent blood gas reading, 10-12 hours later which contains 'CRP: 28' is "not particularly high" but is a sign of infection. The subsequent blood gas reading after that was indicative of infection, Dr Evans tells the court.
2:32pm: Dr Evans says Child G, at birth, was "on the margins of survival", but it was the "skill of staff" at Arrowe Park which ensured her stabilisation. He says there were no signs Child G was unwell prior to her collapse on September 7. He says the only two considerations were the chronic lung condition, which was common and for which she was receiving treatment, and establishing feeds. "Considering her start in life, this was an extremely satisfactory state".
2:34pm: Child G's weight of 1.985kg was a little low, but she was tolerating bottle feeds every other feed (with nasogastric tube feeding on the other occasions). Dr Evans says Child G would likely have still required supplemental oxygen support once she went home.
2:40pm: The photo showing where the projectile vomiting patches landed is shown to the court. Dr Evans says there are three black circles. The one in the cot indicates the baby was sick, which "would be worthy of note, but not unusual". The second one between the chair and cot, on the floor. "For a baby of 2kg to vomit that far is quite remarkable". Dr Evans says there is a condition which can cause projectile vomiting of that length, as had been mentioned earlier today by one of the doctors, but Child G showed no signs of having that condition. Dr Evans adds: "Even more astonishing is the vomit that ends up on the chair. That is several feet away. "I can't recall a baby vomiting on the floor. I can't recall a baby vomiting that distance. It was described quite correctly as extraordinary. "On top of that it was noted the abdomen was distended." Dr Evans said you cannot measure the volume of the vomit that had fallen.
2:43pm: Lucy Letby's note for Child G - 'large projectile milky vomit at 2.15am. Continued to vomit++. 45mls milk obtained from NG tube with air++. Abdomen noted to be distended and discoloured.' Dr Evans said the 45mls aspirated was in addition to the vomit. 45mls of milk was administered by the feed. "There can only be one explanation - [Child G] had received far more milk down the NG Tube. "She may have also received a bolus of air from the feeding tube." Dr Evans says that would also cause the abdominal distention. He says the plunger end of the syringe was put over the end of the tube for the milk, which would have caused distention, then would have caused the baby distress, then "she would have vomited because of the gross distention".
2:46pm: The condition which can cause projectile vomiting can be excluded, the court hears, as the vomiting would have continued until the baby would have been taken into theatre for surgery. Dr Evans says the muscles only 'go one way', and the only time this does not work is if the baby is compromised by something. "In this case the baby was compromised by receiving a large volume of milk to the stomach". In that instance, the stomach muscles contracted and that led to the vomit. He says the mechanism is similar to that seen in adults. He says if an adult drank a large volume of liquid too quickly, there is a chance they could vomit.
2:51pm: Dr Evans says Child G's condition thereafter was "incredibly unstable", with "significant amount of oxygen deprivation" and bradycardia. "Getting [Child G] back to where she was before 2am was extremely challenging and difficult. "They managed to do so...but during that time she suffered prolonged oxygen deprivation...leading to irreversible brain damage." The doctor's note of 'blood at the back of the throat' is referred to. He said the bleeding was found at the initial resuscitation/intubation, and the significance of that was the baby did not have a bleeding disorder, so "therefore the bleeding present from the beginning from more or less the time [Child G] crashed." Dr Evans says this case has been seen before, "much worse", in Child E. The bleeding in this case was less, but still significant as it was "unexpected".
2:53pm: Dr Evans stresses Child G's infection happened "after the collapse".
2:55pm: Dr Evans says Child G's infection was 'CRP related', as those particular blood gas readings went from 'less than 1' to 'over 200' in the hours following her collapse.
2:59pm: Dr Evans's report from 2021 is now being discussed. He was asked to consider whether an infection was the cause of the projectile vomiting. "With respect no, I consider the infection happened afterwards. "An infection would not cause a baby to vomit halfway across the nursery room." He also asks: "Where would the extra fluid come from?" He says Child G must have had "far more" than the allocated 45mls milk feed fed to her.
3:02pm: Dr Evans is asked about Lucy Letby's explanation that babies can swallow a lot of air when they vomit. "Well, they don't." Dr Evans replies. He says excess air was administered to Child G, in addition to the milk. He adds a baby with an infection has never presented in this way. He also says a baby on a nasogastric feed would not vomit. The NGT system would be set up, Dr Evans says, so the undigested milk would be aspirated prior to another feed. If there is a lot of undigested milk, then caution would be taken before administering another feed. The pH would be measured before each feed to ensure the tip of the NGT is in the stomach, and not another orifice.
3:03pm: On this occasion, a pH reading of four would indicate the presence of stomach acid, indicating the NGT was in the correct place, Dr Evans says.
3:05pm: Dr Evans is asked to read out his further report, in which he says administering excess milk and/or air cannot be done "accidentally". The effect of the stomach being overfull, the diaphragm "cannot move up or down", meaning "the baby cannot receive air in its lungs", which leads to oxygen deprivation, loss of oxygen saturation, bradycardia, and collapse.
3:08pm: Ben Myers KC, for Letby's defence, is now asking Dr Evans questions. He says Child G was 'born on the margins of survival', and Dr Evans agrees that is the case, having said so in his May 2018 report. Mr Myers says a lot of work was needed to get Child G stable. Dr Evans agrees. He says that, relative to where she began, she was a lot better. Mr Myers asks if she was still prone to infection. Dr Evans agrees.
3:12pm: Mr Myers refers to Dr Evans, in his report, referring to Child G being treated "inappropriately" at 2am on September 7, 2015. Mr Myers says that is worked on the basis that Child G's tummy would have been empty or almost empty at the time, as the nurse responsible would have aspirated Child G's stomach of all milk. Mr Myers says 'we now know' the stomach was not aspirated prior to 2am. Dr Evans says that was not the case, as the nurse had aspirated to get a pH reading. Mr Myers says the nurse had not aspirated the milk, as she would not have done so in a baby as young as Child G as a matter of procedure.
Dr Evans: "No, this is too simple." He says milk is a neutral pH, so if the reading is '4', then that sample was indicative of acid in the stomach.3:13pm: Dr Evans says after the projectile vomiting, over three areas of a nursery, there was an aspiration of 45mls of milk. "There has to have been a significant amount of additional milk plus air to explain what happened to the little baby at two o'clock in the morning."
3:16pm: Mr Myers refers to the report, saying a nurse empties the stomach contents through aspirates.
Dr Evans: "The pH was 4 [in the stomach], 4 is acid." Mr Myers says Dr Evans is basing what he says upon having her stomach aspirated before the 2am feed. Dr Evans says there would have been no milk in Child G's stomach prior to the 2am feed, as the stomach was checked for pH.3:22pm: Dr Evans says he is "totally satisfied" with his opinion that Child G's stomach was empty prior to the 2am feed. The amount of vomit plus aspirate was "massive" and only had one explanation - "she had a huge amount of milk plus air". Mr Myers asks if Dr Evans is basing his opinion on Child G's stomach being emptied of milk just before the 2am feed. Dr Evans says he is. He says the nurse said she would not normally aspirate all the milk from a stomach [as in completely remove all trace]. Mr Myers says, in the six reports, there is no mention of the plunger to the syringe as a method to force more milk in. Dr Evans agrees it is not in his reports, but he is telling him now.
3:30pm: Mr Myers says 100ml of aspirate was withdrawn at 6.15am, but the quantities of liquid/air were not known. Mr Myers says Dr Alison Ventress said it was "probably air". Dr Evans agrees he heard that evidence. The clinical note for Child G on September 7, by Dr Ventress, is shown to the court. Mr Myers relays Dr Evans's note relating to excess fluid inhibiting diaphragm movement.
Mr Myers: "In fact we know that the later collapse and desaturations came after [Child G] vomited [on the morning of September 7]." He says "that is distinct" as Child G had "settled" by that point.
Dr Evans: "That is not correct, actually - she was in a very unstable condition." Dr Evans says there is 'hardly' an entry where Child G is stable for any significant period of time that morning. He says from the time of the vomiting, Child G "never fully stabilised". He says the medical staff would not have anticipated the oxygen deprivation being "very marked" and for a "more prolonged time than they would have realised", and that was no fault of the staff. He says Child G's condition was "an improvement" but she was "unstable", and had been "compromised from the point of vomiting".3:32pm: Dr Evans says it is difficult for medical staff to "provide a running commentary" when trying to save a little baby's life. The removal of vomit and 45ml aspirate had "got rid of the pressure" and would have led her to be "relatively better" - "and I use the words advisedly". He tells the court he is "very satisfied" with the explanation he has given.
3:35pm: Mr Myers says the bleeding seen is "not even close" to the case seen with Child E. Dr Evans says it is in the same area. Mr Myers says to link it to Child E is to support the prosecution. Dr Evans says that is not the case, and if he did not have access to the other cases, he would have come to the same conclusion. He adds that Child G was, chronologically, was the first case he examined. Mr Myers says there is no evidence of trauma. Dr Evans says he does not know the cause, but seeing such bleeding was "incredibly concerning" and "worrying".
3:36pm: Mr Myers asks if it was possible Child G had a small haemorrhage. Dr Evans says there would have been no reason for it. "No is the answer to that". He says the back of the throat is a small area, and the blood was noticed around there.
3:41pm: Mr Myers says babies may vomit for many reasons. Dr Evans agrees. Mr Myers asks is 'forceful vomiting' can happen. Dr Evans says he is not familiar with the term in that context. Mr Myers says Dr Evans does not agree with Dr Ventress's evidence on projectile vomiting. Dr Evans says he only disagreed with infection being the cause of the projectile vomiting. Mr Myers asks if Child G projectile vomited with such force because she was unwell. Dr Evans disagrees, and asks where the extra fluid would have come from.
Mr Myers: "We don't know [the quantity of vomit as it was not measured]."
"No, but it's a lot of vomit."
"We don't know how much, do we?"
"It was...an awful lot of vomit."3:42pm: Gastro-oesophageal reflux can cause projectile vomiting, Mr Myers asks. Dr Evans says it can, but that was not mentioned as a diagnosis in the Arrowe Park Hospital discharge letter. It would not have caused the type of vomiting seen, Dr Evans tells the court.
3:50pm: Mr Myers refers to the CRP readings for Child G, which had risen throughout September 7, and was "consistent with infection". Dr Evans agrees. Mr Myers says that could have been consistent with infection developing before the vomiting. "No, it cannot." Dr Evans says the CRP reading is raised at the time the infection presents. He says the majority of babies, a CRP reading is raised at the time of the infection being present. In this case, there were no other markers of infection prior to the vomiting. Mr Myers says there was a "large watery stool", to which Dr Evans says was not unusual. Mr Myers says there is no finding of aspiration pneumonia when Child G was taken back to Arrowe Park. Dr Evans says she does not believe she had that, but believes she had an infection which "probably kicked in" during the attempts to resuscitate her. Mr Myers says that does not rule out an infection being present prior to the vomiting.
Dr Evans: "There is no clinical evidence to back up that hypothesis." He adds: "I don't deal with 'ifs', I deal with evidence." He says the charts show everything as they should be up to the point of the vomiting and desaturations.3:54pm: Mr Johnson asks Dr Evans about the 'adding of a suggestion of a plunger being used' in the evidence, in the context of milk feeds. Dr Evans had referred to the forcible additional milk feed method, without the additional context of a plunger, in his May 2018 report. Dr Evans says the method can only be applied with the use of a plunger. Mr Johnson asks about the pH aspirate the nurse would have obtained, if the previous milk feed had not been digested/aspirated. Dr Evans said the aspirate would have looked like undigested milk and the pH reading would have been neutral - around 7.
3:57pm: The feeding chart for September 5 is shown to the court, which Dr Evans says shows no vomiting, and no evidence of gastro-oesophageal reflux. He says gastro-oesophageal reflux does not happen out of nowhere. Dr Evans adds Child G was having normal bowel movements as well.
3:58pm: Dr Evans says, for the feeding charts and observations prior to the vomiting, "this is as good as it gets", with "no red flags", and is "very satisfactory".
4:00pm: Medical expert Dr Sandie Bohin is now being recalled to give evidence.
4:05pm: Mr Johnson takes Dr Bohin through her reports, in which she said there was "no cause for concern" in Child G's condition at the Countess of Chester Hospital prior to September 7, 2015.
4:08pm: Dr Bohin confirms Child G was given a 45ml milk feed via the nasogastric tube at 2am on September 7, 2015. Mr Johnson refers to the subsequent sequence of events, and that Dr Bohin had recorded what had happened from the medical staff's notes and medical charts.
4:11pm: Dr Bohin said Child G was, prior to the collapse, "very stable", with decreasing oxygen support required, and she was "managing very well" on that. "From a respiratory point of view, all was well". Child G was tolerating three-hourly feeds, and she was "progressing very well" for a pre-term baby. The observation chart prior to the 2am feed on September 7 was "completely normal".
4:15pm: The episode of 'projectile vomiting' was 'concerning' as Dr Bohin said she had not seen babies, particularly those weighing 2kg, doing that. She found that "extraordinary". Dr Bohin said the milk must have come from somewhere, and the vomit has to go over the side of a deep-sided cot, on to the floor and the nearby chair "a considerable force has to be generated inside the abdomen". She says there must have been "much more than 45mls of milk inside the stomach." Mr Johnson asks if there is an 'innocent explanation' which could have explained the projectile vomiting. Dr Bohin says "no", as the stomach was empty, with a pH reading of 4. If there was milk in the stomach, it would have 'neutralised' the stomach and the pH reading would have been higher. "I think the stomach was empty, and she was given excess milk and possibly air...which distended the stomach."
4:18pm: Dr Bohin is asked by police about Lucy Letby saying babies can 'take on a lot of air when vomiting'. Dr Bohin was asked if that was correct or not. Dr Bohin tells the court: "That's not correct. Babies do not take on air when they vomit."
Tuesday 13th December 2022
Child G
Dr Sandie Bohin - Statement of Medical engineer Steve Eccles - Police analyst: Recorded events & messages - Unnamed nurse10:23am: At Manchester Crown Court again today for the trial of nurse Lucy Letby. Jurors will continue to hear evidence about the collapse(s) of Child G - who the Crown say Ms Letby tried to murder on three occasions in 2015
10:34am: Medical expert Dr Sandie Bohin is continuing to give evidence today. She tells the court that it was 'extraordinary' for a baby the size of Child G - she was 2kg - to vomit as far as she did.
10:36am: She said: 'She would have had to have exerted a huge amount of force to vomit over the side of the cot and onto the floor and chair…that's surprising given she was only 2kg'
10:47am: Dr Bohin is taking the court back through Child G's medical notes and spelling out the infant's early feeding history and how that developed. The notes show that through summer 2015 she was gradually improving
10:50am: Dr Bohin makes the point that medics were considering giving Child G immunisations around the time of her collapse. She said the baby 'must have been well and stable' as medics 'wouldn’t consider giving immunisations unless a baby is absolutely stable'
11:04am: On the incident of 7 September, Dr Bohin tells the court that Child G 'must at some point have been given an excessive amount of milk to projectile vomit and have a residual 45ml in stomach'
11:09am: Ben Myers KC, defending, is now questioning Dr Bohin. He is taking the court back over Child G's medical notes from June 2015. Dr Bohin agrees at this time the premature girl was as 'sick as you could possibly be'
11:20am: Mr Myers is looking notes that she had a discoloured abdomen. Dr Bohin says that at this stage the girl would have weighed just 500g and there would be no subcutaneous fat - so could see blood vessels (hence discolouration normal) riation normal)
11:44am: We're continuing to view notes on Child G from the first few weeks after her birth. They show she was on steroids (as she was having trouble with ventilation). Bleeding noticed at one point was put down to a 'probable pulmonary haemorrhage'
11:47am: Dr Bohin notes that Child G had a low platelet count, which could explain the bleeding. She says 'certainly in a baby this fragile' a pulmonary haemorrhage could be lethal - states if it was indeed such a haemorrhage it was 'very mild'
11:56am: Mr Myers is taking the court through a note from the end of July 2105 which showed a 'significant' desaturation before Child G was due to travel from Arrowe Park to the Countess of Chester. Dr Bohin agrees that the infant was not well at this stage, 'she was still very young, still very vulnerable and prone to all sorts of complications due to her prematurity'
12:17pm: Mr Myers is making the point that, as an expert witness, Dr Bohin is allowed to hear all the evidence as it is presented to the court. She rejects suggestion that her conclusions have 'come from a dialogue with Dr Evans' (the other medical expert in this case)
12:46pm: Court has just been read a statement from Countess of Chester medical engineer Stuart Eccles. This was on the ventilation equipment at the hospital. Yesterday we heard doctors believed there could have been a problem with a machine as Child G was struggling to breath Service records show that there was no such issues reported on 7 September 2015. He said the machines on the unit were 'very reliable'
12:51pm: Police intelligence analyst Kate Tyndall is now back in the witness box. She is taking the court through sequencing evidence.
12:54pm: After Child G fell ill, she was transferred to Arrowe Park Hospital where she recovered over a number of days. On 16 September she was transferred back to the Countess of Chester. On 21 September, the Crown say there was second incident involving Ms Letby
2:24pm: Nursing notes recorded by Ms Letby show that at around 10:20 on 21 September Child G had two projectile vomits and went apnoeic for a short period. She suffered brief self-resolving colour loss and her blood saturations fell to 30%
2:40pm: Court being shown text messages between Ms Letby and a former colleague on the evening of 21 September. Ms Letby said Child G 'looked rubbish when I took over this morning then she vomited at 9 and I got her screened...mum said she hasn’t been herself for a couple of days'
3:16pm: A former nursing colleague of Ms Letby, who cannot be named for legal reasons, is now in the witness box. She is recalling the events of 21 September
4:06pm: Court told that Child G was cannulated, behind a screen, and placed on a Masimo monitor - a portable device attached to the patient by a sensor that continually measures oxygen saturations and heart rate levels. After the doctors had gone, but Child G was still screened, the nurse told the court that she heard Ms Letby shouting for help. She said she responded, Ms Letby was using neopuff on the infant - who 'did not look very well at all' She noticed that the monitor screen was black and had been switched off.
4:07pm: The nurse said this was not normal procedure (for the monitor to be off)
4:10pm: The nurse however has told the court that she asked to review her original statement to police last month - as she said she had seen in the prosecution opening that there was a suggestion Ms Letby had turned the monitor off - she said 'I knew that not to be the case'
4:12pm: She tells the court that on 21 September two doctors came her to apologise, as they had left the screen in situ and not switched the monitor back on
4:49pm: Court has now adjourned. Back tomorrow.
Chester Standard article 3-12-2022
A MOTHER told Lucy Letby she was "so pleased" she was caring for her baby girl on a shift when the nurse allegedly tried twice to kill her, a court has heard.
The youngster vomited on the neonatal unit at the Countess of Chester Hospital when Letby, 32, is said to have deliberately overfed her with milk on the morning of September 21, 2015.
Later that afternoon, the defendant is said to have switched off a monitor attached to the infant, known as Child G, during a collapse.
The Crown say the two incidents followed a first attempt to murder Child G when Letby is accused of giving her excess milk, and probably air, via a nasogastric tube (NGT) in the early hours of September 7.
That sudden deterioration took place as Letby earlier helped make a banner to mark the 100th day of life for Child G, who was born extremely premature and weighed just more than one pound.
Child G was subsequently transferred to Wirral's Arrowe Park Hospital and she improved with specialist care before she was moved back to the Countess of Chester on September 16.
Five days later – when Child G was originally due to be born – Letby recorded that she gave her a feed of breast milk through the NGT. The infant was asleep at the time at about 9am and was due to receive immunisations later that day, jurors at Manchester Crown Court were told.
She went on to note at 10.15am there were "two large projectile milky vomits" before Child G stopped breathing, her oxygen levels plummeted and she lost colour.
Child G's mother had arrived at the unit shortly after 10am and was later updated about her daughter's deterioration and recovery.
Following completion of her shift Letby messaged a colleague in the evening to say: "(Child G) poorly again.
"Due date today!"
Her colleague, who cannot be identified for legal reasons, responded: "Oh she likes to 'celebrate' the big ones in style (sadface)."
Letby replied: Due imms (immunisations) today too. I got her screened this morning after she vomited."
Her colleague said: "Was she still in (nursery) 4 then?"
Letby said: "Yup and had NN (nursery nurse) all weekend … looked rubbish when I took over this morning, then she vomited at 9 and I got her screened."
The colleague said "See. It really worries me. I wasn't on when she was moved but wouldn't have done it myself."
Letby replied: "I personally felt it was a big jump considering how sick she was just a week ago. Being in 4 is bad enough and then having NN that just doesn't always know what to look for/act on. Mum said she hasn't been herself for a couple of days."
The colleague said: "F***. I wish she'd told a registered nurse."
Letby said: "It's hard isn't it. When mum came in today she was like oh I'm so pleased you've got her which I thought was a little strange as I don't know her that well but wonder if she just felt reassured to have a nurse."
Letby, originally from Hereford, denies murdering seven babies and trying to murder 10 others between June 2015 and June 2016.
Wednesday 14th December 2022
Child G
Unnamed nurse - Dr Peter Fielding (SHO) - Dr John Gibbs - Nurse Caroline Bennion - NNU Manager Eirian Powell - Expert witness statements from Professor Simon Kenny, Dr Stavros Stivaros10:47am: Lucy Letby's trial resumes at Manchester Crown Court this morning. We're continuing to hear evidence in relation to Child G. Ms Letby is accused of attempting to murder the baby three times at the Countess of Chester Hospital in September 2015
10:52am: Ben Myers KC, defending, is questioning a former nursing colleague of Ms Letby about the events of 21 September 2015. Child G had projectile vomited and had difficulty breathing on the morning of that day.
11:00am: Yesterday, the nurse told the court that Ms Letby shouted for help with Child G on the afternoon of 21 September. The nurse responded and noticed that the monitor had been switched off, which was "not normal protocol", but refuted any suggestion Ms Letby had turned it off.
11:01am: She explained to Mr Myers that two doctors had apologised to her, as they had not switched the monitor back on. She agreed that the monitors should have been turned back on.
11:16am: Dr Peter Fielding, who was a senior house officer on the Countess of Chester neonatal unit in 2015, is now in the witness box
11:25am: The court is now being shown Dr Fielding's notes from the morning of 21 September when Child G fell ill. They start with a summary of the baby's health, notes she is premature and has chronic lung disease. Also notes medicines that she was on at the time.
11:34am: Dr Fielding, in questioning from Mr Myers, says he didn't witness the projectile vomiting incident and by the time he arrived on the unit Child G was 'recovering'
11:48am: Dr John Gibbs, who was working as a consultant paediatrician at the Countess of Chester in 2015, is now in the witness box.
11:52am: Dr Gibbs tells the court he attended the neonatal unit and examined Child G after she had projectile vomited and her blood saturations fell to 30%. Dr Gibbs described that as a 'severe desaturation'
11:55am: Dr Gibbs said: 'It’s just unusual for a premature baby who had been feeding entirely satisfactorily since returning from Arrowe Park Hospital to be projectile vomiting'
12:07pm: Dr Gibbs is recalling the difficulty of fitting a cannula on Child G on the afternoon of 21 September. He said given the level of intensive care she had had in her life, it was difficult to find a vein
12:08pm: Dr Gibbs says he cannot remember what room or what type of cot Child G was in, he also cannot remember what he did after fitting the cannula (given this is seven years ago)
12:09pm: Asked if she was attached to a monitor, he can't remember but says 'given her problems she should have been on monitoring yes'
12:13pm: He says if a sensor from the monitor is taken off a baby's body part - in order to fit a canula - then it should be fitted to another body part. He says 'it shouldn't be left off'...he adds that there 'shouldn't be no monitoring at all'
12:15pm: Asked what he did after the cannula was fitted, he says that he doesn't remember but he wouldn't have left Child G alone. He says he would have alerted a nurse on the unit. Asked if there was any subsequent conversations, he says he 'can't remember'
12:22pm: Mr Myers is now questioning Dr Gibbs. He asks the medic whether gastro-oesophageal reflux, that Child G was suffering with, could cause projectile vomiting - he says 'possibly'
12:28pm: Mr Myers is now asking about the monitor. He asks Dr Gibbs if the monitor is switched off during cannulation - he says 'it shouldn't be'....he adds that he can't remember what happened with Child G's monitor on 21 September
12:36pm: Dr Gibbs agrees that it would be a 'serious error' for a baby to be left behind a screen, detached from a monitor and no nursing staff told - but says he cannot remember if he did this
12:38pm: Mr Myers puts it to him that this is what happened and cites evidence from a nurse, who cannot be named for legal reasons, who said he and another doctor apologised for doing this. Dr Gibbs says he cannot remember, but adds if the nurse said this then 'it must have happened'
12:46pm: Senior nurse Caroline Bennion is now in the witness box.
2:16pm: Ms Bennion is being cross examined by Mr Myers KC about her recollection of the events of 21 September. She is being taken back over the clinical notes from that day
2:20pm: Ms Bennion says she does not have a recollection of 'who was doing what' at 15:30 that day (when Child G was cannulated)
2:29pm: Ms Bennion agrees that as Child G was an extremely premature baby she 'did have the potential at any stage to deteriorate'
2:38pm: Eirian Powell, who was the neonatal manager at the Countess of Chester in 2015, is now giving evidence. She is being asked about the events of 21 September. She tells the court she was due to give Child G her immunisations that day
2:40pm: She says that there was 'some instability' with Child G's temperature and was told she 'wasn’t well enough at that time', so the immunisations were withheld
2:46pm: Other than her immunisations, Ms Powell said she cannot remember any other issues reported to her with Child G
2:58pm: Statements from expert witnesses are now being read to the court. The first was from Prof Simon Kenny and second Dr Stavros Stivaros. These statements are agreed evidence, meaning defence agree with content
3:08pm: Court now adjourned, back tomorrow.
Chester Standard article 14-12-2022
A DOCTOR has accepted he must not have turned back on a monitor for a baby girl allegedly attacked by nurse Lucy Letby.
The prosecution says Letby, 32, switched off the oxygen monitor during a collapse of the infant on the neo-natal unit at the Countess of Chester Hospital.
It is alleged it was the defendant's third attempt to murder the youngster, known as Child G, within a fortnight in September 2015, as her oxygen saturation levels "significantly" dropped and she had to be moved to intensive care.
The incident is said to have taken place shortly after a consultant paediatrician fitted an intravenous cannula to Child G behind a privacy screen in a nursery room at about 3.30pm on September 20.
A nurse, who cannot be identified for legal reasons, told jurors at Manchester Crown Court she heard Letby call for help from the nursery.
She said the screen was still up when she entered and a "concerned" Letby was trying to revive the youngster who was not breathing.
And she recalled a nearby monitor, which also measures heart rate, was not switched on.
On Wednesday, she confirmed to Ben Myers KC, defending, that she spoke to detectives last month after reading the opening speeches online which suggested Letby had switched off the monitor.
Mr Myers said: "From what happened you knew that was not the case?"
The nurse replied: "As far as I'm aware I believe that was not the case."
She said two doctors, consultant Dr John Gibbs and registrar Dr David Harkness, approached her the same afternoon to apologise for leaving Child G behind the screen and for not turning the monitor back after completing the procedure.
Mr Myers said: "I suggest Ms Letby was cross that the doctors had left her behind the screen with the monitor off?"
The nurse said: "I don't remember that.
"I remember her being concerned."
Mr Myers said: "Do you recall she said this is something to make a formal complaint about?"
The witness replied: "I don't remember but I went to my manager to report it myself without anyone suggesting it."
Dr Gibbs told the court he could not remember whether Child G was screened.
He also could not recall whether Child G was connected to a monitor but said she "must have been" given her medical history after she was born extremely premature months earlier weighing just more than one pound.
Dr Gibbs said normally he would have told a nurse, ideally in the same room, when he was leaving but added when inserting a cannula a nurse would usually still be around.
He stated to police he couldn't remember whether Child G's monitoring equipment was switched off during a seventh attempt that day by medical staff to insert a cannula Mr Myers said to Dr Gibbs: "I am going to suggest that you and Dr Harkness left without telling any nurse that you had finished, could that have happened?"
Dr Gibbs said: "That should not have happened but I don't remember who I spoke to."
The retired consultant agreed it would be a "serious error" to have left a baby behind a screen without a monitor switched on and not inform a nurse.
Mr Myers said: "Later both you and Dr Harkness spoke to (the nurse) to apologise for that.
"Now that happened, didn't it?"
Dr Gibbs replied: "I'm sorry but I don't remember that."
Mr Myers said: "If you had left a baby unattended without the monitor on and it's a matter you had to apologise for, you would remember that?"
Dr Gibbs said: "I would expect so."
Mr Myers said: "If you had left a baby like this would it have concerned you?"
"Yes," said Dr Gibbs.
Mr Myers went on: "If it was very busy and you were being overstretched across different parts of the hospital, if you had to leave in a rush for instance?"
Dr Gibbs said: "That's one reason I might not have had time to speak to a nurse like I should have done, but I can't remember."
Mr Myers said: "You apologised that she had been left behind a screen unattended?"
Dr Gibbs said: "If that is what (the nurse) says then that must have happened, I just don't remember that."
Mr Myers said: "And left the monitor switched off?"
Dr Gibbs said: "If that is what is she said then presumably that happened."
Letby, originally from Hereford, denies murdering seven babies and trying to murder 10 others between June 2015 and June 2016.
Thursday 15th December 2022
Child G
Dr David Harkness10:30am: I'm back at Manchester Crown Court this morning for the trial of nurse Lucy Letby. Jurors will continue to hear evidence in relation to Child G. Ms Letby is accused of attempting to murder the infant on three occasions in September 2015. She denies all charges.
10:36am: Dr David Harkness, who was a registrar at the Countess of Chester Hospital in 2015, is due to give evidence this morning. Will focus on the events of 21 September 2015. On that morning Child G had a second incident of projectile vomiting and that afternoon needed resuscitation
10:40am: Dr Harkness tells the court he was on a day shift on 21 September. He says he cannot remember, aside from using his notes, the events of that day
10:43am: Court is being shown notes from that day, which show there were seven attempts to cannulate Child G. Dr Harkness' colleague Dr John Gibbs told the court yesterday that in babies, such as Child G, that require a lot of intensive care there can be issues with cannulation
10:45am: Dr Harkness is recalling the cannulation of Child G at around 15:30 BST that day...he says he was assisting Dr Gibbs. He said he was there to pass equipment and keep baby still - jobs normally carried out by a nurse. Asked why a nurse did not assist, he said 'I expect nurses were very busy, but can't be specific why'
10:49am: Dr Harkness is now being asked if he remembers whether Child G was hooked up to a monitor. He says she was. He is asked if the sensor from the monitor was moved while attempting cannulation. He cannot remember
10:51am: He is asked if a sensor would ever be moved, he said it 'would occasionally be moved from one to limb to other'. He agrees it is important to keep a monitor on and attached. He says it is 'not safe' to turn such a monitor off Asked if he turned Child G's monitor off, he says 'I'm even sure I know how to turn off that particular monitor…at no point would I have turned it off'
10:55am: After the cannulation, Dr Harkness is asked whether he remembers having any conversations with anyone. He says he has a 'vague' recollection of speaking to a member of nursing staff
11:03am: Ben Myers KC, defending, put it to Dr Harkness that he and Dr Gibbs left Child G behind a screen, detached from the monitor, and had failed to inform nursing staff. Dr Harkness repeatedly says he 'can't remember'. On the monitor being switched off, he flatly says 'no' On the accusation he did not inform nursing staff and left Child G unattended, he said 'I don’t think so, it's highly unlikely'
11:04am: Yesterday a nurse, who cannot be named for legal reasons, told the court that Dr Gibbs and Dr Harkness apologised to her for not switching the monitor back on after fitting the cannula. Dr Harkness says he 'can't remember' whether such a conversation took place
11:13am: Court now taking a short break for legal discussion
12:34pm: Court back in session, judge has said it is not possible to hear any more evidence today meaning we will now adjourn for Christmas - trial will resume on 9 January
Chester Standard article 15-12-2022
A DOCTOR said he "definitely" would not have turned off a monitor while treating a baby allegedly attacked by nurse Lucy Letby, in the jury's final day of hearing the trial before the Christmas break.
Prosecutors say Letby, 32, was a "constant presence" in numerous collapses of infants at the Countess of Chester Hospital's neo-natal unit.
She denies being responsible for murdering seven babies and attempting to murder 10 others between June 2015 and June 2016.
Letby is said to have made three attempts to murder a baby girl, referred to as Child G, in September 2015.
The final alleged bid took place shortly after a consultant paediatrician fitted an intravenous cannula to Child G with the assistance of a registrar.
Manchester Crown Court has heard Child G was behind a privacy screen and unattached to an oxygen monitor when a nurse responded to a call for help from the defendant.
The colleague, who cannot be identified for legal reasons, said she saw a "concerned" Letby trying to revive the youngster who had stopped breathing.
It is alleged Letby deliberately turned off the monitor but jurors heard the nurse told police last month she believed that was not the case after she recalled a conversation she had with two doctors.
She said consultant Dr John Gibbs and registrar Dr David Harkness apologised to her for leaving Child G behind the screen and for not turning the monitor back on after completing the procedure.
Dr Gibbs said he could not remember whether Child G's monitoring equipment was switched off during a seventh attempt that day by medical staff to insert a cannula.
But he told the court that if the nurse said he had apologised for leaving the monitor off then "presumably that happened".
On Thursday, Philip Astbury, prosecuting, asked Dr Harkness: "Do you have any recollection of switching the monitor or alarm on and off at any stage?"
Dr Harkness said: "Definitely would not have turned it off.
"It's not safe. In fact I'm not sure I know how to turn off that particular monitor. At no point did I turn that monitor off."
Dr Harkness said he could not recall the exchange with the nurse.
Ben Myers KC, defending, said: "You must know very well Dr Harkness that conversation took place?"
Dr Harkness said: "I can't remember."
Mr Myers said: "I suggest a detail like that is something you would not forget?"
The doctor replied: "I disagree."
Letby, originally from Hereford, was remanded in custody and the trial is scheduled to resume on Monday, January 9.
Court Adjourned from Friday 16th December 2022 until Monday 9th January 2023
Monday 9th January until Wednesday 18th January 2023 - no court (jurors absent/ill)
Chester Standard article 16-01-2023
THE trial of Lucy Letby, who denies murdering seven babies at the Countess of Chester Hospital neonatal unit and attempting to murder 10 more, has been further delayed.
Last week the trial of the 33-year-old former neonatal unit nurse was due to resume at Manchester Crown Court following the scheduled break for the Christmas and New Year holidays.
But two members of the 12-strong jury were absent last week.
The trial judge, Mr Justice James Goss, informed the jurors present there were "very good reasons" why the two jurors were absent, but it meant that no evidence could be heard on the day.
It had been hoped the trial could resume today (Monday, January 16), but a further juror illness has meant that has not been possible, as all jurors are required to be present for every day the trial hears evidence.
It is not yet known when the trial will be able to resume, having last heard evidence over a month ago on December 15.
Last week, the court also heard the trial is now likely to continue until "sometime in May". Jurors had previously been told the trial was likely to last until the Easter break.
As a result, members of the jury have now been urged not to book any holidays in the immediate weeks following the Easter break.
It is planned for the trial, once resumed, to continue throughout the upcoming months, pausing only for the Easter break between April 6 and April 17, and thereafter only breaking for statutory public holidays, such as the May bank holiday.
The judge told the jury the prosecution was not yet halfway through its case, with evidence having most recently been heard for the seventh child, chronologically in the case, out of 17.
Members of the jury were also reminded not to conduct their own research or discuss the case, and will only be allowed to discuss the case with each other as a full group when they retire to consider their verdict.
A court order bans the reporting of the identities of the children allegedly attacked by Letby, while identifying parents or witnesses connected with the children is also banned.
Letby, originally from Hereford, remains in custody.
Wednesday 18th January 2023
Child G
Dr Dewi Evans - Dr Sandie Bohin - Summary of police interviews
Child H
Parents' statements - Police analyst: Recorded events & messagesChester Standard Live Reporting
9:09am: The last day evidence was heard in the trial was December 15, 2022. Since then, there has been a break for Christmas and New Year, which was expected. However, juror absences in the past week meant the resumption of the trial had been delayed. All 12 members of the jury are required to be present in court for the trial to continue. It is understood that the jury, collectively, is now in a position to attend.
10:23am: The courtroom at Manchester Crown Court is now filling up with lawyers, reporters, court staff and members of the pubic gallery.
10:30am: Lucy Letby has now also appeared in court.
10:31am: The judge, Mr Justice James Goss, has also now entered the court. The trial will now be resuming.
10:35am: Nicholas Johnson KC reminds members of the jury where the case is up to in terms of the prosecution evidence. The case surrounds the events of Child G, where there are three counts of attempted murder. The first count, dated September 7, 2015, has been dealt with. The prosecution case is dealing with the other two counts of attempted murder on September 21, 2015. It is the prosecution's case that Lucy Letby attempted to murder the baby girl, who cannot be named. The defence deny this was the case.
10:38am: Independent medical expert Dr Dewi Evans, who has given evidence previously, has been recalled to provide evidence in relation to Child G, for one of the two September 21, 2015 events, when Child G vomited and desaturated.
10:42am: The court is reminded that Child G was born on May 31, 2015, at Arrowe Park Hospital at a gestational age of 23 weeks and six days - the most premature birth of any baby involved in this case. She was transferred to the Countess of Chester Hospital on August 13, 2015. Previously the court heard Child G had an incident of projectile vomiting on September 7, and was transferred to Arrowe Park Hospital the following day. She returned to the Countess hospital's neonatal unit on September 16, with the next incident happening on September 21. Dr Evans is now explaining what he observed for the morning of September 21. He said the vomiting was "extremely worrying" and came with concern of the "life-threatening" desaturation levels.
10:46am: The court is shown Lucy Letby's nursing note from that morning 'At 10.15 x2 large projectile milky vomits, brief self resolving apnoea and desaturation to 35% with colour loss. NG tube aspirated'. Letby had given Child G a feed at 9am, the note recorded. The note also adds Child G's abdomen was 'soft' and 'distended'. A doctor's note for the incident records Child G 'was apnoeic for 6-10 seconds, went blue, sats down to 30%. Last feed 9am'. Dr Evans confirms he has seen these notes.
10:50am: Dr Evans said an important feature was the abdomen was larger and distended. He says that could be due to an abdomen full of milk, full of air, or a combination. He says that is despite the vomiting which would mean the contents of the stomach "This is a very significant, concerning issue", he adds, in combination with Child G's oxygen saturation levels dropping. Dr Evans said there was "one explanation", which was that Child G had been given "far more milk via the nasogastric feed". Child G had been tolerating 40mls of milk, which would not explain "two large projectile vomits" plus "30mls of milk left in her stomach". Dr Evans says Child G received "lots more milk" which had resulted in the episode. He says it could have been milk, could have been air, or a combination of the two, but difficult to say what levels of each would have been administered.
10:53am: Ben Myers KC, for Letby's defence, is now asking Dr Evans questions about the September 21, 2015 incident. He says one of Dr Evans' earlier reports said there had not been evidence of a life-threatening event for September 21. Dr Evans said he "overlooked" it when looking through 4,000+ pages of evidence, which had included these nursing notes.
10:58am: Mr Myers is now asking about a nursing note by nurse Melanie Taylor on September 30, 2015, which Dr Evans identified. The note includes Child G had desaturations, with 'one profound desat/apnoea requiring position changed and oxygen this morning'. Dr Evans had recorded the observations required further looking at. Mr Myers returns to the September 21 incident, and says the 'projectile vomiting' is a cause for concern that Dr Evans identified. Mr Myers says the incident does not record the amount of vomit, or how far it travelled (unlike the September 7 incident). Dr Evans said it was not a 'self-resolving' incident, and it was significant that Child G vomited twice, and stopped breathing. He said it was "a serious event", but not as serious as the one on September 7, 2015. Mr Myers says the incident was "brief".
11:04am: The court is shown a note from Dr Peter Fielding from September 21, 2015, in which the bowels were open and the stools were 'loose and green'. Mr Myers asks if this is a sign of Child G's overall poor health. Dr Evans says loose stools would be common in babies. Mr Myers asks if there was a more marked history of Child G vomiting upon her return from Arrowe Park in September 16, 2015. Dr Evans said the events of September 7 left her a "significantly changed baby", and agrees vomiting was more likely. Child G was then receiving feeding by tube.
11:05am: Mr Myers says there are "numerous" occasions of Child G vomiting from September 16, and the incident on September 21 followed a pattern. Dr Evans says he agrees due to "basic arithmetic", in that Child G still had 30mls of milk in the stomach after a 40mls milk feed and "two projectile vomits".
11:07am: Mr Myers says "we don't know" how much milk came up in those vomits. Dr Evans says the nursing notes are "pretty descriptive", and "no nurse" would describe two vomits as "5ml each", as that would amount to "a teaspoon each". It "had to be" more than 40mls milk feed at 9am, which would "also explain" the distended abdomen.
11:09am: The judge asks if there are any other entries of "projectile vomiting" recorded for Child G in the notes. Dr Evans says there is not.
11:12am: Dr Sandie Bohin is now being recalled to give evidence, for the case of Child G. Dr Bohin says Child G had been "tolerating well" up to September 21, and had "two large projectile vomits" after being given a 9am feed while asleep.
11:15am: Nicholas Johnson KC says Dr Bohin refers to a 6am, 45mls bottle feed of milk, and Lucy Letby records a 40mls nasogastric tube feed of milk at 9am. Following the two large projectile vomits, 30mls of milk was aspirated from Child G. Dr Bohin says the event "just didn't add up" from the 40mls feed. She says the two projectile vomits would have been "more than a mouthful of milk" of 5-10mls each, and "basic arithmetic" meant that more than 40mls of milk would have been administered at 9am.
11:19am: Mr Myers KC is now asking questions. He asks Dr Bohin "we don't know" how much milk there was in Child G's stomach prior to the 9am feed. Dr Bohin says that is the case, but Child G had been tolerating feeds well. Dr Bohin says there is a difference between a posit (small vomit), a medium vomit and a large vomit. Mr Myers says "we don't have the basic figures, do we?" Dr Bohin says "we don't", but there are descriptions which nurses use to outline the quantities of vomit. Mr Myers says the incident was not on the same level of the September 7 incident. Dr Bohin disagrees, saying the incident was still serious. She agrees it "was not the same scale", as the events were "almost identical", even if the "repercussions" of what followed were not as serious as that on September 7.
11:25am: Dr Bohin agrees that "vomiting became much more of a feature" for Child G upon her return from Arrowe Park Hospital, but says there were only records of projectile vomiting on September 7 and September 21. Mr Myers says from October 3-8, 2015, Dr Bohin had recorded Child G had '1-2 vomits each day, vary from small to large, and some after a nappy change'. A nursing note from October 8, shown to the court, records 'two large vomits' for Child G, and the feeding regime was changed as a result. On October 9, another nursing note records 'tolerating 3x8 [three feeds, eight hours apart] feeds well...x2 large digested milky vomits'. That is followed by another 'large vomit' on October 9. Dr Bohin says the difference with these vomits is they are not projectile vomiting and did not cause Child G "to be medically compromised".
11:30am: Mr Myers refers to an incident of "projectile and quite large in size" vomiting for Child G on October 15, 2015. Dr Bohin says he has looked through many documents and charts in this case, and may have overlooked that one incident of projectile vomiting. Mr Myers refers to other 'large vomits' on October 17 and October 22, the latter 'with wind following feed'. He refers to Child G's father's statement in which he said since September 7, he had seen Child G projectile vomit and covered the cot. Dr Bohin says "with the greatest of respect", parents can refer to "projectile vomiting" when they mean "vomiting".
11:37am: Nicholas Johnson KC is now relaying Letby's interviews with police. Letby recalls Child G and could not remember why she had taken over care of her. She said "sometimes babies vomit, but not very often is it a projectile vomit". She said she was not involved in Child G's feed. She recalled she may have gone over to Child G when she heard vomiting.
She was asked about the significance of the air in the NGT. She says sometimes air is taken in when babies vomit. She said she was not sure of the cause of the air in Child G's abdomen. She was asked about the "profound desaturation" on September 7, 2015. She could not clearly recall who was there at the time, or where she was at the time. For September 21, 2015, Letby had a "vague recollection" of the shift. She said it was a "busy shift" and she was "looking after other babies as well" at that time. She said there had been "no issue" with the 9am feed, and could not clearly recall the vomit at 10.15am. She was later re-interviewed. For September 7, Letby could not recall any concerns with Child G prior to the event. She said there were two possibilities - that Child G had received more than 45mls of milk, or there was undigested milk in the stomach. She denied force-feeding milk or administering air to Child G. For September 21, Letby agreed Child G's stomach would have been empty when the feed began. She denied intentionally harming the baby girl.
In the third police interview, Letby was asked again about the September 21, 2015 incident. She said she remembered going behind the screen and seeing Child G. She did not recall seeing a monitor which had been switched off. She denied switching the monitor off. She agreed it was bad practice to switch the monitor off, and "someone had made a mistake" in switching the monitor off and leaving the child behind a screen unobserved.
11:41am: That concludes the evidence for Child G. The prosecution will now begin delivering evidence for Child H. The prosecution say there are two counts of attempted murder for Child H, a baby girl born at the Countess of Chester Hospital on September 22, 2015.
11:50am: The case will resume after a short break.
11:57am: A statement from Child H's mother is being read out to the court.
12:02pm: She says Child H was born in September 2015, and had "a healthy pregnancy", the only complication being she was a type 1 diabetic. Checks were carried out, but they were primarily for the mother's benefit, not the child. She was admitted to medical care in September 2015 as her blood sugar levels kept dropping. Once there, staff talked about the possibility of inducing. She went to hospital and had the view she was not [going] to give birth for a few weeks. She was then visited by a consultant and told that, on September 22, for the birth to take place. There was a complication in that Child H would be a couple of weeks premature. There were also 'no beds available' in the neonatal unit, or in any other equivalent centres, even as far away as Birmingham. As preparations were made for the mum to give birth, a bed in the neonatal unit became available. The birth took place, and Child H was "absolutely fine" and "might not even need to go to the NNU". Both parents were allowed to hold the baby girl, but she became pale and began grunting. Child H was then taken to the NNU for oxygen as she was "struggling to breathe".
12:10pm: The mother adds Child H was put on CPAP to assist her breathing. The parents tried to go into the NNU and were informed that Child H had been placed on a ventilator. They were "quite annoyed" they had not been informed about this, and staff said they had been busy and no-one had found the time to inform them. After several x-rays, it was established Child H had suffered a suspected lung puncture. The parents remained with her, but could not pick her up.
The following morning, nursing staff said the mum had to come to the NNU "right away" and inform the father to come too. Child H was being treated, with "lots of medical" people surrounding her. They were resuscitating Child H. The mum was told to sit with Child H and hold her hand. The staff successfully brought Child H back. The staff could not explain her "cardiac collapse". Child H was then "doing really well" that day.
The parents had just gone to bed when staff knocked on the door. They said Child H was "not responding". The parents were met with an "almost identical scene" as Child H was surrounded by medical staff. "Fortunately" this collapse did not last as long. Following this, Child H was transferred to Arrowe Park Hospital on September 27. The staff there removed and replaced the ventilator. They checked Child H over and a brain scan "fortunately showed no long-term damage".
Child H "improved dramatically" as soon as she was at Arrowe Park, and within 24 hours she was off a ventilator and back on to CPAP. 24 hours later she was then taken off CPAP, and made "a dramatic improvement". She was then taken back to the Countess, and the "only difficulty" at that point was getting her to feed. Child H stayed in the NNU until October 9, when she was discharged "earlier than normal" for a baby outpatient. There had been "no long-term complications whatsoever" for Child H.
12:16pm: The father's statement is now read out to court. Child H was "quite healthy" at birth, but was "grimacing" and had complications with breathing, so was taken to the NNU. The father says he was able to see Child H soon after, and saw she was on an incubator, with breathing assistance.
He recalls being woken up on September 26 and being called to the hospital, and seeing "a lot of commotion going on". He remembers Lucy Letby being there, doing chest massaging. It was explained to the parents Child H had had "a collapse". He recalls Child H was "a very strange colour" and had "mottling running towards her fingers". A doctor explained the pressurised air in the lungs had caused a tear. The parents stayed with Child H that day, and she "remained ok that day".
He said it was after they had gone to bed that they had a knock on the door and returned to the NNU. The staff were in consultation with Arrowe Park. The father says in the early hours of September 27, Child H was transferred to Arrowe Park, where she came on in "leaps and bounds". The Arrowe Park was "a completely different setup" and staff were "more proactive", the father says. Child H returned to the Countess of Chester Hospital and "nothing else really major happened" before she was discharged.
12:19pm: Intelligence analyst Kate Tyndall has been recalled to court to talk the court through the sequence of events for Child H, presented as an electronic bundle of evidence. As before, the sequence of events features medical charts, nursing/doctors' notes, significant events, plus timestamped evidence of messages recovered from Lucy Letby's phone. The events show Child H was admitted to the neonatal unit at 6.40pm on September 22, 2015, shortly after being born.
12:27pm: Letby sends a message to a nursing colleague on September 23 informing her she's rearranging her shifts, and will be working with her. She also informs her mother she's working that night as an extra shift. She also messages another colleague to say how busy the unit is likely to be that night. The following day, Letby messages a colleague to say the "It's completely unsafe", followed by a frowning emoji. She messages a friend that work is "extra mad" so she wouldn't be able to do hula hoop [exercise]. She messages a colleague on the number of babies in the unit, in reference to how busy it was on that shift, and how she had not had chance to 'catch up on Corrie' [Coronation Street].
12:35pm: Letby is then recorded as being the designated nurse for Child H for the night of September 24-25. Dr Alison Ventress records clinical notes of a lung issue for Child H that night. X-rays at 1.40am and 2.29am on September 25 were taken. Child H was diagnosed with a punctured left lung. Dr Ravi Jayaram records a desaturation for Child H and a test was carried out for a collapsed lung.
12:36pm: Letby sent a text to a colleague at 3.07am on September 25: "Can I go now??" The colleague responds a few minutes later: "Yes. Let's run off together and rescue [colleague] too."
12:43pm: Letby's medical note for the morning of September 25 recorded the "profound desaturation" at 5am, with the fings on the right hand noted to be white, along with a white patch on the abdomen.
12:50pm: The intelligence analyst continues to talk through the sequence of events, with descriptions of the care being given to Child H throughout the day on September 25, 2015, which includes another desaturation in the afternoon. The cardiac arrest team is beeped at 4.23pm to attend the neonatal unit.
12:58pm: The sequence goes to the night shift of September 25-26, in which Lucy Letby is listed as a designated nurse in nursery room 1 for Child H. No other babies are in nursery room 1, with four babies (including Child G) in room 2, four in room 3 and four in room 4.
2:01pm: The trial is now resuming following the lunch break.
2:08pm: The sequence of events continues, with clinical/routine records relayed to the court on September 25. A blood transfusion for Child H is begun at 11.05pm. A desaturation for Child H is recorded at 11.30pm, with Letby writing the note up retrospectively at 4.14am the following day. Observations are being taken more regularly due to the blood transfusion, the court hears.
2:19pm: A morphine bolus is administered to Child H at 1.30am on September 26, and the blood transfusion is recorded by Letby as being completed at 2am. However, a separate, handwritten paper record shows the blood transfusion having been completed at 3.05am. This separate record is not signed by anyone. Letby records 'poor blood gas and 100% oxygen requirement' and a third chest drain was inserted around this time, the court hears. Dr John Gibbs records this as being about 2.15am, as the chest x-ray showed a re-accumulation of Child H's left-sided pneumothorax (ie a collapsed lung). A further, third chest drain was inserted to relieve the pressure.
2:24pm: At 3.22am, Child H suffered a 'profound desaturation and colour loss to 30%'. Letby records: 'Good chest movement and air entry, colour change on CO2 detector. Neopuff commenced in 100% oxygen and help requested.' An intensive care chart for Child H on September 26 records 'blood complete 0324 - RESUS'. The record is initialled by Lucy Letby. Dr Alison Ventress confirms in a clinical record she was crash called at 3.24am as Child H "had desat requiring bagging...Sats 60s then heart rate down to less than 100 so nurses crash called, wasn't being handled at all, no trigger identified.' Upon her arrival, Child H was 'being bagged via ETT, good chest movement, capnograph positive, sats 60%, heart rate 70 down to 50'. A test for a collapsed lung was carried out and air was removed.
2:31pm: Dr John Gibbs, consultant paediatrician, records he was called from home at 3.30am and arrived at the neonatal unit at 3.36am. He saw 'CPR in progress', and Child H had no pulse when chest compressions stopped. The sequence of events details the series of medications administered to Child H. Lucy Letby's note records, for 3.46am, 'x3 doses adrenaline and x1 dose atropine given...chest compressions stopped at 0346, heart rate 180, saturations >90, placed back on to a ventilator, 30% oxygen'.
2:34pm: Letby recorded, for the Child H event at 3.22am, 'profound desaturation and colour loss to 30%, good chest movement and air entry, colour change on CO2 detector, Neopuff commenced in 100% oxygen and help requested. Serous fluid +++ from all 3 drains, became bradycardic. Drs crash called and resus commenced as documented'.
2:37pm: Letby records a Child H family communication at 4.28am: 'Parents visiting at start of shift. Updated on condition and advised to try and rest overnight. Midwife contacted during resus to [help take mum to the unit].' A follow-up note said parents were concerned about the possibility of brain damage, and Child H remained poorly and could relapse. Dr John Gibbs offered a blessing to be administered and the parents accepted the offer. Child H was then blessed with parents and family members present.
2:39pm: Letby recorded 'good blood gas at 0700 - ventilation reduced to 22/4, and rate reduced...in 26% oxygen. [Child H] appears settled.'
2:54pm: A series of messages recovered from Letby's phone, of messages sent to and from her phone at around 9am on September 26, are shown to the court. They include Letby's colleague Yvonne Griffiths commending Letby for "all your hard work these last few nights". She says Letby "composed" herself "very well during a stressful situation" and it was "nice to see" her "confidence grow" as she advanced throughout her career. Letby shows this message to a colleague and asks her how she should reply. Her colleague expresses surprise. A series of messages are exchanged between Letby and the colleague acknowledging there had previously been "bitchiness" among staff and there had been "comments" about Letby regarding her role which Letby had found "upsetting".
2:56pm: Medical notes record Child H's parents were present as treatment continued for the baby girl, with further medication administered during the day of September 26.
3:11pm: The trial is now resuming following a short break. Intelligence analyst Kate Tyndall is continuing to talk through the sequence of events, which had reached the night shift of September 26-27, 2015.
3:14pm: At this point, Child H was the only baby in room one of the neonatal unit, and for this night shift (September 26-27), Letby was the designated nurse for two babies in room two.
3:19pm: There is a further, profound desaturation for Child H, with a crash call made at 8.49pm. Dr Matthew Neame recorded attending to the neonatal unit. Letby, on shift, messages a colleague at 9.31pm to give an update on Child H's progress throughout the day. She messages colleague Alison Ventress a couple of moments later to say Child H 'had a stable day', and took out the original drain at 8pm, adding 'just blocked tube, lots of secretions!'.
3:22pm: Letby messages her colleague, for Child H, 'I've been helping Shelley [Tomlins, designated nurse for Child H that night] so least still involved but haven't got the responsibility'. Colleague Alison Ventress messaged Letby: "Never known a baby block tubes so often!! Glad she's had a stable day..."
3:26pm: Letby messages a colleague just before 11pm, lamenting that she had forgotten to record Strictly that night, and BBC iPlayer doesn't work on her iPad. Letby then is recorded as being on Facebook at 12.45am and 12.46am, liking a post and photo. Child H then has a 'profound desaturation' timed at 12.55am. Nurse Shelley Tomlins recorded: 'profound desaturation to 40% despite equal bilateral entry and positive capnography'.
3:31pm: Staff were crash called to the neonatal unit room 1. Dr Matthew Neame reintubated Child H and chest compressions were started at 1.07am. Child H's heart rate dropped to 40bpm. Adrenaline was administered. Chest compressions were discontinued at 1.13am. A request was made to transfer Child H to Arrowe Park Hospital. "No explanation" could be found for why Child H had had such a profound desaturation, the court hears.
3:37pm: Child H had a further desaturation at 3.30am, and medication was administered. The transport team arrived at 4.10am and Child H was handed to the transport incubator at 4.45am and the handover was completed at 5.20am. Child H was cared for at Arrowe Park Hospital between 6.10am on September 27 to 11.30am on September 30.
3:49pm: Child H returned to the Countess at 12.15pm on September 30, and was discharged on 5.05pm on October 9, 2015.
3:51pm: Further messages found on Letby's phone from that morning are relayed to the court. Letby informed two colleagues what had happened to Child H that night. Colleague Alison Ventress replied: "Think of all the babies you have saved and have gone home happily."
3:53pm: On October 5, 2015, Letby searched on Facebook for the mother of Child H, as well as two other parents involved in the case, in the space of three minutes at 1.15am.
3:57pm: A corrected slide from the sequence of events is now shown to the court, showing that for the September 26-27 night shift, Shelley Tomlins was the designated nurse for Child H in room 1 - the only baby in that room that night. Lucy Letby was a designated nurse for two babies in room 2, with another nurse, Christopher Booth, looking after Child G in room 2. Four babies, including Child I, were being looked after in room 3, and four babies were being looked after in room 4.
4:02pm: Intelligence analyst Claire Hocknell has been recalled to talk the court through the neonatal review schedule for Child H.
Thursday 19th January 2023
Child H
Statement of Midwife Deborah Moore - Unnamed nurse - Dr Ventress10:20am: I'm back at Manchester Crown Court for the trial of nurse Lucy Letby. We'll be continuing to hear evidence in relation to Child H. The prosecution allege Ms Letby tried to murder the infant on two occasions in September 2015.
10:22am: There'll be a slight delay to proceedings this morning as judges/lawyers are attending a eulogy at 10.30am for a former Manchester Crown barrister who recently died.
10:39am: Prosecutor Nick Johnson is reading a statement (which is agreed evidence) from Countess of Chester Hospital midwife Deborah Moore. She took Child H's mother to theatre for her emergency C-section
10:41am: Ms Moore says from reviewing her notes it was an 'uneventful birth and the mother did not require any additional treatment'
10:56am: Mr Johnson, prosecuting, is continuing to read statements of agreed evidence from medics working on the evening of Child H's first collapse
11:00am: A member of nursing staff, who can't be named for legal reasons, recalls apologising to the parents of Child H for not informing theme sooner of their daughter's condition. Child H's mother said yesterday, in a statement, that she and the child's father were "quite annoyed" they had not been informed their daughter's first collapse and said it was a "shock" to see their daughter on a ventilator The nurse's statement, read to court, said: "We always try to inform the parents as soon as possible, but not if this is going to comprise health of the baby, if we felt the baby was going to die, parents would be informed right away – never felt the case with (Child H)'
11:16am: Dr Alison Ventress is now in the witness box. She tells the court she will always remember Child H as she was the first baby she performed a pneumothorax aspiration on (needle in the chest to remove air)
11:19am: Dr Ventress is taking the court back over her notes from the morning September 24 2015. Child H had poor blood gas and had a profound desaturation down to 'the 50%s and needed bagging with neopuff'
11:21am: The baby girl slowly recovered and was placed on Bipap (a small machine that pushes air through a mask and into child's airway and lungs), the court is told
11:30am: Her notes from that morning state that Child H's breathing 'remained gasping pattern'. Dr Ventress says this is 'more serious than grunting' and agrees that it was 'indicative of a serious respiratory problem'
11:41am: Notes from the early hours of 25 September show another desaturation. At 1:14am Dr Ventress was 'bleeped urgently' as Child H had 'poor chest movement and poor colour'. She was placed on neopuff The medic noted that Child H's chest drain, which had been fitted as she had a collapsed lung, was 'no longer functioning….blood stained fluid leaking from drain'
11:45am: Dr Ventress says that is 'not uncommon' with chest drains. She says fluid was not indicative of any infection
11:50am: Her notes show that at 1.25am Child H had another profound desaturation. Oxygen levels down to 30s. Dr Ventress performed an emergency pneumothorax aspiration, 70ml of air was aspirated which was 'quite a lot for a baby that size' she tells the court
11:53am: Child H's sats improved after the procedure, but there was a further desaturation at 1.45am. Second aspiration was then needed and another butterfly needle inserted into lower chest, this again worked and drained a further 60mls of air - again sats improved
12:00pm: The baby girl's sats remained in the stable range until 3am when she had another profound desaturation, her blood oxygen fell to 26%. 85mls of air aspirated and her sats again improved. A plan was drawn up to insert a further chest drain
12:16pm: We're now looking at Dr Ventress' notes from her next shift on 25 September (going into 26 September). She records at 23.50 that there had been 'several episodes of desaturation in the previous two hours'
12:26pm: At around 1am on 26 September Child H's ventilation had to be increased, Dr Ventress again suspected a pneumothorax. She called a consultant for further advice
12:38pm: We're now looking at Dr Ventress notes from 03:22 when Child H suffered a profound collapse which needed a full resuscitation. CPR was commenced at 03.26 and three doses of adrenaline were administered between 03.30 and 03.39
12:40pm: At 03.46 chest compressions were stopped as Child H's heart rate had improved and her colour started improving - treatment was successful
12:51pm: Ben Myers KC, defending, is now questioning Dr Ventress. The medic agrees that desaturations in babies like Child H are not 'uncommon'. She agrees that Child H was 'clearly unwell'
12:53pm: Mr Myers sets out that Child H had had three chest drains inserted and numerous desaturations in the run up to 26 September, Dr Ventress agrees. He asks whether those medical procedures are 'likely to put strain on a little body like hers', she agrees Mr Myers asks if it is possible the cumulative impact of those procedures could have resulted in a collapse like the one observed on 26 September, she agrees
2:06pm: A former nursing colleague of Ms Letby, who cannot be named for legal reasons, is now in the witness box. She is taking the court through her notes on Child H from 25 September 2015
3:10pm: Another former nursing colleague of Ms Letby, who cannot be named for legal reasons, is now in the witness box. She is taking the court through her notes on Child H from 23/24/25 September 2015
3:27pm: Asked for her recollections of the events of 26 September, the nurse said she remembers Child H 'became unwell that night and needed some resuscitation'
3:29pm: The nurse is asked about 'a difference of opinion' that occurred that night over whether a baptism should be offered for Child H after her collapse. The baptism was offered to the parents, which was accepted The nurse and a senior manager disagreed over whether it was the appropriate time for it to be offered
3:30pm: This disagreement arose mainly due to the fact it was early hours of the morning and the unit was busy. The nurse said it shouldn't be 'blown out of proportion'
4:01pm: Court now adjourned, back tomorrow.
Chester Standard article 19-01-2023
MEDICS could find no reason why a baby suddenly collapsed during a night shift at the Countess of Chester Hospital, the trial of nurse Lucy Letby heard.
It is alleged the defendant, 33, attempted to murder the premature-born girl on successive shifts in the early hours of September 26 and 27, 2015.
Child H, who cannot be identified for legal reasons, needed full resuscitation from both incidents at the hospital's neo-natal unit before she recovered.
Giving evidence at Manchester Crown Court on Thursday, January 19, registrar Dr Alison Ventress said she received an urgent bleep call from nurses in the early hours of September 25.
She said she was informed Child H had breathing difficulties, poor chest movement and poor colour.
Child H's oxygen levels plummeted shortly after her arrival and she called for a consultant to assist, Dr Ventress told the court.
More desaturations followed as Child H received a series of invasive needle treatments for a tension pneumothorax – an emergency situation where air accumulates between the chest wall and lung which causes it to collapse.
Dr Ventress agreed with Simon Driver, prosecuting, that it had been a "rocky night" for Child H.
Mr Driver asked: "Were the causes for those problems identified?"
Dr Ventress replied: "Yes, a tension pneumothorax is something that does happen. You never find an exact cause but for a premature baby needing breathing support it is a known complication of that."
On the following night shift, she noted a "cluster" of desaturations in a two-hour period.
She said she later found a chest drain – a tube inserted to drain air – was in a sub-optimal position and it had "almost fallen out".
Dr Ventress noted at 1am on September 26 that a combination of Child H needing more respiratory support and a drop in her blood pressure led her to think she may have another tension pneumothorax.
At 3.24am, she received a crash call from the nurses in the neo-natal unit, the court heard.
Child H had desaturated to a "level of real concern", she said, and her heart rate had fallen below 100 beats per minute.
She said she was informed that "no trigger was identified".
Chest compressions commenced at 3.26am when her oxygen levels and heart rate continued to drop, the court was told.
Child H was given several doses of adrenaline before compressions stopped at 3.46am when her heart rate rose to a safe level.
Dr Ventress said: "We followed the cardiac arrest protocol and she recovered, but we never found a reason why she got into that state."
The court heard that three chest drains were put into Child H over several days before her first sudden collapse.
Benjamin Myers KC, defending, asked Dr Ventress: "Do you agree there are numerous reasons why a baby on a chest drain may desaturate?"
"Yes," said the doctor.
Mr Myers said: "If we look at the days leading up to the event on September 26, over those days there have been multiple desaturations with this little girl."
Dr Ventress said: "Yes."
Mr Myers went on: "Indeed in the hours leading up the event we are looking at, there was a series of desaturations over the night, weren't they?"
"Yes," repeated Dr Ventress.
She also agreed Child H had been suffering for a prolonged period of time from tension pneumothorax and "the reality is she had been through an awful lot of medical activity".
Dr Ventress conceded it was "conceivable" that babies under that much intervention could suffer "quite a significant collapse".
Mr Driver asked the witness: "You confirmed desaturations are not uncommon with babies experiencing the sort of problems Child H was experiencing. Are arrests as common as desaturations?"
Dr Ventress said: "No. Arrests are not all that common. I'm not saying they are impossible, but they are not all that common."
Child H was discharged in October 2015 after she continued to improve.
The court heard that 13 children were in the unit in the early hours of September 26, with four nurses allocated to their care.
Letby was tasked with looking after a sole baby, Child H, in intensive care nursery room 1.
The evening's nursing shift leader, who cannot be identified for legal reasons, agreed with Mr Myers that caring one-to-one for a baby such as Child H was "potentially quite a demanding job" for a nurse of Letby's experience.
But she added: "Lucy was qualified in specialist neo-natal nursing at this time and very competent. She was not a totally inexperienced nurse … and I would trust that she would ask me if she had any problems."
Mr Myers asked the witness: "Was there an issue with Lucy Letby being relatively junior compared to others and some debate about her going into Nursery One to look after more poorly babies?"
"Sometimes, yes," she replied.
Mr Myers said: "And sometimes a bit of an under-the-surface dispute about that, is that correct?"
The witness said: "Yes."
Letby, originally from Hereford, denies murdering seven babies and attempting to murder 10 others on the unit between June 2015 and June 2016.
Friday 20th January 2023
Child H
Dr Ravi Jayaram - Dr John Gibbs10:26am: I'm back at Manchester Crown Court for the murder trial of nurse Lucy Letby. We'll be continuing to hear evidence in relation to two collapses of a baby, referred to as Child H, at the Countess of Chester Hospital in September 2015.
10:37am: Court now sitting. Jury had made a request for notepads, Judge Goss tells them there is none in the building. 'I don't know if you know much about government procurement, but it's not as simple as going the stationary and buying it', he says
10:42am: Consultant paediatrician Dr Ravi Jayaram is now in the witness box, he is recalling the events of 26 September 2015. Dr Jayaram was called by junior colleague Dr Alison Ventress in the early hours as medics were having trouble with Child H
10:45am: Child H needed a numerous procedures to drain air from her chest as she had suffered pneumothorax, this is where air leaks into the space between your lung and chest wall. Dr Jayaram is explaining this condition and how it is diagnosed/treated
10:55am: Jury are being shown X-rays of Child H, which show excess air in the chest cavity. Child H had a chest drain and two needles (to drain air) in a bid to treat this
11:02am: Dr Jayaram is currently describing in detail the process of inserting a chest drain
11:07am: X-rays taken in the early hours of the morning of 25 September 2015 show that Child H's lung had re-inflated after the procedures. Lots of the black (air) present on previous X-rays in the chest area had disappeared
11:15am: Ben Myers KC, defending, is now questioning the consultant. He asks whether the act of fitting a chest drain can cause stress to a baby, he says it ‘can raise heart rate’
11:18am: Mr Myers is asking whether a drain could come into contact with internal structures like the heart, Dr Jayaram says he has 'never seen that happen' - he says anatomical he can't see it, as the heart is surrounded by the lungs and the lungs would have to be punctured
11:21am: Mr Myers puts it to Dr Jayaram, that due to improvements in medicine, pneumothorax is less common. He says 'generally speaking doctors now are likely to have less practice on chest drains', Dr Jayaram says he 'wouldn’t disagree with that' He says that is why such treatments are more often carried out by consultants, as they're from a generation when they were more common
11:27am: Mr Myers is asking Dr Jayaram where the optimum space is to insert a chest drain, he puts it to the consultant that the fifth intercostal space is the best area and is standard. Dr Jayaram says 'it doesn’t matter…as long as it is in, it is going to drain air'
11:28am: Dr Jayaram eventually agrees that 'ideally' the fifth intercostal space is where a drain would be fitted
11:37am: Discussion in court is currently centring on the use of different drains - a pig tail train and a straight drain. Child H has a pig tail drain fitted first, by Dr Ventress and then Dr Jayaram fitted a straight drain a short time later. Dr Jayaram concedes that it would have been easier to fit a second pig tail drain, but there were none available
11:38am: Mr Myers shows the jury an X-ray of the two drains in Child H. The first as established was in the 'ideal' fifth intercostal space. The second fitted by Dr Jayaram, is not in the fifth intercostal space (his notes written at the time say it is)
11:40am: Dr Jayaram agrees it is 'clearly' not in there but says the drain is still in a 'good position'. He says it is in the plural cavity and that it is working
11:43am: Mr Myers is repeatedly putting it to the consultant that the chest drain is in the wrong place. 'No it’s in the plural cavity, you’re focused on process rather than outcome. It needed to be put in. It isn’t going to have any great effect on heart function'
11:48am: Mr Myers puts it to the medic that the tip of a drain that close to the heart could cause bradycardia if it moves, 'it could' Dr Jayaram says Mr Myers says if the baby moves, is handled, when it breaths - can all cause the drain to move. Dr Jayaram agrees, but disputes the inference of the questions. He says any movement would be minimal
11:53am: Mr Myers puts it to Dr Jayaram that he inserted the chest drain in a sub-optimal position and that this contributed to Child H's desaturations in the hours and days that followed. The consultant rejects this, he says the drain was not in the wrong place He accuses Mr Myers of being focused on process over outcomes, he says the drain was inserted to drain air which it did.
12:08pm: Dr John Gibbs, who was a consultant paediatrician at the Countess of Chester in 2015, is now in the witness box
12:29pm: Dr Gibbs' notes from around 5pm on 25 September show that the drain inserted by Dr Jayaram that morning had moved. Dr Gibbs fixed the drain more securely to stop it moving any further
12:31pm: Dr Gibbs is asked if there's any consequence to the drain moving, he says: 'The main worry is it moving out completely and falling out and being useless'
12:32pm: Asked if there would be any internal consequence, Dr Gibbs says: 'Not that I’m aware of…you wouldn’t want to keep pulling and pushing, that would be rubbing against the lung. Pushing very far in would push against the heart… 'I wouldn’t expect it to cause any trauma or damage to (Child H)at all', he said
12:52pm: Dr Gibbs is now taking the court back over his notes from the early hours of 26 September, when Child H suffered a serious collapse which required CPR and three doses of adrenaline
1:04pm: Dr Gibbs' notes from the time say that it was 'unclear' why the infant went into cardiac arrest. His notes say the likely cause was hypoxia - low oxygen levels - but not clear what had caused that
2:29pm: Ms Letby's defence counsel, Mr Myers is now questioning Dr Gibbs
2:53pm: Mr Myers puts it to Dr Gibbs that against the backdrop of all Child H had been through - the insertion of multiple chest drains - it was 'no surprise' she had a collapse on 26 September. Dr Gibbs says he 'was surprised' by her collapse as she had been stable
3:11pm: The judge has asked Mr Myers to clarify whether he is suggesting Child H's collapse came as a consequence of the procedures (chest drains/intubations etc), he says yes He says, with particular reference to the drain fitted by Dr Jayaram, that he wants the jury to look 'where it goes and what it could have done'
3:22pm: Court has now adjourned, back Monday.
Chester Standard article 20-01-2023
GIVING adrenaline to help revive babies in cardiac arrest was "uncommon" until 2015 when a series of repeated collapses began, the trial of a nurse has heard.
Lucy Letby, 33, denies going on a killing spree at the Countess of Chester's neonatal unit between June 2015 and June 2016 when she allegedly murdered seven babies and attempted to murder 10 others.
Medics could find no reason why one of those infants, Child H, suddenly collapsed in the early hours of September 26, 2015, Manchester Crown Court was told on Friday, January 20.
The baby girl, who cannot be identified for legal reasons, needed full resuscitation again the following night shift in the early hours of September 27 in similar circumstances.
Chest compressions from nursing staff were under way when consultant paediatrician Dr John Gibbs arrived to the first collapse.
Three doses of adrenaline were administered to help stimulate the heart of the youngster and her heart rate eventually rose to a safe level after 22 minutes of resuscitation.
Philip Astbury, prosecuting, asked the now retired doctor: "Was the use of adrenaline in those circumstances a commonplace occurrence?"
Dr Gibbs replied: "No. It was becoming more common as events continued on the unit with repeated collapses of babies. Until 2015, uncommon."
Earlier on the shift, Child H received emergency treatment for a tension pneumothorax where air accumulates between the chest wall and lung which causes it to collapse.
A chest drain – a tube inserted to drain air – was fitted by Dr Gibbs and was the third drain to have been fitted after a number of pneumothoraxes had been detected in the preceding days.
A number of invasive needle treatments were also required to treat the issue, while Dr Gibbs said he could not explain why pneumothoraxes had occurred on three consecutive nights.
Dr Gibbs said it was the first and only time in his career that three chest drains were needed with one patient.
The court heard that usually only "two or three" such procedures would be carried out at the unit in a whole year.
Ben Myers KC, defending, asked if it was possible that the collapse in the early hours of September 26 could be attributable to the cumulative effect of all the medical interventions on Child H.
Dr Gibbs said he did not believe that was "tenable".
He said Child H was "stable" and in a "good condition" after he inserted the third chest drain – about an hour before the sudden collapse.
Dr Gibbs said he told Child H's parents at the time she was in a "precarious" position because he did not know why her heart rate and blood pressure had plummeted.
Child H was then transferred to Wirral's Arrowe Park Hospital where she improved. She was moved back to the Countess of Chester before she was discharged the following month with no ill effects.
Dr Gibbs recalled Child H's final outpatient clinic appointment when she was aged 16 months old.
He said: "She was doing very well by that stage. Her early development was normal, which was very reassuring given all the problems she had."
Earlier another medic, consultant paediatrician Dr Ravi Jayaram, denied the defence's suggestion he had inserted Child H's second chest drain in the "wrong place".
Dr Jayaram said: "You are focusing on the process, Mr Myers, and you need to look at the outcome and we drained the pneumothorax. We succeeded and actually made (Child H) more stable."
Mr Myers has previously told the jury that Child H's collapses were the result of "suboptimal care" and had "nothing to do with Lucy Letby".
The trial continues on Monday.
Monday 23rd January 2023
Child H
Dr Matthew Neame (Registrar) - Nurse Shelley Tomlins - Nurse Christopher BoothChester Standard article 23-01-2023
A DOCTOR had "no clear explanation" why a baby girl allegedly attacked by nurse Lucy Letby suffered a second significant collapse within 24 hours, a court heard.
It is alleged Letby, 33, attempted to murder the youngster, Child H, on two occasions while on nightshift duty at the Countess of Chester Hospital's neo-natal unit.
The prosecution say she first struck in the early hours of September 26, 2015, and then again the following morning after Child H's designated nurse had temporarily left the intensive care room.
On Monday, January 23, in the 13th week of the trial before the jury, registrar Dr Matthew Neame told Manchester Crown Court about his involvement with the second incident and how he was twice summoned by nurses on the shift.
The first emergency crash bleep was received after a "profound" drop in Child H's blood oxygen levels and heart rate as medics discovered her breathing tube was blocked with secretions, the court heard.
Several hours later at 12.55am on September 27, Child H suffered more profound desaturations while on a ventilator – but this time her breathing tube contained no secretions.
Child H's heart rate plunged to 40 beats per minute at 1.07am and full resuscitation, including chest compressions and doses of adrenaline, was needed for six minutes before she recovered.
Asked how the second crash call was different, Dr Neame said: "The distinction is the lack of clear explanation for the event at this time and the fact that it has happened again in a relatively short space of time.
"Both those things would have made me more concerned about (Child H's) condition."
Dr Neame said he thought Letby was the nurse who he first spoke to upon his arrival to the second crash call.
Soon after Child H was transferred to Wirral's Arrowe Park Hospital where she "came on in leaps and bounds", said her parents, before she was discharged the following month.
In his discharge letter to Arrowe Park, Dr Neame wrote: "Thank you for accepting this baby who has had two significant episodes of bradycardia (low heart rate) requiring resuscitation, adrenaline and CPR in the last 24 hours with no clear precipitating factors.
"Her care has been complicated by the development of respiratory distress syndrome and pneumothoraces (collapsed lung) but the acute episodes with desaturation and bradycardia do not seem to be directly related to the respiratory problems."
Nurse Shelley Tomlins, Child H's designated nurse on the nightshift beginning September 26, said she would not have been in the baby's presence throughout. She said she would have been covered by a colleague while on a break or if she had popped out of the room.
She told the court: "Given that she was unwell, I don't think we would have left her in her room alone but I can't be sure."
Ms Tomlins said she she could offer no explanation why Child H's blood oxygen levels dropped at 12.55am on September 27.
She told Ben Myers KC, defending, that her recollection of Child H was that she was a "very poorly baby".
Fellow nurse Christopher Booth, who was on duty on both nightshifts, told Mr Myers that Letby had completed an overtime shift that week.
He said: "That was not unusual for her. She was very conscientious."
Mr Myers went on: "Was she someone willing to work extra or have shifts changed at short notice?"
"Yes," replied Mr Booth.
Mr Myers said: "Did you find her to be a hard worker?"
Mr Booth said: "Without doubt, yes."
Asked if Letby became upset as events involving babies continued, Mr Booth said: "Oh definitely. It was a harrowing time. We were all upset. Without doubt, Lucy as well."
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Tuesday 24th January 2023
Child H
Dr Sandie Bohin - Dr Dewi EvansMedics accidentally left a butterfly needle inside the chest of a baby who reportedly suffered two cardiac arrests after she was deliberately hurt by nurse Lucy Letby, a murder trial heard today.
They also failed to give the infant a drug to help relax her lungs, while a chest drain to withdraw air was inserted in the 'wrong' space between her ribs.
Details of the mistakes emerged at Manchester Crown Court as two paediatric experts said they could find no medical reasons for Baby H to suffer cardiac arrests on successive days in September 2015.
The prosecution alleges that Letby, 33, somehow sabotaged the infant's treatment on two separate occasions on successive night shifts in the neonatal unit of the Countess of Chester Hospital.
The prosecution alleges that Letby, 33, somehow sabotaged the infant's treatment on two separate occasions on successive night shifts
The prosecution alleges that Letby, 33, somehow sabotaged the infant's treatment on two separate occasions on successive night shifts
Baby H needed resuscitating on September 26 and 27, 2015.
Despite having no heartbeat for up to 22 minutes, Baby H survived and was transferred to a more specialist neonatal unit at Arrowe Park Hospital, Wirral. She is now aged seven with no medical issues.
The jury previously heard that Baby H was given three chest drains as medics treated her for a series of life-threatening lung collapses or pneumothoraces.
Two of these were of a so-called 'pigtail' type that curl up inside the body, and each of these had been inserted in or around the fifth space between the infant's ribs – as is recommended by medical guidelines.
TV doctor Ravi Jayaram, now the lead paediatrician at the Countess of Chester, inserted the third, straight drain much lower down in the chest, believing that was where air was still collecting.
Today Dr Sandie Bohin, one of two paediatric experts brought in by the prosecution, was questioned in detail about the drain fitted by Dr Jayaram.
Nick Johnson KC, prosecuting, asked whether the tip of the drain might have interfered with the baby's heart or vagal nerve and therefore account for her two subsequent collapses.
Having viewed a series of x-ray images shown to the jury, the paediatrician replied: 'If the tip of a drain is abutting structures in the centre of the chest, that can cause – although I've never seen it – a failing heart rate and desaturation.
'But although it had moved, it hadn't moved after the x-ray on September 26, so I don't think that drain can be the cause of the collapses. By then it had been secured'.
Cross-examined by Letby's barrister, Ben Myers KC, Dr Bohin agreed that Dr Jayaram had inserted the drain in what was technically a 'sub-optimal position'. But she added: 'He did it as a life-saving measure'.
The paediatrician agreed that there had been delays in intubating Baby H and in giving her surfactant, a protein used to help relax an infant's lungs.
The latter delay meant that when the baby was ventilated the increased air pressure needed had the effect of worsening her pneumothorax.
But again Dr Bohin insisted that staff were dealing with an emergency and that 'there was no option; it was a lifesaving measure'.
She said the butterfly needle left inside the baby's chest might have punctured lung tissue and contributed to the ongoing pneumothorax.
Mr Myers asked: 'Leaving a butterfly needle in situ is suboptimal practice, isn't it?'
Dr Bohin replied: 'Yes, because it's hazardous'.
She rejected Mr Myers' suggestion that the explanation for Baby H's two mystery collapses might have been the cumulative effect of a series of procedures she had been through.
'A baby will desaturate as the result of an event, but it's not cumulative and it certainly doesn't cause a cardiac arrest'.
Dr Bohin also rejected the barrister's suggestion that the pneumothoraces meant Baby H would have fared better if she had been moved earlier to a tertiary unit such as Arrowe Park.
'No, because they can occur spontaneously – and that would mean every baby would need to be born in a tertiary unit, which isn't practical'.
Earlier, Dr Dewi Evans, the other paediatrician called as an expert witness by the prosecution, said he believed the overall care Baby H received had saved her life.
At one point Mr Myers accused him of 'deliberately identifying positive factors and ignoring the problems to support these allegations'.
Dr Evans replied: 'No, they are a series of problems that they dealt with, and the proof is she is a well little girl now'.
He added: 'I can't explain the (two) collapses, but the fact that she recovered so well before she left for Arrowe Park is a marker of clinical wellbeing and, retrospectively, an indicator that the care she had was satisfactory'.
The trial resumes tomorrow.
Wednesday 25th January 2023
Child I
Mother’s statement - Police analyst: Recorded events & messagesChester Standard Live Reporting
10:27am: The courtroom at Manchester Crown Court is now filling up, with Lucy Letby present.
10:29am: It is expected the case will begin delivering detailed evidence in the case of Child I today. Previously, the prosecution said in their opening that Child I, a baby girl, was murdered by Letby in October 2015, on Letby's fourth attempt at trying to kill her. The defence deny this.
10:33am: The judge, Mr Justice Goss, has entered the courtroom. The trial will resume shortly.
10:36am: Nicholas Johnson KC, prosecuting, is reminding the jury of the prosecution's case for Child I, which has one count of murder. He tells the jury this case, which the prosecution says involves four attempts to murder the baby girl, will be the longest to be heard in this trial.
10:39am: Child I was born in Liverpool Women's Hospital on August 7, 2015, weighing 2lbs 2oz. She was transferred to the Countess of Chester Hospital on August 18. The prosecution say Lucy Letby attempted to kill Child I on September 30, on October 12, on October 14 and on October 22, the last date being Child I's death.
10:43am: The court is now hearing a statement from the mother of Child I, who describes her pregnancy, and found she was having a girl at a 16-week scan. She said at no time during any of the scans were there any concerns. She had "breezed through" past pregnancies, but five weeks after her last scan, her waters broke. She went to the Countess, who conducted some tests to prove her waters had broken. She was transferred to the Manchester Royal Hospital, with more blood tests conducted. She was told the baby girl would be born prior to 34 weeks and was 'safer inside' at this point. She was sent home, with advice to go to the Countess every 2-3 days for blood tests. After the first of those appointments, she was told not to leave due to the blood results. She was transferred to Liverpool Women's Hospital and was continually monitored.
10:46am: On the 7th, the mother was in labour, and needed to get to the ward. She was informed by a midwife she was not in labour, but the mother said she was in contractions. She was not happy and so spoke to another midwife at the hospital she knew. A doctor physically examined her, and she was transferred to the labour ward. The mother said she was "too scared to push", and at some point she was told the baby was in distress, so she pushed. Child I was born at 9.02pm, following an hour-long labour.
10:51am: Child I was "doing really well" when born and was brought to the mum, before going to the neonatal unit. The mother was later told that, as Child I only weighed 2lbs, staff were having difficulty 'getting lines in', requiring scans every time. The mother was later able to see Child I, who was on a ventilator. The following day, the parents saw her and she was still in an incubator, but no longer on a ventilator - she was now on CPAP. A nurse asked if the mother wanted to handle Child I, and the mother accepted, but the saturation levels dropped once the baby went out of the incubator, and the mother was told it was a 'little too soon'. Over the following days, Child I was 'doing really well', although the mother was informed it would depend whether Child I would pull through, which left her 'petrified'. However, Child I continued to do 'fine'.
10:54am: At five days old, Child I was transferred to a high dependency unit at the neonatal unit in Liverpool. The following day, the family were told Child I could go back to Chester. The mother said: "We panicked, [Liverpool] was spotless, and [Child I] was settled there. "At the same time we had heard a virus had broken out among ward 2, so we were then relieved." Child I was transferred to the Countess of Chester Hospital on August 18. At first, the mother said they had reservations about Child I's care at the CoCH as the staff didn't seem to have the time for them, as they seemed so busy.
10:59am: The mother said: "I felt that Chester and Liverpool had different methods (Chester concentrated on feeding, helping babies grow, Liverpool concentrated on getting babies off oxygen support). All the time, the nurses would explain why they were doing this." Child I was on CPAP, but the mother said the mask was too big for her, and cotton pads were used to fill the gap, and this left marks on her, which left the mother "annoyed". Child I was moved to room 2 at the neonatal unit, where the mother met the mother of another baby [Child G]. She was very annoyed at a nurse who appeared to have a cold, which she had had for 'days' and even doctors were aware of, and was in the room. The mother said she did not want her baby to get an infection.
11:02am: The mother was at home when she received a call about Child I deteriorating in health, and she was transferred to Liverpool. Staff at the Countess suspected Child I had NEC as her stomach had swelled. She was transferred to Liverpool Women's so she would be close to Alder Hey, if surgery was required. When the parents arrived, they were informed Child I did not have NEC, and she improved. The mother was 'not happy' that no test was taken to categorically rule out NEC as that could have informed her future care. Child I was transferred back to the Countess. The constant stays in hospital were 'beginning to take a toll' on the parents, so they split their time at the hospital.
11:04am: The mother says she was changing Child I's nappy and was told by Lucy Letby that the baby girl's stomach looked swollen. Letby said she would keep an eye on it. That night, the mother was at home when she was informed Child I had deteriorated again and to come to the hospital. When they arrived, resuscitations were being carried out on Child I. The swelling to Child I's stomach had 'now gone down' and she was 'doing better', the mother was told by one of the nurses. Child I was then taken back to room 2.
11:06am: The mother recalled Child G had also been poorly 'a number of times' at this time in mid-September. Child I was 'looking different' and was looking around, looking like 'a full-term baby', like 'she should be at home in her bed'. The mother had seen so many people 'not washing their hands and then touching things', so she wanted to get Child I home. Lucy Letby offered advice on how to bathe Child I, to the mother. She offered to take photos using Child I's mother's mobile, to which the mother agreed. Letby always appeared 'reserved' compared to other nurses, the mother added.
11:09am: Child I was put on antibiotics 'as a precaution'. She could go from normal to 'almost dying' within a matter of seconds, the mother recalls. She says staff 'made a big deal' of Child I's stomach. A test was carried out for cystic fibrosis. The mother had felt the atmosphere in the hospital 'had changed' and she had concerns whether Child I would be able to go home. She asked a nurse if that could be the case, and the nurse replied 'We'll see - she comes off antibiotics on Wednesday, so we'll see'.
11:13am: One day, the mother was sitting there by Child I, when suddenly Child I's oxygen monitor started bleeping. The nurse - not Letby - said it was nothing to worry about, and began fiddling with the monitor. The mother said when she left that night, things 'didn't feel right', as these had been signs before Child I became very poorly. The mother was informed overnight Child I's monitor had been switched off as she didn't need it, and her temperature had dropped. Child I later deteriorated and needed to be resuscitated 'at least 7 or 8 times'. The hospital believed Child I had a bowel problem. She was not found with a swollen stomach, but was not breathing. The mother believed if the monitors had been kept on, then the situation could've been more closely monitored. Child I recovered, but with swelling to her stomach and bruising under her left breast bone. She 'kept being resuscitated' and the parents were informed about Child I's deteriorations 'every day'. A doctor told the parents they were concerned Child I 'wouldn't be able to make it.'
11:20am: A couple of days later, Child I had 'picked up, but was told by a nurse that Child I's heart rate was 'still too low', and it was suggested that Child I would be Christened. The mother said she felt that by Christening her, it would be like giving up, but they didn't. Following the Christening, Child I's stats dropped and she was transferred by ambulance to Arrowe Park on October 15. Arrowe Park then told the parents there was 'nothing wrong with her'. The mother felt the staff were 'being rude' and she felt she had to defend the Countess staff as they had to save Child I's life 'time and time again'. The Arrowe Park doctor told the mother he 'couldn't understand what she was saying'. The nurse said she was going to give Child I some milk, and the mother said 'no, she's nil by mouth'. The nurse apologised and said she hadn't read the chart. The mother was angry at this. The mother was told Child I was fine, but when the baby was turned over, she collapsed. The mother screamed at the doctor to do something. The mother said the journeys between the hospitals would 'take it out of' Child I. Child I improved and was transferred back to the Countess on October 17. Child I 'didn't look herself' and it was like she was 'looking through me', the mother said to her mother.
11:23am: At 12.30am on October 23, the mother woke up to find she had a missed call from the hospital. She rang through to a nurse and Child I had 'a little turn' and had been put on a ventilator. The mother said she had to get to the hospital as she wasn't happy about Child I being back on a ventilator after all this time. After ringing back, she was told to get to the hospital 'as soon as she can'. When they arrived, they found staff including Letby were trying to resuscitate Child I. That had been done for 20 minutes. After some time, the mother said to them: "You can't keep doing this anymore." Resuscitation efforts ceased and Child I was passed into the arms of the mother, and Child I died shortly afterwards.
11:24am: Two nurses, including Letby, asked if the mother wanted to bathe Child I. While bathing, Letby was "smiling and kept going on about much she was present at [Child I]'s first bath and how much [Child I] had loved it. "I wished she'd just stop talking. I think, eventually, she realised. It wasn't something we wanted to hear right now. "I remember it was Lucy who packaged up [Child I]'s belongings."
11:29am: The mother was told a post-mortem examination would need to be carried out for Child I, as the cause of death was not known. In a subsequent statement, the mother clarified a few points from her original statement. It was at the time she met Letby as she was changing Child I's nappy, and Letby remarked on Child I's stomach. She said she would normally attend hospital at 9am each day and do the same thing, checking on Child I, speaking to staff, and feed (if Child I was not on a feeding tube). She would also meet family in the canteen. At around 3pm, Letby walked in and stood by the window, about 6ft away from mother and baby. She said: "I've noticed her belly is extended today, I'll go and check with the doctor." The mother agreed. A medical staff member checked the belly and noted it was soft, and it would be examined. For the October 14 incident, the mother recalls she was staying overnight at the hospital, woken up as Child I was poorly. On each occasion they were called to the neonatal unit. she does not recall holding Child I's hand as this would have been impossible with so many staff working on Child I.
11:31am: Mr Johnson says the court will now be going through the sequence of events for Child I. Additional documents are now being presented to the jury.
11:33am: Intelligence analyst Claire Hocknell is recalled to talk the jury through the sequence of events for Child I.
11:34am: This sequence of events will focus on 'the first event' for Child I, which happened on September 30, 2015.
11:41am: Child I was born at a gestational age of 27 weeks at 8.47pm on August 7, 2015. She was transferred to the Countess of Chester Hospital on August 18, being cared from 8.30pm. She was transferred back to Liverpool on September 6, before going back to Chester on September 13, at 11pm. On September 21, Letby was working a long day shift. During that day, Child G suffered a significant deterioration at 10.15am. Letby worked a number of night shifts on September 23, 24, 25 and 26. during this time, Child H suffered two significant deteriorations. Letby then had a few days off work before returning on September 30.
11:47am: A note by the day shift nurse, Shelley Tomlins, gave a brief update on Child I for September 29, recording the mother had been present for 'cares', and regular 35ml feeds of expressed breast milk and fortifier were administered every three hours. A subsequent note recorded Child I 'remains pale but managing to complete bottles (slow to feed as windy).'
11:51am: The overnight shift nurse, Jennifer Jones-Key, said Child I continued to be fed regularly, with her tummy 'full but soft', and the father present for cares.
12:08pm: The court is now resuming after a short break. The sequence of events is now going on to the day shift of September 30, 2015, which has Lucy Letby as a designated nurse.
12:11pm: Letby was looking after three babies in room three that day, including Child I. Child G was in room 2, with two other babies. Two babies were in room 1.
12:14pm: Consultant paediatrician Dr Elizabeth Newby records, as part of an inspection for Child I as part of a 'grand round', for feeds to continue. Feeds are continued for Child I during the day at 10am, 1pm and 4pm, of 35mls expressed breast milk and fortifier. The 10am feed is by bottle, the 1pm and 4pm are via nasogastric tube with Child I being recorded as asleep for the latter two feeds.
12:20pm: On September 30, at 12.15pm, Child H is transferred back to the Countess of Chester Hospital. At 1.36pm, Letby records Child I's temperature in the hotcot. She adds, after a note on the 3x8 feeds: "'Abdomen appears full and slightly distended. Soft to touch, [Child I] straining++. Bowels have been opened. Mum feels it is more distended to yesterday and that [Child I] is quiet. Appears generally pale. Not on monitor...[will continue to monitor situation]" 1.48pm: "Mummy visiting, carrying out feeds and cares".
12:22pm: A note for the feed at 1pm is read out to the court - 'EBM+fortifier, NGT, vomit aspirated 5ml, ph5'. It is signed by Letby.
12:24pm: Letby records, for 3pm: 'Reviewed by Drs as [Child I] appeared mottled in colour with distended abdomen and more prominent veins. Advised to continue. Temperature within normal range with hot cot at 38 degrees. Full monitoring recommenced. within normal range.' Observations are commenced more regularly for Child I, the court hears.
12:28pm: A 35ml feed at 4pm for Child I has an aspirate of 3ml, with Child I 'asleep'. It is signed by Letby's initials. Letby notes: 'did not wake for feed at 1600 therefore NG Tube feed given'. Child I then suffers a deterioration at 4.30pm. 4.30pm on the feed chart records, for Child I, 'large vomit and apnoea - nil by mouth'. It is not signed by anyone.
12:32pm: Letby notes: 'At 1630 [Child I] had a large vomit from mouth and nose++ suction given. Became apnoeic with bradycardia and desaturation (30s). Help summoned and IPPV given for approx 3min in 100% oxygen to recover. Drs were crash called. Transferred to nursery 1...' A doctor [who cannot be named] records he is crash called. He notes 'Chest clear... Abdomen distended, active bowel sounds all zones'
12:35pm: Letby's mentor replies to a message Letby had sent earlier, expressing birthday wishes, at 5.23pm: 'Ah thank you so much. You ok? x'
12:37pm: An x-ray is taken of Child I at 5.39pm, with the radiologist recording: 'There is splinting of the diaphragm due to bowel distension...there is moderately severe bowel distention which is thought to involve both large and small bowel. The appearances are suspicious of NEC...'
12:39pm: Medication of glucose and sodium chloride is co-signed by Letby at 5.45pm and 6pm. A CRP blood reading for Child I is 'less than 1'.
12:47pm: Child I suffered another deterioration at 7.30pm. Letby's notes, written in retrospect at 8.26pm, record: 'At 1930 [Child I] became apnoeic - abdomen distended++ and firm. Bradycardia and desaturation followed, SHO in attendance and registrar called... Nil by mouth. NG tube on free drainage. Cannula inserted but tissued during saline bolus (5mls given). Colour appears pale but improved from earlier in shift. Abdomen appears full and distended. Veins more prominent. Not further vomits. Responsive but quiet on handling.' For the family communications: 'Mummy present when reviewed by Drs. Had left unit when [Child I] had large vomit and transferred to nursery 1. [Mother] up to date with current plan...' Nurse Bernadette Butterworth, who took over care of Child I for the night shift, records: 'During handover [Child I] abdo became more distended and hard she had become apnoeic and bradycardic and sats had dropped. IPPV given and despite a good seal with Neopuff there was still no chest movement...'
12:48pm: The doctor records 'ticks' for temperature instability and apnoea for Child I at 8pm.
12:50pm: Letby's final note from 8.26pm: '[Child I] is now very pale and quiet.'
12:52pm: Letby responds to her mentor: 'Yes thank you. Hope you are enjoying your celebrations. X'
1:04pm: The court is shown a series of text messages sent to and from Letby's phone from that night.
2:11pm: The text messages related to one of Letby's female colleagues having an argument with another nurse who 'snapped at her'. Letby messages Jennifer Jones-Key to say: "I am a bit up and down. Have not had nice shifts and not been feeling supported by some people." Letby messages another colleague: "Let's run away!!!" and the subject turns to moving away to New Zealand, which one of the nurses is planning to do. Letby said she could not do so as it would mean leaving her parents behind, they would be "completely devastated". She said she had come to Chester for university and did not go back to Hereford, and added: "I feel guilty being so far away often", but it was what she wanted.
2:14pm: Letby messages colleague Alison Ventress at 10.09pm: "Families are tough aren't they!" followed by two sad face emojis. Alison Ventress replied: "Some more than others!..."
2:17pm: Letby messages Jennifer Jones-Key to say she had been originally taken off the September 30 shift for working the previous Wednesday night, but was later put back on the shift.
2:19pm: The sequence of events relays medications which were given to Child I throughout the night shift, along with regular observations.
2:23pm: For the day shift on October 1, Ashleigh Hudson was the designated nurse, who continues to record observations for Child I. Bernadette Butterworth inputs an incident, written at 8.30am for 8.30pm the previous night, about administering an antibiotic infusion over 10 minutes instead of 30 minutes. 'Although correct dose was given it was delivered at a faster rate. When aware of mistake, infusion was adjusted. Reg and shift leader informed'.
2:26pm: Bernadette Butterworth recorded Child I, at 8.44am, was 'handling much better without desats/Bradys'. Was initially very pale colour has improved, abdo remains distended and firm but less distended than at beginning of shift'. The parents were made aware of the plan of care. A doctor, during the ward round, said it was considered to restart feeds for Child I. The parents were concerned Child I may be lactose intolerant, and that had possibly led to abdominal distention.
2:28pm: Letby messages her mother on October 1 to say she has arranged her shifts so she will be off for Christmas, and will be visiting her parents at that time. The mother replies: "That's fab, I could cry"
2:30pm: Ashleigh Hudson records, at 1.36pm: [Child I] appears pale but pink and well perfused...' followed by a number of medical notes.
2:33pm: The sequence of events goes to the end of October 1, with Ashleigh Hudson recording at 7.48pm: Review by Paeds SHO...abdomen is softer and less distended, ? start cautiously feeding...' Both parents were updated on the plan of care. Letby searches for the mother of Child I on Facebook at 1.16am on October 5.
2:35pm: On November 5, 2015, Letby searches for the mother of twins Child E and Child F at 11.41pm, then searched for the mother of Child G at 11.44pm and, in the same minute, a search for the mother of Child I. Letby also searched for the mother of Child I at 11pm on May 29, 2016.
2:41pm: Benjamin Myers KC, for Letby's defence, is asking Claire Hocknell questions. He asks about the feeding chart in connection with nursing notes by Lucy Letby at 1.36pm on September 30, with addendum at 1.48pm. The nursing note was written at 1.36pm, covering 8am-1.36pm, and the family communication is timed at 1.48pm 'mummy visiting, carrying out feeds and cares'. Mr Myers says the feeding chart for 8am-1.48pm shows one event of mother coming for feed that morning. He says the family communication isn't timed, and can refer to the period of 8am-1.48pm, not the time the note was written at 1.48pm.
2:47pm: Mr Myers refers to hourly observation charts which on occasions are not signed. He refers to two which happened in the case of Child C, where there was an hour which was not signed. The nurses who signed for each hour either side of that are not Lucy Letby, but signed by her colleagues.
2:48pm: Observation charts which are not signed by initials are also shown for Child I, with three in a row not initialled.
2:54pm: Kate Tyndall, intelligence analyst, has now returned to talk the jury through neonatal reviews for Child I.
3:07pm: A statement from a consultant neonatologist at Liverpool Women's Hospital is being read out. She gives details of Child I's birth, and said Child I was born in 'very good condition'.
3:08pm: Child I was 'stabilised very quickly' with no concerns, before being admitted to the neonatal unit after being allowed to be shown to her mother.
3:12pm: Child I had 'very good gases' after being put on breathing support device CPAP. There were readings consistent with an infection, but Child I was on antibiotics. A lumbar puncture and phototherapy were commenced. Feeds were commenced, using expressed breast milk, on August 8 and Child I continued to be 'very stable, in spite of having an infection'.
3:14pm: Child I later had desaturations and bradycardias, so a second line of antibiotics was begun. The CRP infection marker was low, but the white blood cell count was elevated. A programme of five days of antibiotics began, and after a short gap in feeds, Child I continued to be fed. Child I was stable when taken off CPAP for short periods of time.
3:16pm: On August 18, Child I was stable on CPAP, having four hours off it. She was tolerating feeds "very well". She had "normal tone, posture and movement".
3:19pm: The team at Liverpool had to wait until a bed became available at Chester before transfer was authorised on 'day 11', when Child I weighed 90g more than her birth weight, which "was good", as it was expected that babies would drop in weight in the days after birth. "We expected [Child I] would continue to improve at Chester".
3:23pm: Upon Child I's return to Liverpool Women's Hospital, her blood gases and heart rate were "normal". It was thought that Child I had suspected sepsis rather than NEC, and a course of antibiotics began to cover for both possibilities. Child I was kept nil by mouth but was "stable" on the night of September 6. There was a "mechanical obstruction" in the ET tube on September 7 and Child I was re-intubated. After this she "had normal gases and improved very well".
3:25pm: Feeds were gradually increased and the course of antibiotics ended after five days.
3:32pm: Child I continued to tolerate and build up feeds, which was a sign the baby girl did not have NEC. The expectations were that Child I would return to the Countess of Chester Hospital and continue to improve.
Thursday 26th January 2023
Child I
Unnamed nurses - Nurse Bernadette ButterworthChester Standard article 26-01-2023
A NURSE could not remember telling a mother her child "didn't die of prematurity", the murder trial of Lucy Letby was told.
Fellow nurse Letby, 33, is accused of murdering the baby girl, known as Child I, on her fourth attempt, while she was being cared for at the Countess of Chester Hospital's neo-natal unit.
Her then-colleague was asked if she could recall a later conversation with Child I's mother, who had returned to the unit to drop off cash she had raised.
She had looked after Child I the night before she died on October 23, 2015, and had dressed the baby, who had become "very unsettled", Manchester Crown Court heard on Thursday, January 25.
The nurse, who cannot be named for legal reasons, said: "Mum came in and asked why I had dressed her and I explained I wanted to see if it settled her.
"I don't remember saying to her that (Child I) didn't die of prematurity. I only remember the babygro part of the conversation."
Letby's alleged victim weighed just 2lb 2oz at birth in August 2015, but by September 29 was noted by medics to be "gaining weight nicely" and "doing OK".
On the afternoon of September 30, she required breathing assistance from nursing staff via a face mask, after she had a large vomit and her blood oxygen levels and heart rate plummeted.
The defendant, who was Child I's designated nurse on the shift, handed over her care to night-shift nurse Bernadette Butterworth in the early evening, when the youngster deteriorated once more.
The oxygen face mask was used again but no chest wall movement was detected, the court heard.
Miss Butterworth noted Child I's swollen tummy and asked Letby to aspirate her nasogastric feeding tube, which obtained a "fair amount of air" and 2ml of milk.
She told the court: "She settled down. She came back to normal, her heart rate and respiratory rate."
Doctors suspected a bowel problem as they prescribed antibiotics and ordered blood tests and X-rays.
On the afternoon of October 1, Letby messaged a colleague: "(Child I) was found gasping in cot, full resus and vented. Don't know why. Wasn't nice."
In a statement to the court, another nurse, who cannot be identified for legal reasons, said that at about this time there were "massive staffing issues" and people were coming in to do extra shifts on the unit.
She said it was "mainly Lucy doing a lot" of extra shifts as she was qualified to carry out emergency care if required.
The nurse added: "Lucy was young, living in a doctors' halls of residence and saving to buy a house.
"She was single and was willing and wanting to do extras."
The Crown say Letby made further bids to kill Child I in the early hours of October 13 and 14 before her final successful attempt later that month.
It is alleged she harmed the youngster by either injecting air into her feeding tube and bloodstream, or overfeeding her with milk.
The defence say Child I's clinical problems "may have been inevitable given her extreme immaturity".
Letby, originally from Hereford, denies murdering seven babies and attempting to murder 10 others between June 2015 and June 2016.
Friday 27th January 2023
Child I
GP Dr LucyBeebe - Nurse Ashleigh HudsonChester Standard article 27-01-2023
A NURSE accused of multiple baby murders was seen crying as she said: "It's always me when it happens."
Lucy Letby, 33, made the remark amid a series of collapses of infants at the Countess of Chester Hospital's neo-natal unit, Manchester Crown Court heard on Friday, January 27.
GP Lucy Beebe told police she saw a tearful Letby in conversation with a colleague in one of the care rooms at the unit.
Giving evidence on Friday, Dr Beebe said: "I remember Lucy crying with another nurse and it was very much of the gist of 'it's always me when it happens, my babies, it's always happening to me a lot'."
Prosecutor Philip Astbury asked: "Who was saying that?
Dr Beebe replied: "Lucy."
Mr Astbury said: "You can't remember precisely when that was?"
"No," said the witness.
Dr Beebe said she cared for a premature-born girl, Child I, during her spell as a GP trainee doctor at the Countess of Chester.
The Crown say neo-natal nurse Letby murdered Child I in the early hours of October 23, 2015.
It was said to be her fourth attempt to deliberately harm the baby after earlier bids on September 30, October 13 and 14.
Dr Beebe said: "I recall (Child I) because it was unusual that she was seemingly well and then became unwell.
"In my memory I felt like she was shipped out to a tertiary centre, made a rapid recovery and then was brought back very quickly.
"It certainly stuck in my memory because it had never happened to a baby I had been involved in the care of before or since, at any of the neo-natal units I worked at."
Asked about her reaction to Child I's death, she replied: "Shock and frustration at the time because on reflection I felt there was something else going on with (Child I) that we were not getting to the bottom of.
"It was sad because I remember the family and the whole situation was just very sad and frustrating."
Dr Beebe agreed with Ben Myers KC, defending, and also told police, that Letby's tearful exchange "seemed a pretty normal reaction" given the upsetting events at the hospital.
Nurse Ashleigh Hudson told jurors the lights in a nursery were switched off, rather than dimmed, when she discovered Child I "pale and floppy" in her cot in the early hours of October 13.
Miss Hudson was Child I's carer on the night-shift but she said she asked Letby or the nursing shift leader to keep an eye on the youngster as she was required to help a colleague with a routine procedure elsewhere.
She said that procedure took about 15 minutes and she then walked to a store room to collect Child I's milk.
On her return to nursery room 2 she started preparing the milk for a feed on a counter which faced the lit corridor, she said.
She said: "I can remember at one point in time Lucy was standing in the doorway. She was leaning up against the frame. She pointed out from where she was that she thought (Child I) looked pale."
Letby was "about 5ft/6ft" from the cot but Miss Hudson said she was closer and could not see Child I's face as the top half of the cot was obscured by a canopy.
Fellow junior prosecutor Simon Driver asked: "Was there anything about the circumstances, the layout or the lighting within that room, which afforded Lucy Letby a better view than the one you had?"
"No," replied Miss Hudson.
In August 2020, the court heard, Miss Hudson was taken to the unit by police officers to help her recollection of the position of the cot and the lighting at the time.
Mr Myers asked: "It's impossible, isn't it, to recall precisely how the lighting was five years previously?"
Miss Hudson said: "Not precisely. It is an image that has been imprinted on my brain for quite some time. It's quite vivid."
Mr Myers said: "Is it possible that the nursery light may have been low on the dimmer rather than off?"
Miss Hudson said: "No, it was off."
The witness said she had stood in that doorway at night and had looked at a cot in that position but it had not provided her a clear vantage point.
Miss Hudson said she approached Child I's cot side, pushed back the canopy and peeled off her blankets.
Wiping away tears, she told the court: "That's when I noticed she was in quite poor condition.
"She was incredibly pale in colour, almost white. She didn't respond to me. She was very still.
"She was floppy and she was making gasping breathing movements – a handful of times within a minute."
Mr Driver asked: "What was your first thought when you saw (Child I) at close quarters in that cot?"
Miss Hudson replied: "My first thought, and worry, was that she had deteriorated so rapidly that it was too late. The change in her had been remarkable."
She said she gave Child I ventilation breaths via a face mask before Letby took over with the airway while she began chest compressions.
Child I eventually recovered after nurses and doctors fought to resuscitate her for more than 20 minutes, the court heard.
Miss Hudson said Child I was in "good clinical condition" at the start of the shift.
Letby, originally from Hereford, denies murdering seven babies and attempting to murder 10 others between June 2015 and June 2016.
Monday 30th - Tuesday 31st January 2023 - no court (reason unknown)
Wednesday 1st February 2023
Child I
Dr Matthew Neame - text messagesChester Standard article 01-02-2023
A DOCTOR recalled "unusual" skin mottling on a baby girl allegedly murdered by nurse Lucy Letby, a jury heard.
Letby, 33, is accused of injecting air into the youngster's stomach via a feeding tube during a night shift at the Countess of Chester Hospital's neonatal unit.
It is said to have been the defendant's third attempt to kill her before she allegedly succeeded in another similar attack more than a week later in October 2015.
Giving evidence on Wednesday, February 1, registrar Dr Matthew Neame told Manchester Crown Court the premature-born infant, known as Child I, was "stable" when he examined her at 10.05pm on October 13.
He said he thought Letby asked him to see Child I at 5.55am on October 14 as her oxygen requirements had increased.
On examination, Dr Neame noted her abdomen was "distended", "mottled" and with "some tenderness".
He said he noticed Child I's eyes were open and she "grimaced".
Dr Neame said: "I don't recall it clearly but it's unusual to see mottling on the abdomen.
"My impression was the increase in abdomen distension may have caused (Child I's) lungs to be squashed… making it hard for her to breathe."
The court heard Letby retrospectively noted that at 5am Child I's abdomen was "more distended and firmer in appearance with area of discolouration spreading on the right side".
Letby, who was Child I's designated nurse, noted she gave antibiotics at 5.05am.
She also retrospectively noted that at 5.30am Child I's "abdo distended ++".
Jurors were told that at 7am Child I had a "significant" drop in blood oxygen levels and heart rate.
At 7.45am, her heart rate fell "dangerously low" to below 60 beats per minute, said Dr Neame, which prompted CPR to begin.
Thirteen minutes of resuscitation from medical staff followed before she recovered.
The court has heard evidence of numerous babies having a "mottled, discoloured" appearance before collapsing.
Ben Myers KC, defending, asked Dr Neame: "Your view is mottling normally means circulation is not as good as it should be?"
Dr Neame replied: "That's right."
Mr Myers went on: "And the underlying cause could be infection in some cases?
Dr Neame said: "Yes (but) when seen infection is usually accompanied by other signs."
Mr Myers said: "Or low oxygen levels?
The witness said: "It can be."
In WhatsApp messages read to the court, Letby asked a colleague on the afternoon of October 14 if Child I was staying on the unit.
She added: "I'd like to keep her please."
Her colleague, who cannot be identified for legal reasons, replied: "Yes. Staying for now. OK re keeping."
An hour later the colleague messaged: "I've had to reallocate. Sorry."
Letby said: "Has something happened?"
The colleague replied: "No. Was just asked to reallocate so no one has her for more than 1 night at a time. Or 1 shift. Not just night." Letby responded: "Yeah that's understandable."
The Crown says Letby, originally from Hereford, murdered Child I in the early hours of October 23.
It was said to be her fourth attempt to deliberately harm the baby after earlier bids on September 30, October 13 and 14.
Letby denies murdering seven babies and attempting to murder 10 others between June 2015 and June 2016.
Thursday 2nd February 2023
Child I
Statements from: Nurse Shelley Tomlins, Nurse Joanne Williams, Nurse Laura Eagles, Dr David Harkness, Consultant from Arrowe Park Hospital - Police analyst: Recorded events & messages, sympathy card - Nurse Ashleigh HudsonChester Standard Live Reporting
10:26am: The courtroom at Manchester Crown Court is beginning to fill up with lawyers and members of the press, while Lucy Letby has also arrived.
10:32am: The judge, Mr Justice James Goss, has entered the courtroom. The jury will now enter, and the prosecution will continue delivering evidence in the case of Child I. The prosecution allege that Lucy Letby tried to kill Child I four times, murdering her on the fourth attempt. The defence deny this.
10:35am: An 'agreed facts' statement is read out from nurse Shelley Tomlins, who recalls Child I. She said she was the first one who looked after her upon her arrival, and looked after her multiple times. She recalls Child I "definitely" had feeding and gut problems, and problems with a distended abdomen. She said "it was like" there were blockages in her bowel. For September 29, 2015, she was the designated nurse on a long day shift. Child I was "mottled" in appearance, with blotchy skin. She said some babies looked like that "all the time", and for some it was a sign they were not well. She says she cannot say for certain, but the mottled appearance was "probably" all over her body.
10:37am: She says Child I had a cardiac arrest "as we were looking at her". Resuscitation attempts began and the family arrived, along with Dr Ravi Jayaram, consultant doctor. The nurse describes the procedures done to stabilise Child I.
10:42am: The nurse recalls a point when the bowels went "massive" and caused another collapse, as it impacted the lungs. The nurse says the shift was significant for her as it was her last ever shift at the hospital, leaving the hospital a few days later.
10:47am: Nurse Joanne Williams, in a brief agreed facts statement, recalls being involved in chest compressions for Child I. Laura Eagles, in her agreed facts statement, was also asked about the October 13-14 event for Child I. She recalls from the notes the collapses happened at 7am and 7.45am. She said Lucy Letby was the designated nurse, from looking at the notes. She recalls who else was on shift and the other babies on that night, and that it was "very busy". She recalls CPR began at 7.45am, and the 7.45am collapse was more or less a continuation of the 7am collapse. She said from her memory, Child I was ill for a long time, and it was difficult to separate one event from another in her recollection.
10:51am: Dr David Harkness, in his statement, said October 13-14 was "quite an eventful night" for Child I. He said Child I deteriorated and required CPR in the early hours. His next recorded entry was on a ward round later on October 14. He said it was suspected Child I had NEC. She had had two "quite prolonged" cardiac arrests and was on a ventilator. Blood gases were "acceptable but not fantastic, and on the poor side". There "had been a suggestion of a collapse of the left lung", which would explain why there were problems ventilating her. Child I's bowels were open, which was a "good sign". Blood culture tests were awaited, for signs of an infection.
10:53am: Further tests were sought to check for NEC and to monitor Child I's bowels. If the signs were worsening, then surgery would be carried out. Plans for 1-2 weeks down the line were to insert radioactive dye into the bowels to test for bowel obstructions. By 4pm on October 14, Child I's signs had improved.
11:00am: Dr Harkness says NEC is difficult to diagnose without carrying out surgery, and suspected NEC is usually treated with antibiotics. He says he remembers Child I's death, and the parents coming back a few times over the following year. The next statement is from a consultant doctor at Arrowe Park Hospital. The doctor recalls Child I was transported to the unit on October 15, with suspected NEC/inflammation of the gut, which is "not uncommon" in pre-term babies. The intention was that Child I would be "conservatively managed" at Arrowe Park. There was previously discussion on whether Child I should be transported to Liverpool Women's Hospital, but the decision was made to keep Child I in Chester. The following day, following further desaturations, Child I was transferred to Arrowe Park.
11:11am: Child I was "pink, warm and well perfused" and her vital signs were "within normal limits". She was ventilated with oxygen, nil by mouth, on IV fluids then with TPN bags. There was also sedation medication administered. The plan was to stabilise Child I and continue antibiotics, with seven days of antibiotics and nil by mouth. An x-ray showed tubes and a long line were in reasonably good positions. At the end of the shift, Child I was "stable" until a "sudden desaturation" and bradycardia at 12.16am on October 16. She was 'Neopuffed', but there was no chest movement. A test concluded the breathing tube had potentially moved, so it was removed. At the end of the tube was dark blood, likely from Child I's previous collapse in Chester. Child I improved in the early hours of October 16 and notes showed no fresh bleeding, and a different form of breathing support began. Child I was stable in 35% oxygen breathing support, with "no issues" in breathing and it was "reassuring" the tummy looked fine, and the abdomen was soft.
11:15am: Child I was moved to a high-dependency unit at Arrowe Park and her oxygen support requirements were diminishing. There was "no longer a need" for tertiary requirement care, so Child I could be transferred back to the Countess of Chester Hospital. A surgical plan was discussed for Child I, with a dye inserted into Child I to check for bowel obstructions, which would show on an X-ray. On October 17, the transfer back to the Countess of Chester Hospital was confirmed, with Child I being transported back at 11am.
11:25am: Claire Hocknell, intelligence analyst for Cheshire Police, has returned to talk the court through the sequence of events for Child I, focusing on the 'fourth event' in late October 2015. The sequence continues from Child I returning to the Countess of Chester Hospital at October 17, with charts and observations shown from October 22, after Letby had been off work.
11:27am: Nurse Ashleigh Hudson records, for October 22 at 3.04am, that Child I was 'pink and well perfused', with saturation levels above 96%, abdomen 'soft and non-distended'. Child I was 'unsettled at start of shift and rooting, settled with dummy. Settled and sleeping at present'.
11:39am: Nurse Caroline Oakley recorded, for 8am on October 22, Child I's observations were satisfactory. Further observations by a colleague said Child I was 'pink, alert, active handling well'. At the end of the day, Child I was noted to be very hungry. Hourly observations, the prosecution say, were carried through the day and were "unremarkable". Letby begins her night shift that evening. A slide is shown to the court showing Child I was in room 1 with one other baby. Ashleigh Hudson was the designated nurse for both babies. Letby was the designated nurse for a baby in room 2 and one in room 3. Another baby in room 3 was Child G. Two babies were in transitional care, and there was another baby whom the prosecution have been unable to confirm their location for that night.
11:40am: Ashleigh Hudson records Child I, at the start of her shift at 7.45pm on October 22, was 'unsettled and rooting at start of shift, settled with dummy and containment holding'.
11:45am: Letby messages a colleague to say that night had 'only 8 babies' in the unit, and there is a discussion over transporting a baby to Stoke. She adds: "I think I need to see greys anatomy !!!" Later in the conversation, Letby messages to say Child I "had abdo scan that was fine".
11:47am: Letby messages colleague Jennifer Jones-Key, who had enquired "How's work". Letby replies that one of the babies she is looking after that night is being transported out that night. The prosecution say that would then leave her with one designated baby that night.
11:50am: Ashleigh Hudson records at 10.57pm, 'long line removed due to constant occlusions. Neonatal nurse Lucy Letby unable to flush...' The long line was removed and the TPN [nutrition bag] was moved to a peripheral line. Child I was observed to 'tolerate this very well'. 'Sucrose offered, but happy with dummy'. Child I was 'pink and well perfused'.
12:06pm: The jury is returning after a 10-minute break, and the trial is now resuming. Claire Hocknell is continuing to talk through the sequence of events, from 11pm on October 22, 2015. An observation chart shows three-hourly observations are made for Child I through the day (e.g. 11am, 2pm, 5pm, 8pm), but no record is made at 11pm.
12:10pm: Nurse Ashleigh Hudson records a retrospective note at 11.57pm that Child I was "very unsettled...due to huger as rooting. Dummy offered and containment holding to no effect."
"After repositioning, [Child I] became quiet, apnoeic and dusky in appearance. With help of neonatal nurse Lucy Letby, repositioned [Child I] on to her back, and at first applied Neopuff with 30% O2..." A crash call was made to the unit at midnight. Cardiac compressions began. Dr Rachel Chang records, at midnight, confirming being crash called and giving chest compressions. Ashleigh Hudson records consultant paediatrician Dr John Gibbs is also called to the unit. He arrives, according to swipe data unit, at 12.06am.12:12pm: Child I was put on to a ventilator, was more alert, and crying. The abdomen was soft and not distended prior to ventilation, the court hears. An x-ray is carried out at 12.23am.
12:16pm: Child I was extubated and 'coped well', was 'relatively settled' and 'sucking dummy' at about 12.35am. Dr John Gibbs recorded Child I had been 'resisting ventilation', so was extubated. The cause was recorded as 'likely generalised lung collapse'. Int he plan: 'If further similar collapses will need full ventilation (with paralysis)'. Nurse Ashleigh Hudson records informing the parents of what happened.
12:19pm: At 1.06am, there is a further event for Child I - another collapse, the prosecution tells the court. Nurse Ashleigh Hudson records: 'Child I became unsettled again. Dummy/sucrose offered with no effect. Slowly became dusky and O2 dropped to 60s, HR 70s. Ran to labour ward theatre to inform [senior staff].' Letby was one of two nurses administering breathing support to Child I via Neopuff. Dr Rachel Chang is recalled to the unit, arriving at 1.12am. Compressions restarted and Child I was reintubated. At this time, Child I's mother had rung the hospital and she was advised to attend hospital immediately, the court hears.
12:25pm: Adrenaline is administered to Child I and Dr John Gibbs is called to the unit again. He arrives at the unit at 1.23am. A saline bolus is administered to Child I at 1.22am. The medication is co-signed by Lucy Letby and Christopher Booth. Dr Gibbs records, for 1.25am, Child I had 'poor perfusion - mottled, purple-white'. Sats were in the '70s, pulse 50-60'. More adrenaline is administered, along with sodium chloride and atropine.
12:28pm: A dose of 10% glucose is administered at 1.38am, co-signed by Ashleigh Hudson and Christopher Booth. Another dose of adrenaline, the fifth, is made at 1.40am, co-signed by Lucy Letby and Christopher Booth. The administration of calcium gluconate is made at 1.40am. A sixth dose of adrenaline is made for administering at 1.43am. Compressions stopped at 1.45am, having begun at 1.16am. Dr John Gibbs adds Child I 'remained mottled and poorly perfused'.
12:32pm: At 1.50am, Dr John Gibbs records: 'HR to 70, sats 70-80 and no pulse palpable. Cardiac compressions restarted at 1.50am'. Another dose of adrenaline, the seventh, is made at 1.56am, followed by an eighth at 2am. Dr John Gibbs records Child I was 'not responding to prolonged resuscitation and although her heart was beating there was no effective circulation. 2.10am hr 40/min on monitor - no pulse (but heartbeat audible without cardiac compression)'. Ashleigh Hudson records she and Lucy Letby had spoken to the parents about what had happened, and a decision was made to bathe Child I. Child I's time of death was recorded as 2.30am on October 23, 2015.
12:37pm: Ashleigh Hudson records, at 6.25am: 'NGT on free drainage, produced 2mls. Minimal aspirations of clear mucus and air++ during both resuscitations'. A colleague of Letby messages her at 6.51am: 'Hey u ok? Good shift? x' Another colleague messages Letby at 11.58am: 'You ok? I heard about last night. Did you have [Child I]? Xxx'
12:46pm: Caroline Oakley records at the end of the day, '[Child I] with parents and family in bedroom 2... They have expressed they are very unhappy with AHCH [Alder Hey Children's Hospital] for failing to accept [Child I] for her barium enema, and want her back from AHCH post-mortem ASAP. Bereavement co-ordinator has spoken to them...'
12:57pm: A post-mortem examination of Child I takes place on October 26. On November 5, Letby searches for the mum of Child E and F, then the mum of Child G, then the mum of Child I in the space of three minutes between 11.41-11.44pm, on her day off. The funeral of Child I takes place on November 10. At 7.34am that day, Letby has a photo taken of a sympathy card she has written to send to the parents. The card is titled 'Your loved one will be remembered with many smiles'. It adds, in Letby's handwriting, 'Lots of love, Lucy x' on the front. On the other side of the card, Letby has a handwritten message, in which she wrote: "There are no words to make this time any easier. "It was a real privilege to care for [Child I] and get to know you as a family - a family who always put [Child I] first and did everything possible for her..." The message concludes with Letby saying she was sorry she could not attend the funeral.
1:16pm:
1:29pm: Previously, the court heard from the prosecution that Lucy Letby was asked by police about a sympathy card she had sent to the child's parents. She said it was not normal to do so - and this was the only time she had done so.
2:04pm: The trial is now resuming, with intelligence analyst Claire Tyndall returning to court, to talk through the neonatal unit review schedule in late October 2015.
2:12pm: Nurse Ashleigh Hudson is now being recalled to give evidence in the case of Child I.
2:20pm: The nurse is asked to look at nursing notes she had compiled early on October 22, a summary of the care provided to Child I. She says Child I's heart rate was normal, the respiration rate was slightly elevated on a one-off reading, while her temperature was stable. She was in room 1 of the neonatal unit, but "not an intensive unit baby" at this time. She was placed there as "a precaution measure" due to her recent medical history. She was in an incubator, again as a precautionary measure due to her recent history, the court hears. The nurse said the oxygen saturation levels, recorded as "96% and above", were "optimal".
2:25pm: Child I was "pink and well perfused", with "minimal aspirates recorded, clear fluid. Abdomen soft and non-distended," according to nurse Hudson's notes. "She was a very stable baby considering the weeks prior," the nurse tells the court.
2:26pm: Child I would still have been classed as an 'HDU' baby [high dependency], as nurses would have had to check the long lines every hour, the court hears. The nurse says she does not recall anything of note happening during that night shift on October 21-22.
2:31pm: Nurse Hudson recalls she was aware Child I was facing a medical procedure at another hospital which was 'urgent, but not an emergency'. She said she took over care of Child I at 7.45pm on October 22. The prosecution ask why it would be 7.45pm rather than, say, 8pm. The nurse replies the handover was likely briefer than usual, as there was not a lot of information to pass on for Child I from the day shift at this point. Child I's observations for heart rate and respiratory rate were satisfactory, while the temperature and oxygen saturation readings were "optimal". Child I was not receiving ventilator support at this time.
2:36pm: Child I was "unsettled and rooting at start of shift" and the longline was removed due to constant occlusions. Lucy Letby was "unable to flush," so paediatric registrar Rachel Chang was informed. Nurse Hudson's note continues: 'Dressing stripped and line pulled back, still not flushing, so removed.' No Oedema or duskyness' The nurse recalls Child I reacted to the procedure "very well". Sucrose was offered, but Child I was happy with dummy. The baby girl was "pink and well perfused at this time, awake and alert". The sucrose was sugar water which would be offered as pain relief, but if the child was happy enough to stay with the dummy, the sucrose would not be "pushed further".
2:38pm: The nurse said Child I was "generally quite easy to settle" and would settle "quite quickly", and would be "quite happy" when put into a cot or incubator.
2:40pm: The nurse recalls the events leading up to midnight. She says, just prior to midnight, Child I was very unsettled, and tried the usual methods of containment holding, sucrose and dummy, which did not work. She tried repositioning Child I so she was on her stomach, which sometimes settled her, but Child I continued to be very unsettled and cry. She says sucrose would be administered for a child as a comfort measure to a child who was otherwise nil by mouth. Child I would be placed on her stomach with her head to one side. She said the measures to settle her "would generally work" with Child I and with other babies in general.
2:43pm: The nurse says she was familiar with Child I's crying, and this was an "atypical" episode. She said it was a "type of cry I hadn't experienced her make before - loud, relentless, almost constant. "Just a constant, very loud [cry] - something I had not heard from her before." The repositioning was the last of the calming measure attempts. Within seconds of that, Child I "became very quiet" and had "pauses in her breathing". The nurse said she turned the child back on to her back and shouted for help. "Was there a problem at this stage?" the prosecution ask. Nurse Hudson: "Yes." She said Child I's oxygen levels started to decrease, along with her heart rate. Ventilation breaths were given by nurse Hudson, with Lucy Letby providing assistance.
2:49pm: The nurse said after less than a minute, after realising it was an "acute episode", a crash call would be made to alert doctors. The nurse recalls, from her notes, Child I was apnoeic, and dusky in appearance." A Neopuff device was used to provide breathing support with 30% oxygen. 'Neopuff applied due to colour and apnoea. Colour didn't improve and [oxygen saturation and heart rate] began to drop rapidly until [oxygen saturation] 47% and [heart rate] 50. Neopuff increased to 50% then 100% with no effect." Cardiac compressions began, and Child I was placed on a ventilator. Child I had become 'more alert and crying. Abdomen soft and non-distended prior to resuscitation, no change from handover." Child I was recorded to be fighting the ventilator. The nurse says that was a sign Child I had recovered quite quickly, but keeping the child on the ventilator in that condition could cause lung damage, so a decision was taken to remove her from the ventilator. Child I was "seemingly displaying normal behaviour despite what had happened" as she was also 'still rooting'.
2:56pm: The nurse says this episode, at about midnight, was a "very quick resuscitation" from her recollection, and no medication needed to be administered. The court hears Ashleigh Hudson "managed to get through to [Child I's] parents after many attempts" regarding the first resuscitation. She said it was to be expected as it was the middle of the night. Afterwards, Child I was "seemingly back to normal" with "nothing to cause concern" during that time after the first resuscitation. Just after 1am, she was near, but not inside, nursery room 1.
3:03pm: The nurse says she was first alerted to Child I desaturating either from an alarm sounding on the monitor or from Child I crying. Nurse Hudson recalls: "Lucy was already with her [at the incubator], trying to settle her. At that time [Child I's] observations were normal." She says child I was crying "the same cry I had heard her display the first time [that night]. "Loud and relentless and unlike any other cry I had heard make prior to this night shift."
"My initial concern was she was obviously breathing...my concern was the cry was that she was going to have another episode of collapse." She recalls articulating that concern to Lucy Letby within 60 seconds of being there. The nurse says she said words along the lines of: "She's going to do it again, it's the same cry." Letby responded with words of "reassurance": "She just needs to settle," Ashleigh Hudson recalls Letby saying. Child I became quiet, with pauses in breathing, and she became bradycardic and her saturations "started to drift". Oxygen delivery began again, along with ventilation breaths. They shouted for help from colleagues.3:09pm: Nurse Hudson says she does not recall direct further communication with the parents, as the staff were "all in the thick of it" trying to resuscitate Child I. The court is shown the October 23, 6.25am note by Ashleigh Hudson: "*NGT on free drainage, produced 2mls. Minimal aspirations of clear mucus and air++ during both resuscitations. Green stool and urine present post resus." The nurse said, given previous abdominal issues for Child I, she had wanted to "make clear" what was observed during those resuscitations.
3:22pm: Ben Myers KC, for Letby's defence, is now asking nurse Ashleigh Hudson questions.
3:25pm: He says the questions he is to ask, while technical, are not for lack of sympathy. He says that in between the shifts she was looking after Child I, she was aware there had been further arrests and desaturations. Nurse Hudson agrees, and agrees that Child I was "very ill" when she had gone to Arrowe Park Hospital. He asks if Child I needed to be looked at closely, and "there is always the potential for deterioration". Nurse Hudson: "Yes."
"She is never completely out of the woods?"
"Yes."
"You can never become complacent."
"That was my view at the time."3:27pm: Mr Myers says nurse Ashleigh Hudson was in the first 8-9 months of trained care at the time in October 2015, and would not have been intensive trained at this stage. Ms Hudson says there were certain medical procedures which she would not be trained for at this stage, and it meant when those needed to take place, other staff, such as Lucy Letby, would do them for her.
3:29pm: Mr Myers asks if Child I looked unsettled at times because she was getting hungry. "Yes."
"And at times can they be quite shouty and angry [when hungry]?"
"Yes." Mr Myers refers to the night shift of October 21-22, to the nurse's note 'unsettled at start of shift and rooting, settled with dummy'. He asks if that was the behaviour exhibited because Child I was hungry. Ms Hudson agrees.3:37pm: Mr Myers refers to a note by colleague Caroline Oakley, which notes 'unsettled at times; obviously very hungry but settles with dummy'. Another note, by Ms Hudson, for the start of the night shift on October 22, records '[Child I] was unsettled and rooting at start of shift [7.45pm], settled with dummy and containment holding.' Mr Myers says the issue of the long line had to be resolved during the night, which was resolved between 10.15-11pm. Ms Hudson replies Child I was "very sensitive". Mr Myers said due to the cannula insertion and long line removal, Child I was not receiving fluid via the long line at this point. He asks if the handling of the lines can have a disturbing effect on the baby, would there be an increase of the monitoring? Ms Hudson says the monitoring did continue, it was just not recorded on the observation chart at 11pm, and was still visible on the electronic monitor.
3:39pm: Mr Myers says "All the things you would normally do to settle [Child I] didn't work?" [just before midnight] Ms Hudson replies she called for help once she noticed Child I was "seemingly in distress, clinically", after noticing gaps in breathing after repositioning Child I. Letby arrived in response to the call for help.
3:42pm: Ms Hudson explains the note '[Child I] was very unsettled - ? due to hunger as rooting." She says the '?' means she was not sure of the cause. Mr Myers asks if Neopuff was used up to the point of ventilation. Ms Hudson replies she was not sure, she would give Neopuff assistance in response to what could be seen at the time. Child I 'attempted to cry' before being ventilated.
3:45pm: Mr Myers said Ashleigh Hudson was aware of Child I's history of abdominal distentions. Ms Hudson replies she paid "specific attention" to the abdomen with this knowledge, and noted it was 'soft, non-distended' at this time. Mr Myers said Child I recovered and 'looked better than before the incident took place?' Ms Hudson: "Yes."
3:47pm: At 1.06am, Child I deteriorated once more. Ms Hudson said she was alerted either via an alarm or Child I crying. Mr Myers said once she entered, Lucy Letby was trying to settle Child I with a dummy. "Was this, in effect a repeat of what had gone on earlier?"
"Yes."
"You said you were concerned there was going to be a repeat...and Lucy Letby was trying to reassure you...she was going to be all right?"
"Yes."3:50pm: Mr Myers refers to the family communication note, in which it was discussed with parents for Child I to be bathed, to make hand and foot prints, have photographs and gave consent for hair to be cut, and kept in the memory box. Ms Hudson said this was the first time she had been involved with this bereavement procedure, and Lucy Letby assisted, before colleague Caroline Oakley later took over and completed the procedure.
3:52pm: The prosecution rise to clarify the noise made by Child I. "It was loud, almost like a repetitive noise, relentless. In my interpretation, it would indicate distress, and was markedly different from before when she would express hunger, for instance." The judge asks Ms Hudson for this 'rooting gesture' to be explained. Ms Hudson says it's a classic gesture by babies, usually done before they cry. It can be a very specific behaviour where they rock their heads and stick their tongue out, smacking their lips.
3:53pm: That concludes the evidence from nurse Ashleigh Hudson.
Friday 3rd February 2023
Child I
Professor Owen Arthurs (radiologist) - Dr Rachel Chang - Statements from: Nurse Christopher Booth, Nurse Melanie Taylor, Nursery nurse Valerie Thomas10:07am: I'm back at Manchester Crown Court this morning for the murder trial of nurse Lucy Letby. We'll be continuing to hear evidence in relation to the death of Child I in October 2015.
10:40am: Consultant paediatric radiologist Owen Arthurs is first up in the witness box this morning. He's giving expert evidence on CT scans, X-rays and other images in this case
10:45am: Dr Arthurs published a study in 2015 on the prevalence of air, post mortem, in infants. That study looked at 48 children. Of the 48, six were comparable to this case - but in each of those cases there were clear explanations for the presence of air in vessels He agreed with prosecutor Nick Johnson that it is 'very rare' to find air vessels without an obvious explanation
10:49am: We've gone backwards a little in timeline (the expert wasn't able to make it to court earlier), Dr Arthurs is discussing the case of Child E. It is alleged that Ms Letby fatally injected air into the bloodstream of the baby in June 2015
10:57am: Court is now being shown a radiograph of Child E. Dr Arthurs agrees there is 'no significant abnormalities' present. Prosecutor Nick Johnson asks if an air embolus would show up on such a radiograph Dr Arthurs says an air embolus is not present and to see it there would have to be 'a lot of air' and the radiograph would have to have been 'done almost immediately' after the injection
10:58am: Dr Arthurs is now being asked about Child E's twin, Child F, who the Crown say was also attacked by Ms Letby but survived
11:00am: Dr Arthurs says he can make no real comment on the case of Child F. We're now moving to Child G. Ms Letby is accused of attempting to murder the premature girl three times in September 2015
11:02am: The prosecution alleges Ms Letby overfed Child G with milk through a nasogastric tube or injected air into the same tube
11:06am: Dr Arthurs is taking the court through radiographs, taken at Arrowe Park Hospital and the Countess of Chester, of Child G.
11:28am: Dr Arthurs says 'there isn’t anything specific' to suggest Child G was suffering from sepsis/NEC or any other infection. He said 'there's nothing on the X-rays that would really provide a diagnosis' for Child G's condition
11:30am: We're now moving on to Child H. Ms Letby is accused of trying to kill the infant on two occasions in September 2015. The prosecution claim she first attacked Child H in the early hours of 26 September and then again the following morning
11:36am: Jurors previously heard Child H, who was born six weeks premature, needed treatment for a pneumothorax, which occurs when air leaks into the space between the lung and chest wall. On the evening of 24 September 2015, Dr Alison Ventress inserted a pigtail chest drain to prevent any accumulation of air within the chest. However, in the early hours of 25 September more air had accumulated a second drain was inserted
11:38am: Ms Letby's defence counsel Ben Myers KC previously claimed that Dr Ravi Jayaram inserted the second drain in the "wrong place". Dr Arthurs is now going over the X-rays of Child H which show the drains
11:42am: Dr Arthurs notes that the position of the drains have moved, but he says that the 'precise location isn’t really critical if it’s having the desired effect if it’s draining the pneumothorax' - essentially supporting what Dr Jayaram has previously.
12:00pm: Dr Arthurs is now moving on to Child I. Ms Letby is accused of injecting air into her stomach via a feeding tube
12:10pm: Dr Arthurs has said there is evidence of pneumatosis (gas within the wall of the small or large intestine) on an X-ray from 30 September of Child I
12:19pm: Dr Arthurs has said Child I had a 'normal' bowl, as per her X-ray on 18 October and into 20 October. Looking at an X-ray from 23, there is a 'massive' dilatation of the stomach
12:20pm: Dr Arthurs says it is 'quite unusual to see babies with this degree of dilatation of the stomach', he says it can cause 'splits in the diaphragm' and that can lead to 'respiratory complications'
12:31pm: Asked how much air it would take to generate such images, Dr Arthurs said: 'We don’t know, I don’t think anybody really knows. Those experiments can’t really be carried out, we can’t experiment on babies giving them 50 or 100mls of air and taking x-rays' He adds: 'I would guess more than 20mls of air' He is asked, in the absence of another explanation, whether 'someone has deliberately injected air' Dr Arthurs says 'I think that stands to reason'
1:58pm: We're back after a break for lunch. Ben Myers KC, defending, is now questioning Dr Arthurs
2:07pm: He's asking Dr Arthurs about Child H and the positioning of her chest drains. Mr Myers asks if he is aware of guidelines on where chest drain should be inserted, in terms of the intercostal space Dr Arthurs says that the guidance, to which Mr Myers is referring, 'refers to where they go in terms of the chest wall, not where they are inside chest'
2:08pm: Dr Arthurs accepts that a neonatologist is better placed to comment on positioning of drains and clinical impact
2:31pm: Mr Myers is now moving on to Child I. He put it to Dr Arthurs that from X-rays alone it was "not possible to establish a precise cause" of the air being present, Dr Arthurs agreed
2:32pm: Registrar Dr Rachel Chang, who was on shift the night Child I died, is next in the witness box
2:39pm: Dr Chang is being asked about the events of midnight, 22 October 2015. She tells the court she 'cannot remember' how she was alerted to Child I's crash, but she is reading out her notes from that night
2:41pm: Dr Chang said when she was bleeped she would have perceived that as a 'medical emergency'. Her notes show that when she arrived Child I was being manually ventilated
2:52pm: Dr Chang said Child I 'was in cardiac arrest' when she arrived. The infant was stabilised and an X-ray was taken shortly after (she says this is routine for baby like Child I)
3:00pm: The medic is now recalling events from around 1am on 23 October. Again she does not have a recollection of events and is reading out her notes. Child I again needed chest compressions and ventilation
3:08pm: Slight pause as Dr Chang breaks down in tears while recalling the desperate hour long battle to save Child I. Between 1:16am and 2:10am on 23 October the infant was given numerous rounds of CPR and eight doses of adrenaline, to no avail
3:13pm: Reflecting on Child I's death, Dr Chang said: 'I've never been able to truly explain it, it was awful. 'I knew we’d done everything, I trusted everyone around me'
3:32pm: Prosecution are now reading statements of agreed evidence. First one is from nurse Caroline Oakley - Ms Oakley was on day shifts and wasn't there when Child I died. She described Child I as a 'lovely beautiful but problematic baby'
3:40pm: Another statement from nurse Christopher Booth is being read, he said the events of 23 October were 'very, very distressing for parents' he said the whole team was 'heartbroken' after the death of Child I
3:53pm: Court has now adjourned, back Monday.
Chester Standard article 03-02-2023
A DOCTOR broke down in tears while recalling the efforts to save a baby girl allegedly murdered by Lucy Letby.
Letby, 33, is alleged to have murdered seven babies and attempted to kill 10 others while she worked at the Countess of Chester Hospital's neo-natal unit.
Premature-born infant, Child I, who cannot be identified for legal reasons, is said to have been the ninth child the defendant attacked from June 2015 to June 2016.
The Crown says the nurse murdered Child I at her fourth attempt by administering a fatal dose of air during the night shift of October 22/23, 2015.
Giving evidence on Friday, registrar Dr Rachel Chang said there were no concerns over Child I prior to midnight.
She was then crash bleeped to attend the cotside of the youngster who suffered a sudden drop in heart rate and blood oxygen levels.
Child I stabilised after she received cardiac compressions and breathing support, the court heard.
Dr Chang said: "I didn't have any worrying thoughts. She has had an event. She had had lots of events.
"But I had to work with what was in front of us, which is that she recovered very quickly."
About an hour later Child I similarly deteriorated but doctors and nurses, including Letby, were unable to revive her in a prolonged resuscitation attempt.
Dr Chang tearfully recalled how Child I did not respond to initial chest compressions and ventilation efforts.
Philip Astbury, prosecuting, asked: "Have you reflected on the death of (Child I) and the causes?"
"Yes," replied Dr Chang.
Mr Astbury said: "And the shift, generally?"
Dr Chang said: "Yes."
Mr Astbury said: "What has that caused you, if anything, to think?"
The witness replied: "Just that I have been never able to truly explain it. That it was awful.
"But I was never worried. I knew we had done everything and I did everything I'd done the first time I attended.
"I trusted everyone around me implicitly."
In a statement read to the court, nurse Christopher Booth said staff had got to know Child I and her family "really well" from her time on the unit since August 2015.
Child I was "quite a character herself", he said.
Mr Booth said: "We all were fond of her and had high hopes for her. It was gut-wrenching for the (nursing) team as a group."
He said he wrote to the ward manager to say the team involved in the resuscitation efforts were "all heartbroken".
Mr Booth said: "I wanted her to know that as a team everyone had tried their hardest and did their best.
"If we were not such a good team we would have crumbled because there were so many horrible things going on."
Fellow nurse Melanie Taylor said staff were "devastated".
She stated: "It was just pure shock. She was stable before that.
"I think her parents came in during resus. I remember them walking into nursery 1 and standing there, not really knowing what to do and myself not knowing what to say.
"The actual resuscitation is a bit of a blur to be honest.
"I remember right at the end, the doctor decided to call it and said we should stop.
"I had been looking at (Child I) and the monitor, thinking she is going to come out of it.
"My heart just dropped. When he said 'stop' I was just devastated, especially when I looked at the parents."
Nursery nurse Valerie Thomas recalled she took a phone call from Child I's mother who asked for an update from the first collapse.
She said: "I went into room 1 and said (Child I's) mum was on the phone, not realising (Child I) was being resuscitated there.
"Lucy Letby said her parents should come in."
The prosecution say the defendant made earlier bids to deliberately harm Child I on September 30, October 13 and 14.
Letby, originally from Hereford, denies all the allegations.
Monday 6th - Wednesday 8th February 2023 - no court
Thursday 9th February 2023
Child I
Dr John Gibbs - Dr Dewi EvansChester Standard article 09-02-2023
A BABY girl was killed by an injection of air into her bloodstream, the murder trial of a nurse has heard.
It is alleged Lucy Letby, 33, murdered the premature-born infant at the fourth attempt by administering the fatal dose during a night shift at the Countess of Chester Hospital's neonatal unit.
The death of Child I, who cannot be identified for legal reasons, in the early hours of October 23, 2015 followed sudden collapses on September 30, October 13 and 14.
On Thursday, February 9, retired consultant paediatrician Dr Dewi Evans gave expert evidence at Manchester Crown Court, in the trial's first day of evidence since the previous Friday.
He stated that, in his opinion, Child I had on the first three occasions been injected with air into her stomach via a feeding tube.
But an "extremely disturbing phenomenon" of Child I's noted "relentless, loud" crying prior to her final collapse led him to believe a different method was used.
The first collapse, he told the court, was "out of the blue".
Dr Evans said: "She was entirely stable right up to the point of collapse.
"My opinion was that (Child I) had been subjected to an infusion of air. In other words, air had been injected into her stomach.
"That interferes with your ability to move your diaphragm up and down, and that interferes with your breathing."
He said there was "striking evidence" from an abdominal X-ray which showed "lots of air".
Dr Evans said he came to the same conclusion that Child I had suffered "splintering of the diaphragm" in the early hours of October 13.
On the following night shift he said her condition deteriorated again "as a result of some kind of event that had interfered with her breathing".
In one report he prepared he wrote this collapse was "also suspicious and suggestive of inappropriate care, most likely due to the perpetrator injecting a large amount of air via the naso-gastric tube".
He told the court an X-ray showed an "astonishingly large amount of air" in her stomach.
Dr Evans said Child I was again stable prior to a sudden deterioration shortly before midnight on October 22.
The court has heard Child I quickly recovered after medical staff gave her breathing support but less than an hour later she deteriorated again.
Nurse Ashleigh Hudson told jurors about Child I's "relentless" and "very loud" crying from her incubator at just before midnight.
Dr Evans said: "Ashleigh Hudson's evidence was very moving because nurses and doctors know what a normal cry sounds like.
"Babies will cry if they are hungry, or if you take a blood test because it hurts.
"This was very abnormal. A different kind of a cry. I interpreted it as the cry of a baby in pain and in severe distress.
"That is an extremely disturbing phenomenon. There was no obvious explanation why she was crying relentlessly and it was very loud."
Asked by prosecutor Nick Johnson KC as to what his conclusion was for the cause of the fatal collapse, Dr Evans replied: "I think she was the victim of air being injected into her blood circulation. This probably explains her crying and distress, and the failure of the medical team second time round to save her life."
Dr Evans agreed with Ben Myers KC, defending, that Child I had recurrent episodes of a swollen stomach and oxygen desaturations during her time at the unit.
But he disagreed with his suggestion that Child I was "in general a very poorly baby regardless of the events we are looking at".
Dr Evans said he thought both collapses on the night shift of October 22/23 were due to injections of air which caused a blockage to the passage of blood.
He said he could not say how much, or how quickly, air was administered as there was "not a great deal of research" available on air embolisms in babies.
Dr Evans denied Mr Myers's assertion that it was "utter guess work" on his part.
The expert said: "It is consistent with what has happened in previous cases here."
Letby, originally from Hereford, denies murdering seven babies and attempting to murder 10 others at the Countess of Chester's neonatal unit between June 2015 and June 2016.
BBC News 9/02/2023 - Lucy Letby: Doctor could find no clear cause for baby girl's death
A consultant paediatrician said he could not understand why a premature baby collapsed and died, nurse Lucy Letby's murder trial has heard.
The 33-year-old is accused of murdering the girl, referred to as Child I, at Countess of Chester Hospital in October 2015.
Dr John Gibbs said he had written in his medical notes that he could not assign "a clear cause of death".
Ms Letby denies murdering seven babies and attempting to murder 10 others.
It is alleged the neonatal nurse attempted to kill the infant on 30 September and again during night shifts on 12 and 13 October.
The prosecution claim she harmed the baby by injecting air into her feeding tube and bloodstream before she eventually died in the early hours of 23 October 2015.
Manchester Crown Court heard how Dr Gibbs was called in urgently after Child I had rapidly deteriorated, arriving on the neonatal unit at 00:06 GMT.
'Abnormal cry'
"The nurses were telling me that she suddenly seemed very distress and was making an abnormal cry and that was about 10 minutes before I arrived," he said.
Child I required chest compressions but these were no longer needed by the time Dr Gibbs arrived on the unit.
He told the court Child I was "fighting" the ventilator, which meant she was resisting and was a "good sign".
But he told the court he "could not understand what natural disease could have affected her that she would have recovered so quickly".
In his medical notes, he had written: "Likely generalised lung collapse - very stiff, small vol [volume] lungs due to distress and crying".
"My suspicion was that she had cried in distress and her lungs had become much smaller and it was hard for her to breathe," he told the court.
But he added: "I admit I was struggling to understand exactly what had happened to [Child I]."
He said he returned home once Child I seemed stable, adding she was "settled, sucking her dummy [and] looking like a well baby when I left".
But within 30 minutes, he had been urgently called back to the neonatal ward as Child I had collapsed again, arriving at 01:23.
The court heard Child I was given CPR and repeated adrenaline but at 02:10 resuscitation efforts were stopped.
"We had been trying to help Child I vigorously for 50 minutes and she still had no pulse of her own, no breathing on her own and we had tried I think eight doses of adrenaline. It's often futile to continue," he said.
Child I was pronounced dead at 02:30.
"I didn't know or couldn't understand why she had collapsed and died," he said, adding he had reported her death to the coroner's office because of this.
"I felt [Child I] needed a post-mortem but it was the coroner's decision," he said.
The court also heard how Dr Dewi Evans, who has been called as a medical expert by the prosecution, believed the baby had been subjected to an infusion of air into the stomach via a feeding tube on the first three occasions.
However, he told the court he believed the baby had been subjected to a different method of harm before her final fatal collapse.
"I think she was the victim of having air injected into her blood circulation and this probably explains her crying and distress and the failure of the medical team second time around to save her life," he added.
During cross examination by Ms Letby's defence team, Dr Evans said there was "compelling evidence" to support his findings and denied that he had shown "prosecution bias".
The court heard Dr Evans was asked to provide a medical report for another unrelated case in June 2021.
The judge presiding over the case later described the report as "worthless", said it contained "partisan expressions of opinion" and stated Dr Evans made "no effort to give a balanced opinion".
Dr Evans told the court the case had nothing to do with Ms Letby's trial and was a "one-off" and something he found "quite upsetting".
He said it was the "only judgement that went against me in a family court in 30 years" and there was "huge demand for my opinion in the family court because of my track record as a witness and an independent witness".
He added that the "persistent fiction that I am a prosecution person" was "pure fantasy".
"It is incorrect, it is incorrect in all of these cases," he said.
The trial continues.
Friday 10th February 2023
Child I
Dr Sandie Bohin - Summary of police interviews
Child J
Mother - Police analyst: Recorded events & messagesChester Standard Live Reporting
9:17am: This is the 15th week of the trial before a jury. The court did not sit on Monday, Tuesday or Wednesday this week due to juror absence, but resumed on Thursday.
10:26am: The trial is expected to resume at about 10.30am - the courtroom at Manchester Crown Court is filling up.
10:33am: The judge is informing members of the jury of a few upcoming days on which the trial will not be sitting. They are February 17, March 13 and March 17. In addition, on February 21, the trial will not be sitting before 1pm.
10:34am: Medical expert Dr Sandie Bohin, who has given evidence before in the trial, has been recalled to give evidence in the case of Child I.
10:42am: Dr Bohin says the cause of the first of Child I's collapses were via air administered into the nasogastric tube. She said it would cause the abdomen to distend and "squash" the lungs, further compromising them. Dr Bohin said, other than the distended abdomen, there were no other symptoms of NEC, a gastro-intestinal condition that Countess staff had considered as a diagnosis. She tells the court there were no pathological reasons why the abdomen was distended, having seen an x-ray.
Dr Bohin said Countess staff did not always fill in the boxes on the chart whether a nasogastric tube was removed or replaced. She adds the nursing staff tend to leave nasogastric tubes in place for several days, as the procedure, while it takes "seconds", can be uncomfortable for the baby. For the symptom of bruising on the baby girl in the second collapse, Dr Bohin rules out the cause of CPR, and "deduced" it was down to an air embolism.
10:43am: For the third collapse of Child I, Dr Bohin says her opinion, based on the x-ray, the collapse, the distended abdomen and the discolouration, was via air administered into the bowel and vein.
10:48am: For the fourth collapse, in which Child I ultimately died, Dr Bohin says the cause of the collapse was an air embolus, via air administered via an IV line. She said the "extremely unusual" level of crying by Child I was "very different" and the baby girl must have been in "severe pain", and that led her to believe the cause had been via an air embolus.
10:55am: Benjamin Myers KC, for Letby's defence, is now asking Dr Bohin questions. He says Dr Bohin had peer-reviewed Dr Dewi Evans's reports. She replies she has given an independent report. Dr Bohin adds she believes Mr Myers is asking if she has merely rubber-stamped Dr Evans's reports, which she says is "less than discourteous", saying she has disagreed with some of his findings and added her own evidence. She says she has reviewed the case and come with her own opinions, and has not "backed up" Dr Evans's reports.
Mr Myers says Dr Bohin would not have come up with the conclusion of an air embolus without first reading Dr Evans's reports. Dr Bohin disagrees. She says she has twice seen the symptoms of air embolus, in one case involving a baby. In one case it was during a complicated medical procedure which had risks, and in which a child was seriously ill, and the child had a cardiac arrest as a result of the air embolus. Dr Bohin is now describing how an air embolus can result in a mottled appearance on the skin and how it can affect the body.
10:59am: Mr Myers suggests Dr Bohin is adapting the air embolism cause to these collapses.
Dr Bohin: "That is not the case." She tells the court she has looked for pathological causes to explain the collapses, and had not been able to find any. Mr Myers says Dr Bohin is 'reaching' for air embolism as a 'catch-all' cause. Dr Bohin disagrees.11:02am: Dr Bohin tells the court when something is "out of the ordinary", it will be noted, as was the case when Dr John Gibbs noted 'mottling' at the time of Child I's first collapse.
11:04am: Mr Myers asks if air embolus presents very specific type of discolourations. Dr Bohin replies the description of the discolourations can vary among medical staff in a cardiac arrest situation when the staff have other priorities and different notes to make.
11:06am: Mr Myers says Child I failed to put on weight as well as she should have. Dr Bohin says Child I was very ill and did not put on weight during her time at Liverpool Women's Hospital. At the Countess of Chester Hospital, feeds were stopped due to complications and that meant she could not put on weight. She says staff at the Countess stopped and started feeds and fortifier, and the reasons for the lack of weight gain were explicable.
11:19am: Mr Myers refers to an event on August 23, 2015 which Dr Bohin had described in her report as "suspicious", when Child I had developed an abdominal distention. This incident was when Lucy Letby was not on duty. Mr Myers also refers to nursing notes from September 5, 2015, in which Child I was a 'well baby' but 12 hours later, 'desaturations' had been recorded, 'requiring intermittent wafting O2 [oxygen]'. The desaturations continued and Child I's oxygen saturation levels dropped to 60%. Dr Alison Ventress recorded a 'profound desaturation, down to 50% sats', and was 'quiet, does cry when disturbed, but not usual strong cry', and 'slightly mottled'. At 11.15pm, Child I had 'another profound desaturation to 50%'. The following morning, at 3.26am, Child I had a 'profound desaturation on ventilator' and Dr Ventress was crash called.
Dr Bohin says this was a baby with an infection who was deteriorating. Child I, had a septic screen, was on antibiotics but continued to slowly decline and was ultimately transferred to Liverpool Women's Hospital. Dr Bohin says these weren't "sudden, catastrophic collapses" but moderate deterioration in a baby which had an infection.
11:21am: Mr Myers says babies such as Child I can decline quite steeply. Dr Bohin says babies don't suddenly collapse and have a cardiac arrest without warning. The subsequent events to September 5/6 were "very unusual".
11:22am: Dr Bohin says Child I had chronic lung disease, something which could be diagnosed under the microscope, but it was not affecting her breathing at that time. Mr Myers says such a condition could lead to an accelerated decline in a baby such as Child I.
11:30am: Dr Bohin said Child I was gaining weight, not as quickly as one might expect, but she had been "very ill" and there had been stop-start points in her feeds.
11:37am: Mr Myers refers to the September 30 incident, in which Dr Bohin says Child I had air administered via the nasogastric tube. Dr Bohin says she does not have any idea how much air would have gone down the nasogastric tube, as it would be "impossible to say". She says the x-rays showed "massive" distention in the abdomen, and "there had been a change". For the October 13 incident, in which Dr Bohin says air was administered via the nasogastric tube and via a vein, Dr Bohin had said she believed the apnoea machine had been switched off or tampered with. She says, having heard nurse Ashleigh Hudson's evidence, Child I was breathing enough, but very slowly, not to have triggered the apnoea alarm. She says that information was not available when she compiled in her report.
11:41am: Mr Myers says Dr Bohin had recorded there was no evidence the nasogastric tube was in situ at the time of October 13. Dr Bohin says staff were "notoriously poor" on noting whether nasogastric tubes were in situ, inserted, replaced or removed. Mr Myers says Dr Bohin had said there was no evidence it was in situ as Child I was bottle feeding, so the tube couldn't be in. "Well, someone could've put one in," Dr Bohin replies.
12:03pm: Lucy Letby's note of 'some bruising/discolouration evident on sternum and right side of chest, ?from chest compressions', written from 19 hours after the incident. Dr Bohin says this note is not from the time of the incident. Dr Matthew Neame's note from the time of the October 13 incident is shown to the court, and Mr Myers says there is 'no reference to any discolouration' in that note, which described the collapse and the efforts to stabilise Child I. Dr Bohin agrees there is not. Mr Myers suggests the bruising appeared later and the discolouration 'does not link to that incident'. Dr Bohin says it does, as bruising is not a result of chest compressions. It was first noted 18-19 hours later. Mr Myers suggests Dr Bohin is using that unrelated evidence to support an air embolism. Dr Bohin disagrees. After a short break, Dr Neame's note is shown again to the court. Mr Myers says he has been made aware the word 'mottled' appears in the note. Dr Bohin agrees she can see it.
12:11pm: Lucy Letby's note from the morning of October 14 is shown to the court. the note includes 'at 0500 abdomen noted to be more distended and firmer in appearance with area of discolouration spreading on right hand side'. Dr Matthew Neame's note, made at 5.55am, is shown to the court. Mr Myers asks if it is a note from 5am. Dr Bohin says it does not say it was written retrospectively. She says if that note was related to 5am, then she had missed it. Mr Myers asks if, from Dr Neame's note showing Neopuff was used, it could have contributed to the distended abdomen. Dr Bohin said it would not have done so to that extent.
12:19pm: Dr Bohin said the team did not have an obvious cause for Child I's deteriorations and she was always going to be transferred out to Liverpool on October 15. Mr Myers refers to the location of the ET tube, NG tube and long line from a report shown to the jury. He says there is early evidence of NEC. Dr Bohin disagrees, saying the report needs to be taken in conjunction with clinical findings showing Child I had a collapsed lung and an over-inflated lung. Child I was reintubated before transfer.
12:23pm: Mr Myers says Dr Bohin reported for the final collapse, Dr Bohin had recorded air had been administered by the NGT and via an air embolus. Dr Bohin says she cannot be clear whether both happened on each event, or whether it was one on each. Mr Myers says Dr Bohin had earlier described how Child I presented at the time. Dr Bohin said Child I had an NGT in place, but that would not have caused a distended abdomen to the extent shown. Mr Myers says the air embolus cause was "very speculative" based on Child I's crying. Dr Bohin says the crying was "very unusual" and air embolus was a "compatible finding" for the cause.
12:25pm: Mr Myers says the repeated collapses would lead a child to become weaker and sadly die. Dr Bohin said Child I recovered so well from the first collapse she was extubated, and that she was doing well, and the first collapse had no relation to how Child I reacted to subsequent collapses.
12:28pm: The prosecution, led by Nicholas Johnson KC, rises to clarify a few of the questions. The events around September 5 are discussed, and Dr Bohin said the incident was not notable as Child I had an infection, so there was an identifiable cause, and it was not NEC. She said it was "not a suspicious event" so had no need to flag it up as one. She tells the court Child I "continued to be unwell and was intubated", and "had a very rocky time for a few days" before "she recovered". The other events, Dr Bohin said, was when Child I collapsed and recovered "very quickly", or in the last case, "sadly", Child I had died.
12:31pm: The prosecution ask about the October 13-14 collapse, and how quickly a nasogastric tube can be inserted and removed, and Dr Bohin confirms that can be done in "seconds". Mr Johnson says there is no evidence "from the records" showing an NGT was in place, but "on the balance of probabilities", that was the cause - Child I receiving excess air via the NGT - which Dr Bohin favoured. Dr Bohin agrees.
12:34pm: That concludes Dr Bohin's evidence for Child I.
12:38pm: Mr Johnson now talks the court through a summary of Lucy Letby's police interviews for Child I. For the first incident on September 30, Letby had no independent recollection of it. She said she did not know whether the distended abdomen was her observation or Child I's mother. For the October 13 incident, she did recall that incident. She said she put on the light when she entered the room with nurse Ashleigh Hudson and noted Child I looked pale. Child I was shallow breathing and gasping, and the apnoea alarm was not activated. Letby could not recall giving Child I treatment prior to that event. For October 14, Letby said she could not recall that shift. Letby could not recall the night when Child I died, other than recalling she had died. She said there was a feeling Child I had been transferred between hospitals too quickly.
12:41pm: Lucy Letby, in a subsequent police interview, said she had sent a sympathy card to the parents, and had taken a photo of the card on her phone. She denied giving air via the NGT. For the October 13 incident, Letby agreed it would have been difficult to see if Child I was pale without the lights being on. She thought she and Ashleigh Hudson had been at the doorway when noting Child I was pale. She could not recall if there was a prior examination. She said “maybe I spotted something that Ashley wasn’t able to spot” because she was “more experienced than Ashley”. She said there was still light coming into the room from the corridor and there would be some natural light. For October 14 and 22, Letby denied causing Child I any harm.
12:43pm: In a third interview, Letby was asked about texts following the October 14 shift, she agreed she had sent texts to a colleague saying Child I looked 'not good' and had asked to be assigned to her care. She was asked why she had searched for Child I's mother on Facebook, and said she did not know, and could not recall doing so.
12:44pm: The court will next hear evidence in relation to Child J.
1:46pm: The trial is now resuming after a lunch break, and will hear evidence from the prosecution in the case of Child J. In the prosecution opening, the Crown say Letby attempted to murder Child J, a baby girl, on the night shift of November 26-27.
1:53pm: The mother of Child J is called to give evidence. She says she had a difficult pregnancy, and following a difficult operation in London, one of her planned twins was lost. She said she gave birth to Child J, a baby girl, at 32 weeks and two days gestation on October 31, 2015. Child J "appeared to be extremely well" and was shown to her after birth, and there appeared to be "no concern" before the baby girl was taken to the neonatal unit. The mother said she visited Child J later at the unit, she was in an incubator. The baby girl was seen in the 10-minute time there to produce a bit of brown bile. Child J was then taken to Alder Hey by ambulance. The mother said she was told there were concerns about Child J's bowel at the time.
1:58pm: The mother said it was discussed afterwards that Child J had 'NEC' [necrotising enterocolitis: a serious gastro-intestinal disorder where a portion of the bowel becomes inflamed] and had emergency surgery at Alder Hey. The bowel was 'cut', 1cm was removed - "a little amount", and the decision was made to give Child J two stomas. Child J returned to the Countess of Chester Hospital on November 10, and the mother recalls being there frequently., establishing a routine. Child J was "absolutely" progressing well, going from being treated in room 1 (most intensive treatment), to room 2, to room 3, to room 4, over the course of four weeks in November.
1:59pm: Child J's mother recalls there were issues with the baby girl's weight gain, which 'concerned her' and she relayed those concerns "frequently". She said those concerns were treated "not very seriously - they weren't overly concerned". There were "quite a lot of challenges" with the stoma management.
2:03pm: Child J's mother says, between November 10-27, there were no major concerns with the stoma management, but the bags were not lasting as long as expected, and breastfeeding was impractical, but attempts at breastfeeding were made as Child J was doing well. She tells the court the approach of staff at the Countess was different to Alder Hey. While Alder Hey was 'inclusive', the communication did not feel the same at the Countess.
2:07pm: Events leading up to the morning of November 27 are discussed, when Child J collapsed. Child J's mother said the family were "really excited" to get Child J home, as she was off the heart monitor, and the mother was at the hospital ready to provide daytime cares, having also been involved in the night-time process. The court hears it was 'a dry run' for life at home. Overnight on November 25-26, Child J's mother was at the hospital, attending for cares, including stoma bag management. On November 26, Child J's mother went and stayed home, intending to return as usual at 8am on November 27. She said 8am would be after the handover, and staff preferred parents not to be on the ward at the time of the handover.
2:08pm: The mother recalled receiving a telephone call on the morning of November 27 telling her Child J had collapsed, and to attend hospital as soon as possible. She said that would have been about 7.10am. The mother attended the hospital as quickly as she could with her husband. Child J was in room 2 in a 'hot cot', connected back up to a monitor and looked "very floppy...pale, yellowy in colour and not very responsive".
2:10pm: Child J's mother said she was "totally and utterly shocked because prior to this, she was extremely well, she was coming home...we were preparing for her to come home. "Other than the weight gain, everything was fine." Child J's father spoke to Dr John Gibbs and the mother recalled joining in the conversation, being "very stressed about what I was seeing and experiencing".
2:11pm: After the collapse, Child J's mother said nurses led the care, and the parents stayed overnight. It was established there was not an infection - it was "unknown at that stage", the mother tells the court, and Child J recovered "quite quickly". By the afternoon of November 28, Child J was "back up to full feeds", the mother tells the court.
2:14pm: In the following weeks after that, Child J had another collapse around December 16, 2015. "That was when we really started to see issues with the stomas and the bags", the mother tells the court, with the bags not lasting anywhere near as long as before, and would stop working as they should. After the second collapse, there were "concerns" when Child J was pressed in the abdomen, she would wince and feel pain, so Child J was transferred to Alder Hey to have the operation reversed and the stomas were closed, the bowel reattached. On January 5, 2016, Child J returned home.
2:24pm: Mr Myers, for Letby's defence, asks the mother about Child J's birth, and that 'things seemed to be all right'. The mother agrees. The mother said she saw the brown bile from Child J's mouth and informed staff at the Countess. She agrees staff were "concerned". Mr Myers says if there was a point when they were asked if Child J should be Christened. The mother agrees. The court hears Child J had an 11-day stay at Alder Hey, during which she had a bowel operation. The details of the procedure and how to use the stoma bags are relayed in court, and the mother says she and her husband had it explained to them. The mother said she would not say the stoma bags procedure was explained as well to them by Countess staff.
Mr Myers asks if the mother was told 'this could be a bit of a rollercoaster - that babies could go up and down' for Child J. The mother replies she is not sure when that was said to her, and could have been after Child J collapsed. The mother says Alder Hey checked with the Countess of Chester Hospital to do the recycling of the stomas, and the Countess hospital had said yes, but did not seem to be as prepared.
The mother, having looked at a statement she gave to police, says that on reflection, the Countess staff were not as prepared for such procedures, and the 'time-consuming process' meant she offered to help with the stoma and the bags. She adds that without the expertise of her husband, she would not have been able to position the stoma bags correctly, and without the prior experience, it would be considered a 'challenging' procedure. The mother tells the court she felt if she raised concerns on the stoma care, they were not taken as seriously by Countess staff as the staff at Alder Hey.
2:26pm: The mother says there were concerns raised 'frequently' about the lack of weight gain for Child J, and they were raised with Countess staff. Those concerns were "not met with any changes - not taken very seriously", the mother tells the court. After the first collapse, Child J's mother says they were much more alert on medication as 'things were missed'.
2:30pm: The mother says there was "a general concern" for Child J for an increased risk of infection. Mr Myers asks if there was a case when Child J was not tidied up. The mother replies 'yes', as there was one case where she arrived to find Child J's bottom had waste visible, and was wrapped around with a towel. She raised the issue with a consultant, after asking staff "what would you do in my situation?". The mother said she felt "pushback" on raising those concerns.
2:34pm: Intelligence analyst Kate Tyndall has returned to talk the court through events for Child J, who was born at 3pm on October 31, 2015, weighing 3lb 12oz. Child J was admitted to the neonatal unit 10 minutes later. A picture was taken of the baby girl. She remained at the Countess until 4am on November 1, being transferred to Alder Hey, before coming back to the Countess on November 10, being admitted to the neonatal unit by Lucy Letby.
2:35pm: The same day, Letby messages a colleague saying "It's chaos here" and she had had a row with another colleague.
2:42pm: A selection of messages, recovered from Letby's phone, are shown to the court for the period from November 10-26. Letby sends a lengthy message to her colleague explaining why the unit was 'chaos' and why she had a disagreement with a colleague, adding staff were "peeing her off". Her colleague replies: "Nothing like a bit of team spirit eh! x" Letby apologises for her rant, saying: "Just really gets me down sometimes and some...want the easy life"
2:51pm: Letby asks a colleague on November 16 about how often a procedure for the Broviac line for Child J needed to be carried out. She receives a reply that it is carried out weekly. Letby says she had three missed calls on November 25, having been to Las Iguanas and was at salsa, saying no-one at the unit knew how to administer immunoglobin, and they rang her. Her colleague sympathises, saying they should not be ringing staff not on duty, but should be contacting Liverpool Women's Hospital first.
2:54pm: The events of November 26 are now being talked through the court. At 10.30am, a doctor's note says Child J was 'pink, well perfused, no respiratory distress' 'Abdomen- soft. Mum says mild distention soft abdomen. Stoma looks healthy'. The note adds 'if [increased] distention to inform' as the plan, along with the feed for expressed breast milk and donor.
2:56pm: Letby messages a colleague saying 'staffing really needs looking at', before messaging colleague Jennifer Jones-Key to say 'sounds like you had a mad day'. Letby adds the situation is 'just not manageable'.
3:00pm: Letby adds: "It's a nightmare isn't it...especially with no management x" Jennifer Jones-Key said the staff [on duty] were going to ring Letby or Yvonne Griffiths the previous night [regarding how to administer immunoglobin], but thought that would have been done so sooner.
3:12pm: Letby adds the staff there should not have been in that position. She adds, for her November 26-27 night shift: "Ah well. Hopefully be a bit calmer for me tonight lol x"
3:15pm: A colleague messages Letby at 5.16pm: "U well rested for work? x"
Letby replies: "Yep I've had a chilled day and slept well..." She adds: "Ready to face anything" with a strongarm emoji, before discussing about being contacted the previous night, and querying why she had been contacted when staff on duty had other lines of enquiry, such as Liverpool Women's Hospital or the transfusion department.3:20pm: Letby, as she sets off to work, messages her colleague: "Off to the mad house x" with a neutral face emoji. Once inside, she messages the colleague to say she is in room 3 of the neonatal unit for the night shift. A shift rota for that night is presented to the court. There are two babies in room 1, two babies in room 2, two babies in room 3 (both designated nurse Letby), and two babies in room 4, one of them being Child J. In addition, there are two babies in transitional care, and two babies whose location could not be confirmed from the records.
3:26pm: Nurse Ashleigh Hudson records, for Child J at the November 26 night-shift handover: 'Observations satisfactory as charted...Broviac remains in situ...[Child J] appears to be in no pain or discomfort.' Letby received and sent messages between 7.36pm and 10.53pm, but not related to Child J. At 1.57am on November 27, swipe data shows Letby recorded as entering the neonatal unit, at 3.47am and at 4.29am.
3:31pm: At 4.40am, an apnoea/brady/fit chart records Child J having an episode of apnoea, heart rate down to 100, lasting for three minutes. At 5.03am, a desaturation to '30s' is recorded, heart rate to 100, lasting two minutes. In each event, a Neopuff device is administered. Nurse Nicola Dennison records Child J looking unwell at 4.40am. In an untimed note [written retrospectively at 7.37am], Child J is moved from nursery room 4 to room 2.
3:34pm: Letby says, in a message to a colleague, she had not had a good shift, as Child J had '2 profound desats' and there were 'only 5 staff' on duty. The colleague replies: 'We closed again then? x' Mr Johnson explains to the court 'closed' by this definition means the unit would be closed to new arrivals, not closed entirely. Letby confirms the unit is closed until they can get someone in.
3:36pm: There is an event timed as 6.56am which marks Child J's desaturation. A retrospective note created by Mary Griffith, referencing Lucy Letby, is made at 7.11am. The note says '[Child J's] monitor went off at 6.56 myself and L Letby attended. Found baby with pale hands and baby very ridged...'
3:41pm: A note is made at 7.15am recording that the parents of Child J are informed of the collapse and to come to the hospital as soon as possible. Child J had a further collapse at about 7.24pm. Dr John Gibbs records the event in his notes. Resuscitation efforts are made and a range of medication is administered, while observations are recorded and an x-ray made.
3:42pm: Letby is recorded as using her swipe card at the neonatal unit access door at 8.55am.
3:47pm: Lucy Letby messages Jennifer Jones-Key just before 10.30am: "Wow it turned manic - left at 9.15 but others still there."
The reply: "Warned you..don't know what it is", adding that things seem to go "pear-shaped".3:55pm: Jennifer Jones-Key messages Letby saying, of the staffing situation, 'more staff will just go off sick'. A colleague of Letby messages her on the afternoon of November 27 to say: 'Oh and Tony Chambers n some woman turned up earlier! x'
Letby replies: 'Gosh it's mad. At least things are moving in right direction. Is it bit calmer now? Still only 5 tonight? Hope Tony got stuck in and helped!!'4:00pm: Letby is on a night shift on November 27-28. She recorded Child J's vital signs and her fluids. Nurse Mary Griffith messages Letby to say she had left the hospital at 9.45am, getting back home at 10.30am, adding she hopes Letby has a better shift tonight.
Letby replies: "You must be tired. Thanks for staying....still busy as only 5 on. [Child J] quiet hasn't done anything else abnormal and xray etc ok..."4:03pm: Notes from a doctor on November 28, 2.30am, for Child J record '...no respiratory distress...' The plan was 'continue to slowly increase feeds...to achieve full feeds by 1800 today'.
4:06pm: Letby records further observations for Child J at 5.06am on November 28, with 'shallow breathing observed at times' and, in a family communication note, Child J had been 'out for cuddles' with parents, who 'seemed happier' that Child J was recovering and feeds were gradually being increased.
4:08pm: Child J continued to be cared for at the Countess of Chester Hospital's neonatal unit until 3.30am on December 18, 2015, when she was transferred to Royal Manchester Children's Hospital.
Monday 13th February 2023
Child J
Dr John Gibbs - Dr Stephen Brearey - Nurse Mary GriffithChester Standard article 13-02-2023
A BABY girl allegedly harmed by nurse Lucy Letby suffered two unexplained seizures within 30 minutes, a court heard.
Letby, 33, was on duty at the Countess of Chester's neo-natal unit when the blood oxygen levels of the premature-born infant unexpectedly dipped.
Giving evidence on Monday, February 13, consultant paediatrician Dr John Gibbs said two "profound" desaturations around 5am on November 27, 2015 were "alarmingly low".
He told Manchester Crown Court that the youngster, Child J, was stable for weeks after she previously underwent bowel surgery a day after her birth.
Child J recovered quickly after she received breathing support, but more desaturations followed at 6.56 am, together with a marked fall in heart rate.
Dr Gibbs also noted all of Child J's limbs were "stiffly extended with her hands clenched".
He said the stiffness took 10 minutes to settle which was a "reasonably long seizure".
More breathing support, via a facemask, led to an improvement – but a further similar episode took place at 7.24am, jurors were told.
Dr Gibbs, now retired, said: "Again, (Child J's) oxygen and heart rate dropped and she needed support for her breathing just as in the first episode.
"This episode was much shorter. She did display the stiffness of all her limbs and clenches of her hands, and on the second episode her eyes deviated to the left. It stopped after three or four minutes."
He said that Child J had not suffered a seizure either before or since.
Simon Driver, prosecuting, said: "You cannot be certain as to what was the cause?"
Dr Gibbs replied: "All the investigations did not reveal any causes for her seizures."
Ben Myers KC, defending, said: "It's not possible to say for sure whether the seizures caused breathing difficulties or breathing difficulties caused the seizures?"
Dr Gibbs said: "That's correct."
Mr Myers went on: "To be clear, you favour breathing difficulties first because your assessment was the drop in oxygen (levels) came before seizure?
Dr Gibbs said: "Yes. Exactly why and how the oxygen dropped, I don't know."
Fellow consultant Dr Stephen Brearey told the court: "She (Child J) normalised very quickly over the course of the day and all the investigations we had undertaken couldn't identify why she had the desaturations or explain why she had a seizure.
"I do know hypoxia causes seizures so that would be possibly the most likely cause.
"There remains the question why was (Child J) hypoxic when two or three weeks beforehand she had been breathing normally in air and there was no suggestion of infection.
"In fact, we stopped antibiotics 36 hours after starting them because there was no evidence of infection in the blood tests and she remained well for weeks afterwards."
Earlier, nurse Mary Griffith – who worked more than 40 years at the Countess of Chester before retiring in 2016 – agreed with Mr Myers that Letby was "knowledgeable", "caring" and "thorough" in her job.
She also agreed there seemed to a "very high admission rate" to the neo-natal unit around 2015/2016.
Child J was discharged home in January 2016 and was described as progressing "very well" at her final outpatient clinic more than a year later.
Letby, originally from Hereford, denies murdering seven babies and attempting to murder 10 others between June 2015 and June 2016.
BBC News 13-02-2023 - Lucy Letby: Baby making progress before collapse, trial hears
A baby girl who was allegedly attacked by nurse Lucy Letby was making "steady and encouraging progress" before she collapsed, a court has heard.
Ms Letby is accused of attempting to kill the girl, known as Child J, at the Countess of Chester Hospital in 2015.
Manchester Crown Court heard how medical tests carried out shortly after her collapse found "nothing to explain why she had deteriorated".
Ms Letby, 33, originally of Hereford, denies all of the charges against her.
Child J, who cannot be named for legal reasons, was born at 32 weeks plus two days gestation at the Countess of Chester Hospital in October 2015.
The court heard Child J had a condition called necrotising enterocolitis, where a portion of the bowel becomes inflamed, as well as a perforated bowel.
She was transferred to Alder Hey Children's Hospital in Liverpool for surgery.
Child J needed two stomas, where part of the bowel is left outside the body to allow it to rest after surgery.
The baby girl returned to the Countess of Chester Hospital on 10 November 2015 with her condition described as stable, the court heard.
Dr John Gibbs, a consultant paediatrician, said Child J had been making "steady, acceptable and encouraging progress".
He added that within two-and-a-half weeks, Child J had moved on to bottle feeds and was "fine" and without any respiratory complications.
"It was a challenge managing Child J's stomas because we rarely had babies with a stoma needing recycling feeds [at the Countess of Chester Hospital]," he said.
He added this was discussed with the neonatal team at Alder Hey Children's Hospital, who dealt with stomas "fairly frequently", and they "were satisfied with her progress".
But in the early hours of 27 November 2015, Child J suffered seizures and four desaturations with her heart rate also dropping on the third and fourth occasion, the court heard.
"Both occurring together is of more concern than one occurring by itself," Dr Gibbs told the court.
Dr Stephen Brearey, who reviewed medical tests carried out that day, said "nothing explained" why the infant had collapsed.
"She [Child J] normalised very quickly over the course of the day and all the investigations we had undertaken couldn't identify why she had the desaturations or explain why she had a seizure.
"I do know hypoxia causes seizures so that would be possibly the most likely cause.
"There remains the question why was [Child J] hypoxic when two or three weeks beforehand she had been breathing normally in air and there was no suggestion of infection.
"In fact, we stopped antibiotics 36 hours after starting them because there was no evidence of infection in the blood tests and she remained well for weeks afterwards."
He reviewed further tests two days later on 29 November 2015 where he described her as in a "good condition".
"I didn't have any concerns at that stage," he said.
"Looking back on it now we didn't have an explanation for the events on 27 November.
"Sometimes these can show themselves later down the line."
Mum shocked at baby's collapse, Letby trial hears
Baby in extreme pain as she died, Letby trial hears
Doctor puzzled by baby's death, Letby trial hears
But he added "there was nothing of anything of concern at that time" following investigations undertaken by the hospital and discussions with Alder Hey Children's Hospital.
Earlier, nurse Mary Griffith - who worked more than 40 years at the Chester hospital before retiring in 2016 - agreed with Ben Myers KC, defending, that Ms Letby was "knowledgeable", "caring" and "thorough" in her job.
She also agreed there seemed to a "very high admission rate" to the neonatal unit around 2015-2016.
Child J was discharged home in January 2016 and was described as progressing "very well" at her final outpatient clinic more than a year later.
Manchester Crown Court previously heard the baby's collapse was consistent with some form of obstruction of the airways, such as smothering.
Ms Letby denies murdering seven babies and attempting to murder 10 others.
The trial continues.
Tuesday 14th February 2023
Child J
Dr Dewi Evans - Dr Sandie BohinChester Standard article 14-02-2023
TWO seizures suffered by a baby girl did not happen naturally, the murder trial of a nurse has heard.
Lucy Letby, 33, is accused of attempting to murder the premature-born infant in her cot at the Countess of Chester Hospital's neonatal unit.
Child J had two "profound" drops in blood oxygen levels at about 5am on November 27, 2015.
Two further episodes took place two hours later, Manchester Crown Court was told, when her heart rate also plunged and she showed signs of a seizure.
On Monday, consultant paediatrician Dr John Gibbs said her limbs stiffened on the latter two occasions and her hands were "clenched".
He said the first fit was "reasonably long" and took 10 minutes to settle, while the second stopped after "three or four minutes".
Tests showed no signs of infection and did not identify a cause for the seizures, the court heard.
Giving evidence on Tuesday, expert medical witness Dr Dewi Evans told prosecutor Nick Johnson KC: "The first pair of collapses were unexpected because she was nice and stable before that.
"The second pair of events were more serious and required more in the way of resuscitation, but again were unexpected and I noted the markers for inflammation were normal which tended to rule out infection.
"The second pair coincided with what the doctors describe as a seizure or a fit. This is indicative of something going wrong with the brain.
"My opinion was that (Child J's) brain was deprived of oxygen for a sufficient level of time to cause hypoxia ie loss of oxygen to the brain causing fits.
"As far as I know this was the only occasion when she had seizures and the cause of this was the hypoxia, the lack of oxygen to the brain."
Mr Johnson asked the retired consultant paediatrician: "So far as the hypoxic incidents that had caused these seizures were concerned, could you identify any natural process that might have caused that?"
Dr Evans replied: "No, I could not. There was no reason why she should suddenly become hypoxic."
Mr Johnson went on: "If infection had been the cause of her rapid decline would she have recovered as quickly as she did?"
Dr Evans said: "I don't think she would. Babies who develop an infection usually recover over a period of days."
Dr Evans agreed with Ben Myers KC, defending, that he could not rule out infection "for sure".
However fellow expert witness, consultant paediatrician Dr Sandie Bohin, said she had excluded infection.
She told the court: "(Child J) was a well baby. She was ready to go home. Babies who are ready to go home do not have major desaturations which lead to prolonged resuscitation.
"These were completely unexpected and she required the Neopuff (face mask) ventilation for a long time before she came round and was well again.
"I thought that seemed extremely unusual – the speed of the collapse, the longevity of the resuscitations and the fact that she seemed to recover quite quickly.
"That is not the way that infection normally plays out."
Dr Bohin noted that Child J was clinically well and back to her normal self before she even received antibiotics.
She said: "I exclude infection. I don't think that was the cause of her collapse."
Dr Bohin told Mr Myers she had not been able to identify an "obvious cause" for her collapses.
Child J had previously undergone bowel surgery a day after her birth but medics have said she was stable in the weeks that followed.
On the morning of November 27 she was being cared for in nursery room 4 in readiness for returning home to her parents.
Child J was later moved to room 2 for closer monitoring ahead of the second pair of collapses.
She eventually was discharged in January 2016 and was described as progressing "very well" at her final outpatient clinic more than a year later.
Letby, originally from Hereford, denies murdering seven babies and attempting to murder 10 others between June 2015 and June 2016.
Wednesday 15th February 2023
Children L & M (twins)
Police analyst: Recorded events & messages - Parents' statements - Midwife's statement, Dr Sudeshna Bhowmik (Paediatric trainee) - Nurse Amy Davies - Dr Anthony UkohChester Standard Live Reporting
10:29am: The trial is due to resume imminently.
10:39am: Prosecutor Nicholas Johnson KC tells the jury the case is now proceeding to the cases of twins, Child L and Child M. This is slightly out of the order in the sequence of the trial, chronologically, so far. The case of Child K will be heard slightly later in the trial. Intelligence analyst is talking the court through the sequence of events for Child L and Child M, twin boys born on April 8. Child L was admitted to the neonatal unit at 10.30am, and had observations taken by Lucy Letby, with a blood sugar reading of 1.9 recorded at 10.58am. He was treated with a 10% dextrose (sugar) infusion.
10:41am: Lucy Letby's note, written in retrospect at 5.42pm, noted the blood sugar reading of 1.9, with the registrar commencing dextrose and expressed breast milk. At 12.14pm, the blood sugar reading had risen to 2.5.
10:45am: Lucy Letby records communication with Child L and Child M's parents: "Parents were shown babies in theatre and had a quick cuddle....Photographs given and visiting hours discussed. Daddy visited the unit and had cuddles."
10:47am: For Child L, a blood sugar reading of 5.8 is recorded at 4pm.
10:52am: Letby records for Child L at birth "Initially had some recession with a raised respiratory rate, quickly normalised and remained self ventilating in air. Blood gases good... "2 Hourly feeds, NG/bottle. Minimal aspirates obtained..." Recording communication with the parents: "Parents updated by myself on CLS and photograph taken....fully updated on care by myself and reg Bhowmik. Aware of need for septic screen..." A 6pm blood gas reading records blood sugar of 3.3
10:57am: Letby messages a colleague at 6.15pm - "Unpacking! Stuff everywhere lol! May do an extra shift this weekend x" The court previously heard Letby had recently moved into a home near the hospital. Letby messages her mother: "Think Im going to do tomorrow [Saturday, April 9] as an extra but go in a bit later." Child L's blood sugar reading at 9pm is 2.3. Letby's colleague Sophie Ellis messages her: "How's the house pal? Xxx"
Letby: "Hey, it feels a bit weird having a whole house but it's good thanks, although stuff everywhere as moved in properly on Tue and been at work Wed, Thurs and today...", followed by a monkey emoji with its hands over its eyes.
Sophie Ellis: "...it'll feel more homely once you've sorted everything out." She also asks about how busy the unit is.
Letby: "...Unit is busy, no-one particularly unwell just volume and few people off sick. I prefer 4 days to 4 nights..." Letby adds: 'We've got nice mix of babies at the mo really. Shift goes quick anyway!'11:02am: Child L's blood sugar reading is 2.2 at 10pm, then 3.6 at midnight. Further medications are administered throughout the night. Agency nurse Tracey Jones records notes for Child L from the night shift, noting the cannula was knocked out by the baby boy during the night so was reinserted. There had been no contact with the parents during the night.
11:04am: For the day shift on April 9, 2016, Lucy Letby is a designated nurse for two babies in nursery 1. Mary Griffith is the designated nurse for Child L and Child M, who are the other two babies in room 1. Four babies are in room 2, three in room 3 and four in room 4. There are seven designated nurses for the neonatal unit babies in total.
11:06am: Child L records a blood sugar reading of 1.9 at 10am, pre-feed. Nurse Mary Griffith records notes, written retrospectively, saying the IV dextrose [infusion] was increased for Child L.
11:08am: Letby messages colleague Alisa Simpson at 10.34am, wishing her good luck at picking the horses at the Grand National that day, and that her feet don't get too sore. Child L's blood sugar reading is 1.6 at 11am.
11:17am: A handwritten entry for hypo screen results at noon, not attributed to a name, record results for Child L. Child L's blood sugar reading is 1.6 at noon, pre-feed. Letby co-signs a 10% dextrose infusion for Child L, around noon. Notes for Child M record that designated nurse Mary Griffith took a break around 12.30pm. Letby is engaged in messaging people between 11.12am and 12.33pm. Letby messages Alisa Simpson shortly afterwards: "Oh good hope you have a fab time. Im in work doing an extra! x" Letby also messages her mother, asking if her father was betting on the Grand National, and if so, to put a bet on grey horses for her. Her mother replies that has already been done.
11:25am: The court hears Letby continues to be involved in messaging, including a group message to colleagues and friends: "Sorry guys mad 4 busy days in work..." then invites the three people to crash at hers, apologising she hasn't fully unpacked yet. She adds: "Got magnum prosecco and vodka woop. No disco ball but sure we can manage. x" Child L's blood sugar reading is recorded as 2.0 at 2pm, and 1.5 at 3pm. Letby is a co-signer for the administration of medication at 3.35pm. Mary Griffith records a blood sample was taken from Child L at this time, which was taken to the Royal Liverpool Teaching Hospital for analysis. The prosecution say the blood sample had a very high insulin level recorded, and a low level of C-peptide. Child L was also given a bolus of dextrose, prescribed at 3.35pm and administered at 3.40pm.
11:30am: A note from the hospital's pathology department records the blood specimen sample for Child L. The blood was "taken for lab but due to emergency not poded at once", nurse Mary Griffith records. That one emergency identified in the neonatal unit, the prosecution tells the court, was for the twin brother, Child M's "dramatic collapse".
11:34am: Child L's blood sugar reading at 4pm is 1.5. Child M's collapse is recorded at this time. A crash call is put out. Friends message Lucy Letby around this time, saying they can have "an unpacking party". For Child L, the dextrose administration is increased to 12.5%, from 10%. Child L's blood sugar reading at 5pm is 1.7, which was "still very low", the prosecution say.
11:38am: Letby's mother messages Letby at 5.28pm telling her: "You've won rule the world :-D xxx" Child L's blood sugar reading at 6pm is 1.9. Letby responds to a colleague at 6.01pm: "Haha why not!! Work has been s***e but...I have just won £135 on Grand National!!" She also sent a group message: "Unpacking party sounds good to me with the flavoured vodka...Just won the Grand National!"
11:44am: The pathology records the lab specimen of a blood sample for Child L. Among the blood test results sought for the sample are insulin and C-peptide. The insulin level is recorded as 1,099, and the C-peptide is recorded as 264. These readings are entered into the system on April 14, having obtained the results from Liverpool. The C-peptide "should be 5-10 times the level of insulin", but the ratio is recorded as 0.2.
11:46am: Child L is recorded to have hypoglycaemia [low blood sugar]. Doctors record the hypoglycaemia continued despite the regular infusions of dextrose throughout the day.
11:50am: Child L has a blood sugar reading of 2.0 at 8pm. Child L's blood sugar at 9pm is 2.4. Letby records notes for Child M at 9.22pm.
12:13pm: Child L's blood sugar reading at 10pm is 2.3. A colleague of Letby, Belinda Simcock, messages her at 10.11pm: "Thanks for listening, I'm ok x"
Letby: "Don't need to thank me, glad you felt able to tell me..." Child L's blood sugar reading at midnight is 2.1, and remains "low" at 2.1 at 2am. A long line is inserted, with an x-ray taken, and medication administered. The blood sugar reading at 4am is 2.3, and 2.2 at 6am. The glucose is further increased, but the blood sugar reading "remains stubbornly low" at 2.2 at 7am. It remains at 2.2 at 9am. Letby receives a message from Yvonne Farmer asking if she wanted to do more overtime shifts on Sunday night, Monday day or Monday night, appreciating she may be tired, with Letby responding: "Sorry but need some days off now." She adds she could be on call for nights, and would be free for Thursday day/night shifts. Child L's blood sugar reading at 2pm on Sunday had "normalised" at 3.0.12:16pm: Letby refers to her previous shifts as "not nice" in a message to Jennifer Jones-Key. Jennifer Jones-Key says Letby 'hasn't got many nights' coming up on the rota, adding she likely won't see Letby as she works mainly nights herself. "We never see each other if we do work together as always mad shifts".
12:26pm: Child L was still receiving 15% dextrose through the afternoon of Sunday. A nursing note made by Laura Eagles that afternoon records: "Blood sugars maintained...remains on 15% dextrose via long line...very unsettled at times." The family had been kept updated of the situation, according to a family communication note. Child L's blood sugar levels were "normal" at 2.8 at 5pm. Samantha O'Brien becomes the designated nurse that night for Child L, and the 15% dextrose administration continues through the night. The blood sugar levels are 2.7 at 9pm, 2.9 at 11pm, 2.7 at 2am. Samantha O'Brien, in her nursing note, records: "...1% glucose infusing via long line in left leg,. 3 hourly blood sugars, all have been above 2.6 so far this shift. Plan to continue [current medication administration]... "Baby unsettled at times, settles with comfort measures." The blood sugar level is 2.9 at 5am on Monday, April 11. Letby messages a colleague at 8.45am, saying: "The unit is in dire way with staff," highlighting which trained staff were on duty and who else was on in the last shift, and who was off at that time. A colleague replies, in her message: "that's terrible" Letby replies the overall situation was "not good", "mad and poor skill mix".
12:31pm: Child L's blood sugar readings are 2.8 at 11am. Dr Huw Mayberry, in a clinical note, records the feeds/fluids for Child L, which were increased due to low blood sugar and falling sodium levels. Child L's blood sugar at 3pm is 3.5, remaining at 3.5 at 5pm. Nurse Belinda Simcock said registrar Mayberry was aware of the 3.5 readings, and if they continued to remain above three, then feeds would be increased. The blood sugar increases to 4.7 at 7pm.
12:32pm: Child L continued to be cared for at the hospital's neonatal unit until May 3, and was then discharged.
12:36pm: The court is now hearing a statement from the mother of Child L and Child M, who had had a "routine pregnancy" until a stage when she was "not well". She recalls being "surprised and shocked" at being told she had to be admitted to hospital. She stayed there for 15-17 days and was asked if she was going to deliver naturally or via a C-section. Staff had looked through her file and were "worried", so the decision was made for the birth to take place, via c-section, on April 8. The babies, weighing 3lb each, looked "very nice". The family were taken to the neonatal unit to see them in room 1 the following day and the family were "happy", and at that time it was not known what they were going to be called - deciding on the names a week later.
12:39pm: Later, the mother was asked by a nurse named Yvonne to come down as soon as possible. She came down and saw Child M had collapsed and chest compressions were under way. She was praying to see her, asking God to see them. Child L was ok on the other side of the room, and Lucy Letby was present. She said her mind was "totally blank" and she just prayed. After what felt like "hours", Child M had stabilised. Each day, the mother would come down daily to see the twins, who had stabilised. Three weeks later, the mother was discharged, and she continued to visit daily until the twin boys were discharged. They hadn't put much weight on and were small, but otherwise healthy. Child M had "no after effects for what happened to him".
12:44pm: A statement from the father is now being read out. He said he was "shocked" at the news his wife needed to go to hospital due to concerns over the pregnancy, and she stayed there for "over two weeks" before the C-section birth took place. The doctor said the babies looked "very healthy" before being taken to the neonatal unit by Lucy Letby and another nurse. He saw the twins a couple of hours later and they were "both still fine". The following day, the family visited - "we were both proud parents, and very happy". Within 10 minutes of being on the ward, the father "rushed" back to the neonatal unit, where he saw a doctor doing chest compressions on Child M. He said: "It was a very distressing image, and one that still is in my mind." The staff said they didn't know what had happened to Child M, and Child M had had a heart attack. Child M later stabilised after about half an hour, and there were no further issues with the twins in subsequent care. Child M had a brain scan, with 'no damage' recorded. The twins were "only on the unit because they didn't weigh enough", and it was "a relief to get the boys home".
12:47pm: A statement from the midwife is now being read out to the court. She said there was concern one of the twins was not growing as he should have in the womb, so an elective surgery took place so there were no further complications with the lack of growth. Both babies "were in good condition" and there was time for "a quick cuddle" with the parents before the twins were taken to the neonatal unit "without any problems".
12:49pm: Both twins began crying after birth, one of them requiring a little extra help to do so. The 'Apgar score', which records the conditions of the babies shortly after birth, recorded 10/10 scores for both twins at 10 minutes after birth. Child M has a low oxygen saturation rate, but he had that rectified with breathing support.
12:57pm: Dr Sudeshna Bhowmik, who was working as a paediatric trainee at the time in April 2016 at the Countess of Chester Hospital, has been called to give evidence. She says, outside of the clinical notes, she has no memory of the twins, Child L and Child M. She confirms, from the notes, she was present at the birth of the twins, citing an IV line for Child L on April 8 at 11.15am, which was "quite a routine procedure to be done on the neonatal unit". The baby was "generally well", although the breathing rate was "a little elevated". The court hears that was not a concern as that would usually be the case for babies born via C-section. The weight of 1.465kg [3lb 3oz] was "quite low", and the blood sugar of 1.9 was "a little bit low", which can be found in premature babies who are quite small. With glucose feeds, that would "stabilise".
1:00pm: The plan was to commence dextrose via IV fluids and feeds via expressed breast milk, to see if the latter would be tolerated 'in small amounts'. She added at that time, there was no need to administer antibiotics. Dr Bhowmik tells the court with Child M showing signs of jaundice, however, that plan may need to have been revisited. The plan was also to repeat the blood sugars in half an hour.
2:02pm: The trial, having had its usual lunch break, is expected to resume shortly.
2:07pm: Dr Sudeshna Bhowmik is continuing to give evidence. She says most pre-term babies will have IV fluids, and this was altered for Child L because of the baby boy's weight and glucose levels.
2:17pm: Benjamin Myers KC, for Letby's defence, asks Dr Bhowmik to clarify the blood sugar readings for a healthy baby. 2.6 and above is healthy. Mr Myers says Child L was recorded as having a 1.9 reading a couple of hours after birth. He asks Dr Bhowmik questions about a 'hypoglycaemic pathway'. Dr Bhowmik says the correct course at the time would have been to start treating hypoglycaemia at the neonatal unit via IV fluids. She tells the court she does not recall when the bag of IV fluids was put up, or who administered that bag.
2:20pm: An infusion chart is shown three records of the first 10% dextrose infusion. The first two are crossed out, with the third being the dose which was administered. The judge asks to clarify that the only difference between the three records is the rate of infusion for the 10% dextrose bag. Dr Bhowmik confirms that is correct. That concludes Dr Bhowmik's evidence.
2:43pm: The court is now hearing evidence from Amy Davies, a neonatal practitioner who was employed in the neonatal unit at the Countess of Chester Hospital in April 2016. At the time, she was in Band 6. She says she does not have any independent recollection of Child L. From her notes, she was on the day shift on April 8, 2016, as shift leader. Lucy Letby was the designated nurse for Child L on the 8th, and Ms Davies confirms she assisted in the care. She is asked if there was a specific pathway for babies with low blood sugar. Ms Davies confirms there was, and would involve giving milk before giving IV fluids with glucose, but each case differed. In this case, a discussion would have taken place with the doctor, Ms Davies confirms. She said it was a decision which would not put the baby at risk, but was an alternative pathway. Asked if she had any concerns about that pathway, Ms Davies replies: "No, no concerns."
2:49pm: The blood gas records show glucose levels for Child L on April 8 at 1.9 (10.58am) and 2.5 (12.14pm). The readings go above 2.5 in subsequent blood gas records for April 8, which only test for glucose levels. She confirms she would have checked the infusion bag containing 10% dextrose with Lucy Letby, making sure it was in date, going to the right baby, and signing it. The infusion is noted as starting at noon on April 8. Ms Davies says the pre-made dextrose concentrations available for infusion bags are 5% and 10%.
2:55pm: Ms Davies says the bags would be changed, regardless, every 48 hours. Ms Davies is asked if she, at any point, administered Child L with insulin. She replies she did not, and is not aware of anyone doing so. She says the circumstances for doing so would be two consecutive blood sugar readings of 12 or above, if a baby was hyperglycaemic.
3:03pm: Mr Myers, for Letby's defence, asks if Ms Davies was one of the nurses who transferred Child L and Child M to the neonatal unit. Ms Davies confirms she would have been the designated nurse for Child M at that time. Ms Davies is asked about the hypoglycaemic pathway. She says she is familiar with it, but keeps checking as policies regularly update. She confirms one was in place at the time. Mr Myers says the policy was milk first, then IV fluids, in normal circumstances. He says circumstances mean a doctor might change that and go to IV fluids. Ms Davies agrees. Mr Myers says there are three types of nutrition bag available - start-up bags for the baby's first couple of bags, maintenance bags, and specifically prescribed TPN bags which would have a baby's name on it. Ms Davies agrees. She tells the court the bag for Child L wouldn't have been referred to as a start-up bag, but would have been a standard 10% dextrose bag, as prescribed, to be infused. That completes Ms Davies's evidence.
3:18pm: Dr Anthony Ukoh is called to give evidence. He says his recollection was that Child L and Child M were born premature, not extremely so, and for Child L, he did not have any 'red flags' as a baby who would become unwell.
3:26pm: Dr Ukoh's notes for Child L from April 9, 2016, at 10.20am, are shown to the court. He noted the baby was breathing well, and Child L was on an extra 10% dextrose dose as the blood sugars were running at a "relatively low level for his age", but was "not unusual" for premature babies. There were no 'red flags' from the observations. The plan was 'as per hypoglycaemic protocol', to increase the infusion of 10% dextrose administration, "to make up for the low blood sugars", and to repeat blood sugar checks.
3:49pm: Dr Ukoh confirms a hypo screen test result, taken at noon on April 9, which is handwritten, is in his writing. He says it is not a complete hypo screen results sheet, and said that would have been done in response, and at the time of, a low blood sugar reading. Some of the results would have required sending away for analysis. He says the test results would have been received by the lab at 6.26pm.
3:58pm: Mr Myers, for Letby's defence, asks to clarify Dr Ukoh's explanations for the way some of the results are presented.
4:02pm: The judge asks for the hypoglycaemic blood test, if there was just one blood sample taken from Child L for the various tests carried out. Dr Ukoh agrees that was the case, and that some of the results would not come back straight away.
Thursday 16th February 2023
Children L & M (twins)
Dr A - Dr John GibbsChester Standard article 16-02-2023
A NURSE accused of multiple murders at a hospital neo-natal unit broke down in tears as a doctor began giving evidence at her trial.
Lucy Letby, 33, abruptly left her seat in the middle of the glass-panelled dock at Manchester Crown Court on Thursday, February 16 as the medic, who cannot be identified for legal reasons, confirmed his name.
She was visibly upset as she walked towards the exit door before she had a brief, hushed conversation with a woman dock officer.
Still appearing unsettled, she spoke with her solicitor through the glass panel before her barrister, Ben Myers KC, indicated to trial judge Mr Justice James Goss that proceedings could continue, as the trial completed its 16th week before a jury.
The doctor, a registrar at the Countess of Chester Hospital in 2016, continued his evidence screened from the public gallery and the defendant.
Letby listened on as she wiped away tears with a tissue and took a few sips of water.
The doctor told the court about his care of Child L, a twin boy born prematurely, who the Crown say the defendant attempted to murder by poisoning him with insulin.
He treated Child L in the early hours of April 10 2015 – the day after Letby is said to have attacked the baby.
The youngster's blood sugar levels were decreasing during the night shift and were "lower than what I would have wanted", he said.
Asked by prosecutor Philip Astbury why it was necessary to stop the levels falling, the doctor said: "Because low blood glucose levels in a baby can cause seizures.
"It's damaging to a baby. If it falls to a much lower level, then it can cause liver damage and brain injury."
Child L went on to make a full recovery, the court has heard, and was discharged the following month.
The infant's twin brother, Child M, was released at the same time after he too recovered from a collapse on April 9 – said to have been caused by the defendant injecting air into his bloodstream or obstructing his airway.
Letby, originally from Hereford, denies murdering seven babies and attempting to murder 10 others between June 2015 and June 2016.
Extract:
Later Dr John Gibbs, the lead paediatrician on the unit at the time, told the court blood tests carried out on Baby L confirmed he had been 'given insulin that he should not have received'.
He added: 'I was not thinking at the time that someone might have administered insulin. The results showed that, but unfortunately the junior doctors who read them didn't realise the significance'.
Letby, originally from Hereford, denies all the charges against her. The trial continues.
Friday 17th February 2023 - no court
Monday 20th February 2023
Child L
Dr Anna Milan (Clinical biochemist) - Dr. Gwen Wark (Director of the Guildford RSCH Peptide Hormone Laboratory) - Summary of police interviews
Child M
Police analyst: Recorded events & messages10:22am:
I'm back at Manchester Crown Court for the murder trial of nurse Lucy Letby. Jurors will continue to hear evidence in relation to Child M this morning. The Crown say Ms Letby injected air into the infant's bloodstream in April 2016. She denies all charges
10:55am: Court now sitting after a slight delay (due to problems with IT). Before we get to Child M, we're hearing evidence from two witnesses in relation to Child M's twin brother - Child L, who deteriorated at “pretty much the same time”
The Crown say Ms Letby poisoned Child L with insulin.
10:57am: Anna Milan, a clinical biochemist, is giving evidence about a blood sample analysis that was carried out for Child L. The analysis was to test for insulin
11:06am: Court is being shown blood analysis results for Child L (they were collected on 9 April 2016). Ms Milan said the 'only way you get a pattern like that is if insulin has been given to a patient'
11:15am: Ben Myers KC, defending, is now questing Dr Milan on the process for analysing blood - from ward to lab. She says 'ideally' blood will be taken and cooled within 30minutes to preserve it. Mr Myers asks if blood is left for hours, will it cause issues - 'it can do yes'
11:18am: Mr Myers asks if a sample hasn't been handled correctly, will it effect the relatability of the findings - and specifically in this case. Dr Milan says it can effect findings, but it 'wouldn't create insulin in this sample'
11:21am: Dr Milan repeats, that the only explanation for the readings in this sample is external administration
11:24am: Dr Gwen Wark is now in the witness box. She is the director of the Guildford RSCH Peptide Hormone Laboratory. Her evidence again focuses on the blood analysis of Child L
11:36am: Dr Wark's evidence relates to the veracity of the blood test results. She confirms Child L's reports met all required standards
11:52am: Court is now being read evidence from another clinical scientist who reviewed Child L's blood analysis
11:59am: Court has just been read a statement from a pharmacy technician who has worked at the Countess of Chester since 1991. A review of her records show that in 2014, three vials of insulin were ordered to the neonatal unit, six in 2015 and two in 2016
12:33pm: Jury is now being read a summary of Ms Letby's police interview in relation to the collapse of Child L. She denied deliberately administering insulin and rejected the notion it could have been administered accidentally.
12:34pm: When police put it to Ms Letby that insulin was deliberately administered, she said 'that wasn't done by me'
12:35pm: Kate Tyndall, intelligence analyst employed by Cheshire Police, is now giving evidence. She is going over sequencing evidence (basically a long timeline) for the case of Child M - important to say both Child L and his brother survived the alleged attacks
2:06pm: We're back after a break for lunch. Ms Tyndall is continuing to take the court through sequencing evidence. The evidence contains door swipe data (showing staff movements on the ward), medical charts and any social media messages incoming/outgoing from Ms Letby on April 9
2:12pm: Notes show that at 16:02 on April 9 2016 Child M collapsed and required full resuscitation - medics administered four doses of adrenaline in just over ten minutes in a bid to stabilise the infant
2:16pm: In all, Child M required nine doses of adrenaline and CPR for 29minutes before he stabilised on a ventilator shortly after 16:30
2:35pm: Judge has just called a five minute break, he remarks that prosecutor Nick Johnson KC has a rather 'flat monotone' voice....
2:45pm: We're back, continuing to go through sequencing evidence - in all there's 423 point to go through. We're on 311 at the moment
3:35pm: Court has adjourned, back at a later time of 1pm tomorrow.
Chester Standard article 20-02-2023
NURSE Lucy Letby told detectives any deliberate dose of insulin given to a twin baby boy was "not done by me", her murder trial heard.
Letby, 33, is accused of intentionally poisoning the youngster while on duty at the Countess of Chester Hospital's neo-natal unit.
The Crown say she harmed the infant on April 9, 2016 and also on the same day caused the sudden collapse of his brother who stopped breathing as his oxygen levels and heart rate dipped.
Both boys went on to recover and were discharged home the following month, Manchester Crown Court was told.
When later interviewed by Cheshire Police following her arrest Letby denied deliberately administering insulin to Child L, who cannot be identified for legal reasons.
She said to her knowledge neither she nor a nursing colleague had accidentally administered the substance, which had not been prescribed.
Letby added she could not believe such a mistake would have been made.
When suggested by detectives it was a deliberate act of sabotage, the defendant replied: "That was not done by me."
Asked if she had any explanation for the presence of insulin in Child L's circulation she said it "must have been in one of the bags or fluids he was receiving".
Earlier, Dr Anna Milan, a consultant clinical scientist at Royal Liverpool Hospital said a blood sample from Child L sent to its lab by the Countess of Chester showed the insulin was "exogenous".
The readings confirmed it was given to the patient rather than being naturally produced by the pancreas, she told the court.
The results were later communicated by phone to the Countess of Chester's biochemistry lab on April 14.
Jurors were also told that three vials of insulin were issued to the neo-natal unit in 2014, six vials in 2015 and two vials in 2016.
Insulin was kept in a locked fridge in an equipment room but the keys for access would be passed between nurses on duty as and when required, the court heard.
Letby, originally from Hereford, is also accused of attempting to murder another youngster, also a twin boy, with the administration of insulin in August 2015.
She denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Tuesday 21st February 2023
Child M
Nurse Mary Griffith - Unnamed nurse - Dr Anthony Ukoh1:17pm: I'm once again at Manchester Crown Court for the murder trial of nurse Lucy Letby. The jury will be continuing to evidence in relation to Child M. The prosecution allege Ms Letby injected air into the infant's bloodstream in April 2016
1:20pm: Mary Griffith, who was Child M's designated nurse in April 2016, is first in the witness box. She is taking the court through her nursing notes from that period
1:27pm: Court is being shown Child M's heart rate/respiration/temperature charts from April 8 in April 9. At around 16:00 on April 9 Child M suffered a 'dramatic' and unexpected collapse, that would require 25mins of CPR and six doses of adrenaline
1:33pm: Her notes from that afternoon state Child M was 'settled'. But at 16:00, her notes state: 'Baby went apnoeic and had a profound bradycardia and desaturation. Full resus commenced at 16:02'
1:49pm: Asked about the crash, she recalls: '(Child M's)alarm went off, I looked over my shoulder, the lights were flashing. Lucy went over to see and said yes it's an event, it needs to be sorted. At that point I stuck my head out round the door and asked for a resus call to be put out'
2:01pm: Court is being shown a photograph of a paper towel which was used by Ms Griffith and other medics on the afternoon of April 9 to note the medicines given to Child M between 16:02 and 16:31. The nurse says 'everything on it would have had to have been recorded' afterwards
2:05pm: The towel is now being passed around the court for the jury to look at
2:14pm: Jury have just been shown a photograph of a blood gas report for Child M - this document was recovered from Lucy Letby's house in Chester when she was arrested in 2018. Court has previously been told that, when questioned, Ms Letby denied the notes were taken as a souvenir and denied deliberately trying to harm Child M
2:32pm: Lucy Letby's defence lawyer Ben Myers KC is now questioning Ms Griffith
2:45pm: Court now taking a ten minute break, we'll be hearing from another witness this afternoon
3:13pm: A nurse, who cannot be named for legal reasons, is now in the witness box. She is recalling the events of Child M's collapse, she said 'Lucy and I walked over, she said he wasn't breathing, she asked for a crash call to go out' She added: 'Lucy administered recuse breaths...I was beside Lucy'
3:57pm: Dr Anthony Ukoh is now in the witness box, Dr Ukoh was working a day shift at the Countess of Chester on 9 April 2016
4:00pm: Dr Ukoh is reading over his notes from the morning of 9 April. He says Child M 'looked well, he was settled. There wasn't any major concerns, no red flags. There wasn't any signs he was in any pain'
4:08pm: Dr Ukoh is recalling the 'frantic' resus call he and other medics received shortly after 16:00. He says it took just under 30mins to stabilise the boy
4:13pm: Dr Ukoh tells the court that when he arrived on the neonatal unit Child M 'appeared lifeless'
4:50pm: Court has now adjourned.
Chester Standard article 21-02-2023
A "LIVE" note of medications given to a baby boy while he fought for his life was later found under a bed at the home of nurse Lucy Letby, her murder trial heard.
The record of emergency drugs provided to the youngster was written on a paper towel by nurses involved in his successful resuscitation at the Countess of Chester Hospital's neo-natal unit.
Letby, 33, gave rescue breaths to the infant after she responded to his cot monitor alarm on the afternoon of April 9, 2016, Manchester Crown Court was told on Tuesday, February 21.
The infant, known as Child M, suddenly collapsed in room 1 of the unit at 4pm as he stopped breathing and his heart rate and blood oxygen levels dipped.
Chest compressions commenced when he failed to respond, and six doses of adrenaline were required before his heart rate eventually rose to safe levels about 30 minutes later.
Giving evidence on Tuesday, nurse Mary Griffith said she was responsible for drawing up and checking the resuscitation drugs for Child M.
She told the court the paper towel would have been on the resuscitation trolley and provided a record for doctors of what drugs had been given and when as events unfolded.
Mrs Griffith said she recognised two of the entries for adrenaline administration were in her handwriting.
Simon Driver, prosecuting, told the court the paper towel – along with a blood gas measurement report for Child M – was discovered in a Morrisons shopping bag beneath a bed in a bedroom at the defendant's former address in Westbourne Road, Chester, on July 4 2018.
Mr Driver asked Mrs Griffith: "Have you ever taken a blood gas record home with you?"
Mrs Griffith said: "No."
Mr Driver went on: "Have you ever taken home with you the contemporaneous notes for medications given during a resuscitation?"
"No," repeated the witness.
Ben Myers KC, defending, suggested to Mrs Griffith that some of the notes on the paper towel were also written by Letby.
Mrs Griffith replied: "I can't say. I'm not going to guess."
Mr Myers made the same suggestion to another nurse, who cannot be identified for legal reasons, who said she thought "possibly" one of the entries was in Letby's handwriting, but added: "I can't be sure."
Letby, originally from Hereford, denies attempting to murder Child M and his twin brother, Child L, who she is alleged to have poisoned with insulin during the same day shift.
She denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Wednesday 22nd February 2023
Child M
Nurse Belinda Williamson - Statement of Nurse Ashleigh Hudson - Dr Ravi Jayaram10:31am: I'm back at Manchester Crown Court this morning where we'll be continuing to hear evidence in the trial of nurse Lucy Letby. Ms Letby is accused of murdering seven babies and attempting to murder 10 others at the Countess of Chester Hospital between 2015/16. She denies all charges
10:35am: Nurse Belinda Williamson is first in the witness box today. She is giving evidence in relation to the collapse of Child M on 9 April 2016. The prosecution say Ms Letby injected the infant with air - causing a near fatal collapse.
10:41am: Ms Williamson is recalling Child M's sudden collapse at 16:00 on 9 April. She says he looked 'pale and mottled. not quite right'...soon after a crash resus call went out and the infant needed 25mins of CPR and six doses of adrenaline
10:45am: The nurse did not take part in the resus directly, but she did send word to get Child M's parents who were still at the hospital. She recalls that there was 'talk of discontinuing' before Child M stabilised
10:57am: Jury are being read statements from other nurses that were present at the time of Child M's collapse (this is agreed evidence). Nurse Ashleigh Hudson said she recalls Letby shouting ‘can I have some help please' She said there was 'no panic in her voice, which is normal to avoid alarming patients who may be on the unit'
10:59am: Paediatric consultant Dr Ravi Jayaram is now in the witness box. Dr Jayaram was the on call consultant on 9 April
11:01am: Asked if any concerns about Child M had been brought to his attention at the start of his shift that day, he said 'no, not at all'
11:04am: Dr Jayaram recalls receiving a crash call - as it was a Saturday he doesn't remember whether he was on site or at home at the time. When he arrived on the unit, Child M was receiving CPR
11:08am: Dr Jayaram is taking the court through his notes from 9 April. They show he arrived at 16:15. Child M had already received three doses of adrenaline and had been intubated
11:28am: Dr Jayaram recalls having a conversation with Child M's family after 20mins of resus about whether they should stop. 'Generally the longer it goes on for, the less likely it is to have a good outcome. These decisions are very, very difficult', he tells the court. He said after 25mins, Child M 'suddenly recovered' - he said it wasn't due to a 'any specific intervention' by medics
11:30am: 'I couldn’t really explain what had caused it and why he suddenly got better', he added. Dr Jayaram tells the court that during CPR he noticed 'bright pink blotches' on Child M's torso - these blotches 'would appear and disappear'
11:31am: He said once circulation was restored and Child M was stable 'they vanished'. Dr Jayaram tells the court that he observed similar blotches in another baby in this case - they later prompted him to begin researching air embolus (the injection of air) as a potential cause
11:46am: He told the court: 'In June 2016, after a number of further unusual, unexpected and inexplicable events on the neonatal unit, the whole consultant body sat down and thought we have to work out what's going on here. 'One of the things that came up in discussion was could this be air embolus, I can’t remember who suggested it. 'It prompted me to do a literature search. I remember sitting on my sofa at home with my iPad, researching. I remember the physical chill that went down my spine when I read that because it fitted with what we were seeing'
12:10pm: Ben Myers KC, defending, is now questioning Dr Jayaram. He points out that his notes from the time of Child M did not make any reference to 'pink blotches' - he says surely this would be an important detail that should have been recorded
12:19pm: Mr Myers suggests it is 'incompetent' not to have noted the blotches - Dr Jayaram explains at the time many other things were happening and full relevance of blotches wasn't realised
1:10pm: Mr Myers said: 'Details of decolourisation doesn’t appear in notes or statements because it is not what you saw, is it?' Dr Jayaram again rejected the assertion. Mr Myers went on to claim that Ms Letby had been “a focus of interest” for Dr Jayaram since the death of another child in this case, Child D, in June 2015. He told the court another senior medic, Dr Stephen Brearey, had “flagged” to Dr Jayaram that Ms Letby had been working when a number of infants had collapsed or died in that month. “All eyes were on Ms Letby then”, Mr Myers said. “Clearly yes”, Dr Jayaram said.
1:11pm: Mr Myers said in that case, there is “absolutely no way” he would have failed to record the blotches on Child M. Dr Jayaram again explained: “I recorded what I felt was relevant.”
2:12pm: We're back after a break. We're hearing statements of agreed evidence from other nurses who worked on 8/9/10 April 2016 (at time of Child M's collapse)
Chester Standard article 22-02-2023
A DOCTOR said a "chill went down my spine" when he found a possible explanation for numerous collapses of babies, the murder trial of Lucy Letby heard.
Dr Ravi Jayaram said a number of "unusual and "inexplicable events" at the Countess of Chester Hospital's neo-natal unit led to a meeting of consultants at the end of June 2016.
Nurse Letby, 33, is accused of murdering seven babies and attempting to murder 10 others on various dates between June 8, 2015 and June 25, 2016.
On Wednesday, consultant Dr Jayaram told Manchester Crown Court how he saw "bright pink" patches that "flittered around" the abdomen of one infant he treated in April 2016.
Jurors were told how he responded to an emergency call from nurses to attend Child M, a twin baby boy, who had stopped breathing as his heart rate and oxygen levels plummeted.
He said it was a prolonged resuscitation that lasted "close to 30 minutes" and at one point he thought of stopping the efforts to revive him.
However, Child M "suddenly recovered" as his heart rate rose and he started breathing again, he said.
Dr Jayaram said: "I was very pleased but I couldn't really explain what had caused it and why he had suddenly got better."
He later stated to police he witnessed Child M's "unusual" skin discolouration when he arrived during the resuscitation.
Dr Jayaram told the court: "They were patches of very bright pink on his torso that flittered around. They would appear and disappear.
"Once circulation was restored and his heart rate came up above 100 (beats per minute) they vanished."
He said the discolouration was "very similar" to what he had seen in his treatment of Child A, the first alleged murder victim.
Other colleagues had spoken of seeing skin discolouration in other babies who had also collapsed on the unit, he said.
A meeting of a consultants was held on June 29, 2016, the court heard.
Dr Jayaram said: "After a number of further unusual, unexplained and inexplicable events on the neo-natal unit the whole consultant body sat down and said 'we really need to work out what is going on here'.
He said that "one thing that came up in our discussion" was air embolism – when gas bubbles enter a vein or artery and can block blood supply.
Dr Jayaram said it prompted him that evening to conduct a literature search in which he found a research paper which described the effects of air embolism.
He said: "I remember sitting on my sofa at home with the iPad and reading that description, and the physical chill that went down my spine because it fitted with what we were seeing."
Dr Jayaram emailed colleagues a link to the research paper the next day.
Letby, originally from Hereford, is said to have attacked several of her victims by injecting air into their bloodstream.
Jurors have heard Dr Jayaram did not refer to skin discolouration in his clinical notes concerning Child M.
Dr Jayaram disagreed with Ben Myers KC, defending, that that was because he had not seen such an appearance.
He said: "There were far more important things. The important thing was dealing with his cardiac arrest."
Mr Myers said: "I am going to suggest it would be incompetent to leave that out of the clinical note if you saw it."
The consultant replied: "I disagree. In many ways I wish I had written it down.
"At that time I had no knowledge or suspicion that the discolouration could have been related to something else that could have caused cardio-respiratory arrest, which is probably why I didn't specifically put it in the notes."
Mr Myers said given his previous similar observations about Child A then there was "all the more reason" to note changes in skin colour.
Dr Jayaram replied: "At the time it was not the priority. I wish I had and we would not be sitting here years later having this rather academic discussion."
In a sharp retort, and pointing to the defendant in the dock, Mr Myers said: "It's not academic. She is on trial here for multiple murders and attempted murders."
He agreed with Mr Myers he had also failed to mention skin discolouration in his clinical notes on Child A, or in his subsequent statement to a coroner.
The court went on to hear that Dr Stephen Brearey, head of the neo-natal unit, reviewed the circumstances surrounding the case of Child D shortly after her death in June 2015.
Dr Jayaram said it was not a formal review and he discussed the findings with Dr Brearey who had looked at case papers and files.
Mr Myers said: "He identified Lucy Letby as a person of interest."
Dr Jayaram replied: "I think he noticed that Lucy Letby was the nurse looking after these babies and that was it."
Mr Myers went on: "He raised with you the fact that Lucy Letby was present on these occasions?"
"Yes," said Dr Jayaram.
Mr Myers said: "With that in mind, she became the focus of interest as events unfolded. She had been flagged up as somehow linked in some way."
Dr Jayaram said: "There was an association with her being present. Nothing more."
Mr Myers said: "You and Stephen Brearey were already talking about Lucy Letby in June 2015, weren't you?"
The consultant replied: "In terms of association but as clinicians we have to think about all possibilities … we don't generally consider unnatural causes or deliberate things.
"Nothing like that was being contemplated at that stage.
"It was simply an association."
Mr Myers said: "Miss Letby had been a person identified as a potential link by June 2015."
Mr Jayaram said: "Yes and other colleagues had noticed the association as well."
Mr Myers said: "So all eyes on Ms Letby then?"
The consultant replied: "Well clearly yes because there is an association."
Jurors heard the defendant continued to work in the unit for the following 11 months.
She denies all the allegations.
Thursday 23rd February 2023
Child M
Dr John Gibbs - Statement of consultant paediatric cardiologist Dr. Arjamand - Dr Dewi Evans - Dr Sandi Bohin - Summary of police interviews10:41am: I'm back at Manchester Crown Court where the murder trial of nurse Lucy Letby is continuing. We'll be hearing from Dr John Gibbs this morning, who has since retired but was previously a consultant paediatrician at the Countess of Chester Hospital
10:43am: Dr Gibbs is taking the court over his notes for the collapse of Child M on 9 April 2016. The prosecution say Ms Letby injected air into the infant's bloodstream causing a near fatal collapse. She denies all charges
10:47am: Dr Gibbs examined Child M on the morning of 10 April. He said he queried whether infection/sepsis was the cause of the boy's cardio/respiratory collapse the previous day - 'it transpired he didn’t have either of those, so there was no proper explanation', Dr Gibbs said
10:56am: Dr Gibbs said subsequent X-rays and heart scans offered no explanation for the child's collapse
11:00am: Dr Gibbs said Child M 'still wasn’t behaving normally' on April 10, he was 'quiet and breathing slow' but he said that was 'explicable for a child that had very nearly died the previous afternoon'. The baby did eventually stabilise and was later discharged
11:28am: Court has just been read a statement from consultant paediatric cardiologist Dr Arjamand Shauq - he reviewed an ultrasound of Child M's heart on a request from medics at the Countess of Chester. They believed he could have had a thrombosis Dr Shaq said having reviewed the images the structure 'is not a thrombus' but a eustachian valve, which is 'perfectly normal in infants'
11:29am: Medical expert Dr Dewi Evans, who was approached by the National Crime Agency to review the case in 2017, is now in the witness box
11:42am: Dr Evans said from his review of the medical notes, he concluded that Child M's collapse was 'completely unexpected'
11:49am: Dr Evans said: 'this begs the question whether (Child M) received some noxious substance prior to his arrest or a bolus of air via his long line'
11:50am: Dr Evans said he ruled out infection (like pneumonia) as the cause of Child M's collapse as he would not 'have made such a prompt respiratory recovery' in the hours after
12:20pm: Ben Myers KC, defending, is now questioning Dr Evans. Mr Myers puts it to Dr Evans that if air was injected, it wouldn't just disappear within 30mins. Dr Evans said it would dissipate within the lungs
12:21pm: Dr Evans also says that an 'accidental air injection is virtually unheard of it just doesn’t happen' due to the sophistication of modern medical equipment
12:26pm: Mr Myers puts it to Dr Evans that air is made up of 70/80% nitrogen - which is insoluble in blood at that level, 'it doesn't vanish' Mr Myers said so it would still be present. Dr Evans says it would have dissipated somewhere
12:28pm: Dr Evans says most likely the cardiac compressions resulted in air moving from one side of heart into lung. Mr Myers puts it to the medic that he has no empirical evidence to back up these claims, Dr Evans says it would not be ethical to carry out such research on babies
12:32pm: Mr Myers has brought up a blood gas chart for Child M from April 8. They show it was not monitored for a number of hours - Dr Evans dismisses significance of this, saying 'we try to avoid sticking pins and needles in babies if we can avoid it'
12:37pm: Mr Myers puts it to Dr Evans that Child M's collapse could have been due to 'some residual underlying issue', he disagrees and repeats his belief that air was injected. A claim Mr Myers says he has 'no supporting evidence whatsoever' for
12:46pm: We're now being shown diagrams of the lines from an IV bag to a cannula (Dr Evans said that air could have been injected in through a bung on the line)
12:48pm: Mr Myers is pointing that the bung is there for a rapid injection of say adrenaline and goes into the system very quickly. Dr Evans agrees. That brings to an end Dr Evans' evidence for today - we're now hearing statements of agreed evidence, before another expert after lunch
2:06pm: Medical expert Dr Sandie Bohin, who reviewed Dr Evans' findings, is now in the witness box
2:20pm: Dr Bohin says 'there are very few things that can cause a baby to collapse in this way', she says it doesn't fit with infection or issues with feeds (as he was nil by mouth at the time). She also says there was no issues with his heart, 'this was completely unexpected'
2:26pm: Nick Johnson KC asks Dr Bohin if she believes air was administered with 'malevolent intention' - she says 'yes'
2:41pm: Mr Myers is now questioning Dr Bohin, he puts it to her that there is 'not much' to support her conclusions. She says that the infant suffered a cardiac arrest, 'something caused that, the baby almost died...for me air embolus fitted with that'
3:08pm: Prosecutor Nick Johnson KC has just read a summary of Ms Letby's police interview in relation to Child M. Earlier this week the court heard how after Ms Letby was arrested in 2018, police recovered a blood gas report of Child M under a bed at her home
3:09pm: She told police that there was 'no reason why she had kept it' and that it was an 'error on her part' perhaps not emptying pockets before she left work. She denied taking it to 'remind her of an attack' on Child M
3:57pm: Court now adjourned till tomorrow.
Chester Standard article 23-02-2023
A SLOW injection of air caused the sudden collapse of a baby boy allegedly harmed by nurse Lucy Letby, her trial has been told.
Expert witness Dr Dewi Evans said he believes air "trickled" into the infant's circulation via a connecting port on his intravenous drip.
He told Manchester Crown Court on Thursday, February 23 it could have taken "several minutes" for it to take effect before the youngster, Child M, rapidly deteriorated and almost died as staff battled for nearly 30 minutes to revive him.
Letby, 33, is accused of trying to kill Child M on the afternoon of April 9, 2016 while he was being treated in nursery room one on the Countess of Chester Hospital's neonatal unit.
The defendant co-signed for an antibiotic given via a port on the drip at 3.45pm – 15 minutes before Child M stopped breathing followed by a dip in his heart rate and oxygen levels.
Letby was near the doorway of room one, helping a colleague prepare medication for Child M's twin brother, when the alarm sounded at 4pm, the court heard on Thursday.
Consultant paediatrician Dr Evans said using a syringe to inject air via a port would be slower than a direct injection into the bloodstream.
Prosecutor Nick Johnson KC asked: "Would it follow, if someone chose to do it that way, they would not necessarily be standing over the baby at the time of the collapse?"
Dr Evans replied: "Yes, because you would not necessarily get an instant collapse. It could have occurred over several minutes.
Ben Myers KC, defending, said: "If there was air in his system sufficient to cause cardiac arrest, there is not going to be a recovery as rapid as this within 30 minutes."
Dr Evans said: "I disagree with that. The resuscitation was absolutely incredible. This was a very, very robust period of resuscitation that was required. This is something that is fairly consistent with a baby having air into the circulation. I can't think of any other cause.
"The volume required is pretty small. No nurse or doctor would allow a bubble of air into the circulation."
Dr Evans said any bubbles would disappear if cardiac massage was carried out.
Mr Myers put it to Dr Evans that he no had empirical research to support his opinion that air could vanish within 30 minutes.
Dr Evans said he relied on his knowledge of "basic anatomy and physiology".
Mr Myers went on: "You don't know as a matter of fact how much air is required to cause a collapse?"
Dr Evans replied: "No. 'Very little' is all I can say."
Letby, originally from Hereford, denies murdering seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Baby boy collapsed because of ‘slow injection of air’, Lucy Letby’s trial hears
A slow injection of air caused the sudden collapse of a baby boy allegedly harmed by nurse Lucy Letby, her trial has been told.
Expert witness Dr Dewi Evans said he believes air “trickled” into the infant’s circulation via a connecting port on his intravenous drip.
He told Manchester Crown Court it could have taken “several minutes” for it to take effect before the youngster, Child M, rapidly deteriorated and almost died as staff battled for nearly 30 minutes to revive him.
Letby, 33, is accused of trying to kill Child M on the afternoon of April 9 2016 while he was being treated in nursery room one on the Countess of Chester Hospital’s neonatal unit.
A prison van arrives at Manchester Crown Court, where the Lucy Letby murder trial is taking place A prison van arrives at Manchester Crown Court, where the Lucy Letby murder trial is taking place (PA) The defendant co-signed for an antibiotic given via a port on the drip at 3.45pm – 15 minutes before Child M stopped breathing followed by a dip in his heart rate and oxygen levels.
Letby was near the doorway of room one, helping a colleague prepare medication for Child M’s twin brother, when the alarm sounded at 4pm, the court heard on Thursday.
Consultant paediatrician Dr Evans said using a syringe to inject air via a port would be slower than a direct injection into the bloodstream.
Prosecutor Nick Johnson KC asked: “Would it follow, if someone chose to do it that way, they would not necessarily be standing over the baby at the time of the collapse?”
Dr Evans replied: “Yes, because you would not necessarily get an instant collapse. It could have occurred over several minutes.
Ben Myers KC, defending, said: “If there was air in his system sufficient to cause cardiac arrest, there is not going to be a recovery as rapid as this within 30 minutes.”
Dr Evans said: “I disagree with that. The resuscitation was absolutely incredible. This was a very, very robust period of resuscitation that was required. This is something that is fairly consistent with a baby having air into the circulation. I can’t think of any other cause.
“The volume required is pretty small. No nurse or doctor would allow a bubble of air into the circulation.”
Dr Evans said any bubbles would disappear if cardiac massage was carried out.
Mr Myers put it to Dr Evans that he no had empirical research to support his opinion that air could vanish within 30 minutes.
Dr Evans said he relied on his knowledge of “basic anatomy and physiology”.
Mr Myers went on: “You don’t know as a matter of fact how much air is required to cause a collapse?”
Dr Evans replied: “No. ‘Very little’ is all I can say.”
Letby, originally from Hereford, denies murdering seven babies and the attempted murders of 10 others between June 2015 and June 2016.
The trial continues on Friday.
Friday 24th February 2023
Child L
Dr Emma Lewis (Consultant clinical biochemist at the CoCH) - Professor Peter Hindmarsh10:30am: I'm at Manchester Crown Court again this morning for the murder trial of nurse Lucy Lebty. We're continuing to hear evidence in relation to the near fatal collapse of a baby, referred to as Child M, in April 2016.
10:33am: First in the witness box is Dr Emma Lewis, who is a consultant clinical biochemist at the Countess of Chester. Dr Lewis is explaining to the court the process by which bloods are tested at the hospital
10:54am: We're now being shown a blood test record for Child L (Child M's twin brother, who crashed around the same time as him on April 9). The Crown say Ms Letby poisoned Child L with insulin.
11:23am: Peter Hindmarsh, professor of paediatric endocrinology at University College London, is now in the witness box
11:27am: The medical expert was approached and asked to review blood charts for Child L. He last appeared in court in November last year, where gave expert evidence on another baby in this case, Child F
11:28am: In relation to Child L, he said that poisoning (with insulin) was the only reasonable explanation for the premature-born twin boy’s sudden deterioration
11:37am: Prof Hindmarsh has just spoke at length about various blood readings and calculations...Prosecutor Nick Johnson KC says, as he concludes, 'that's probably quite hard for the jury to follow' - the judge says 'me too'. Similar feelings in press gallery
11:38am: Mr Johnson is now taking Prof Hindmarsh back over his analysis
1:09pm: Prof Hindmarsh has told the court that in his opinion the blood glucose readings (and absence of other causes) point to insulin being administered to Child L.
Explaining how this could be done, he says 'so my feeling is that the likely mode of delivery of insulin was through an intravenous infusion by the addition of exogenous insulin to the infusion bag system'
1:10pm: He says to yield the blood results that Child L had, at least three bags would have had to have been contaminated - this could have been done by injecting insulin into the portal at the bottom of the bag while it was being/or after it had been made up
2:01pm: We're back after a short break. Ms Letby's defence lawyer Ben Myers KC is now questioning Prof Hindmarsh
2:32pm: Prof Hindmarsh says 'We can be quite certain (on 9 April) that exogenous insulin was present, thereafter, despite a variety of background infusion rates of dextrose, there isn’t really much change in glucose measurements which would imply that there is ongoing insulin present'
Lucy Letby: Baby's blood sugar dangerously low, trial told
A baby boy's blood-sugar level dropped dangerously low after he received fluids contaminated with insulin, Lucy Letby's trial has heard.
Ms Letby is accused of adding insulin to at least three of the infant's feed bags while on duty at the Countess of Chester Hospital in April 2016.
The nurse is charged with murdering seven babies and attempting to murder 10 others, between 2015 and 2016.
The 33-year-old, originally from Hereford, denies 22 charges.
Giving evidence, medical expert Prof Peter Hindmarsh told Manchester Crown Court that poisoning was the only reasonable explanation for the blood readings of the baby, referred to as Child L, who was on the neonatal unit in early April 2016.
Child L's blood glucose levels remained low throughout 9, 10 and 11 April, even after the intravenous line, and the connected bag containing the nutrients, were replaced.
Subsequent blood examinations found the baby boy's insulin level was at the very top of the scale the equipment was capable of measuring, the court heard.
Prof Hindmarsh, expert in paediatric endocrinology at University College London, agreed the readings could only be explained by "somebody having given insulin to [Child L]."
He noted that, on the basis of Child L's already low blood glucose levels on 8 April, there was no need "whatsoever" for insulin to be given.
He explained to the court that as insulin cannot be given orally, due to its molecular makeup, it would "most likely" have been administered intravenously.
Given the number of hypoglycaemic episodes Child L had over 8 and 9 April, Prof Hindmarsh said the insulin was likely to have been "added to bags used to deliver food".
Asked how much insulin would be needed to cause the low blood sugar levels in Child L, Prof Hindmarsh said: "I have taken quite a conservative view of this, but I would suggest you could add somewhere in the region of 10 units of insulin to a bag, that would be sufficient to produce the hypoglycaemic effect that was measured in the sample.
"Vials of insulin contain 100 units per millilitre, so the volumes we're talking about are quite small and not noticeable on a routine stock check.
"When added to infusion bags you wouldn't notice a change in volume within the bag, nor because insulin is a clear solution."
Boys recovered
Prof Hindmarsh said insulin could be added "fairly easily" through a portal that's located at the bottom of the feed bags.
He told the court that in his opinion, to produce the blood glucose levels detected, around at least three or potentially four bags could have been contaminated.
Ms Letby is accused of trying to kill Child L around the same time she allegedly tried to murder his twin brother, Child M, by injecting air into his bloodstream.
The boys went on to recover and were discharged from hospital the following month.
When interviewed by Cheshire Police following her arrest, Ms Letby denied deliberately administering insulin to Child L, the court was told.
She said that to her knowledge, neither she nor a nursing colleague had accidentally administered the substance.
In his opening address last October to the jury, Ben Myers KC, defending, said there was "nothing in fact" to establish Ms Letby had poisoned Child L and that there was "no obvious cause" to the collapse of Child M.
The trial continues.
Chester Standard article 24-02-2023
A BABY boy allegedly poisoned by nurse Lucy Letby had dangerously low blood sugar levels on three successive days, a court has heard.
Letby, 33, is said to have added artificial insulin to a bag of intravenous liquid the infant was receiving at the Countess of Chester Hospital's neo-natal unit.
Jurors at Manchester Crown Court heard on Friday, February 24 how the brain is reliant on a "constant supply" of glucose to function and the risks of low blood sugar included seizures, coma and death.
A medical expert told Manchester Crown Court that the youngster, Child L, suffered a hypoglycaemic episode which lasted from the morning of April 9, 2016 to the middle of the afternoon on April 11.
Peter Hindmarsh, professor of paediatric endocrinology at University College London, said the results of a blood sample taken some time on the afternoon of April 9 meant he was "quite certain" that non-natural insulin was present in his system.
Nick Johnson KC, prosecuting, said: "So somebody gave insulin to (Child L)?"
Prof Hindmarsh replied: "Yes, I agree with that statement and I think we should add that it was not prescribed insulin."
Giving evidence on Friday, he considered the most likely method of administration was intravenously into a bag of dextrose, a sugar supplement, which was connected to Child L's drip.
Prof Hindmarsh said the volume of insulin required would be "quite small" and would not be noticeable in the bag or from a routine stock check.
He added: "Once in the bag it's – in a sense – sealed off from you being able to detect it by smell."
Jurors heard the dextrose concentration was increased as medics tried to bring Child L's blood sugar levels up – which necessitated a change of bag – and the rate of infusion was also stepped up.
Prof Hindmarsh said despite that there was "not really much change in the glucose measurements which would imply there was ongoing insulin present and ongoing insulin action".
He told the court that insulin could "potentially" have been added to at least three dextrose bags if the giving sets were also changed.
Prof Hindmarsh also raised the possibility that if the giving set remained the same then insulin could stick to its plastic, come off and then release into the bag.
He agreed with Ben Myers KC, defending, that "sticky insulin" would eventually run out.
Mr Myers asked: "It is the case that sticky insulin could be operative over a similar period?"
Prof Hindmarsh replied: "I don't think anyone has done this sort of study to be honest. I think the answer is I don't know."
He told Mr Myers the "relatively steady" blood sugar levels did not seem to be influenced by the increased infusion rates.
Mr Myers asked: "Would that be more consistent with it being added to the bag as you go on, rather than the sticky insulin?"
Prof Hindmarsh replied: "Yes."
Letby is also accused of attempting to murder Child L's twin brother, Child M, who collapsed at 4pm on April 9.
She is said to have injected air into his bloodstream while he too was on an intravenous drip in the same nursery as his brother.
Letby, originally from Hereford, denies the murder of seven babies and the attempted murder of 10 others between June 2015 and June 2016.
Monday 27th February 2023
Child K
Mother's statement - Police analyst: Recorded events & messages - Dr Jonathan Ford - Dr James Smith - Nurse Joanne WilliamsChester Standard Live Reporting
10:27am: Having given evidence in the cases of twins, Child L and Child M, today the court is expected to go back, chronologically in the case, to Child K, who was born in February 2016. It is the prosecution's case that Lucy Letby attempted to murder Child K, a baby girl, on February 17. The defence deny this. Child K remained unwell and died on February 20.
10:33am: The 12 members of the jury have come into court, and the trial is now resuming. Prosecutor Nicholas Johnson KC is reminding the jury of its case for Child K.
10:34am: Mr Johnson tells the court the case is being dealt with out of step, chronologically, due to witness availability. He says it is alleged Lucy Letby attempted to kill Child K before the baby died a few days later, and it is not a murder charge.
10:38am: The court is now hearing a statement from the mother of Child K, who described being thrilled at the news she was pregnant. At the 12-week scan at the Countess of Chester Hospital, an issue was identified - Child K had a build-up of fluid at the back of her neck. At the 15-week scan, she was reassured everything was normal. She had regular scans, and further check-ups showed the fluid was disappearing gradually. At 18-20 weeks, it was discovered Child K had a pocket of fluid at her lungs, but follow-up checks saw this had gone. Just before 25 weeks, the mum recalls waking up with 'a few niggles and pains'. She was still working at this time. The midwife was called, and she advised to call the labour ward at the Countess of Chester Hospital - she was advised to attend. She was informed by a midwife there she had gone into labour "we couldn't believe it".
10:41am: The mother stayed at the hospital and received treatment. Discussion took place over transferring the mother to a tertiary centre, but the nearest one, Arrowe Park, was full. On February 16, the mother was given further steroids, and the possibility of a C-section birth was discussed. There were "no indications of any concerns" of Child K, who was showing no signs of any distress. The decision was made to leave things as they were at that time. That evening, the mother recalls waking up in pain, and the button was pressed to alert medical staff. Child K, a baby girl, was born at 2.12am. Staff worked on Child K for 30-45 minutes. The mother later found she had been born weighing 692g - 1lb 8oz.
10:47am: The consultant explained that the gestational age of 25 weeks meant there would be a medical team solely to look after Child K, who would be placed into an incubator. Once stable, she would be transferred to the special care on the neonatal unit. A female nurse came in and told the parents Child K was "fine and stable", and if they wanted to see her. The nurse offered to take photos of the three of them, on the father's phone. The pictures are timestamped at 4.31am on February 17, making Child K only a few hours old. The mother was woken up later informing a bed had become available at Arrowe Park. At 9am, the transfer team arrived at the Countess of Chester Hospital. They explained what was going to happen. The process took "some time" as the team had difficulty stabilising her. It was then when the parents considered a name for Child K. At noon, it was "now or never", for Child K to be transferred to Arrowe Park. The mother had not been discharged at this point, and the medical team "desperately" tried to make it possible so she could be allowed to go to Arrowe Park, which was done at 2pm. The parents arrived at Arrowe Park at 2.30-2.45pm. Later, arrangements had been made for the parents to stay at the purpose-built accommodation.
10:50am: The mother recalled "the strangest feeling which she could not describe" on the morning Child K died. At the neonatal unit, parents had no restrictions on visiting times. They went in As soon as she walked in, she could see the readings, including saturations, were low. She knew straight away things weren't great. A doctor was in the room at the time. "I looked and said, she's not good is she?" The doctor "confirmed the worst," explaining Child K had been fighting all night. The parents had a long conversation with the doctor, and the decision was made to switch off life support machines. Child K passed away in her father's arms.
10:51am: A cot was brought into the room to allow the parents time privately with Child K, who had died on February 20.
10:56am: Cheshire Police intelligence analyst Kate Tyndall is now talking the court through the sequence of events for Child K. They begin with text messages recovered from Letby's phone. Letby messages a colleague about the unit being a "hive of activity" on February 16 in preparation for a visit from "the big bods", and there is a discussion on the possible of delivery of Child K. Letby mentions one colleague had suspected conjunctivitis, but had still come into work, and adds "Hope I haven't caught anything". Said colleague had also not "done anything but moan" that day, Letby says. Letby messages the ill colleague saying she hopes that colleague is feeling better soon. The colleague responds she was feeling better after a day of bed rest, and thanks Letby for her message.
10:59am: The night shift for February 16 is shown to the court. The paediatrician of the week is John Gibbs, the on-call consultant is Dr Ravi Jayaram. Lucy Letby is on duty, looking over two babies in room 2 at the start of the night shift. There are two babies in room 1, three babies in room 2, three in room 3 and three in room 4. A further baby is in the Transitional Care Unit. Child K is later transferred to room 1 after she is born.
11:03am: Child K is born with 'dusky, floppy, no resp effort' at birth, and a heart rate of 60bpm. The 'Apgar score' is 4/10 at one minute, 9/10 after five minutes and 9/10 at 10 minutes after birth. Previously, the court has heard the Apgar score measures how well a baby is doing in the minutes after being born. Child K was admitted to the neonatal unit at 2.40am due to her "extreme prematurity", Mr Johnson tells the court, as well as the fact she was to be transferred to a tertiary centre at a later point.
11:09am: Dr Ravi Jayaram makes a note to the transport team at 3.15am. Observations are taken for Child K at 3.30am. A blood sample later showed no bacterial growth recorded. Further communication is made with the transport team at 3.35am.
11:10am: Swipe data is recorded showing Child K's designated nurse Joanne Williams leaving nursery room 1 at 3.47am to go to the labour ward. It is just after that, the prosecution say, the event alleged in the case of Child K happened, and the baby girl collapsed.
11:13am: The event is recorded as happening by Dr Jayaram and Dr James Smith at 3.50am - "sudden deterioration" - sats dropping to 40%, Child K bagged via ET tube with Neopuff. The 'sats recovered quickly' following treatment, and Child K was reintubated. Designated nurse Joanne Williams also recorded the event. She is a co-signer for Child K to be administered morphine, with the other co-signer being Lucy Letby. Lucy Letby is the co-signer for further medication for Child K at 4.20am, the other co-signer being nurse Caroline Oakley.
11:26am: Further observations and medication administrations are given through the early morning. A nursing note is made for Child K by Lucy Letby, who was not Child K's designated nurse, at 6.04am-6.10am. An x-ray records the ET tube is in the right place at 6.07am. Dr Jayaram notes an event at 6.15am: '@0615 began to have lower sats & IV down to 2.5...Tube pulled back to 6cm". Retrospective notes by Dr Jayaram record: 'Tube noted to have slipped to 8cm @ lips - withdrawn and heart rate picked up immediately.' Nurse Melanie Taylor takes over designated care for Child K for the day shift at 7.30am. Lucy Letby has signed for a 7ml saline bolus for Child K at 7.30am.
11:34am: Further records show that, throughout the morning, ventilation requirements for Child K gradually increased. The transport team arrived at the hospital at 8.50am, for transferring Child K to Arrowe Park. Dr Jayaram discusses transport arrangements in notes which are recorded at 9.15am. A message sent to Letby at 10.04am from a colleague says: 'Hope you had a good shift and are in the land of nod now!'
11:46am: Further records are made of attempts to stabilise Child K so she can be transferred to Arrowe Park, through medication administrations. At noon, Child K is moved into a transport incubator. The formal handover from the neonatal unit to the transport team took place at 12.25pm-12.30pm. Child K arrived at Arrowe Park by 1pm on February 17. Medical records showed Child K was cared for at Arrowe Park Hospital from 1.15pm on February 17.
11:48am: Letby messages her colleague at 5.48pm: '25wkr delivered so fairly busy...' The message was in reply to a colleague saying she had hoped the shift had gone well, and expecting she was asleep at that time ('in the land of nod'). Letby adds: 'Everything ok? Not like you not to text back'. The colleague apologises. Letby then messages about staffing limitations at the hospital for the following shift.
11:51am: On Saturday, February 20, 2016, the decision is recorded to withdraw life support from Child K. The time of death is recorded as 5.28am. The doctor records, as the cause, 'extreme prematurity' and 'severe respiratory distress syndrome'. Lucy Letby made a Facebook search on April 20, 2018, at 11.56pm, for the surname of the family of Child K.
12:09pm: The court has just had a short break. Claire Hocknell is now talking the court through the neonatal unit review schedule, which documents that Child K was admitted to neonatal unit nursery room 1 at 2.40am on February 17, 2016. The designated nurse for Child K was Joanne Williams, who was also a designated nurse for a baby in room 2. Lucy Letby was the designated nurse for two babies in room 2.
12:29pm: An agreed statement is now being read from Dr Jonathan Ford, a former registrar at the Countess of Chester Hospital. He reviewed the mother of Child K before the baby girl was born, and discussed the issues of extreme prematurity. He said the longer the pregnancy could be, and delaying of the birth, the better. He reviewed the mother again at 9pm on February 16, and it was agreed for 'conservative management'. She was called back on February 17 at 1.20am, when the mother was 'in pain, in active labour'. It later became 'inevitable' the mother would give birth. He delivered the baby. The birth was "uneventful" and Child K was passed over to the paediatricians. It was noted, at the 14-week scan, Child K had a cystic growth at the back of her neck. A detailed scan at week 16 and week 20, that was resolving, and there were no problems with how Child K's heart looked.
12:39pm: The next witness to give evidence in court is Dr James Smith, who was employed at the Countess of Chester Hospital in February 2016 as a specialist registrar. Dr Smith recalls he did have a memory of Child K. He recalls being notified there would be a delivery of a '25-weeker' baby. He recalls being present at the birth, and the baby girl was born in 'expected condition'. The Apgar scores of 4, 9 and 9 are 'good'. Asked about the 'dusky, floppy, no resp effort' note, Dr Smith says the gestation presentation can be variable, but a good/reasonable sign is a heart rate, 'no resp effort' is not unexpected and the baby would present as 'floppy' as there had yet to be any breathing support supplied by medical staff.
12:40pm: He tells the court full airway breathing resuscitation support would be required, but that would 'not be unexpected' for a baby as premature as Child K.
12:49pm: Dr Smith describes the procedures he would have taken to stabilise a baby such as Child K in this scenario. He says Child K's heart rate improved to 100bpm within two and a half minutes, and she was making respiratory gasps. The decision is then made to intubate. The intubation is "technically difficult", he tells the court, due to the baby's size, and can take multiple attempts. He says Child K was stabilised after each attempt, and he had no worries about doing the procedure himself, without needing to hand over the procedure to the consultant, Dr Ravi Jayaram. He successfully intubated Child K on the third attempt with a size 2.0 tube.
12:53pm: He tells the court if he had seen any signs of trauma, such as bleeding, on Child K at the time of intubation, he would have passed the procedure on. To the best of his recollection, he did not see any signs of trauma. He tells the court there is nothing in the notes of any sign of trauma at this point. The general clinical picture was Child K's signs were 'good', the resuscitation 'had gone successfully' and the first blood gas record was 'good - reasonable for the first reading'.
12:57pm: He tells the court that for all babies of this prematurity, antibiotics would be administered.
12:59pm: Dr Smith tells the court he would have been, to an extent, guided by advice from Arrowe Park Hospital in the treatment of a baby of this prematurity at the Countess of Chester Hospital.
2:00pm: The trial is now resuming following its lunch break. Dr Smith will continue to give evidence.
2:06pm: Dr Smith says he would not have played any part in the connection of Child K to the ventilator at the neonatal unit, following transfer, and would not have had any knowledge of how to do so, as that connection would be a task carried out by nurses.
2:12pm: Dr Smith says he remembers coming back into the neonatal unit early on February 17, probably for labelling blood bottles. He does not recall where the nurses were, but recalls Dr Ravi Jayaram giving breaths to Child K via the Neopuff, and that was already under way. He said the readings, while unable to recall what they were precisely, "were not improving", and further measures were to be carried out. The explanation for a "sudden deterioration" was either the breathing tube being dislodged or blocked. The "correct decision" was for the tube to be removed. Breathing mask support was supplied to Child K without a tube. Child K's oxygen saturation levels improved and Child K was reintubated. A morphine bolus was administered to help the reintubation process.
2:13pm: Dr Smith says he did not see any evidence of trauma, and if there was anything obvious to show that, he would have informed Dr Ravi Jayaram, but he "did not see anything".
2:19pm: The prosecution ask if the Countess team followed the advice from Arrowe Park to take x-rays of Child K to check for tube placement. Dr Smith confirms they did, and a chest x-ray was carried out. The radiology report said, from the x-ray, the ET tube was 'in satisfactory position' following the reintubation, along with the NG tube, while a UVC line required further adjustment. The radiology report also recorded possible lung infection, which Dr Smith was expected in babies of Child K's gestational age.
2:23pm: Dr Smith re-examined Child K at 6.15am, when it had been noted Child K had lower saturations, with a blood gas reading which was "not good" and "worse than the previous gas". The tube was 'pulled back' to improve the oxygen saturation levels, but the readings had 'not improved'. The decision was then taken to remove the tube from Child K. 'Bagging' breathing support was provided to stabilise oxygen saturation levels, and Child K was reintubated once again. Child K had responded 'very quickly' to the 'bagging' support.
2:25pm: Dr Smith says, from the notes, there is nothing to say the tube removed from Child K was blocked, and his memory has nothing to add to that.
2:27pm: A repeat x-ray reported: 'Satisfactory position of the ET tube. NG tube in situ...this would benefit from advancement by 5-10mm. UVC in satisfactory position.' A lung infection was still suspected for the left lung, which appeared increased in density - 'looking more white', and reduced in volume compared to the right lung.
2:29pm: Dr Smith later wrote a transfer letter to Arrowe Park Hospital, which summarised the care given to Child K at the Countess of Chester Hospital, including details of intubations, medication administrations and a blood result.
2:33pm: Benjamin Myers KC, for Lucy Letby's defence, is now asking questions in respect of the events for Child K. He says Child K was born in extreme prematurity, and asks if there would inevitably be problems for the baby girl's care, particularly in relation to the lungs. Dr Smith agrees. Dr Smith remembers being in the room when Child K's resuscitation efforts were taking place, and they were going well. He says neonates with this gestation need a lot of support and resuscitation. He cites a study that babies of that gestation age, found a 75% survival rate. Mr Myers suggests that figure could be more like 40-50% from another study. Dr Smith says he has cited the most recently available study he looked at.
2:36pm: Mr Myers says a tertiary unit is the most suitable place for treating babies of Child K's gestational age. Dr Smith says they are more experienced at a tertiary unit, but level 2 units (such as the Countess of Chester Hospital at this time) have the equipment and have staff capable of treating babies of this gestational age, for the short term. He says the correct thing to do would be to contact the level 3 unit in advance to enquire if transfer to there was possible in advance of birth.
2:39pm: He says seeing Child K's bruising on her hands and feet at birth was not something he had seen frequently in births, and was more likely seen by staff at tertiary centres. He said he had asked for an expert opinion on the subject of the bruising.
2:45pm: Dr Smith says level 2 centres do not look after babies of this prematurity, long term. He says if mothers of 23-week gestational arrived at the hospital via ambulance, and delivery was imminent, that delivery would take place at the nearest hospital, with a set procedure in place to arrange transport to a tertiary centre when viable. Dr Smith recalls it would have been better if he had written his own independent notes, in addition to Dr Ravi Jayaram's complete notes. He added he did write up the transfer letter listing the events and care for Child K. Mr Myers asks why would Dr Jayaram write up those notes in the first place. Dr Smith says he would also have been on the paediatric unit on that night shift. He says as long as a senior doctor has been involved in writing, then the notes would be 'completed'. He says that 'ideally', he would have written notes up himself, independently.
2:54pm: Mr Myers asks about the initial intubation process for Child K. He asks if Dr Jayaram should be the one to do that process, as the more senior doctor. Dr Smith says: "No, not if the baby is stable." He says the decision to take over could be the 'wrong decision' as the doctor carrying out the procedure would be familiar with the placement of where everything is. Mr Myers asks if it's standard practice guidance for babies to be intubated within 15 minutes of birth. Dr Smith says he is not familiar with that number, and asks Mr Myers where that guidance has come from. Dr Smith says if that was the number that is standard practice, then he would go with that. He says there are two different numbers for how long it was after birth for intubation to have taken place - one of them is 12 minutes.
2:59pm: Dr Smith is asked about lung surfactant which a note records as being administered at 3am, and if that, at about 35 minutes after intubation, is 'too long'. Dr Smith says if there is good oxygen saturation recorded at the time, and Child K is stable, that would not be an issue, but if guidance is to administer that surfactant five minutes after intubation, then that would be considered too long.
3:01pm: Dr Jayaram's note is shown to the court, written retrospectively. Dr Smith points out the note of surfactant administration is recorded as being made at '0245'.
3:11pm: Mr Myers asks about the insertion of a central line, done 'several hours' after Child K was born. Dr Smith says the procedure requires assistance, is difficult, takes time, needs a sterile environment and a stable baby. It also requires x-rays afterwards. The line is 1mm thick being put into an umbilical cord line that is 1-2mm thick. It is, in this instance, 'a non-emergency UVC'. Mr Myers says this is a procedure which, 'ideally' should be done by a consultant neonatologist at a tertiary centre. Dr Smith says ideally, the baby would be born at a tertiary centre, but in these circumstances, the most experienced staff available at a level 2 centre, who are capable of this type of procedure, would carry out the procedure. Mr Myers asks if it was 'too long' a time period. Dr Smith said the baby would not have been compromised by a longer time period. Mr Myers asks if it was 'sub optimal'. Dr Smith says it would depend on the circumstances and the condition of the baby, and in Child K's case, the 'correct thing to do' was to prioritise the airway and breathing support, and lines could be put in later. Mr Myers asks if the insertion of the line at this time fell outside the 'golden hour' principle. Dr Smith says there is no difference in the method of the administration of initial medicines - the UVC was one option, but there are others. Dr Smith agrees with Mr Myers the initial administration of antibiotics fell outside the 'golden hour' principle timing. The antibiotics were administered at 4.40am, according to electronic prescription records, sometime after the first hour of Child K's birth which ended at 3.12am. Dr Smith adds, from a blood test, there was no marker of infection, but if was sub-optimal that the antibiotics and vitamin K (administered at 4.20am) were not administered in the first hour, and cannot recall why that was the case.
3:34pm: After a short break, Mr Myers is continuing to question Dr Smith. He refers to the intubation attempts made for Child K. Dr Smith says he used a 2.5 tube at first, then a smaller 2.0 tube was used, successfully. Mr Myers asks about an air leak which was reported. Dr Smith says he was aware, and made reference to it in his third statement to police. The 3.30am reading of '94' for air leak, Dr Smith does not know what that means, as it does not correlate to any of the other readings. He says the blood gas record for Child K was good, and the oxygen saturation for Child K was good, and oxygen requirement had come down. He says he does not believe that would mean only 6% (100% minus 94) of oxygen was getting into Child K. He said a large air leak would result in a change to a larger ET tube being considered, but that process would require reintubation. He said, knowing there was good oxygenation and good gas, that would reduce the need for reintubation. He adds that a tertiary neonatologist with more experience of ventilators might give a different opinion, but they would need to be called to give evidence. Dr Smith adds he also does not know what the 'resistance' figure on the chart signifies either.
3:39pm: Mr Myers asks about the reintubation of the tube for Child K, which involved a larger tube. Dr Smith says the first ET tube was working fine, then it was not, and reintubation was required. The morphine bolus was applied to have "a sedative effect" on Child K.
3:42pm: The desaturation at 6.15am is referred to. Dr Smith says the ET tube was pulled back, but saturation levels continued to decrease, so the ET tube was removed and bagging commenced. The saturation levels improved, and Dr Smith says that meant there "was a problem with the tube". Mr Myers says pulling the tube back and seeing no change [prior to the tube's removal] meant there was no problem with the positioning of the tube. Dr Smith says the cause of the tube's movement could have been it 'slipping' from the clamp, for this deterioration.
3:44pm: Dr Smith says he did not recall any injury/blood/trauma with Child K, and if he had done so, he would have referred it to Dr Ravi Jayaram and asked them to take over the intubation process.
3:47pm: Mr Myers asks if, hypothetically, he had seen blood before intubation, if he would have checked for the source of it. Dr Smith says it would depend on the amount of blood seen that would lead to how concerned he would be. He said if he had seen blood-stained secretions, he would make a note of it.
4:08pm: The next witness to give evidence is Joanne Williams, who was employed as a neonatal nurse at the Countess of Chester Hospital. She has returned to give evidence in respect of Child K. She confirms she was working a night shift that night. She remembers Child K being born, and being on that night shift. She remembers being called through at the birth of Child K, and recalls her being born at 25 weeks gestation. She said the delivery happened at the Countess, and Child K would be transferred later to a tertiary centre. Ms Williams remembers Child K being bruised on her feet, which was not unusual a sight, as she had seen that in the past. Immediate resuscitation was provided and Child K was intubated.
4:22pm: An observation chart is shown to the court for 'Baby Girl', as Child K had yet to be named. Child K was on a ventilator for 45 breaths a minute when she was on the neonatal unit room 1. As designated nurse, Ms Williams confirms she would check to make sure the ventilator was secure for Child K.
4:24pm: The oxygen saturation reading for Child K of 70% at 2.45am would be considered 'low', while the 94% reading at 3.30am was 'normal' and 'improved'. The prosecution say that would be indicative the ventilator was working as it should be.
Tuesday 28th February 2023
Child K Nurse Joanne Williams - Dr Ravi Jayaram - Elizabeth Morgan (Cheshire Police Nursing Advisor)Chester Standard Live Reporting
9:30am: Yesterday the prosecution began delivering evidence in the case of Child K. The prosecution allege Lucy Letby attempted to murder Child K, a baby girl born on February 17, 2016, within a couple of hours of her being born. The defence deny this.
9:31am: Nicholas Johnson KC, prosecuting, told jurors on Monday: “It is alleged Lucy Letby interfered with the endotracheal (ET) tube and Dr Ravi Jayaram walked in to the immediate aftermath of that.” When going through the sequence of events yesterday, Mr Johnson told the jury Dr Jayaram would be called in to court to give evidence.
10:28am: The trial is expected to resume shortly.
10:31am: At the end of Monday, Countess of Chester Hospital nurse Joanne Williams began giving evidence. She is continuing to do so this morning.
10:36am: Ms Williams is being talked through her nursing note from the morning of February 17, 2016, in which she described Child K being born in 'fair condition'. She was 'intubated at approx 12 minutes of age with size 2 ETT'. Ventilation commenced, and a 'high leak noted'. Ms Williams said that is noted via the ventilator, and if there are any concerns, they are highlighted to the medical team. She says that can sometimes be down to the size of the ET tube. Staff would be alerted to the leak via the ventilator giving off an alarm, the court hears.
10:42am: Ms Williams says there were no concerns over the leak, as the overall clinical picture for Child K was stable. Ms Williams says the alarms would go off if the baby's clinical picture declined, such as the heart rate dropping or oxygen desaturation. Initially it would be a 'soft alarm', which is amber and makes a noise, then a more urgent alarm in red and 'more of an alerting' sound. There is a way to pause the alarms, Ms Williams says. That could be paused for several minutes, once it had been activated, in the event of doing a procedure. Ms Williams says she cannot recall if the alarm could be disabled in advance. The court hears a newer version of the monitors have since been installed in the hospital, where that is possible.
10:45am: Ms Williams says at the time of the 'high leak', the clinical picture for Child K would have been assessed, and a check the tube was in the right place at the mouth. The prosecution is now asking about the time period when Ms Williams left the nursery room to inform the family on what had been happening. She said she would not have done so if Child K was not satisfactorily stable. She tells the court, other than being born very premature, there was nothing of concern. She does not remember asking anyone in particular to look after Child K in her absence.
10:47am: Ms Williams recalls Child K being 'quite active' as she left, which was normal to see in prematurely born babies. The court hears Ms Williams left the unit at 3.47am.
10:51am: The intensive care chart for Child K on February 17, 2016 is shown to the court. A reading at 3.30am says, for morphine, 'commenced'. Ms Williams is asked if that means morphine commenced for that time. Ms Williams agrees. A reading for 0350 '100mg/kg morphine' is recorded. The note is not in Ms Williams's handwriting, and the court hears that would have been a bolus of morphine.
10:56am: There is a prescription note for 0350 for a morphine infusion dose. Ms Williams says this is also not in her handwriting, and it is written by a doctor. Asked again about the '3.30am' reading, Ms Williams says that would not have begun at 3.30am precisely, but in the time period after. She cannot say whether that happened before she left the room at 3.47am. She tells the court Child K would have been stable when she left.
11:04am: When Ms Williams returned, she heard a red alarm, "it seemed like an emergency, something was going on". She says she felt upset, and it "always frightening to go back into a situation like that". She recalls Dr Jayaram asked her what had happened, likely near the nursing station after Child K had stabilised. Ms Williams said Dr Jayaram had asked 'how did the [ET tube] move'. She recalls Child K was reintubated, with a bigger ET Tube.
11:06am: Asked about her '?ETT dislodged, removed and re-intubated' nursing note, Ms Williams tells the court there was a query that the ET tube had been dislodged.
11:08am: Ms Williams had also recorded on her nursing note, for the ET Tube, 'large amount blood-stained oral secretions'.
11:09am: The nursing note also adds 'Initially active on handling but now more settled'.
11:11am: Ms Williams tells the court a morphine bolus would be given, instead of a morphine infusion, when carrying out a procedure such as inserting a UVC line.
11:12am: Ms Williams's family communication note includes 'photos taken and treasure box and Bliss bag given...encouraged parents to come to the unit to visit and mum and dad both touched her...mum to be discharged to [Arrowe Park Hospital] to be with baby.'
11:14am: Ms Williams's further nursing note explains Child K had '2 further episodes of apnoea and de-saturation with loss of colour. Has been re-intubated twice and now has a 2.5ETT...' Ms Williams tells the court she would have remained the designated nurse throughout that night shift for Child K.
11:16am: Benjamin Myers KC, for Lucy Letby's defence, is now asking Joanne Williams questions. He picks up on what Ms Williams had just said, that she did not have much experience in dealing with babies born at 25 weeks gestation. Ms Williams agrees that was the case at the time in 2016. Mr Myers says there is the potential for deterioration in such babies, as they can be 'unpredictable'. Ms Williams agrees.
11:22am: Mr Myers asks about the process of administering a 'lung surfactant'. Ms Williams says it would be kept in storage. It would be prescribed, but could be signed for retrospectively. Doctors would work out how much to prescribe based on the baby's weight, and they would administer it. A prescription form is shown to the court, showing a '120mg dose' 'administered 0300'. Asked if 0300 is the time of the dose given, Ms Williams says: "Yes." She adds that would be an "estimated" time the dose was given. The scheduled time appears as '0544' is because it is a retrospectively written note, the court hears.
11:25am: Mr Myers asks about the '94' leak reading for 0330 for Child K. He asks if that is a high air leak. Ms Williams agrees. Mr Myers says it would be a reading 'to keep in mind'. Ms Williams agrees.
Mr Myers: "The aim would not to be to have a leak of 94%?"
Ms Williams: "Yes."11:26am: Mr Myers asks if ET tubes can be dislodged if a baby moves or not, Ms Williams agrees. She also agrees that requires careful observation, and it can change from minute to the next, but there are procedures, such as clamps, to keep the tube in place. Mr Myers asks if Child K had been 'quite active'.
Ms Williams: "At times, yes."11:30am: Mr Myers asks about the morphine administered, which he says can sedate a baby and stop them being as active. Ms Williams says Child K would have received morphine after being intubated, not at the time of intubation. Mr Myers asks about when this morphine was administered. Ms Williams says the morphine could start via a bolus or an infusion, then the other being administered.
11:31am: A prescription for a morphine injection is shown to the court. Mr Myers asks if this is a bolus. Ms Williams agrees. Ms Williams agrees she has co-signed for it, and agrees with the administration time of '0350' recorded as being the time the morphine was injected.
11:36am: The morphine infusion prescription and administration chart is shown to the court. This is prescribed by a doctor, and has a handwritten start time of '0350'. Ms Williams says 0350 could be the start time, or it could be later. Mr Myers says the prescription wouldn't have a start time after it had already been administered. Mr Myers asks about the 0330 fluid chart. Mr Myers says although it is said morphine commenced at '0330', it is an hourly chart, and that means the morphine could have been commenced at any time between 3.30am and 4am. Ms Williams agrees.
11:38am: Ms Williams says, for the '0350 100mg/kg morphine' note, that is not in her handwriting, but having someone else write in that note box is not uncommon when working as a team.
11:40am: Mr Myers asks if the morphine bolus and the morphine infusion began at the re-intubation process, after Child K had suffered a desaturation.
Ms Williams: "Yes."11:45am: Mr Myers asks about the alarm going off, and a conversation with Dr Ravi Jayaram. Ms Williams says the conversation took place not in nursery room 1. He asked her, Ms Williams had said in her police interview, what had happened, and she had replied she did not know as she was not in the room, having gone to see the parents. Mr Myers asks to clarify about what Ms Williams had said moments earlier: 'I thought the ET Tube was secure, but I was not there'. Ms Williams agrees.
11:47am: Mr Myers asks about the nursing note made by Ms Williams 'large blood-stained secretions'. Ms Williams says she does not recall where that came in the timeframe of events. She adds it is difficult to write notes retrospectively and highlight the significant events. She says it is likely that would have been seen at the time of the re-intubation as she would have been present.
11:52am: The prosecution rise to ask Ms Williams further questions. Ms Williams is asked about the lung surfactant administration note. Prosecutor Philip Astbury asks about the timings of the note. The 0544 would be the time the surfactant was prescribed, retrospectively. It would not have been done concurrently as Child K would not have been added as a new baby identification on the hospital's system at that point. The time at 5.48am, when the note was filed, would have been the point when it was considered what time the surfactant was given, the court hears. The note records it administered as '0300'. She says she does not recall who administered the surfactant.
11:58am: Ms Williams's nursing note is shown to the court. She is asked if the note, written retrospectively, is written chronologically. Ms Williams says that ideally, that would be the case. Mr Astbury asks about the infusion chart, where hourly records are made. The 0330 note is referred to. Ms Williams is asked if records are kept as close to the times where possible. She agrees. Ms Williams says she does not remember being present for the 0350 morphine bolus.
12:01pm: Mr Astbury asks about the conversation Ms Williams had with Dr Jayaram. Ms Williams is asked if Dr Jayaram asked her: "How did the tube move?" Ms Williams agrees. The judge asks about the purpose of the morphine bolus, whether given before or after the infusion. Ms Williams said it would be done '3-5 minutes' for a procedure such as re-intubation, for pain relief to the baby.
12:02pm: That completes Joanne Williams's evidence.
12:14pm: The next witness to give evidence is Dr Ravi Jayaram.
12:17pm: Dr Jayaram confirms he would have been on call as a consultant on the night shift of February 16-17, 2016. He says he would have been called at home, and would have been called to come in for the delivery of a 25-week gestational age baby such as Child K, as the hospital would be aware there could be complications. He tells the court, until the early 2000s, there was less structure, but in more recent times, if possible, mothers are taken to tertiary centres [such as Arrowe Park] to give birth. If that is not possible, babies can be cared for in the short term at level 2 centres such as the Countess of Chester Hospital.
12:18pm: He says, on balance, the risk would have been too great to transfer Child K and the mother for the birth at a tertiary centre. He adds he was present at Child K's birth.
12:26pm: Dr Jayaram says it is significant, when talking through the medical notes he had written retrospectively, the mother had a 'spontaneous rupture of membranes' 48 hours before birth, as that could lead to a risk of infection. He said it was relevant there were 'no fevers' recorded. The medical notes record Child K was 'initially dusky, floppy, no respiratory effort'. Dr Jayaram said that was significant and in this situation, a pathway is followed including 'inflation breaths', which stimulates the baby's first gasps. He says it is like blowing a balloon up for the first time - the lungs are difficult to inflate for the first time as they are filled with fluid. The inflation breaths are completed after two cycles, and Dr Jayaram says the chest is then seen to be moving up and down. The heart rate is then above 100 beats per minute, recorded two and a half minutes after birth. Gasps are recorded after three minutes. Dr Jayaram said Child K would have initially been 'a little stunned', but the gasps are what the medical staff are looking for. Oxygen saturation levels of 'above 85%' at six minutes are 'satisfactory'.
12:28pm: The initial intubation process is discussed. Dr Jayaram says it can be difficult and risky, and it is important the oxygen saturation levels are high before starting the procedure. A doctor has 30 seconds to attempt the intubation procedure. The court hears the intubation was done on the third attempt, with a smaller, size 2, ET tube. He says, "ideally", a 2.5 ET tube would be used, but in these circumstances a size 2 tube was sufficient.
12:32pm: Child K was transferred to the neonatal unit, on a ventilator. Dr Jayaram describes Child K required around 60% oxygen. He says he could hear air going in and out of the baby girl's lungs. The initial blood gas readings are taken, and it is acceptable for a 'little bit of leeway' on carbon dioxide levels. Child K was given surfactant at 2.45am, Dr Jayaram had recorded in the notes. A blood culture test was taken to screen for infection, as a routine test, and the baby girl would be treated on the assumption she already had an infection and would be treated with antibiotics.
12:35pm: A morphine infusion is recorded on the medical notes. Mr Astbury asks when that would be administered. Dr Jayaram says he does not recall when that would have been, but it would not be immediately after transfer to the neonatal unit nursery room 1. Dr Jayaram said he could hear Child K's heartbeat, and air going in and out of both lungs. He said, for a 25-week gestation baby, he was "happy" with Child K's progress.
12:38pm: Dr Jayaram said he was happy the ventilator was working, as observed by Child K's chest moving, and being in good colour. He tells the court that at this point, he informed the transport team about the situation, and they had advised there was a bed at Arrowe Park Hospital, and they advised for a UVC line to be inserted prior to transport.
12:41pm: Dr Jayaram is now being asked about Child K's desaturation at 3.50am. A plan of the neonatal unit layout is shown to the court. Dr Jayaram said he was "happy" with how Child K was "very very settled", having had to make only minor adjustments to the ventilator settings. An infusion chart for the morphine is shown to the court, with a start time of 3.50am. He confirms that 3.50am would be the time that would be administered.
12:48pm: Dr Jayaram says he was aware Joanne Williams was going to the labour ward to update the parents on Child K. He said he was sitting at a desk, around the corner from the entrance to nursery room 1. He says he was writing in notes, or waiting for the transfer team to come back to him regarding arrangements. He said he had been told Lucy Letby would be 'babysitting' at the time - a common term used by the hospital to describe a neonatal nurse temporarily looking after a baby in the absence of its designated nurse. He says, at this point, in February 2016, he was aware of 'unexpected/unusual events' that had happened recently, and that Lucy Letby had been present.
He said: "I felt extremely uncomfortable [with Lucy Letby being there alone in the room with Child K] "You can call me hysterical, completely irrational, but because of this association... " This thought kept coming into my head. After two, two and a half minutes...I went to prove to myself that I was being ridiculous and irrational and got up. "I think it was 2.5, 3 minutes after Jo had gone to the labour ward. "I had not been called to review [Child K], I had not been called because alarms had gone off - I would have heard an alarm.
I got up and walked through to see [Child K]." Dr Jayaram entered nursery room 1 through the entrance doors closest to his desk. Child K was at the far side of the nursery room, with Lucy Letby present. He said: "I saw Lucy Letby standing by the incubator. I saw her, and looked up at the monitor, and K's saturations were dropping, in the 80s and continued to drop. The ventilator was not giving out an alarm. "I recall looking up and saying 'what's going on?' and Lucy said something along the lines of 'She's having a desaturation'." Asked what Letby was doing, Dr Jayaram replied: "Nothing." He says Letby didn't say anything to Dr Jayaram until he had walked over and he had asked her what was going on.
12:51pm: Dr Jayaram said he was looking at Child K. He disconnected the ventilator from the ET Tube and he tried to give breaths via the ET Tube, but Child K's chest was not moving. He said he switched into 'professional mode' to resolve the situation, and it 'didn’t make sense why the tube was dislodged' He said he removed the tube - which wasn't blocked - and put a face mask to ventilate Child K. As soon as that was done, Child K's chest went up and down, without too much difficulty. He says he does not remember anything else Lucy Letby said. He says he was probably telling her to bring equipment.
12:53pm: Dr Jayaram says the original tube was not blocked, and there would be no reason for that to have been blocked, for the time it had been on Child K. Dr James Smith reintubated Child K, and the same ventilator settings were selected, indicating - Dr Jayaram tells the court - Child K had not been declining.
12:57pm: Dr Jayaram's notes are shown to the court, where he had described it as a 'sudden desaturation'. The oxygen saturation levels fell to 40%. The tube was removed, Child K was bagged via a face mask, and 'sats recovered quickly'. A size 2.5 ET tube was placed. 'Ventilator settings as previously'. The size of the tube "did not have an impact" on the previous ventilation, Dr Jayaram tells the court, as Child K was "ventilating effectively" and did not have an impact on the "sudden deterioration".
12:59pm: Dr Jayaram says he cannot recall how long Joanne Williams had been away before the sudden deterioration had taken place. He tells the court the transport team and the parents were updated, but he does not believe they were updated about "this event".
1:55pm: The trial, which has had its usual lunch break, should be resuming at 2pm.
2:01pm: Prosecutor Philip Astbury is continuing to ask Dr Ravi Jayaram questions.
2:10pm: The court is shown Dr Jayaram's notes, plus writing by someone else at 5.40am recording a vial of Curosurf given. Notes by Dr Jayaram are written retrospectively at 7.50am. He recorded at 6.15am, Child K 'began to have lower sats'. He says the blood gas record from that point suggested the cause of that 6.15am deterioration was an issue with ventilation. He tells the court low blood pressure is also recorded. Saline is administered but the blood pressure remained low. The ET tube was pulled back but saturations remained low, so the ET Tube was removed. Child K's oxygen saturation levels improved in response to bagging. The blood pressure dropped again at 7.25am. The saturations and heart rate dropped. Child K was taken off the ventilator and Neopuff was administered. Cardiac compressions were started as it was 'not sure enough blood was being pumped around the body' - Child K had not gone into cardiac arrest, but the heart rate had gone under 100 beats per minute. The ET Tube "wasn't working", as it had 'gone in further' than it should have gone, the court hears. Child K was recorded as 'now stable'.
2:13pm: Dr Jayaram says he had observed a chest x-ray for Child K showing the ET Tube was in the right place. The transport team was estimated to arrive at 8.30am, and they led on treatment from later in the morning, the court hears.
2:16pm: Dr Jayaram says using the smaller, size 2 ET Tube, is not a problem as long as the baby was being ventilated. He says a leak is recorded, and in itself is not of any clinical significance even if it is high, as it is important to ventilate the baby. Dr Jayaram says the size of the ET Tube has no impact on the likelihood of it being dislodged.
2:18pm: Dr Jayaram says he was "happy" with the original intubation and "happy" they were adequately ventilating Child K. He tells the court they would do investigations (such as x-rays) if they thought there was something they would need to change in management. He says at the time Joanne Williams left the nursery room, there were no concerns of any potential deterioration for Child K.
2:20pm: He tells the court: "You wouldn't not have expected" Child K's lungs to have deteriorated to the extent shown in the few minutes Joanne Williams was away from the nursery room. He says his thought processes for going into the room, when Lucy Letby was present, were only to prove to himself that everything was ok.
2:26pm: Mr Myers says Dr Jayaram was worried about being irrational at the time. Dr Jayaram said he was concerned and didn't want to see Child K in a different condition. They were not based on a clinical reason, or if Child K had any underlying conditions. Mr Myers said he believed, from Dr Jayaram's interview with police, the suspicious behaviour had been deliberate.
Dr Jayaram: "That had crossed my mind, yes."
Mr Myers: "You 'got her', then?"
Dr Jayaram: "No." Dr Jayaram said he wanted this investigated objectively in a proper way, and there was "absolutely no evidence that we could prove anything - as that is not our job, we are doctors." Mr Myers said he had told the police if the tube had been dislodged on purpose. He asks if he had confronted Lucy Letby. "No, absolutely not." Dr Jayaram said he was focused on the situation. Mr Myers says it did not happen in the way Dr Jayaram describes.
Dr Jayaram: "I am interested in why you say that." Mr Myers says it is not documented in medical notes. Dr Jayaram says that would not be the sort noted in medical documentation. Mr Myers says there is nothing to say the tube is dislodged. Dr Jayaram says it is obvious from the medical notes.2:30pm: He says, in isolation, the incidents were unusual, and more concerning in a pattern of behaviour. He said: "We, as a group of consultants by this stage, had experience of an unusual event, and there was one particular nurse. "All of these events were unusual. Yes, if we put in Datix [incident forms] we could have investigated sooner and been here [in court] sooner." He said he, and his other consultants, wanted to know how this could be investigated, and tried their best to escalate concerns higher up the hospital. Mr Myers says there is no record anywhere of the suspicious behaviour noted. Dr Jayaram says he did not anticipate being sat in a courtroom, years down the line, speaking to Mr Myers. "If you feel someone is deliberately harming [children], you would do so, wouldn't you?" Dr Jayaram said concerns had been raised before February 2016, and were raised again following this incident. Mr Myers says Lucy Letby continued to work at the unit for a further four months.
2:34pm: Dr Jayaram says the concerns were first raised in autumn 2015 with senior management, but were told that there was likely nothing going on. He said the consultants went 'ok', and against their better judgment, carried on. "We were stuck, as we had concerns. "In retrospect, we wished we had bypassed them [senior management] and contacted the police."
"We by no means had played judge and jury, but the association was becoming clearer and clearer. "This is an unprecedented situation for us - we play by a certain rulebook, and you don't start from a position of deliberate harm. "It is very easy to see things that aren't there - in confirmation bias. "But these episodes were becoming more and more and more frequent by association." Dr Jayaram said it should have been documented throughout more. He says he discussed the incident, but did not formally document it. Dr Jayaram said he was getting "a reasonable amount of pressure from senior management not to make a fuss".
2:36pm: Dr Jayaram says he does not understand why an alarm did not go off, and why a call for help had not gone out when Child K was desaturating. He said, in relation to the suspicions, he "did not want to believe it". He said it "took a long time for police to be involved".
2:39pm: Dr Jayaram says the tube is 'very unlikely' to have been dislodged by a 25-week gestational age infant, in that short timeframe. He says that can happen when a baby is 'very vigorous' - heavier, stronger babies, or when a baby is being handled or receiving cares. Mr Myers said it was still possible for the tube to be dislodged by Child K. Dr Jayaram says 'anything is possible', but Child K was 'not a very active baby', and a baby of this weight, size and age meant that was unlikely.
2:42pm: Dr Jayaram said the receiving consultant would not have assumed the tube had been dislodged by anyone else. Mr Myers says the alarm on the ventilator was not alarming, according to Dr Jayaram. Dr Jayaram says he had not got up because the alarm was going off. He said if it was, he would have been prompted to go in, and that would have been his reason for going in the nursery room. Mr Myers asks if a conversation took place with Ms Williams after the desaturation. Dr Jayaram says he does not recall the conversation. He says: "Why would I ask her what happened in the room when she wasn't there?"
2:48pm: The court is shown swipe data for Joanne Williams, who left the neonatal unit at 3.47am. Mr Myers says it is very precise in coinciding with Dr Jayaram's recollection of waiting two-three minutes before the desaturation is timed at 3.50am, and asks if Dr Jayaram always has such a precise memory. Dr Jayaram says "In this event, I did." He adds: "I kept telling myself, don't be ridiculous [about my suspicions]. I looked at my watch - I didn't have a stopwatch." Dr Jayaram says he has never seen the swipe data, nor had cause to look at any data. Dr Jayaram says it would be appreciated if Mr Myers gave an indication of where he was going with his questioning. Mr Myers says an earlier police interview had Dr Jayaram not giving a precise estimate how long Joanne Williams had been out, but is able to give a more precise estimate now, several years later. Dr Jayaram says he has had more time to reflect on this incident.
Dr Jayaram: "The point is, this incident happened in the window when she [Joanne Williams] was out." He tells the court the incident of this night is "emblazoned" in his mind.2:54pm: Dr Jayaram adds he "refutes" the allegation the care the hospital team provided contributed to the outcome of Child K. Mr Myers asks if the focus on this incident was to "distract" from the overall care provided by the medical team to Child K.
Dr Jayaram: "Well, that's an easy one to answer: Absolutely not."
"Are you seeking to bolster suspicion against Lucy Letby?"
"Absolutely not." Mr Myers asks if there was an opportunity, within the 48 hours before Child K's mother gave birth, to transfer her to a tertiary centre. Dr Jayaram says he does not have that decision to make, and cannot answer that, but adds there were many factors to consider.2:57pm: Dr Jayaram is asked about the intubation process. Mr Myers says the process was carried out by a 'relatively junior registrar', Dr James Smith. Dr Jayaram said Dr Smith had been assessed as competent and experienced enough, and it was 'standard practice' to carry out these procedures. "I could see he could do this, and safely." He adds if Child K was struggling to be ventilated at the time, and the heart rate and saturations were not being maintained, then he would have taken over.
3:00pm: Mr Myers asks about the high air leak. Dr Jayaram says the 94% leak is a measured value, and is significant is the baby is struggling to be ventilated; but if the baby is being ventilated, then it is just noted. Mr Myers says lung surfactant should be administered within five minutes of intubation.
Dr Jayaram: "Ideally, yes." He says it is used to improve gas exchange. If it is given slightly later than expected, it would "not make much difference in the long run", as it is important the baby is receiving ventilation at the time.3:07pm: Mr Myers asks why only Dr Jayaram and not Dr James Smith made notes. Dr Jayaram says he does not know why that was the case. Dr Jayaram's medical notes are shown to the court, and the medicines are highlighted. Mr Myers says it appears the antibiotics have been delivered at the right time.
3:10pm: A prescription chart is shown for one of the medicines, 'time given 0445'. Dr Jayaram agrees it appears it was administered at that time, and should have been administered sooner. He says the late administration of the antibiotics is important, the vitamin K not so. Mr Myers says he will next talk about the morphine infusion.
3:20pm: The questions continue, following a short break.
3:28pm: Dr Jayaram is asked about the morphine infusion recorded, which appears on the notes above a note added, timed at 3.50am. Dr Jayaram says, having seen the prescription chart, the morphine infusion would not have happened before the desaturation. Mr Myers said Dr Jayaram had told police Child K had been sedated with morphine. Dr Jayaram said that was what he had believed at the time. Dr Jayaram says Child K was not on a morphine infusion prior to the desaturation. "However", she was not a vigorous baby. He says, in retrospect, he will accept the morphine was not running prior to the desaturation. He says he is "surprised" it was not running sooner. He says he believed, "in good faith", the morphine was running at the time.
Mr Myers: "Have you tried to shift your evidence? That you can't blame it on morphine?"
Dr Jayaram: "Even accounting for the fact she was not on morphine, she was a 25-week gestational age", small, and weighing 600g and was stable - 'poorly, but stable'. He says that the dislodging happened in such a short space of time was "concerning". He says Child K was able to move her arms and legs, but not enough to dislodge a tube. He says his previous statement was based on a "genuine misunderstanding based on my notes". He says he does not accept he made a "deliberate error".3:30pm: Dr Jayaram says he is not aware of a nursing note recording 'blood-stained oral secretions'. The nursing note by Joanne Williams which refers to this is shown to the court. Dr Jayaram says that is in the back of Child K's mouth, not in the tube, and is not clinically relevant. It was "not a significant finding". He says he would have noted if the tube had been blocked, and he would have noted it.
3:33pm: Dr Jayaram says the tube blockage would lead to a gradual deterioration, quite quick, but did not fit the pattern of Child K's deterioration. Mr Myers suggests the care of Child K provided could have been improved. Dr Jayaram said it could have been better. Mr Myers suggests Dr Jayaram has added to his account over the years.
Dr Jayaram: "I would disagree with that - you would be questioning my brevity and honesty."3:36pm: The prosecution rise to ask about a couple of matters. Dr Jayaram is asked if he has ever seen the electronic sequence of events [being shown in court], or the swipe data collated. Dr Jayaram replies he has never seen either, nor had cause to see them.
3:43pm: The judge asks about the morphine infusion prescription chart, and asks Dr Jayaram which sections are in Dr Jayaram's handwriting. The sections including the 0350 start time are in his writing. The infusion would have been administered by the nurses, Dr Jayaram tells the court. That completes Dr Ravi Jayaram's evidence for Child K.
3:47pm: The court now hears an agreed statement from Elizabeth Morgan, who says in her experience, it is very unlikely a nurse would leave the nursery of a baby if the baby's ET tube was not settled in a position and the baby was settled. For a baby of this gestational age, it would be standard practice for a nurse to take corrective action, carry out checks and call for help if a desaturation was noted. It would 'not be normal practice' to wait and see if the baby self-corrects, for a baby of this gestational age.
Wednesday 1st March 2023
Child K Summary of Police InterviewsChester Standard article 01-03-2023
A NURSE accused of multiple attacks on babies told police she may have been waiting to see if an infant "self-corrected" before intervening, a court heard.
Lucy Letby, 33, is accused of murdering seven babies and attempting to murder 10 others while she worked as a neo-natal nurse at the Countess of Chester Hospital.
One of her alleged victims was Child K, who was born in February 2016 at 25 weeks weighing just 692 grammes.
The Crown says Letby attempted to murder the baby girl within two hours of her birth by deliberately dislodging her breathing tube during a night shift.
The youngster was briefly left in the care of Letby by her designated nurse, who had gone to update her parents on the labour ward, Manchester Crown Court has heard.
Consultant Dr Ravi Jayaram told the jury that Letby was doing "nothing" when he walked into nursery room 1.
He said he saw her standing beside Child K's incubator and then he looked up at the monitor and saw her saturations (blood oxygen levels) were in the 80s and falling.
Monitors were set to alarm when saturations dropped below 90% but they were silent at the cot, he added.
On Wednesday, March 1, prosecutor Nick Johnson KC read to jurors a summary of Letby's police interviews about the incident, in which she denied any wrongdoing.
Letby told detectives at Cheshire Police she only recalled Child K because she was a "tiny baby" and the Countess of Chester did not usually take babies of her gestation and weight.
She said she had no recollection of the tube slipping and agreed that designated nurse Joanne Williams would not have left Child K unless she was stable and her ET (endotracheal tube) was correctly positioned.
Mr Johnson said: "She stated she would have raised the alarm if Dr Jayaram had not walked in and if she had seen the saturations dropping or that the tube had slipped.
"Miss Letby thought it possible that she was waiting to see if (Child K) self-corrected. She explained that nurses don't always intervene straightaway if levels were not 'dangerously low'."
Following further questions from police, she suggested that maybe the tube had not been secured properly, he said. She denied that had been done deliberately.
Child K was transferred later that day to Wirral's Arrowe Park Hospital where she died three days later.
The Crown does not allege Letby caused her death.
Mr Johnson explained to the jury he was not calling medical experts Dr Dewi Evans and Dr Sandie Bohin.
He said the prosecution and defence had agreed there was nothing they could add to the evidence already heard about Child K.
Letby, originally from Hereford, denies all the offences said to have taken place between June 2015 and June 2016.
Thursday 2nd March 2023
Child N
Parents' statements - Police analyst: Recorded events & messages - Dr. Jennifer Loughnane - Statements from Dr Sudeshna Bhowmik, Caroline Oakley, Melanie Taylor, Sophie Ellis, Christopher Booth, Valerie ThomasChester Standard Live Reporting
9:01am: The prosecution is expected to begin delivering evidence in the case of Child N, a baby boy who was born in June 2016. The prosecution allege Lucy Letby attempted to murder Child N three times. The defence deny this.
9:30am: Previously, the court heard June 2016 was the last full month in which Lucy Letby worked at the Countess of Chester Hospital's neonatal unit. The following month, the neonatal unit was redesignated from a 'Level 2' unit down to a 'Level 1' unit. Earlier this week, the court heard very premature babies, such as Child K, would be cared for, long-term, at a tertiary centre - or 'Level 3' unit, such as at Wirral's Arrowe Park Hospital.
10:31am: The trial has now resumed, with evidence being given in the case of Child N.
10:39am: The court is now hearing a statement from the mother of Child N, who was born on June 2, 2016 at 1.42pm, via C-section. The mother first visited the neonatal unit, where Child N was, at 10pm that night. Child N was kept there due to prematurity, and for the first 13 days there were no problems reported to the parents. Child N had haemophilia and on June 15, the parents were informed the baby boy had had a bleed. The parents were informed to attend hospital as soon as possible. Child N was in intensive care, and on arrival Lucy Letby was there with other people. They were told they had tried to intubate Child N between 4-8am. Child N had two collapses that day - the parents were told to go out and get some fresh air in between the two collapses. While they were out, Child N had his second collapse. A 'spur of the moment' baptism took place. Lucy Letby stayed beyond the end of her shift, and Child N was transferred to Alder Hey, where he recovered quickly over the following couple of days.
10:42am: A statement is now being read from Child N's father, who says Child N's mother was a haemophilia carrier. He said he could not go to all the scans, but at one of them there was a concern Child N appeared to stop growing, so steroids were prescribed. A C-section was planned, several weeks early. When Child N was born, he weighed 3lb 11oz. It was "a little scary" when he was first born, as Child N needed a little oxygen, but he was then ok. For the first 13 days, the only issue reported to the parents was an issue with Child N's liver, which he was being treated for with light therapy. The parents visited daily.
10:45am: On the day Child N was due to come home, on June 15, the father was at work. He received a call from Lucy Letby saying Child N was 'a bit unwell' during the night, but was fine now. He did not get the impression that Child N was still unwell. He then received a call from child N's mother to come to the hospital as soon as possible. When he arrived, Lucy Letby was in the room with Child N, giving cares. There was "no urgency". Lucy said: "Hi. He's been a bit unwell during the night." He said he was "shocked" when he saw Child N, as he had dried reddy-brown blood around the mouth. "I remember being confused and thinking, 'what's wrong with him?'"
"No-one told us what happened, or why." After going outside for a bite to eat, they returned to the neonatal unit and found the blinds were down. A staff member on reception said Child N was "really unwell" and if they would like a priest.10:51am: Someone came into the maternity room, where Child N's mother was staying with the father. The staff member said: "You'd better come - he's really ill this time." Upon their arrival to the intensive treatment unit, resuscitation efforts were being administered to Child N. The father said he could not watch what was going on. Staff from Alder Hey Children's Hospital were among the staff members in the room. After a breathing tube was fitted, Child N stabilised and 'calmed down'. The parents spoke to a haemophiliac specialist nurse who had come from Alder Hey via taxi. Child N was taken to the transport team, in a process "which seemed like forever", by 11pm. Lucy Letby came to the parents and said she had stated beyond the end of her shift and hoped that Child N was going to be alright. Child N was taken to Alder Hey, where he stayed for a couple of weeks before going home. When home, the parents noticed Child N had 'twitches', then later 'spasms', and at one point was not breathing. He was taken to the Countess of Chester Hospital, and transferred to Alder Hey, where he stayed for 1-2 weeks.
11:01am: Cheshire Police intelligence analyst Claire Hocknell is now talking the court through the first of two sequences of events for Child N. The first is a Facebook message from a Countess of Chester Hospital doctor at 11.56am on June 2, asking Lucy Letby for an 'opinion on something'. Lucy Letby replies: "Hope I can help!" Child N is born via C-section at 1.42pm, weighing 1.67kg, at 34 weeks plus 4 days gestation. His 'APGAR' scores, recording how well Child N was doing immediately after birth, are 9/10 at 1 minute and 9/10 at 5 minutes. Nurse Caroline Oakley records Child N was admitted to the neonatal unit at 2pm, and Child N had 'prematurity and clotting disorder'. A blood sample was taken at 2.30pm. A clinical note by Dr Anthony Ukoh reports: '34+4 baby boy cried immediately, required no active resus'. Not for IM Vit K for now until haemophilia status known'. Observations: ...intermittently grunting++'
11:03am: A desaturation down to 67% oxygen saturation, lasting one minute, is recorded by nurse Caroline Oakley at 3.10pm. The nurse adds, in a nursing note: '[Child N] Allowed to rest. Sounds very mucousy. Grunting intermittently...dropped saturations to 67% when upset; temp being recorded and required 60% O2 to recover...awaiting blood results before being given Vit K.'
11:06am: The note adds: 'Decision made to screen and [nil by mouth], IV fluids/Vit K IV as prescribed as still grunting'
11:12am: An x-ray result before 6pm recorded that Child N likely had an infection. Nurse Caroline Oakley recorded at 6.47pm that Child N's temperature, which had been low, was recovering. A family communication is recorded: 'Dad has visited baby on unit and updated by [Belinda] Simcock. She has also visited mum... and updated...' A haemophilia diagnosis is confirmed for Child N.
11:14am: Lucy Letby is recorded as starting her night shift on June 2 at 7.30pm, in time for the 7.30pm-8pm staff handover. Letby is a designated nurse, with shift leader being Melanie Taylor and other designated nurses being Christoper Booth and Sophie Ellis. Booth has two babies in room 1, including Child N, Ellis had one in room 2 and two in room 3, and Letby had two in room 4. Two babies were in transitional care, and another baby was 'rooming in with her parents' - that baby's designated nurse was Letby.
11:17am: A few minutes after entering the neonatal unit, Letby WhatsApps a colleague and says she had a 'paper handover' as colleague Caroline had gone home. Nurse Christopher Booth records 'care taken over approx 2000...oxygen saturations predominantly in mid 90s-100%'. He also records the usual handover checks.
11:20am: Letby messages 'We have got a baby with haemophilia' Reply: 'How many weeks?'
LL: '34'
R: 'oh'
LL: 'Everyone bit panicked by seems of things but baby appears fine'
R: 'male?
LL: 'yeah'
LL: 'Oh and had weird FB message from [doctor] earlier...' Letby adds she does not know much about haemophilia. Her colleague replies to be careful with cannula and blood samples.11:26am: The conversation continues about discussion of other babies, and Letby messages her colleague: 'Had strange message from [doctor] earlier...'
Reply: 'Did u? Saying what?'
'Go commando? 😂
Letby: 😂😂😂😂
Letby: 'Asking when I was working next week as wants to talk to me about something, has a favour to ask..?'
R: 'Think he likes you too...'
R: 'Hmm did u not ask what it was?'
LL: 'No just said when I was working and he said wants my opinion on something'
LL: Hmm...🤔
R: 'Hmm'
LL: 'Do you think he's being odd?
R: 'Thought as flirty as u'
LL: 'Shut up!'
R: 'What?!'
LL: 'I don't flirt with him!'
R: 'Ok'
LL: 'Certainly don't fancy him haha just nice guy'
R: 'Ok'11:27am: The conversation continues back on work, asking why there was a staff shortage on the unit. One of the staff members is speculated to be off with stress.
11:28am: The conversation on WhatsApp, now continuing after 10pm, discusses another baby's condition.
11:33am: Further observations are recorded regularly for Child N up to 1am. Child N then suffered a desaturation at 1.05am. Nurse Christopher Booth: 'One episode whilst I was on my break, whereby infant was crying++ and not settling. He became dusky in colour, desaturating to 40s. Responded to facial oxygen within 1-2 minutes, crying [subsided] after 30 minutes'. The note adds Child N's colour returned to pink perfusion.
11:34am: Nurse Booth added, up to 2.04am: 'No further episodes observed. Oxygen saturations have been consistently mid 90s-100%...in view of earlier episode, infant remains nil by mouth...'.
11:36am: Nurse Ashleigh Hudson takes over care of Child N for the day shift on June 3. Tachypnoeic on handover, unsettled'
11:39am: Letby messages the same colleague: 'been busy...' adding what had happened to a number of babies during the night shift, and what staff on duty had been doing. She adds: 'Glad to be off, survived my nights tho' followed by a smiley face emoji.
11:42am: Dr Sudeshna Bhowmik records a list of 'problems' for Child N, including prematurity, jaundice and respiratory distress. A plan was to discuss with Alder Hey Children's Hospital haematology, and that discussion was carried out.
11:47am: A dose of vitamin K is prescribed for Child N during the day shift. Nurse Ashleigh Hudson records a 'slightly mucky aspirate' for Child N towards the end of the day shift, at about 6pm. The note of a summary of care between 8am-6pm records Child N was 'settled for the rest of the day', with 'minimal aspirates obtained. Aspirates clear with tiny old blood specks'. Paeds have liased with AHCH'
11:49am: Nurse Christopher Booth, at the time of the night shift handover for June 3-4, records at 8pm Child N was settled. A family communication note by nurse Hudson: 'Both parents updated on current condition and plan of care. Mum very anxious, worried about baby being in the incubator. Explained need for it, to keep baby warm and make observation easier...'
11:52am: The sequence of events goes up to June 4 at 3am, where Christopher Booth records 'No significant desaturations, bradycardias or apnoeic episodes observed overnight...'
12:18pm: Kate Tyndall, intelligence analyst for Cheshire Police, is now talking the court through the neonatal review schedule for the events in the case of Child N.
12:24pm: Prosecutor Philip Astbury says Dr Jennifer Loughnane will next give evidence. She confirms she is a consultant paediatrician at the Countess of Chester Hospital, and was employed as a registrar on the night shift of June 2/3, 2016.
12:28pm: She says she has no independent recollection of Child N or that night shift, other than that recorded in her notes. At 10.55pm, she carried out a routine review, which included an examination of Child N.
12:32pm: Dr Loughnane has noted Child N's history up to that point in the first 12 hours of his life, and noting a concern of a growth restriction during pregnancy, and the weight of 1.67kg indicating Child N was "a small baby". No risk factors for sepsis were detected. Child N was 'screened [for infection] - due to grunting at four hours'. The grunting was, the court hears, due to Child N having extra fluid in the lungs. Child N was 'self ventilating in air', 'respiratory rate 60', 'Sats 96% room air'
12:41pm: An antenatal plan had been put in place as Child N's mother was a haemophilia carrier. At 1.10am, Dr Loughnane is informed about Child having a desaturation. She does not recall who did so. The note at the time records: Child N 'got upset, looked mottled, dusky, sats 40%, O2 100%'. On my arrival, 40% O2, screaming, sternal recession, poor trace on Sats probe, pink'. The desaturation was "significant", Dr Loughnane tells the court.
12:43pm: Mr Astbury asks about the significance of the word 'screaming'. Dr Loughnane says that 'screaming' is not a word she would tend to write very often in her neonatal notes. She says that would indicate Child N was particularly upset.
12:50pm: Dr Loughnane said attempts were made to settle the baby, but was crash bleeped away. On her return, Child N's saturation levels recovered to 100%, and he was "asleep". The time of Dr Loughnane's return is not recorded. The plan was to continue to observe Child N and carry out the blood gas reading at 2am, indicating the note was made sometime before 2am. A blood gas reading is carried out at 2.04am, and Dr Loughnane says there is a raised lactate reading for Child N.
1:00pm: Benjamin Myers KC, for Letby's defence, is asking Dr Loughnane questions. He says Dr Loughnane covered a lot of areas of the hospital on that night shift. She replies the arrangement was standard for most hospitals. Mr Myers refers to notes made before the handover took place, in relation to Child N "intermittently grunting++" and an event of Child N desaturating to 67%. He asks if it is possible for a baby to desaturate because they are upset, via a 'false desaturation' from the Sats probe not picking up the trace. Dr Loughnane says that can be the case, but it would usually be recorded as such in the medical notes. The number on the oxygen saturation reading could be lower, or not be displayed at all.
1:05pm: Mr Myers asks about Child N 'screaming' and being 'pink', which he says if Child N had suffered a desaturation, he was "certainly recovering" from that. Dr Loughnane agrees. Mr Myers asks about the relevance of the 'poor trace on Sats probe'. Dr Loughnane says she had been told of the 40% sats reading, but on her arrival, she had seen Child N was pink. Mr Myers says there were no signs of Child N having any fresh blood anywhere. Dr Loughnane agrees. Dr Loughnane also agrees it is rare to be looking after a baby at the Countess of Chester Hospital - or any hospital - who has haemophilia.
1:10pm: Mr Myers says other than the raised lactate reading, the blood gas record at 2.04am was normal. Dr Loughnane agrees. The prosecution rise to clarify the '40% O2 (on my arrival)' note, and ask if that is a saturation reading or the oxygen support for Child N. Dr Loughnane says she cannot be sure, but believes it would be the latter. Mr Astbury says if the 40% oxygen saturation recorded by the nurse was inaccurate, it would have been noted as such in medical notes. Dr Loughnane agrees that would be the case. That completes Dr Loughnane's evidence.
2:11pm: The trial will resume imminently, with intelligence analyst Claire Hocknell returning to talk through the second sequence of events for Child N.
2:20pm: Firstly, a statement from Dr Sudeshna Bhowmik is read out to the court. Dr Bhowmik says tests were carried out on Child N for haemophilia. It was discussed with the parents that Child N would be taken to the neonatal unit due to his prematurity, and would need an incubator for temperature control. Child N had intermittent grunting at one hour of age, which was not unusual for babies born via C-section as there would be increased fluid in the lungs. The usual practice was to observe for four hours to see if the baby would settle down. Vitamin K was withheld on the risk of increased bruising/bleeding for Child N, until test results came back. Child N was later screened for sepsis as he had continued grunting beyond the four-hour observation period. He was breathing without any support required. He had had 'an episode' where he desaturated to 40%, with colour change noted, but had "settled thereafter" and did not need "supplementary oxygen for very long".
2:21pm: The rest of the examination by Dr Bhowmik on June 3 was "normal", and Child N was seen to be pink and well perfused, and doing "well from a respiratory point of view".
2:27pm: A statement from Caroline Oakley is read out to the court, in which the nurse describes Child N being born, transferred to the neonatal unit, and describes being aware the mother was a haemophilia carrier. Child N was dressed and placed in a 'hot cot'. He was 'grunting intermittently', which was not unusual. At 3pm, his temperature dropped to 36.4 degrees, and the temperature of the cot was increased to 39 degrees. Child N had a desaturation to 67% and was given 60% oxygen support, and was screened. Child N was presenting "quite typically" for a baby of his gestational age, and there were no overriding concerns at the time of the handover. A second statement by nurse Caroline Oakley said there was nothing to suggest the nasogastric tube had been moved, nor any difficulties with the tube being initially inserted.
2:30pm: Nurse Melanie Taylor, in her statement, says she "vaguely" remembers Child N by the name, but does not recall the shift. She confirmed she was the shift leader for the night of June 2/3, 2016. She was aware Child N had suffered a collapse during the night, but did not remember it happening or responding to it. Nurse Sophie Ellis, in her statement, says for the night shift of June 2/3, 2016, she had a vague memory of Child N as had haemophilia, which was unusual. She did not remember the details of the night shift she worked. She says she knows, from the notes, Child N had a collapse, but does not remember being involved in the efforts to stabilise Child N. She knows the collapse happened when Christopher Booth was on a break.
2:34pm: Christopher Booth, in his statement, is asked about the night shift he was on for June 2/3, 2016. He said he remembered Child N as it was unusual for a neonatal baby to be a haemophiliac. He adds his memory of the shift is "limited". He says he is "almost certain" he was caring for Child N that night. He recalls Child N was stable, with oxygen saturations "almost 100%, and "no abnormalities" presented. He says it was likely on the hour when he left for his one-hour meal break, saying he had "no concerns". He handed over care to a nurse, but does not recall who that was. When he returned from his break, he was "surprised" to learn Child N had become 'unsettled' and 'fractious' suffered a desaturation. He adds he had not been called back from his break.
2:35pm: Valerie Thomas, in her statement, says she does not recall Child N or the night shift of June 2/3, but does know she was on that night shift. She says she was likely working in nursery room 3 or 4. She knows Child N had collapsed when nurse Booth was on a break. She said it was "very unlikely" she would have been involved in any subsequent care.
2:37pm: Intelligence analyst Claire Hocknell has returned to court to talk the court through the second series (out of two) of the sequence of events for Child N.
2:45pm: The sequence says Child N continued to be cared for at the Countess of Chester Hospital's neonatal unit between June 3 and June 14. The rest of the sequence of events, presented electronically to the jury, begins from June 14, 2016. Lucy Letby is the designated nurse for Child N on the day shift of June 14. At 7.40am, Child N takes on a feed of expressed breast milk. Letby records notes at the handover at 8am. Letby messages a colleague to complain about having to finish up a previous shift' nurse's work, and had left a bottle 'dirty'.
2:51pm: Lucy Letby records regular temperature readings for Child N which are all recorded in a 'normal range'. The court had previously been told readings in the 'yellow area' (too high, or too low) would be considered abnormal, but none of the temperature readings recorded as being too high or too low. Letby notes: 'Demand feeding EBM via own bottle, completing more than required volumes....repeat SBR this morning on downward trend but not yet >50...otherwise ready for home'. In a family communication note: 'Mummy visiting this morning, carried out cares and feed. Put infant to breast. Discussed feeding at home' The notes show Child N was ready to go home, apart from further treatment required for jaundice, and was on phototherapy. Other family members visited Child N at the neonatal unit that day.
2:53pm: For the night shift of June 14, Child N was in nursery room 3. Nurse Jennifer Jones-Key, in a note written retrospectively, records Child N was 'nursed in incubator with eye protection insitu. Baby demand bottle feeding' at the start of the shift at 8pm.
3:01pm: Letby is involved in a WhatsApp message conversation with a nurse, and a Facebook messenger conversation with a doctor at this time. The nurse colleague complains about work colleagues on that night shift. Letby says she has had a "lovely run of shifts in 3". "Nice babies and parents" Letby messages the doctor to say she was planning to go to Torquay with her parents in July 2016, and discusses about her having had hypothyroidism since she was 11, and had 'blips over the past 12 months'.
3:04pm: A nursing note by Jennifer Jones-Key just after 1am on June 15 records Child N had become 'very unsettled' and was 'pale, mottled and veiny' with slight abdominal distension. A blood test was taken for analysis. Further observations are taken.
3:07pm: Letby messages her colleague at 5.10am: 'Awake already' Her colleague replies: "I wouldn't come in!"
Letby: "Oh...why" The colleague replies: "5 admissions, 1 vent"
LL: "OMG" Colleague: "Baby [N] screened, looks like s**t"3:12pm: Jennifer Jones-Key's note before 6am: 'baby looked worst this morning and cap refil after 3 secs. Reviewed again by paeds...' Letby messages a doctor colleague saying she might be back in '1' again for her next day shift, in nursery room 1.
3:17pm: Lucy Letby is recorded as entering the neonatal unit at 7.10am. She messages the doctor: "No repeat today. I've escaped being in 1, back in 3". The sequence of events shows Child N had a desaturation at 7.15am.
3:28pm: Jennifer Jones-Key records: 'at 0715 baby crying and dropped saturations - as seen by NNU nurse Lucy [Letby].'
3:31pm: The nurse adds Child N had to be given 100% oxygen support by a doctor. Child N was transferred to nursery room 1 at 8am. A note is made on the resiting of the NG Tube - 'NG resited in right nostril with acide reaction. At handover baby dropped saturations and required Neopuff. Care handed over to NNU nurse Lucy Letby'. Lucy Letby is recorded as being the designated nurse for the day shift on June 15, and records, in a note written retrospectively: 'Infant transferred to nursery 1 on handover. Mottled, desaturating requiring Neopuff and oxygen...cold to touch.'
3:35pm: Lucy Letby records, in a not written at 1.53pm for care at about 9am: 'Unable to intubate - fresh blood noted in mouth and yielded via suction ++.'
3:38pm: Letby messages her colleague on WhatsApp before 10am: 'Thanks for staying to help. Much appreciated.' Letby records '1ml fresh blood aspirated' from Child N at 10am.
3:42pm: A doctor colleague messages Lucy Letby before 11am to ask: "Is he ok?" Letby notes, at 11am: 'Small amount of fresh blood orally and 1ml from NG tube' Letby messages the doctor in response: 'Small amounts of blood from mouth & 1ml from NG. Looks like pulmonary bleed on xray... "Sorry if I was off during intubation...I like things to be tidy & calm (Well, as much as possible!)"
3:44pm: The doctor responds: "No, you were perfectly fine with me...I thought you were wanting to just get on with in case there was another desat."
3:47pm:
Letby replies: 'Well I have got my hair in a bun today, it's only fitting that I was 'serious Lucy' !!' Letby adds 'no more bleeding thankfully', in relation to Child N.
Friday 3rd March 2023
Child N
Police analyst: Recorded events & messages - Nurse Jennifer Jones-Key - Dr D (Registrar)10:00am: Nurse Lucy Letby's murder trial continues at Manchester Crown Court this morning. We'll be continuing to hear evidence in relation to Child N. Ms Letby is accused of attempting to murder the premature baby boy on three occasions in June 2016. She denies all charges.
10:35am: Cheshire Police intelligence analyst Kate Tyndall is taking the jury through sequencing evidence for June 15, when the Crown say Ms Letby twice attacked the boy
10:36am: Ms Letby's nursing notes from June 15 record that Child N was 'pale/mottled' and required oxygen support
10:39am: Ms Letby's notes state that Child N's parents had been informed and that they were 'understandably upset'
10:40am: At 14:50 on June 15, Ms Letby recorded that Child N had a profound desaturation. Notes state: 'Infant became apnoeic with desat to 44%. heart rate 90bpm. Fresh blood noted from mouth'...minutes later a number of senior medics were crash bleeped to attend the child
10:43am: Nursing notes record that there was difficulty trying to insert an ET tube. With two doctors failing to 'obtain a secure airway'
10:47am: Two consultants from the anaesthetic team were called to help, but they also had difficulty fitting an ET tube, the nursing notes show.
10:56am: Court now being shown messages between Ms Letby and colleagues that evening. A doctor, who cannot be named for legal reasons, asked her if she was okay and told her to cry if she needed to. Ms Letby responded: 'I’m ok just feel like ive been running around all day and not really achieved anything positive for him….don’t want to cry in front of people here maybe when I’m home'
10:57am: At the end of her shift, Ms Letby sent a WhatsApp message to a nursing colleague, who also cannot be named, saying: 'Losing the will'
11:04am: Notes from 19:40 on June 15 show that there was a further 'profound desaturation'. Child N had 'colour loss' and required neopuff breathing support
11:07am: At 19:48 the baby boy required resuscitation and a number of doses of adrenaline
11:24am: He eventually stabilised. Ms Letby said in a message to a colleague, who can't be named for legal reasons, that Child N's parents were present and had had the boy christened.
11:31am: Court has been shown numerous messages between Ms Letby and a doctor, who cannot be named for legal reasons. In one of those messages she asks 'What do you think caused his (Child N's) bleed?'
11:34am: The doctor responds: 'I think there will be a haemangioma or collection. If it was epiglottitis his crp should have been higher because he was starting to become unwell'
11:35am: Doctor says he's 'optimistic he'll be okay' Ms Letby responds: 'That's brilliant news, thanks for letting me know' - soon after the boy was discharged from Alder Hey hospital
12:10pm: Nursery nurse Jennifer Jones-Key is now in the witness box. She was on a night shift on 14 June 2016 and was Child N's designated nurse along with Neonatal assistant Lisa Walker. They took over Child N's care from Ms Letby, she tells the court there was no concerns on handover
12:14pm: Ms Jones-Key's nursing notes, written retrospectively at 5:51am on 15 June, state that 'just after 1am baby looked very pale mottled and veiny'
12:17pm: She recalls that over that morning Child N 'started to have a few desaturations' and was placed on full monitoring
12:24pm: Ms Jones-Key tells the court that Child N 'settled down' but 'from 7am onwards he was having more desaturations'
12:28pm: The nurse says shortly after 7am, Ms Letby came in to 'say hello'. At that point, she said 'I think the monitor went off, so Lucy went over to see. He went quite pale, I think he’d stopped breathing, I got the neopuff'
12:29pm: She's asked by the prosecutor where Ms Letby was in the room, she doesn't remember. She is asked again why Ms Letby was in the room - 'just to say hello, because we were friends', she says
12:31pm: She doesn't remember any conversation between them. She says the decision was taken to provide respiratory support to Child N . A nursing note from that morning states: 'noted to be mottled all over body and blue in colour and cold to touch'
12:41pm: Ben Myers KC, defending, is now questioning the nurse. He asks if Ms Letby was 'quite a good friend', 'Yes' she responds. He asks, in her opinion, if Ms Letby was a 'capable and hard working nurse', she agrees Mr Myers asks, in her knowledge, whether Ms Letby only gave 'the highest level of care' to the babies she cared for, she responds 'yes definitely’
12:49pm: Mr Myers is referring back to Child N's desaturation that morning, he says essentially Ms Letby said hello to Ms Jones-Key then responded when the baby boy's monitor went off - Ms Jones-Key agrees
2:28pm: A doctor, who cannot be named for legal reasons, is now in the witness box. She was working on June 15. She's taking the court over her notes from that day
2:45pm: The doctor has told the court she remembers the events of that evening and Ms Letby. She said the nurse 'she seemed quite agitated' when a team of specialists arrived from Alder Hey to help with Child N's treatment 'She approached me a few times and said who are these people, who are these people....from working alongside the nurses and doctors at Chester, I felt that it was out of character from what I’d experienced previously in a medical emergency', she said
3:47pm: Court now adjourned,
Chester Standard article 03-03-2023
MURDER-ACCUSED nurse Lucy Letby told a colleague she "wanted to cry" after a baby in her care had collapsed, her trial has heard.
She is accused of attempting three times to kill the infant, Child N, at the Countess of Chester Hospital's neo-natal unit.
The prosecution allege Letby, 33, made her first attempt on June 3, 2016, hours after exchanging messages with a friend who teased her for being "flirty" with a doctor.
On June 15 – when she is alleged to have made two more bids to murder Child N – she swapped Facebook messages with the same doctor, who cannot be identified for legal reasons, the court heard.
Manchester Crown Court heard that the registrar, who was working nights, messaged Letby: "Only a few hours to go and it's holiday time – do you think you'll manage to hand over quickly?
At about 5.25pm Letby replied: "I'll still be here. He's (Child N) poorly, bled again and became apnoeic.
"Sat having a quiet moment and want to cry. Just mad with so many people and lack of space etc."
The doctor said: "Oh Lucy, poor little thing and you.
"Are you OK? Have a cry, you'll feel better for it I'm sure. You're welcome to take my car home if you're too tired to walk. I sort out picking it up in the morning.
"So sorry you've had a rubbish day at the end of your long run – holiday well and truly deserved."
Letby responded: " I'm OK just feel like I've been running around all day and not really achieved anything positive for him.
"Don't want to cry in front of people here, maybe when I'm home! That's very kind re the (car) but should be OK. Have you managed to switch off at all and sleep?"
The doctor messaged: "No not really. Your day sounds as though as it's been horrible. Poor you. Are you going to be OK?
"I'm sure he's had the best care possible today and that you will have done everything you can for him.
"Are you doing anything nice before you go on holiday? You're not having to do a long run of shifts to get the time off for that are you?"
Letby said: "No off for nearly 2 weeks!"
The doctor replied: "Oh what an end to a rubbish day. I haven't been back to Torbay for a few years .. I'm always surprised how little it changes when I go back. Happy memories.
"I used to love Cockington in the summer – it always looked so pretty when the flowers were out. Have you handed over yet?" He added: "Look on the top shelf. Right hand side. For the walk home. Your still welcome to the car."
Letby replied: "Cockington is gorgeous!! We always go there for afternoon tea. Dad was offered a job in Paignton many moons ago, could have been a very different childhood growing up by the sea. Looking forward to going back.
"Hope little man is OK and your night isn't too stressful. On the home straight now at least.
"You are a sweetie (name of doctor), thank you."
The doctor messaged: "Chocolate makes bad days a little better. Hope you liked it."
Letby said: "That's true. Just a shame I don't usually eat chocolate … but on this occasion …"
The doctor replied: "It was well deserved today. Are you OK?
Letby said: "Yes thank you . Just glad he's (Child N) OK.
"Hopefully I'll sleep well tonight and can enjoy getting ready for hols. Are you OK?"
The doctor said: "He's just left the building. I'd be surprised if you didnt sleep well after so many long days zzz."
Letby said: "Glad he got off safely."
The doctor replied: "My night is complete! Just been handed a 3-week-old for a cuddle, who am I to refuse!!"
Letby messaged: "Aww baby cuddles make everything seem better."
Letby, originally from Hereford, is said to have attempted to murder Child N shortly after she arrived for her day shift on the morning of June 15 and later at about 3pm.
She denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Monday 6th March 2023
Child N
Dr Huw Mayberry - Dr A - Dr John Gibbs - Dr Stephen Brearey - Dr Francis Potter (Alder Hey)10:16am: I'll be bringing live updates from Manchester Crown Court this morning where the murder trial of nurse Lucy Letby continues. We'll be hearing evidence in relation to Child N, who the Crown say Ms Letby tried to kill on 3 occasions in June 2016. She denies all charges.
10:35am: Dr Huw Mayberry is first to give evidence today - via live link from Australia. Dr Mayberry currently works as a registrar in Melbourne, back in 2016 he was at the Countess of Chester Hospital
10:37am: Dr Mayberry is being asked about the events of June 15, 2016. Child N crashed several times throughout that day - at one point requiring full resuscitation and six doses of adrenaline
10:38am: Dr Mayberry was crash bleeped to attend the neonatal unite at around 15:00 due to a 'sudden desaturation following 3ml aspirate of blood from NG (tube)'
10:43am: The doctor tells the court he tried to intubate Child N, but he 'was unable to get a very clear view because there was substantial swelling within the airway'. He said that this swelling was 'unlike anything I had encountered previously'
10:45am: He said the infant's epiglottis (flap of tissue at the back of the throat) was 'quite swollen, it looked quite large and reddy pink in colour'. He adds 'I had not seen this in my practice before, only in textbooks'
10:46am: He tells the court that his initial thought was that this could be epiglottitis - this often caused by an infection, but can also sometimes happen as a result of a throat injury
10:53am: Dr Mayberry tells the court that he does not recall seeing any blood in Child N's throat. Asked if he could he could give a cause for the swelling, he says 'no it’s not something I've had much experience of'
10:56am: Ben Myers KC, defending, is now questioning Dr Mayberry. He asks in his professional opinion what can be the cause of blood - he says he told Cheshire Police it could have been a result of gastric irritation or Necrotising enterocolitis (NEC)
10:58am: He says it could also have been a result of Child N's blood disorder, which resulted in a deficiency of an essential blood-clotting protein
11:06am: We're now hearing from another doctor [Dr A], who cannot be named for legal reasons, about the events of June 15.
11:11am: The medic tells the court that he recalls Child N as he had trouble trying to intubate him, he says 'which for me is not a frequent occurrence'
11:16am: Notes from the early hours of June 15 show that [Dr A] ordered a blood test as Child N was mottled in appearance and he wasn't sure why
11:25am: The mottling eventually resolved, but over the next few hours Child N suffered five desaturations. [Dr A] said this made him think the baby boy had an infection. A septic screen of his bloods was then ordered
11:44am: He tells the court that results ruled out infection as a cause. He said there was some concern about blood 'not being delivered to the skin in way that is normal'. By 8am on 15 June, Child N's mottling had returned. [Dr A] took the decision to move him to Nursery 1 Nursery 1 allows for more intensive care and treatment
11:56am: [Dr A] tells the court that on that morning he took the decision to intubate Child N and put him onto a ventilator. He recalls seeing 'unusual' swelling and blood in the back of the baby boy's throat
11:58am: After three unsuccessful attempts to intubate, [Dr A] abandoned the procedure. His note from that morning states: 'intubation abandoned due to blood present at oropharynx and likelihood of trauma due to repeated attempts' Child N was then placed on non-invasive respiratory support
12:08pm: Ms Letby's defence lawyer Ben Myers KC is now questioning [Dr A].
12:37pm: Myers is asking [Dr A] when he saw the blood in Child N's throat. He said 'I believe blood was there at insertion attempt number one' Myers puts it to him that 'if you can't see, you wouldn't attempt it?' He replies: ‘You can do, if quite certain of position'
12:42pm: Mr Myers has just quoted [Dr A]'s police statement from 2018. In this he says he was 'not sure' if the bleeding was his 'fault' due to his attempts to move the tongue with a medical implement to intubate
2:00pm: We're back after a short break. Retired consultant paediatrician Dr John Gibbs is now in the witness box. He was called to attend Child N at around 16:00 on June 15
2:04pm: Citing his notes, Dr Gibbs recalls that a specialist team had been called to help doctors with Child N's breathing (due to various problems with trying to intubate)
2:15pm: The team from Alder Hey Children's Hospital arrived in Chester at 19:20. They were made up of experienced intensive care consultants and an ear, nose and throat surgeon. Plan was to take Child N try to intubate, if that failed an emergency tracheostomy would take place
2:17pm: Dr Gibbs tells the court that Child N suffered a 'sudden deterioration' before the team could carry out the procedure however. Heart rate dropped to 60bpm, oxygen dropped to 40% - 'clear he was not being ventilated properly', Dr Gibbs said
2:22pm: At this point, Dr Gibbs said chest compressions were started and six doses of adrenaline were given over 30mins. A specialist doctor from Alder Hey also finally managed to intubate the baby, which allowed him to be placed on a ventilator
2:30pm: Asked for his conclusions about the events of June 15, Dr Gibbs says the blood could have been a result of a bleed on the lung - but adds 'why (Child N) had that swelling documented by colleagues, I really don’t know'
2:36pm: Dr Gibbs says that 'in the end I don’t think infection was the cause' of Child N's collapse
2:48pm: Dr Stephen Brearey is now in the witness box. He was on duty on the afternoon of June 15. He was called to help with Child N by a colleague as doctors were having difficulty intubating the infant
2:52pm: Dr Brearey made an unsuccessful attempt to intubate the baby boy. He tells the court from reviewing his notes it wasn't successful due to blood and swelling at the back of Child N's throat, which blocked vision of his airway
3:21pm: Mr Myers is now questioning Dr Brearey, he's asking him about Child N's blood disorder, which increases the risk of bleeding
3:34pm: Mr Myers is taking the court back over notes of that day, they show that there was seven attempts to intubate Child N (before Alder Hey team succeeded). Mr Myers asks if this is something that should have been possible to do, he replies 'in normal circumstances yes'
3:42pm: The medic tells the court that he 'can think of no natural, normal cause for why (Child N) deteriorated multiple times' and then improved afterwards at Alder Hey
3:43pm: Dr Francis Potter is now in the witness box. He was part of the Alder Hey team that assisted on June 15 - he said he remembers the case as it was 'quite unusual' for his team to get a call to go out and assist
3:57pm: He says when he arrived Child N was 'mottled and grey' in appearance - he recalls starting use of a bag and mask to ventilate the baby boy. When this didn't work, chest compressions were commenced
4:09pm: Dr Potter says after Child N stabilised and was transported to Alder Hey he recovered 'fairly rapidly' - within 48hrs he had left intensive care
4:24pm: Mr Myers is now questioning the medic. He asks whether repeated attempts to intubate could cause stress to the baby, he says it would cause stress to the person trying to intubate
4:27pm: He said 'failure makes the second attempt more difficult and third more difficult'...he adds that rather than making repeated attempts, they should be limited and someone with more experience should be called to help quickly
Chester Standard article 06-03-2023
AN "unusual" presence of blood and swelling was seen in the throat of a baby allegedly attacked by nurse Lucy Letby, a jury heard.
She is accused of attempting three times to kill the infant, Child N, at the Countess of Chester Hospital's neo-natal unit.
Letby allegedly made her first attempt on June 3, 2016 and then tried twice more 12 days later – shortly after she started her day shift and again in the mid-afternoon.
A registrar doctor, who cannot be identified for legal reasons, told Manchester Crown Court on Monday, March 6, how he was asked to review Child N from about 7.30am on June 15.
The youngster had suffered a "profound" drop in blood oxygen levels and a falling heart rate.
He said he made three unsuccessful attempts to insert a breathing tube so Child N could be mechanically ventilated.
Giving evidence on Monday, [Dr A] said: "I saw blood at the back of the throat … that prevented me from seeing where the entry to his airway was."
He said he also noticed "a degree of swelling".
Prosecutor Simon Driver asked: " What did you notice first?"
[Dr A] replied: "I think I will have seen the blood first because that is such an unusual thing to see at the time of intubation."
He said he could not see where the blood was coming from or what had caused the swelling.
[Dr A] told Ben Myers KC, defending, that he had told police in 2018 that he was not sure if he had "inadvertently" caused the bleed during the procedure.
He agreed that because of Child N's haemophilia – an inherited blood clotting disorder – there was a concern he would bleed.
Another doctor told the court he too could not intubate Child N following a further sudden deterioration in the afternoon, after 3ml of blood was withdrawn from his nasogastric tube.
Dr Huw Mayberry said: "I could see the vocal cords but I was unable to get a very clear view because there was substantial swelling within the airway.
"The swelling was unlike anything I had encountered previously. It looked quite large and reddy-pink in colour."
Retired consultant paediatrician Dr John Gibbs told the court that Child N was "progressing very well" up until June 15, and he understood he was ready to go home.
However at about 7.40pm, Child N's blood oxygen levels and heart rate plummeted again.
Chest compressions followed and six doses of adrenaline were given to stimulate his heart before he recovered after about 30 minutes, he said.
Dr Gibbs said the "serious life-threatening deterioration" only improved after a consultant anaesthetist, called from Liverpool's Alder Hey Children's Hospital, managed to intubate at his first attempt.
He told the court he "couldn't understand" why two consultants, two registrars and two anaesthetists had failed previously to intubate Child N throughout the day, but said the adrenaline may have helped reduce the swelling.
Dr Stephen Brearey, the lead consultant at the neo-natal unit, said he "could not think of a natural cause" why Child N had multiple deteriorations on June 15.
Alder Hey anaesthetist Dr Francis Potter told jurors that he did not see blood or swelling in Child N's throat when he successfully inserted the breathing tube.
Following his transfer to Alder Hey, Dr Potter said Child N's stay was "fairly uneventful", although there were episodes of "apnoea" in which he would temporarily stop breathing.
Dr Potter said apnoea could simply be a sign a child was unwell or it could have a more specific reason.
He said Child N was breathing for himself and off intensive care by June 18 before he was discharged later that month.
Dr Potter agreed with Mr Myers that Child N was readmitted on July 3 with further episodes of apnoea, but no explanation was found and the situation settled after he was given breathing support.
In his opening address last October, Mr Myers told the jury that Child N was another baby who received "suboptimal care" and should have been treated elsewhere at a specialist tertiary unit, rather than at the Countess of Chester.
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Tuesday 7th March 2023
Child N
Statements from doctors & nurses - Elizabeth Morgan (Cheshire Police Nursing Advisor) - Professor Sally Kinsey - Dr Dewi Evans - Dr Sandie Bohin10:22am: Nurse Lucy Letby's murder trial continues at Manchester Crown Court this morning. We'll be hearing evidence in relation to a baby boy, Child N, who Ms Letby is accused of trying to kill on three occasions in June 2016. She denies all charges.
10:33am: The prosecution allege Ms Letby made her first attempt on Child N's life on 3 June, before carrying out two more attacks on 15 June. The Crown say Child N's deteriorations were consistent with some kind of "inflicted injury" or him having received an injection of air.
10:44am: Jury are currently being read statements of agreed evidence from doctors and nurses who worked 15 June. They're in relation to the treatment of Child N, who crashed several times that day
11:07am: A nurse, who cannot be named for legal reasons, said in her statement that she remembers being 'shocked' at Child N's deterioration that day. She said that he was previously stable and ready to go home that day
11:13am: Court being read a statement from Independent Nursing Healthcare Advisor Elizabeth Morgan, who was asked by Cheshire Police whether Ms Letby's 'failure' to alert other medics that fresh blood had been aspirated from Child N's mouth that day fits with 'good practice' Ms Morgan said in her professional opinion, it would be 'standard good practice' to escalate anything unusual - first verbally and then later recoded
11:24am: Blood expert Prof Sally Kinsey is now in the witness box. She was approached to review Child N's case
11:30am: Child N has a rare blood disease, Prof Kinsey is explains to the jury that this can cause 'catastrophic' bleeding following minor injury. Child N had a 'moderate' variant of the condition, she tells the court
11:56am: Prof Kinsey is asked whether the blood seen in Child N's throat that day could have been caused as a result of self-injury or a spontaneous bleed due to his blood condition - she says no
12:14pm: Ben Myers KC, defending, is now questioning the witness. He says his questioning will focus on whether a physical act can be established for causing the bleed
12:34pm: Prof Kinsey tells the court that Child N's blood disorder did make him "more likely to bleed", but said: "He won’t just bleed for no reason."
12:35pm: Medical expert Dr Dewi Evans is now in the witness box, he was asked to review the case by Cheshire Police.
12:37pm: Dr Evans’ opinion is that the bleeding in Child N's throat was not caused by the attempts to intubate, but instead some preceding trauma
12:41pm: Dr Evans says Child N's 'progress was pretty uneventful' and was 'making satisfactory progress for a baby that was premature but otherwise well' in the weeks from birth to 15 June
12:49pm: Court being taken back over timeline of Child N's crashes on 15 June - which culminated in CPR and him having six doses of adrenaline, before he was eventually transferred to Alder Hey Hospital
12:56pm: Dr Evans is giving his analysis on Child N's first collapse on June 3. The baby suffered a profound and sudden collapse in the early hours of that day. This was preceded by, what one doctor recalled, as 'screaming' - Dr Evans said that is 'very unusual' for a child of this age
12:57pm: Dr Evans says he went and reviewed scientific research papers on air embolus (injection of air) - these found that in some cases where babies had been injected accidently with air, there was a period of screaming before desaturation an death
12:58pm: He said what happened with Child N was 'repeated' in what we have seen in previous cases
1:07pm: On the 15 June incident, Dr Evans said in his opinion the bleeding 'was a result of trauma to his upper airway'
2:06pm: We're back after a short break. Ms Letby's defence lawyer Ben Myers KC is now questioning Dr Evans
2:11pm: Mr Myers points out that Dr Evans wrote several reports on the collapse of Child N. In his first report written in 2018, the medic didn't mention the incident on 3 June. He tells Mr Myers he 'overlooked' it and later included in subsequent reports
2:12pm: Mr Myers says 'if you considered it significant you would have said so in your first report'
2:17pm: Mr Myers puts it to Dr Evans that there is 'nothing' in the medical notes for Child N 'to support a suggestion that there was an inflicted injury'. Dr Evans disagrees, he says that was his opinion when he authored his report in 2019 and says 'that is my opinion now'
2:36pm: On whether Child N had received an injection of air on 3 June, Mr Myers put it to Dr Evans that there was no evidence of an injection of air and that the medic was attempting "to work a piece of evidence in to support" his theory on air embolus. He disagreed and said he was "applying standard clinical practice" in his review and said it was written with knowledge of previous babies in this case. "I think that we have to seriously consider that this baby was a victim of air embolus on 3 June", he said.
2:59pm: Mr Myers has just been questioning Dr Evans about how he was approached to review these cases. He says he was approached. Mr Myers pulls up an email from 2017 that Dr Evans sent to the National Crime Agency telling them the death's at Chester 'sound like my kind of case'
3:00pm: He accuses Dr Evans of 'touting for work' and says he was using his review to 'fit the allegation not the facts'. He puts it to him that air embolus was mentioned to him by Cheshire Police before the review, he denies accusations - accuses Myers of 'going on a wild goose chase'
3:34pm: Dr Sandie Bohin, who also reviewed the case, is now in the witness box. She said the bleeding suffered by Child N on 15 June could have been caused by 'local trauma to the mouth'
3:45pm: On the incident on 3 June, Dr Bohin says she has 'never experienced' a neonatal baby crying for 30mins. She says it is an 'extraordinarily long' time and puts it down to an 'inflicted painful stimulus'
5:06pm: Back tomorrow
Chester Standard article 07-03-2023
A MEDIC has denied "touting" for the job of assisting a police probe into baby deaths and "giving them what they wanted", the murder trial of Lucy Letby heard.
Letby, 33, is accused of the murders of seven infants and the attempted murders of 10 others when she worked as a nurse at the Countess of Chester Hospital's neo-natal unit.
Retired consultant paediatrician Dr Dewi Evans has been called by the prosecution to give expert evidence to the court, after he was tasked by Cheshire Police in the summer of 2017 to look at a series of collapses on the unit.
Dr Evans went on to write a number of reports about his findings, Manchester Crown Court has been told.
On Tuesday, March 6, jurors were read an email sent by Dr Evans to the National Crime Agency (NCA) in May 2017, ahead of his involvement with Cheshire Police.
In his message to "Nick" at the NCA's national injuries database, Dr Evans wrote: "Incidentally I've read about the high rate of babies in Chester and that the police are investigating.
"Do they have a paediatric/neonatal contact? I was involved in neonatal medicine for 30 years including leading the intensive care set-up in Swansea. I've also prepared numerous neonatal cases where clinical negligence was alleged.
"If the Chester police had no-one in mind I'd be interested to help. Sounds like my kind of case.
"I understand that the Royal College (of Paediatrics and Child Health) has been involved but from my experience the police are far better at investigating this sort of problem."
Ben Myers KC, defending, said to Dr Evans: "This is you putting yourself forward. In effect, touting for this job."
Dr Evans replied: "I was offering my professional opinion if that was in their interest."
Mr Myers said: "It's you ready to give them what they wanted, Dr Evans?
The witness said: "No, no. I have dealt with several police cases where I have said 'this case doesn't cross the threshold of suspicious death or injury', or whatever.
"My opinions are impartial and independent.
"I also give evidence to law firms representing defendants. In the last five years I have given more reports relating to defendants than the police or the prosecution."
Mr Myers went on: "At some point before you started writing reports you were told by the police about suspicious rashes and air embolus, weren't you?"
Dr Evans said: "That is completely untrue. It's totally untrue.
"The first time I heard a local doctor mention air embolus was a couple of weeks ago.
"The first person I know to raise the area of air embolus was me. I did that in case number one and I thought 'oh my god, what is going on here?'
"I was not told anything about any suspect. I knew absolutely nothing."
Last month Countess of Chester consultant Dr Ravi Jayaram told the jury a "chill went down my spine" in June 2016 when he read a research paper that described the effects of air embolism.
He said it "fitted" with the fleeting appearance of purple and pink patches seen on the skin of a number of collapsed babies that he and colleagues had treated.
Letby is accused of attacking several of her alleged victims by injecting air into their circulation and causing an air embolism – a blockage in their blood supply.
The defendant, originally from Hereford, denies all the offences said to have taken place between June 2015 and June 2016.
Wednesday 8th March 2023
Children O & P (triplets)
Statements from mother & grandmother, father's statement by video
Child O
Police Analyst: Recorded events & messages - Statements of Dr B & Nurse Kate Bissell - Nurse Sophie EllisChester Standard Live Reporting
9:19am: Today the prosecution is expected to begin delivering evidence in the case of Child O, the 15th of the 17 babies, chronologically, that the Crown allege Lucy Letby murdered or attempted to murder. The defence deny this.
9:22am: Previously, the prosecution said in the opening that Child O was one of three triplet brothers born at the Countess of Chester Hospital on June 21, 2016. The prosecution say Lucy Letby murdered Child O, and brother Child P, on June 23 and June 24 respectively.
10:23am: The trial is due to resume at 10.30am.
10:35am: Members of the jury are now coming in to court.
10:39am: The prosecution is now beginning its evidence for Child O and Child P, two boys who were triplets born on June 21, 2016 at the Countess of Chester Hospital. Simon Driver, prosecuting, tells the jury the case of Child O will be heard first, over the next few days, before the case of Child P begins.
10:42am: A statement from the mother of Child O, Child P and the other triplet is read out to the court. She says she had a 12-week scan at the Countess of Chester Hospital 'which seemed to take a bit longer than normal', where her partner realised there was more than one baby. It was confirmed she had triplets. The triplets would be identical, she was informed, and she was referred to Liverpool Women's Hospital to see a specialist. She was informed there was an 80% chance one of the triplets would be smaller than the other two.
10:46am: Two weeks later she went for a follow-up scan, and everything was 'fine', as were further fortnightly scans. She was informed the triplets were 'unlikely' to stay at the Countess of Chester Hospital neonatal unit, as there would not be the space for three nursery beds, and they may have to be treated at Birmingham. On June 21, the mother was admitted to the Countess of Chester Hospital, was assessed, and advised to go for a C-section. She went to theatre at 2pm, and the triplet boys were born shortly afterwards. They had been named in advance, and the babies were named in the order they came out. In recovery, she was brought pictures with the boys and their birth weights recorded.
10:47am: The mother was taken to see all the baby boys, and handled all of them. On the neonatal unit, there "didn't seem to be any routine for washing hands". All the triplets were in nursery room 1, and they were all brain scanned, with no concerns.
10:49am: The following day, the mother was taken to see the triplets, and was informed all were doing well. She said she asked on numerous occasions, about expressing milk, but no-one came to help until after Child O passed away, when a nurse called Lucy handed her an information leaflet.
10:52am: On June 23, the mother was in the ward and still struggling to walk. About 10-15 minutes after the father had been to the unit, he came back with a consultant doctor, who informed her Child O's stomach had swollen and 'needed a little help to breathe, so a tube had been put down his throat'. He was calm and said this was normal. The mother was put into a wheelchair, and upon arrival at the nursery, she said: "By the time I got there, it was a scene of chaos". A lot of doctors and staff surrounded Child O. "I remember nurse Lucy was there, all the time."
"The staff appeared to be in a state of panic, and it didn't seem controlled at all." The mother said she sat outside, and could not bring herself to be too close, as Child O kept arresting and changing colour. "He was swollen all over his body".10:55am: At some point, another doctor arrived and told the mother "things weren't looking good" for Child O, and said if he did survive, he would likely have brain damage. Child O passed away at 5pm. Child P and the other boy were in nursery room 2. The mother said: "This whole episode had come like a bolt out of the blue. On the face of it, everything seemed to be going well with the triplets. "As a family, we were naturally devastated. "With hindsight, there were a number of things we found unusual." The mother said she didn't expect a student nurse to be looking after one of the babies. She said they kept seeking reassurance that the other two boys were fine.
10:57am: A doctor [Dr B], who was "quite upset", said she was very sorry for what had happened to Child O, and photos were taken of the baby boy. The mother said she didn't sleep at all that night. She, at one point, asked the midwife to check if the other two boys were ok. She was reassured they were fine. The following day, they went to the neonatal unit and were informed by a nurse the two boys had "been like angels", behaving all night and feeding regularly.
10:59am: The mother recalled having breakfast and freshening up. She then heard voices and saw a midwife was present and advised to go to the neonatal unit, as Child P was unwell. "I was devastated. A couple of hours earlier he had been fine. "I called my mum to tell her it was happening again." When she arrived, she said it was "like deja vu" and the situation was "chaotic" with people "running around" in nursery room 2, where both boys were.
11:03am: The mother said she sat outside "for long periods of time". At one point, a young doctor looked to be Googling 'how to insert a line'. They needed to do this process as Child P's lungs had collapsed during CPR. "This alarmed me". The mother was informed they were looking to transfer Child P to Liverpool, but they needed to stabilise the baby first as he kept collapsing. She was told things were "looking a lot more hopeful" for Child P - he looked veiny, but his stomach was not distended like Child O's was. At some point, the transport team arrived. The reaction from the transport team was "incredible to watch" as "they just took over". Even the consultant took a back seat'. "We were reassured, he seemed calm." Child P passed away. The mother said she and her partner "begged" the transport team to take the surviving boy with him to Liverpool Women's Hospital.
11:07am: The mother said she had to discharge herself from the Countess of Chester Hospital, and asked for her care to be transferred to Liverpool. "They refused, which was the last thing I needed." The mother travelled to Liverpool, having stopped to pick up some clothes along the way, and were . "We were just made to feel at ease - the two hospitals felt like night and day." The staff said the surviving baby boy could be treated there for as long as there was a bed available, but did not need intensive treatment. The surviving baby stayed at the hospital for three and a half weeks. The mother said she was "surprised" there was not 1:1 nursing care for the triplets, and a student nurse was looking after them, with Lucy Letby 'popping in'. Lucy Letby was "extremely emotional" and "in pieces" after Child P passed away. She was "in floods of tears", the mother said. A doctor also arrived and "was also upset".
11:18am: A statement from the grandmother of the triplets is now being read out. She said she was aware the triplets were identical and couldn't be told apart, apart from their identity tags, and were in differently coloured blankets, and were all of good weight. "All was well, up until June 23." She was informed "something was wrong" with Child O. She left work and travelled to the hospital, and upon arrival, Child O was being baptised, and the parents were "hysterical" and "at a loss". The grandmother recalls Lucy Letby was there, and was "softly spoken". Child O continued to deteriorate, and a Dr John Gibbs was called to the unit, who asked Lucy Letby how many shots of adrenaline had been administered, and Lucy said she was not sure, three or four. Dr Gibbs replied: "Well, what was it, Three or four?" Lucy Letby appeared to be referring to a scrap of paper for records which had yet to be updated. Lucy Letby was in the unit, and the grandmother said: "I remember thanking her for her assistance during the ordeal." The grandmother said she could not recall what happened with Child O, as she was too busy consoling the parents. When she received the "awful call" about Child P being unwell, the grandmother was at home. She arrived at the hospital and saw a number of doctors surrounding Child P. There had been "a significant improvement" in Child P's condition. His condition 'seemed fine' for an hour or two, but then took a dramatic turn for the worse. Outside the nursery room, a nurse researched a procedure on a desktop computer. "I was a little surprised at this, as I assumed the staff knew what they were doing. I thought they were possibly just confirming the procedure." Child P continued deteriorating and the call was made to transfer him to Liverpool, but Child P sadly passed away. It was decided that as the transport team were already present, they would take the surviving boy to Liverpool Women's Hospital, as they were not sure if there was a congenital condition. A doctor informed the family there would be post-mortems for Child O and Child P to establish the causes of death.
11:26am: A 15-minute video interview is now being played, as agreed evidence, with the father of the triplets. The video interview was recorded in December 2019. He says, for June 23, the scene was "a mess". He recalls being taken to the unit by a nurse 'asap', "there's something going on". He said he and the mother both "panicked". He recalls there was "definitely swelling" on Child O, but could not recall why, and, getting upset and pointing to his hands, he says there were 'bright blue' veins.
11:30am: He said medical staff were doing 'not a lot', and seemed to be concentrating on Child O's temperature. He said there were "lots of people, rushing in and out". He recalls seeing a 'pot belly' appearance for Child O, which then had 'gone down'. The ordeal lasted "ages" for Child O. It "seemed like hours". The doctor could offer 'no explanation' for what had happened to Child O which has resulted in him dying, the father recalls.
11:38am: The interview talks about the events of June 24. The father recalls having spent time with the two boys. He recalls the scene for Child P was "worse than the day before", and was "pandemonium". He said there was nothing of the sign for Child P of a swollen belly. He said the medical staff did not have any explanation for why Child P was unwell. The transport team arrived, but Child P passed away within 10-15 minutes. He recalls he and the mother asked the transport team to take the surviving baby boy to Liverpool Women's Hospital. The father adds: "I am sure it was Lucy Letby who wheeled the two boys to us. She said how sorry she was. "I'm pretty certain she dressed them up." He said it was Lucy Letby's job to do up the memory box, which included an SD card containing memories of Child O and Child P. The surviving baby stayed in Liverpool for 'about 11 days' and there were 'no complications at all' apart from a 'small hole in his heart', and remained stable.
11:55am: Intelligence analyst Kate Tyndall is now talking through the sequence of events for Child O, who was born at 2.24pm on June 21, 2016, the second of the three triplets born. Child O was born in 'good condition', 'cried immediately' and had a 'good tone' and a heart rate over 100bpm. He weighed 2.02kg - 4lb 7oz.
11:58am: The sequence of events then records what happens from 1pm on June 22. Child O had been admitted to the neonatal unit after birth and cared for there. The court hears during this time, Lucy Letby is on holiday in Ibiza. She is informed by a doctor colleague [Dr A] via Facebook Messenger that triplets have been born and are being cared for at the neonatal unit.
12:02pm: Letby responds to a WhatsApp from colleague Jennifer Jones-Key that she is working Thursday, Friday and Saturday, on her return from holiday. She adds: "Yep probably be back in with a bang lol"
12:05pm: [Dr A] Facebook messages Letby on Wednesday, June 22 at 5.13pm: 'How was the flight?...Day has been rubbish. Lots of unnecessary stress for nnu and too much work to fit into one day. I may have (over)filled the unit again..."
Letby: "...Oh that's not good back to earth with a bump for me tomorrow then!..." [Dr A]: "...Yes, you might be a bit busy..."12:08pm: A nursing note by Samantha O'Brien at 6.29pm on Wednesday records: 'No signs of increased work of breathing...CBG carried out this AM at 1045, good result....respiratory rate remains stable. Baby nursed in incubator...temp within normal limits.' Fluid requirements checked and correct...10% dextrose infusing via cannula in left hand, site became puffy throughout day....feeds of donor EBM also commenced at 1300hr, currently having 4mls 2 hr...'
12:13pm: Letby messages [Dr A] 'Yep just got a few bits for lunch (although maybe I won't have time to eat).
[Dr A] replies he wasn't sure he'd eaten apart from a cereal bar before the triplets arrived.
Letby asks: "What gestation are the trips? I don't mind being busy anyway..."
[Dr A]: "33+5 [weeks gestation]. 3x Optiflo..."
After more messages, [Dr A] asks Letby if she has any choice where she is working.
Letby: "No, not with this new handover. Shift leader of night shift allocates for the day shift and vice versa. If your on a run of shifts you tend to stay with same babies."
Letby adds due to the skillsets, she tends to work in nursery room 1.12:16pm: Letby adds she feels "most at home with ITU [intensive treatment unit] and the girls know that Im quite happy to be in 1 so works out well most of the time."
[Dr A] replies: "...I like it when you're in itu - everything feels safe and well organised..."
Letby: "Awe that's nice to hear, Huw often says that too - see what happens tomorrow."
Letby adds there is a potential job opening on the unit which she believes she might be lined up for.12:18pm: [Dr A]: 'If you didn't want it now, could you defer?'
Letby: 'Yes good to know and worth thinking about...& yes, I'm sure she would let me defer.'12:20pm: Nurse Sophie Ellis records, on the night shift for Child O, in a note written at 2.19am on June 23: '[incubator] temperature reduced due to temperature of 37.3C - to check hourly as appropriate. All other observations stable. Pink, warm and well perfused....abdo full but soft.'
12:24pm: A note at 6.41am recorded a TPN nutrition bag was stopped as Child O had reached full feeds of donor expressed breast milk, and was 'tolerating well'. At 7.32am 'abdo loos full slightly loopy. Appeared uncomfortable after feed.' Child O was checked and settled. The day shift begins at 7.30am. During this shift, Child O died.
12:26pm: A rota for the day shift records four babies in nursery 1, three in nursery 2 - including Child O and Child P, three in room 3 and two in room 4. Samantha O'Brien is the designated nurse in room 1 for the other triplet, Christopher Booth is the designated nurse for Child Q in room 1, Lucy Letby is the designated nurse for Child O and Child P and one other baby in room 2.
12:29pm: Letby records, for Child O:...'Observations within normal range...nil increased work of breathing. Donor EBM via NH tube. Minimal milk aspirates obtained...'
Letby messages a colleague after 8.30am to say she had a student nurse in but 'no time to do anything'.
Letby adds: 'She's nice enough but bit hard going to start from scratch with everything when got 3 babies I don't know and 2 hourly. Ah well...'
The WhatsApp conversation continues over the following hour.12:32pm: Dr Katarzyna Cooke records for Child O: 'No nursing concerns observations normal'. The plan was to continue weaning Optiflo, establishing feeds and prescribing vitamins for Child O.
Letby messages a doctor colleague [Dr A] to ask if he will be present in the NNU after he has been at the clinic.
[Dr A] replies he is.
Letby adds the student is 'glued to her'.12:36pm: Letby messages the doctor: 'I lost my handover sheet - found it in the donor milk freezer!! (Clearly I should still be in Ibiza)'
[Dr A] adds he 'dropped some sweets off to keep everyone going'
Letby: 'Ahh wondered where they had come from'
Letby adds she had forgotten her sandwich, and jokingly asks if she can go home.
[Dr A] replies there's a cheese roll going spare, then offers to get her something for lunch.
Letby replies: 'Tapas?'
She adds: 'It's ok thanks I've got a few bits with me'
Vitamins are prescribed for Child O.12:41pm: [Dr A] records a brain scan for Child O at 12.10pm, noting normal observations. Letby records a fluid chart at 12.30pm with 'trace aspirates'. A similar reading was recorded earlier that morning. A doctor's clinical notes record at 1.15pm, Child O 'vomits and has distended abdomen. 'Trace aspirate...no bile 1x vomit post feed No blood' Unlikely NEC, most likely distention secondary to PMec.' Letby records, for 1.15pm: '[Child O] had vomited [undigested milk], tachycardiac and abdomen distended. NG tube placed on free drainage...blood gas poor as charted...saline bolus given as prescribed with antibiotics. Placed nil by mouth and abdominal x-ray performed. Observations returned to normal'
12:42pm: Letby messages a nurse colleague 'How's it going have you got some sun?' at 2.07pm.
The nurse replies: '...How's your day?'
Letby: "It's busy!!.."12:54pm: An x-ray report of 'possible onset of sepsis' by a consultant radiologist said Child O's appearance had improved on a subsequent image. 'NEC or mid gut volvulus cannot be excluded'. The x-ray is not time stamped but is understood to have happened prior to Child O's collapse. A doctor notes: 'Called to see [Child O] at [about] 1440. Desaturation, bradycardia and mottled. Bagged up and transferred to Nursery 1. Neopuff requirement in 100% oxygen...' Letby records: 'Approx 1440 [Child O] had a profound desaturation to 30s followed by bradycardia. Mottled++ and abdomen red and distended...' Shift leader Melanie Taylor is recorded as entering the neonatal unit at 2.46pm. The doctor records Child O was intubated '1503-1508' 'at first attempt'. Dr Stephen Brearey records for Child O at this time: 'small discoloured ? purpuric rash on right wall' Child O suffered another event at 3.44pm, the court hears. Bleep data for a crash call is made at 3.49pm. A consultant writes a retrospective note '[Child O] had been intubated about 3pm when [doctor colleague's] fast bleep went off. Arrived to find [Child O] was being bagged. Desat to 35...' Lucy Letby's note 'Drs crash called 15:51 due to desaturation to 30s with bradycardia, minimal chest movement and air entry observed. Reintubated...'
12:58pm: Morphine is administered to Child O. A doctor records a further collapse for Child O at 4.15pm, and chest compressions commence. Lucy Letby records, in notes written retrospectively at 8.35pm for 4.19pm: 'CPR commenced 16:19 and medications/fluids given as documented...IV fluids 10% glucose...morphine...'
2:01pm: The trial is resuming following its lunch break. The courtroom is cold today, as Lucy Letby - who has been present throughout this trial - now appears to be wearing a scarf.
2:10pm: Kate Tyndall continues to talk through the sequence of events for Child O. Adrenaline is given to Child O at 4.26pm, as well as a prescription for sodium bicarbonate. A consultant records adrenaline and compressions given to Child O. Dr Stephen Brearey records being called back at 4.30pm. Lucy Letby records, at about 5pm: 'Placed back on to ventilator. Dopamine commenced....Flecks of blood from NG tube. Discolouration to abdomen. Unable to obtain heel prick...due to poor perfusion.' The records show attempts to resuscitate and stabilise Child O were unsuccessful. Child O was baptised.
2:12pm: Child O passed away at 5.47pm on June 23, 2016. Dr Stephen Brearey records: 'After 30 mins of resus, futility of resus explained to parents. Parents and team agreed to stop CPR. [Child O] passed to mum.'
2:13pm: Child P suffers an event at 6pm, the court hears.
2:15pm: A post-mortem blood test revealed 'nothing untoward', the court hears.
2:17pm: Lucy Letby records, for the family communication: 'Parents kept updated on events throughout the afternoon - were present for some of the resuscitation and maternal grandmother present for support. ...Time alone [for parents and Child O] given. Photographs taken on mobile. Aware of need to keep lines/ET Tube in at present. [Child O] taken to family room to be with parents. Cooling cot arranged.'
2:20pm: The doctor messages Letby if she is ok.
Letby: 'Think so, just finishing my notes. Can't wait to get home.' Letby also messages a nursing colleague about how the day had gone badly 'Lost a triplet'. She adds, in a message to the doctor, she was not going to vote that day. Letby messages the nursing colleague to say Child O 'went very suddenly' and 'had a big tummy overnight but just ballooned after lunch and went from there'. The nurse replies: 'Big hugs'.2:22pm: Letby says the other two babies were being screened, as it was not known why Child O had collapsed. She adds: 'I want to be in Ibiza' The nurse replies: 'Poor parents' Letby said Child O had died on the student's first day of a four-week placement. She adds who was on duty that day. The nurse replies: 'Lots of consultants then'.
2:26pm: The nurse messages: 'We don't have any luck with 33-34wkrs' Never seem b able to tell do u'
Letby: 'No, deteriorate so quick'. Letby said one colleague was upset about what had happened. She adds: 'Yeah worried she's missed something' The nurse, in part of her reply, says: 'Wow identical triplets! Didn't know that even happened'2:29pm: Letby's mother messages her daughter to say it was sad what had happened on the first day back after Lucy Letby's holiday.
Letby replies: 'Yep it's just as well I love my job!' The doctor messages Letby to say the debrief didn't find anything that was missed for the events of Child O.2:34pm: Letby messages the doctor to say 'apparently' she had sounded bossy around the time of the baptism call for Child O. The doctor says he would interpret it as being proactive. Letby says she has 'broad shoulders' and had apologised, saying it could have been interpreted as being overly direct. The two agree it had been a stressful situation. Letby said she had been 'blubbering at work' and the doctor replies a cry is needed at times, adding 'You should have seen me at the Hoole Roundabout'.
2:42pm: Child P dies at 4pm on June 24, and an event for Child Q happens at 9.10am on June 25. The doctor messages Letby on Monday, June 27 about the care for Child Q, and a Facebook conversation takes place. A reference is made to clarify paperwork for a prescription for Child O during the resuscitation attempts. On June 29, a Datix form is filed in which Child O 'suddenly and unexpectedly collapsed'. Letby files a Datix form on June 30, in which it was recorded that equipment required for a procedure during resuscitation was not available on the unit. It was clarified in July 2016 Child O did not lose peripheral access.
2:43pm: On June 23, 2017, Letby searched for the surname of Child O, Child P and the surviving triplet on Facebook.
2:47pm: A statement from a doctor is read out to the court. The doctor said she was aware of the triplets beforehand. She recalled that Child O was a good size for the gestational age, and for being a triplet. His heart rate was "absolutely fine". He was "crying and making good respiratory efforts". The oxygen levels were "just on the low side", so CPAP was supplied and the oxygen levels rose. Child O was "stable and nice and warm", wearing a hat. Child O was shown to the father and the doctor congratulated him.
2:51pm: Child O was given mild breathing support. The doctor explained to the father Child O was "doing really well". The doctor recalled feeling "positive" and it was "a good day", and the triplets "were definitely progressing well". On June 22, no issues were highlighted during her long day shift, and on June 23, she was not in work. She received the news Child O had died on her next night shift.
2:53pm: Kate Bissell, senior nurse, in her agreed statement, says she was involved in Child O's care from delivery. She recalled all triplets were a good size, and the mum had done well to get to 33 weeks. Child O needed a 'little respiratory assistance', which was 'to be expected'. He was put on antibiotics, which was standard care. Child O 'remained stable' throughout the rest of the shift.
2:55pm: The judge, Mr Justice James Goss, says the courtroom has warmed up this afternoon, having been chilly this morning. Lucy Letby is continuing to wear a scarf as a 10-minute break now takes place.
3:09pm: The trial is now resuming, with nurse Sophie Ellis giving evidence. She confirms she was the designated nurse for Child O and Child P for the night shift on June 22-23, 2016. She recalls Child O was reviewed towards the end of that night shift as he had "quite a full abdomen".
3:15pm: The nurse recalls Child O was "very stable" that night with no concerns, and the only thing to report was a full abdomen at the end of that shift. At one point, nurse Ellis says the temperature is 'a little high', so the incubator temperature is turned down. The oxygen saturation readings were recorded as 'very good - what we would like', at 97% and above. Child O was recorded as not requiring additional oxygen, and was on Optiflo.
3:24pm: Feeds were "gradually increased throughout the day", and administered "every two hours". The nurse's note is shown to the court, made at about 2.30am, and records 'stable' observations for Child O and that the baby boy was 'tolerating feeds well. Part digested milk aspirates, under half of feed volume 4 hourly. Abdomen full but soft'. The recordings were 'reassuring', nurse Ellis tells the court.
3:28pm: The addendum at 7.32am records '[Abdomen] looks full slightly loopy. Appeared uncomfortable after feed. Reg Mayberry reviewed. Abdo soft, does not appear in any discomfort on examination. Has had bowels open. To continue to feed but to monitor' Nurse Ellis says this was something notable for Child O, hence the need for a second opinion. It was not a concern in itself, taking into context other observations, but it was "one to keep an eye on".
3:36pm: Notes show Child O had 'ECG dots' - a way to measure heart activity - removed at 11pm as it was no longer needed. A cannula was removed at 5.30am on June 23, and antibiotics had been stopped at 6.41am as it was understood "everything was ok". Child O's Optiflo was also weaned down at 6.30am as the baby boy was "managing well".
3:37pm: The nurse tells the court Child O had managed feeds, antibiotics were stopped, and he had a "very stable" and "positive" night overall for June 22-23.
3:39pm: The nurse was informed Child O had passed away at the time of her next night shift.
3:48pm: Benjamin Myers KC, for Letby's defence, is now asking Sophie Ellis questions. He asks about the feeds and aspirates for Child O during the night shift. He asks if the feeds of 10-12ml of donor expressed breast milk every two hours is normal. The nurse replies it was normal feeding policy for babies of that weight and gestational age. Mr Myers asks if it is usual for babies to have aspirates of under half their feeds. The nurse replies that reading would suggest Child O was tolerating his feeds that night.
3:50pm: The nurse says she wouldn't always record a full aspirate for every feed, but would do so if there was a concern for the baby.
Thursday 9th March 2023
Child O
Dr Huw Mayberry - Dr. Kataryna Cooke (SHO) - Nurse Melanie Taylor10:30am: I'll be bringing live updates from Manchester Crown Court today, where the murder trial of nurse Lucy Letby continues. We'll be hearing evidence in relation to the deaths of Child O and Child P in June 2016. Ms Letby is accused of killing the brothers, who were triplets, within a 24hr period at the Countess of Chester Hospital. The prosecution say Ms Letby murdered the boys by injecting air into their bloodstreams. She denies all charges.
10:36am: First in the witness box is Dr Huw Mayberry, via live link from Australia. He is recalling his night shift of June 22 into 23 2016 and his examination of Child O that night - yesterday we heard from a nurse Sophie Ellis, who told the court he was 'stable' throughout that night
10:37am: Dr Mayberry agrees with the nurse's observation, he says he remembers coming back on for his second night shift on 23 June and 'was obviously very shocked' to hear Child O had died that day. 'I felt that he was very well', he said
10:43am: Dr Mayberry is asked if he saw anything to indicate Child O was in discomfort, during the early hours of June 22, he says 'not at all'
10:46am: Ben Myers KC, defending, is now questioning Dr Mayberry - he says 'do you actually have an independent recollection of how (Child O) was that you saw him?' 'Yes', he says Mr Myers says 'you have no notes of your own to rely on, do you?' 'No', he responded
10:47am: Dr Mayberry doesn't have any notes as he was crash bleeped away from Child O's cotside in the early hours of 22 June to attend another baby - only record of his examination was recorded by nurse Ellis
10:48am: Mr Myers notes that between 10am on the morning of 22 and 9.30am on the morning of 23 June there is no clinical notes for Child O, he asks if that is standard practice He responds 'if you have a child were you are not concerned about them then it would not be unusual'
10:50am: Dr Mayberry does say he was asked by a senior doctor why he had not made a note about his examination in the early hours - he tells the court he should have made one
10:54am: Mr Myers repeats that without a note, it's difficult for him to recall all details of examination and Child O's condition. Dr Mayberry says 'if I could go back I would write it'
10:57am: Dr Mayberry says he does remember being 'shocked' at Child O's deterioration the following day
11:02am: Prosecution are asking Dr Mayberry further questions - they've asked him to spell out his responsibilities for the night of 22 June. He tells the court he was a registrar on call for four different units, neonatal, birthing, general paediatrics and emergency dep
11:08am: Dr Kataryna Cooke is now in the witness box - she was a senior house officer at the Countess of Chester from 2015-2017. She is asked if she has an independent memory of her involvement with Child O's care - 'the only thing I remember was it was around Brexit referendum'
11:13am: She is now referring back to her notes. She went on a ward round on the morning of 23 June - a note on her examination of Child O at 9.30am, shown to the court, state 'observations normal'
11:14am: The notes state that he was moving onto a lighter form of breathing support, which was a 'positive sign'. Antibiotics were also stopped for suspected sepsis - Dr Cooke says most premature babies are screened for sepsis
11:23am: Asked for her overall observations about Child O that morning, Dr Cooke says 'from the notes it doesn’t appear like I had any concerns about (Child O) and his clinical course was uncomplicated and he was making good progress'
11:32am: The court is told that Child O was later found with a hematoma in his liver (which is an accumulation of blood). Dr Cooke is asked whether that could have been present at time of her examination at 9.30am
11:33am: She says if that hematoma was present her 'review wouldn’t be normal, by which I mean observations would suggest baby is undergoing deterioration as oppose to normal observations and no concerns from night team or nursing team'
11:34am: The judge clarifies that the hematoma was found post-mortem and that it's not alleged the hematoma was in existence at the time of her examination. Ben Myers KC, defending, agrees - saying they are not alleging it was present at that time
11:37am: The court has previously heard that on post mortem un-clotted blood was found in abdominal space from a liver injury. There was damage in multiple locations on and in the liver which had bled into the peritoneal cavity
11:38am: The court has previously heard that in the view of the Crown's medical expert Dr Dewi Evans the liver injury occurred before Child O's collapse and contributed to it
12:08pm: Nurse Melanie Taylor is now in the witness box recalling the events of 23 June
12:11pm: Ms Taylor was working the day shift on 23 June as shift leader. Ms Letby was Child O's designated nurse that day
12:15pm: Ms Taylor is asked how Child O was on that morning, from reviewing her notes she said 'I had no concerns about him, obviously he was premature....we felt he was stable at the beginning of the shift'
12:37pm: Ms Taylor has told the court that afternoon - around middayish - she recalls seeing Child O. 'I remember I thought I don’t think he looks as well as he did before'. She told the court she suggested to Ms Letby that he be moved to nursery 1 for closer observations
12:38pm: Ms Taylor said that Ms Letby said 'no, she felt he was okay and wanted to keep him in nursery 2 and wanted to keep the three triplets together' - Ms Taylor says she felt she was 'put out' by this
12:39pm: 'I couldn’t put my finger on it, I just had a gut instinct I didn’t feel like he was as well', Ms Taylor said. Ms Taylor said she 'felt like (Ms Letby) was undermining my decision'
12:40pm: Child O remained on nursery 2 until he collapsed later that afternoon and moved to nursery 1. He eventually needed resuscitation, which was unsuccessful - Ms Taylor said she was surprised by the severity of his collapse
1:00pm: Ms Taylor has finished giving evidence. Judge has asked the jury to temporarily retire while he 'gets an update on the weather' and whether we can continue this afternoon
2:08pm: Court has now adjourned until tomorrow morning (due to concerns over weather/traffic)
Chester Standard article 09-03-2023
A COLLEAGUE felt "put out" when murder-accused nurse Lucy Letby insisted a triplet should not be moved to intensive care, a jury has heard.
Letby, 33, is accused of murdering the newborn boy just hours after the exchange.
She is alleged to have fatally injected air into the circulation of the infant, Child O, during a day shift at the Countess of Chester Hospital's neo-natal unit.
Child O was stable and raised no concerns for doctors on the morning ward round on June 23, 2016, Manchester Crown Court heard.
Letby was caring for the youngster in nursery room two, a high dependency unit, along with one of his brothers, Child P, who she allegedly murdered the following day.
Giving evidence on Thursday, March 9, nurse Melanie Taylor said that at one point she had looked into room two and had a "gut instinct" something had changed with Child O.
The shift leader said: "I can't specifically remember what it was that I was not happy about but he didn't look as well as when I started the shift.
"I can't remember the reasoning behind it. Sometimes it can be just a gut instinct. Sometimes they (the baby) can present very slight things.
"I remember saying it out loud to Lucy.
"I asked whether she felt we should move him into nursery one. She said 'no'. She felt it was OK and wanted to keep him in nursery two and wanted to keep the brothers together.
"I guess it's a joint decision. Lucy was the one looking after him. She knew him and was with him all day."
Ms Taylor went on: "With hindsight, I wish I had been a bit firmer. I remember being put out that she was quite insistent. I think because I felt she was undermining my decision.
"She said 'no'. Quite plainly 'no, I don't feel like he should be moved'.
"I don't think from me it was 'he needs to be moved now'. It was more of a feeling than any hard evidence.
"I had a gut instinct he didn't seem as well."
Philip Astbury, prosecuting, asked: "What was the advantage of room one?
She replied: "Just the ability to have more space if anything was to deteriorate. We have more equipment on hand. We have got the emergency trollies in there.
"The resources are closer to hand and easier to get to."
She said her "gut instinct" came about "an hour or two" before the first collapse of Child O in the mid-afternoon.
Ms Taylor said she could not recall how she was alerted to the deterioration but that Letby was in room two when she attended.
Child O stabilised before he was moved to intensive care room one where he collapsed again about an hour later but could not be resuscitated.
Ms Taylor told the court she was "surprised" at Child O's deterioration.
Ben Myers KC, defending, asked the witness: "Do you recall Miss Letby explained she wanted to keep him (Child O) with his brother?"
"Yes," Ms Taylor said.
Mr Myers said: "All other things being equal, keeping them together as far as you can is desirable, isn't it?"
Ms Taylor repeated: "Yes."
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Friday 10th March 2023 - court adjourned due to bad weather
Chester Standard article 10-03-2023
THE trial of Lucy Letby, who denies murdering seven babies at the Countess of Chester Hospital neonatal unit and attempting to murder 10 more, was adjourned on Friday, March 10.
Jurors have been attending Manchester Crown Court to hear the trial of Lucy Letby, who was working as a neonatal unit nurse at the Countess of Chester Hospital during the time of the indictment between June 2015 and June 2016.
She denies all 22 charges in relation to the fatal and non-fatal collapses of babies in the neonatal unit during that time.
Today (Friday, March 10) was due to hear further evidence in the case on Child O, in the 19th week before a jury, but the trial was adjourned due to bad weather conditions.
The trial had been cut short at lunchtime on Thursday, March 9, due to heavy snowfall.
The next day of the trial is scheduled to be Tuesday, March 14.
Monday 13th March 2023 - no court (pre-planned)
Tuesday 14th March 2023
Child O
Statements of neonatal nurse practitioner Amy Davies - Unnamed nurse - Dr Stephen Brearey - Unnamed doctor10:10am: The murder trial of nurse Lucy Letby continues at Manchester Crown Court this morning. I'll be bringing live updates as we hear further evidence in relation to Child O, who Ms Letby is said to have killed in June 2016 via the injection of air. She denies all charges
10:11am: The boy was one of triplets and his brother, referred to as Child P, died just over 24hours later after also being allegedly attacked by Ms Letby.
10:38am: Court is currently being read agreed evidence. First statement is from Amy Davies, who was a neonatal practitioner in 2016, she recalls having no concerns about the triplets in the days after their birth in late June 2016
10:47am: A statement from another member of the neonatal team, who cared for Child O on the nightshift of 22 June into 23 June. She recalls seeing Child O with a swollen stomach - she was assigned to give him a milk feed via an NG tube
10:48am: She raised concern over his stomach to nurse Sophie Ellis - she told her that she was aware and that she had flagged for him to be reviewed by a doctor. But she had been told 'to go ahead' with the feed and 'closely monitor' him The neonatal worker said she remembers Child O 'squirming a little' when she began the feed
10:54am: Dr Stephen Brearey, who was head of the neonatal unit in 2015/16, is now in the witness box. He is recalling his memory of the events of 23 June 2016 - the day Child O died
11:06am: Dr Brearey wasn't the consultant on call that week - but he was in the hospital for a meeting. He passed through the unit and spoke to another doctor, who cannot be named for legal reasons, and was briefed on Child O. He stayed and offered to help
11:07am: Manchester Crown Court has previously heard that Child O was in good condition and stable up until the afternoon of 23 June when he suffered a "remarkable deterioration" and died.
11:08am: Dr Brearey has just reviewed a number of Child O's charts from that morning - he said 'none of those results were concerning; and that they were all in the 'normal range' and no evidence of infection
11:10am: Court has just been shown an X-ray taken that morning, the radiologist notes 'the appearance is nonspecific but necrotising enterocolitis or mid gut volvulus cannot be excluded'
11:12am: On another X-ray taken later that day, the radiologist notes 'the bowel is considerably less distended by comparison with the previous image, earlier that day' - notes no evidence of pneumothorax
11:21am: Dr Brearey recalls Child O's first crash shortly after 14:30 on 23 June. He helped intubate the baby boy. He tells the court during this procedure he noticed an 'unusual' rash on the boy's chest
11:22am: He said the rash was purpuric was 'noticeable'. He tells the court this was 'very, very concerning' in a neonate - his first thought for the case of the rash was infection. He notes Child O was on antibiotics and a blood test ordered
11:40am: Child O crashed several more times that afternoon. On his last and fatal collapse at 16:15, Dr Brearey says that there was 'years of experience in that resuscitation' and that it was going as he would have wanted. 'But we just weren't getting a response back in terms of what we would normally expect', he said. Resus continued for well over 30mins but no pulse was recorded for Child O
11:49am: The medic tells the court that by late afternoon the earlier rash noticed had 'vanished', which he found 'perplexing' - he said that ruled out it being a purpuric rash, as they're around for a 'good few days'
11:51am: He said after 30mins the 'team agreed that to continue resus was going to be futile', this was discussed with parents it was stopped. Child O was then passed to his mum
12:01pm: Dr Brearey tells the court that after the death of Child O's brother, Child P, the following day he attended a debrief with other medical staff. He said Ms Letby was present in that debrief. He said he asked how she was feeling and 'can remember suggesting to her to take the weekend off to recover' 'She didn’t seem overly upset to me in the debrief and told me at the time she was on shift next day which was a Saturday'
12:02pm: He said he was concerned about this because he, along with other consultants, had 'already expressed our concerns' about deaths on unit and a potential link to Ms Letby
12:05pm: He said on the evening of June 24 he called the duty exec senior nurse in the urgent care division. She was 'familiar with concerns'. The doctor told her he 'didn’t want nurse Letby to come back to work the following day or till all this was investigated properly;
12:06pm: He was told 'no' and that 'there was no evidence', the exec was 'happy to take responsibility' for Ms Letby continuing
1:21pm: Dr Brearey told the court that "further conversations" took place the following week and the decision was taken to remove Ms Letby from frontline nursing duties - instead placing her in a clerical role. Ben Myers KC, defending, noted that Dr Brearey had first "identified" Ms Letby as someone of interest as early as June 2015 after the death of the first three babies in this case. Dr Brearey had noted, with colleagues, that Ms Letby was present when those three children died in 2015. Mr Myers put it to the doctor that he was guilty of "confirmation bias" towards Ms Letby and failed to look at "suboptimal care" given to the children in this case. "Absolutely not", he said.
1:56pm: Mr Myers put it to Dr Brearey that if there was a basis for his suspicions, he would have gone to the police. Dr Brearey said he and his colleagues were trying to "escalate appropriately" and needed "executive support" to decide the "correct plan of action going forward". Dr Brearey added: "It's not something anyone wanted to consider, that a member of staff is harming babies. The senior nursing staff on the unit didn't believe this could be true." Dr Brearey said with every "unusual" episode of baby collapse between June 2015 and June 2016 there was "increasing suspicion" about Ms Letby, which led him to eventually escalate his concerns and request she be taken off shift.
2:00pm: A doctor, who cannot be named for legal reasons, is now in the witness box. She is recalling the events of June 23 - when Child O collapsed several times and eventually died
2:10pm: The doctor said she was 'shocked' by the appearance and deterioration of Child O on June 23. She tells the court she had seen him the previous day and was 'progressing very well' When she saw the boy shortly before 4pm, she said she remembers him 'just being lifeless and mottled' and thinking 'what has happened'. She said it was 'completely unexpected'
2:25pm: The doctor said she wondered whether the cause of Child O's collapse had been to do with his heart. She asked Dr Brearey, who specialised in cardiac medicine, whether he should have an echocardiogram - he felt one wasn't required
2:31pm: The medic is now recalling Child O's final and fatal collapse. She tells the court 'whatever we gave him was having no effect', she adds this was 'not something I’d seen happen so suddenly in a baby'
3:19pm: Court has now adjourned till tomorrow
Chester Standard article 14-03-2023
LUCY LETBY allegedly tried to murder a baby after a hospital boss refused to remove her from nursing duties, a court has heard.
A senior paediatrician at the Countess of Chester Hospital told an executive that he and his consultant colleagues were "not happy" with the defendant continuing to work on the neo-natal unit.
Dr Stephen Brearey said he raised the matter with nursing chief Karen Rees following the deaths of two brothers on successive days in June 2016.
The prosecution say the infants, Childs O and P, were the 15th and 16th victims of Letby, 33, who denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
On Tuesday, March 14, Dr Brearey, head consultant on the unit, told Manchester Crown Court he held a staff debrief following the deaths of Childs O and P on June 23 and June 24.
Nurse Letby was present at the debrief, he said, and he asked her how she was feeling.
Dr Brearey said: "I can remember suggesting to her she would need the weekend off to recover from the traumatic events.
"She didn't seem overly upset in the debrief, or upset at all, and she told me she was on shift the next day, which was a Saturday.
"I was concerned about this because we had already expressed our concerns to senior management about the association with nurse Letby and the deaths we had seen on the unit.
"So, following the staff debrief, I phoned the duty executive on call, Karen Rees, senior nurse in the urgent care division.
"She was familiar with our concerns already. I explained what had happened and and I didn't want nurse Letby to come back to work the following day or until this was all investigated properly.
"Karen Rees said 'no' to that and that there was no evidence.
"I put it to her was she happy to take responsibility for this decision in view of the fact that myself and my consultant colleagues all wouldn't be happy with nurse Letby going to work the following day.
"She responded she was happy to take that responsibility.
"We had further conversations with executives the following week and action was taken."
On Saturday June 25, Letby is accused of attempting to murder Child Q during a day shift by injecting him with air.
Letby, originally from Hereford, denies all the allegations.
Wednesday 15th March 2023
Child O
Dr Dewi Evans - Summary of police interviewsChester Standard article 15-03-2023
A BABY allegedly murdered by nurse Lucy Letby was injected with air, a court heard.
The infant was said to have been attacked by the defendant during her day shift at the Countess of Chester Hospital's neo-natal unit in June 2016.
Giving evidence on Wednesday, March 15, expert witness Dr Dewi Evans told Manchester Crown Court he believed Child O was the victim of an "air embolus" – in which gas bubbles block blood supply.
The retired consultant paediatrician said a "small discoloured purpuric rash" had been noted on the youngster's chest during his rapid deterioration on the afternoon of June 23.
Dr Evans said: "I considered that the rash was consistent with (Child O) having received a injection of air into his circulation, his blood circulation.
"My opinion was that (Child O's) terminal collapse was him being the victim of an air embolus.
"I couldn't find any evidence where this could have occurred accidentally."
Dr Evans said it "repeated the pattern" seen in the case of Child B, a twin girl, who also had a noticeable rash during her collapse – which she survived.
Jurors were told Dr Evans had concluded in an earlier report, in June 2018, that the cause for Child O's collapse was trauma to the liver.
A haematoma – bleeding – had been found in the liver during a post-mortem examination.
Dr Evans said: "If there was a purpuric rash – little blood spots under the skin – there had to be a cause. It was indicative of direct trauma."
He later learned from the police that the doctor who observed the rash had further explained it disappeared a short time after.
Dr Evans said: "This made a big difference to the interpretation of the rash. If it's a purpuric rash it will last quite some time – days, hours."
Letby is also accused of murdering Child O's newborn brother, Child P, on the following day.
The surviving triplet was later discharged from another hospital after their parents "begged" a doctor to remove him from the Countess of Chester.
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Yesterday, the court heard that in June 2015, senior paediatrician at the Countess of Chester Hospital Dr Stephen Brearey conducted a review into the circumstances of the death of Child D that month.
An "association" with Letby and her presence at a number of collapses up to that point were noted, the court heard.
Dr Brearey told the court a meeting followed with director of nursing Alison Kelly in late June or early July 2015.
He said: "I think my comment at the time during the meeting was 'it can't be Lucy, not nice Lucy'.
Ben Myers KC, defending, said: "I would suggest that once Ms Letby had been identified as someone, or a factor, that caused concern there was naturally a bias against her in the way she behaved and the way it was interpreted, do you agree?"
Dr Brearey replied: "I disagree."
A further review of collapses at the unit from a neonatologist based at Liverpool Women's Hospital took place in February 2016, the court was told.
Dr Brearey said he sent a report of those findings to the director of nursing and the hospital's medical director as he asked for another meeting.
He confirmed that during this period there was no formal complaint made to the police.
Mr Myers asked: "If somebody hurt a baby on your unit and you believed you had the identity of the person responsible, you'd report it to the police wouldn't you?"
Dr Brearey said: "I think you are making it a bit more simplistic than it was. It was not something that anyone wanted to consider, that a member of staff is harming babies.
"Actually, the senior nursing staff on the unit didn't believe this could be true up until the point and beyond when the triplets (Child O and P) died.
"None of us (the consultants) wanted to believe it either.
"This all became very exceptional and it took a step back to think about it. The nature of these collapses, the unexpected nature of them, the lack of response to resuscitation, the unusual rash noted on a number of occasions and each time the association with Nurse Letby."
He said he wanted to "escalate" concerns within the hospital management rather than go directly to the police.
He said: "I needed executive support and that was what we were after."
Dr Brearey said there were "no more events" after Letby left the neo-natal unit.
He said: "It was the same staff doing the same job and there were no sudden collapses."
The consultant told Simon Driver, prosecuting, that between the deaths of Child D and Child O he was unaware that two other babies had returned blood results which showed abnormally high insulin levels.
Thursday 16th March 2023
Children O & P
Professor Owen ArthursChester Standard article 16-03-2023
AN "unusual" amount of gas was detected in a baby just hours after his brother was allegedly murdered by nurse Lucy Letby, a court heard.
Letby, 33, is said to have administered fatal doses of air to both infants who died at the Countess of Chester Hospital on successive days in June 2016.
Child O – one of identical triplet boys – was pronounced dead at 5.47pm on June 23 only two days after he and his brothers were all born in good condition.
Following the death, his brother Child P was reviewed on the neo-natal unit by a consultant who ordered an abdominal X-ray.
The subsequent X-ray, timed at 8.09pm, noted "gas filled loops throughout the abdomen", Manchester Crown Court heard.
Letby was the designated nurse for Child O and P on the day shift of June 23 and continued to care for Child P the following day.
On June 24, Child P collapsed on numerous occasions from 9.35am onwards and required resuscitation after his heart rate and blood oxygen levels plummeted.
Medics, including Letby, were unable to revive the youngster from his final collapse at about 3.15pm and he was pronounced dead at 4pm.
A transport ambulance team had arrived at the Countess of Chester at 3pm in preparation for transferring Child P to a specialist hospital.
When he died, his parents "begged" the team doctor to take their surviving triplet instead, which he agreed to.
Giving evidence on Thursday, March 16, Dr Owen Arthurs, professor of radiology at London's Great Ormond Street Hospital, said the June 23 X-ray of Child P was "very similar in appearance" to one taken of Child O.
He told the court: "This is gas throughout the gut. This degree of gas is quite unusual in a baby like this."
He said potential causes were infection or necrotising enterocolitis (NEC), a common bowel disorder in premature-born babies.
An alternative explanation was the administration of air via a nasogastric tube, he said.
Dr Arthurs came to the same conclusions regarding an X-ray of Child O, captured hours before his death.
He said: "This shows a lots of gas in his stomach, small and large bowel. This is more than what would be expected in a normal baby."
Dr Arthurs agreed with Ben Myers KC, defending, that another possible explanation for Child P's dilation was an "unidentifiable cause".
On June 24, Letby was also assigned the day shift care of the surviving triplet, the court heard.
Ahead of the shift a doctor, who cannot be identified for legal reasons, messaged Letby: "Are you OK? It's rubbish not to sleep well in the middle of 3 long days. Hope your day goes OK."
Letby replied: "Hmm maybe. I'll be watching them both (Child P and the surviving triplet) like a hawk.
"I'm OK. Just don't want to be here really. Hoping I may get the new admissions."
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Friday 17th March 2023 - no court (pre-planned)
Monday 20th March 2023
Child P
Police analyst: Recorded events & messages - Dr A - Dr Ukoh - Nurse Sophie Ellis10:16am: I'm back at Manchester Crown Court for the murder trial of nurse Lucy Letby. The jury will be continuing to hear evidence in relation to the death of a baby boy, referred to as Child P, in June 2016. Ms Letby is said to have administered a fatal dose of air to the boy. Child P's death came just 24hrs after the death of one of his identical triplet brothers, Child O. Ms Letby is also accused of injecting him with air. She denies all charges.
10:34am: Police intelligence analyst Claire Hocknell is first in the witness box - she's continuing to take the court through sequencing evidence for Child P (a 700 tile timeline of that baby boy's collapses and subsequent death)
10:38am: On June 24, 2016 Child P suffered a number of profound desaturations and at various points required CPR and adrenaline. The boy collapsed for the final time at 15:14 that day and was pronounced dead at 16:00
11:04am: An hour after Child P's death, Ms Letby text a colleague to say 'Life is too sad', 'lost another and third going to women’s' Her colleague responded: 'Omfg!! what the hell is going on! Don’t know what to say…will have a big hug for you when I get there'
11:27am: A nursing note, recorded by Ms Letby, following Child P's death stated: 'I have dressed (Child P) at (the parents) request and taken photos of (Child P) and (Child O) together. Support given to parents and extended family'
11:28am: In a message to a doctor [Dr A], who cannot be named for legal reasons, later that night Ms Letby said the two boys - who were part of a set of triplets - looked 'beautiful' together, but added that it was 'beyond words how awful it is'
12:09pm: [Dr A], who cannot be named for legal reasons, is now in the witness box. He cared for Child P in days after his birth on 21 June. He tells the court that he was born in good health, he was 'pink, well perfused and temperature acceptable'
2:04pm: We're back after a break for lunch. [Dr A] is continuing to give evidence. He's going over notes from 24 June, when Child P collapsed on a number of occasions
2:15pm: [Dr A] tells the court that on the afternoon of 24 June he fitted a chest drain for Child P as he was suffering a suspected pneumothorax
2:24pm: The court has just heard how Child P went into cardiac arrest at 15:14, [Dr A] recalls how chest compressions were commenced along with breathing support and four doses of adrenaline administered
2:26pm: After 45mins the decision was taken, in conjunction with his family, to stop resuscitation. Prosecutor Simon Driver asks the doctor: 'Can you understand the course his life took over those few days (since his birth)' 'No', the medic responds
3:00pm: Dr Anthony Ukoh, who also helped with Child P's treatment on 24 June, is now in the witness box
3:23pm: Dr Ukoh assisted with one of Child P's earlier collapses. He told the court that he examined the baby boy and was called back 20mins later as he his heart rate had 'plummeted'. Two other doctors were called to assist and Child P was eventually stabilised
3:48pm: A former nursing colleague of Ms Letby, Sophie Ellis, is now in the witness box
Chester Standard article 20-03-2023
NURSE Lucy Letby fainted at work after she and fellow medics could not revive a baby boy, her murder trial has heard.
Letby, 33, is accused of murdering the newborn triplet on a day shift at the Countess of Chester Hospital's neo-natal unit in June 2016.
She is alleged to have given a fatal dose of air to the youngster, Child P, and also one of his brothers, Child O, who died a day earlier.
Child P's condition deteriorated on June 24 as he required CPR on four separate occasions before he was pronounced dead at 4pm.
Letby received a needle prick to her finger during the final resuscitation attempt, jurors were told.
Routine blood checks were required at the hospital A&E department where Letby later fainted.
She was later offered a lift home by a concerned doctor [Dr A] who friends had previously teased her about flirting with him.
Facebook message exchanges between the pair were read out on Monday, March 20 at Manchester Crown Court, in the 21st week of the trial before a jury.
[Dr A], who cannot be identified for legal reasons, asked Letby: "Have you been seen yet?"
Letby replied: "Yes just got back. I made a fool of myself whilst there."
[Dr A], who was also involved in the resuscitation efforts, said: "I asked them to be quick for you. How did you make a fool of yourself?"
Letby responded: "They said someone had asked for me to been seen asap and they knew what had happened today.
"Everyone talking about it whilst I was there. I fainted."
[Dr A] asked: "Oh are you OK now?"
Letby replied: "Bit shaky but OK. Writing my notes. They were reluctant to let me go as on my own."
[Dr A] said: "You could have bleeped me. I'm almost a responsible adult!
"Do you need a lift home?"
After she was dropped off by [Dr A] at her home address, Letby messaged him: "Thank you for the lift and for talking to A&E."
[Dr A] said: "I can't have you walking back in the dark after a rubbish day, mini needlestick and an A&E faint."
He later asked: "What are u doing? I can't concentrate on anything."
Letby said: "Wanting to (cry emoji)."
[Dr A] said: "Did in car. Must have looked a right mess when I got in."
Letby replied: "I keep thinking of them (Child O and Child P) both in the cot together. So peaceful yet beyond words how awful it is.
"So sad. The family thanked me when I took (Child P) in dressed. And I know age doesn't make it any easier/harder but such a lot to go through at a young age."
[Dr A] said: "I don't know how it would be possible to get over losing a child, let alone 2."
Letby responded with a crying emoji and wrote: "Think my head may explode…"
On June 25 – when Letby is accused of attempting to murder another baby, Child Q, during the morning of a day shift – she messaged the same doctor: "Nice lunch break, Told by mum about needlestick and got a huge lecture about not being careful enough, overworked, doing too much etc."
[Dr A] replied: "That's not what you need. She'll be concerned that you're not looking after yourself. Huge lectures aren't fun are they?"
Letby said: "My parents worry massively about everything and anything, hate that I live alone etc. Didn't know whether to tell them or not but I thought I better had in case anything comes of it. Lectures are not fun."
[Dr A] responded: "It sounds hard for all of you. I'm sure 'letting go' of your child (probably the most precious thing in your life) is difficult, especially if you don't stay local or do a job renowned for bad conditions and potential risks. What did you tell mum?"
Letby said: "I know, I feel bad because I know it's really hard for them especially as I'm an only child and they mean well, just a little suffocating at times and constantly feel guilty.
"Told her I was fine, accidents happen, wasn't anyone's fault, just one of those things and bloods etc all precautionary."
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Tuesday 21st March 2023
Child P
Senior nurse Kathryn Percival-Calderbank - Unnamed consultantChester Standard article 21-03-2023
NURSE Lucy Letby found caring for less sick infants in hospital was "boring", her murder trial was told.
Letby, 33, is accused of murdering seven babies and attempting to murder 10 others at the Countess of Chester Hospital's neo-natal unit.
She is also said to have argued with a senior colleague when asked to work in an 'outside nursery' where babies were treated in preparation for going home.
The unit was split into four rooms – intensive care in nursery one, high dependency care in nursery two and the 'outside nurseries' of rooms three and four, Manchester Crown Court has heard.
On Tuesday, March 21, senior nurse Kathryn Percival-Calderbank told jurors that Letby was "unhappy" if she was allocated shifts in either room three or four.
She said: "She expressed that she was unhappy at being put in the outside nurseries.
"She said it was boring and she didn't want to feed babies. She wanted to be in the intensive care".
Mrs Percival-Calderbank, who qualified as a nurse in 1988, added: "If anything was going on within nursery one you would find she would migrate there, as we would all do to go and help. She would definitely end up in nursery one to assist.
"It was more that we were worried for Lucy's mental heath because it can be upsetting, emotional and sometimes exhausting as well at the end of a shift, if you're constantly put in that stressed situation all the time.
"Sometimes you've got to come out of that environment and be in an outside nursery."
She recalled an argument – some time before June 2016 – with Letby who was "upset" at a shift allocation.
"Lucy went into the outside nursery but she was not happy with the decision," she said.
'Particularly keen to assist'
Ben Myers KC, defending, asked the witness: "Is it right she made it plain that she preferred to work in the intensive care aspect of operations?"
"Yes," replied Mrs Percival-Calderbank.
Mr Myers said: "Did she use the word 'boring'?"
The witness said: "Yes, that's what she said."
Mr Myers said: "There were times when she ended back in nursery one and everyone would be ready to help when there was an issue, wouldn't they?"
"Yes," said the witness.
Mrs Percival-Calderbank agreed with Mr Myers that Letby would be "particularly keen to assist" and "would be there very quickly if an issue arose".
She also agreed the concern among nursing staff was it could be "very stressful and upsetting" to work long periods in intensive care and it was beneficial for mental well-being to spend time away from nursery one.
Mr Myers said: "But she didn't really want to hear that and she wanted to do the intensive care, is that right?"
"Yes," said the witness.
Letby, originally from Hereford, denies all the alleged offences said to have been committed between June 2015 and June 2016.
Wednesday 22nd March 2023
Child P
Dr John Gibbs - Dr Stephen Brearey - Dr Oliver Rackham (Arrowe Park)- Dr Dewi Evans10:06am: Nurse Lucy Letby's murder trial continues at Manchester Crown Court this morning. We'll be hearing evidence in relation to the death of Child P, who the Crown say Ms Letby murdered in June 2016 by injecting a dose of air. She denies all charges
10:10am: Jurors yesterday heard from a consultant who told the court that Ms Letby had asked her whether Child P was “leaving here alive” while they were waiting for a planned transfer of the infant to another hospital Recalling the conversation the consultant told the court: “I just said, the transport team are going to be here soon, almost thinking out loud. Lucy Letby then said ‘he is not leaving here alive, is he?’, which I found absolutely shocking at the time.”
10:11am: Ms Letby's defence lawyer, Ben Myers KC accused her of “dramatising for the benefit of the jury and these proceedings”
10:12am: When proceedings resume, at around 10.30am, we'll be hearing from more senior consultants - who worked with Ms Letby and a number of medical experts, who'll be giving their view on the cause of death of Child P
10:44am: Consultant Dr John Gibbs is first in the witness box. He is recalling the events immediately after Child O's (Child P's brother) death on June 23 2016
10:45am: Dr Gibbs tells the court that when he saw Child O, in the moments before his death, he remembered 'feeling uncomfortable and thought oh no, not another one' … He said he had become 'increasingly concerned at the accumulating number of unusual, unexpected and inexplicable collapses that had been happening on the neonatal unit and that staff nurse Letby had been involved in all of them'
10:49am: Dr Gibbs tells the court that after Child O's death, his brother Child P was started on antibiotics and sent for an abdominal X-ray as a precaution
10:58am: Dr Gibbs said that Child P was a 'well baby' on 23 June. He said he was 'extremely concerned' to learn of Child P's death the following day, he said he 'would not have expected that at all'
11:11am: Dr Gibbs tells the court that the death of the brothers was a 'tipping point for realising something very abnormal and wrong was happening on our neonatal unit'
11:13am: Ben Myers KC puts it to the medic that if he had a genuine concern, he himself would have taken action - Dr Gibbs says he was aware his colleague Dr Stephen Brearey had raised concerns with nursing management and senior managers at the hospital
11:21am: Mr Myers repeatedly put it to Dr Gibbs that if he had concerns he would have taken action. Dr Gibbs repeated that he knew it had been raised by colleagues with management. He said the senior consultants had openly discussed 'the one common factor' in the baby deaths
11:23am: He said it was noted that Ms Lebty had been present on the unit or caring for the babies when they had collapsed in unusual circumstances. Mr Myers asks why it hadn't been reported to the police, Dr Gibbs said it was 'difficult' as they didn't have 'the full picture'
11:26am: Eventually, Dr Gibbs said that consultants insisted that Ms Letby be removed from the unit. He tells the court that management pushed for her to return a month later - they said only if CCTV is installed in each unit He said the 'TV cameras never came and neither did nurse Letby'
11:27am: Dr Gibbs said 'over the next 11months we had to resolutely resist attempts by management to have staff nurse Letby back on the unit'
12:35pm: Dr Stephen Brearey is now giving evidence about the death of Child P.
12:50pm: Dr Brearey said he carried out a review of the case, that highlighted 'some minor deficiencies in care but none of which would have affected the outcome of (Child P)'
12:51pm: The medic said the events of 24 June were 'horrific' and that they would have 'traumatised' even the most experienced members of staff
12:52pm: He said he would expect 99% of babies born at 33week gestation on fourth day of life to survive
12:54pm: Dr Brearey starts to make a broader point about the times at which the deaths had occurred in 2015 and 2016. Mr Myers raises objections, judge says broader conclusions can be made elsewhere in other means
2:08pm: We're now back after a short break for lunch. Dr Oliver Rackham is now in the witness box. He was part of the transport team from Arrowe Park Hospital (he was overseeing the transport of Child P to the hospital before his death)
2:10pm: Dr Rackham was on the neonatal transport team responsible (called Connect) in June 2016. He remembers being given a briefing on 24 June about Child P (he had suffered a number of desats that morning)
2:23pm: The medic tells the court that soon after he arrived at the Countess of Chester, at around 3pm, to transport Child P he collapsed and needed resuscitation. During the course of that resus he received seven doses of adrenaline - all to no effect
2:25pm: Dr Rackham said the medics 'had no explanation for why' Child P collapsed. Asked, with his experience, if he could give any reason for Child P's collapse, he said 'there was no obvious cause, it didn't fit with any obvious reason'
2:33pm: The medic said following Child P's death, there was a debrief on the unit. He said it was a chance for staff who work on resuscitation to 'make sure' that there was nothing missed. He said: 'We felt we had carried out resus well and in accordance with all appropriate guidelines'
2:58pm: Ben Myers KC has just invited Dr Rackham to give his view on adrenaline charts for Child P from that day. They show he received 16 bolus injections of adrenaline over the course of the day and was also given a slow infusion of the drug
2:59pm: From the numbers on the slow infusion chart, Mr Myers says this is 'significantly' higher than the dose that would be ideal - the doctor, with some caution, agrees
3:00pm: Mr Myers asks him to spell out what an excessive amount of adrenaline could do to a neonate - he says that it can cause increased heart rate, blood pressure and have an adverse effect on lactic acidosis
3:02pm: The judge seeks some clarification from the witness. He says that if Child P had been given excessive adrenaline, you would expect to see the effect within 10/15mins
3:24pm: Medical expert Dr Dewi Evans is now in the witness box, he was asked to review the baby deaths by Cheshire Police in 2017
4:02pm: Dr Evans said he was 'at a loss to explain how this baby had collapsed'. He noted 'a lot of gas' in Child P's bowel from the evening before his death, he said it 'begs the question whether excess gas in the abdomen 8pm on night before, was the result of air being injected down his NG tube'
4:21pm: Dr Evans will be cross examined tomorrow.
Chester Standard article 22-03-2023 article 1
A DOCTOR was "shocked" when Lucy Letby asked whether a baby was "leaving here alive", the nurse's murder trial heard.
Letby, 33, was said to have made the "absolutely shocking" comment ahead of a planned transfer of the infant to another hospital.
The youngster continued to deteriorate as his heart rate and blood oxygen levels dropped, and died less than four hours later before the move from the Countess of Chester Hospital could take place.
Recalling the conversation with Letby, a consultant, who cannot be identified for legal reasons, told Manchester Crown Court on Tuesday, March 21: "I just said, the transport team are going to be here soon, almost thinking out loud.
"Literally counting down the minutes before they arrived and desperately wanting this baby to get better, and thinking we are just totally out of our depth and maybe someone else can help.
"Staff nurse Lucy Letby then said 'he is not leaving here alive, is he?', which I found absolutely shocking at the time."
"I said 'don't say that' and left the room."
Letby is accused of murdering the newborn infant, known as Child P, and his triplet brother, Child O, on successive day shifts in June 2016.
Later the consultant said she remembered another "unusual" event involving Letby after Child P had been pronounced dead.
She said: " I went to speak to the parents, myself and Lucy Letby were there. I remember feeling, I don't how to face them or how to say this.
"I told them about that (Child P) was going to need a post-mortem.
"Staff nurse Letby was behind me – one of the things I found unusual was she was almost very animated.
"She was saying to the parents 'do you want me to make a memory box like I did for (Child O) yesterday?' I remember thinking this is not a new baby, this is a dead baby. Why are you so excited about this?
"I found that very inappropriate, the way it was said."
She said she remembered the brothers' father was "absolutely sobbing and literally begging" for the surviving triplet to be taken from the Countess of Chester.
The consultant said: "Even though I didn't beg, in my heart and mind I just wanted him to leave because that's the only way he was going to live."
Ben Myers KC, defending, asked her: "Is that because you thought the Countess of Chester's neonatal unit was unable to cope or are you suggesting that Lucy Letby poses such a danger to small babies?"
The doctor replied: "It definitely was not because the Countess of Chester was not able to cope with a baby like (the surviving triplet). They were completely normal triplets who were expected to run a healthy course.
"I was extremely worried. I couldn't understand what had gone on in the last two days. In my mind what had gone on was not normal.
"At that point in time I just wanted (the surviving triplet) to be in a safe place."
Mr Myers asked: "Because of the danger posed by nurse Letby?"
"Yes," she said.
The barrister went on: "Did you call the police?"
"No," said the consultant.
Mr Myers said: "If you really thought a nurse was hurting or killing babies you would have been yelling it from the rooftops, wouldn't you? What about other babies on the unit?"
She explained that at the time she thought the "correct thing" to do was to raise the matter with her colleagues a few days later, and with the neonatal ward manager.
Mr Myers accused her of "dramatising for the benefit of the jury and these proceedings".
The doctor replied: "No, that's honestly how I felt at the time. I have no intention of dramatising events. It's tragic enough as it is."
She told Mr Myers she was unaware there was a "focus" on Letby being present at the time of child deaths.
She said she had no reason to suspect her of anything up to the point of the deaths of Child O and Child P.
Mr Myers asked: "Did you hear gossip, comment, finger-pointing about Lucy Letby?"
She replied: "Yes, but vaguely. Nothing concrete implicating deaths and increasing mortality rates."
Mr Myers said: "Who were making these comments?"
The doctor said: "Other junior doctors, some consultant colleagues. But again not in a way that would make you think anything untoward in the way of harm being done was going on."
Mr Myers suggested Letby was only voicing her concern about Child P in the hours before he died.
The consultant replied: "I can only speak for myself."
Mr Myers went on: "Do you think there is a danger here – because it's Lucy Letby we are dealing with – for her comments to be taken out of context and made to sound quite a lot worse?"
The consultant said: "I found it unusual given the circumstances."
She agreed all the medics involved with Child P, including Letby, were trying their best in looking after him.
Letby denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Chester Standard article 22-03-2023 article 2
SENIOR doctors demanded the installation of CCTV cameras at a hospital unit if Lucy Letby was allowed to return to nursing duties, her murder trial has heard.
Concerns over an "accumulating number of inexplicable collapses" reached a "tipping point" with the deaths of two newborn triplets in June 2016, a consultant told Manchester Crown Court on Wednesday, March 22.
Dr John Gibbs told jurors that a number of "key safety measures" were then introduced including the removal of Letby from the neonatal unit.
However a month later he said hospital bosses wanted Letby – whom the consultants had identified as "the common link" to the collapses – back on the unit.
He told the court: "We said that should only happen if CCTV was put in each room in the unit.
"The CCTV didn't come and neither did staff nurse Letby."
Dr Gibbs, now retired, went on: "In the 11 months before the police got involved, after we raised concerns about the deaths of (Child O and Child P), senior management were extremely reluctant to involve the police to discuss what had happened because we had to keep insisting the police be involved."
Letby is accused of murdering seven babies and attempting to murder 10 others on the neonatal unit between June 2015 and June 2016.
She is said to have administered fatal doses of air to both Child O and P on successive day shifts.
Dr Gibbs reviewed Child P's condition shortly after the death of Child O on June 23.
He told the court: "'I remember feeling uncomfortable when I arrived on the unit and saw (Child O) and I thought 'Oh no, not another one'.
"I'd become increasingly concerned, and my consultant colleagues shared the concerns, at the accumulating number of unusual, unexpected and inexplicable collapses and deaths happening on the neonatal unit and the fact that staff nurse Letby had been involved in all of them.
"The deaths of the two triplets was a tipping point for realising something abnormal and wrong was happening on our unit."
Ben Myers KC, defending, said: "The reality is, as we stand here now, you are heavily influenced by a bias against nurse Letby that applies to all of you."
Dr Gibbs replied: "I was most heavily influenced by what was happening to babies on the unit… there was only one common factor."
Mr Myers asked: "You didn't contact the police, did you?"
Dr Gibbs said: "That was difficult. Nurse Letby seemed to be involved in all of the cases that involved me. Other consultants were involved with other babies.
"None of us regrettably realised two babies had been poisoned by insulin, so we didn't have the full picture.
"After the deaths of the triplets – very regrettably too late for them – because the concerns had reached a tipping point, safety measures were introduced and one of the key safety measures which the consultants were insistent on was Lucy Letby be removed from the neonatal unit and that was not a simple, straightforward decision."
Mr Myers said: "You took your time asking for CCTV if your suspicions were so great, Dr Gibbs?"
Dr Gibbs replied: "I said increasing concerns were growing over that time. The tipping point was the tragic deaths of the triplets which, looking back, should not have happened in healthy boys."
He said that Dr Stephen Brearey, the senior consultant in charge of the unit had previously flagged concerns to management in 2015 about the association with Letby and collapses of babies.
Last week Dr Brearey told the court he urged a hospital executive not to allow Letby to work the day shift after the death of Child P on June 24.
He said that she refused and it is alleged Letby attempted to murder another baby, Child Q, on June 25.
Jurors were told Letby submitted a formal grievance to management after she was removed from the unit.
The court has heard the surviving triplet brother was transferred to Liverpool Women's Hospital after his parents "begged" for a move following the deaths of his siblings.
Letby, originally from Hereford, denies all the allegations.
Thursday 23rd March 2023
Child P
Dr Dewi Evans - Dr Sandie BohinChester Standard Live Reporting
10:34am: The trial has now resumed. Benjamin Myers KC is cross-examining medical expert Dr Dewi Evans, who has written reports on all babies involved in the trial. The cross-examination today is focusing on Child P, one of two triplets who died at the Countess of Chester Hospital.
10:40am: In his reports, Dr Evans suggested the cause of death for Child P was complications from his pneumothorax. He was, however, suspicious of the large volume of air in the stomach and intestines evident on an x-ray. In his subsequent reports Dr Evans concluded that excess air in the stomach could have “splinted” the baby's diaphragm compromising his breathing. Mr Myers is first asking about the efforts to save Child P's brother Child O, about damage to the liver. Mr Myers asks if this could come as a result of chest compressions. Dr Evans says if the compressions are done properly, this would not be the case.
10:42am: A video is shown to the court showing the correct procedure on providing chest compressions to an infant. Mr Myers again asks if it is possible for damage to be caused to the liver by several minutes of 'vigorous' chest compressions. Dr Evans says he has never seen it in his experience.
10:47am: The questions now move on to Child P. Mr Myers confirms what Dr Evans had written for his three reports concerning Child P, involving complications to the pneumothorax. Dr Evans said his view was that he could not explain, at the time of the first report, any other cause for why resuscitation was not successful.
10:48am: Dr Evans confirms he could come up with no 'natural cause' for Child P's death.
10:54am: Mr Myers asks about the 'splinting' of the diaphragm Dr Evans had written about in his report for Child P. He says in a following report, 'it is necessary to scrutinise the night care from June 23/24'. Dr Evans said it was the 'option at the time'. He says there was excess air in the x-ray from the night before which destabilised the baby, and meant he was unable to take feeds properly. He says in light of evidence given by local staff over the past few days, additional air was given to Child P during the morning of June 24 which splintered the diaphragm and caused the collapse. He says there were two events - excess given prior to the x-ray, which destabilised the baby, and further air into the stomach on the morning of June 24. He says that is a "more accurate way of explaining the events".
10:58am: Dr Evans says the most recent of his reports is from 2019, and he has since had a far better understanding of the clinical sequence of events as a result of the trial in 2023. He said he was "more concerned" from his evidence at the time about the night care, when Child P was not taking feeds and had a bradycardic event. He adds he does not believe Child P would have collapsed without an additional administration of air in the morning. Mr Myers says Dr Evans has "shunted" the sequence to the point where Lucy Letby was on duty for that day shift on June 24. Dr Evans denies this, saying if he was wanting to put Letby in the frame, he would have included events from the June 23 day shift, when Letby was also on duty.
11:00am: Dr Evans says an "extra dollop" of air would have been administered just before 9.40am on June 24. He says Child P could have been suffering the consequences of an administration of air from the previous night by the following morning, but that would have been insufficient to cause a collapse, not without a further administration of air.
11:01am: Mr Myers says Dr Evans is "coming up with ideas and theories" rather than relying on the medical evidence available. Dr Evans says that is "incorrect". Mr Myers says Dr Evans has "invented an extra dollop of air". Dr Evans says he is satisfied, from a clinical perspective, about the additional administration of air on the morning of June 24. He says it is not a "guess" but a "clinical assessment".
11:08am: A blood gas result for Child P is shown to the court from June 23, showing 'normal gas readings'. Dr Evans says an administration of air would not necessarily lead to a baby "crashing". It would lead to them not tolerating milk. Observations for Child P are shown for the night of June 23. Dr Evans says there is more to a baby than a pair of lungs, there is also the stomach and intestines. The 'first administration of air' did not affect the breathing, he tells the court, but led to Child P being unable to feed. The 'second administration of air' the following morning caused splinting of the diaphragm, he says.
11:16am: Mr Myers repeats that Dr Evans has 'invented a theory' of a dollop of air to get it 'over the line'. Dr Evans denies this.
11:19am: That concludes Dr Evans's evidence for Child P. Dr Sandie Bohin is now called to give evidence. Prosecutor Nicholas Johnson KC says Dr Bohin has completed a total of five reports for Child P.
11:30am: Dr Bohin confirms she had looked through all the clinical notes for Child P, including one by Lucy Letby where she had written about the NG tube being on free drainage at 8am. A note at 6.39am by Sophie Ellis, from the night shift, said Child P's abdomen was 'soft and non distended', with '25mls air aspirated' and 'NG Tube placed on free drainage'. Letby later noted, at about 9.30am, Child P had an apnoea, brady, desat with mottled appearance, requiring facial oxygen and Neopuff for approx 1min. Abdomen becoming distended.' A consultant doctor was called to the nursery where Child P was.
11:41am: Child P had a 'speedy recovery' that morning and Dr Bohin is asked if that was normal.
Dr Bohin: "No, it was not." Child P then desaturated again at 11.30am and was given adrenaline and paralysed with a drug to aid ventilation. His circulation was restored but he continued to deteriorate throughout the day.11:51am: Dr Bohin is now telling the court about the adrenaline doses which were administered to Child P throughout June 24, their concentrations and totals.
11:55am: Dr Bohin explains the rate of adrenaline administered to Child P, according to the medical notes, was not calculated correctly - it was double what it should have been.
11:58am: Dr Bohin says the excess adrenaline would not have had any adverse effect, as it began to be administered after Child P had the collapse and was already suffering metabolic acidosis. She says it is "impossible" to quantify any effect on lactic acidosis. It did not adversely affect the blood pressure or heart rate, Dr Bohin adds.
12:01pm: Dr Bohin tells the court she was concerned about the gas in the initial abdominal x-ray, which had been taken as a 'precaution' with no concerns about the abdomen, but it was "full of gas" and "abdominal distention right through". The x-ray was "abnormal". Throughout the night, Child P became intolerant to feeds, and the abdominal distention was reduced, but then Child P's abdomen became "distended and loopy" in the morning. That was "difficult to explain".
12:03pm: Dr Bohin says Child P should have had a further x-ray sooner after he first collapsed, and more attention paid to the pneumothorax.
12:04pm: The ventilatory pressures were "quite high" for Child P, who had no underlying lung disease. This was not a criticism of the staff, Dr Bohin says.
12:06pm: For a cause to the collapse, Dr Bohin says she could find no reason why there was excess air from the previous night, and there was splinting of the diaphragm. It was something "striking and out of the ordinary". Child P had shown no signs of infection, and no evidence was found. Dr Bohin says her conclusion was air had been administered via the NG Tube. She cannot explain why Child P had further collapses on June 24.
12:24pm: The court is resuming after a short break. Mr Johnson has one more point to raise with Dr Bohin. He asks her about the adrenaline dose rates being double what they should be, and if that was beyond a safe limit. Dr Bohin explains the limits, in accordance with guidance, would have been within limits, but the higher the rate, the more the risk of side-effects. Higher doses would be administered in extreme circumstances, on guidance from a consultant. Side effects would be rising blood pressure, rising heart rates, irregular heart rates, and, in very high doses, and constricting of blood vessels.
12:26pm: Mr Myers is now asking Dr Bohin questions. He asks about the need for an x-ray to have been taken sooner. Dr Bohin said that would have been needed when looking for the cause of a collapse. Mr Myers says Dr Bohin had, in her report, identified a particular issue with the adrenaline, which she had recorded as a "high starting dose".
12:30pm: Mr Myers says the ventilator settings were also 'high'. Dr Bohin agrees the settings did not need to be as high as the oxygen requirement was not so high.
12:32pm: Dr Bohin says the pneumothorax could have contributed to the collapse, but would not have caused it.
12:39pm: Mr Myers says the care offered to Child P was, in Dr Bohin's words, 'muddled' and 'unusual' following the baby boy's collapse. Dr Bohin said 'questions need to be answered' about the ventilatory strategy and the high doses of adrenaline, but the latter issue had been raised and answered by doctors in court. She adds that neither of those issues had caused the initial collapse of Child P.
12:41pm: Mr Myers asks about the rate of adrenaline administration. Dr Bohin says the starting rate depends on what the child has, their condition, and what they have been administered before. Dr Bohin says doctors wanted to give a 'large dose to kick-start the heart', as Child P had suffered a cardiac arrest. Even at this rate, the dose was ineffective, Dr Bohin adds.
12:52pm: Mr Myers asks about a "very high" lactate reading Child P had at 10.46am on June 24. Dr Bohin says it is "impossible" to quantify, to what degree, the effect adrenaline doses would have had on the lactate levels, particularly on Child P, who had previously had a cardiac arrest which would have raised lactate levels in any case.
12:58pm: Mr Myers moves on to question about the cause of Child P's collapse. He says it is not mentioned in Dr Bohin's reports about any additional administrations of air that morning. Dr Bohin says there is not. He says the only evidence of abdominal distention is from 4am. Dr Bohin says it was identified then, it went away, then it is noted as appearing 'distended and loopy' again in the morning. Mr Myers asks if Dr Bohin says the splinting of the diaphragm is from air administered the night before. Dr Bohin disagrees.
1:05pm: Dr Bohin says the collapse was 'unexpected and completely unexplained'. The collapse happened 10 minutes after Dr Anthony Ukoh examined Child P and found the abdomen 'moderately distended / bloated'. Dr Bohin says an issue she has had in the course of the trial is there does not seem to be consistent practice among nursing staff in the aspirations of feeding tubes, but in this case, when there was 25mls of air aspirated early on June 24, that was "normal".
2:05pm: The trial is resuming following its lunch break.
2:18pm: Benjamin Myers KC continues to ask Dr Sandie Bohin questions. He refers to the case of Child G, in reference to milk and pH levels, where a pH level from the aspirates was recorded as '4' on September 7, 2015, at 2am. Dr Bohin had said a pH level of 4 was 'very acidic', and there was not milk in the tummy, as the milk would 'buffer' the pH level and 'neutralise it'. For Child P, the feeding chart on June 23, 2016 at 8pm records 14ml of milk aspirated and a pH level of 3. Mr Myers says 20mls of milk is aspirated several hours later, with a pH level of 3. Mr Myers says that it can mean milk could have been present in the stomach for Child G, even with a pH level of 4. Dr Bohin said milk would 'buffer' the pH level. She adds the trial has moved through so many babies since Child G, she would need to know the clinical context for Child G. Mr Johnson asks to clarify the meaning of 'buffer'. Dr Bohin said it would effectively neutralise it.
2:20pm: Nicholas Johnson rises to clarify pulmonary hypertension as a possible diagnosis. Dr Bohin says it can affect blood flow and blood pressure. In neonates, it’s an attempt for them to return to the conditions where they were in their mummy's tummy, but staff don't want that in terms of making sure a baby is clinically stable. "It's a very difficult thing to treat," Dr Bohin adds. Dr Bohin adds one of the treatments is making sure the blood pressure in the body, not the lungs, is high, through treatment.
2:21pm: That concludes Dr Bohin's evidence for Child P.
2:25pm: The judge, Mr Justice James Goss, is informing the jury they will not be required on Friday. It remains unknown whether they will be required for next Monday. If not, their next day of evidence will be on Tuesday, March 28.
2:28pm: The jury is told the case of Child Q will begin next week, and evidence will take place over three days. Child Q is the last of the 17 babies, chronologically, in the case.
2:33pm: Work is ongoing between the prosecution and defence to have an agreed version and length of Lucy Letby's interviews with police to be shown to the jury, the court hears. Those will be played, it is intended, before the Easter break, which begins on Good Friday (April 7) and the jury will return on April 17 at noon. The court hears the jury will also not be sitting on April 18.
Friday 24th March 2023 - no court (pre-planned)
Monday 27th March 2023 - no court (pre-planned)
Tuesday 28th March 2023 - no court (juror ill)
Wednesday 29th March 2023
Children A, C, D, I & O
Pathologist Dr Andreas Marnerides10:09am: Lucy Letby's murder trial continues this morning. We're expecting to hear evidence from expert witness Dr Andreas Marnerides. He'll be taking the court over pathology reports. Ms Letby is accused of murdering seven babies and attempting to murder 10 others. She denies all charges
10:41am: Jury are currently being read the pathology reports for a number of children in the case - they have been warned that there is a lot of incredibly dense medical detail and will be provided with a glossary of terms afterwards. Dr Marnerides due in witness box later this morning
11:59am: Dr Marnerides, who leads the forensic children's pathology service at Guy's and St Thomas' Hospitals, is now in witness box. He reviewed tissue samples from Child A, who the Crown say was murdered by Ms Letby in June 2015 via air injection The medic says from his review, he found 'globules' in the veins in the lungs and brain tissue that were most likely air, he said this air 'most likely went there while this baby was alive'
1:06pm: Dr Marnerides was also asked to review the case of Child C, who died in June 2015. The Crown say Ms Letby murdered the five-days-old boy by injecting air into his stomach through a nose tube, making him unable to breathe. The medic said in his opinion, on basis of all evidence reviewed Child C's sudden collapse was caused by an 'injection/infusion of air into the NG tube'
2:31pm: Dr Marnerides was asked to review the case of Child D, who also died in June 2015. The Crown say she too was killed by Ms Letby via an injection of air. The medic said from his pathological review, air embolism is the 'likely explanation' for Child D's death
3:14pm: On the case of Child I, the medic comes to the same conclusion - that she died as a result of an injection of air
3:52pm: To assist the jury with his findings in relation to triplet brother Child O, who died in June 2016, Dr Marnerides presented a photograph of the baby boy's liver, taken at post-mortem, to the court. The court has previously heard that Child O died after suffering "trauma" to his liver and an injection of air into his bloodstream. The images showed a "rather large bruise" to the boy's liver that would have caused an internal bleed, Dr Marnerides said.
Chester Standard article 29-03-2023
A TRIPLET baby boy allegedly murdered by nurse Lucy Letby suffered a liver injury akin to a road traffic collision, her trial has heard.
Letby, 33, is said to have attacked the new-born infant on a day shift on June 23, 2016 at the Countess of Chester's neo-natal unit following her return from a holiday to Ibiza.
Child O is alleged to have been one of 17 babies she targeted between June 2015 and June 2016.
He was born in good condition, Manchester Crown Court has heard, until he suddenly collapsed two days later in the care of Letby and went progressively downhill as medics failed to revive him.
On the following day shift, the Crown says she murdered Child P, one of Child O's triplet brothers.
On Wednesday, March 29, paediatric pathologist Dr Andreas Marnerides said Child O died partly due to an "impact-type" internal liver injury – discovered after the baby's death.
Jurors were shown post-mortem examination photographs which showed two separate sites of bruising, as well as areas of a blood clot.
Prosecutor Nick Johnson KC asked the consultant: "How does that injury come to be in a child of (Child O's) age?"
Dr Marnerides, who practises at London's St Thomas' Hospital, said: "The distribution, the pattern and the appearance of the bruising indicates towards impact-type injury. I'm fairly confident this is impact-type injury."
He explained the photograph showed "extensive haemorrhaging into the liver", which he had only seen previously in a road traffic collision and in non-accidental assaults from parents or carers.
Mr Johnson said: "Looking at this sequence of photographs, can you rule out the possibility that these injuries were caused by CPR?"
Dr Marnerides said: "I cannot convince myself that in the setting of a neonatal unit this would be a reasonable proposition to explain this. I don't think CPR can produce this extensive injury to a liver."
Mr Johnson said: "In so far as you have spoken about an impact-type scenario for causing that internal injury, would you necessarily expect to see any outside sign on the skin itself?"
The consultant replied: "You can have the most devastating injury internally and nothing can be observed externally. That is very common."
Mr Johnson went on: "What in your view was the cause of death of (Child O)?"
Dr Marnerides said: "In my view, the cause of death was inflicted traumatic injury to the liver, profound gastric and intestinal distension following acute excessive injection/infusion of air via a naso-gastric tube and air embolism due to administration into a venous line."
The consultant was approached by Cheshire Police in late 2017 to review the deaths of a number of babies at the hospital, the court heard.
He gave his opinion on their causes of death after having reviewed the pathological evidence as well as information received from clinical and radiological reviews.
Dr Marnerides said it appeared Child A, a twin boy, died as a result of an injection of air into his bloodstream.
Child C, a boy, was subjected to an excessive infusion/injection of air into his nasogastric tube, he said.
The "likely explanation" for the death of Child D, a girl, was an air embolism into her circulation.
Another girl, Child I, received an excessive injection of air into her stomach, he said.
He told the court he could no offer no opinion on the death of Child E, a twin boy, because no post-mortem examination took place.
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others.
Thursday 30th March 2023
Children A, C, D, I & O
Pathologist Dr Andreas Marnerides9:59am: Lucy Letby's murder trial continues with evidence from expert pathologist Dr Andreas Marnerides this morning. The medic told the court yesterday that it was 'likely' a number of babies died at the Countess of Chester Hospital as a result of air injection
10:09am: Dr Marnerides was asked to review the case by Cheshire Police in 2017. He is currently taking the court through his review of Child P, who was one of triplets born in June 2016. Ms Letby is accused of killing the boy the day after allegedly murdering his triplet brother, Child O. The Crown say he was killed by an injection of air into his bloodstream.
10:22am: Dr Marnerides said in his review of Child P, he could not find anything to 'indicate natural disease for the baby's death'
10:24am: To assist the jury with his findings in relation to Child P, Dr Marnerides is presenting photographs of the baby boy's liver, taken at post-mortem, to the court. The images show small bruises on the outside of the boy's liver
10:30am: Dr Marnerides tells the court that the bruising, although a lot smaller, is in the same area that it was found in Child P's brother Child O. The court heard yesterday that Child O suffered a liver injury akin to a road traffic collision.
10:32am: The medic says the bruising found 'could' be the result of CPR - asked whether it could be another impact injury, he says 'I don’t have enough to say that'
10:39am: Dr Marnerides says having reviewed all the evidence, it is his opinion that Child P died as a result of 'excessive injection of air into the stomach'
10:46am: Ms Letby's defence lawyer, Ben Myers KC, is now cross examining Dr Marnerides - he starts by telling the court that there are 'strict rules about the extent to which an expert can give an opinion on matters outside their specialism' - he agrees
10:48am: The medic accepts he cannot offer a view on day to day care, feeding, breathing support or resuscitation of the babies in this case. Mr Myers says when there is no specific finings 'one way or another' in the pathology, he works on the basis of the opinions of the clinicians 'unless something directly contradicts that' - Dr Marnerides agrees
11:13am: Mr Myers is now taking the medic back over the cases he has reviewed, starting with Child A. Mr Myers quotes his review, in which Dr Marnerides said the cause of death was 'unascertained' and that there was no 'convincing indication the death was due to an unnatural cause' Mr Myers asks the medic if he agrees, he responds: 'Yes, I wrote it'
12:45pm: Cross examination of Dr Marnerides continuing, Mr Myers has taken the medic back over his evidence for Child C, D and now I. The defence lawyer is focusing his questioning on the fact he has had to rely on Dr Dewi Evans and other medics for his review. Dr Marnerides earlier said to discount the clinical evidence in forming his reports was akin asking someone to explain physics without using mathematics
2:10pm: We're back after lunch and have moved to Child O. Yesterday the court heard that the boy allegedly suffered a liver injury akin to a road traffic collision - Mr Myers has been asking Dr Marnerides about the minimum force needed to cause such an injury
2:14pm: Dr Marnerides says there is 'no way of measuring the force in a baby because we cannot conduct such experiments on babies'. He says from his experience, the minimum force required 'would be of the magnitude of forces generated from a baby jumping on a trampoline and falling'
2:29pm: Mr Myers puts it to the medic whether vigorous CPR could have caused the injuries found in Child O's liver - he says no. Mr Myers asks whether it can be categorically excluded as a possibility The medic goes a bit leftfield with his response. He says to the court that if a man is found dead in the Sahara desert with a pot next to him, it could be possible that a helicopter flew over and dropped it on his head - but it's not probable
Chester Standard article 30-03-2023
"FORCEFUL CPR" could not explain liver damage suffered by a baby allegedly murdered by nurse Lucy Letby, a court has heard.
Letby, 33, is said to have attacked the new-born triplet on a day shift on June 23, 2016 at the Countess of Chester’s neo-natal unit following her return from a holiday to Ibiza.
Child O is alleged to have been one of 17 babies she targeted between June 2015 and June 2016.
He was born in good condition, Manchester Crown Court has heard, until he suddenly collapsed two days later in the care of Letby and went progressively downhill as medics failed to revive him.
Paediatric pathology expert Dr Andreas Marnerides had told jurors he concluded Child O died because of "inflicted traumatic injury" to the liver, as well as receiving fatal injections of air into the stomach and bloodstream.
He compared the extent of the liver injuries to those suffered fatally by children involved in road traffic accidents and non-accidental assaults.
On Thursday, March 30, Ben Myers KC, cross-examining, said: "Can you assist with how little force could be involved?"
The consultant at London’s St Thomas’ Hospital said: "I think there is no way of measuring a force in a baby because we don’t conduct such experiments on babies.
"I have never seen this type of injury in the context of CPR so I would say the force required would be of the magnitude of that generated by a baby jumping on a trampoline and falling."
He agreed that smaller internal bruising to the liver sustained by Child O’s triplet brother Child P – who Letby is alleged to have murdered the next day – could be capable of being caused by CPR.
But asked if "rigorous" chest compressions could be the cause of the internal bruising in Child O’s case, Dr Marnerides said: "I don’t think so, no.
"This is a huge area of bruising for a liver of this size. This is not something you see in CPR."
Mr Myers said: "So you don’t accept the proposition that forceful CPR could cause this injury in general terms, do you agree it cannot be categorically excluded as a possibility?"
Dr Marnerides replied: "We are not discussing possibilities here, we are discussing probabilities.
"When you refer to possibilities, I am thinking for example of somebody walking in the middle of the Sahara desert found dead with a pot and head trauma.
"It is possible the pot fell from the air from a helicopter. The question is ‘is it probable?’ and I don’t think we can say it is probable."
Mr Myers asked: "Is it possible in your opinion for at least some of what we see in the damage to the liver arising from the insertion of a cannula?"
The consultant said: "I would consider it extremely unlikely. I would expect some kind of perforation injury."
Earlier, Dr Marnerides said the most likely explanation for the death of Child P was excessive air injected via a nasogastric tube into his stomach.
Letby, originally from Hereford, denies the murders of seven babies and the attempted murder of 10 others.
Friday 31st March 2023
Child Q
Parents' statements - Police analyst: Recorded events & messages - Statements of Midwife & Nurse Christopher Booth - Nurse Tanya DownesChester Standard Live Reporting
9:05am: This is the 22nd week of the trial. Today, the prosecution is expected to begin delivering evidence into the case of Child Q, the final of 17 babies that the Crown allege Lucy Letby murdered or attempted to murder between June 2015 and June 2016. The defence deny this.
10:06am: The trial is expected to resume at 10.30am.
10:32am: The prosecution allege Lucy Letby attempted to murder Child Q on Saturday, June 25, 2016, one day after Child P died and two days after Child O died. It was the penultimate week Letby was working as a neonatal unit nurse at the Countess of Chester Hospital.
10:33am: The prosecution begin the case of Child Q, a baby boy. A statement is read from Child Q's mother.
10:38am: She said Child Q was born on June 22, 2016 at 04.09am. She describes her pregnancy as "difficult" and pushed for a 9-week scan at the Countess of Chester Hospital. Outside the womb, a problem was found. One twin was inside the womb, the other was outside the womb. She was sent for surgery and Child Q's twin was removed. Child Q was born at 31 weeks + 3 days gestation. The mother had a heavy bleed and had to have emergency surgery. She was not able to see her son for 12 hours after the operation. Child Q was admitted to the neonatal unit in room 1 as he had problems with his breathing, the court hears.
10:40am: The mother said she was not able to hold Child Q, but able to put her hands in the side of the incubator. When she talked to him, he opened his eyes for the first time. The following day, Child Q had a feeding tube, off breathing support, but at the end of the day, she was told he would have to go back on breathing support, which made her upset. She says at no point were they told Child Q had a collapse, and believed the staff would try and 'play things down' in regard to his situation. At one week of age, Child Q was transferred to Alder Hey for a potential procedure to have part of his bowel removed, although this was not required ultimately.
10:45am: Child Q has 'been in and out of hospital' several times a year since as he has a weakened immune system, the mother adds. The father's statement says his wife had a "very difficult pregnancy", and was in and out of hospital every six weeks, and taken in at 26 weeks due to 'very heavy bleeding.' She was stabilised and put in the women and children's building at the hospital, and would have a number of bleeds. At 31weeks +3 days, the father received a phone call telling him the mother was going into labour. He was not allowed to attend the birth due to the mother's condition. He saw Child Q when Child Q was being transferred to the neonatal unit, and "he was tiny". The mother was still under anaesthetic.
10:50am: At one afternoon, the father went to visit Child Q and was prevented entry by staff. He was told: "There was nothing to worry about", Child Q had a 'chest infection', and the unit was 'screened off and shut down'. He returned to the mother, and they decided to go to the neonatal unit together. He said the staff told them they were running some tests. Later, the parents were allowed to return to the neonatal unit. They asked a doctor what had happened and Child Q had had a 'blip', was 'tired', and needed breathing support. Within the following couple of weeks, the parents were told Child Q had a 'serious bowel infection' and awaiting an ambulance to transfer to Alder Hey. By the time Child Q went to Alder Hey, he had recovered. He returned to the Countess and recovered 'really well', progressing through the neonatal unit nursery rooms. Child Q was later diagnosed with cerebral palsy and still had bowel issues, but was 'coping well'.
11:00am: Intelligence analyst Kate Tyndall is now talking the court through what is likely to be the prosecution's final sequence of events, this being the case of Child Q. Child Q was born at 4.09am on June 22, 2016, in initially poor condition, appearing 'blue, occasional gasp, poor tone'. Inflation breaths were given and oxygen support at 80% O2 was administered. The 'Apgar scores', indicating a newborn baby's condition out of 10, are '4' at one minute, '7' at five minutes and '9' at 10 minutes. Registered nurse Amy Davies said child Q cried at delivery, was stabilised and transferred to the neonatal unit, intubated and given antibiotics. The sequence says Child Q was treated at the neonatal unit between 8.30am on June 22 to 7.40am on June 24. On June 23, at 5.47pm, Child O died and at 6pm, Child P had an event where his abdomen was distended.
11:02am: The day shift of June 24 is when Child P - triplet brother of Child O - died, prosecutor Nicholas Johnson KC reminds the court. Child P had a collapse at 9.30am on June 24.
11:09am: The sequence records a series of observations taken for Child Q throughout the day. Child P's time of death is 4pm on June 24. Nursing notes for Child Q, written by Amanda MacKenzie, record at 9.06pm: 'Thought to have a few bradycardias in a cluster this morning but seemed to be a loose ECG lead when checked - none noted following changing the lead. Nystatin not given - very heavy workload on unit'.
11:11am: The medication for nystatin is prescribed at 11pm. A Facebook message sent from a doctor to Lucy Letby at 11.49pm: 'Did you talk to Belinda about allocation for tomorrow?'
Letby: 'Yes, she's going to try and give me a lighter workload...' Letby adds this will be difficult given there are only five on the staff rota.11:16am: Child Q was noted as having small levels of bile in his aspirates from the fluid chart, but these were not enough to stop him being fed as normal. Nurse Samantha O'Brien recorded, within her nursing notes at 5.20am on June 25: 'Having trophic feeds of donor expressed breast milk, 0.5mls 2 hourly due to moderate aspirates. Abdomen is full but soft.' No respiratory distress was observed.
11:18am: Letby messages a nursing colleague at 6.36am enquiring about the night shift. The reply begins 'OK', before giving details of what was done that night and babies in the unit.
11:22am: Nurse Samantha O'Brien records at 7.30am a blood gas test result was 'not as good' as the one previously, but still 'acceptable'. The day shift handover takes place at 7.30am. Lucy Letby is a designated nurse for Child Q, in room 2, and a baby in room 1. Three babies are in room 1, two in room 2, three in nursery 3 and four in room 4. One nurse is looking after two babies in room 1, one nurse is looking after four babies in rooms 2-4, and another nurse is looking after four babies in rooms 3-4.
11:24am: An observation chart is shown for Child Q for June 24-25. The heart rate and breathing rate are shown as being in the normal range up until 9am, when Child Q collapsed. Both then increase to an area out of the normal range at the time of the collapse. Child Q had been 'in air' prior to the collapse.
11:29am: A fluid balance chart is shown for Child Q. The 9am reading is not initialled, and do not record a feed at that time. Child Q collapsed at 9.01am.
11:35am: An apnoea/brady/fit chart is shown to the court - the brady is '98', desat '68', fit '?', duration '3 minutes intermittently'. Baby found to be very mucousy, clear mucous from nasopharynx oropharynx, clear fluid+++ , O2 via Neopuff, given post-suctioning. Dr...emergency called to attend. 'NGT used to aspirate stomach by nurse Lucy Letby'. The prosecution say Child Q had been fed 1.5mls of milk from the night, and had been due to be fed at 9am. Lucy Letby, in a nursing note, records: '0910 ...Child Q had vomited clear fluid nasally and from mouth. Desaturation and brady, mottled++. Neopuff and suction applied. Air++ aspirated from NG Tube...' The doctor called to the unit records 'called to NNU @ 0917 desaturation Had just vomited and then desaturated to low 60s. Minor bradycardia. Bagged with Neopuff circuit...' Child Q was transferred from nursery room 2, the high dependency unit, to nursery room 1, the intensive treatment unit.
11:41am: Medication is administered to Child Q during the morning. Child Q is x-rayed and the report notes: 'Respiratory deterioration now needing CPAP'. The x-ray records nothing unusual, the prosecution say. Letby writes notes for child Q, written retrospectively at 12.53pm: 'Septic screen carried out....NG Tube on free drainage. -3mls milk/mucous aspirate. Abdomen soft and non-distended. Perfusion improved...intermittent episodes of tachypnoea...'
11:44am: Letby records for family communication at 1pm: 'Parents visited shortly after [Child Q] had been screened and commenced on CPAP. Mum upset++ and dad has since stated mum upset that she was not contacted on postnatal ward about need for intervention.' Letby adds she explained the situation and apologies were given.
11:46am: Letby messages a nursing colleague about the situation on the neonatal unit, adding: 'All going on lol' Letby also messages a doctor colleague between 12.18-1.16pm.
12:01pm: A correction is being made to the sequence of events - the timing of Child Q's collapse should not read '09.01am'. The court had heard the time of the collapse has been noted as 9.10am.
12:05pm: Further observations are made for Child Q during the afternoon. Letby notes: 'Observations stable, continues to have low respiratory rate with minimal effort at times. Appears plethoric++ this afternoon....Remains on free drainage...' For the family communication note, Letby notes: 'Midwife phoned on behalf of mum to express concern that staff had not contacted parents when [Child Q] needed CPAP. Explained reasons for this and encouraged mum to visit...' The parents visited the unit. Letby adds: 'Apologies were given for not updating them but...[treating Child Q] was priority at the time. Mum appears happier...'
12:08pm: Letby messages a nursing colleague via WhatsApp at 6.40pm 'Girls all rushing around outside', adding one of the nurses was 'stressing', and the situation was 'madness lol'. Further medication is administered to Child Q in the evening.
12:12pm: A deterioration is noted in Child Q which required his intubation. The notes are recorded by a doctor. Letby notes before the shift handover at 7.30pm: 'Respiratory rate declining (15-19bpm) and intermittent pauses in breathing. Blood gas stable but on downward trend and [Child Q] appearing 'tired'. Oxygen requirement developing....decision made [following consultation with doctor] to electively intubate. Drugs given as prescribed...'
12:18pm: Care of Child Q was handed over to staff nurse Amy Davies. A record of Facebook messages between Letby and a doctor colleague is recorded between 4.11pm and 8.31pm. Letby then adds: 'Wow, I think I might be almost finished' to the doctor. She also messages her mother. Colleague Minna Lappalainen then messages: 'Thank you for being a good friend today', adding a heart emoji.
Letby: 'Don't need to thank me Minna, I'm always here for you. Please don't feel you're alone...' Lappalainen: '...But really I'm really happy u were there for me....'
Letby: 'Take care, hope you sleep well, see you tomorrow'. Sophie Ellis messages
Letby: 'Hope your feeling ok today'
Letby: 'Thanks Soph, another busy day today but ok today and off tomorrow....'
Ellis: 'I think you deserve more than a day off...'
Letby: '...It's been awful but we'll be ok'.12:20pm: Nurse Amy Davies, in her nursing notes, records Child Q was '...unsettled at the beginning of the shift but has settled. Temperature is elevated, humidity and incubator temp altered accordingly. HR is elevated up to 208 at times. Dad has visited...' Observations are taken for Child Q.
12:27pm: Letby messages a doctor at 10.48pm: 'Do I need to be worried about what Dr Gibbs was asking?' Response: 'No. He was asking to make sure that normal procedures were being carried out' What exactly did he ask?' Letby replies Dr Gibbs had been asking colleague Mary Griffiths who was present in the room (when Child Q had collapsed) and how quickly someone had gone to him because Lucy Letby had not been there. The response: 'All he was doing was checking there was not a delay and that a room had been left empty...there is nothing to worry about'. The doctor adds: 'You can't be with two babies in different nurseries at the same time, let alone predict when they're going to crash'.
Letby: 'I know, and I didn't leave them alone'. The response: Nobody has accused you of neglecting a baby or causing a deterioration'. Letby responds she wonders if, following the deaths of two babies, she is doing well enough. The doctor replies he would be willing to provide a statement to back Letby up in any event. He adds: 'It's why I am so happy to work with you. You don't flap, you give perfectly sensible suggestions... No more doubt - it's not you, it's the babies.' Letby adds: 'So relieved that it's you who has been there throughout.'12:28pm: The doctor replies: 'It's true. You are one of a few nurses across the region...that I would trust with my own children...
Letby: Don't know what to say, thank you. The doctor replies: 'Self-doubt finished?'
Letby: 'I think so, thank you ++'12:30pm: The sequence of events says the messages between Letby and the doctor continue from 12.18am-1.36am on June 26, on topics not related to Child Q.
12:33pm: At 8.15am on June 26, nurse Amy Davies records for Child Q, improved blood gas readings through the night. From 0200-0600 [Child Q] was very settled, minimal handling carried out, HR reduced to 158-170....Gas repeated at 0623, poor result...Dr contacted [and reviewed]...' Child Q was transferred to Alder Hey on June 26 and was treated there until June 28.
12:37pm: On June 26, Letby is messaging a nursing colleague from 7.50am. The nursing colleague was working at the time. The nurse says Child Q was improving but then had 'crap gas' at 5am. She adds 'staffing is s***e isn't it'.
Letby: 'Bloody hell. It's not safe is it especially with what's gone on' I worry that we have got a bug or virus on the unit' The nursing colleague replies: 'Virus would explain a lot'.12:39pm: Letby messages the doctor colleague: 'Will you let me know how [Child Q] gets on today please' Of course I will' is the reply. The messages continue throughout the morning. The doctor adds at 12.19pm: '[Child Q] has nec'
Letby: 'Ok that's good in a way to have a cause. Going to AHCH [Alder Hey Children's Hospital]? Is he stable?' Doctor: 'Ish. Ventilation was up and down overnight...'12:44pm: Letby messages a nursing colleague to say Child Q was 'unwell with NEC, going to picu' The response: 'Oh no poor [Child Q]! Who's told you that?' Letby responds that the doctor let her know. The nurse later messages
Letby: They think [Child Q] could be a volvulus apparently' Letby responds: 'Oh no.'12:51pm: The doctor messages Letby on June 27 at 10.55am - 'Not sure if the unit is open for transfers. Few managers/directors around this morning'. The doctor adds it's 'odd' Child M was only at Alder Hey for 14 hours as he was coming back to the Countess of Chester Hospital. He says there is a lack of beds at Alder Hey, and it's disruptive for the parents. Letby agrees. The final sequence of events concludes by noting Child Q was looked after at the Countess of Chester Hospital between June 28 and July 25, 2016, when he was discharged.
1:04pm: A diagram shown at the end of the June 25, 2016 day shift shows there are three babies, including Child Q, in nursery 1, two in room 2, three in room 3 and four in room 4. Letby is the designated nurse for Child Q only at the end of the shift, with care of her other designated baby being transferred to another nurse.
1:54pm: Here is a fuller version of the text messages between Lucy Letby and the doctor from 10.47pm on Saturday, June 25, 2016. The doctor, who cannot be named, is for this purpose listed as 'R' for 'Response':
Letby: Do I need to be worried about what Dr Gibbs was asking?
R: No
R: He was asking to make sure that normal procedures were being carried out.
R: What exactly did he ask?
LL: I walked into equipment room, he was asking Mary who was present in room and how quickly someone had gone to him as I wasn't in the room.
LL: He asked who was there, I said I had popped out of room but Mary was in room and Minna at the desk.
R: All he was doing was checking that there wasn't a delay and that a room had been left empty. Was he HDU level because of uvc? There is nothing to worry about.
LL: Ok. Was worried because I Wasn't with him at time, but Mary was in room and Minna outside, I had [designated baby who was not Child Q] in 1. ITU because of uvc
R: You can't be with two babies in different nurseries at the same time, let alone predict when they're going to crash......
LL: I know, and I didn't leave him on his own. They both knew I was leaving the room. Feel better now1:56pm: R: Nobody has accused you of neglecting a baby or causing a deterioration.
LL: I know. Just worry i haven't done enough
R: How?
LL: We've lost 2 babies I Was caring for and now this happened today, makes you think 'am I missing something/good enough'
R: Lucy, if anyone knows how hard you've worked over the last three days it's me. The standard of care delivered is tertiary nicu level. if *anybody* says anything to you about not being good enough or performing adequately I want you to promise me that you'll give my details to provide a statement. I don't care who it is and I don't care if I've left the trust.
R: Promise?
LL: Well I sincerely hope I won't ever be needing a statement But thank you, I promise1:59pm: R: And I don't either. You'll know that the coch nicu mortality rate is a bit higher than the network average. It makes people (consultants) look at trends and patterns. That may have been why DrG came to ask. As for the self-doubt - you asked me this morning did I dream because I was worried about having missed something? No, and I don't think you did either. In fact for [another baby] you knew he was unwell and flagged it up immediately. I don't know the beginning of the [a separate baby] story because i arrived after the bleep. You didn't miss anything that I would expect an experienced itu trained nurse to spot. From a resus point out view you were flawless. It's why I am so happy to work with you. You don't flap, you give perfectly sensible suggestions and things run seamlessly. (You must be good Rackham said so (seldom praises)).
R: No more doubt - it's not you, it's the babies. I don't know what happened to [Child O] and [Child P], and accept that the pm may not give any useful answers. I Do wonder if they may have had adenovirus - it's terrible in neonates / perinates. [Child Q] is different. His behaviour is more bacterial (tachy, temp, reduced uo) I wouldn't be surprised if his bc comes back positive.
LL: Thanks, really appreciate you saying that.
LL: So relieved that it's you who has been there throughout.2:01pm: R: It's true. You are one of a few nurses across the region...that I would trust with my own children. If you're worried - I'm worried. You should do the APNP course, you'd be excellent.
LL: Don't know what to say Thank you
R: Self-doubt finished?
LL: I think so, thank you ++ The messages continue on a social/work nature until 1.36am, but have no further reference to Child Q.2:10pm: Prosecutor Philip Astbury is now reading out some agreed statements. The first is from a midwife at the Countess of Chester Hospital, who describes the condition of Child Q at birth. The mother had lost a total of over 1.8 litres in blood prior to giving birth via an emergency C-section. The baby was born in 'good condition for his gestational age'. Child Q was taken to the neonatal unit and there were 'no major concerns' for the mother or baby, taking into account the mother's blood loss.
2:14pm: Neonatal nurse Christopher Booth, in a statement, said he did not remember Child Q independently, but did so from looking at notes made at the time. He recalls Child Q was receiving CPAP, then taken off that breathing support during the day. Child Q was 'coping well, self ventilating in air'. He had an 'unremarkable shift' and had 'no concerns' for Child Q, before passing care to nurse Tanya Downes.
2:21pm: Nurse Tanya Downes has now been called to court to give evidence. She confirms that, at the time in June 2016, she was working as a nurse at the Countess of Chester Hospital at the neonatal unit, and worked the night shift on June 23-24. She says Child Q was in room 1 of the neonatal unit. She says when waiting for the handover, she was standing by room 2, she recalled a baby in an open-top cot. She looked in and saw a baby 'didn't look too clever' in terms of condition and perfusion. She recalls it was on the night of June 23, the night of the EU Referendum. She said she had got in early to get herself a cup of tea and get ready for the shift. Room 2 was 'quite busy' with staff. A female staff member with blonde hair was standing by the cot. She does not recall the name of the baby. She said she had 'never seen anything like that' on Child Q - they looked 'mottled, but not mottled - a darker kind of mottling'. She says she could see from the baby's chest upwards, the top part of the body. She says the nurse was 'just standing by the bottom of the cot'. She said this did not look unusual as there was a lot of activity in the room.
2:28pm: Ms Downes is asked to look at her nursing note from 10.02pm on June 23. Observations are recorded and Child Q is 'in air requiring no respiratory support'. The note adds 'Aspirated 2mls bile and blood flecked aspirate at 2130, awaiting paed review, stomach not bloated, bowel sounds in all four quadrants'. The feed of milk was stopped following the bile aspirate being recorded on June 23, Ms Downes tells the court, following consultation with the paediatrician. Nutrition was increased via TPN bags.
2:33pm: A milk feed of 0.5ml is made via the NG Tube at 2am. Minimal' aspirates are recorded at 1am and 2am. An observation chart records 'normal' heart rate, respirations and temperature for Child Q.
2:41pm: Benjamin Myers KC, for Letby's defence, says Ms Downes was working as a 'bank nurse' at the Countess of Chester Hospital on that night. Mr Myers asks about the incident in room 2 Ms Downes saw. Mr Myers says, according to Ms Downes, the nurse was wearing 'dark blue scrubs', which would be worn by senior nurses. Ms Downes agrees with Mr Myers that Child Q was one of a number of babies at the neonatal unit who appeared to have bowel problems. For the June 23 night shift, Mr Myers refers to the intensive care chart earlier that day, for '2ml light bile' aspirate recorded at 09.31am. Ms Downes said she was aware of that, but had no major concerns. A '2ml bile/blood' reading is made by nurse Downes at 2130. Mr Myers said Ms Downes had asked for a review by a paediatrician. Ms Downes says there was a concern as it was blood-flecked. The cause of it could be 'a number of things', but it was 'a warning sign'. Ms Downes agrees this led to enteral feeds being stopped.
2:44pm: Mr Myers asks about the 1.5ml aspirate at 4am on June 24. Ms Downes says it could be a mixture of milk and stomach acid. No blood is noted and a pH reading isn't made.
2:46pm: Ms Downes recalls Child Q was recalled to hospital following his discharge in July 2016, with 'gut problems'. Ms Downes recalls she treated him at the out-of-hours clinic.
2:47pm: The prosecution rise to clarify about the make-up of the blood-flecked aspirate for Child Q. Ms Downes explains the aspirate had the appearance of coffee granules.
2:49pm: That concludes Ms Downes's evidence.
Monday 3rd April 2023
Child Q
Nurse Samantha O'Brien - Unnamed doctor - Nurse Mary Griffith - Nurse Minna Lappalainen (shift leader)10:19am: I'm back at Manchester Crown Court this morning for the murder trial of nurse Lucy Letby. The jury will continue to hear evidence in relation to Child Q, who the Crown say Ms Letby attacked in June 2016. The premature baby boy was her final alleged victim
10:38am: First witness of the day is nurse Samantha O'Brien, who was working a nightshift on 24 into 25 June 2016. She was the designated nurse for Child Q on that shift
10:47am: From reviewing her notes, she tells the court that Child Q was 'stable' on the night of 24 June. The court has previously heard that the baby boy collapsed on the morning of 25 June and required breathing support
11:13am: A doctor, who cannot be named for legal reasons, is now in the witness box - she was working a night shift on 24 going into 25 June 2016
11:29am: Her clinical notes from that shift record that Child Q was 'very unsettled' into the early hours of 25 June - she said he was 'more unsettled than I would expect'. Her notes question whether he could be suffering from sepsis
11:40am: Nurse Mary Griffith, who was working a day shift on 25 June, is now in the witness box
11:54am: Nurse Griffith tells the court that on the morning of 25 June she was in nursery two. She was caring for another baby, when Ms Letby asked her to keep an eye on Child Q while she went to check on another child in her care in nursery one Minutes after Ms Letby left, Child Q's alarm sounded and Nurse Griffith attended him with another nurse - soon after doctors were called onto the unit, as Child Q needed breathing support
12:24pm: Nurse Minna Lappalainen is now in the witness box. She assisted Nurse Griffith when Child Q collapsed. She tells the court she turned Child Q on his side, gave breathing support and suction (as he had vomited) Nursing notes, written in retrospect, stated that Child Q was 'mottled' in appearance
Chester Standard article 03-04-2023
ALARMS sounded at a baby’s cot shortly after nurse Lucy Letby left the room, her murder trial has heard.
Letby, 33, is alleged to have attacked the infant – allegedly her 17th and final victim – by injecting air into his stomach.
Nursing staff, including Letby, and doctors rushed into nursery two at the Countess of Chester Hospital’s neonatal unit to attend to the baby boy, who went on to recover from the incident just after 9am on June 25, 2016.
The Crown alleges that Letby had attempted to murder the youngster, Child Q, and that it was the culmination of a three-day attack spree in which she murdered two triplet brothers on the previous two days.
Giving evidence at Manchester Crown Court on Monday, April 3, during the 23rd week of the trial before a jury, nurse Mary Griffith said Letby had asked if she could keep an eye on Child Q while she went to check on another baby in a different nursery.
Mrs Griffith said she had started feeding the baby in her care when she heard an alarm go off at Child Q’s incubator.
She told the court: "I looked over my shoulder and I noticed his saturations had dropped."
She said she called for help from nursing shift leader Minna Lappalainen, who was at the nursing desk station opposite.
Mrs Griffith said the passage of time between Letby leaving and the alarm sounding was "minutes" but she could not say exactly how many.
Asked what she saw when she was first to arrive at the incubator, Ms Lappalainen said: "He had been sick. I turned him on his side and made sure his airway was alright."
She had noted clear mucous coming from the baby’s mouth and nose which was suctioned clean.
Asked why she recorded "clear fluid +++", she said: "The clear fluid means the mucous I’m cleaning. There is no feed in it, no milk in it. It’s like saliva."
A face mask was then used on Child Q to help pick up his blood oxygen levels, the court heard, and an emergency call was put out for a registrar to attend.
Ms Lappalainen also recorded Child Q’s nasogastric tube was used to aspirate his stomach by "Nurse L Letby".
The court heard the defendant made a separate note of "air++ aspirated from tube".
Ms Lappalainen said, according to her notes, Child Q recovered from the episode – which lasted three minutes "intermittently".
She said she was not aware of any further incident on the day shift involving Child Q.
The court heard Child Q was moved to intensive care nursery one after the incident and Ms Lappalainen took over the care of Letby’s second designated baby.
Nick Johnson KC pointed out an unsigned observation chart entry for this baby was made at 8.30am.
He asked Ms Lappalainen: "If this child had observations at 8.30am, would you expect the child to be observed at 9am?"
The witness replied: "Not necessarily if the patient is stable."
Ms Lappalainen agreed with Ben Myers KC, defending, that Child Q stabilised "relatively quickly".
Mr Myers said: "And the doctors were called because this was an appropriate thing to do?"
"Yes," said the witness.
Mr Myers went on: "It was not the type of incident where you were overly concerned."
Ms Lappalainen said: "I was not overly concerned but I wanted him to be checked out."
She said it was "perfectly acceptable" for nurses to ask a colleague to keep an eye on a baby if they had to leave a nursery.
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Tuesday 4th April 2023 - no court (juror ill)
Wednesday 5th April 2023
Child Q
Dr A - Dr John Gibbs - Dr Dewi Evans10:42am: Lucy Letby's murder trial continues at Manchester Crown Court this morning (couldn't sit yesterday due to a juror illness). We'll be hearing evidence in relation to Child Q, who the Crown say Ms Letby attacked in late June 2016. The nurse denies all charges
10:43am: Ms Letby is accused of attempting to murder the infant on 25 June 2016 after allegedly murdering two triplets, Child O and P, on the previous two days. First in the witness box today is a doctor, who can't be named for legal reasons. He worked the 25 June day shift
10:46am: The medic was called to the neonatal unit shortly after 9am to treat Child Q after he vomited and needed breathing support. The court previously heard that Ms Letby was Child Q's designated nurse that day. Ms Letby was caring for another baby when Child Q desaturated
11:02am: The doctor's notes record that after an hour Child Q's sats had improved and was no longer needing as intensive breathing support
11:15am: His notes from that morning state 'presumed sepsis with secondary jaundice' for the cause of Child Q's collapse
11:22am: Child Q made a reasonable recovery through the day, but by 19:20 he was described as 'looking tired' and the doctor took the decision to intubate him and place on a ventilator
11:36am: The following day, Child Q's gases were unsatisfactory and it was suspected that he had necrotising enterocolitis (a serious condition that can affect newborns). He was transferred to Alder Hey where he quickly stabilised - his breathing tube was removed on 27 June
11:44am: Ms Letby's defence lawyer, Ben Myers KC, is now questioning the doctor. He points out that the medic arrived on neonatal unit at 09:17 (Child Q crashed just after 9am). Myers says 'a fair amount of activity had happened already at that point', the doctor agrees
11:47am: He also agrees that Child Q had a 'rapid' recovery from the collapse.
12:19pm: Mr Myers has just asked the doctor to explain to the court, in simple terms, what NEC is and what impact it has on babies
12:39pm: Mr Myers is taking the doctor over messages he sent to Ms Letby in late June/early July in regards to Child O - one of the triplet brothers who died. The court has previously heard that the boy was found with an 'impact' injury to his liver in post-mortem
12:41pm: In the messages, the doctor tells Ms Letby that another doctor on the unit was concerned that Child O's liver injury 'may have been caused by her chest compressions'
12:42pm: He says in those messages to Ms Letby that he spent '20mins in a cubicle going over everything' with the doctor, he says 'CPR was all at fifth rib space between the nipples'
12:43pm: But he says to Mr Myers that he does not have any independent recollection of that resuscitation and that he was managing the airway during it
12:44pm: The defence have previously argued that the liver injury sustained by Child O was a result of CPR - this is something that was rejected by expert pathologist Dr Andreas Marnerides, who reviewed the case, last week
1:57pm: We're back after lunch. Consultant paediatrician Dr John Gibbs is up in the witness box next. The court has previously heard that after the deaths of triplet brothers Child O and P on the 23 and 24 June, Dr Gibbs had become 'concerned' about Ms Letby's presence on the unit.
2:33pm: Dr Gibbs is asked about a message, Ms Letby sent to a doctor - who cannot be named - on the night of 25 June. Letby asks if she should be 'worried' about what Dr Gibbs had been asking nurses on the unit that day From his recollection, Dr Gibbs tells the court he was asking nurses who was caring for Child Q at the time of his collapse as he had become increasingly concerned about unusual collapses and deaths on the unit. He said he would not normally ask who was looking after a child
2:52pm: Medical expert Dr Dewi Evans, who was asked to review the case by Cheshire Police in 2017, is now in the witness box
3:31pm: Dr Evans has said that he believes Child Q's collapse on the morning of 25 June was a result of air and liquid - possibly saline or water - being injected via the NG tube into his stomach. This he says caused Child Q's breathing problems, as it splinted diaphragm
Chester Standard article 05-04-2023
A BABY boy allegedly attacked by a nurse had a clear liquid forced down his throat which caused him to vomit, a court has heard.
The Crown alleges Lucy Letby, 33, harmed the youngster in the culmination of a three-day attack spree at the Countess of Chester Hospital after she murdered two triplet brothers.
It is alleged Letby murdered seven babies and attempted to murder 10 others on various dates between June 2015 and June 2016.
Giving evidence on Wednesday, April 5, expert medical witness Dr Dewi Evans said he believed water or saline, possibly together with air, was put down Child Q's stomach via a nasogastric tube (NGT).
The trial at Manchester Crown Court has heard the infant vomited clear liquid shortly after 9am on June 25, 2016.
His heart rate fell and his blood oxygen levels also plunged before he recovered "relatively rapidly" after he received breathing support from neonatal staff.
Dr Evans told the court that Child Q was "not quite well" from the night before and was apparently unable to tolerate small feeds of milk.
But he said the feeding problem would not explain the "very significant" deterioration.
Dr Evans said: "I think we are dealing with two separate incidents."
Medics later suspected that Child Q may have a bowel disorder common to premature babies, the court heard.
The youngster was transferred to intensive care at Alder Hey Children's Hospital but surgeons there found no further issues and he was returned to the Countess two days later.
Prosecutor Nick Johnson KC asked Dr Evans: "If a significant quantity of clear fluid was vomited, what view did you come to?"
The retired consultant paediatrician said: "There was enough clear fluid injected down into his stomach to make him vomit.
"He was unable to breathe properly because his tummy was full of liquid."
Dr Evans said that "air++" was noted to have been emptied from Child Q's stomach after he received breathing support from a Neopuff face mask but he said "very little" of the latter was taking place.
He went on: "So it could well be as well as having clear fluid down his NGT he had some air injected into his stomach as well."
Dr Evans said he was "certain" that the suspected bowel problem, necrotising enterocolitis (NEC), was not a factor in the vomiting incident.
Ben Myers KC, defending, pointed out to Dr Evans that in three earlier reports he had concluded that the deterioration was due to "inappropriate care" with "a lot of air" given via his NGT.
Mr Myers said: "I am going to suggest that fluid is something you have added at a late stage."
Dr Evans replied: "I think in all these cases I have said in evidence, on a number of occasions, that I had to rely on notes that I have been presented with, and the more accurate the information we get, the more accurate the opinion is."
Mr Myers said: "What you are focusing on at that point exclusively is air. Now you have reached this point where you have added fluid now to keep the mechanism going, keep the allegation going, rather than reflect the facts?"
Dr Evans said: "No, no, no. You have got it wrong again.
"We are here now and we have heard the evidence from the people who were looking after him.
"So going on about what I wrote in 2017 and 2018 is rather missing the point."
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
A premature baby boy collapsed and needed breathing support after fluid and air was "forced" into his stomach, a court has heard.
Nurse Lucy Letby is accused of attempting to murder Child Q on 25 June 2016 and murdering two triplets, Child O and P, on the previous two days.
She is accused of murdering seven babies and attempting to murder 10 others at the Countess of Chester Hospital between 2015 and 2016.
The 33-year-old denies all charges.
Manchester Crown Court has heard how Child Q, who was Ms Letby's final alleged victim, was "stable" on the evening before his collapse.
Jurors heard the infant deteriorated and needed breathing support shortly after 09:00 BST on 25 June.
The Crown said Ms Letby injected air and fluid into the boy's stomach via a nasogastric tube in an attempt to kill him.
Medical expert Dr Dewi Evans, who was asked to review the case by Cheshire Police in 2017, told jurors vomit found on Child Q on the morning of 25 June was evidence liquid had been given to him by someone.
He said: "Clearly there was enough fluid injected down his nasogastric tube into his stomach to make him vomit, he only would have vomited if he had quite a significant amount of fluid."
He agreed with prosecutors the fluid had been "forced" down the tube.
Dr Evans said the subsequent respiratory problems experienced by Child Q was likely caused by the fluid, which placed pressure on his diaphragm and prevented him from breathing normally.
"Once he vomited, it was nature's way of un-splinting the diaphragm and easier for the resuscitation to be successful".
The court earlier heard from consultant paediatrician Dr John Gibbs, who told jurors how he demanded to know who was caring for Child Q after his collapse.
Dr Gibbs said that by late June 2016 there was a "heighted concern" about baby deaths at the hospital.
"I remember wanting to know who had been looking after [Child Q] at time he had desaturated," he said.
"I wouldn't normally want to know who was looking after patients.
"I was worried about what was happening on the unit," he added.
Dr Gibbs has previously told jurors between June 2015 and June 2016 Ms Letby's presence had been noted as a "common factor" in "unusual" baby collapses and deaths at the Countess of Chester Hopsital.
The consultant said the deaths of triplet brothers, Child O and P, on successive days in late June 2016 became a "tipping point" for his team.
Ben Myers KC, defending, earlier questioned a doctor, who cannot be named for legal reasons, about messages he sent to Ms Letby in late June 2016 in relation to the death of Child O.
The court has previously heard the boy was found to have an "impact" injury to his liver in a post-mortem examination that was akin to having been in a road traffic collision.
In Facebook messages to the nurse, originally of Hereford, he said that another doctor on the unit had told him she was "upset" and concerned that Child O's liver injury "may have been caused by her chest compressions".
He told Ms Letby he spent 20 minutes "in a cubicle going over everything" with the doctor.
The doctor told Mr Myers it was a "busy time on unit" and "a lot of introspection" was occurring.
He said he wanted to "reassure" the doctor the correct CPR procedure had been followed, but when pressed by Mr Myers as to whether he could remember the CPR he said "I don't".
"I think I was managing the airway and at some point changed positions, I don't recall who was doing what. I was focusing on the task in hand," he said.
Thursday 6th April 2023
Child Q
Dr Sandie Bohin - Police analyst: Texts & messages10:17am: Lucy Letby's murder trial continues at Manchester Crown Court this morning. We'll be hearing evidence from a medical expert in relation to Child Q, Ms Letby's final alleged victim. The nurse denies all charges against her.
10:37am: Medical expert Dr Sandie Bohin is now in the witness box. She was asked to review the findings of Dr Dewi Evans - who reviewed all the cases on instruction from Cheshire Police in 2017
11:08am: Prosecutor Nick Johnson KC asks Dr Bohin if there could be a natural/obvious explanation for 'clear fluid' being aspirated from Child Q on the morning of 25 June (soon after the baby boy collapsed and required resuscitation)
11:10am: She says: 'No, I don’t know where plus plus plus of clear fluid (as written on nursing note) comes from given at that time he had not had any feed since 2hrs previously, only a very tiny amount of milk..' She added: 'What was aspirated here was clear fluid not milk, I can’t explain where it would have come from'. She concludes that liquid/air was forced down his NG tube
11:15am: Ben Myers KC, defending, is now cross examining Dr Bohin. He references evidence from a nurse, who cannot be named, who said she saw mucous at Child Q's mouth, he puts it to her that this could be clear liquid referred to and asks if it was could it cause breathing difficulty She says it is unlikely it would be mucous, but says if it was, in that volume, it could cause issues
11:45am: Nick Johnson KC has just read a summary of Ms Letby's police interview in relation to the collapse of Child Q. In this she denied doing anything to harm the baby boy and said it was a 'coincidence he became unwell when she came on duty'
12:03pm: The jury is now being shown text/facebook messages from 26 June onwards between Ms Letby and colleagues (in relation to Child Q)
12:09pm: In messages to a colleague on 27 June, Ms Letby complains that the neonatal unit is 'way over capacity', she says the 'unit needs properly assessing, I don’t think equipment gets cleaned properly….we haven’t got space to maintain hygiene'
12:12pm: We've just been shown messages between Ms Letby and a colleague were she says she is 'worried' after being asked by a senior nurse not to come in for her night shift and that she would be on days from now on
12:13pm: She said to one colleague it was 'worrying in case they think I missed something or whatever'. She says the fact she had a call late on 27 June was 'messing with her head' and making her worry - in responses, two of her colleagues are reassuring her
12:17pm: Ms Letby tells a colleague that the call from a senior nurse telling her not to come in had sent her into a 'meltdown' and that she was 'completely overwhelmed' with worry
12:32pm: We've seen an extensive number of messages between Ms Letby and a doctor who cannot be named for legal reasons in early July 2016. We're currently being shown an email that the doctor forwarded to Ms Letby on 6 July - it was addressed to him from Dr Stephen Brearey
12:33pm: The court has previously heard that it was Dr Brearey who had first raised concerns that Ms Letby was working when a number of babies at the hospital had crashed
12:34pm: The email from Dr B to the doctor is asking him to set out details of some of the collapses of babies. The doctor tells Ms Letby 'this email has to stay between us'
12:37pm: Court now being shown an email, sent by a senior nurse, to all staff. It states that there would be an external review and that for a period members of staff would have to be placed under clinical supervision - starting with Ms Letby The nurse said that it was 'not meant to be a blame or competency issue but a way forward to ensure our practice is safe'
12:38pm: Ms Letby says, in a message to a colleague, that she has made a 'timeline' of all the events over the last year adding: 'If they have nothing or minimal on me they’ll look silly'
3:27pm: Wrap of today’s evidence. Back April 17. Lucy Letby was given a role in a hospital's risk and patient safety office after doctors raised concerns over her alleged involvement in baby deaths 👇🏻
Chester Standard article 06-04-2023
LUCY LETBY messaged a nursing colleague: "If they have nothing or minimal on me they'll look silly" during a Countess of Chester Hospital investigation into unexplained baby deaths.
The trial at Manchester Crown Court saw the latest collection of messages recovered from Letby's phone, revealing relevant messages between June and September 2016.
Letby denies murdering seven babies and attempting to murder 10 others between June 2015 and June 2016.
The messages displayed to the court were after Child Q – the 17th and final baby in the case, chronologically – had suffered a collapse which could not be explained at the time.
'I'm worried I'm in trouble'
On June 27, 2016, Letby messaged a doctor colleague at 5.41pm: "Eirian [Lloyd Powell, neonatal unit manager] has just phoned telling me not to come in tonight & do days instead. I asked if there was a problem & she said No, just trying to protect me a bit & we can have a chat about it tomorrow but now I'm worried."
Letby also messaged a nursing colleague at the same time: "E just phoned telling me to do days this week and not Go in tonight as trying to protect me. 😔"
Neither of the colleagues can be named.
After the nursing colleague asked: "What's that mean?", Letby replied: "I don't know. Asked if there was a problem and she said No just trying to protect me as had a difficult run just before holidays, less people on nights etc and we can have a chat etc tomorrow.
"But Im worried Im in trouble or something."
The nurse colleague replied: "Don't worry, how can you be in trouble you haven't done anything wrong.
"Just very unfortunate."
Letby: "I know but worrying in case they think i missed something or whatever. Why leave it til now to ring."
The nurse colleague replied: "It is very late I agree. Maybe she's getting pressure from elsewhere?"
Letby: "She said it's busy so more support for me on days and can look at the paperwork bits etc. She was nice enough I just worry. This job messes with your head"
Letby later messaged the doctor: "I can't do this job if it's going to be like this. My head is a mess. Why is she ringing at this time. There must be a problem."
The doctor replied: "Lucy - you did nothing wrong at all. It is an odd time to ring, but you've had a rough few days and a good manager would realise that."
'Meltdown'
After the doctor messaged with further reassurance, Letby responded: "I can't talk about this now. Sorry, I just need a bit of time.
"Sorry, that was rude. Felt completely overwhelmed & panicked for a minute. We all worked tirelessly & did everything possible, i don't see how anyone can question that. E has always been very supportive.
"Im having a meltdown++ but think that's what I need to do."
Letby worked long day shifts from June 28-30 at the neonatal unit – her last days there.
On July 6, the doctor messaged Letby: "You need to keep this to yourself. The meeting this afternoon looked at everything with Baby O & Baby P from birth onwards. [NB. Name of Baby O and P redacted]
"We reviewed everything. Room / meds / medical reviews and actions. We looked at all documentation med & nur. If you've any doubt about how good you are at your job - stop now.
"The documentation was perfect, everybody commented about the appropriateness of your request for a review of Baby O following vomit. (name of baby O redacted). Your documentation of the resus / incubation / drugs was faultless.
"There is absolutely nothing for you to worry about. Please don't.
"There are going to be some recommendations based on staffing / kit but there was no criticism of either resus.
"This is staying quiet until has been to exec's. We're looking at [third triplet] care on Thur.
"E had nothing but good things to say about you."
Letby replied: "Ok......I Really appreciate you telling me - it won't go any further. I was one member of a huge team effort, but you know I've been carrying the worry of the 'what if I wasn't enough' - it's reassuring to hear that it doesn't appear that anything could have been done differently, or that I didn't act on or do something I should have. Thank you."
Letby is sent an email, made by Countess Dr Stephen Brearey, advising that the deaths of Child O and Child P were likely to result in an inquest, as the cause of both deaths was 'unexplained'.
Letby asked: "It's a bit of a worry if it's going that far. Do you think I'll be involved?" Letby is reassured: "Probably not."
The doctor added: "I know you won't say anything - this email has to stay between us, is that ok?"
On July 15, 2016, neonatal manager Eirian Lloyd Powell messages nursing staff advising them in preparation for "the external review", "all members of staff need to undertake a period of clinical supervision", acknowledging there are "staffing issues".
Lucy Letby is recorded as agreeing to undergo the supervision commencing from July 18.
The email adds: "I appreciate that this process may be an added stress factor in an already emotive environment, but we need to ensure that we can assure a safe environment, in addition to safeguarding not only our babies but our staff.
"This is not meant to be a blame or competency issue – but a way forward to ensure that our practice is safe."
The same day, Letby messages her nursing colleague: "I've done a timeline of this year."
'I haven't done anything wrong'
The colleague responds: "Fab. And how quite afew babies weren't compatable with life anyway. I wonder if midwives get this with amount of stillbirths......"
Letby: "Yeah and some went off within hours/on handover.
"Or were already acutely unwell when I took over.
"And put that when Baby Q went off No other staff able to care for him etc (name of Baby Q redacted)."
The colleague responds: "Not like all behaving fantastically till right into shift."
Letby: "Hoping to get as much info together as possible -if they have nothing or minimal on me they'll look silly, not Me."
On July 19, Letby began work in the patient experience team.
On August 8, Letby messages the nursing colleague: "Tony phoned. He's going to speak to Karen and insist on the review being no later than 1st week of Sept but said he definitely wouldn't advise pushing to get back to unit until it's taken place. Asked about social things and he said it's up to me but would advise not speaking with anyone in case any of them are involved with the review process. Thinks I should keep head down.and ride it out and can take further once over.
"Feel a bit like Im being shoved in a corner and.forgotten about by.the trust. It's my life and career.
"He's not been.given any information about the evidence he asked for.which is good. He's not sure what the external people.are going to look at in relation to me but we are in the process now.so have to ride it out"
The colleague responds: "Ok well just have to take his advice then suppose 😞"
Letby: "Still can't believe this has happened. It's making me feel like I should hide away by saying not speak to anyone and going on for months etc - I haven't done anything wrong."
The colleague responds: "Me neither! I know it's all so ridiculous."
Letby: "I can't see where it will all end"
The colleague responds: "I'm sure this time after xmas it'll all b a distant memory."
After Letby received an email announcing she had been seconded to the Risk & Patient Safety office for three months, she messaged the nursing colleague again, saying: "Bloody hell fuming. Im in email and makes it sound like my choice."
The timeline records Letby met with a review panel on September 1. On September 7, she registered a grievance procedure.
The trial, currently in its 23rd week before a jury, adjourns today (Thursday, April 6) for the Easter break, and is expected to resume on Monday, April 17.
7th April until 17th April 2023 - no court (Easter break)
Monday 17th April 2023
House search: post-it notes, diary, handover sheets - Police interviews re Child AChester Standard Live Reporting
10:38am: As previously arranged, the trial will have a later start for today. The jury will also not be sitting on Tuesday, April 18. The rest of the week is expected to proceed as normal sitting days.
10:40am: It is now more than six months since the jury first started hearing evidence in the Lucy Letby trial. Not counting the weeks where the court did not sit for Christmas and Easter, this is now the 24th week in which members of the jury will be hearing evidence.
11:53am: The trial is expected to resume from 12.15pm.
12:17pm: The court is now filling up, and Lucy Letby has arrived, as she has done for each day when the jury has been hearing evidence.
12:30pm: A 'technical issue' is delaying the resumption of the trial, we've been told. It could relate to the iPads the members of the jury and other users of the court have been using throughout this trial.
12:31pm: The trial is now resuming.
12:37pm: Agreed facts are now being read out to the court. Letby was arrested on three occasions, the court hears. The first was at 6am on July 3, 2018, at Letby's home address, the other two occasions when Letby had moved back with her parents in Hereford. In 2018, at Letby's home address, a police search was carried out, as was her parents' address, and Letby's workplace at the Countess of Chester Hospital in July 2018. Further searches took place in June 2019.
12:39pm: Agreed facts are evidence which has been agreed by both the prosecution and defence. Cheshire Police officer DC Collin Johnson has been called to give evidence, as exhibits officer in the Lucy Letby investigation. He is confirming what his role and duties are as an exhibits officer and the process of gathering exhibits.
12:42pm: The prosecution asks about the home searches in July 2018, and a "considerable number of exhibits" being recovered. Crime scene investigators took photos and recorded what they saw. A chronology of this part of the investigation is now taking place, firstly with Letby's home search at Westbourne Road, Chester, at 6.05am on July 3, 2018. The search ended on July 6 at 5.30pm.
12:46pm: A diagram of Letby's home is displayed to the court. Photos of Letby's home interior are now shown to the court. In her bedroom, the prosecutor points out, are two handbags, near the stand-alone mirror. Inside the handbag, three handwritten notes were uncovered.
12:55pm: The three handwritten notes are shown to the court. One is a blue post-it note, with handwriting featuring Letby's thoughts. The other two feature the name of a doctor several times, one saying "[name of doctor] I loved you" and "[name of doctor] my best friend." Other messages on the notes, which have been densely-packed and messages among swirls of writing, read: "I can't do this anymore"
"Help me"
"We tried our best and it wasn't enough"
"I want someone to help me but they can't" One message, in thicker handwriting overlaid on the yellow note, has the message "HELP".1:00pm: Another photo of Letby's bedroom is shown, with a wall slogan 'Leave Sparkles wherever you go'. The message is repeated on a small tabletop decoration. A page from Letby's 2016 diary is shown to the court, with a note on April 8: 'LD [long day] twins'. The following day is 'LD twins resus]. It is followed in a different coloured pen by 'Salsa - Buckley'. A page of June 20-26 from Letby's diary, has for June 23: 'LD ([name of Child O's initial])' June 24: 'LD ([name of Child P's initial) A+E' June 25: 'LD ([name of Child Q's initial)'
1:03pm: The diary also shows, on June 25, 'Salsa Mold', and for June 26 'Las Iguanas 1800'.
1:07pm: The post-it note, found inside the diary, is one which was shown in the first week of the trial. It has the message 'I am evil I did this' at its end. Also featured are the words 'Slander discrimination', 'I haven't done anything wrong', 'I can't breathe', 'All getting too much', 'I killed them on purpose because I'm not good enough' and 'I am a horrible evil person'.
1:08pm:
1:15pm: A very densely packed handwritten note is shown to the court, again in Letby's handwriting. The broken sentences feature medical terms, and the words 'debriefing' 'sterility', 'foreign objects', 'workforce', 'haemorrhage', 'non-availability', 'cellulite' 'aggravating factors', 'confidentiality', 'Don't know if I want to do this', 'Inadequate', 'Diagnosis', 'Implicating', 'Administration'. Several of the words are written multiple times. The first names of Countess staff are also written occasionally. A section which is scribbled and crossed out reads 'I don't know if I killed them maybe I did maybe this is all down to me'.
1:25pm: A photo of an Ibiza-emblazoned bag for life is shown to the court, recovered from Letby's bedroom. The contents of the bag feature a number of documents and Lucy Letby's NHS name badge 'registered children's nurse neonatal unit'. Nursing handover sheets for June 23 and June 24, 2016 are shown to the court. The names of babies not on the indictment have been blacked out for the court. They do include the names of Child O and Child P. Handwritten documents of medical information and observations for babies, including for Child O and Child P, are shown to the court. A nursing handover sheet for June 25 is also shown, with Child Q named. On the back of the sheet are handwritten notes and observations for Child Q and another baby.
1:28pm: A handover sheet for June 28, 2016 is shown which, the court hears, is outside the indictment period so no names of babies are shown to the court on this document. The court hears there is handwriting on the rear of this note, which mentions Child O, and again the document features medical observations and notes.
2:12pm: The trial will resume shortly, following a 45-minute lunch break.
2:18pm: The trial is now resuming. The trial judge is informing the jury there will be several days in the next few weeks which the jury will not be sitting. They include Tuesday and Friday this week. A full rundown will be provided at the end of the day.
2:21pm: Prosecutor Philip Astbury is continuing to ask questions about the exhibits found with DC Collin Johnson. A Morrisons bag for life was recovered from Letby's home, which included a blood gas printout and a paper towel with handwritten resuscitation notes for Child L.
2:39pm: Also in the Morrisons bag were a number of nursing handover neonatal unit notes - 31 in total. Most of the notes refer to babies which did not feature in the indictment, and included on 17 of the notes there are multiple references to 13 of the 17 babies in the indictment period.
2:42pm: The court is shown photos of other rooms in Letby's home. One room, which has a cartoon painted tree and wood animals on the wall, has a black paper shredder in the corner. Shredded paper was identified. Police investigators identified the documents as bank statements.
2:46pm: A floorplan of Letby's parents' home is shown to the court. A photo of Lucy Letby's bedroom at the Hereford address is shown to the court. A photo is shown inside Letby's wardrobe, and Mr Astbury asks about the 'Asda five-sheet strip cut paper shredder' - there was no shredder in the box, but inside were five nursing handover sheets, not related to the indictment. Handwriting on the box says 'keep'.
2:52pm: Letby's work address was also searched, between 10.15-11.50am on July 3, 2018. A blue folder of papers was recovered from a desk, containing 'various items of paperwork'. One sheet, an 'annual leave request', has a lot of handwriting by Letby on both sides of the paper. This includes hearts, 'Tigger + Smudge', 'I loved you but it wasn't enough' PLEASE HELP ME [name of doctor] LOVE PLEASE HELP ME [name of doctor] You were my best friend [name of doctor]' I just want to be as it was I want to be happy in the job that I loved....Really don't belong anywhere - I am a problem to those who do know me and it would be much easier for everyone if I just went away.' The names of a few Countess staff are named, repeatedly, as are the words 'malnutrition' and 'assessment'.
2:58pm: A photo of Letby's Westbourne Road home garage is shown. Inside the garage is a black bin liner, and inside was a further note seized by police. The note contains very densely packed handwriting. Notes include 'Appropriate workforce', 'Consultant', 'Countess of Chester Hospital' 'Equality and Diversity', 'No-one will ever know what happened and why + I am a failure' I can't recover from this' Keep this between ourselves', I don't think I can ever go back Too much has happened/changed' Insulin diabetes' Killing me softly' features at least twice. The words 'management' and 'ombudsman' feature about a dozen times on the sheet of paper. Cheshire place names also feature.
3:00pm: Benjamin Myers KC, for Letby's defence, says a total of 257 handover sheets were recovered in the police search. Of those, 21 related to babies in the indictment. Four of them were in the 'Ibiza bag' and 17 were in the Morrisons bag. DC Johnson agrees. Mr Myers says that meant 236 handover sheets were not in relation to the indictment.
3:02pm: DC Collin Johnson confirms four of the babies in relation to the indictment do not feature in any of the handover notes recovered at Letby's addresses.
3:32pm: That completes DC Johnson's evidence. The next stage of the trial will be evidence of police interviews with Lucy Letby after she was arrested. The court has previously heard summarised evidence read out at the end of each case during the trial.
3:36pm: The interview transcripts from the three times Lucy Letby was arrested will be read out to the court. These will be summarised from the original full-length footage of the interviews, which were fully transcribed. The summaries are agreed by both the prosecution and defence.
3:46pm: Prosecutor Philip Astbury and a Cheshire Police officer will be reading through the transcripts to the court. Letby recalls, in the first interview, the care she provided for Child A. She recalls Child A appeared 'quite pale and mottled' and required 'full resuscitation'. She remembered Child A, and going to his cotside. He appeared 'a bit jittery' - 'making involuntary jerking movements', 'can be a sign of low blood sugar'. "It's common for pre-term babies." She said staff were conscious to get Child A fluids. At the time of fluid administration of the time of the shift handover, there were "no concerns". She was with nurse Melanie Taylor. Child A had gone a few hours without fluids, which was "not ideal". She said after the fluids were connected, Child A's "colour changed".
3:50pm: Letby said she did not recall having physical contact with Child A at that point, until after he deteriorated. It was 'within maybe five minutes' of the TPN bag being administered that Child A became 'pale and mottled'. He had become 'pale, almost white', and said there was 'something wrong' - Child A could have had a 'sudden collapse'. The mottled appearance 'could be a sign of low blood sugars', where a baby could be pale but have 'reddy-purple' patches. Child A was 'pale' in the centre and the mottling was on the 'hands and feet.' Child A was not breathing.
3:54pm: Letby said she went to observe Child A and saw he 'was not breathing'. Dr David Harkness was also in the room, Letby said, as was nurse Melanie Taylor. Dr Harkness was called over. Asked to describe the rash, Letby says she thinks it was 'on the side the line was in', on the left side, but there was 'predominantly paleness'. The advice was to 'stop the fluids immediately' as there may have been an issue with the long line for Child A.
4:01pm: Letby says there was 'no reason' why Child A's perfusion was very poor. Letby said it was 'awful' that Child A had passed away, and twin Child B was present when this was 'all happening'. I think just all of us, as a team, dealed with it', and a formal debrief was held a few days later. Letby says there was nothing in particular from the outcome, although one possibility was health issues the mother had. Letby said she had seen babies pass away before, from her time working in Liverpool Women's Hospital involving very pre-term babies, but Child A's death was 'unexpected'.
4:04pm: Letby says she believed Melanie Taylor would have connected the TPN bag, as she was sterile (and in a position to attach the bag). She tells police there may have been uncertainty over what the bag of fluid contained. She says she and Melanie Taylor would have checked the TPN bag together prior to administration.
4:08pm: Letby says she had about 20 minutes in contact with Child A in total.
4:09pm: Letby told police there may have been an issue with the line, and/or the fluid attached from the TPN bag - whether it had contained the correct prescription.
4:11pm: The trial judge, Mr Justice James Goss, tells the jury the sitting days over the next two weeks will be Wednesday and Thursday of this week, and Tuesday, Thursday and Friday of next week.
Tuesday 18th April 2023 - no court (planned)
Wednesday 19th April 2023 - no court (juror ill)
Thursday 20th April 2023
Professor Arthurs (Child Q) - Police interviews re Child A-H10:34am: I'm back at Manchester Crown Court this morning for the trial of nurse Lucy Letby, we're first hearing from medical expert witness Dr Owen Arthurs - he is back in to give evidence on Child Q (he couldn't appear before Easter to do this)
10:35am: Ms Letby is accused of attempting to murder Child Q on 25 June 2016 after allegedly murdering two triplets, Child O and P, on the previous two days. The 33-year-old denies all charges.
10:36am: Manchester Crown Court has previously heard how Child Q, who was Ms Letby's final alleged victim, was 'stable' on the evening before his collapse. Jurors have heard that the infant deteriorated and needed breathing support shortly after 09:00 on 25 June. The Crown say Ms Letby injected air and fluid into the boy's stomach via a nasogastric tube in an attempt to kill him.
10:39am: Dr Arthurs was asked by Cheshire Police to review a number of radiographs for Child Q. He tells the court that on one of the radiographs, taken 20hours after the baby boy's collapse, he noticed an 'abnormality'
10:46am: Dr Arthurs is talking the jury through the radiograph, he points out two areas in the bowel of Child Q - he says it could be a sign of pneumatosis, which is an early sign of necrotizing enterocolitis (a serious condition in newborns)
11:06am: Jury are now being read summaries of Ms Letby's police interviews in relation to Child A. Cheshire Police detective Danielle Stonier is reading Ms Letby's responses, while prosecutor Philip Astbury is reading the questions asked
11:09am: In that interview, Ms Letby was told about the expert opinion of Dr Dewi Evans that Child A had been injected with air - her response was 'I did not deliberately give him any air'
11:10am: She was told about the expert opinion of Dr Owen Arthurs, who noticed air on radiographs of Child A - she was asked if she could explain how the air got there, she said 'no I can’t explain how that air got there'
11:11am: We're now moving onto Ms Letby's interview in relation to Child A's twin sister, Child B. The Crown say Ms Letby attempted to murder the infant in June 2015
11:25am: Ms Letby was asked in her interview her recollections of Child B, she recalled seeing the baby girl with a 'sort of purply red rash' and looking mottled. She didn't recall in that interview what she did after seeing the rash (she wasn't Child B's designated nurse)
11:34am: Asked if she had an explanation for Child B's collapse she said 'No, there's no explanation' She added: 'I didn’t do anything deliberately to (Child B) to harm her' Asked if she was responsible for attempted murder, she said 'no'
11:37am: We're now onto the summary of the interview in relation to Child C - a premature baby boy, who weighed just 800grams on birth in early June 2015. Ms Letby is said to have caused baby's death by inserting air into the boy's stomach via a nasogastric tube.
11:52am: In her interview, Cheshire Police put it to Ms Letby that one of her nursing colleagues, Sophie Ellis, had told them that when she heard Child C's alarm and went in to nursery 1 to check on him, Ms Letby was already in there stood at his cotside
11:54am: At the time, Ms Letby was a designated nurse for another baby in nursery three. She was asked why she was in nursery one - she responded 'I don’t recall from memory' and said she may have been in N1 to carry out checks, use the computer or may have heard C's alarm
12:17pm: The court has heard that six minutes before Child C's collapse, Ms Letby was texting an off-duty colleague saying that she had wanted to be in N1 as it would be cathartic – would help her wellbeing - to see a living baby in the space previously occupied by Child A
12:18pm: Ms Letby agreed with the interviewing officer that she was 'frustrated' by the text conversation as she wasn't receiving the emotionally supportive messages she expected
12:19pm: The officer asked: 'Did you cause him to collapse six minutes after that conversation?' 'No', Ms Letby said
12:20pm: Ms Letby agreed that she was 'feeling frustrated and upset' at not being in N1 and with the text conversation, but denied attacking Child C
12:22pm: We're now moving onto the interview summary for Child D. The prosecution allege that the baby girl was the third child murdered by Ms Letby in a two-week period in June 2015
12:32pm: Ms Letby again told police in her interview that she 'did not deliberately do anything to harm (Child D)'
12:34pm: Police asked Ms Letby why she messaged a colleague after Child D's death saying ‘I think there is an element of fate involved. There is a reason for everything.’ Ms Letby said she was 'not sure' and said was just 'because sometimes things can’t be fully explained'
12:36pm: We're now onto interview summaries for Child E, a premature twin boy born in late July 2015. The court has heard that Child E lost 25% of his blood volume before his death in the early hours of 4 August. Medical expert Dr Dewi Evans has previously told the court that this could have been the result of an "inappropriate" use of a medical tool.
2:28pm: In those interviews Ms Letby again denied causing any harm. We've moved now to Child E's twin brother, Child F - who the Crown say Ms Letby allegedly poisoned with insulin
2:32pm: The Crown say the insulin was most likely added to the baby's Total Parenteral Nutrition (TPN) bag, which is used to intravenously provide feeds to infants. The investigating officer asked Ms Letby in her interview whether anything would be added to the bag - 'no, not that I’m aware of', she said
2:50pm: When asked whether she had added insulin to the infant's TPN bag she said 'no' and asked officers if the bags had been kept/checked after the incident - they had not
2:55pm: Ms Letby was asked by officers why she had carried out searches for the mother of Child E and F on Facebook. She said she did not remember carrying out the searches, but would have been to check to see how Child F was doing.
2:57pm: Ms Letby was asked if she was 'obsessed' with the family of E and F as five months after they had left the hospital, she was still searching on Facebook for the family - she said 'no'
3:20pm: We're now moving onto a summary of Ms Letby's interview in relation to Child G. At the start of that interview, the officer pointed out that there had been a 'spike' in baby deaths/collapses in June 2015. He noted Ms Letby had been involved in all the cases The officer said 'you dealt with all of these, what do you put that down to, bad luck?’ She said ‘yes’
3:50pm: We're now onto the interview summaries for Child H, Ms Letby is alleged to have caused the girl to collapse on successive shifts in the early hours of September 26 and 27, 2015
3:52pm: Asked by police if she did anything to harm Child H, she said: 'I didn’t do anything'
4:59pm: Court now adjourned, back on Tuesday.
Chester Standard article 20-04-2023
NURSE Lucy Letby agreed she was "upset and frustrated" six minutes before the collapse of a baby boy she allegedly murdered, her trial has heard.
Letby, 33, messaged a colleague during a night shift at the Countess of Chester Hospital about not being allocated to work in the neo-natal unit's intensive care room, jurors were told.
Five days earlier another baby boy – her alleged first victim, Child A – had died in intensive care room one.
On the evening of June 13, 2015, the court heard she texted a fellow nurse: "I just keep thinking about Mon(day). Feel like I need to be in 1 to overcome it but (nurse) said no x."
Her colleague, Jennifer Jones-Key said: "You need a full-on break from ICU. You have to let it go or it will eat you up."
Letby said: "I just feel I need to be in 1 to get the image out of my head. To be in 3 is eating me up. All I can see is him in 1.
"It probably sounds odd but it's how I feel."
Her colleague replied: "It sounds very odd and I would be complete opposite."
Letby responded: "Well that's how I feel… You don't expect people to understand but I know how I feel and how I have dealt with it before.
"I voiced that so can't do any more but people should respect that."
Letby went on to explain when working at Liverpool Women's Hospital she had "lost a baby one day and a few hours later was given another dying baby just by the same cot space".
At 11.09pm she texted her colleague: "Forget it… I'll overcome it myself. I'm obviously making more of it than I should x."
At 11.15pm the baby boy, Child C, suddenly deteriorated in room one, jurors have heard.
Medics failed to revive him and "token resuscitation" took place until the arrival of a Church of England vicar to baptise the youngster.
Child C was pronounced dead at 5.50am on June 14.
When interviewed by police about the death of Child C, the defendant said she did not recall the text conversation.
Asked what she felt she needed to overcome, she replied: "I'm assuming… I previously had a bad experience in (room) one."
Letby thought the image she "wanted out of my head" was that of Child A.
She told officers: "It's very difficult, when you see dead babies it's hard to get that image out of your head."
The detective asked: "Why would going into nursery one help?"
Letby replied: "Because I would see a different baby in there, and see a different scenario to the scenario I had at the time when he died."
The detective said: "How would it be a different scenario?"
Letby said: "It's a different baby, it's different staff, it's a different night.
"Because I think when you are going to the same incubator space and there is a different baby there you know you let the one you lost go. Until you go into that space, you see that baby until another baby goes in there."
The detective said: "You sent the final text at 11.09pm. Six minutes after you sent that (Child C) collapsed."
"Right," said Letby.
The detective went on: "What are you thoughts on that?"
Letby responded: "I don't have any thoughts on that."
The detective said: "The text messages suggest you were frustrated at not working in nursery one, do you agree?"
The defendant said: "Yes, I think it would have helped me if I could have been in nursery one."
Letby agreed she was the only staff member in room one when Child C collapsed and that she was seen at his cot-side when a monitor alarm sounded.
The detective asked: "And at that time you were feeling upset and frustrated?"
"Yes," said Letby.
The detective said: "You went on to attack (Child C)?"
Letby said: "No I haven't. No."
The detective said: "Lucy, did you murder (Child C)?"
"No," the defendant said.
The detective asked: "Can you give any explanation as to how (Child C) died?"
Letby replied: "No."
The defendant is accused of murdering Child A and Child C by injecting them with air.
She also allegedly attempted to murder Child A's twin sister, Child B.
Letby, originally from Hereford, denies the murders of seven babies and the attempted murders of 10 others between June 2015 and June 2016.
Friday 21st April 2023 - no court (planned)
Monday 24th April 2023 - no court (planned)
Tuesday 25th April 2023
Police interviews re Children I-P10:18am: I'll be bringing live coverage from Manchester Crown Court again this morning as the murder trial of Lucy Letby continues. We'll be hearing summaries of her police interviews (in 2018, 2019 and 2020) Last week we heard how officers asked the nurse if she thought her presence during the collapse of a number babies on the Countess of Chester's neonatal unit was just "bad luck" - she said "yes".
10:27am: In one interview a detective asked her: “What were you thinking during that period?” Letby replied: “That it was a shock to have that many deaths.” The detective said: “It must have been devastating.” “Yes,” replied Letby.
10:28am: Ms Letby denies murdering seven babies and attempting to murder 10 others between 2015 and 2016.
10:35am: We'll be hearing interviews in relation to Child I first today - a baby girl who Ms Letby allegedly murdered on 23 October 2015
10:44am: Cheshire Police detective Danielle Stonier is reading Ms Letby's responses, while prosecutor Philip Astbury is reading the questions asked. We're currently hearing about Child I's first (of four) collapses on 30 September. Ms Letby was the infant's designated nurse
10:46am: Ms Letby said she was not 'unduly concerned' about Child I at the start of her day shift. At around 15:00 Ms Letby noted that Child I appeared mottled in colour with a distended abdomen. At around 16:30 an emergency crash call went out as her heart rate had dropped
10:52am: Ms Letby told detectives she could not recall the specifics of this incident. She is then asked about the baby's second collapse on 12/13 October. Ms Letby recalls this incident, 'oh yes, this was when she was found apnoeic in her cot at night', she said
10:53am: She told detectives she and a nursing colleague found Child I 'gasping' for breath - she gave rescue breaths via neopuff and doctors were called to assist
10:59am: Asked about Child I's final and fatal collapse on 23 October 2015 - Ms Letby she can't recall the specifics of the night, but said she 'remembers her dying and her parents having time with her'
11:02am: Ms Letby said she wanted to attend Child I's funeral but she couldn't as she was working
11:04am: Ms Letby was asked about the below card she sent to the parents of Child I after her death, she told detectives she sent it as it was 'not very often you get to know a family as well as we did with child I'
11:10am: Detectives found the above image on Ms Letby's phone. She was asked why she took a pic of the card, she said it was 'upsetting losing (Child I) and I think it was nice to remember the kind words I shared with that family' She also said she 'often takes pictures of any cards I send even birthday cards'. She said this was the first and only card she had sent to a family of a baby she had treated
11:16am: Ms Letby is asked about the incident on 12/13 October. Her colleague Ashleigh Hudson told police that she saw Ms Letby was stood in the doorway of the nursery where Child I was in the early hours and commented that she looked pale. Nurse Hudson turned on the light and saw that Child I appeared at the point of dying and was not breathing. Detectives asked Ms Letby if she 'knew she was looking pale because you just attacked her?' 'No', Ms Letby said
11:19am: Detectives point out that Ms Letby had carried out Facebook searches for the family of Child I seven months after her death. She is asked why she did this, she told detectives she did not remember carrying out the searches
11:32am: We're now moving to interview summaries for Child K - a baby girl Ms Letby allegedly attempted to murder on 17 February 2016. It is claimed a doctor, Ravi Jayaram, walked in on Ms Letby as she attempted to kill her.
11:36am: Ms Letby told detectives that she had 'very little memory' of Child K, other than the fact she was a 25week prem baby
11:40am: In his evidence Dr Jayaram reported that when he arrived on the unit Child I's ET tube had slipped and her oxygen saturations were in 80s. Ms Letby was, according to the medic, stood near to the baby's ventilator
11:41am: Ms Letby denied dislodging the baby's ET tube and said if she had noticed the saturation levels she would have summoned help
12:00pm: We're now onto summaries for Child L, a twin boy who it is alleged Ms Letby attempted to murder on 9 April 2016. Asked if she 'inflicted any injury' on Child L she told police 'no'
12:14pm: The Crown say that Ms Letby gave Child L an unauthorised dose of insulin. In her interview Ms Letby is asked where insulin is kept on the unit and what the process for administering it to a patient is - she told officers it was kept in a fridge and it would have to be prescribed
12:15pm: Ms Letby explained that the insulin was in a locked fridge in the equipment room - the keys for which are passed around among neonatal nursing staff as and when they are needed
12:26pm: Detectives asked Ms Letby if she attempted to murder Child L by injecting him with insulin, she said 'no'. Asked if he could have been injected by mistake, she said 'I don’t really see how' and said it was 'unlikely' such a mistake could be made
12:27pm: Police put the expert evidence of Dr Dewi Evans to Ms Letby, that insulin had been administered - she said 'that wasn't done by me'
12:28pm: Ms Letby was asked if she had 'any explanation whatsoever' for how insulin ended up in his circulation. She said 'no, not unless it was already in one of the bags he was already receiving'. Asked if she added insulin to a bag, she said no
12:29pm: We're now moving onto interview summaries for Child M - Child L's twin brother - who the Crown say Ms Letby attempted to kill on the same day
12:30pm: The court has previously heard that Child M suffered an unexpected life-threatening collapse at around 16:00 hrs on 9 April 2016. His heart rate and breathing dropped dramatically and he required full resuscitation by medical staff.
12:37pm: Ms Letby told detectives she did not know why Child M desaturated. The only thing she could recall was that it was a 'busy shift' as it was 'not very often we had that many babies in nursery one'
12:38pm: Asked if she had caused the infants collapse, she said 'I didn’t cause that and I don’t know who would have'. She denied administering air in a bid to kill Child M
12:43pm: Ms Letby was asked about a paper towel found at her home address when it was searched in 2018. The towel was used in 2016 as a make do drugs chart for Child M during his resuscitation - police asked Ms Letby why this was in her possession and why was it in her home
12:44pm: Ms Letby said it was an 'error' on her part that it had been taken home. Asked why it had not been destroyed, she said it must have been put to one side and forgotten about. She denied keeping it to remind her of 'when she attacked' Child M
12:47pm: Among the items seized by police was also Ms Letby's diary, on 8 April 2016 is written: "LD [long day] twins". The following day is written: "LD twins resus" Ms Letby was asked why she had logged this - she said it was because it was a 'significant event'
12:48pm: We're now onto summaries for Child N - a baby boy it is claimed Ms Letby attempted to murder three times - once on 3 June 2016, and twice on 15 June 2016.
2:05pm: Jury back in after a short break for lunch - we're continuing with interview summaries for Child N
2:11pm: Manchester Crown Court has previously heard that in the early hours of 3 Ju, Child N experienced a "sudden deterioration" and was heard “screaming" and then crying for 30minutes
2:14pm: The court has also previously heard that on 15 June, Child N suffered further collapses and bleeding was noted at the back of his throat. The Crown allege that the bleed could have been the result of an "inflicted injury".
2:15pm: In her police interview, Ms Letby said she was 'not sure' why Child N was bleeding
2:20pm: Asked 'are you responsible for the attempted murder of (Child N)', Ms Letby said 'no'
2:35pm: We're now onto the summaries for Child O, a baby triplet who Ms Letby is alleged to have murdered on 23 June 2016.
2:38pm: Manchester Crown Court has previously heard how Child O was in good condition and stable up until the afternoon of 23 June when he suffered a "remarkable deterioration" and died
2:42pm: Ms Letby agreed when asked if Child O's death was 'unexpected'
2:45pm: She denied harming Child O. 'I did not physically injure (Child O)', she said
3:04pm: We're now onto the interview summary for Child P - Child O's triplet brother, who the Crown say was murdered by Ms Letby the day after Child O's death
3:16pm: Ms Letby said Child P's death was unexpected. She told police the parents had asked her to take pictures of the twins after their deaths top and tail in a Moses basket. 'If that’s what they wanted, I wanted to do it', she said
3:23pm: Police asked Ms Letby about a comment from nurse Kathryn Percival-Calderbank. She said Letby expressed that she was unhappy at being put in the outside nurseries. "She said it was boring and she didn't want to feed babies. She wanted to be in the intensive care." Ms Letby said 'I don’t recall calling my work boring in any capacity'
4:35pm: Court now adjourned. Back on Thursday.
Chester Standard article 25-04-2023
NURSE Lucy Letby photographed a sympathy card sent to the grieving parents of a baby girl to remember her "kind words", a court has heard.
Letby, 33, captured the image of the card on her mobile phone ahead of the youngster's funeral, Manchester Crown Court was told.
She is accused of murdering the prematurely-born infant, known as Child I, in the early hours of October 23, 2015, which the Crown say was the fourth attempt to take her life.
Letby is alleged to have murdered seven babies and attempted to murder 10 others at the Countess of Chester Hospital's neo-natal unit.
On Tuesday, April 25, excerpts of Letby's interviews by Cheshire Police following her arrest were read out at Manchester Crown Court.
Asked how she coped with the death of Child I, she replied: "It effects everybody on the unit because we all knew (Child I) quite well and we'd got to know the family.
"And then I wanted to go to (Child I's) funeral. I was unfortunately working at the time so didn't go."
Shown her photograph of the card, the officer asked: "Can you explain, Lucy, what that is?"
Letby said: "Yeah, I sent a sympathy card to the parents 'cos I wasn't able to attend the funeral."
The detective said: "OK, is this normal practice, Lucy?"
Letby replied: "No. Well, it's not very often that we would get to know a family as well as we did with (Child I)."
The detective said: "OK, is there a reason why you didn't go to the funeral?"
Letby said: "I was working. I wasn't able to change my shift. It was suggested that I could send a card via one of the other nurses who was going."
The detective asked: "Have you sent cards to other parents before, Lucy?
"No," she replied.
The detective went on: "That's the only one you have ever sent?"
Letby said: "Yes."
The detective asked: "Why did you take photographs of it on your phone?"
Letby said: "To remember what I had sent to them."
The detective said: "Why did you do that?"
Letby replied: "I often take pictures of any cards that I have sent, even birthday cards – anything like that. I often take pictures of them."
The detective said: "Did you forward these photographs on to anyone?"
Letby replied: "Not that I remember, no."
The detective said: "Why did you want to remember what you'd wrote to them, Lucy?"
She said: "It was upsetting losing (Child I) and I think it was nice to remember the kind words that I hoped I'd shared with that family.
"And as I say, I usually photograph any birthday cards that I send, anything like that. That's what I usually would do."
Letby wrote on the card: "There are no words to make this time any easier.
"It was a real priviledge (sic) to care for (Child I) and get to know you as a family – a family who always put (Child I) first and did everything possible for her.
"She will always be a part of your lives and we will never forget her.
"Thinking of you today and always – sorry I cannot be there to say goodbye.
"Lots of love Lucy x."
The card contained the printed message: "Your loved one will be remembered with many smiles."
Letby was also asked about two twin boys, Child L and M, whom she allegedly attempted to murder on April 9 2016.
A diary found at her then home in Westbourne Road, Chester, contained a reference to "LD twins" on an entry for April 8.
The detective asked: "LD?"
Letby replied: "Long day."
"Twins?" said the detective.
Letby said: "That there was a twin on the unit at that time."
The detective asked: "Does that relate to (Child L and M)?
Letby replied: "Was that the day when they were born? … Yes."
The detective said: "Is there a reason why you put that in your diary?"
Letby said: "Because I attended their delivery."
The defendant was then asked about entries for April 9 in which she wrote 'LD (extra) twins resus'.
She explained: "Because I have done an extra shift and I have documented what happened on that day."
The detective said: "To reflect on?"
Letby said: "Because that was a significant event on that day. It was an extra shift, it was my fourth long day in a row."
Jurors have heard a paper towel listing resuscitation drugs and the times they were given to Child M was also recovered from a search of Letby's address in July 2018.
Asked why this was in her possession, Letby said: "They have inadvertently come home with me on the night shift."
The detective asked: "Do you remember taking them home?"
"No," she replied.
Asked why she had not put the towel in the hospital's confidential waste, Letby said: "It was an error on my part that I have not emptied my pockets on leaving."
Letby said she said did not know why she had not destroyed the paper towel.
The detective asked: "Was this to remind you when you attacked (Child M)?"
She replied: "No. It was just put to one side and then forgotten about."
Letby denies all the alleged offences said to have taken place between June 2015 and June 2016.
Wednesday 26th April 2023 - no court (planned)
Thursday 27th April 2023
Police interviews re Child Q - Police interviews on other matters e.g. the notes, competencies & staffing, handover sheets, training - Eirian Powell - Other agreed factsChester Standard Live Reporting
9:10am: The trial is now in its 25th week before a jury. Today, the prosecution is expected to finish reading out police interviews which were carried out with Lucy Letby following her arrests.
10:30am: The courtroom in Manchester Crown Court has filled up with legal representatives, press and members of the public. Lucy Letby is, as has been the case throughout the trial, present. The judge, Mr Justice James Goss, has now arrived.
10:36am: Members of the jury have now come into court. There are, the judge tells the jury, "an unfortunate set of circumstances" which mean the next two weeks of the trial will only see the trial sitting for two days each.
10:40am: The read through the interviews continues with Child Q. Letby recalls the medical observations/procedures carried out at the neonatal unit. She recalls that Mary Griffith was the other nurse in room 2, and there was a concern Child Q had a low temperature, but was 'well enough to be left'. She recalls she had been in room 1, returned to room 2, and saw Child Q had had 'an intervention' and she recorded Child Q having a 'mottled' skin appearance.
10:44am: Letby said she believed she told Mary Griffith when she was leaving room 2. She recalls the other nurse was at the incubator. She said she came back from room 1 and saw there was at least one nurse treating Child Q when she returned, and there was administration of Neopuff by the other staff. She said she did not see Child Q vomit, but it would have been described to her. Letby said she was unsure why Child Q would have vomited. She says sometimes babies do vomit and that can lead to a desaturation. Letby tells police she does not recall if she aspirated Child Q. When asked about the excess air aspirated from his stomach, she suggested babies sometimes gulp air when they vomit.
10:47am: Letby says she believes she continued to look after Child Q as her designated baby following the desaturation. In a follow-up interview, Letby said she did not cause Child Q's collapse. She said she had taken observations and raised Child Q's incubator temperature. She said Child Q was "stable" before she left room 2. She denies being responsible for Child Q's collapse, or injecting air into Child Q.
10:52am: In a third police interview, Letby says she did not give Child Q anything prior to the collapse. She denies leaving the room so the blame for the collapse could be put on another member of nursing staff. Asked about a text message she sent to a doctor colleague about whether she should feel 'worried' about what Dr John Gibbs had been saying, Letby said: "I became aware of Dr Gibbs asking where I was - it was discussed then, obviously...I was concerned that I was going to be a problem" Asked if she was seeing reassurance from the doctor she had messaged, Letby agrees. She adds: "I wouldn't have just left a baby unattended," having said Mary Griffith was also in room 2.
11:02am: The interviews now move on to more general, 'overarching' questions including questions on exhibits found at Letby's address. Letby was asked about a post-it note: "I just wrote it as everything had gone on top of me."
"I felt people were blaming my practice...and made me feel guilty...they made me stop talking to people. "I was blaming myself, not for what I've done, but [for the way people were blaming me]." Asked about the underlined 'not good enough' note, Letby replies that was what people felt she was in terms of her competence. She says she did not know how to feel or what to do. "It just felt like it was all happening out of my control." Letby says she received some anti-depressants from her GP. She said she had been told she may have to redo her clinical care 'competencies' as part of the process, and she would not be the only member of nursing staff to do so. Letby said she had concerns over the raised mortality rate in the neonatal unit, saying there were more babies with more complex needs, and this was "unusual". After being removed from the unit in July 2016, she believed other staff felt she was not competent, and "they were going to think I had done something wrong", "that the police would get involved and I would lose my job". She added that she "loved her job". Asked about why she thought the police would get involved,
Letby replies: "I don't know, I just panicked." She said she thought she would be referred to the NMC - [the Nursing and Midwifery Council] - and they would refer it to the police. She said she felt 'so isolated and alone', as she could only speak to two friends, and had written a 'kill myself' note. She said she believed she had not done anything wrong, but was worried they would believe she was not good enough.11:16am: She said she believed the trust and consultants - Dr Ravi Jayaram and Dr Stephen Brearey - were blaming her in harming the babies. She felt she had had a good working relationship with the two consultants. She said: "They were trying to make it my problem, because I was there." She said she did not have any issues with the two consultants, and had a professional relationship with them. She had spoken to her 'best friend', a nursing colleague, about some of the issues, but not about the 'kill myself' feelings she had. Letby said she had been banned from contacting anyone, and the redeployment to another unit in the hospital 'would have gone on her record'. Letby said she had "lost everything", and had lost being part of a "good nursing team", who were "like a family". She said the note was a way of getting her feelings on paper, and this note was written "all in one session". Letby adds: "I didn't kill them on purpose." She said she was worried: "Other people would perceive me as evil if I had missed anything". "I felt so guilty that they [mum and dad] had to go through this." Asked about the 'kill them on purpose' note,
Letby replies: "I didn't kill them on purpose." Letby said at the time she felt there may have been practices and competencies in clinical care which she may have missed, which led to the deaths of babies. She said, having reviewed her practices, she did not feel she had failed on the competencies. She said she was the first member of her family to go to university, and her parents were disappointed she had been removed from the neonatal unit. She confirms she had told him. She said she was "career focused" and was worried that the investigation would lead to her losing her job and "change what people would think of me". Asked about the 'I AM EVIL I DID THIS' note: "That's how it all made me feel at the time...not intentionally, but I felt if my practice was not good enough, then it made me feel like an evil person..." She adds she 'wouldn't deserve to have children' on the basis she had been redeployed to another unit. She said the trust had redeployed her as they felt her competencies were an issue. She said she felt, at the time, she had caused the disappointments. She asked 'Why me' on the note as she wondered why she was the only one to undergo the redeployment.11:18am: Asked about 2016 as a whole, Letby said nursing staff morale fell during the year as the unit continued to have sick babies. "We were seeing more babies with complex needs and chest drains...stomas...quite a few extreme prematurity babies with congenital defects...we had the twins and the triplets."
11:22am: Letby says a lot of staff were "feeling the strain, physically and emotionally", and staff were not offered enough support, and there were issues with equipment availability on the unit. "I felt there wasn't a good management support structure...that was my personal opinion." She said the unit was "quite bottom heavy" with a lot of new starters, plus staff on sick leave. She says no staff intentionally gave poor care at the unit. Letby says while equipment availability was an issue, it was not the cause of any initial collapses of the babies. She said if staffing was "better" in terms of numbers, the care could have been better. Child Q was an instance, Letby says, where she was stretched between caring for babies in room 1 and 2. She says for one of the babies, it was "quite chaotic" when resuscitating.
11:24am: Letby said she was made aware in May 2016, formally, of the higher mortality rate among babies, and that was when she was moved to day shifts. She said she first noted it was unusual to have a high mortality rate on the unit in June 2015, when three babies died.
11:30am: Letby agrees she felt people's attitudes changed towards her when she was moved to day shifts in April 2016 and she felt she doubted her abilities. Letby is asked if she had taken any paperwork home in relation to the babies, Letby denies she has taken papers home, then adds: "I don't know - I might have taken some handover sheets accidentally. Not medical notes. "They [the handover sheets] might have been taken [home] in my pocket." Asked about another of the notes, which has the word 'HATE' in a circle in bold letters, Letby said she had just been removed from the job she loved and she had been prevented from talking to people. She said about the note: 'they thought I was doing it in purpose - not that I felt I did do it on purpose'. She adds: "I am very hard on myself...I felt as though I wasn't good enough." Police ask: "Lucy, were you responsible for the deaths of these babies?"
Letby: "No."11:36am: In a third overarching interview, Letby is asked about the handover sheets. She said, 'ideally', the handover sheets should be put in the confidential waste bin at the end of her shifts. She said that at times, they would come home with her. She is asked about 'a large quantity of handover sheets' at Letby's home address. She replies there was "no specific reason" why she had taken them home. She said she would have been aware she still had the handover sheets when she got home, and put them in a folder in the spare room. She said she "didn't know how to dispose of them" and no-one else had seen them. She said she would have seen those handover sheets at home "hardly ever". She said she did not have a shredder and those sheets were at home 'inadvertently'. Other paperwork at home would have been policy sheets from different hospitals, in relation on how to care when a patient presents with various symptoms.
11:41am: Letby said she 'had just not done anything' about the handover sheets when she got home. Asked about the mobile phone she used in 2015-2016, she said she would have used the phone at work, and not have let anyone else use it. There was one nursing colleague she would have contacted often, Letby says, using WhatsApp, FB Messenger and text messages. The messages would discuss patients, relaying information if they were unwell or had passed away. She said she had a "support network" and it was "helpful to speak to a colleague" in relation to babies. She added she would speak to her mum each day. She would not speak in as much detail if a baby had passed away to her, as she would to nursing colleagues, but would talk for support. Letby says she had reassurance from a doctor colleague, and was "close to him in the later stages".
11:47am: Letby said after a difficult day at work, she would 'seek reassurance', including a doctor colleague, and she would seek information about some debriefs when babies had died in which she had been involved in their care. Letby says she had started working on a neonatal unit in January 2012. She continued her training across a range of skills over the following years. In May 2015 there was a course for medicine administration via a bolus at the hospital, where - under supervision from a doctor - nurses would be able to administer medication via a long line. She said it was "different", and a "lot more risk", and said she was "competent" having done that training.
11:49am: Letby confirms she attended resuscitation training for infants, a course which is done every four years. She says there was no training she had failed, that she was aware of.
11:51am: Letby is asked about air embolism training. Letby says she did not have training for that, and was only aware of air embolisms in adults, after people had had a pulmonary embolism. Asked if air embolisms had been an issue in the neonatal unit, Letby replies it had not.
11:58am: The final overarching interview saw Letby identify her personal diaries, and confirmed only she wrote and had access to those diaries. Letby says she does not recall, in what way, why she had written the names of babies in her diary on particular dates. She said: "I just internalise things and think about them in my own time." She says she would have written them to note which babies she was looking after and how many babies she was the designated nurse for them. Asked about the 'kill me' note, she said she 'hated' working in the office and had 'lost everything'. She said, about on the of the notes, it had 'become a doodle thing', having started out as a note. Asked why she had kept the 'doodle note', she replies she was "not sure". Although undated, the note being in the 2016 diary meant the note could have been written after Letby had been redeployed away from the neonatal unit in July 2016. Letby agrees that would be the case.
12:04pm: Benjamin Myers KC, for Letby's defence, is now asking Cheshire Police detective Danielle Stonier, who has read out the interviews, a few questions. The detective confirms Letby and her legal representative, in advance of the interviews, would have received 'advanced disclosure', which would include a number of the documents police had, such as key nursing notes, feeding charts and observation charts "but not a detailed suite" of all the documents featured throughout the course of the trial. As an example, Letby had provided details of a particular shift for one of the babies, having had sight of relevant nursing documents for that child.
12:13pm: Mr Myers asks about one day when Letby asked for the interview to stop as she was tired. He says on that day, Letby had been asked about a large number of babies, in interviews spanning several hours.
12:32pm: The trial is now resuming after a short break. Eirian Powell, who was the neonatal unit ward manager at the Countess of Chester Hospital between 2011-2017, is being recalled to give evidence. Mr Myers has a few questions to ask Ms Powell.
12:34pm: Ms Powell first met Lucy Letby when the latter was a University of Chester student on a four-week placement. She agrees Letby was "very keen to improve her practice" and saw her to the point when she was working on the neonatal unit.
Mr Myers: "She was an exceptionally good nurse?" Ms Powell: "Yes, she was."12:38pm: Ms Powell confirms Letby was "committed" in progressing with her training, including training in intensive treatment units. She said Letby was 'hard-working and flexible' - "extraordinarily so", and worked a lot with premature babies in the neonatal unit. "She was very particular with attention to detail".
12:39pm: Mr Myers asks about the 2016 reallocation to day shifts, following a number of deaths on the neonatal unit. Ms Powell said the move to the day shift was to give Letby "more support" in staffing numbers, and was not "a punishment". Mr Myers said the unit remained busy during those days.
12:44pm: Mr Myers asks about the redeployment of Lucy Letby away from the neonatal unit in July 15, 2016, which was announced in an email signed by Ms Powell, as part of a period of clinical supervision. The email said 'This is not meant to be a blame or a competency issue', and was in preparation for an external review. Ms Powell confirms Lucy Letby was "upset" at being removed from the unit.
12:49pm: Ms Powell recalls the review meeting was "very upsetting" for Lucy Letby and herself. She does not recall if Lucy Letby was told not to talk to several other members of staff. "She was distraught at that point". Ms Powell said Letby was upset at what was said in the meeting, about what was suggested Letby may have done. Ms Powell said everyone's competency was being reviewed at that time, but "not to the extent" of Letby's. She adds she was "keen" to get Letby back on the unit.
12:51pm: Nicholas Johnson KC, for the prosecution, rises to ask a couple of questions. He asks if Letby made mistakes. Ms Powell said Letby made mistakes, as everyone did, but was "good at reporting mistakes", and would report mistakes that other nurse practitioners or medical staff had made, regardless of seniority.
12:54pm: Mr Johnson asks what was said in the review meeting. Ms Powell said that Letby would have to come off the unit, but could not recall what else was said. Mr Johnson asks what was being suggested in that meeting. "That she was the common [element] in all of the deaths".
12:55pm: The judge asks Mr Johnson if the prosecution case will end today. Mr Johnson replies that is the case.
2:27pm: The trial will resume shortly following an extended lunch break.
2:32pm: Members of the jury have now returned to the courtroom, and the trial is resuming.
2:34pm: The prosecution is now presenting some more 'agreed facts', that is evidence agreed by both the prosecution and defence. Philip Astbury, prosecuting, says this is in addition to agreed facts presented before.
2:40pm: The facts are that Letby was interviewed in police custody in Blacon, Chester, over a series of 13 interviews in July 3-5, 2018. Further interviews, a total of 14, were held in June 10-12, 2019. A further three interviews were held in November 10-11, 2020. The interviews were fully recorded with Letby having legal representation throughout.
2:57pm: Further agreed facts are now being read out. They include that an HTC One smartphone was seized from Letby's home address. The digital contents were extracted from it, featuring WhatsApp, text message and Facebook Messenger messages. Photos recovered included ones of a thank-you card taken from the parents of Child E and Child F. Child E had died but the parents thanked the nursing staff for being able to bring Child F home. There is also a photo of a sympathy card, with Letby's handwriting, for Child I, for the day of Child I's funeral.
2:59pm: A digital forensic investigator downloaded the contents of Letby's Facebook messages and emails, including Facebook search data.
3:05pm: A chart showing which members of the neonatal unit nursing staff were on duty for the shifts when the babies in this case collapsed is shown to the court. The chart covers the period from June 2015-June 2016. Lucy Letby's name is highlighted as being the only one present on all 24 shifts for when the babies collapsed. A second sheet shows which junior doctors and consultants were present for those events. This chart was shown during the prosecution opening in the first week of the trial.
3:08pm: A 'heat map' of total staffing presence says Letby was present for all 24 events. The next highest is consultant Dr John Gibbs, present at 10 events. Five nursing staff, and one doctor, were each present for seven of the events. The 'heat map' shows which of the other medical staff were present for six, five, four, three, two and one of the events.
3:11pm: The agreed facts now discuss how some photos and videos were taken as part of the investigation. They include one which represented a nursery room in low-level lighting, as part of evidence.
3:13pm: A competency assessment for administration via IV lines was also obtained. The competency checklist for Lucy Letby shows ticks for all 20 required boxes, and the candidate - Letby - is deemed to have passed. The assessment is dated May 31, 2015.
3:18pm: A blood transfusion workbook was also obtained from Lucy Letby's HR file at the Countess of Chester Hospital. One of the questions lists 'Give 4 potential complications of having a UAC/UVC line in situ'. Letby writes, for one of the four answers, 'air embolysm [sic]'. A transfusion competency assessment also has questions listed, which Letby has provided responses. The assessment is dated May 11, 2016.
3:20pm: It was agreed the handwritten notes seized from Letby's home included resuscitation notes for Child M.
3:24pm: Letby, the court hears, has no previous criminal convictions or cautions. The Countess of Chester Hospital Trust's neonatal unit was redesignated as a 'level one' unit on July 7, 2016. This was a decision taken by the trust.
3:25pm: That concludes the prosecution case, the court hears.
3:38pm: The jury has returned to the court following a short adjournment. The judge is informing them there is a "matter of law" which will be discussed in court tomorrow, so they will not be required. The jury will be expected to attend for Tuesday, May 2 - after the May 1 Bank Holiday. Next week is one of two, two-day weeks for the trial. The only sitting days are Tuesday and Friday. The following week, the trial is expected to sit on May 11-12. The following week after that is expected to be a normal, five-day week for the trial. The judge thanks the members of the jury for their patience.
Friday 28th April 2023 - no court (planned)
Monday 1st May 2023 - no court (bank holiday)
Tuesday 2nd May 2023
Direct Examination of Lucy Letby by Ben Myers KC - Day 1
Background and general topicsChester Standard Live Reporting
8:55am: After 25 weeks of evidence before a jury, the prosecution concluded its case against Lucy Letby last Thursday. Today, Letby's defence is expected to begin.
9:44am: A reminder that, due to availability difficulties and public holidays, the trial is only sitting on Tuesday and Friday this week.
10:21am: The courtroom at Manchester Crown Court is beginning to fill up. The trial is expected to resume at 10.30am.
10:23am: There are considerably more journalists in court to report today's events.
10:31am: The judge, Mr Justice James Goss, has entered court. Members of the jury are now arriving.
10:32am: Lucy Letby, wearing all black, is now giving evidence.
10:34am: Benjamin Myers KC asks Lucy Letby to confirm her full name and date of birth, which she does. She now tells the court about growing up in Hereford, with herself, her mum and her dad. She said she always wanted to work with children, and developed a preference for nursing towards the end of secondary school.
10:35am: She said she did a three-year programme of nursing at the University of Chester, splitting her time between the university '50:50' and placements to gain clinical experience. The majority of her clinical experience was at the Countess of Chester Hospital, split between the children's ward and the neonatal ward. She qualified as a band 5 nurse in September 2011.
10:37am: She says, during a 12-month period, she would've cared for "hundreds" of babies. Asked if she had done anything to harm the babies deliberately, she says that was not the case. "I only did my best to care for them." Asked further about it, she adds: "That is completely against everything a nurse is."
10:38am: Asked about how she felt about being removed from nursing duties, she says she was "devastated", having "prided myself on being competent". She says it "really affected" her, it was a "life-changing moment" in being put into a non-clinical role she did not enjoy. "From a self-confidence point of view, it made me question everything about myself."
10:40am: In September 2016, Letby says, she received a letter from the Royal College of Nursing about the "true reason" for her redeployment, that she was being held responsible for the deaths of babies on the neonatal unit. She says she was putting in a grievance procedure about being redeployed. She says she did not know, at that time, how many babies she was being held responsible for. She says she felt it was "sickening" to be held as a person responsible for the deaths of babies. "I don't think you can be accused of anything worse than that."
"I just changed as a person, my mental health deteriorated, I felt isolated...from my friends on the unit."10:43am: She said she was told not to have contact with anyone on the unit, other than three friends. Two were nurses, one was a doctor. She said she saw her GP, and she was diagnosed with depression and anxiety, and was placed on to anti-depressants. She says she takes medication for her depression now, as well as medication to help her sleep at night. She adds she cannot sleep without the medication.
10:44am: Becoming tearful, Letby says her job was "her life". She said, to have that taken away, "my whole world just stopped". She says the situation has "progressively got worse".
Mr Myers: "How hard is it to be what you're accused of?"
Letby: "It's very difficult."10:45am: Letby says "everything" has "completely changed" in the hopes in her life, and it had "all gone". Since November 2020, Letby says she has been remanded in prison.
10:49am: Mr Myers asks Letby about her being arrested for the first time. Letby says this was nothing like she had ever experienced before. Wiping away tears, Letby says there was a knocking on the door at 6am from police, at her Westbourne Road, Chester home. At the time, her father was with her. They had "no idea at all" the police were coming that day. "They told me I was being arrested for multiple counts of murder, they put me into handcuffs and took me away" in her pyjamas. After three days of police interviews, Letby was released on bail. She says she was not allowed to return to her Chester home, and went to live with her parents in Hereford. Becoming tearful, she says the second arrest in 2019 was a "mirror image" of the first arrest. "It was just the most...scariest thing I have ever been through."
"It's just traumatised me."10:50am: Mr Myers asks if the trauma has left Letby sensitive to certain things. Letby replies she is now sensitive to noises, and is "easily startled" by new things. She says she has been diagnosed, in prison by a psychologist, with PTSD.
10:51am: She says the journey to and from court, from prison, is about an hour and a half each way. Letby has been at court each day throughout the trial. She says she usually returns to prison at 7pm from court.
10:53am: Mr Myers asks about notes. Letby says, about her notes, "it's something I have done my whole life". She adds she has "difficulties" throwing things away, and that includes notes. Mr Myers asks about one of the notes she had written. Letby says she does not have a precise date of when she had written it - between July 2016 and July 2018. The note is headlined 'Not good enough'.
10:55am:
10:56am: Letby says she had written "I haven't done anything wrong" because she hadn't done anything wrong. She said in the "worst case scenario", the police would get involved. Re: 'slander and discrimination', she says that was how she felt the trust was towards her in regard to the allegations.
10:58am: re: 'I am an awful person...', Letby said at the time she did feel an awful person as she was worried she had made any mistakes. She said she was being taken away from the job she loved for things she had not done. She adds, at the time, she could not see a future for herself, in relation to 'I'll never children or marry'. She says "my whole situation felt hopeless, at times".
11:00am: Re: 'HATE' and 'Hate myself for what this has' - "At the time, I did hate myself". She says she was made to feel incompetent in some way. She says her mental health at the time of writing this note was "poor". She says it was "difficult", with the "isolation I felt", and this lasted "two years".
11:05am: Re: 'I killed them on purpose because I am not good enough to care for them, I am a horrible evil person'. Asked what she means by that note, Letby responds: "I [felt as though I] hadn't been good enough and in some way I had failed [in my duties, my competencies]...that was insinuated to me." Re: 'I AM EVIL I DID THIS' - "I felt at the time if I had done something wrong, I must have been an awful person..." Letby says she feared she may have been "incompetent" and because of that, she had "harmed those babies". She adds she could not understand "why this happened to me". She says, looking back, she was "really struggling" at the time of writing the note.
11:08am: Mr Myers says he will go through the background material for Letby first, then talk through the cases involving the babies. Letby is asked about the Countess of Chester Hospital, and working there. She says her first placement on the neonatal unit was in 2010. As a full-time qualified nurse, her first work there was in January 2012. At that time, she was qualified to care for special care and high dependency babies - 'predominantly in nursery rooms 3 and 4'.
11:09am: Asked about how much she valued her nursing work: "Massively, it was everything...and I always strived to go on every course, to be the best I could."
11:10am: Letby adds she completed a mentorship course so when students came in, she could be their sole mentor at work. She qualified as a mentor "fairly early on", 'probably in 2012.' She says she "really enjoyed that aspect".
11:13am: Mr Myers says for two of the babies in the case, there was a student being mentored, under Lucy Letby's supervision and guidance. Letby says it would depend on their training stage, but it would be under her direct supervision. Letby obtained her 'QIS' qualification allowing her to look after intensive care babies, following a university module, which included a placement at Liverpool Women's Hospital involving hands-on clinical experience. The six-month course concluded in March/April 2015.
11:18am: At the time, Letby and one other band 5 nurse had the QIS training. During June 2015-June 2016, another band 5 nurse acquired QIS training. Band 6 nurses all had QIS training. During a typical shift, Letby explains, there would be two band 6 nurses on duty, plus one band 5 nurse with QIS training. Letby says there would be "a lot of" intensive care babies on the unit, and Letby would be looking after them, having had the experience of looking after babies in a 'Level 3 centre' at Liverpool. The court has previously heard the Countess of Chester Hospital neonatal unit was level 2. Letby said she was "very flexible", and had been on hospital overnight accommodation prior to getting her house. She said she "did enjoy" the intensive care side, and she made other nurses aware that was her area of preference and where she was "most happy". She denies saying other areas of her work, in non-intensive care areas on the unit, were "boring". She does not recall ever having an argument with anyone about where she should be working.
11:20am: Mr Myers asks about the electronic system nurses used to take notes, which would be inputted on terminals in the unit. One would be in room 1, Letby explains, the others would be outside the rooms. Each staff had specific login details to input notes.
11:22am: Mr Myers asks about the notes being made retrospectively, usually at the end of a shift and can cover a period of several hours. Letby says, to remember what had happened through the course of a shift for a baby, her retrospective notes to be documented would be compiled from a mixture of documentation at the time and notes she had written on the back of her handover sheet.
11:25am: Mr Myers asks about an example, for one of Child I, a note written by Letby at 8.43am, at the end of Letby's shift. Letby explains she would have made notes on paper prior to writing them on the terminal, as a retrospective note, at the end of her shift. Letby explains there are nursing notes and family communication notes, which are separate. The former are clinical notes, the latter specifically for family.
11:27am: Asked about the notes, Letby says "ideally", they would be disposed of at the end of a shift in the confidential waste bin. Letby says she would normally store the handover sheets in her pocket, and as a result would take them home. The court has previously heard several handover notes were found at Letby's home at the time of her arrests. Asked about the timings of the notes made, Letby says they would be as accurate as they could be made, and the prescriptions would be accurate "to the minute". The nursing notes would be approximations.
11:30am: Mr Myers refers to an observation chart for Child O, with observations for heart rate, temperature and respirations. Letby explains how the readings would be taken. The routine observations would take "a couple of minutes".
11:36am: Letby adds that for each observation, "ideally" it would be signed off with the nurse's initials. In the "reality" of a busy shift, it "happens to everybody" that an initialled signature could be occasionally left off the bottom of the observation chart. The chart shown does not have initialled signatures for three of the readings. One is from a student nurse. Asked if that would indicate something "sinister", Letby says it would not. A second chart is shown, where there is a gap at 4am on an observation reading for the signature initials. None of the signatures are Letby's. Asked if there is anything "sinister or strange" about this, Letby says it is not. Mr Myers repeats this for an intensive care chart. Letby says there is nothing sinister about a lack of a signature for one of the readings.
11:40am: Mr Myers refers to an intensive care chart for Child Q. The final set of observations, at midnight, has no initialled signature. The signatures can be 'missed from time to time', the court hears.
11:54am: The court is currently having a short break. The judge, Mr Justice James Goss, has explained to the jury that as Lucy Letby will be giving evidence throughout a long day, the breaks will be slightly longer at 15 minutes. The break for lunch is expected to remain at its usual time of 1pm.
11:56am: The trial is now resuming.
12:00pm: Mr Myers asks about feeding babies at the neonatal unit. Lucy Letby explains the process of administering milk, saying you would "aspirate the NG Tube first" and testing the acidity of the contents of the stomach. Asked if that is a process done every time, Letby responds: "No." The process of feeding a couple of millilitres would take "only a few minutes". For larger babies, it would again be done by gravity feeding, but a dose of 40mls [as an example] would take "10-15 minutes". The process would be via 10ml syringes so the baby would be fed 10mls at a time. As a lot of the babies were premature, the process of feeding would take longer, and for a 40ml bottle feed, the process would take about 'half an hour'.
12:04pm: Mr Myers asks about blood gas tests for babies. A blood gas test result for Child Q is shown to the court. Lucy Letby explains the process on how a blood gas test is obtained, causing a prick on to the heel and getting the blood sample into "a very small tube". A second member of staff would run the sample through a machine outside of the nursery rooms, to obtain the result. "It would usually be a different member of staff" as the first nurse would stay with the baby to check the bleeding stops. The blood gas machine would be "down the corridor from room 1". Occasionally, if the machine was broken, an alternative machine on the labour ward would be used.
12:12pm: Mr Myers refers to the neonatal review for Child B. This was a document compiled by police which compiled which nursing staff did what for each baby. They include dates and times for observations, prescriptions and feeds. Lucy Letby says the times are approximate to the nearest quarter of an hour, such as 'weaning change'. A note at 9.30pm of a feed given and an observation would be an approximate time for both. The court hears it is not a precision time for both, as those are two separate activities carried out by the same nurse. Asked about the time between these charts, Lucy Letby explains nursing staff would be busy elsewhere, communicating with families, responding to alarms and other duties, in addition to set tasks as designated by the shift leader.
12:16pm: The chart goes into the times of which nursing staff carried out what for Child B up to the point of Child B's collapse. Mr Myers refers to prescriptions for Child B. Lucy Letby explains two nurses would be required for the signatures of prescriptions. Mr Myers asks about June 2015-June 2016. Letby says the time was "much busier" than previous years. "We seemed to have babies with a lot more complex needs." Letby says staffing levels were not changed to accommodate for this.
12:19pm: Letby says they had not encountered a baby on that unit before with chest drains requirements, or stomas, or haemophilia, as they did during June 2015-June 2016. Letby says she would, "quite often", do more shifts as overtime, after being asked to do so, than her typical monthly quota. She says "at times it could be very short notice", sometimes from lunchtime and being asked to cover that night. She says she would not know in advance which babies she would be caring for. Mr Myers asks if it's possible to ask for a particular baby to care for. Letby says it's possible, usually to facilitate continuity of care.
12:22pm: Between June 2015-June 2016, Letby was "generally well" and did not have any sick days off. The court hears Letby had optic neuritis - an inflammation of the optic nerve, which causes pain and blurred vision. Letby said she had that in 2015 and received treatment for it at the Countess and the Walton Centre. Letby said her condition resolved itself.
12:25pm: Mr Myers now refers to the babies in the case, asking general questions. He asks about when there is a death on the unit. Letby says the death "does have an impact on everyone on the unit", as it was a small unit. Everyone would have different reactions to it. She says there would be "nothing formal" as a means of support to deal with such instances, but there would be support among the colleagues. Messages would be exchanged among staff. There was "no form of support", and no formal structured assistance, the court hears. Moving to a day shift in 2016 did not help, Letby says, and Mr Myers says she continued to work nights anyway.
12:27pm: Lucy Letby says staff had to "be professional and carry on" in caring for the babies who were on the unit. For families, support on offer would come from nurses who had a bereavement guideline. "Largely it would be from the nurses". "We would support them as much as we possibly can". The 'bereavement checklist' was formal guidance, and that would include collecting memories for the family. It would normally be the designated nurse for that baby to compile such memories, Letby explains.
12:30pm: A checklist is shown for Child A. Lucy Letby's signature is present on the entries. She was the designated nurse. The checklist includes 'hand and foot prints', 'lock of hair taken', 'having religious support', 'taking photos', 'baby dressed in own clothes'. The note includes a 'memory box', which would, Letby tells the court, be a box donated by neonatal charities and be a storage box for the hand/foot prints, a lock of hair, and a teddy bear - one for the baby, one for the family to keep.
12:32pm: A staff debrief would be held, "not always", and led by the consultant, following the death of a baby on the unit. All staff would be invited to attend. It could be held 'days or weeks' following the baby's death. Asked about the death of babies for staff, personally, Letby says: "It was very upsetting - you don't forget things like that, they stay with you."
12:36pm: Letby is asked about activities outside of work. She says she had quite an active social life, attending salsa classes, going on holiday with friends, going to the gym. She would meet friends after work - she lists five colleagues, four of them nurses and one doctor, as people she would meet socially. "They were the only form of support I had, really." She is asked about the doctor. He started in 2015 as a registrar, Letby explains. They started knowing each other through work, then would meet socially. "Was it a friendship?"
"Yes."
"Was it anything more?"
"No." The friendship was close, Letby agrees. Sometimes he would come to her house, and they would go out, and would go for walks. He had since ended work at the Countess, the court hears. Their friendship continued until the early part of 2018, and then "fizzled out", the court hears.12:38pm: Letby says she and other staff would "regularly use" their phones when at work. The general rule would be not to use the phones in clinical areas. Anywhere outside of the nurseries was acceptable, the court hears.
12:42pm: Letby is asked about how well staff could get to know families. Letby says those families could be there for several months. She agrees she would also get to know families of babies not on the indictment. She says she would not be the only nurse to keep in touch with families after they have been discharged. She agrees she has looked for parents on Facebook. Mr Myers asks about her Facebook usage. "I was always on my phone." Letby says she would look up many names "out of curiosity", such as colleagues, people she had met at salsa. They would be people who were "just on my mind". She agrees she has also looked up names of parents on Facebook for babies not named in the indictment.
12:46pm: An agreed piece of evidence is now shown to the court. It is titled 'Facebook searches by Lucy Letby June 2015-June 2016'. The searches include the ones previously referred to in court, searching for the parents of babies named in the indictment, plus - on those same days - the Facebook searches for other babies' parents' names, work colleagues, and social and non-work related matters.
12:50pm: As an example, on June 9, 2015, in addition to a search for the mother's name of Child A and Child B, Letby carried out searches for three social contacts, two staffing colleagues - Ashleigh Hudson and David Harkness, and the name of a mother from a child from Liverpool Women's Hospital neonatal unit. Letby says, for the various searches, they were people "on my mind" at that moment. The 'social' names would be ones she'd met at salsa, school friends, people she had met socially. The total number of Facebook searches made by Lucy Letby in June 2015 was 113.
12:51pm: Letby says it would be "general curiosity" why she would look up the names of parents. She adds it was a "normal" thing for her and she would do it "frequently".
12:54pm: Mr Myers clarifies, following a question from the judge, that some of the social names, or 'other mother of child from LWH NNU', or 'other mother of child from COCH NNU', which have all been redacted to the court, are duplicates. In other words, Letby would search for many of the names on Facebook more than once.
12:57pm: One of the searches was for a fundraising challenge, which Letby says would have been to raise money for hospital equipment, or for the new neonatal unit. In July 2015, the total number of Facebook searches was 70. In August 2015, it was 175. The number of searches in September 2015 is 209.
2:00pm: The trial is now resuming.
2:04pm: Mr Myers asks about further Facebook searches carried out by Lucy Letby. Asked why she would carry a search for one of her nursing colleagues she regularly worked with, Letby replies it was someone who would have been on her mind.
2:09pm: The total number of Facebook searches in October 2015 is 173. One of the days, November 5, 2015, there are nine searches in nine minutes. Most are social and two are the names of mothers of children from Liverpool Women's Hospital neonatal unit. Letby says it would not be unusual for her to make several searches in a few minutes on somebody on Facebook. "That would be normal for me". The total number of searches in November 2015 is 277. Five of those related to parents of children in the indictment. The total number of searches in December 2015 is 211. In January 2016, it's 199, in February it is 178.
Mr Myers: "Generally speaking, would your pattern of searches be consistent across the month?"
Letby: "Yes."2:12pm: The number of Facebook searches in May 2016 is 164 and it's 233 for June 2016. For the latter month, none feature any searches for the names of parents of babies in the indictment. Letby denies there is any 'sinister' reason why she should be looking up the names of parents of babies. Letby adds she was "always" on her phone in her spare time.
2:17pm: Letby is asked about staying at Ash House, hospital accommodation for staff. She confirms she stayed there, moving out 'around June 2015'. For a time, Letby says she moved to a flat 'in town' in 2015, before moving back into Ash House 'towards the end of 2015'. A page from Letby's 2015 diary is shown. A note, '*Ash House*', is on June 1, 2015. It is clarified that Letby had moved back to Ash House in June 2015, having moved out for 'about six months'. The judge says this is 'not a memory test'.
2:20pm: A page from Letby's 2016 diary is shown from April. It has the note 'out of Ash H'. Letby says that is the time she moved from Ash House to her house in Westbourne Road. Messages between Letby and a colleague on April 8 mention her 'unpacking! Stuff everywhere lol'. Letby says she was "very preoccupied" with sorting the house out that weekend.
2:22pm: A photo of the front of Letby's house and her car is shown to the court. Presented with the photo, Letby says it is "quite difficult" to look at them. Photos of Letby's back garden from Westbourne Road are shown to the court. A photo of Letby's garage is shown to the court. "All that stuff in there, is that yours?" Letby says some of it is, some were tools that belonged to her dad.
2:29pm: The inside of Letby's house is now shown to the court, featuring the living room, stairs, dining room, kitchen, and a noticeboard is displayed. It contained 'photographs, various letters that were important to me'. A note 'No. 1 godmother awarded to Lucy Letby!' is made by one of Lucy Letby's godchildren. Another note from another godchild is shown. Also on the noticeboard are photos of family members and a mock-up front page of The Telegraph featuring her parents, the headline 'Hay Festival Exclusive'. Also on the board is a photo of Lucy Letby, as a band 5 nurse, with two nursing colleagues. On the landing area stairway, there is a photo of Lucy Letby and her two cousins, and a photo of her two godchildren. A photo of Letby's bedroom is shown to the court, with the bedspread 'Sweet Dreams' displayed. Cuddly toys are on the bed, of Winnie-the-Pooh and other characters. Letby becomes tearful as a photo is shown of the scene after police had investigated the bedroom.
2:32pm: A photo of the downstairs living area is shown to the court, with a cupboard shown containing a number of files and paper documents, plus DVDs. The records of Letby's two cats at the time, 'Tigger and Smudge', are also documented. Letby becomes emotional at recalling this. Letby says she kept everything from her training, and were in folders.
2:34pm: An image of Letby's 2016 diary is shown, with the sheets of paper kept in the diary. The green post-it note, 'Not good enough', was in there, as well as a vaccination record for one of the two cats, Smudge. Another photo of Letby's bedroom is shown. It shows two handbags. One was pink and 'daily' used for work, and the other was smaller, black and for 'casual, social' use.
2:36pm: Letby says prior to her arrest, she had been on a family holiday with her parents. The handbags contained three notes which have previously been shown to the court.
This was one of the notes, which Letby says contain random thoughts which were "sporadically written".
2:42pm: Letby says she would struggle to decipher some of the notes. One of the notes says 'Lovewasallweneeded'. Letby says they refer to Craig David lyrics from a 2016 song, and were just on her mind. She refers to a doctor colleague as 'my best friend' in the note. Letby says that was the case at the time. Letby says the notes have 'no sort of structure...' and they are repetitive. The name 'Kathryn de Beger' refers to a woman in occupational health.
2:44pm: Much of the note, Letby tells the court, is written for the anniversary of the death of one of the babies. Re: 'We tried our best but it wasn't enough' - Letby says the note was written as 'we' - the 'team'. She says it was not written for anyone in particular, and was written after she was being blamed for baby deaths. Re: 'I can't do it any more' - Letby is asked what she means by 'it', she means 'life'.
2:45pm: Re: 'HELP' - Letby says, tearfully: "I wanted someone to help me at that point, but nobody could help me."
2:47pm:
This note is now shown to the court. Letby says, for her care given to babies: "I only ever did my best" Asked what it felt like to be accused of what she did,
Letby replies: "I don't think you can really put it into words, it was devastating and it changed my whole life."2:48pm: Asked about a swear word on the note, which Letby says she does not normally swear, she says it was directed at Dr Ravi Jayaram and Dr Stephen Brearey, "because of the things they have been saying about me".
2:52pm: A further note is shown to the court, featuring a lot of names. One of the names is 'Whiskey', the name of Letby's former pet dog.
Mr Myers: "Why are you writing these names over and over again?"
Letby: "Because they are important people to me and they were on my mind. At the time I had a limited support network." The names include colleagues and the names of Letby's cats. Mr Myers is asked why there are different coloured inks on the note. Letby replies the note would have been added to at different times. Letby is asked about the word 'LOVE', which is in a rectangle. Letby replies "it was for the love of the people that were important to me".2:58pm: Letby says she has "always kept a diary", and would document her work shifts, activities, appointments, "everything really". Pages from Letby's 2016 diary are shown to the court. One is from February 29-March 6. For March, there is the first name of a patient. Letby says she would note the name for own records. 'LD' would mean long day, 'N', would mean night shift. The shifts include the names of a patient of 'something significant', or something which she had learned, from that day.
3:03pm: Notes of social engagements are shown to the court - including a meet-up at the Stretton Fox pub with colleagues, salsa in Buckley, a meal at Zizzis and a concert to see Ellie Goulding. The notes are in different inks. Letby says blue ink would usually be used for work-related commitments. Mr Myers, making reference to Letby's house move: "How big a thing was it to have this house?"
Letby: "Oh it was huge, a big milestone."3:05pm: Asked why the name of a particular baby is featured on one of the days in the diary,
Letby replies: "Something has stood out for that baby...it was for my own reflection."3:10pm: A diary entry for April 12, 2016 is for meeting friends at her new home, including one of her work colleagues. Shifts for April 15-17 were changed from 'N' to 'LD'. Further social engagements are noted for Tatton Park, Las Iguanas, salsa in Mold. Notes on May 2016 show, in blue ink on an 'LD' shift, the first names of two babies not on the indictment. Letby says those names were written as something notable had happened. A note on May 14 also has the name of a student nurse, which Letby says was 'documented' as it was important at work when mentoring took place.
3:25pm: The trial resumes after a short break.
3:32pm: A further note is shown, with very tightly written writing in different directions, to the court. It is written by Lucy Letby. The note 'started off as a work-based role' note, with words of 'handover', 'audit', 'workforce', 'scheduling', 'timeframe'. A close-up of the bottom-left corner is shown, with writing in different directions. Words include 'Bombay' [written several times] - Letby's pub quiz team name. A colleague's name is written - 'people who were important to me'. A name of Letby's high school teacher is also written. A crossed-out section is also shown. Behind the crossed-out part, Mr Myers tries to identify the words: 'I don't know if I killed them. Maybe I did, Maybe this is all down to me'. Letby agrees those are the words. Letby says this is how she was feeling at the time. She says crossing it out is 'just something she would do - a way of me processing and dealing with things'. She says at the time 'I hated myself'. She says 'This is how I was made to feel, that I had done something wrong'. The words are 'very random, very sporadic...there is no structure to them as such.'
3:33pm: The words 'I want to die' are written elsewhere, multiple times. Letby says that was the way she felt at the time.
3:34pm: The other side of the sheet of paper is shown to the court. The words are largely written as a note in relation to Letby's office role. Within the 'office speak', there is 'Help me', encircled. Letby says: "That is what I wanted". Also circled is the word 'tired'.
3:38pm: Letby says she did not know how many handover notes she had kept at her home. She says they were not all in one place. She said they would stay in the pocket of her uniform, where it would be on shift, and she would not dispose of it prior to leaving. "It would just get put somewhere"
"Anywhere in particular?"
"No." The number of handover sheets totalled 257.
Mr Myers: "Did you ever think to yourself, blimey, I have got a lot of handover sheets, I had better get rid of them?"
Letby: "No." Letby says the notes had no purpose at home and she did not think of them. Mr Myers says a shredder was found at Letby's home. Letby had previously told police in interview she did not have a shredder. Asked about this, Letby says it was an "oversight", and the shredder had come into her possession quite recently.3:40pm: Letby says she is "not good at all" at throwing away bits of paper. Letby adds she was aware the police might get involved in the investigation, but did not think to remove any documents. She says she did not know she had them.
3:42pm: A photo of a Morrisons bag is shown to the court. It was recovered from Letby's home. It was Letby's 'work bag'. An 'Ibiza bag' replaced the Morrisons bag for Letby. It was used for taking her uniform to work, her lunchbox, work documents and shoes. The Morrisons bag had 31 handover notes, 17 relating to babies in the indictment. Letby says she did not know when, how they came to be in her bag. She says they came in "by mistake" as part of her general pattern of behaviour.
3:43pm: Letby says she would "inadvertently" bring home handover notes from work.
3:47pm: Letby says the handover notes would have stayed in her bags from the last days of her working on the neonatal unit in 2016. A photo of a cupboard at Letby's parents' home in Hereford is shown to the court. The cupboard is in Letby's bedroom. The box is labelled 'keep' and contained five handover sheets not relating to babies in the indictment. Mr Myers asks why those handover sheets were there. Letby replies she was not sure. Letby said she had never fully moved out of her parents' home, so items would go back to that home. She said she did not know she had them.
3:50pm: Mr Myers says that concludes his questions on items found at the addresses. He says his attention will next turn to the cases of the babies themselves. He asks about Letby's recollection of the events in general. Letby agrees that, like several of the witnesses who have come into court, her memory of the events is not as clear as it was seven or eight years ago.
3:54pm: Mr Myers refers to the number, and length, of the police interviews which took place with Letby following her arrests - "in excess of 21 hours". Letby said the process of recollecting was "extremely difficult", and she relied "heavily" on police's explanations for what happened.
Mr Myers: "Have you ever tried to kill any baby you cared for?"
"No." Have you tried to intentionally harm any baby as is alleged? "No, never." Letby denies using insulin, overfeeding, forcing air or committing a physical assault to intentionally harm a baby.3:57pm: Mr Myers says the case will next discuss the case of Child A.
4:06pm: That will, the court hears, begin on Friday. The trial is adjourned until then.
Wednesday 3rd May 2023 - no court (planned)
Thursday 4th May 2023 - no court (planned)
Friday 5th May 2023
Direct Examination of Lucy Letby by Ben Myers KC - Day 2
Children A, B, C, D & EChester Standard Live Reporting
10:29am: The trial is now resuming, with members of the jury entering the courtroom.
10:32am: Benjamin Myers KC is continuing to ask Lucy Letby questions today. The focus turns to the case of Child A, born on June, 7, 2015, twin of Child B. Child A died the following day.
10:34am: Mr Myers is retelling the notes for Child A's birth. Child A, a baby boy, was born with antiphospholipid syndrome. He died the following day.
10:36am: Mr Myers refers to nursing notes, referring to the UVC line being in the wrong position on June 8 for Child A. It was reinserted but was still in the wrong position. A long line was inserted. Care was handed over to Lucy Letby at 8pm.
10:38am: Mr Myers refers to retrospective nursing notes written by Lucy Letby on the morning of June 9. The notes include: 'Instructed line not to be used by registrar. [Child A] noted to be jittery, was due to have blood gas and blood sugar taken. At 20.20 [Child A's] hands and feet noted to be white. Centrally pale and poor perfusion. [Child A] became apnoeic. Reg in the nursery. [Child A] making nil respiratory effort...' Child A later died.
10:42am: Lucy Letby says that, around the time of this taking place, she had moved to Ash House in June 2015. She said she was "still in the process of moving an unpacking" at the time of Child A's events. She says she had received a text message that morning asking her to work that night's shift. A text message from Yvonne Griffiths from 9.21am on June 8, 2015 is shown to the court asking Lucy Letby to work that night. Letby tells the court she was "frequently" asked to come in and cover neonatal unit shifts at short notice, saying she was very "flexible".
10:45am: Letby tells the court the first she knew she was going to be caring for Child A, in nursery room 1 was when she arrived for the handover at 7.30pm. She recalls there was "a lot of activity" in the nursery, with Dr David Harkness doing a line procedure and nurse Melanie Taylor sorting fluids for Child A. She explained Child A had been without fluids for a few hours.
10:52am: An intensive care chart is shown for Child A - after 4pm on June 9, the 'cannula tissued' which meant Child A's fluids had stopped, the court is told. A clinical note is shown to the court about the UVC and long line insertions. Letby says she was told by Dr Harkness and nurse Taylor the long line was suitable for use to administer 10% glucose. A collective handover had taken place prior to Letby arriving at the nursery, lasting about 20 minutes. Letby tells the court when fluids are administered via a long line, one of the two nurses present has to be sterilised, and in this case that was nurse Melanie Taylor, handling the bag, cleaning the long line, attaching the bag to the long line 'port' on Child A's left arm and making sure the line was 'flushed'. Letby was, she says, the 'dirty nurse' (ie unsterilised) for this procedure. Letby say she turned her attention to hanging the bag on to the drip stand cotside and programming the pump.
10:55am: Letby says the "usual practice" is for the line to be flushed with sodium chloride prior to fluid administration. She says she did not observe if that took place. The 10% dextrose solution is shown from a fluid prescription chart as beginning at 8.05pm.
10:57am: Letby says Melanie Taylor went over to a computer to start writing up notes. Letby said she was doing some checks - on cotside equipment, suction points, emergency equipment. She says Dr Harkness at this point was doing a procedure on twin Child B at this point. Letby says she observed Child A to be "jittery".
10:58am: Letby says "jittery" was an abnormal finding for Child A. It was "an involuntary jerking of the limbs". She says she remembered it was "noticeable". Child A's monitor sounded and his "colour changed".
11:00am: Letby says the alarm sounded, but she did not know what it indicated at the time. She says she noted Child A' "hands and feet were white". She went over to Child A, who was not breathing, so they went to Neopuff him. Letby and nurse Taylor disconnected the 10% dextrose, on Dr Harkness's advice.
11:02am: Referring to 'centrally pale', Letby says that refers to Child A being pale in the abdomen and torso. Child A was apnoeic - "not breathing". Nurse Caroline Bennion was also in nursery room 1, and had been during handover, the court hears.
11:04am: Letby says she began the 'usual procedure' of administering Neopuff to Child A. Child A's heart stopped and a 'crash call' was put out. Letby says that is an emergency line for doctors to arrive urgently. Dr Ravi Jayaram arrived immediately and another nurse arrived shortly afterwards. Letby says she cannot recall the resuscitation efforts, and says it was "an unexpected, huge shock", saying she had just gone through the doors and "then this was happening".
11:07am: Child A died shortly before 9pm. Letby says she, as designated nurse, arranged hand and foot prints for Child A as part of the hospital's 'bereavement checklist' which the court heard about on Tuesday. A nursing colleague helped assist in the hand and footprints, as that was a two-staff procedure. A baptism was offered to Child A during resuscitation, and Child A and Child B were baptised together. The court hears this was part of the practice. Letby said she felt after Child A, the bag of fluids and the long line "should be retained". She says she labelled the bag as "at the time...we should be checking everything in relation to the line and fluids" as it could be "tested" afterwards. She says she did not know what happened to the bag afterwards.
11:08am: Letby said, in reaction to Child A's death, she was "stunned, in complete shock...it felt like we had walked through the door into this awful situation - that was the first time I met [Child A] and [Child A's] parents".
11:11am: A nursing colleague messaged Letby on June 9, praising her for how she handled the situation with Child A: "...You did fab." Letby responded: "...Appreciate you saying that & Thanks for letting me do it but supporting me so well x" Letby says the network of support among colleagues in messaging each other outside of work was "something we all did".
11:13am: Mr Myers asks why Letby searched for the mum of Child A on June 9 at 9.58am. Letby says "it was just curiosity" that she wanted to see the people behind that "awful" event, and the parents "were on my mind". She says it was a "pattern of behaviour" she had, as she searched the name as part of a "quick succession" of name searches in a short period of time.
11:15am: Letby says there was a debrief after Child A had died, a few days later, led by Dr Jayaram, which discussed if there was anything to learn from the event. Letby said it was "more clinically based" rather than emotional support. She said the event "affected her" emotionally, and denies causing Child A any deliberate harm. Letby says, of that night: "You never forget something like that".
11:21am: Mr Myers turns to the case of Child B, Child A's twin sister. Child B was born on June 7, 2015, weighing 1,669g. Mr Myers says Child B was born with antiphospholipid syndrome, as noted on a clinical note. Mr Myers notes that, at birth, Child B was 'blue and floppy, poor tone, HR approx 50.' Resuscitation efforts were required, with a series of inflation breaths. Intubation was successful after a couple of attempts, and Child B stabilised on the evening of June 7.
11:24am: Mr Myers refers to nursing notes written retrospectively on the morning June 10. Child B had desaturated to 75% 'shortly before midnight', with Child B's CPAP prongs pushed out of nose. Prongs and head reposition. Took a little while and O2 to recover. HR remained stable.' 0030. Sudden desaturation to 50%. Cyanosed in appearance. Centrally shut down, limp, apnoeic. CMV via Neopuff commenced and chest movement seen...' Became bradycardic to 80s. Successfully intubated...and HR improved quickly. 0.9% saline bolus given and colour started to improve almost as quickly as it had deteriorated. Started to breathe for self...'
11:26am: Lucy Letby says she does not have much recollection of the night shift for June 9-10, in respect of Child B. A diagram shows Letby was in nursery room 3 for that night shift, looking after two babies. Letby says without that diagram, she would not have recalled who was doing what from that night.
11:33am: Mr Myers asks how Letby would know if a nurse needed assistance in a non-emergency situation. Letby says they would come and ask. Letby says CPAP prongs can be dislodged "very easily" and it happened "frequently" in babies. Before 12.30am, Letby says she believed she carried out a blood gas test on Child B, at about 12.15am. A fluid chart is shown to the court. She says at 10pm on June 9, lipids were administered. A blood gas chart is shown with a reading at 12.16am, with Lucy Letby's signature initials. She says it was "usual practice" that two nurses would be involved in the blood gas test, and she says she had no other involvement with Child B in the run-up to her deterioration.
11:35am: Letby is asked about a morphine bolus administered to Child B, as referred to in police interviews, when establishing contact with the baby. Mr Myers says, to be clear about the timing of this morphine bolus, a prescription is shown to the court, with the 'time started' being 1.10am. The court hears this is 40 minutes after the collapse.
11:40am: Letby says she cannot recall, "with any clarity", events in the build-up to Child B's collapse. She says she knows there was a deterioration "fairly soon" after the blood gas test. She said both she and a nursing colleague were in nursery 1 when Child B's colour changed - "becoming quite mottled", "dark", "all over". She says the nursing colleague alerted her to the deterioration. Letby is asked if she had seen that mottling before. Letby said it was not unusual but it was a concern, in light of Child A's death the night before. Child A was "pale" but Child B had "purple mottling". She says she and the nursing colleague were joined by a doctor at that point. Letby said she was asked to get the unit camera from the manager's office to take a picture of the mottling. She says on her return, Child B had stabilised and returned to normal colouring, and there was no mottling to photograph. She said she had the camera with her, and she had returned to the nursery "very quickly". Letby says she believes she administered some of the prescribed drugs for Child B after the collapse.
11:42am: A blood gas test taken at 12.51am is signed by Letby. She says as it is a two-nurse procedure, the signature does not indicate whether that was also the nurse who took the initial blood sample.
11:45am: Letby says following Child B's collapse, other doctors came to the nursery room, but she cannot recall who. She says presumably the designated nurse would have communicated with the family following the collapse. An observation chart shows Letby took observations for child B at 1am. She says this was "not unusual" for nurses to do this, especially if the designated nurse was busy elsewhere. The court hears this could be if that designated nurse is speaking with the parents.
12:01pm: The trial is now resuming after a short break.
12:04pm: Mr Myers now turns to the case of Child C, a baby boy born on June 10, 2015, weighing 800g, at 30 weeks +1 day gestation. An event happened on June 12 where Child C's stomach was distended, Mr Myers explains. Child C collapsed after a projectile vomit. Resuscitation efforts commenced, but he died on the morning of June 14.
12:08pm: A note by nurse Sophie Ellis is shown to the court, made retrospectively after Child C died on June 14. The note provides observations for Child C from the night shift. It adds: 'First feed of 0.5mls given at 23.00...At around 23.15, [Child C] had an apnoeic episode with prolonged brady and desat. Crash call...resuscitation commenced. Resus drugs given...care handed over to senior nurse Mel Taylor...' Further notes written retrospectively by Sophie Ellis on June 16: 'Had 2x fleeting bradys - self-correcting not needing any intervention'. A feed was taken and bile was aspirated.
12:12pm: Nurse Melanie Taylor's notes, written retrospectively: 'Called to help as baby had brady desat, when arrived to baby, baby apnoeic, loss of colour, Neopuffed, but not able to bag, no chest movement....medical team crashed bleeped. No heart rate heard, started chest compressions...intermittent gasping, continued resus. Intubated....good chest movement and air entry, continued chest compressions. Emergency drugs administered as documented...' Resuscitation efforts continued. Child C was later baptised and died that morning on June 14.
12:14pm: An x-ray examination of Child C on June 12 showed 'marked gaseous distension of the stomach and proximal small bowel'. Letby confirms, as shown from her work shift pattern displayed to the court, she was not in work that day. She worked night shifts on June 8-9, 9-10, 13-14 and 14-15.
12:16pm: Letby had messaged Yvonne Griffiths if there were any spare shifts going on June 11. The response was the unit was ok for staffing levels through the week, but may get busier at the weekend. Letby responded 'Think I need to throw myself back in on Sat x' Asked to explain that message, Letby says she wanted to get back into the unit, looking after babies. "That was what I was taught at Liverpool Women's, after a difficult shift...to get back in and carry on".
12:20pm: Mr Myers refers to police interviews with Letby regarding Child C. Letby told police she was involved, from her memory, in resuscitation efforts. She told police she thought she did chest compressions. Letby tells the court she has no recollection of any of the events leading up to Child C's collapse. She says it was "a normal shift" and has "no memory" of what happened until Child C's collapse, which was a "significant event". She says she has looked after "hundreds of babies".
12:21pm: A shift rota is shown to the court, showing Letby was looking after two babies that night on June 13. She tells the court she was in nursery room 3, with Child C in room 1 that night.
12:31pm: A timeline of staff duties from the neonatal unit is shown to the court for June 13-14. Lucy Letby is recorded as carrying out observations for the two babies she was the designated nurse for in room 3, plus an entry made on a fluid balance chart for one of those two babies. Mr Myers asks how long those would have taken. Letby says one of those would have taken "minutes", the other procedure would have taken "a little longer". Child C's event is listed at 11.15pm. Letby says her duties were allocated for two babies in room 3. Among her duties, as shown on the timeline chart, are signing for medication for babies in that room between 10.08-10.21pm, making nursing notes regarding grunting for one of the babies at 10pm, and making observations. She says she became aware of Child C at the time of his collapse, and her being called to help. Prior to that, she says she was not aware of his events, and was not in room 1. She says she was called over by nurse Sophie Ellis and asked her to put out a crash call. Melanie Taylor was "in the nursery when I arrived [in room 1]", with Child C. He was "apnoeic and needed respiratory support". Another nurse was present in the nursery at the time. Sophie Ellis put out the crash call.
12:38pm: Letby says she was involved in chest compressions as part of resuscitation efforts. Letby is asked why she can now confirm she was in room 3 of the nursery, having not been able to remember to that in police interview. Letby says she was able to remember being in nursery room 3 after since being made aware of which babies were in room 3 that night. Letby says she can recall alarms going off, but not standing cotside, or saying anything regarding Child C's observations to Sophie Ellis. She says she was said to have been in room 1 based on the statement by Sophie Ellis, but she tells the court she had not been in that room prior to Child C's collapse. She says she had been 'put' in that room 1 based on Sophie Ellis's statement. Letby tells the court she has no recollection of being there. She says she suggested explanations to police in interview of what she was doing in room 1 based on the statement, not on her independent recollection.
12:40pm: Letby says her memory of that night was: "I believe that I had been called to help [Child C following his collapse]". She says she had assumed what police had told her in interview to be true, based on Sophie Ellis's statement.
12:45pm: Messages between Letby and colleague Jennifer Jones-Key are shown to the court, in which her colleague says: "You need a break from full on ITU. You have to let it go or it will eat you up I know not easy and will take time x" Letby had initially messaged her about wanting to be in room 1, but a colleague had said no. Nurse Jones-Key replied she agreed with the colleague. Letby is asked, following a disagreement between her and nurse Jones-Key at 11.05pm, whether those messages had led to her taking any action on Child C minutes later. Letby denies that was the case.
Mr Myers: "Do those messages have anything to do with [Child C]?"
Letby: "Not at all."12:48pm: Letby says she would have been aware of Child C's family during resuscitation efforts, and that was the first time she had seen them. Asked why she had searched for the parents on Facebook, Letby says they were on her mind. She adds: "When you go home you don't forget about the babies you cared for." She says, about what the parents had gone through: "It's unimaginable."
1:59pm: The trial is now resuming following the lunch break.
2:04pm: Mr Myers is now referring to the case of Child D, a baby girl born on June 20, 2015, weighing 3.13kg. The mother's waters had broken several hours earlier. Notes show Child D '12 mins age - in dad's arms - lost colour, floppy. 5 rescue breaths + 2mins IPPV. Reviewed by SHO - on arrival, good resp. effort'. Child D 'started grunting in theatre' and the midwife was 'not happy' with Child D's colour. Child D later stabilised and had been transferred to the neonatal unit.
2:06pm: Child D suffered three collapses on the morning of June 22, the court is told, the last of those at 3.45am. Child D later died at 4.25am. Mr Myers refers to police interviews with Letby, in which she said she did not recall Child D.
2:21pm: The nursing rota for the night shift of June 21 is shown to the court, in which Letby was on duty in room 1, designated nurse for two babies. Nuse Caroline Oakley was the designated nurse for Child D in room 1 that night. Mr Myers refers to Child D's mother's statement in which she said a conversation was had with Letby at 7pm, and also saw Letby at the point Child D collapsed - "hovering around not doing much", holding a clipboard. Letby says she does not recall the 7pm conversation. She said she would not have been on duty in the clinical nurseries at that time, and would have arrived after 7pm for work, then going on to the nursery. Swipe data for Letby is shown at the entrance to the maternity neonatal entrance doors at 7.26pm. Letby says that would be to prepare for her shift. A text message is sent from Letby's phone at 7.15pm where she says: "Im just about to leave for a night shift so no problem. Hope all ok x". Letby says she would have been in Ash House at the time she sent the message. Nursing notes by Kate Bissell for Child D are inputted into the system, the last of those at 7.45pm. Observations for Child D are shown to the court, which do not have Letby's initials on them. Letby denies she was in the nursery unit at 7pm. Nursing notes by Caroline Oakley are now shown for Child D, written retrospectively at June 22. '0130 called to nursery by [nurse] and Letby. [Child D] had desaturated to 70s. The notes add Child D also desaturated (to 70s) at 3am and 3.45am. For the latter 'stimulation given to no effect; bagging via Neopuff at 3.52am. SHO on unit and called to help. Dr crash called and resus commenced...'
2:22pm: Lucy Letby says she has no recollection of the first event or the build-up to it.
2:25pm: A timeline of nursing duties is shown for June 22 from midnight is shown to the court. Letby is shown as one of two nurses for an infusion at 1.25am with Caroline Oakley. Letby says she has no recollection of this event. She says that night she would have been caring for babies on room 1 and helping other nurses, along with other miscellaneous duties.
2:30pm: A timeline shows Lucy Letby and Caroline Oakley are "checking medication for" Child D at 2.18-2.39am, and had started an infusion at 2.40am. The order of the signatures did not have any indication on who administered the infusion, Letby tells the court. At 2.44am, Letby and Caroline Oakley give medication to Child D.
2:33pm: Letby says she does not recall any details for the 3am entry made on a fluid chart for Child D. An infusion for Child D is made by Letby and Caroline Oakley at 3.20am. Mr Myers says there is nothing recorded on the timeline for Letby's involvement in respect of Child D between 3.20am-3.45am. Letby says she has no memory of the events leading up to Child D's collapse at 3.45am.
2:35pm: Letby says she cannot recall what happened to Child D.
2:45pm: Mr Myers moves on to the cases of twin boys Child E and Child F. The twins were born on July 29, 2015. Child E was born weighing 1.327kg, gestational age 29 weeks +5 days. On the evening of August 3, Child E bled from his mouth, Mr Myers tells the court. Child E died in the early hours of August 4. Mr Myers reads out nursing notes by Letby which include: 'prior to 21:00 feed, 16ml mucky slightly bile-stained aspirate obtained and discarded, abdo soft, not distended. SHO informed, to omit feed'. Child E declined through the night after vomiting blood. Resus happened at 1.15am and Child E bled from the mouth. In family communication: 'Mummy was present at start of shift attending to cares...aware that we had obtained blood from his NG tube and were starting some different medications to treat this.'
2:50pm: Mr Myers asks Letby about the nursing note, about the 16ml aspirate. The note has her signature initials. Letby says the aspirate was obtained before the 9pm feed. The note adds: 'At 2200 large vomit of fresh blood. 14ml fresh blood aspirate obtained from NG Tube'. Mr Myers says a 15ml aspirate is obtained on the chart, by Belinda Simcock. Letby says the '14' is a typo on her behalf and should be 15.
2:56pm: A night shift staff diagram is shown to the court for the night of August 3-4. Letby was the designated nurse for Child E and Child F in nursery 1. As Child E's needs increased that night, Belinda Simcock took care of Child F, Letby tells the court. Mr Myers shows a feeding chart for August 3 for Child E. No feed is recorded for 9pm. Letby says she had a large mucky aspirate obtained prior to then, so it was "standard practice" not to give the feed. The aspirate was shown to Belinda Simcock "as it was an abnormal finding" and the SHO was informed. Letby says she did not know who informed them. Letby tells the court the advice was to omit the feed.
3:00pm: At 10pm, the registrar attended, Dr David Harkness, when fresh blood was obtained from Child E. Mr Myers asks if Letby can provide an exact time Dr Harkness arrived. Letby says she cannot. She says she is not sure if Dr Harkness was there on the unit just for Child E or whether he was there for anything in addition. Letby says she can recall Child E and Child F's mother being on the unit that night, until about 10pm.
3:05pm: A nursing note shows 'mummy was present at start of shift attending to cares. Visited again approx 2200'. The mother had said Child E was, when she visited, "screaming" with "fresh blood around his mouth". Letby is asked if Child E had been screaming.
She replies: "No."
"He was unsettled at some points, but not screaming." A diagram the mother had drawn of where she said fresh blood was on Child E is shown to the court, around the mouth. Letby is asked if she can recall this when the mother visited.
She replies: "Not that I can recall, no." Letby says she cannot recall why the mother came down specifically, but she came down with breastmilk. Letby denies telling the mother to leave. She says that is not something that would be done. Letby says there was "no" blood around Child E's mouth at 9pm. She says the blood was noticed on Child E at 10pm.3:12pm: The court is shown the timeline for the night shift on August 3-4. Letby is shown administering medication for Child F at 9.13pm, with nurse Caroline Oakley also present, in room 1 - the same as Child E. Letby is asked if Caroline Oakley observed blood on Child E's face at that point, or if it was noted.
Letby replies: "No."3:22pm: The trial will resume shortly after a 15-minute break.
3:27pm: The trial is now resuming. Mr Myers is now asked to look at her police interview in the section of Child E.
3:30pm: Police ask about 9pm, which the mother said was when she arrived at the neonatal unit, seeing Child E crying and having blood come out of his mouth. Letby said this was not the case. She said a 'large vomit of fresh blood' is at 10pm. She said she was not accepting the mother's statement that blood was in Child E's mouth at 9pm.
3:34pm: Letby said she could not recall what Child E was like when the mother visited, but did not accept blood was present on Child E's mouth. Letby says she first saw blood at 10pm.
3:36pm: Letby replies: "Not that I can recall, no" and there was "no blood at that point" in response to if she had cleaned up blood from Child E's mouth at 9pm. She says there was a large mucky aspirate obtained prior to 9pm, but it did not have blood in it.
3:41pm: Letby said she did not ignore a bleed, and nor did any of her colleagues, as there was no bleed at 9pm. She denies failing to record a bleed. She says when there was a bleed, she escalated it to the registrar. Letby recalls, from 10pm onwards, the 15ml fresh blood aspirate was "very concerning". A red line around Child E's abdomen was also displaying, around the umbilical cord area. Letby says that could have been a sign of a bleed in the abdomen.
3:46pm: The note '0036 acute deterioration' is made by Letby. She tells the court Child E was intubated, was 'actively bleeding', and continued to decline. Becoming tearful, Letby says Child E was "bleeding from his mouth and his nose". She says Child E's parents were present for resuscitation. She denies Child E's deterioration was something she had wanted to happen. Following Child E's death, Letby says teddy bears were given to Child E and Child F, and on the parents' wishes, a photo was taken of the twins. Letby says she continued to look after Child F after the night shift. For Child E, she said she found his death "very traumatic", having not seen that kind of sight before.
3:48pm: Mr Myers moves on to the case of Child F, after asking if Lucy Letby is ok to continue. Child F was born weighing 1.434kg.
3:52pm: Mr Myers says the issue of Child F will focus on his blood sugar and insulin levels. On August 5, from 1.55am-7pm, there were "issues" with Child F's blood glucose levels being too level. At 5.56pm, a blood sample was taken which, when the results were returned, came back with extremely high insulin (4,657) and very low insulin c-peptide (169) levels.
3:53pm: (Note: Apologies for the continued technical issues)
3:59pm: Letby is asked to talk through blood glucose level readings taken for Child F throughout the day. The readings are low until 9.17pm on August 5.
4:02pm: Letby was not the designated nurse for Child F on August 4-5, and was the designated nurse for a baby in room 2. Child F was also in room 2, with another nurse the designated baby. An intensive care chart on August 1 is shown to the court, for Child F. Performing "various cares" for Child F is Lucy Letby, the court hears, as hourly observation readings are signed by her on the chart throughout the night, until 7am on August 2.
4:04pm: Letby was also providing cares for August 2-3, and part of the way through August 3-4 until Child E deteriorated, the court hears.
4:06pm: Letby is asked what she wanted to do on that August 4 night shift.
Letby: "I wanted to care for him."
Mr Myers: "Did you want to 'finish off' anything you had started anywhere else, as is alleged?"
Letby: "No."4:08pm: Letby says her priority was to get Child F well and get him home.
4:14pm: That concludes today's evidence. The case will resume with Lucy Letby giving further evidence in respect of Child F. Members of the jury are reminded not to discuss the case with anyone and not to conduct any research into the case.
4:20pm: The trial will resume next Thursday, May 11.
Monday 8th May 2023 - no court (bank holiday)
Tuesday 9th May 2023 - no court (planned)
Wednesday 10th May 2023 - no court (planned)
Thursday 11th May 2023 - no court (juror ill)
Friday 12th May 2023 - no court (juror ill)
Monday 15th May 2023
Direct Examination of Lucy Letby by Ben Myers KC - Day 3
Children F, G, H & IChester Standard Live Reporting
10:25am: The courtroom at Manchester Crown Court is filling up with legal teams, members of the public and press. Lucy Letby has already arrived.
10:30am: The judge, Mr Justice James Goss, has now entered.
10:32am: The trial is now resuming. Lucy Letby will continue to give evidence on the case of Child F. She confirms that, in the 10 days since her last day of giving evidence, she has not spoken with her legal representatives.
10:36am: Benjamin Myers KC tells the court Child F had low blood glucose levels throughout the day on August 5, 2015, and had a blood test which, when analysed, showed Child F had returned a very high insulin measurement of 4,657 (extremely high) and a very low C-peptide level of less than 169.
10:38am: A chart is shown for Child F's blood glucose readings on August 5, which were 0.8 at 1.54am and remained low throughout the day, the highest being 2.9 at 5am but most readings were below 2.
10:43am: A neonatal parenteral nutrition prescription chart is shown to the court, which shows Lucy Letby signed for a lipid infusion on August 1, the infusion starting at 12.20am on August 2. Lucy Letby tells the court it lasted just under 24 hours, being taken down at 12.10am on August 3. There was already a TPN bag (a nutrition bag) in place on August 2, the court hears, as shown by the chart. It was a "continuing 48-hour bag". Midnight was "around the time" which fluids were changed. Letby has signed for a TPN bag at August 3, with a co-signer. The new bag is, on the chart, beginning at 12.10am. TPN bags last 48 hours, and lipid infusions last 24 hours.
10:49am: A further sheet is shown for August 3-4, 2015. The 'continuing 48-hour bag' is signed for, but is not a new TPN bag, the court is told. That bag was discontinued at 12.25am on August 5. The chart shows a crossed-out prescription for August 5 for a TPN bag, where there is no lipid infusion. Letby tells the court Child F had been on milk. "Something changed" with those requirements and a second prescription was made for a TPN bag with lipids to be administered. The new TPN bag was hung up at 12.25am on August 5. The bag was the same, the lipids requirements had changed, which meant a new prescription was written up. Two nurses were involved in hanging up the new TPN bag, the court hears. Letby is one of the two nurses who signed for it. Two nurses - neither of them Letby - are involved in the new lipid infusion.
10:50am: Mr Myers asks if there is anything Letby did which accounted for Child F's drop in blood sugar at that point.
Letby: "No."10:58am: A prescription chart is shown to the court, showing Child F received a 3ml, 10% dextrose bolus at 2.05am. Child F's blood sugar had risen by 2.55am, the court hears. Another 3ml, 10% dextrose bolus is given at 4.20am, and Child F's blood sugar level rose. Mr Myers says Letby's night shift would have ended as usual. A chart is shown for a new TPN bag and lipid infusion for Child F at noon on August 5, which Letby confirms would have been after her shift ended. The TPN bag was hung up and a new long line was inserted as it had been "tissuing". Letby says if "tissuing" happens, it is "standard practice" to stop the administration, discard everything and start again with a new bag, as the TPN bag would have been sterile.
11:02am: Mr Myers says "even after that", Child F's blood sugar levels remained low throughout the day. Mr Myers says this is not the same TPN bag Letby had hung up just after midnight. Letby confirms this. Mr Myers asks why Letby searched for the mother of Child E and F nine times on Facebook between August 2015 and January 2016, and the father on one occasion.
Letby: "Searching people on Facebook is something I would do. Searching for [Child E and F's mum] would be when she was on my mind. "...That is a normal pattern of behaviour for me." Asked why Letby had taken a picture of a thank-you card written by the family of Child E and F,
Letby replies: "It was something I wanted to remember - I quite often take photos of cards...I receive."11:06am: Letby said she took a photo of the card at 3.40am one morning in the nursing station, while she was at work. She says there was "nothing unusual" about that. Mr Myers now turns to the case of Child G, a baby girl born on May 31, 2015 at 23 weeks + 6 days gestation, weighing 1lb 2oz at Arrowe Park. The court hears Child G was cared for in the early part of her life at Arrowe Park, being transferred to the Countess on August 13.
11:10am: The events are on September 7, 2015, involving Child G projectile vomiting and having a desaturation. She was transferred to Arrowe Park between September 8-16, returning to the Countess. Two projectile vomits, a self-resolving apnoea and a desaturation for Child G take place on September 21. The second incident, a desaturation, also took place on September 21. Lucy Letby says she called for help in this incident. Child G's monitor was off.
11:11am: Letby says she recalls Child G at the time: "She stood out as a baby who had complex needs, and was a very premature baby. "We all got to know [Child G] and her family quite well." She says she would have cared for Child G "many times" during her time at the Countess of Chester Hospital.
11:15am: A shift rota for September 6-7 is shown. Lucy Letby was the designated nurse for a baby in room 1. Child G was in room 2, being looked after by another nurse. Letby says she was in room 1 with colleague Ailsa Simpson shortly before Child G vomited. "My memory is Ailsa and myself were sat at the nursing station - we had been there for a few minutes...we heard [Child G]'s monitor [alarm] going off, and heard a retching sound. "We both immediately went in there and found [Child G] vomiting and struggling to breathe." No-one else was in the nursery room, Letby tells the court.
11:17am: Nursing notes by the designated nurse for Child G, written retrospectively, are shown to the court. They include 'Abdomen full but soft with no discolouration. Aspirates minimal, partial digested milk....short period of straining/uncomfortable at start of night when having cuddles with dad...Nurse L Letby taken over care following vomit/apnoeic episode at 0200'
11:19am: A feeding chart is shown for 45ml of breast milk at 2am, via the nasogastric tube. An acidity test showed 'pH 4' for Child G. Mr Myers asks if the chart showed the stomach had been aspirated prior to the feed.
Letby: "No."11:22am: Lucy Letby's notes for 2am onwards: '[Child G] had large projectile milky vomit at 0215. Continued to vomit++. 45mls milk obtained from NG tube with air++. Abdomen noted to be distended and discoloured. Colour improved few minutes after aspirating tube, remained distended but soft...' Letby says she has no memory of, and had not been asked to do the, caring for Child G prior to this incident.
11:29am: A nursing duties chart for the neonatal unit on September 7 is shown to the court. Letby's first entries are recorded at 2am, carrying out observations and giving a feed for the room 1 designated baby, a process which would take "a matter of minutes", Letby tells the court. She says she was then with Ailsa Simpson for a few minutes. The court hears, at 2am, Letby's nursing colleague had administered the feed for Child G, as recorded in her nursing note: 'Nurse L. Letby taken over care following vomit/apnoeic episode after 02.00 feed'. At the time of the event, Child G was seen 'vomiting from her mouth and nose' and 'struggling to breathe'. Letby says she observed this on her arrival. Child G's abdomen was 'quite firm and distended and red'. Letby says room 2 would always have lighting on, as a high dependency unit needed to have lights on to be safe, to observe babies. "We were both quite shocked...we could see vomit on the chair and on the floor - we were very shocked by that." Letby adds that babies don't vomit like that and it wasn't something she had seen before. A crash call was put out.
11:34am: Letby says the vomit on September 21 was a "forceful vomit", but not as significant as the one on September 7. Letby tells the court Child G needed further breathing support and Child G was intubated later that morning. Letby says she recalled Child G had further desaturations and required intubation, but the problems with oxygen saturation continued. Letby says she does not know why they continued. She says she confirmed giving care to Child G. She improved after being reintubated.
11:55am: The trial is now resuming after a short break. Mr Myers asks Letby about the September 21 events for Child G. The first is at about 10am, the second after 3.15pm. For that day shift, the court is shown the rota, and Lucy Letby was the designated nurse for Child G that day in room 4, along with two other babies. Two of the three members of the management team were on an office-based day, the court hears. Lucy Letby was also responsible for a fourth baby 'rooming in with parents', which was, the court hears, a baby staying in on-site accommodation with their parents as the family prepared to go home. Letby said she would periodically be going to that accommodation to check things were ok and answer any questions parents may have.
12:07pm: Letby's notes for that day are shown to the court. They include... 'at 1015 x2 large projectile milky vomits, brief self resolving apnoea and desaturation to 35% with colour loss. NG tube aspirated - 30mls undigested milk discarded. Abdomen distended, soft. Drs asked to review. Temperature remains low, tachycardiac >18bpm since vomit. Mum states that [Child G] does not appear as well as she did yesterday...' The court is shown a feeding chart for Child G. A 40ml feed of expressed breast milk was given at 9.15am, signed by Letby. After the feed, there were 'two projectile milky vomits', Letby noted. Child G also had a large bowel motion. Letby says she would have tested the stomach pH level prior to a feed, but would not have aspirated the contents. She says that would not have been needed as Child G was a '40-week baby', and would be treated as a full-term baby by this stage. Mr Myers asks if it would be known how much milk would be in a baby's stomach. Letby says she would not, as there would only be an aspiration to check for the pH levels. This projectile vomit "did not leave the cot space", Letby tells the court. She says that would have amounted to 10mls. Letby says she cannot be sure, but believes Child G's mother would have been present at the time. Letby says she, herself, would have been in the room but not at the cotside of Child G when the vomit happened, and would have been alerted to it by the monitor going off. She says Child G stabilised after that. Letby said she asked if Child G could be seen 'sooner' than usual on the ward round, as room 4 would normally be the last to be seen. Letby says there was no large-scale medical response to the incident. Letby explains care was transferred to another nurse as it was identified Child G required a higher level of care, and Letby was already looking after three babies that day.
12:17pm: The court hears evidence about the second incident on September 21. Letby says parents would be allowed and in the unit at about 3pm that day. Letby says for this incident, she remembers being 'conscious there were other parents' in the room. Screens were put up as "normal practice" for privacy, as Child G was having cannulation following her event. The note records: 'Numerous failed attempts then at cannulation. Finally inserted by Dr Gibbs. Without fluid for 6 hours, as [nil by mouth]. Blood sugars were stable throughout....further significant apnoea/brady/desat following cannulation requiring Neopuff and 100% oxygen. Help summoned...' Letby says she discovered the desaturation, and called for help. She said Child G had been behind the screen for some time, and had been looking after her other designated babies. She says she was aware the cannulation process took some time, but was not present to see it taking place as it was behind the screens. A long line chart is shown to the court, which noted the cannula was inserted at the 7th attempt. Letby said she cannot recall why she went in, but saw behind the screen that she was alone. She was 'dusky and blue and not breathing'. The monitor was "not on". Letby says Child G was on the 'procedure trolley' - used for procedures such as cannulation. Letby says the baby should not have been left alone on the trolley like that. She says she picked up Child G and put her back in her cot, applied Neopuff and called for help. Letby says she did not know why the monitor was off. The nurse colleague "froze" and got someone else to help. Another nurse, Caroline Bennion, came in. Letby said she was "very concerned" about three issues - a baby being unattended on a procedure trolley, alone behind screens, and with a monitor switched off. Letby said she raised those concerns with a nursing colleague, and was keen to file a 'Datix report'. The nursing colleague was less keen, Letby says, to raise the issue, as the procedure had been carried out by Dr Gibbs. Letby said she "took assurances" the issues would have been dealt with as discussed.
12:24pm: Letby confirms she continued care for Child G after that day. The case now moves to Child H, a baby girl born on September 22, 2015, weighing 2.33kg. The court hears Child H did not receive surfactant [a protein which helps the lungs] until 41 hours after her birth. Child H required three chest drains, and had a number of desaturations in her first few days. At 3.22am on September 26, Child H had a profound desaturation to 30%. The following morning, Child H had another desaturation to the 40s at 12.55am on September 27. Letby tells the court she remembers Child H and her care needs, but not specific details without referring to the notes. She says for September 2015, the unit "was busy at that time".
12:29pm: A message from Letby on September 24 referred to 'staffing levels on the unit' as being "completely unsafe", the court is told. In a message to another colleague, Sophie Ellis, Letby says: 'Oh Soph it was pretty bad - 18 babies, intubating on handover & a baby with a sugar of 0.1!' Letby tells the court the capacity was 16 on the unit.
Mr Myers: "Had the unit always been this busy?" "No." - Letby said it had been getting increasingly busier. She adds she had never seen a baby with chest drains at the Countess until Child H. She adds she had never seen a baby with three chest drains, even at a tertiary centre. "The most I had seen was two." Letby said during this time, doctors had to 'look things up' and discussions were held on how to manage the chest drains. She says from her experience, chest drains were sutured into the skin, so they didn't move. "Very few" chest drains were kept on the unit. Arrowe Park couriered out some drains, Letby tells the court.12:32pm: A nursing handover sheet for September 23, 2015, recovered from Letby's home in the 'Morrisons bag', is shown to the court. Letby is asked why she had that sheet, and four others with Child H on it. "It has just come back with me inadvertently and was left at home. "They have not been taken out of my pocket at the end of the shift and I have taken them home."
Mr Myers: "Did you mean to take them home?"
Letby: "No." Letby adds she did not know she had that many handover sheets at her house. "I did not keep track of them."12:37pm: The nursing notes by Letby for September 25-26 are shown to the court. They include: '...x2 chest drains in situ at start of shift - intermittently swinging. Serous fluid++ accumulating. 2330 bradycardia and desaturation requiring Neopuff in 100% to recover. 10ml air aspirated from chest drain...following poor blood gas and 100% oxygen requirement consultant Gibbs attended the unit and inserted a third chest drain. All 3 drains swinging... [Child H] desaturating++ on handling - minimal handling observed when possible. At 0322 profound desaturation and colour loss to 30%, good chest movement and air entry, colour change on CO2 detector...Neopuff commenced...Serous fluid++ from all 3 drains. Became bradycardic. Drs crash called and resus commenced...'
12:40pm: Letby is asked about the chest drains 'swinging' - she says that shows they are working, with fluid moving back and forth the drain as needed. Serous fluid is naturally occurring fluid in the body. For September 25-26, Child H was the only baby in room 1, and Letby was the designated nurse that night. She required two nurses on a high level of care, and Letby had a colleague to assist her with drugs for Child H and maintenance of the chest drains.
12:46pm: Letby refers to a note 'at 0200 blood transfusion completed', saying the timing of that is an error, and should be 3am. A blood transfusion chart shows the transfusion had started at 3pm on September 25, and ended at 3.05am on September 26. The note is co-signed by Letby. A separate chart, with Letby's handwriting, shows 'chest drain 0210' and a bolus at 0250. The 'blood complete' is sometime after 3am, prior to 3.24am, Letby tells the court. Letby says the '2am' note error she made was nothing "sinister", and 'just a mistake', and other accessible notes showed the timing the blood transfusion for Child H stopped at 3am.
12:52pm: A message from Yvonne Griffiths, part of the management team, to Letby is shown to the court, in which she commends Letby for her hard work over the previous shifts. The message is on September 26. She adds: 'You composed yourself very well during a stressful situation' and it was good to see her confidence grow. Letby relayed that message to a colleague. Letby said this message exchange had followed a disagreement over baptism for Child H. Yvonne Griffiths had felt it was 'not appropriate for that time of night' as Child H had stabilised at that point and the shift was busy. Further messages between Letby and her colleague are exchanged. Letby says, for context, she was 'choosing not to have [Child H] due to lack of appropriate support' as she wanted extra staff to assist her in the care of Child H, as Child H had several chest drains for which she had not been familiar with.
12:56pm: Letby's response to Yvonne Griffiths: 'Thank you. That's really nice to hear as I gather you are aware of some of the not so positive comments that have been made recently regarding my role which I have found quite upsetting. Our job is a pleasure to do & just hope I do the best for the babies & their family.' Letby tells the court there had been frustration about comments made by colleagues that Letby and another nurse were being allocated room 1 shifts on the rotas, and there was frustration about the unit being 'busy'. Letby agrees the court the frustration was 'particularly prominent at this time' and did not go beyond this period in September 2015.
2:10pm: The trial is now resuming following its lunch break. Benjamin Myers KC is continuing to ask Lucy Letby questions in relation to Child H. The second event is being discussed. For the night of September 26-27, Lucy Letby was the designated nurse for two babies in room 2. Nurse Christopher Booth was the designated nurse for Child G in room 2, and Nurse Shelley Tomlins was the designated nurse for Child H in room 1. The court is shown nurse Tomlin's notes for that shift, which include: '...around 2030 [Child H] had profound desat and brady, air entry no longer heard and capnography negative therefore ETT removed and Drs crash bleeped. New ETT sited...on second attempt...' This event is something, the court hears, Letby is not being blamed for. 2145 - Desaturation to 40% despite good air entry and positive capnography. ETT suctioned quickly with thick blood-stained secretions noted. [Child H] recovered quickly after...'This was also not an event Letby was blamed for, Mr Myers tells the court.
2:12pm: 0055 - profound desaturation to 40% despite equal bilateral air entry and positive capnography. ET suction yielded nil secretions. [Child H] then went bradycardic at 0107 to 40bpm and required chest compressions and adrenaline at 0108. Saline bolus given at 0112...' Letby is asked if she had any involvement with this event.
Letby: "No."2:14pm: 0330 - profound desaturation to 60s, again requiring Neopuffing with no known cause for desat....copious amounts of secretions yielded orally, pink tinged. Small amount of ET secretions gained, again pink tinged. Heart rate mainly normal during desat. Recovered slowly.' Letby is asked if she had any awareness of any of the events, including at 0055, the event Letby is being blamed for by the prosecution.
Letby: "No."2:29pm: A neonatal review chart is shown to the court, showing nurses' responsibilities and duties throughout the night of September 26-27. Lucy Letby confirms from the chart she was involved in the administration of medicine and a 'sodium chloride flush', with Shelley Tomlins, on Child H at 10.12pm. This was recorded on the computer the following minute at 10.13pm. The 'flush' was a normal procedure following the administration of such medicine, the court hears. The next recorded involvement Letby has with Child H is at 10.38pm. Letby tells the court that was for a morphine infusion. That was recorded on the computer at 10.39pm. The next recorded involvement on the neonatal chart for Letby is at midnight, when Letby is making an observation for a different baby. Letby says she was not near Child H at this time. Letby confirms to Mr Myers the next involvement with Child H on the chart is from 3.41am, with the administration of prescriptions. She does not recall what those would have been for.
2:37pm: Mr Myers moves on to the case of Child I, a baby girl born on August 7, 2015 at Liverpool Women's Hospital at a gestational age of 27 weeks. She was transferred to the Countess of Chester Hospital on August 18. 'Active problems' noted by Dr Sally Ogden at the time of transfer included 'preterm, [respiratory distress syndrome], establishing feeds, jaundice, suspected sepsis'. September 5-6, 2015, saw a number of events where Child I deteriorated and she was transferred to Liverpool. Mr Myers says Letby is not being blamed for those events. Child I was transferred back to the Countess later that month, and on September 30, at 4pm, Child I had vomiting, brady, apnoea and desaturation, followed by a similar event later that day. Another event happened on October 13 with Child I deteriorating. The following morning, Child I deteriorated and required resuscitation. She was transferred to Arrowe Park on October 15 before returning to the Countess on October 17. Child I had a desaturation on October 22, and died the following morning.
2:39pm: Letby is asked if she had a recollection of Child I. Letby says she does. She was a baby "with us for many months and got to know her [and the family] really well." She had 'complex problems' which required frequent transfer to Liverpool. Child I's abdomen "was always more distended than normal" and there were occasions when that distention would increase, Letby tells the court. Letby confirms to Mr Myers she looked after Child I on many occasions.
2:42pm: A radiograph from August 23, 2015, is shown to the court. Mr Myers says this had been part of what experts classed as a 'suspicious event', with a clinical note at the time recording 'non-specific gaseous distention of the abdomen which is suggestive of [NEC]' in Child I. A record of Letby's work shifts shows Letby was not in work that day.
2:52pm: Letby says she was looking after Child I and two other babies in room 3 on her long day shift of September 30. She says she has "some memory" of that day, "but not great detail". She denies doing anything to cause either of Child I's events that day. She says at 7.30pm, during the handover, she was giving the handover when Child I became apnoeic. Neopuffing was given, and it was noticed the abdomen was distended. An NG Tube was inserted and air was aspirated. Letby reads her notes from that day, including a note that Child I's mum noted the abdomen seemed more distended than yesterday, and Child I had an ongoing low temperature. For the abdomen, it was 'soft to touch', and the bowels had been opened. The 1500 Drs review noted Child I's abdomen was distended, and she appeared 'mottled in colour'. Letby said she asked for the review upon seeing Child I's mottled appearance. At 1600 Child I was fed, and at 1630 Child I had a large vomit and desaturation, and Drs were crash called, and Child I was transferred to room 1. Letby said for the 4.30pm event, she was not at Child I's cotside, but was in the room. She says: "She had vomited and I went over to her, and needed Neopuffing, briefly." Child I was placed on an incubator, a cannula was inserted but tissued. 'Colour appeals pale but improved'. There had been no further vomits, the abdomen still appeared distended. Child I had 'self-correcting desaturations to 80s', which Letby says was not a case when the alarm would be needed. "You have to give the baby time - to see if they self correct, which most babies do...in 30 seconds to a minute." In this case, Letby says, Child I was self-recovering without the need for help.
2:58pm: Letby says she could not say, definitively, whether Child I's mum had left at the time of handover. Letby's notes add: 'At 1930 [Child I] became apnoeic, - abdomen distended++ and firm. Bradycardia and desaturation followed, SHO in attendance and registrar crash called....'Air++ aspirated'. Letby says the air was aspirated after the Neopuff device was used. Bernadette Butterworth's nursing note: 'During handover [Child I] abdo had become more distended and hard she had become apnoeic and bradycardic and sats had dropped. IPPV given and despite a good seal with Neopuff there was still no chest movement, aspirated NGT air +++ and 2mls of milk obtained, eventually got chest movement and sats and heart rate normalised...' Letby says she recalls Child I recovered well afterwards.
3:02pm: Text messages are shown to the court from Jennifer Jones-Key to Lucy Letby, in which she complains a colleague had repeatedly, in the unit, commended Letby for her ability to swap shifts. Letby had replied in the messages, saying it was nice to hear as there had been some 'not so positive' comments about her. Letby added everyone is 'tired' on the unit. Letby tells the court the 'not so positive comments' referred to her being on room 1 shifts when others had felt they needed the experience in room 1. She agrees with Mr Myers everyone had been busy on the unit.
3:07pm: The messages shown to the court -
JJK: Oh it's just [colleague] annoyed everybody last night as she was going on about how amazing you were doing so many swaps and how naughty you weren't taken off today x
LL: Oh was she? Kinda nice to hear something positive tho as been a few not so nice comments X
JJK: It wasn't for us and [expletive deleted] people off. I've done loads of swaps and extras. It was more the fifth time she said it!!! Why won't not nice comments x
LL: Everyone pulling their weight. I think she's just sticking up for me as knows I've had some rubbish said about me w
JJK: No she just sticking up for her friends and winding everybody else up. Shldnt of said anything x
LL: I can't speak for [colleague] & I wasn't there. We've all been working hard. X
LL: That's half the problem, everyone tired x3:24pm: The trial is resuming after a short break. Mr Myers refers to the next events for Child I. Nursing notes by Ashleigh Hudson on October 13 are shown to the court. The notes include: '...'pale, pink in colour but well perfused. 0322- when in the nursery, neonatal nurse Lucy Letby noticed that [Child I] looked quite pale., when turning the light on for closer examination, we found [Child I] to be very pale in colour and not moving. Apnoea alarm in situ, had not sounded, breathing was shallow and rr appeared low....monitoring commenced....30% Neopuff O2 commenced...chest compressions commenced at 0325, no heart rate heard...' Lucy Letby's note, 'written for care given from 0345' - '[Child I] noted to be pale in cot by myself at 0320, S/N Hudson present. Apnoea alarm in situ and had not sounded...full resuscitation commenced as documented in medical notes'. A nursing shift rota is shown for October 12-13, with Lucy Letby in room 1, designated nurse for one baby. Ashleigh Hudson was designated nurse for three babies in room 2, including Child G and Child I. Letby says she cannot recall looking after Child I prior to 3.20am. She recalls going with Ashleigh Hudson the room 2 together, and noticing Child I looked pale. "Ashleigh was doing something on the worktop...with her back to the cot. I was in the doorway, talking to Ashleigh."
Mr Myers: "What was the illumination level like?"
Letby: "I can see clearly enough that [Child I] was pale in the cot. [Child I] was in front of a window. At no point is any nursery in complete darkness. "The only time we have that is in room 4, for babies preparing to go home. "It's important we need to see them visually. "We need to see the monitors and the babies themselves." Letby adds the colour level of a baby "is one of the most important things we assess". "I could see her face and her hands...she just looked very pale. "I said to Ashleigh she looked very pale and we turned the lights up". Letby says she cannot recall if the light had been on a dimmer switch, but the lighting was turned up. Child I was "very unwell" so care was given. The apnoea alarm had not gone off as, Letby says, Child I was 'gasping' and occasionally taking in air. Letby says she and Ashleigh Hudson called for help.3:32pm: Letby says she cannot recall, definitively, whether she had turned up the lights before or after seeing Child I. The court hears a police interview with Letby had said she had told them the lights were turned on before. A subsequent police interview had Letby saying she did not know whether it was before or after seeing Child I that the lights were turned up. "I know what I saw," Letby tells the court.
3:34pm: The court hears further from the police interview. The officer asks if Letby remembered, exactly, the sequence of events. Letby said she did not. "I thought we put the lights on when we went in the room." Letby added, in interview: "Maybe I spotted something Ashleigh wasn't able to spot." Letby tells the court Child I was "in my direct eyeline" when she was at the doorway.
3:39pm: The court is shown photographs of the lighting level in room 2. The photos were taken in August 2020 and form part of the agreed facts. "Do you recall the room being as dark as this appears to be?"
"No."
"Would you ever have a high dependency unit...as dark as this."
"No."
"Why not?" Letby tells the court it would not be safe. Mr Myers asks if it was necessary to turn the lights up afterwards. Letby says it was, as it was necessary for the care of Child I, such as use of syringes.3:50pm: Mr Myers now moves on to the event for Child I for October 13-14. Lucy Letby was a designated nurse for Child I in room 1, with Joanne Williams designated nurse for two other babies in room 1.
Mr Myers: "Was there anything you did to make [Child I] feel unwell...on any shift?"
Letby: "No." Letby's notes from the shift at the beginning: '...aspirate obtained. Abdomen appears full but soft. Some bruising/discolouration evident on sternum and right side of chest, ?from chest compressions. [Child I] pale in colour...' Letby says the bruising appeared to have come from CPR the previous morning. Further notes: '...[Child I] tolerating handling better, tone appears improved, remains pale. Abdomen distended but soft... At 0500 abdomen noted to be more distended and firmer in appearance with area of discolouration spreading on right-hand side, veins more prominent. Oxygen requirement began to increase, colour became pale...gradually requiring 100% oxygen...blood gases poor as charted...chest movement reduced...continued to decline. Reintubated at approx 0700 - initially responded well. Abdomen firm and distended. Overall colour pale...' Letby says she cannot recall this sequence of events from the morning. Shelley Tomlins: '0730-present. Care of [Child I] taken over...arrived on NNU minutes before arrest. [Child I] had just been retubed when desat/brady occurred and full resuscitation was required to bring her back...[Child I] stable on ventilator...abdomen very large, pale and veiny...area of discolouration noted on right side of abdomen.' Letby recalls there was discolouration, but not specific details. She says she was not involved in the continued care of Child I, and denies having caused anything which allowed this to happen.3:55pm: Mr Myers moves to the event of Child I on October 22-23. Lucy Letby is a designated nurse for a baby in nursery room 2 and one in room 3. Ashleigh Hudson is the designated nurse for Child I in room 1 and one other baby. Letby says she does not have much independent recollection from the night. She says her memory begins from when Child I was being resuscitated. She was alerted to Child I being 'unsettled' at some point, but cannot recall during the night when that was. Child I was 'rooting and appeared hungry', was 'crying and appeared very hungry' - 'sucking on fingers and lipsmacking'. Child I had been 'nil by mouth for a period of time' - Letby cannot recall how long for.
4:01pm: Ashleigh Hudson's notes for that night: '...[Child I] was unsettled and rooting at start of shift, settled with dummy and containment holding. Longline removed due to constant occlusions. Neonatal Lucy Letby unable to flush... 2357: [Child I] was very unsettled, ?due to hunger as was rooting...' Child I did not improve with increased Neopuff oxygen requirements and saturation and heart rate dropped. A crash call was put out by midnight, and Child I was intubated. Child I was later extubated as she was 'working against the ventilator'.
4:08pm: The neonatal schedule chart is shown to the court for October 22, which Mr Myers says does not record Lucy Letby having any involvement with Child I. Letby says she recalls seeing Child I and seeing she was "upset", but was not sure at which time that was. Letby says she cannot recall where she was prior to the 01.06am event when Child I became unsettled again.
Tuesday 16th May 2023
Direct Examination of Lucy Letby by Ben Myers KC - Day 4
Children I, J, K, L & MChester Standard Live Reporting
10:25am: The trial is expected to resume from 10.30am. Lucy Letby has arrived in the courtroom, and is expected to continue giving evidence in the case of Child I.
10:38am: Benjamin Myers KC, for Letby's defence, rises to continue asking Lucy Letby questions in the case of Child I. He asks about the events of October 22-23, 2015, and Letby's involvement in those events. He asks if she was involved in the efforts to assist Child I after 1.06am. She confirms she did. She recalls going to see Child I at one point, and helping nurse Ashleigh Hudson settle her, but does not recall at what point that was. She recalls being present when Child I died, and recalls the parents being there. She says it was the first time Ashleigh Hudson had experienced a loss as designated nurse, and Letby says she assisted her in the bereavement procedure for the parents. The funeral of Child I was on November 10, 2015. Letby says "more than two" members of staff attended that funeral, and this was not a usual occasion. She tells the court she was not at the funeral as she was working. Letby's working shifts rota is shown to the court for November, showing Letby was working a series of nights on November 9-10, 10-11 and 11-12. Letby said she was advised by other members of staff to send a card to the family, which would be passed to them at the funeral. Letby's sympathy card is shown to the court. She said she gave it to one of the nurses who was going to the funeral. She tells the court she took the photo while at work. She said it was "normal behaviour" for her to take a photo of the card.
10:42am: A photo of another card written by Lucy Letby is shown to the court, of her congratulating her "close friend" on the birth of her daughter. Letby says she would "regularly" take photos of cards that she would send, and had done so "for many years". She says she would also take photos of cards she would receive.
10:50am: Mr Myers moves on to the case of Child J, a baby girl born on October 31, 2015 at 32 weeks + 2 days gestation, at the Countess of Chester Hospital. Mr Myers says there were a "number of problems in pregnancy" and Child J was diagnosed with a necrotic and perforated bowel (NEC), and required transfer to Alder Hey for a stoma to be fitted. Child J returned to the Countess of Chester Hospital on November 10. Mr Myers refers to the events on the night shift of November 26-27. Mr Myers says Child J had desaturations at 4.40am and 5.03am on November 27. The designated nurse for Child J that night was Nicola Dennison. Child J had further "low desaturations" at 6.56am and 7.24am, with "eyes deviated to the left", "stiff arms" and "clenched fists".
10:54am: Letby tells the court she had "very little experience" with stomas, having seen a couple at Liverpool Women's Hospital during training. Other staff at the neonatal unit had no relevant recent experience of stomas, Letby adds, saying stoma surgery would only be carried out at a tertiary centre such as Alder Hey [the Countess of Chester Hospital was a level 2 centre]. Asked if Countess staff would regularly handle babies with stomas, Letby said: "No."
"I don't recall anybody being overly confident." She adds Child J's parents "took the lead" as they had the relevant experience from what they had been told at Alder Hey.11:04am: Letby messaged a friend on November 19: "It's shocking really that they are willing to take the responsibility for things that they have no training or experience etc on. Don't think they appreciate the potential difficulties X" Asked who she means by 'they', Letby says "the band 4 nurses". Mr Myers asks who would ask them to do it. Letby says it would be up to the shift leader to allocate them. Asked why they would be asked to look after a baby with a stoma, Letby tells the court: "the unit was so busy at the time". Letby messaged the same friend at November 25: "Went to las iguanas was really nice. At salsa. Had 3 missed calls they don't know how to give immunoglobulin and I was last person to give so just phoned and told them. [Nurse] said it's mad. Ravi is there. What a nightmare it's all getting they'll have to send babies out?? X" Letby tells the court it was "mad busy" on the unit, and the staff numbers were not at the level required for the number of babies on the unit. The night shift rota for November 26-27 is put up. Two band 4 unit nurses are named in the rota. Child J was in room 4. The designated nurse was Nicola Dennison, a band 4 nurse also looking after one other baby in room 4. Letby was the designated nurse for two babies in room 3 that night.
11:20am: Letby tells the court she had no involvement in Child J prior to her first desaturation. A rota of the end of the shift is shown to the court, with Letby having taken on a new arrival to the unit as their designated nurse during the night. She said that night was "very busy". Nicola Dennison's nursing notes are shown to the court. they include: 'Shortly after the feed at 0400 [Child J] became unwell and desaturated to the 30s. Initially not apnoeic but then did require some Neopuff to recover. Colour looks pale and mottled...' A doctor records two 'profound desats', the 1st to 30s, the 2nd to 50s. Both episodes required bagging. 'Since then pale + mottled'. The apnoea/brady/fit chart is shown to the court, recording two events at 4.40am and 5.03am. The 4.40am event lasted three minutes, the second lasting two minutes.
Mr Myers: "Did you have any idea this was happening at the time?"
Letby: "No." Letby is asked if she has recollection of the second pair of events. "Yes." She adds she has independent recollection of those events. She said, for 6.56am, she heard the monitor alarm in room 4 and Child J was "fitting", "She wasn't breathing properly...her eyes were rolling to one side of her head."
"We both heard the monitor and we [Letby and Yvonne Griffith] went in." Letby said no-one was in room 4 at the time the alarm first went off. Dr Gibbs arrived "very quickly" and Child J was transferred to room 2. Letby says for the second event, she was called to help, but does not recall who. Letby is recorded on the chart subsequently administering an infusion with Mary Griffiths. Letby says she stayed "a little later" on the unit that day for the end of her shift, but cannot recall when that was. Letby tells the court she was unaware of the first pair of events for Child J that night, but was aware and involved in the care during the second pair of events.11:26am: Lucy Letby was the designated nurse for Child J for the following night (November 27-28), the court is shown. A nursing note for Child J written by Letby from that night is shown to the court.
Mr Myers: "Any issues for [Child J] from that night, in your care?"
Letby: "No." Letby messages a colleague about the shift of November 27-28 being "much better". Mr Myers asks what she means by that. Letby replies the workload on the unit was much more manageable than the previous night. Mr Myers asks if a 'nicer,' lighter workload would be what she wanted.
Letby: "Yes."
Mr Myers: "Would you want things to be going wrong?
Letby: "No."
Mr Myers: "Would you want babies to be hurt?"
Letby: "No."11:41am: Mr Myers moves on to the case of Child K, a baby girl born on February 17, 2016, weighing 692g at 25 weeks gestation. Mr Myers says there are three parts to this event, 3.45-3.50am, when a desaturation and a dislodged tube were noted, 6.10-6.15am, and 7.30am. Dr Ravi Jayaram's notes are shown to the court. He records: 'Initially dusky, floppy, no respiratory effort' for Child K at birth. 'Successfully intubated ~20mins at third attempt by Dr Smith, transferred to NNU' For 3.50am: 'At 0330hrs 0350hrs sudden deterioration O2 sats dropped to ~40%. Bagged via ET tube with Neopuff...poor chest movement... Tube removed and bagged via facemask - Sats recovered quickly...reintubated...' Nurse Joanne Williams records in nursing notes: '...approx 4-5 minutes later began to desat to 80s. Dr Jayaram in attendance and on examination colour loss visible and no colour change on CO2 detector, ?ETT dislodged, removed and reintubated on second attempt...large amount blood-stained oral secretions.' A further note by Joanne Williams: 'Baby has had 2 further episodes of apnoea and desaturation with loss of colour. Has been reintubated twice...' Dr Jayaram's note, written at 7.50am, records: '@0615 began to have lower sats...tube pulled back to 6cm, sats dropped further, therefore extubated...responded to bagging, reintubated. Settled for next 30mins 0725 - Mean BP dropped to 14...sudden drop in sats, hr dropped to 100...cardiac compressions commenced for 1min. Tube noted to have slipped to 8cm...withdrawn and heart rate picked up immediately.' Child K was transferred to Alder Hey later that day, but remained unwell and died on February 20. Mr Myers asks if it was normal for a 25-week baby to be at a level 2 unit. Letby says it was not normal; babies would usually be cared for at a tertiary centre. She says she does not know why Child K was at the Countess of Chester Hospital.
11:58am: The trial is resuming after a short break. The layout of the neonatal unit is shown to the courtroom for February 16-17. Lucy Letby is the designated nurse for two babies in room 2 at the start of the shift. Child K was brought into room 1 during the night shift after her birth. Letby is asked if she has any independent recollection of Child K. "I remember it was unusual [seeing a 25-week gestation age baby], and seeing her at some point...but cannot recall any of the contact." Letby said she would go into room 1 to collect medication, and it was a "frequently used" room. Two other babies were in room 1, with designated nurse Caroline Oakley.
12:09pm: Mr Myers says there is a point, alleged, when Dr Jayaram sees Letby by Child K, and Child K's tube is dislodged.
Mr Myers: "Did you interfere with [Child K's] tube?
Letby: "No." Letby denies being at the cotside when Dr Jayaram entered room 1, and says she does not recall any conversation with Dr Jayaram that night. Mr Myers refers to a police interview with Letby from July 2018. Letby was asked if she remembered Child K's deterioration - "No" was the answer. Letby said she recalled Child K only as she was a 25-week baby, which was unusual on the unit. Letby was asked by police if she was present when Child K's ET tube dislodged. "I don't remember." Letby says she signed for morphine to be administered to Child K. She tells the court she had no involvement with Child K beyond that point. Letby says in police interview she was not by Child K's incubator at the time Dr Jayaram entered room 1. She told police if the desaturations dropped to 80s, she would expect the alarm to go off for Child K. She said to police: "I don't know why the alarm would not have sounded." Letby was asked by police if she had turned off or deactivated the sound on the monitor. "No." Letby tells the court "it does happen" that a tube can move "with an active baby". She told police "tubes can slip if not properly attached". Letby says if she was there, and had seen the observations drop and/or the tube slip she would have summoned help. She denies being there at that point, or having any involvement in the tube being dislodged, or 'just watching'. She denies Dr Jayaram's report was accurate.12:26pm: The neonatal schedule for February 16-17 is shown to the court. Letby is involved in the care of her two designated babies up to 12.30am, plus a baby in room 1 at 12.51am, 'assisting with cares'. Letby cares for her designated babies up to 2am, and assists in the medication of a fourth baby at 2.04am and 2.14am. The chart shows Letby's records with her designated babies up to 3.30am, when - at that time - observations are made and a feed given to one of the designated babies. Letby says 3.30am would be a "rough time" of when it happened. The feed, observations, and a nappy change, could take half an hour - the quickest '20 minutes', the longest "up to an hour". She says in this case, this could have taken "15-20 minutes". Letby is asked if, by doing this, she had any reason to be in room 1 at that time. Letby says she would not have had a reason. Letby is then recorded, on the neonatal schedule, as caring for Child K after the event has taken place. The first recorded activity is for morphine administration, with Joanne Williams signing for the medication and Letby being a co-signer. Letby says this was because Child K was being reintubated and required morphine. She does not recall being called to the nursery room. She does not recall being involved in the subsequent events for Child K. Letby is asked about a Facebook search for the surname of Child K, made on April 20, 2018, at 11.56pm. Letby says: "You still think of patients you've cared for." She says she does not recall why she looked up the name at that point. Letby says that night "was a busy shift" but, asked whether she had done anything that night to merit questions about it years later, Letby says: "No."
12:33pm: Mr Myers moves on to the cases of twins, Child L and Child M, born on April 8, 2016 at 33 weeks and 2 days gestation. Letby confirms she is still working and caring for babies, working a mixture of day and night shifts, at the hospital, during this time. She says, in reply to what her intentions were for the babies: "To provide the best care possible." She estimates she had cared for about "100" babies during these few months. Child L was born weighing 1,465g. Child L later struggled with low blood sugar. A blood sample was taken for Child L - the insulin level read 1,099, insulin C-Peptide 264. The insulin was "far higher" than the C-peptide reading, indicating, Mr Myers, insulin had been administered to Child L. Child M weighed 1,705g. Child M later had a desaturation, which it is alleged Letby had caused.
12:42pm: On April 8, Sophie Ellis messaged Letby: "How's the house pal? Xxx"
Letby responds: "Hey, it's feels a bit weird having a whole house but It's good thanks, although stuff everywhere as moved in properly on Tue & been at work Wed Thurs & today ?. Doing tomorrow as an extra so I'll see you tomorrow night. Won't be such an early start for you now back in Chester!..."
The reply: "Yeah I bet it does, it'll feel more homely once you've sorted everything out. Jeeeez 4 [Long Day shifts] in a row, are you ok?! ? I know yay and I don't have to pay for petrol, it's cost me a fortune ?゚リᄅ. Yeah they are ? haven't seen them for a while. What's the unit like? Xxx"
Letby: "Yeah I'll get there in time. Petrol & tunnel soon mounts up doesn't it! Can you claim travel expenses? I couldn't for 405. Unit is busy, No one particularly unwell just volume & few people off sick. I prefer 4 days to 4 nights. Least tomorrow is an extra & Sat pay! ?. Awe that'll be nice hope weather a bit better for you! X"
SE: "Yeah we can. Omg really, how come? That's 7 weeks as well isn't it? Yeah, 4 nights are awful. Ah that's not too bad then. Think I'd prefer to keep busy. I think it's meant to rain...dammit xxx"
LL: "Eirian said something about the induction being paid for by the trust whereas the 405 comes out of network budget so won't pay as its an expected part of role to progress etc. Mad really & costs a bomb! We've got nice mix of babies at the mo really. Shift goes quick anyway! Grr typical April showers haha. [Colleague] is in Thailand & It's been 44degrees today! X" Letby said it was a "massive" life moment for her to move into her new house, and her main focus was on "sorting out the house". Letby says the unit was "still fairly busy" at this point. On April 11, Letby messages a colleague: "The unit is in dire way with staff..." She says the unit had 'banker agency staff' and band 5s who did not have the ITU course. She says the unit being busy was "often discussed by staff".1:01pm: Letby recalls being involved with the care of the twin boys, and looked after one of the twins in the transfer to the neonatal unit. The twins were placed in nursery room 1, and Letby cared for Child L that first day. The following day, April 9, Child M was in a different place in room 1, following admission of other babies overnight. Child L and Child M were in adjacent beds in room 1, the court hears. Letby tells the court a baby's blood sugar levels are checked "within the first hour of life". Child L's first blood sugar reading is "low" - 1.9. The baby would be offered "a milk feed" via a bottle or NG tube, and the blood sugar would be checked after another hour. This did not happen with Child L, and he was administered 10% dextrose [sugar infusion], which Letby says was outside the guidelines, a decision made by Dr Bhowmik. Letby's notes: 'Advised by Dr Bhowmik to commence 10% glucose...' Letby added in the notes that she and the shift leader advised this deviated from the usual policies. A glucose bag was hung up for Child L. Letby said she cannot recall who hung up the bag - she said it would either have been herself or nurse Amy Davies. Child L had normal blood sugar levels the rest of the day. She tells the court she would have ended her shift at about 8pm. Mr Myers says for April 9, 2016, there are no recordings of blood sugar for 3am, 4am or 5am. A 10am reading of 1.9 is "too low". It is 1.6 at noon. 2pm it is 2. Letby had come on duty at 7.30am. The infusion rate has been changed at noon. A 10% dextrose bolus is administered at 3.40pm. Letby says she cannot recall who was involved in that administration. At 4pm, the blood sugar level is 1.5. At 4.30pm, a 12.5% dextrose bag is administered by two nurses including Ashleigh Hudson. The readings remain "low" up to midnight. On April 10, at 2am, the reading is 2.1, then a new 15% glucose bag is administered. 4am it is 2.3, 6am 2.2, at 2pm it is 3 - "an adequate level", but then drops for the rest of the day. A 15% glucose bag's rate is changed early on April 11, and a new bag is administered that day. The readings are 2.7, 2.9, 2.8 throughout that morning. At 3pm it is 3.5, and blood sugar is said to have stabilised.
2:19pm: The trial is resuming following its lunch break. Benjamin Myers KC is continuing to ask Lucy Letby questions in the cases of twins Child L and Child M. The infusion therapy prescription sheet is shown for Child L, with prescriptions for April 8-9. The first entry is for April 8, 11am, for a 500ml, 10% dextrose infusion, via the IV line. Dr Bhowmik authorised the prescription and the bag additive. Lucy Letby and Amy Davies set up the infusion. The first two infusion prescriptions have a line through them as, Lucy Letby explains, the rate of infusion was changed twice. It went from 4.2ml/hr to 3.6ml/hr to 4.4ml/hr. The 4.4ml/hr rate was started, using the same bag, at noon. The bags were stored in a cupboard in room 1. This was in a separate room from the insulin bags in a cupboard in a corridor.
2:25pm: Mr Myers asks how commonly dextrose is used on the unit. Letby says "very commonly", adding that a 10% dextrose solution would be administered 'all the time'. They would be used "for generic use". Letby sent a message to her mother on April 8: "Think Im going to do tomorrow as an extra but Go in a bit later. Extra money and Sat pay xX" This was to be Letby's fourth long day shift in a row (April 6-9), the maximum normally allowed for Countess staff at the unit, the court hears. For the April 9 long day, Letby was designated nurse for two babies in room 1, and Mary Griffith was designated nurse for Child L and Child M, also in room 1.
2:34pm: Child L's 10% dextrose bag was changed on April 9 to a new 10% dextrose bag, at noon, signed by Letby and Mary Griffith. That bag "would have come from the generic bags in room 1", Letby says. She does not recall who would have put it up for Child L. The equipment involved in setting it up would come from nursery room 1. Mr Myers says prior to this, Child L had a blood glucose reading of 1.9 at 10am. Letby says the initial infusion bag would still have been in place at this time. She says she cannot explain why that reading was low, and did not do anything to cause that low blood sugar reading. She adds she did not do anything to cause the later recorded insulin levels to be high for Child L.
Mr Myers: "Had you done anything to affect insulin?"
Letby: "No." Letby says as well as herself and Mary Griffith being the two designated nurses in that day, there were other nurses 'coming and going' in room 1, along with parents "present throughout the day". Nursing notes for one of Letby's designated babies - a high-dependency baby - are shown to the court. They include: 'Parents visiting carrying out feeds and cares....At 1600 parents were asked to leave the nursery due to a sick baby needing treatment, parents were understanding of this and left for the evening.' Letby says this was when Child M had deteriorated. She said this would be "common practice" to ask parents to leave in such an event. Letby adds the visiting times were 24 hours and parents would visit throughout the day.2:47pm: Nursing notes by Mary Griffith record, for Child M on April 9: '...at 12.15 noted that his stomach was a little distended and his work of breathing was increased. Was then sent for my break and [colleague] did the 12.30 feed...had an aspirate of 5mls...temp returned to normal and baby settled. At 1600 baby went apnoeic and had a profound brady and desat. Full resus commenced at 1602...care handed over to SN L Letby.' Letby tells the court Mary Griffith was, at this point, not trained for the type of intensive care Child M required, which was why care was handed over to her. A prescription chart shows Lucy Letby is involved, with Mary Griffith, in the administration of antibiotics for Child M at 3.45pm. Letby says the line would also be 'flushed' after this is administrated. Letby says at the time of Child M's deterioration, Child L was requiring further dextrose. A chart shows Letby was involved in administering a 4.3ml, 10% dextrose bolus at 3.35pm, administered at 3.40pm. A 12.5% dextrose infusion is made up by nursing staff "in response to ongoing low blood sugars", which begins at 3.35pm and the infusion starts at 4.30pm. The infusion start is administered by Belinda Simcock and Ashleigh Hudson. Letby says she and Mary Griffith had been "preparing a bag" for Child L. She says Mary Griffith was the "sterile nurse" and Letby was assisting her between 3.45pm and 4pm. Asked when she first became aware of a problem, Letby said the alarm went off and Child M was "not breathing" and "clearly struggling". Mary Griffith and another nurse were in there. Letby recalls asking parents to leave. Letby says she began initiating Neopuff "straight away", but because it didn't reach, the face mask fell on the floor, and Letby asked for another face mask for Child M. She adds she and Mary Griffith "abandoned" the making up of the bag, and "the focus was on [Child M]". Two other nurses 'started the procedure from the beginning' [of making up a new dextrose bag for Child L]. Letby said that would be "standard practice", to make sure staff were sure the new bag had the correct, required concentrations.
2:56pm: Letby, asked again by Mr Myers, denies doing anything to affect Child L's insulin levels. She agrees Child L's blood sugar levels remained low, and cannot explain why that was the case. Letby says another nurse and Dr Ravi Jayaram came to assist Child M. She says she cannot recall any observation or discussion of discolouration on Child M's skin. Letby says she left later than 8pm that night as she had a lot of documentation to file at the end of her shift. A nursing note for Child M by Letby is recorded as being written between 9.14pm-9.22pm on April 9. Letby said this was after attending to the clinical needs of Child M. Letby said she would write contemporaneous notes on the back of handover sheets or on paper towels to keep track during the day. The court is shown a few notes written on paper towels which were recovered from 'the Morrisons bag' at Letby's home by police. There are also medical notes on sheets of paper. They feature notes in the resuscitation of Child M. Letby says the notes were kept in the pocket of her uniform, and came home in her uniform. She says she did not have any other use for them. Also among the notes is a blood gas printout for Child M. Asked to explain that note, Letby says she had put it in her pocket and taken it home. Asked by Mr Myers why she hadn't binned it: "That is an error on my part." She denies having any use for the notes.
3:02pm: Letby confirms she continued to care "quite frequently" for Child L and Child M following their events, until they were both discharged from hospital on May 3. Nursing and family communication notes by Letby in respect of Child L and Child M are shown to the court on April 16, 17, 24, 25, including when Letby had been their designated nurse. "I did my best for them," Letby tells the court.
3:19pm: Mr Myers now turns to the case of Child N, a baby boy born on June 2, 2016, gestational age 34 weeks plus 4 days, weighing 1,670g. Mr Myers asks Letby how important it was for her to treat these babies. "Very important - I took the job extremely seriously...we want to make sure the babies go home." Mr Myers says Child N was born with haemophilia. Mr Myers says the first event was on June 3, at 1am when Child N was said to be "screaming or crying", desaturating, and was treated with breathing support. The second event was on the morning of June 15, when Child N had a "profound desaturation", and following from that, there were attempts to intubate him, and blood was found in the oropharynx. The third event was a "profound desaturation" at about 3pm on the same day and 3ml of blood aspirated from the NG Tube, followed by multiple attempts to intubate Child N. At 7.40pm, as a team arrived from Arrowe Park, there was a further desaturation for Child N.
3:32pm: Mr Myers asks Letby about Child N. Letby says she had not encountered a baby with haemophilia and staff on the unit were "quite panicked" about the prospect of caring for a baby with haemophilia, as they had little/no experience either. A message Letby sent to a colleague on June 2: "Everyone bit panicked by seems of things although baby appears fine" The response: "Male?"
LL: "Yeah" The response: "Factor 8?"
LL: "Not sure I only know what's on handover sheet as Dr etc all in with him doing head scan etc" Letby said at the time, she did not know what 'factor 8' referred to. The response: "Lad with haemophilia when worked community with Leighton on placement"
LL: "Ah ok I'll have to Google it later lol don't know much about it" Response: "Have to b careful with cannula/heel pricks etc "Give Factor 8 or Factor 9 I think it is dependent on which clotting factor deficiency is "Have as infusion for rest of life"
LL: "Wow" Response: "Nearly always make [then corrected to 'male']"
"We were going out supervising parents starting to give the boy his prevention injections themselves "Wonder if knew antenatally "Must have done suppose to know now "Sure boy we went to had it thru port-a-[cath]"
LL: "Complex condition, yeah 50;50 chance antenatally" Letby says her nursing colleague had more experience, and it was a 50:50 chance that the mother would pass on the condition to the baby. She said it was something she had heard of, but did not know the details of that.3:46pm: The shift rota for June 2-3 is shown to the court. Lucy Letby is on duty. She says she has no memory of the shift. A note by Dr Jennifer Loughnane for Child N at 0110: 'desat, unsettled...got upset, looked mottled, dusky, sats down to 40% - 100% O2. On my arrival 40% O2. screaming, poor trace on sats probe, pink, attempt to settle, crashed bleeped away. On return...sats 100%, asleep...' Letby denies having any involvement in the incident. A note by nurse Christopher Booth for Child N: '...One episode whilst I was on my break, whereby infant was crying++ and not settling. He became dusky in colour, desaturating to 40s. Responded to facial oxygen within 1-2 minutes. Crying subsided within 30 minutes...' Letby again denies having any involvement in this event for Child N. A neonatal schedule for June 2-3 is shown to the court. She tells the court she was doing feed/observations for one baby and assisting in prescriptions for another baby. Neither of them are Child N. The event is recorded for Child N at 1am. Letby is next recorded on the schedule at 2.30am. "Did you know there had been an incident with [Child N]?"
"No." Swipe data is shown that Letby entered the neonatal unit at 1.15am. The court has heard swipe data is collected when staff members enter the unit, not exit. Letby tells the court she may not have been in the unit at 1am. "The allegations against you are of the most grave nature, aren't they?"
"Yes." In June 2016, Letby is asked about 'concerns outside of work' - Letby said she had "an active life" with hobbies and friends. Instant messages are shown to the court, from the morning of June 13, in relation to packing for a holiday Letby took with a friend and a nursing colleague. The discussion refers to a series of Love Island and who hosted Love Island/Temptation Island. Mr Myers explains to the court who Abbey Clancy is. Mr Myers asks if Letby was thinking about killing babies during that time. Letby denies that was the case.4:02pm: A shift pattern for Letby for June 2016 shows Letby worked long day shifts on June 8, 10, 11, 13, 14 and 15.
A doctor colleague says, on June 14: "Am I right in thinking you'll have done 6 long days in the last 8? No wonder you're tired" Jones-Key: Letby says at the end of her June 14 shift, for the handover of Child N's care to Jennifer Jones-Key: "I don't recall there being any concerns at that time" for Child N. A nursing note by Lucy Letby for June 14 is shown to the court. It includes: '...repeat SBR this morning on downward trend but not yet >50 below treatment line but otherwise ready for home'. Letby says Child N was being treated for jaundice and required further phototherapy. Once that was complete, he was ready to go home. Jennifer Jones-Key notes: '...baby very unsettled early part of night. I noticed that just after 0100 feed baby looked very pale, mottled and veiny. Abdomen slightly bigger - seen by NNU nurse Belinda Simcock, advised to place baby on saturation monitor...after 30 mins noted to be having desaturations to low 80s, no intervention required but quite frequent. Rest of observations within range....baby looked worst this morning...10% dextrose commenced...' Letby agrees Child N deteriorated during the night. ...at 0715 baby crying and dropped saturations - seen by NNU nurse Lucy. Neopuff given with 100% oxygen...noted to be mottled all over body and blue in colour and cold to touch. Decision made to transfer to nursery 1... At handover baby dropped saturations again and required Neopuff. Care handed over to NNU nurse Lucy Letby'. Swipe data shows Letby and a colleague entering the neonatal unit before 7.15am, in time for the 7.30am shift. Letby recalls she went to nursery room 3 to talk to Jennifer Jones-Key "She was a good friend of mine" - as part of getting ready to work. The handover had not yet taken place "not that I'm aware of". She said the chat happened and "within minutes" Child N's monitor went off and Child N appeared mottled. Letby says Jennifer Jones-Key was tending to another baby. Letby says she was within the doorway and had not entered the room. Child N was in a cot by the doorway. Letby said she went straight over to him and he was a 'bluish colour' and she called for help. Letby says Jennifer Jones-Key finished what she was doing and came over to help. A registrar doctor came over almost immediately to help. Child N recovered from the initial episode but deteriorated again "very quickly". "His colour was not good, he was mottled, and the decision was taken to move [Child N] to room 1". Letby says she had been in the unit for "minutes". The doctor said the decision was made to intubate Child N. Letby tells the court she got the equipment ready for intubation, including routine drugs.4:10pm: A neonatal schedule shows Letby assisted in the administration of medication for Child N at 8am-8.06am. Letby is asked if she saw blood at some point during the intubation process. Letby says she does recall that, but cannot recall at what point that was. The doctor's notes: 'Attempted intubation x3...using size zero blade. Blood present at oropharynx. Unable to visualise tracheal inlet. Suction did not clear the view. Intubation abandoned due to blood present...oropharynx...trauma due to repeated attempts.' Letby recorded in her notes: '...unable to intubate - fresh blood noted in mouth and yielded via suction ++' Letby tells the court her interpretation of the note is the blood would have appeared after the attempt to intubate.
4:17pm: A 3pm note on a fluids chart records '3ml fresh blood' as an aspirate. Letby says she did recall seeing blood in the afternoon. The note is signed by a nursing colleague of Letby - the other hourly observations are signed by Letby. 1ml fresh blood is noted by Letby at 10am and 6pm. Blood++' is also recorded by Letby on a note, which the court hears is "after 8am". "Blood in mouth" is recorded at 9am.
4:27pm: Mr Myers refers to police interviews Letby had. Letby says none of what was discussed in the questioning referred to any blood seen on Child N prior to the 8am intubation. She told police the "airway issue" was from 3pm-4pm, in attempts at intubation, and recalls, from memory, seeing blood prior to 4pm. Letby denies saying she saw blood prior to 8am.
Wednesday 17th May 2023
Direct Examination of Lucy Letby by Ben Myers KC - Day 5
Children N, O, P & Q
Cross-examination by Nick Johnson KC for the Prosecution beginsChester Standard Live Reporting
10:29am: The trial is due to resume at 10.30am. Lucy Letby will be giving evidence for her fifth day, over a period spanning nearly two weeks due to public holidays and non-sitting court days. Legal teams and Lucy Letby have arrived in court.
10:39am: Benjamin Myers KC, for Letby's defence, is asking Letby questions for the third event for Child N on June 15, 2016. Lucy Letby's nursing note on that day, written retrospectively, includes: 'Infant has had periods of apnoea during the morning...improving by afternoon. Observations stable... Approx 1450 infant became apnoeic, with desaturation to 44% hr 90bpm, fresh blood noted from mouth and 3mls blood aspirated from NG Tube....Neopuff commenced and Drs crash called...unable to obtain secure airway...[Drs] unable to insert ET Tube...I Gel airway inserted and infant ventilated' Letby says after this event, she has some memory of it. "It was becoming increasingly chaotic- more and more staff [were called out to assist]. "There was a sense of panic that we weren't sure how we were going to manage [Child N]. "There were loads of people [called to care for him], I would say 10-15. "[Child N] needed such care that he needed two people to care for him [at all times]. A transport team from Alder Hey was called out to assist, and bring 'Factor 8' "as an emergency". Letby says Factor 8 was required for Child N, but none was available on the unit. Mr Myers says it was known Child N required Factor 8, and Child N had been at the unit since his birth.
Letby: "It became a panic then."
"I think baptism was offered to the parents at some point...there was a lot going on in the room. "The team from Alder Hey came and there was a lot of discussion...the team had brought a lot of specialist equipment over...at this time, handover was taking place [around 7.30pm] and around this time, that was when the episode happened."10:44am: Doctor's notes record: 'At 1940 desat 80 [down to] 50 [down to] 40% + associated brady. Resus...' Letby's notes written at 8.53pm recorded: 'Medical team from AHCH arrived approx 1900. Assessed [Child N] and decision made to attempt intubation in CLS theatre...at 1940 profound desaturation (30s) with colour loss. stiff and back arching. Became bradycardic....mottled++. Drs present. Resus commenced...care handed over. All events took place on NNU prior to moving to CLS theatres. NWTS team arrived 2040.' Letby says Child N "was the focus of the whole unit" at that point, and there were concerns staff could not get him intubated. "It was a real concern, we were all worried about him."
"It was something I had never experienced before - I had never seen that many people in the nursery for one baby. "The concern was if we couldn't get an airway...then we would have to undergo surgery... "It was frightening...for his safety."10:50am: Mr Myers now turns to the case of Child O, one of three triplet brothers born on June 21, 2016, weighing 2,020g, at a gestational age of 33 weeks and 2 days, at the Countess of Chester Hospital. Child P is another one of the triplet brothers. Mr Myers recalls the events for Child O, who died at 5.47am on June 23. A post-mortem examination showed damage to the liver. Lucy Letby says prior to this, she had been abroad on holiday with her nursing colleague and a friend. A rota of Letby's shifts showed she was off June 16-22. The rota shows she was on long day shifts for June 23-25 and June 28-30.
10:57am: Messages are shown to the court between Letby and Jennifer Jones-Key from June 22, Letby confirms when she is back in, adding: "Yep probably be back in with a bang lol" Asked to explain that, Letby says she would be back in a busy shift. Asked by Mr Myers, Letby denies she was planning "anything terrible". Letby said she was "very available" for work as she had no commitments outside work and lived nearby.
A message from a doctor [Dr A] to Letby:
"How was the flight? Unpacked as well 😉 - it's the only way!! (washing machine on?) Day has been rubbish 😡. Lots of unnecessary stress for nnu and too much work to fit into one day 😣. I may have (over)filled the unit (again) 😱. SHO's have all been fed & watered and the babies are generally ok - so maybe not as bad as I'm thinking!"
Letby: "Glad it's over but flight was & airport was fine thinks (on 2nd load of washing!!) "
"Oh that's not good back to earth with a bump for me tomorrow then!!"
"You seem to be quite good at acquiring babies to fill our empty cots....?"
The reply: "It's a skill I've had for years 😄. To be fair, there wasn't a social admission! Yes, you might be a bit busy. Oh - you're right, I made sure they went first. Just realised when I last ate (oops)"Letby says it was not unusual for the unit to be busy. She adds there was also discussion, at this time, about removing level 4 unit nurses from the neonatal unit. A shift rota for June 23 is shown. Letby was designated nurse for the triplets in room 2. Mr Myers asked if managing three babies in a high dependency was outside the ratio required for nurses to babies. Letby says it is - it should be one nurse to two babies in that room. In room 1, two nurses are looking after four babies. Letby says the care should be 1:1 [ie one designated nurse to one baby], and the room is full.
11:14am: Notes by Sophie Ellis are shown to the court for the night of June 22-23, recording observations for Child O. They include: 'TPN stopped as reached full feeds of DEBM [donor expressed breast milk], tolerating well, 12mls 2x12. Antibiotics stopped...blood gas completed at 0532 - lactate 2.3' Letby says that lactate reading is outside the normal range, and she would inform a doctor about that reading. Sophie Ellis adds: 'Abdo looks full slightly loopy. Appeared uncomfortable after feed.' Letby says Rebecca Morgan was a student nurse on her first day of placement on the unit, and Letby was the designated mentor. She tells the court the student nurse would be orientated on to the unit by a senior member of staff, but that was not possible due to the unit being busy, so she carried out the induction process herself. "On top of looking after three high dependency babies?"
"Yes - I didn't know I was going to be looking after a student [until I arrived at the unit]." Letby messaged a colleague: "It's busy but no vents [patients on ventilators] anymore. I've got triplets in 2 all ok. But got a student and first day, 2 hourly feeds etc no time to do anything lol and Yvonne f in but said i can show her sound etc x"
The reply: "What?! That's ridiculous. When r u meant to get time to do a proper induction?"
Letby: "No idea, she's nice enough but bit hard going to start from scratch with everything when got 3 babies i don't know and 2 hourly etc. Ahh well." Letby also messaged a doctor: "My student is glued to me....." Letby's nursing notes for Child O included: '...abdomen appeared full, but soft and non-distended...reviewed by [registrar] at 1315 - [Child O] had vomited (undigested milk), tachycardiac and abdomen distended.' Letby says two-hourly observations were required for all three babies in room 2, and the student nurse would also be involved. A fluid balance chart shows student nurse Rebecca Morgan has completed the reading for 8.30am, and had been doing the feed. For 10am and noon, the court hears Letby has signed the observation, but Rebecca Morgan has filled in the entries for feeds and aspirates. For Child O's observations chart, Rebecca Morgan has signed and filled in the observations at 8.30am and 10.30am. Letby says she has written in the observations for 1.30pm and 2.30pm. Letby says the 12.30pm observations have been filled in by Rebecca Morgan, but were not signed "due to human error". She denies there was anything "sinister" in leaving out the initials on the chart.11:19am: For 1.15pm, Letby recalls being outside room 2 and hearing an alarm going off. She went in and found it was Child O's alarm. She does not recall if any other nurses were in the room at that time. She recorded: "at 1315 - [Child O] had vomited (undigested milk), tachycardiac and abdomen distended.'" Letby said it was "not a concerning vomit" for Child O, who was not moved from room 2. The notes add: 'approx 1440 [Child O] had a profound desaturation to 30s followed by brady. mottled++ and abdomen red and distended. Transferred to nursery 1...perfusion poor....Drs crash called at 1551 due to desaturation to 30s with brady...reintubated...CPR commenced 1619...' Letby says, for 1440, she heard "a monitor alarming" and went in, and found it was Child O's alarm. She said she called the doctor who was next door. "This was more significant as [Child O] needed intervention at this point....he looked different...unwell at this point. "He appeared mottled...his abdomen was redder than it had been previously. "Mottling is something we see quite often with babies." Mr Myers asks if Letby had introduced air into Child O, or any baby in the case.
Letby: "No."11:38am: The neonatal schedule for June 23, 2016 is shown to the court. The event is marked for Child O at 2.40pm. At 2.39pm, two medications are given intravenously to Child O and the records are made on the computer, by Samantha O'Brien and Melanie Taylor. An infusion for Child O is made at 2.40pm by Lucy Letby and Samantha O'Brien. Letby says the order, as it appears to the court [before the event], is incorrect - the infusion should be listed in sequence after the event, in response to what had happened. She says she cannot comment on the 2.39pm medication as she was not there. Medicine prescription charts are shown to the court for the 2.39pm prescriptions. Swipe data shows Letby has arrived on the neonatal unit from the labour ward at 2.39pm. A doctor's notes record for the event: 'Called to see [Child O] at ~1440, desaturation, bradycardic and mottled. Bagged up and transferred to nursery 1... 10ml sodium chloride bolus already given' Letby says the 10% saline bolus is given, as shown on an IV chart, at 2.40pm, in response to Child O's deterioration. She tells the court that one minute prior, she was not on the unit. Child O was transferred to room 1 and the decision was made to intubate him. Letby says she cannot recall "with any clarity" the events from then on. A note from Dr Brearey is shown to the court at 6pm: 'Assisted with initial intubation...small discoloured ? purpuric rash on right chest wall. Good perfusion.' Letby says this is not something she had observed, or was identified to her at any point. Letby says she could not recall the next few hours as events for Child O merged into one. She recalls CPR taking place and there being two doctors and two nurses present. She does not recall taking part in the CPR. The court is shown there were two episodes of CPR at 4.19pm and 5.16pm. Letby recalls a drain being inserted during resuscitation. Asked about what the atmosphere is like when a baby dies on the unit, Letby tells the court: "It's completely flat, there is a complete change in atmosphere...to me personally, it's devastating, you want to save every baby in your care. "You're not supposed...to watch a baby die." Mr Myers says a post-mortem examination identified an injury on the liver. He asks if Letby knows how that happened.
Letby: "No."11:48am: Text messages between Letby and a doctor from June 30-July 1, 2016 are shown to the court, concerning the liver injury. Letby recalls a colleague being "very upset" and "was crying" at what had happened. The doctor had messaged: "I'm not sure where the information has come from. "It seems that on the SHO grapevine somebody at LWH has said that one of the triplets was found to have a ruptured Liver. "[Colleague] was upset that this may have been caused by her chest compressions."
Letby: "Oh no, that's awful. "No wonder she's upset. Were you able to reassure her?" The doctor replied: "We spent 20 mins in a cubicle going over everything. The CPR was all at the 5th rib space - between the nipples. The duoderm on [Child O] was high. If there was anything it will have been due to fluid volume causing Liver distension. "I'm not sure I believe it. "It was a coroners pm. "It usually takes weeks to get any report."
Letby: "It seems a bit like a rumour mill has gone into overdrive - the boys were only returned today, can't see how info would be out that quick?" Doctor: "No me neither."
Letby: "Not nice for [colleague] though, can see how it would play on her mind." Doctor: "This has come at the end of a 7 day run for her. Not a good time."
Letby: "No. It's good that she felt able to tell you"12:25pm: The trial is resuming after a short break. Mr Myers is now turning to the case of Child P, who weighed 2,066g. Mr Myers says there was "mild abdominal distention", recorded in Child P's clinical notes at 6pm on June 23, with "milk and air aspirates" recorded overnight. At about 9.40am on June 24, Child P had desaturation, distended abdomen, mottling. At 12.28pm, there was a further desaturation and bradycardia. Around that time, a pneumothorax was identified on the chest x-ray. At 3.14pm Child P collapsed, and later died at 4pm. A shift rota for June 23 is reshown to the court. Letby was designated baby for Child O and P and one other baby in room 2. Letby says the focus was on Child O that afternoon, and does not recall anything significant for Child P at that time. Her nursing notes from June 23: '...nursed in an incubator, observations within normal range, continues with 2hourly feeds...minimal aspirates obtained. Abdomen appears full but soft and non-distended...difficulty obtained IV access - secured after numerous attempts...' Letby says there was nothing concerning regarding Child P at this time. A doctor's note that afternoon for Child P records: 'Abdomen full; mildly distended' Letby tells the court there was "nothing unusual" about that. An abdominal x-ray for Child P is taken at 8.09pm, after Letby had stopped giving care for Child P. Letby tells the court she had stopped at 2pm that day "officially", as her care was focused on Child O that afternoon, and care of Child P was handed over. The x-ray report included: '...Gas-filled bowel loops throughout the abdomen...' Letby says student nurse Rebecca Morgan was still involved in the care of Child P. An observation chart for Child P for June 23 is shown. Letby says she signed at 8am and co-signed at 10am, with the observations filled in by the student nurse, Rebecca Morgan. The court hears Rebecca Morgan signed and filled in observations for noon, 2pm, 4pm and 6pm. Sophie Ellis records observations from 8pm onwards. The feeding chart is shown for June 23. Letby says she has co-signed at 8am, 10am, noon, and 2pm and 4pm, while Rebecca Morgan has signed and completed the entries. Trace' aspirates are recorded for Child P throughout the day, other than a 'small vomit' at noon. Letby says "other nurses" and Rebecca Morgan were looking after Child P by 6pm. Letby says after the overnight shift, Sophie Ellis said she was "quite concerned" for Child P due to the abdomen exam and following the events for brother Child O, and Child P was placed nil by mouth as a precaution. Nursing notes by Sophie Ellis on June 23-24 included: 'observations have been within limits. Did have 1 desat into 80s and 1x brady into high 90s. Self corrected, no intervention required. Does at times have a low lying HR between high 90s and 110. SHO aware. Feeding...14ml part digested milk aspirate gained at 2000 feed. Nurse in charge informed...continued with feed. 0000 feed, 20ml part digested milk aspirate obtained. Abdo is full but soft... In an addendum: 'Abdo has been soft and non distended. 25ml of air aspirated...NGT placed on free drainage.' Letby says the 14ml aspirate at 2000 was "a change", following "trace aspirates". A 20ml aspirate was taken and discarded at midnight. Letby says that was a sign the baby "was not digesting the milk", and that was a "decline" in the baby's health.
12:34pm: Letby says she would have expected the stomach for Child P to be empty at that point. Child P, from midnight onwards, was nil by mouth and was put on 10% dextrose fluids. 25mls of air was aspirated from Child P at 4am. Letby: "That is a very large volume of air.
Mr Myers: "Should it be there?"
Letby: "No." 5ml of air and 2ml of milk is aspirated at 7am. Letby tells the court that is something you would not expect to find at that time for a baby nil by mouth, and said there had been a "noticeable decline" in Child P's health. The day shift for June 24 is shown to the court. Student nurse Rebecca Morgan is on the rota. Letby is the designated nurse for a baby in room 2. The other surviving triplet is also in room 2, with designated nurse Christopher Booth. Letby said she was asked to continue looking after Child P. Asked for her opinion on that by Mr Myers, Letby said: "I felt that was the right thing to do, for the parents to have that continuity." Letby recalls, for the morning of June 24: "I was conducting my safety checks...noticed [Child P's] abdomen was quite loopy - you could see the stomach had changed, was raised. I spoke to the nurse in charge about this and wait for the [doctors to review]."
"Very soon" after the doctors reviewed Child P, Child P had an apnoea "that needed attention". Letby says herself, Dr [Anthony] Ukoh and Rebecca Morgan were in the room at the time of the deterioration. "[Child P] was apnoeic...I went out to call for help." Other doctors were in room 1 as part of their ward round and came to assist, the court hears. Child P stayed in room 2 -
Letby: "at this point room 1 was busy and it was felt safer to keep him in room 2"12:45pm: Letby's nursing note for June 24, written at 9.18pm and finished at 10pm, is shown to the court. It includes: '...[Child P] nursed in an incubator...abdomen full - loops visible, soft to touch. Reg Ukoh arrived to carry out ward round - '[Child P] had apnoea, brady, desat with mottled appearance requiring facial oxygen and Neopuff for approx. 1 min. Abdomen becoming distended' Shortly after acute deterioration...'. Letby says Child P was intubated and "seemed stable at this point". Child P had a further desaturation at 11.30am - he was given adrenaline and he was paralysed with a drug to aid ventilation.
Letby says there was no issue with a tube dislodging, or one recorded in the notes. She recorded a pneumothorax, which had been identified in Child P after the collapse. Asked, outside of the notes, to recall Child P the rest of June 24: "I just remember there being a general decline through the rest of the shift." Letby said she "gave a lot of medication" to Child P. She said, for her nursing note written at the end of the day, notes were written contemporaneously on a piece of paper. Letby does not recall a distinct change in colour for Child P that afternoon. "There was an increasing sense of anxiety [on the unit]...and a huge sense of relief when the transport team did arrive [from Arrowe Park, a tertiary centre]".
Five Countess staff were there throughout the day, and one of the doctors "frequently left the building to have a cigarette", which the court hears was something they would normally do. Child P's medical needs were "beyond our level of care", Letby said. She tells the court that "potentially", she may have said words to the effect of "he’s not leaving here alive is he?". Letby says she was present when Child P died. She says support was given afterwards to the family. She remembers dressing Child O and Child P. Asked about the atmosphere in the unit after the second triplet died, Letby says: "It was completely flat atmosphere - everybody was shocked, devastated. The whole unit was just flat, generally. It wasn't the usual positive atmosphere we would have normally. "I was really upset - two days in a row, to imagine what the patents had gone through, it was harrowing."
1:01pm: The family communication note for Child P, by Letby, is written retrospectively at 10pm. I have dressed [Child P] at their request and taken photos of [Child O and Child P] together. Support++ given to parents and extended family. Time spent on lavender suite as a family.' Letby says the note was written "so late" as she had gone to A&E herself for a needle-stick injury. One of the needles for Child P had pricked her finger, the court hears. Letby says there was a pathway she had to follow, and she had to take boosters and vaccinations. She said she was "unwell - I had fainted" - she said from the stress of the day, she hadn't eaten. "The enormity of the past two days had taken its toll."
Letby confirms she completed her notes after her A&E visit, for Child P. Letby says a doctor she had been messaging had offered her a lift home, having been aware she had gone to A&E, and would be otherwise walking home alone at night. The doctor gave her a lift, and Letby tells the court he then drove home.
The court is shown handover sheets for June 25, 2016, recovered from Letby's home by police in 2018. Various notes were written on the back of that, the court hears. Asked to explain why this, and ones for June 23-24, were found at her home: "They have come home in my uniform, and I have not done anything with them." The handover notes also include other babies Letby was the designated nurse for. A message from Letby to a doctor on June 23 said: "I lost my handover sheet - found it in the donor milk freezer!! (clearly i should still be in Ibiza)" Letby is asked to explain a search for the surname of Child O and Child P on June 23, 2017. Letby said the date was the anniversary: "they were on my mind. "It was such a harrowing experience seeing parents lose two of their children. "In two days running, you don't forget something like that." This note is shown to the court:
The note, the court hears, is a reference to the anniversary of Child O and Child P's death. Letby adds her writing also was how she felt at the time of writing the note.
2:09pm: The trial will resume shortly. Mr Myers will be asking Lucy Letby questions in the case of Child Q, the final of the 17 babies in the trial. Child Q, a baby boy, was born on June 22, 2016, weighing 2,076g.
2:21pm: Child Q was born at 31 weeks and 3 days gestation at the Countess of Chester Hospital. Mr Myers tells the court there was one event for Child Q on the morning of June 25, vomiting, desaturation, bradycardia, with "air++" aspirated from the NG Tube. A doctor gave a diagnosis of "probable NEC" the following day and Child Q was transferred to Alder Hey on June 27, returning to the Countess of Chester Hospital the following day. A handover sheet for June 28, 2016 is shown to the court, in which Lucy Letby is designated nurse for three babies, not Child Q, that day, in room 3. Letby said she was "drained and emotionally exhausted" by June 25, following the events for Child O and Child P. A day shift for June 25 is shown. Rebecca Morgan is on duty as a student nurse. Letby tells the court she was no longer the mentor as she had said she could not give her that time to do so, and so Ms Morgan was overseen by other nurses. Letby is the designated nurse for Child Q in room 2 and a baby in room 1. Letby tells the court: "You'd have to split yourself between the nurseries" when given designated care for two babies in two different nursery rooms. Nursing notes for June 24-25: '...[Child Q] self ventilating in air...feet pink and warm. New lipid syringe put up overnight...having trophic feeds of donor ebm, 0.5mls 2 hourly due to moderate aspirates. Abdomen full but soft.' Letby says the 'trophic feeds' are to get a baby's digestive system going. The aspirates indicated Child Q was not ready to tolerate larger feeds yet.
2:43pm: A feeding chart for June 23 is shown to the court for Child Q. A '2ml milky' aspirate is recorded at 2030. At this point, the court hears, Child Q had received a total of 3.5ml of milk. Letby said "you would hope" the aspirates would be decreasing throughout this time. A 3ml aspirate is recorded at 3am on June 24. Letby says it "wouldn't be of great concern...but ideally we would want the aspirate [to be] the least possible". At the time of the handover on the morning of June 25, Letby said she noticed from the observation chart he was "on the cold side" and she would want him reviewed by a doctor before the 9am feed. Letby said she was concerned about the temperature, Child Q was "on the borderline" of being too cold on the chart, and the incubator temperature was increased from 30.2C to 32C throughout the day. The temperature remained low which Letby said "was a concern". Letby said she should not feed Child Q until the doctors had reviewed him at 9am.
Letby said she was also caring for an intensive care baby in room 1. She said for cares to be given in room 1, she would have to ensure a nurse remained present in room 2. She informed two nurses when she said she needed to go to room 1. One nurse was sat at the nursing station and the doctors were starting their ward round at about 9am. Letby said she went to room 1 just after 9am. She does not recall how the room 1 baby was doing. A neonatal schedule for June 25 is shown to the court. Letby is recorded as making observations at 9am for Child Q. Letby assists a nurse in room 1 for medication at 9.04am. Letby says she was in room 1 for "a few minutes" and could hear something going on outside the nursery. "I went out through the door and I could see down the corridor" Letby went to Child Q's cotside, where there were two nurses present. Letby heard from a colleague Child Q had vomited a 'mucusy vomit'. He had stopped and "recovered" by the time Letby arrived.
Letby's notes: '[0800]...observations as charted - temperature low, incubator increased x2. Tachycardiac. Active and alert...abdomen soft and non-distended. 0910 [Child Q] attended to by S/N Lappalainen - he had vomited clear fluid nasally and from mouth, desaturation and bradycardia, mottled++. Neopuff and suction applied. Reg attended. Air++ aspirated from NG Tube.' Letby says all this was relayed to her, and not from her observation. Nurse Minna Lappalainen wrote: 'Baby found to be very mucousy, clear mucus from nasopharynx oropharynx removed. Clear fluid+++ O2 via Neopuff...Dr...emergency to attend...NGT used to aspirate stomach by nurse Lucy Letby.' Letby confirms the description of the type of fluid was the only one she heard. She did not administer the Neopuff breathing support. Letby confirms she continued to care for Child Q after he was transferred to room 1.
2:48pm: Mr Myers asks, in the context of the trial and every day at the hospital, whether this had been a significant event.
Letby: "This wasn't a significant event - this is something we deal with on a routine basis. Not that it's not important...he needed minimal intervention."
Mr Myers: "And in the course of the day, did [Child Q] have any further collapse?"
Letby: "No." Lety's notes: '...respiratory rate declining...and intermittent pauses in breathing...blood gas stable but on downward trend and [Child Q] appearing 'tired'. Oxygen requirement developing. Discussed with consultant Gibbs and decision made to electively intubate...uneventful intubation...care handed over' Letby says, other than Child Q requiring CPAP, there were no other outstanding issues for him. A nursing note by Lucy Letby for Child Q is shown for June 29 and June 30. Letby confirms she was Child Q's designated nurse for those days. She does not recall, outside of the notes, being the designated nurse for Child Q those days.2:53pm: Messages are shown between Letby and a doctor: "Do I need to be worried about what Dr Gibbs was asking?" Letby said she had become aware during the shift on who was present in the nursery when Child Q had his episode. She said she was worried she would be blamed for leaving him alone in the nursery. Letby messaged: "I walked into equipment room, he was asking Mary who was present in room and how quickly someone had gone to him as I wasn't in the room. "He asked who was there, I said I had popped out of room but Mary was in room and Minna at the desk."
The reply: "All he was doing was checking that there wasn't a delay and that a room had been left empty. Was he HDU level because of uvc? There is nothing to worry about."
Letby: "Ok. Was worried because I Wasn't with him at time, but Mary was in room and Minna outside, I had B in 1. ITU because of uvc" Letby tells the court Child Q had not been left unattended, but felt she may have been accused of leaving him unattended, and/or that she should not have left room 2. Letby did not work on the unit after June 30, 2016.3:06pm: Letby says for the annual leave on July 4-6, 2016, she was on a family holiday. She recalls, the day before she was due to go back to work, she received the news she was going to a meeting with Eirian Powell. She would not be going back to the unit 'for the time being', the court hears. Further messages between Letby and the doctor are shown to the court: "Did you manage some sleep? Back on nnu....They want to send [Child Q] back as a medical NEC. Not sure if the unit is open for transfers. Few managers / medical director around this morning."
Letby: "Yes got some sleep , did you? Good news about both. Hope they don't rush [Child Q] back…" Letby tells the court other babies had been brought back to the Countess too soon, including Child I and Child G. The doctor: "Got about 3 hours, coffee is good! It was odd - he's only been there for 14 hours, I think this is a sign of how AH it's going to be. They are so short of beds that they can only accommodate emergency patients. It's not good holistic care, and it's rubbish for his parents." Letby says 'they' refers to Alder Hey, and Child Q was 'no longer an emergency baby', so was sent back. Letby's messages between herself and a nursing colleague are shown, for June 27:
Letby: 'I reckon there's going to big meetings etc about what's gone on with unit being closed, lack of staff etc'. Letby tells the court the unit being 'closed' was closed to new arrivals. Letby had messaged: 'were way over capacity, and its skill mix too.' - Letby tells the court it was "an ongoing issue".
Late that day, Letby messaged her: "E just phoned telling me to do days this week and not Go in tonight as trying to protect me 😔""
Response: "What's that mean?"
LL: "I don't know. Asked if there was a problem and she said No just trying to protect me as had a difficult run just before holidays, less people on nights etc and we can have a chat etc tomorrow. "
"But Im worried Im in trouble or something"
Letby said "it seemed an unusual thing to do".
Response: "Don't worry, how can you be in trouble you haven't done anything wrong "Just very unfortunate"
LL: "I know but worrying in case they think i missed something or whatever. Why leave it til now to ring."
Letby says she thought she might have overlooked something. She tells the court getting things right in her work "was my life, my job". Letby is asked why a Datix report is on her phone - Letby said this was something she needed to do for Child O and Child P. Letby says she cannot recall if she did these tasks.3:19pm: The email from Yvonne Griffiths on July 15 is shown to the court referring to Letby's redeployment to an office-based role in the hospital. Letby said she "wasn't happy" about the move, and it had been imposed on her. She said she was aware that, by this time, the Countess neonatal unit had been redesignated to a level 1 unit.
Letby's message on August 8 to a nursing colleague:
"Tony phoned. He's going to speak to Karen and insist on the review being no later than 1st week of Sept but said he definitely wouldn't advise pushing to get back to unit until it's taken place. Asked about social things and he said it's up to me but would advise not speaking with anyone in case any of them are involved with the review process. Thinks I should keep head down and ride it out and can take further once over."
"Feel a bit like Im being shoved in a corner and forgotten about by the trust. It's my life and career."
"He's not been given any information about the evidence he asked for which is good. He's not sure what the external people are going to look at in relation to me but we are in the process now so have to ride it out"
Reply: "Ok well just have to take his advice then suppose 😞"
LL: "Still can't believe this has happened.
"It's making me feel like I should hide away by saying not speak to anyone and going on for months etc - I haven't done anything wrong."
Letby said she was expected to lie about things going on, that she was 'happy' to be redeployed elsewhere.
After the email was sent about secondments, Letby said: "Omg She's sent email about secondments!"
Reply: "😂😂😂"
"Email is on fire!"
LL: "Bloody hell fuming"
"Im in email and makes it sound like my choice"
The court hears Letby had filed a grievance procedure against the hospital. Letby tells the court that by this point: "I didn't know what to do - it was having a massive impact on all aspects of my life. "It was emotionally very difficult, I was lonely...I didn't know what was going on."3:45pm: The court is resuming after a short break. A picture from Letby's office is shown to the court. Letby says she would not have written it all at once. The writing is at various angles. Asked about it: "That is what I do...I write things down." It includes Letby's signature - "doodling". Letby says "she couldn't say" if this was at the time she was being blamed. There are repeated 'Everything is manageable', written six times. A lady in the occupational department had said that to Letby, which 'resonated' with her. The love hearts are "just doodling". Various names including a doctor, Karen Rees - "director of nursing", Minna, "They were important people to me at that time - they were the main people I could talk to." Also written is "I can't do this anymore" Letby said she was "fighting for my life, my job" Also written is "HELP ME" and "Please help". Letby says "at this point I had lost everything...I just wanted someone to help me. I couldn't understand how all this was happening to me." Another sheet is shown to the court. It has densely-packed handwriting at different angles. The allegations were, Letby said: "beyond comprehension"
Mr Myers: "Could you cope with it?"
Letby: "No." The note: "I really can't do this anymore - I just want to be as it was I want to be happy in the job that I loved...Really I don't belong anywhere - I am a problem to those who know me..." The note adds "Please help me [doctor] LOVE PLEASE HELP ME [doctor] You were my best friend [doctor]." Becoming tearful, Letby denies causing harm or there was any truth in her intending to kill babies, in administering insulin. "I only ever did my best." That concludes Mr Myers questions.3:46pm: Nicholas Johnson KC, for the prosecution, begins the cross-examination by asking why Letby becomes tearful when talking about herself, and not when the subject is about babies who have died. Letby says she has been tearful for babies that have died. Mr Johnson asks if there is anything Letby wishes to change about her evidence in the last few days. Letby says she cannot think of anything.
3:58pm: Mr Johnson provides Letby with a copy of her defence statement - "quite a long document", running to 20 pages. Mr Johnson says Letby has been served with documents over the past few years. He says in that time, Letby would have had time to look back on her police interviews in 2018, 2019 and 2020, and had in her statement accepted those interviews as being accurate. Mr Johnson asks if Letby ever said Dr Ravi Jayaram was a "liar who was inventing". "When was the first time you said that?"
LL: "I can't recall" J: "I'm going to suggest a date to you - yesterday." There is a silence. Letby then says she had never accepted in police interview Dr Jayaram's version of events. Mr Johnson accuses Letby of saying Dr Jayaram had been deliberately misleading a jury when giving evidence. He says that was never put to Dr Jayaram by the defence. "Was Mr Myers suggesting to Dr Jayaram that he never saw you looking over [Child K]?"
"It is very difficult to remember everything over a seven-month trial." Letby denies she is lying now by not remembering. Mr Johnson asks about handover sheets. He suggests that when Letby moves from property to property, she took the handover sheets with her.4:04pm: Mr Johnson says Letby completed a three-year nursing course, during which time Letby confirms she was living in student accommodation in Chester, in more than one place, changing each academic year. Letby says she began her employment in January 2012. Before that time, she went back to her parents' place in Hereford, and then moved to Ash House when obtaining her job. She then went to a flat of one of her colleagues, living there alone from March 15, 2014 to June 1, 2015, then back to Ash House. She moved to her Westbourne Road home in April 2016. Mr Johnson asks who provides the uniforms: "The hospital," says Letby. The staff launder the uniforms, and Letby says she launders them every time they are used. There is a rotation of three uniforms. Mr Johnson says when laundering, the pockets would be emptied. He asks where the items would be placed.
Letby: "I would accumulate papers in [random] places in my home."4:07pm: The computerised records are discussed. Mr Johnson says two people are involved in the administration of medication - one is the 'user' and the other is the 'co-signer'. Letby agrees. Mr Johnson asks if the record shows who created the record. Letby says you would have to log on to the 'Meditech' system with your login details. "It requires two people to sign". She says either of the nurses would fill in the details of the medication. The co-signer would verify the information.
4:21pm: Mr Johnson says Letby was a "mentor to students". Letby gives details of what that would involve. Mr Johnson asks for paperwork, what would their responsibilities be - if one of them was given a handover sheet, what would they do with it? Letby says they would dispose of it, although student nurses would not have handover sheets in the first place. Mr Johnson asks why Letby kept bringing handover sheets home. Letby said it was a few.
Mr Johnson: "Well, 250 times, it isn't"
Letby: "That is over many years"
Mr Johnson: "Well even if it's 50, that's over five years."
Mr Johnson: "What is your normal practice?"
Letby: "With handover sheets? To dispose of them - they have come home with me."
Mr Johnson: "You have taken them home."
Letby: "Not with the intent of keeping them."
Mr Johnson says what would Letby's responsibilities be with sensitive data such as handover sheets?
Letby: "To keep it confidential." Mr Johnson asks what would the hospital do, in disciplinary terms, if they found Letby had over 250 handover sheets?
Letby: "I don't know the full details - they were at my home address, but they were held in confidence."
"In a bin bag in your garage?"
Letby: "I was the only one in the house." Johnson: "And the ones in your parents' house?" Letby says the parents would not have access to the box in what would have been her bedroom.
Mr Johnson: "Do you obey the rules when it suits you?"
Letby: "No." Mr Myers rises says it was put to Dr Jayaram that he had not been challenged on his account in evidence. He said in his evidence he had put it repeatedly to Dr Jayaram on his account, although the word 'liar' might not have been used. The judge says, from his recollection, it was not put directly to Dr Jayaram if Letby was present in the nursery room.
Thursday 18th May 2023
Cross-examination of Lucy Letby by Nick Johnson KC - Day 2
General topics - Children A, B & CChester Standard Live Reporting
10:31am: The judge, Mr Justice James Goss, has entered the courtroom. Lucy Letby will continue to be cross-examined by Nicholas Johnson KC, for the prosecution.
10:39am: Mr Johnson asks if Lucy Letby wishes to change any of her answers from yesterday.
Letby: "No." Mr Johnson asks if handover sheets were handed out to student nurses. Letby said she would have handover sheets as a student nurse at some placements, but in the neonatal unit she cannot recall specifically. She tells the court it was not standard practice at the neonatal unit to hand out handover sheets to student nurses "for the time we are talking about".
Mr Johnson says one of the handover sheets, dated June 1, 2010, was in a keep-sake box with roses on the box, when Letby was a student nurse [Letby having started full-time employment at the hospital on January 2, 2012].
Letby says she cannot recall it.
Mr Johnson asks what is "unusual" about the handover sheet, and how it differs from the others.
Letby is unsure what Mr Johnson means.
Mr Johnson: "It is in pristine condition."
Letby: "It's the original?"
Mr Johnson: "Yes."
Letby: "Ok."10:55am: Mr Johnson says Letby took the sheet for June 23, 2016 home as it had notes of drugs for Child O and Child P. Letby said there was documentation on there, but cannot be sure what details were on it. Letby said she took the note home deliberately to bring it back the following day for finishing up writing of medications. A copy of the handover sheet is circulated to the jury and Letby. Mr Johnson says he is interested in the back, on the medical notes. Letby describes what is on the note - medication for Child P - caffeine. Nothing was written for Child O. No medications were noted for a third child. Letby said she had taken it back with the paper towel, which had further details. Letby is asked when the Morrisons work bag was placed under her bed. Letby says she cannot recall the Ibiza bag became her new bag after her trip to Ibiza around June 2016. Letby is asked how the handover sheets ended up in her bag. She says after emptying her pockets, the sheets would end up in her work bag.
Nicholas Johnson: "You're ferrying work sheets to and from work."
Letby: "I can't say definitively."
NJ: "They must have been...why put them in that bag at all?"
LL: "I can't recall."
NJ: "Can't or won't?"
LL: "They were just bits of paper to me." Letby says she accepts pieces of paper were taken between different areas and properties - "it's the paper I accumulate, not the content." Letby says she has difficulty throwing things away.
NJ: "Is that why you bought a shredder?"
LL: "I bought a shredder for certain documents when I bought the house...predominantly bank statements."
NJ: "Why not the handover sheets?"
LL: "I wasn't aware I had them."10:58am:
LL: "I wasn't thinking - they were just bits of paper."
Mr Johnson says the shredder was bought after Letby moved into her Chester home in April 2016.
LL: "They were insignificant."
NJ: "They are significant."
NJ: "They have the names of dead children on them."
LL: "They have the names of a lot of children on them - I agree I shouldn't have taken them home."11:02am: Mr Johnson asks about other work documents found in Letby's Morrisons work bag, such as a blood gas record for Child M.
NJ: "Were they insignificant?" Letby says at the time the documents were insignificant, as they went home along with a lot of other documents for babies not on the indictment.
LL: "These have come home with me...not with any intention."
NJ: "You have taken them home." Letby accepts the wording.11:04am: Mr Johnson asks if Letby recalls a colleague nurse's evidence for Child M on the blood gas reading. Mr Johnson says she took it, wrote it on the chart, and disposed of it. Letby is asked how she got the sheet, if it had been put in the [hospital's] confidential waste bin.
LL: "I can't recall specifically."
NJ: "It was for your little collection, wasn't it?"
LL: "No."11:07am: Mr Johnson asks why Letby purchased a shredder if she wasn't going to use it - was she on so much money she could make such purchases? Letby, after saying she is not sure what finance has to do with this, says she used the shredder to shred bank statements. "Why did you lie about [not having a shredder] in interview?" Letby said she didn't recall having a shredder, it was not a significant item in her house. "Like the pieces of paper?" Letby agrees.
11:15am: Letby, asked how she could have disposed of handover sheets, said to police in interview she did not have a shredder and, if she did, that would be how she would dispose of confidential documents. Letby tells the court: "I can't recall at the time - I had just been arrested by police, locating a shredder wasn't on my mind." Mr Johnson asks when the shredder was bought. Letby says "shortly before this [police] interview - if I said it was bought recently." Mr Johnson asks about a shredder box in Letby's parents' home, in her bedroom wardrobe. Letby said "it probably moved with me". She says she cannot recall "definitively" whether it was her parents' shredder. Mr Johnson says "it was settled" that the box had the word "keep" written on it. Letby said that was to "keep the box and the shredder".
Mr Johnson: "But there is no shredder in the box"
Letby: "The shredder was elsewhere in the house". Letby agrees her parents would not go in her room at their parents' place. Mr Johnson asks why the word 'keep' would be written on the box in that event. "I can't answer that."11:22am: Mr Johnson asks about a sympathy card written to Child I's family. Letby is asked where she wrote the card. Letby says she bought the card, but cannot recall where specifically she wrote it. Letby says she wouldn't have written it on shift. Letby is asked why the photo was taken when she was at work. "The card is written, it has been taken to work to hand over to a colleague who is going to the funeral."
NJ: "Why did you take a picture at the place where the child...died in dreadful circumstances?" Letby said the place the photo was taken was "insignificant", it was taken before the card was handed over to staff.
Mr Johnson: "Another thing that is insignificant?"
Letby: "I think that is taken out of context."
Mr Johnson: "Did it give you a bit of a thrill?"
LL: "Absolutely not."11:33am: Mr Johnson says in the defence, Letby's name is not referred to in the schedule surrounding the events for some babies. "Are you suggesting the absence of your name [from the schedule]...is showing you hadn't had contact with the child?" Letby agrees "...in terms of the documentation at that time." She agrees that does not record events such as minor nursing responses if a baby starts crying. Letby says she has been to the unit on days off, such as finishing documentation that hasn't been done in the day, or seeing colleagues who have been on a course. Letby says a record would be made as the swipe data would record her entrance, as the only way she could get into the unit. Mr Johnson says for Child G, Letby did not leave work until 10am on September 7. Letby says: "That's not unusual." A message is shown from 10.56pm on September 7 -
Letby: "She looks awful doesn't she. Hope you get some sleep." Letby said if there was a sick baby on the unit, "you would go and check on them, that's not unreasonable." She had looked at Child G's charts, and accepts she was not on duty at that time. Letby said she had been in to finish some documentation. Mr Johnson tells the court this was a "big day for" Child G, as it was her 100th day. Letby said: "Yeah she's declining bit by bit". Mr Johnson says there is no record of Letby entering the unit. He suggests Letby does not need a pass to gain entry to the unit. Letby says she would need a pass to swipe in, and accepts: "Unless another colleague opened the door for me." Letby adds if she had a legitimate reason to enter the unit, she would have entry accepted. Letby is asked why she entered the unit at around 11pm, not earlier that day.
Letby: "It's quieter at night - I don't know, I can't say why I've gone in at night."11:49am: The trial is resuming after a short break.
11:55am: Mr Johnson asks to clarify an issue relating to nasogastric tube feeds. Letby explains to the court how an NG Tube feed is administered to a baby.
NJ: "Have you ever used a plunger syringe to speed up the flow of milk?"
LL: "No."
NJ: "Have you ever sent texts to your friends while giving an NGT feed?"
LL: "No." Letby says that would be inappropriate and impractical. She says the times on the feed charts would be done to the next 15 minutes - [such as, for 9am, that feed would be between 8.45am-9.15am]. Letby says she has never used her phone in a clinical area. She says the baby would take priority over texting her friends/colleagues. She says she has not texted anyone while a resuscitation is taking place on the unit, one that she was involved in. Letby said she would not 'provide commentary' during a resuscitation.11:58am: Mr Johnson asks about staffing levels. Letby agrees that babies in room 1 are not necessarily always intensive care babies, or that babies in room 2 are always high dependency babies.
Mr Johnson says if the jury conclude a baby was attacked, then it would be the attacker who was the common link
Letby: "Just because I was on shift doesn't mean I have done anything."
Mr Johnson says if the jury conclude attacks happened in four cases, then the common link between them all would be the attacker.
LL: "That is for them to decide."
NJ: "On principle, do you agree?"
LL: "I don't think I can answer that."12:06pm: Mr Johnson asks about Letby's colleagues. Letby says she did not have a disagreement with Dr Gail Beech or Dr Andrew Brunton, and had a good working relationship with them. For Dr Stephen Brearey, Letby said she did not have a problem with him at the time she was at work with him - she wrote a note calling him a profanity after she was redeployed, as he and Dr Ravi Jayaram "had been making comments" about Letby being implicated in the deaths of babies. "They were very insistent that I be removed from the unit." Letby denies being in love with a doctor who cannot be named - "I loved him as a friend, I was not in love with him." A note in Letby's handwriting is shown to the court. There is a suggestion the writing, previously said as 'Timmy', is 'Tiny Boy'. Letby says her dog as a child had a nickname of 'Tiny boy', while another of her childhood dogs was named 'Timmy'. Letby said she had no issues with other doctors on the unit, including Dr John Gibbs, Dr Sally Ogden, Dr Alison Ventress and Dr David Harkness. For one other doctor, she said she did not have the best working relationship, but they got on. For Dr Jayaram, "we had a normal working relationship".
NJ: "You searched for him on the internet."
LL: "I searched for a lot of people."12:11pm: Letby says four doctors were in the 'conspiracy group', including Dr Jayaram, Dr Gibbs and Dr Brearey - "that they have apportioned blame on me". Letby is asked about "failings in the hospital". Letby is asked if Child E was poisoned with insulin. "Yes I agree that he had insulin."
"Do you believe that somebody gave it to him unlawfully?"
"Yes."
"Do you believe that someone targeted him?"
"No."
"It was a random act?"
"Yes...I don't know where the insulin came from."
"Do you agree [Child L] was poisoned with insulin?"
"From the blood results, yes."
"Do you agree that someone targeted him specifically?"
"No...I don't know how the insulin got there." Letby adds: "I don't believe that any member of staff on the unit would make a mistake in giving insulin." The judge asks if that is the case for Child E. Letby agrees. She denies it was her who administered the insulin.12:12pm: Letby is asked about the dangers of unprescribed insulin.
Letby: "It would cause them to be unwell, it would cause them to be hypoglycaemic... seizures, apnoea, even death."12:16pm: Letby is asked about her training which, when completed, allowed her to care for intensive care babies. Letby is asked if that meant she would have access to room 1 more often than before. Letby agrees. The training involved education about lines, access, and the complication of air embolus, the court hears. Letby said she had heard of air embolus by the time police interviewed her. She tells the court: "All staff know that air introduced...can lead to death."
NJ: "Everybody knows the danger of air embolus."
LL: "I can't speak for everyone."12:18pm: Mr Johnson asks about the case of Child A. Letby says she did have independent memory of Child A. "Before [Child A], had you ever known a child to die unexpectedly within 24 hours of birth?"
LL: "I can't recall - I'm not sure." Letby says she can recall "two or three" baby deaths prior at the Countess of Chester Hospital, and "several" at her placement in Liverpool Women's Hospital. Mr Johnson says Letby had previously told police it was "two" at Liverpool. Letby says her memory would have been clearer back then.12:24pm: Letby says it was discussed at the time Child A's antiphospholipid syndrome could have been a contributing factor at the time. Letby tells the court "in part", staffing levels were a contributing part in Child A's death, due to a lack of fluids for four hours and issues with the UVC line. She says they were "contributing factors", and put Child A "at increased risk of collapse". "I can't tell you how [Child A] died, but there were contributing factors that were missed." Letby says the issues with Child A's lines "made him more vulnerable", with one of the lines "not being connected to anything". Letby is asked why she didn't record this on a 'Datix form'.
LL: "It was discussed amongst staff at the time...I didn't feel the need to do a Datix, it had been raised verbally with two senior staff, one Dr Jayaram, one a senior nursing staff." She adds: "I don't know why [Child A] died." Letby says if the cause of death was established as air embolus, then it would have come from the person connecting the fluids, "which wasn't me".12:27pm: Mr Johnson: "Do you accept you were by [Child A] at the time he collapsed?"
LL: "I accept that I was in his cot space, checking equipment, yes...I was in his close vicinity."
NJ: "Could you reach out and touch him?"
LL: "I could touch his incubator - the incubator was closed."
NJ: "Could you touch his lines?"
LL: "No."12:32pm: Letby says "there's no way of knowing" from the signatures, who administered the medication between the two nurses, Letby or nurse Melanie Taylor. Dr David Harkness recalled to the court: "There was a very unusual patchiness of the skin, which I have never seen before, and only seen since in cases at the Countess of Chester Hospital." Letby disagrees with that skin colour description for Child A. She agrees with Dr Harkness that Child A had "mottling", with "purple and white patches". Letby says she cannot recall any blotchiness. "I didn't see it - if he says he saw it...that's for him to justify. "It's not something I saw. "I was present and I did not see those."
12:36pm: Dr Ravi Jayaram said Child A was "pale, very pale", and referred to "unusual patches of discolouration."
Letby: "I don't agree with the description of discolouration, I agree he was pale." Letby disagrees with the description of Child A being blue, with pink patches 'flitting around'. An 'experienced nurse of 20 years', who the court hears was a friend of Letby, said: "I've never seen a baby look that way before - he looked very ill." Letby agrees Child A looked ill. She disagrees with the nurse's statement of the discolouration, or the blotchiness on Child A's skin. "I agree he was white with what looked like purple markings." Letby agrees with the statement that the colouring "came on very suddenly".12:46pm: Mr Johnson refers to Letby's police interview, in which Letby was asked to interpret what she had seen on Child A. Letby explained to police mottling was 'blotchy, red markings on the skin' "Like, reddy-purple". Child A was "centrally pale". In police interview, Letby was asked about what she saw on Child A. She said: "I think from memory it [the mottling] was more on the side the line was in...I think it was his left." Letby tells the court she felt Child A was "more pale than mottled". She says it was "unusual" for Child A to be pale and to have discolouration on the side", but there was "nothing unusual" about the type of discolouration itself. Mr Johnson asks about the bag being kept for testing. Letby says she cannot recall if she followed it up if the bag was tested. She had handed it over to the shift leader. Letby is asked if she accepts Child A did not have a normal respiratory problem. Letby agrees.
12:53pm: Mr Johnson asks if Letby has ever seen an arrhythmia in a neonate.
Letby: "No, I don't think so, no."
Mr Johnson says air bubbles were found in Child A afterwards. "Did you inject [Child A] with air?"
"No." Mr Johnson asks if Letby was "keen" to get back to room 1 after this event. Letby says from her experience at Liverpool Women's, she was taught to get back and carry on as soon as possible. Letby had been asked what the dangers of air embolus were, and she had not known. "Were you playing daft?"
"No - every nurse knows the dangers." Letby said she did not know how an air embolus would progress, but knew the ultimate risk was death.1:55pm: The court will be resuming at 2pm, following its lunch break.
2:01pm: The trial is now resuming. Nicholas Johnson KC says there is one thing he overlooked from the morning's evidence. He asks Lucy Letby why she said "blotchiness" rather than "mottling" in part of her police statement. "I think they are interchangeable," Letby tells the court.
2:06pm: Asked if staffing levels or mistakes had contributed to the collapse of Child B, Letby says she does not know what caused Child B's collapse. She says she does not recall Child B's father lying on the floor following Child B's collapse. A text message from Letby includes:...'Dad was on the floor crying saying please don't take out baby away when I took him to the mortuary, it's just heartbreaking." Letby says she does not recall that. Letby says in this case, she did not want to care for Child B so soon after the death of Child A, as unlike the Liverpool example she had been taught of 'getting back on the horse' (Mr Johnson's words) and being back in nursery room 1, this was with the same family. Letby accepts Child B did well on the day shift of June 9.
2:11pm: Letby is asked if Child B's parents 'stood guard' in the unit following the death of twin, Child A.
Letby: "They were very much present on the unit and we allowed for that." A diagram for the night shift of June 9-10 shows Letby was in nursery room 3 for that night shift, looking after two babies. Child B was in room 1. Letby says she "got on well" with all her nursing colleagues. Letby recalls evidence from court by a nurse colleague on March 21, in which Letby had said working in nurseries 3 and 4 was "boring". Letby tells the court: "I have never been bored [at work], I would never describe my work as boring."2:24pm: Mr Johnson goes through the timeline of Child B's events. A message from Letby to Yvonne Griffiths said: "...Hard coming in and seeing the parents". Mr Johnson says she is "engaged in chit-chat with a friend" between 8.41pm-9.10pm on the night shift in a social context. Letby says that sort of conversation was not limited to just her. Mr Johnson says further messages are exchanged between 9.12pm-9.32pm. Letby says "all members of staff use their phones on the unit". She says it was "accepted". She says she cannot comment for the whole unit, but her designated babies were being cared for. She says she does not believe there were staffing issues - "I can't see what's going on with the other babies [at this time]." Further messages are exchanged involving Letby, some in a social context, up to 10.28pm. Mr Johnson says in the middle of the block of messages, Letby signs for medication for a baby at 10.20pm. Letby says she didn't use her phone in clinical areas. A "further block of messages" are exchanged on Letby's phone between 10.38-10.59pm.
NJ: "Were you bored?"
LL: "No."
NJ: "As a matter of fact, do you text a lot when in [room 3]?"
LL: "I text regardless where I am on shift."
NJ: "Even with an ITU baby [in room 1]?"
LL: "Yes, and I think everyone else would say the same if they were honest."2:32pm: Letby says she was working in nursery 1 "at points" during the shift. She accepts that following Child B's collapse, she was in room 1. A document for a TPN bag and lipid administration is signed by Letby, at 11.40pm on June 9. Letby says an observation form at what appears to be 0010 has what Letby accepts could be her handwriting. It is similar to the writing in the next column, which is initialled by Letby. A blood gas record is shown for 12.16am. Letby accepts she is there at that time as two nurses are needed to carry out the test.
2:45pm: Letby says she was "unsure" whether she or a colleague had alerted the other to Child B's deterioration.
LL: "I can't sit here and say definitively which way now, no."
NJ: "You injected [Child B] with air, didn't you?"
LL: "No I didn't." Mr Johnson asks about Child B's appearance - Letby had earlier told her defence Child B "becoming quite mottled", "dark", "all over". Letby was asked if she had seen that mottling before. "Yes, it was like general mottling that we do see on babies," adding: "It was not unusual" but it was a concern, in light of Child A's decline the night before. Letby tells the court the mottling was more pronounced than usually found. In police interview, Letby had said the mottling was more than seen on Child A, who was pale centrally. "It was darker". Letby also said there was a "rash appearance". Letby tells the court it was a "more pronounced mottling", but was still mottling.
NJ: "Are you saying this was normal?" Letby says it was not normal, but something which would be seen. It was "more pronounced than general mottling". She says it "came very quickly", and in the context of Child A, everyone "acted very quickly". Mr Johnson asks why a doctor asked for someone to get a camera.
LL: "In view of what had happened to [Child A] the night before...we did not want to take any chances." Child B's mother describes the mottling event, and the consultant had "never seen this before", and the mother was "surprised" at this. "Do you accept what [Child A and B's mother] said?"
LL: "I accept there was mottling, yes." She says she does not recall the consultant saying that, as she was not there when it was said. Letby tells the court she went "immediately" to get a camera, and when she returned, the mottling had gone.2:49pm: A doctor had said Child B was a "very pale, dusky colour", and then developing widespread blotches...patches of a purpley-red colour. Letby said she was not there at that point, as she may have been getting the camera. She says she did not see that on Child B. She says no conversation was ever had about that. The judge asks if there was anything that could have led the doctor to be mistaken in her description.
Letby: "No, I just saw mottling." Letby says the mottling was purpley-red.3:00pm: Another doctor had described a blotchiness "to one side". Letby says she did not "take over care" of Child B, from a senior nurse of 20 years experience. She says the senior nurse was busy with the family. The court is shown Letby is co-signer for a number of medications following Child B's collapse, with the senior nurse. Letby denies suggesting antiphospholipid syndrome was a cause of Child B's death. Mr Johnson asks if Letby accepts Child A and Child B had air administered.
LL: "No."3:15pm: The trial is resuming following a short break.
3:25pm: Mr Johnson turns to the case of Child C. Letby is asked to look at her defence statement. Letby recalls she did not believe she was in room 1, and cannot recall how she ended up in room 1 - possibly it was as a result of Child C's alarm going off. Letby, in her statement, said she had been involved in speaking to the family afterwards, but not to the extent Child C's mother had said. Mr Johnson said a nurse had given evidence to say Letby had to be removed from the family room after Child C died.
Mr Johnson says Letby's "vague" recollection of events is untrue.
LL: "I don't agree with that."
NJ: "I'm going to suggest you enjoyed what happened, and that was why you were in the family room."
LL: "No." Letby is asked why she did not remember Child C in police interview. Letby says she remembered once provided with further details. She adds: "I don't know how [child C] died." She rules out staffing levels, medical incompetencies, or someone making a mistake.3:27pm: Mr Johnson says this is a case where one of the nursing notes, by Yvonne Griffiths, was 'misfiled' to a different baby, and was, after Child C died, refiled back to Child C. Mr Johnson asks Letby if nursing notes, timestamped by their start and end, are editable.
Letby: "No." The court hears because of this, the note had to be re-entered into the system.3:35pm: The rewritten note is shown to the court. The note is for the June 12 day shift. It includes: '...no apnoeas noted and caffeine given as prescribed. Longline inserted by Dr Beech on second attempt...[Child C] unsettled at times soothes with pacifier and enjoyed kangaroo [skin-to-skin] care with parents." A nursing note by Joanne Williams is shown to the court for Child C on the day shift: '...[Child C] very unsettled and fractious...[Child C] taken off CPAP while out having skin to skin with mummy. Calmed down straight away with mummy...' Letby agrees this was a "positive picture" for Child C. Child C was on CPAP breathing support to 10am, then was taken off it for a couple of hours, then was on Optiflo breathing support for the rest of his life.
3:55pm: Mr Johnson moves on to the shift in which Letby was present. A shift rota is shown to the court, showing Letby was looking after two babies that night on June 13. She was in nursery room 3, with Child C in room 1 that night.
Mr Johnson says this was another shift when Letby had "migrated" to room 1.
Letby: "Yes, in response to [Child C's] care needs." She says she has no recollection of going to see Child C prior to his collapse. Letby says she was unhappy at being in room 3 for that shift - as opposed to room 1 - but that was the decision of the prior shift leader. Letby's nursing colleague had said Letby's designated baby in room 3 needed attention, after Letby had asked if she could be redeployed to room 1 that night.
Letby: "Yes, [they] did need attention and I gave [them] attention."
Letby had sent a message to Jennifer Jones-Key: "I just keep thinking about Mon. Feel like I need to be in 1 to overcome it but [colleague] said no x"
JJK: "I agree with her don't think it will help. You need a break from full on ITU. You have to let it go or it will eat you up i know not easy and will take time x"
LL: "Not the vented baby necessarily. I just feel I need to be in 1 to get the image out of my head, Mel has said the same and [colleague] let her go. Being in 3 is eating me up, all I can see is him in 1" "It probably sounds odd but it's how I feel X"
JJK: "Well it's up to you but don't think it's going to help. It sounds very odd and I would be complete opposite. Can understand [colleague] she trying to look after you all"
LL: "Well that's how I feel, from when I've experienced it at women's I've needed to go straight back and have a sick baby otherwise the image of the one you lost never goes. Why send Mel in if she's trying to look after us, She was in bits over it. X "Don't expect people to understand but I know how I feel and how I've dealt with it before, I've voiced that so can't do anymore but people should respect that X"
JJK: "Ok x
JJK: "I think They do respect it but also trying to help you. Why don't you go in one for a bit. X"
LL: "Yeah I've done couple of meds in 1. I'll be fine X"
JJK: "It didn't sound like you would be? Sorry was eating my tea x"
LL: ...Forget i said anything, I'll be fine, It's part of the job just don't feel like there is much team spirit tonight X"
JJK: "...I'm not going to forget but just think your way to hard on yourself. It is part of the job but the worst part but I do believe it makes us stronger people."
LL: "Unfortunately I've seen my fair share at the women's but you are supported differently & here it's like people want to tell you how to think/Feel. Anyway. Onwards & upwards. Just shame i'm on with Mel & [colleague].Sophie in 1 so haven't got her to talk to either."
JJK: "Work is work. A lot of the girls say women's don't support and tell them to get on with it. I think they don't mean to tell you thou and were over caring sometimes Yeah that's not good but you got Liz x"
LL: "Women's can be awful but I learnt hard way that you have to speak up to get support. I lost a baby one day and few hours later was given another dying baby just born in the same cot space. Girls there said it was important to overcome the image. It was awful but by end of day i realised they were right. It's just different here X ". Anyway, forget it. I can only talk about it properly with those who knew him and Mel not interested so I'll overcome it myself. You get some sleep X" Letby accepts there were two babies in room 1, but does not accept she was specifically wanting to look after Child C. Letby tells the court: "It wasn't about me wanting to get my own way." Letby accepts she was upset, "just generally", that her feelings weren't being considered by a colleague and Melanie Taylor.
Mr Johnson says if this was the Melanie Taylor who Letby had said "potentially" caused a child's death.
Letby: "Potentially, yes."
JJK: "That's a bit mean isn't it. Don't have to know him to understand we've all been there. Yep off to bed now x"
LL: "I don't mean it like that, just that only those who saw him know what image i have in my head X "Forget it. Im obviously making more of it than I should X" Letby tells the court she had hoped Jennifer Jones-Key would have been more understanding to how she was feeling, and was frustrated, and the conversation was not going anywhere, so she wanted to "leave the conversation".3:58pm: Letby says colleague Sophie Ellis was the least experienced member of staff on that shift and "did not have the skills for the job" of looking after small, premature babies in room 1. "I did not think she was qualified for the job...She did not have the skills for the premature babies [in room 1]." She denies that Sophie Ellis did anything to cause Child C's collapse.
Mr Johnson: "She had something you wanted?"
Letby: "No."4:06pm: The court hears Sophie Ellis's statement saying when she entered room 1, Letby was by Child C's cotside, saying: "He's just dropped..his heart rate/saturations" or words to that effect. The court is shown the neonatal schedule for the night shift of June 13-14, 2015. Letby is shown recording observations for her designated babies, and made medication prescriptions for babies not in room 1. Letby says the medications for those babies would have been drawn up in room 1. "They could not have been done in a special care nursery". Letby says if Sophie Ellis has documented correctly, there would have been no air in Child C's stomach after an aspiration was made for the baby's feed. Letby denies taking, in Mr Johnson's words: "an opportunity to sabotage [Child C]."
4:13pm: In police interview, it is put to Letby that Child C collapsed six minutes after she sent the last of her text messages.
Letby: "I don't recall where I was at the time" - Letby says she may have been in a nursing station before going into room 1. Letby said she did not recall being cotside, but accepted Sophie Ellis's account at the time it was put to her by police. "The death of [Child C] was very memorable, wasn't it?"
"Yes."
Friday 19th May 2023
Cross-examination of Lucy Letby by Nick Johnson KC - Day 3
Children C & DChester Standard Live Reporting
9:08am: Yesterday, jurors received an answer to their question as to when the trial would be over. The judge, Mr Justice James Goss, said a precise answer could not be given, as that partly depended on how long their deliberations would be when they go out to consider the verdicts, but he said the latest expected date would be the end of July. He added he was hopeful it would be concluded sooner than that. The information would be relayed to the respective jurors' employers informing them of this.
10:23am: The courtroom at Manchester Crown Court is filling up with legal teams and members of the press. Lucy Letby has already arrived. The trial is expected to resume at 10.30am. The court also heard Lucy Letby agree with prosecutor Nicholas Johnson KC that two babies had been 'poisoned' with insulin on the neonatal unit - Child E and Child L. She denies those babies were targeted and denies that she was the one who poisoned them.
10:40am: The trial is now resuming, following a short legal discussion. Nicholas Johnson KC, for the prosecution, is continuing to cross-examine, and is asking Lucy Letby questions in the case of Child C.
10:44am: Mr Johnson says text messages were exchanged between Letby and Jennifer Jones-Key between 11.01pm and 11.09pm. Letby says she does not accept she was in room 1 at the time of Child C's collapse. She says she has "no memory" of it. Nurse Sophie Ellis had said she was in room 1 at the time, and Letby said in police interview, based on that, she was in room 1.
Letby says she "disputes" that, as she has "no memory" of it.
"Do you dispute being born?" Mr Johnson asks.
"No." Letby replies.
NJ: "But you have no memory of it?"
LL: "No."10:50am: Letby is asked why she let a band 4 nursery nurse look after her designated baby.
Letby says it's "not unusual" for band 4 nurses to assist her in her duties.
LL: "I have no memory of that".
NJ: "Did you have something better to do?"
LL: "No."
Mr Johnson says the text at 11.01pm sent by Letby to Jennifer Jones-Key meant she must not have been in a clinical area, and would not have had time to feed her designated baby in room 3.
LL: "I can't answer that."
Mr Johnson says it took her out of the nursing area.
Letby said she would have been "in the doorway" of the unit.11:00am: Mr Johnson says Melanie Taylor, in evidence, described Letby as "cool and calm". Letby does not dispute that. She disputes saying to the Melanie Taylor that Child C had had a brady, as she has no memory of it. Notes by Dr Katherine Davis are shown to the court for Child C's collapse. At the time of arrival, "chest compressions in progress"
"Occasional intermittent gasps noted". "Unable to pass ET Tube as cords++" - the court hears the cords were "swollen". Mr Johnson asks Letby if it was a "theme" that when doctors went to intubate, they had difficulties, with swollen cords and/or bleeding. Letby accepts that was the case. She denies putting anything down Child C's throat.
Mr Johnson: "Do you agree something caused [Child C]'s stomach to dilate before the collapse?"
Letby says the stomach dilation "could have been caused by the Neopuff resuscitation".
Letby is asked if she had seen the kind of decline as seen by Child C before.
Letby says she has, but not the way Child C 'clinged to life'.
NJ: "You enjoyed the aftermath of this, didn't you?"
LL: "No."
NJ: "Why were you so keen to spend time with the [Child C] family as they cradled their drying child?"
LL: "I don't agree with that, I wasn't there a lot of the time."
Letby disputes being "repeatedly" in the family room afterwards, adding: "I don't recall [colleague] having to pull me out [of there]." She disputes the statement made by her colleague.11:03am: Letby is asked "what useful function" she was contributing to the family during the "dreadful situation" they were going through. Letby said she cannot recall, other than gathering the mementos, which is a two-person job. Letby says she would have to see the bereavement checklist charts to see if there was anything she had co-signed, as otherwise she does not recall and has no memory. The judge asks if hand and footprints are collected when the baby is still alive. Letby replies they can be, or after they have passed.
11:05am: Letby denies that she was "enjoying what was going on".
11:11am: Mr Johnson now moves on to the case of Child D. Letby's defence statement said she did not believe she had any involvement with Child D until the baby girl's collapse. Letby says she was affected by Child D's death, as were all staff on the unit. In police interview, Letby had said she could not recall Child D. Letby recalls looking after two babies in room 1 on the night of June 21-22. Caroline Oakley was the designated nurse for Child D and a baby in room 2. Letby accepts "from time to time" she would have been alone in room 1 as Caroline Oakley split her time caring for the two babies between the two rooms.
11:35am: Part of a statement from Child D's mother is read out. Letby disputes she was the nurse who held a phone to Dr Andrew Brunton's ear while resuscitation efforts were going on. Letby says she can recall there was such an incident, as it was talked about after the event. She agrees it happened, but she disagrees it was her who made the phone call. Mr Johnson asks about a series of Countess nursing staff's descriptions of the "unusual" skin discolouration and an 'odd' rash. Some of them said it was something they had not seen before. Letby says she does not dispute the staff's descriptions, but cannot comment on what they did or did not see.
NJ: "Do you still not remember [Child D]?"
LL: "I didn't recall at the time of my police interview, no."
NJ: "Do you remember her now?"
LL: "Yes."
NJ: "Do you remember the circumstances surrounding her death?"
LL: "No." Letby messaged a colleague on June 22: '...[Child D] came out in this weird rash looking like overwhelming sepsis'. Letby said she had not seen the type of rash often before, but she had seen something similar in her training years before. The message added: 'Then collapsed and had full resus. So upsetting for everyone. Parents absolutely distraught, dad screaming' Mr Johnson asks if Letby was lying to police when she said she didn't remember Child D.
Letby: "No." Letby's message added: 'Andrew [Brunton] and Liz [Newby] said it'll be probably be investigated'. Hmm well it's happened & that's it. Got to carry on...' Mr Johnson said he had earlier asked if that was Letby's reaction to Child D's death.
Letby: "I don't think it was meant in the context you are suggesting...we've got to move forward...it's not meant to be any insensitivity to the parents or [Child D]."11:54am: The trial is resuming following a short break. Mr Johnson asks about the Facebook search for Child D's mother on June 25, 2015. He asks how he remembers the name of Child D's mother if he did not recall Child D in police interview in 2018. Letby says she recalled the name of the mother in June 2015.
NJ: "You have got a good memory for names?"
LL: "Yes."
NJ: "You carry them in your head?"
LL: "Yeah."
NJ: "Would you say you've got a good memory?"
LL: "Yeah."12:06pm: Letby is asked about messages she had exchanged with Minna Lappalainen on June 26 in which she said: "What I have seen has really hit me tonight." Minna Lappalainen suggests a counsellor for Letby.
LL: "I can't talk about it now, I can't stop crying..." The reply suggests Letby take time off and consider if she should be at work during this time. Letby replies she has to keep carrying on working after saying "I just have to let it all out".
NJ: "This was a very memorable time of your life, wasn't it?"
LL: "Yes." Messages between Letby and a colleague are exchanged. The colleague said there was "something odd" about what had happened. Letby is asked if 'What do you mean?' was what she really thought, as per her response.
NJ: "Were you worried that people were starting to put two and two together?"
LL: "No." Letby had messaged: "Odd that we lost 3 in different circumstances?" Letby tells the court the circumstances were different. The colleague: "I dunno. Were they that different? "Ignore me. I'm speculating." The colleague says there was talk of doing a joint post-mortem for three babies who had died. Letby searched for the father of Child D on October 3, 2015. "You didn't really forget [Child D], did you?"
LL: "I didn't recall specific details in interview."
Mr Johnson says Facebook does not archive the name searches beyond a certain number, so every time Letby searched a name, it would be from memory.
Letby accepts that. Letby says Child D "did not have appropriate treatment at the start of her life" and that "may have had an impact" on her later in life.
NJ: "The [lack of antibiotics early on] don't cause an air embolus, do they?"
LL: "No."12:10pm: Letby is asked if Caroline Oakley's notes showed Child D was stable prior to the collapse. "Do you accept the evidence that [Child D's designated nurse in room 1] Caroline Oakley was on a break when [Child D] collapsed?" Letby says she cannot recall. "I cannot say either way because I don't know."
"Do you want to make any further comment about it?"
"No." Letby accepts that if Caroline Oakley was on a break, the other nurse in room 1 was herself. Kathryn Percival-Ward had also given evidence saying Caroline Oakley was on a break, Mr Johnson tells the court.
NJ: "Do you accept that Caroline Oakley was on a break?"
LL: "Yes."12:14pm: The neonatal schedule is shown to the court.
Mr Johnson says there is nothing for Letby's name between 1am and 1.30am - the latter when Child D collapsed. A blood gas record is shown for Child D at 1.14am.
NJ: "That was done by you, wasn't it?"
LL: "I don't know."
NJ: "That's your writing, isn't it?"
LL: "It could be?" Mr Johnson asserts it is.
Letby: "It looks like my writing, yes." Mr Johnson asks why it isn't signed by her. "It's just an oversight, like the next line [which also isn't signed], it's an error."12:24pm: Observations for Child D are shown, including readings at 1.15am. It is signed by Caroline Oakley. Mr Johnson says Caroline Oakley had told the court she got those details for the 1.15am observation "from the girls". Letby says she does not remember that bit of evidence. Letby says she does not recall who was looking after Child D when Caroline Oakley was on her break. An infusion chart is shown where Child D is given a saline bolus. Letby says the handwriting in the 'date and time started' column is likely to be hers. "Did you take the opportunity while Caroline was out to sabotage [Child D]?"
"No."
Mr Johnson says "You were standing over her when the alarms went off, weren't you?"
LL: "I don't recall."
Mr Johnson says who the 'candidates' could have been. One of the nurses says she wasn't there in evidence. Another is Kathryn Percival-Ward, and Letby agrees she could have been there. Another nurse is discounted. Letby says she cannot recall if it was her who was in room 1. A fluid balance chart is shown to the court, with the note 'oral secretions++'. Letby says the handwriting "could" be hers. Letby said it could have been something she had documented alongside Caroline Oakley. Mr Johnson suggests Letby was "babysitting" Child D. Letby adds she "cannot comment" if she had been in nursery room 1 throughout. The neonatal schedule is shown to the court. Letby denies she has "ever" falsified paperwork to make it look like she was doing one activity at one time when doing another.12:27pm: The schedule shows Letby was involved in giving medications to Child D before the second collapse at 3am.
NJ: "Do you remember that?"
LL: "No." An infusion for Child D is made by Letby and Caroline Oakley at 3.20am.
NJ: "[Child D] died because you injected her with air, didn't you?"
LL: "No, no...I did not give her air."12:28pm: Letby said she was looking after other babies, "not just [Child D]".
LL: "I tried to be as co-operative as I could be [to police in interview]."12:32pm: Letby asks for a break. Mr Johnson says he just requires to tidy up something which should take two minutes, in the case of Child C. He refers to the bereavement checklist. Letby says hand and footprints were taken before death in certain cases. Mr Johnson says the checklist is 'for staff following neonatal death'. The judge says there will be an early lunch break, and court will resume at 1.45pm.
2:07pm: We have been told court will not be resuming until 2.30pm.
2:41pm: Legal teams and members of the public and press have now returned to court.
2:50pm: The judge, Mr Justice James Goss, has entered the courtroom. The judge is informing members of the jury the trial will not resume today. He says the adjournment is for reasons that should not concern them. The next day the trial will be held, as planned, will be Wednesday, May 24. Members of the jury are being reminded not to conduct independent research or communicate with anyone involved in the case.
Monday 22nd May 2023 - no court (planned)
Tuesday 23rd May 2023 - no court (planned)
Wednesday 24th May 2023
Cross-examination of Lucy Letby by Nick Johnson KC - Day 4
Children E, G, & HChester Standard Live Reporting
10:36am: The judge, Mr Justice James Goss, has entered the courtroom. The trial will now resume.
10:43am: Nicholas Johnson KC, for the prosecution, will now cross-examine Lucy Letby. He first asks about the 'conspiracy gang' of four doctors, as Letby previously said there was in the Countess of Chester Hospital last Thursday. He clarifies a minor matter about it. Mr Johnson KC asks about the case of Child E. Letby says: "Possibly yes" to the question if there was medical incompetence that led to Child E's death, in that the night shift team "could have reacted sooner" to the child's bleed. She says once Child E was bleeding at 10pm, a transfusion could have been made sooner. She says the "collective team" were responsible.
10:53am: Letby says it was "an important thing to know" that plumbing issues were a potential contributory factor to the decline of babies' health in the unit. She said "raw sewage" would come out of the sinks in nursery room 1, as flowback from another unit. Mr Johnson asks if Letby ever filled in a Datix form for that. Letby says she did not. Mr Johnson says Letby did fill in a Datix form for Child E. The form is shown to the court. It is dated August 4, 2015, at 5.53am, which is when the form was signed and filed. It is classed as a 'clinical incident'. The risk grading was 'high potential harm'. Letby says she is "not sure about that", as it also says 'Actual harm: None (No harm caused). It refers to the death of Child E at 1.40am. 'Description: Unexpected death following GI bleed. Full resus unsuccessful. Time of death 01:40.' The baby's history is recorded in the events leading up to his death. It was filled in by the incident review group panel. Letby's input on the panel is reporting the incident on the first page of the nine-page report.
10:56am: Letby is asked if she remembers sending a text message to Jennifer Jones-Key saying it was "too Q word" on August 2, 2015. Letby says she cannot recall, but accepts that would be something she could send. The 'Q word' is 'quiet', the court hears. Letby says "there is always something to do", but "sometimes they can be long nights if you haven't got many babies". She says she enjoyed being busy "when it was managed".
11:01am: Letby is asked why she, and not Child E's designated nurse Melanie Taylor, signed a correction to a prescription for Child E. Letby says it's standard practice for two nurses to administer prescriptions, and corrections on the form are not based on seniority. She agrees she was keen to raise issues if they needed correcting.
NJ: "Had you fallen out with Melanie Taylor by this stage?"
LL: "No." Letby denies she had fallen out with anyone. She agrees she had confidence in her clinical competencies.
NJ: "Do you agree you were a cut above some other nurses, including Mel?"
LL: "No."11:08am: A nursing note for Child E from the evening of August 3, 2015 is shown. Letby agrees he was progressing well, although he needed insulin. Letby agrees Child E at this stage showed no sign of gastro-intestinal problems. A rota is shown to the court, showing Letby was the designated nurse for Child E and Child F in room 1. No other babies/nurses were allocated in that room that night.
Letby is asked if there was anything wrong with this arrangement.
Letby: "No."
Mr Johnson says when Letby was giving evidence to Mr Myers, she said when the mother arrived at the unit, she was "bringing milk".
Letby says she does not recall from her memory.
Mr Johnson says that was what she said on May 5.
Letby: "I can't recall right here right now."
Letby says she cannot remember it specifically, but accepted that version of events. "I don't have any clear memory."
Mr Johnson refers to the transcript from that day, in which Letby told Benjamin Myers KC she believed Child E's mother had arrived at the unit bringing expressed breast milk.
Letby says: "I said 'I think' she brought expressed breast milk." She says it's the same thing.11:15am: Mr Johnson asks about the significance of 9pm that night.
Letby says: "I don't know what you mean."
Mr Johnson says it's the mother's evidence that she knew Child E was due a feed at 9pm, so came down to the unit for that feed. Mr Johnson says Letby's recollection that Child E's mother brought milk with her fixes the time as being 9pm.
Letby: "I don't agree."
Mr Johnson asks about the 16ml 'mucky aspirate', which Letby agrees was taken before 9pm. Mr Johnson asks where the milk for the 9pm feed was coming from.
Letby says the milk would come from the milk fridge in nursery room 1. She says she does "not remember" where the milk would come from for this feed specifically. No feed was recorded for 9pm. Mr Johnson says the SHO did not record no feed for 9pm, having said in evidence that would be the sort of thing he would record for a baby. Letby says sometimes doctors don't record such notes.11:25am: Letby is asked why the 'large vomit of fresh blood' is not recorded on the observation chart for 10pm.
Letby says she recorded it in her nursing notes, and Dr David Harkness was present when it happened.
Letby is asked why she waited over an hour for the observation of the aspirate to be raised with the doctor.
LL: "I don't recall speaking to a doctor", but Letby recalls speaking to an SHO on the phone about it. Letby says there was no observation of blood prior to 10pm.
NJ: "Was [Child E's mother] telling the truth about you?"
LL: "In what sense?"
NJ: "In the sense of what you said to her - when she says she came down to see her boys, she saw [Child E] with blood around his lips." Child E's mother's illustration of what she says was present on Child E's lips is shown to the court.
NJ: "Did you ever see anything like that?"
LL: "[Child E] did have blood like that - after 2200." Letby adds "there was no blood prior to that." Letby accepts she was alone in room 1 when the mother came down. She says that would have been around the handover time at 8pm.
NJ: "You are not telling the truth about that, are you?"
LL: "Yes I am." Letby says she does not accept causing an injury to harm Child E. She denies at any stage 'having a fall out' with Child E's mother. Letby says she has never seen a baby with blood like that around her mouth in her career. She agrees it was "wholly exceptional". She denies telling Child E's mother the cause of the bleed was via insertion of the nasogastric tube. She says the insertion could cause "a small amount of blood" from the tube.11:29am: Letby is asked if she recalls telling police in the case of Child N that NG Tubes can cause bleeding. Letby says it does cause blood, but not in the mouth. Mr Johnson says Letby has said that previously it can cause oral bleeding.
Letby: "Ok." She denies saying that happened in this case. She says "medically speaking", "any baby" could have a bleed like the sort seen by Child E. A text message from Letby to Jennifer Jones-Key is shown: "...He had massive haemorrhage could have happened to any baby x" Letby says "at the time" it was thought Child E could have NEC, and "any baby could have had the condition [Child E] had."11:37am: Letby is asked to look at her defence statement. She says Child E's mother had come down with some expressed milk. The statement is dated February 2021. Letby, in her statement, said "This may have been later than 2100". Mr Johnson says Letby is now ruling out a time before 2200. Letby says she cannot say it definitively, but there was no blood prior to 2200. Letby is asked why she did not mention the vomit when blood went down the NG Tube in her defence statement. Mr Johnson says Letby is lying by adding additional detail afterwards. Letby denies this. Mr Johnson asks about the 'mucky aspirate' for Child E, asking if that is 16ml of 'bile', as per Letby's defence statement. Letby says there was bile in the mucky aspirate. Mr Johnson says there is a difference between 'bile-stained' and 'bile'. Letby accepts 'there was 16ml of bile' in her defence statement is "an error".
She is asked why she put that in, in those terms.
LL: "I don't know." Letby says this is a clarification of her earlier statement.
NJ: "You are lying, aren't you?"
LL: "No."11:40am: The defence statement also refers to 'blood in the nappy' for Child E after he died. Mr Johnson says if that has been heard in her evidence. Letby says she cannot recall. Letby says it is written in her nursing notes, and nothing was done about it as Child E was deceased by that time. Letby is asked to look at her nursing notes.
11:57am: The court is resuming following a short break, during which time Letby has had chance to look at her nursing notes.
12:04pm: Mr Johnson says Letby's nursing notes for Child E, as read by Letby during the break, do not record blood in the nappy. Letby says she could not recall her notes specifically at this time. Mr Johnson reads about what other medical staff observed following Child E's collapse. Dr David Harkness recorded, for Child E's observations following the collapse, 'kind of strange purple patches that appeared on the outside of his tummy'. Letby says it was purple, but not patches. Letby said the other parts were 'more pale' than the pink described by Dr Harkness. Dr Harkness said he'd only ever seen it before with Child A. Letby disagrees. She says it was "not the same". Asked to explain the differences between the two, Letby says it was a "solid block of purpleness" for Child E, and a "more mottled look" for Child A. Letby agrees it was over the abdomen, but disagrees the purple patches moved around.
12:06pm: Mr Johnson reads through another doctor's observations, who said she had not seen the discolouration, but Dr Harkness was "animated" when he was describing what he had seen to her. Letby says she was not there for any conversation between the two of them.
12:16pm: Letby is asked to read her retrospective nursing note for Child E, which described Child E's collapse and subsequent decline until he died in his parents' arms at 1.40am. The note would have been made with reference to medical notes, Letby tells the court. Letby is asked to look at an observation chart and a blood gas chart. Letby says when things are going on, it would be standard practice to write, also, on the back of handover sheets or spare bits of paper. Letby is asked about a "purple band" of discolouration she had recorded for Child E. In her police interview, Letby accepts struggling to recall the size of it at that time. Mr Johnson says for May 5's evidence, Letby said it was a "red horizontal banding across his abdomen", and only on the abdomen. Letby agrees with Dr Harkness it was on the abdomen, but does not agree with Dr Harkness's observation it was patches.
12:21pm: Letby is asked to look at a chart showing aspirates for Child E, which included 'minimal aspirates' prior to the collapse. Letby agrees that showed no signs of gastro-intestinal issues for Child E, until the 9pm reading of 16ml 'mucky' aspirate, in her writing. Letby "cannot recall" why Belinda Simcock had written in the 10pm aspirates column. Letby "assumes" the blood came out following those 10pm readings. "Why was Belinda there at all?"
"I can't say for sure." Letby says Belinda had come to assist for the 16ml aspirate observed an hour earlier. Letby says she "cannot say" why Belinda was carrying out observations at that time.12:28pm: Letby says she "cannot explain" why the blood aspirate is not recorded in the aspirate chart, but is in her nursing notes. Letby is asked to read a note on the schedule for Child E, in which it is said Belinda Simcock gave a feed to a child in room 2 at 10pm. Letby says she cannot recall why Belinda Simcock had come to room 1 for the 10pm readings. Mr Johnson asks if Belinda Simcock was brought in to sign paperwork at the time of the collapse to cover for Letby's actions. Letby denies this. Letby said Belinda Simcock had carried out the drip readings for Child E, and signed it, as specific information like that is not passed on from one nurse to another.
12:31pm: Letby is asked if she recalls who rang Child E's mother when Child E collapsed. She said it would have been a "collective decision" to contact the midwifery staff. Letby accepts Child E's mother made a phone call at 9.11pm, but does not accept the evidence of the conversation about Child E 'bleeding from his mouth' and there was 'nothing to worry about'. Benjamin Myers KC, for Letby's defence, rises to say Letby cannot say what was or was not said in a phone call she was not part of.
12:37pm:
NJ: "You killed [Child E], didn't you?"
LL: "No."
NJ: "Why in the aftermath were you so obsessed with [Child E and F's mother]?"
LL: "I don't think I was obsessed." Letby says she "often" thought of Child E and Child F.
Mr Johnson says the name of Child E and F's mother was searched for nine times, and the name of the father once.
Letby said she searched "to see how [Child F] was doing."
One of the searches was when Child F was on the neonatal unit.
Letby said the other searches were made after Child F had left the unit, so "collectively" what she had said was correct.
Mr Johnson says Letby was looking for the family's reaction.
Letby disagrees.
One of the searches is on Christmas Day. "Didn't you have better things to do?" Letby said the family were on her mind.12:41pm: Mr Johnson tells the court he is now looking at the case of Child G. He will go 'out of sequence', chronologically, and deal with Child F at a later point. Letby says she cannot recall what Child G's due date would have been [Child G having been born at a gestational age of 23 weeks and 6 days on May 31, with the date of one of the events "not standing out" to her. A message from Letby's phone to a colleague: "Due date today!" Letby says she knew at the time [September 21, 2015]. Letby says the date of the event for Child G was "a coincidence".
12:43pm: Letby says Child G had "extreme prematurity" which had complications requiring additional care. Letby disagrees that Child G was "fine" by the time she came to the Countess of Chester Hospital, saying she had a number of ongoing issues.
1:00pm: Letby denies that Child G was ready to go home by the date of the first event on September 7, saying babies in the special care room, nursery 4, can still be there for several weeks. Letby says Child G had a number of previous problems including relating to feeding, and had sepsis. Letby says Child G was on oxygen and had feeding issues by September 7, 2015. Mr Johnson asks Letby to look at Child G's nursing records for her days leading up to her projectile vomit. Letby agrees there is nothing "unusual" in those days. Feeding charts are shown for Child G for September 5 and 6. Child G is being fed expressed breast milk via the NGT or bottle. Letby agrees the picture is looking good for Child G from these charts.
Mr Johnson says the feed at 11pm on September 6 would not have been done twice by mistake.
Letby says she has never suggested that has happened. Letby agrees the observations for Child G before 2am on September 7 are "good".
NJ: "You knew this was day 100 of [Child G's] life, didn't you?"
LL: "Yes."
NJ: "It was a big day for her."
LL: "Yes." Letby agrees she and other nurses would celebrate 100-day-old babies on the unit, and a banner had been prepared to mark the occasion. A staffing rota for the night shift of September 6-7 is shown to the court. Letby is in room 1 as the designated nurse for one baby, and Ailsa Simpson is the designated nurse for one other baby in room 1. A nursing colleague is in room 2 as the designated nurse for Child G. Letby rules out staffing levels or staff incompetence as a contributory factor in Child G's death. Asked if anyone had made a mistake, Letby says "potentially", Child G had been overfed by a nursing colleague, but that was not what she was saying had happened.
Letby: "I can't say for definite that didn't happen. I'm not saying she did do that, but it is a possibility." Letby says it is a "possibility" the amount of milk was mismeasured when calculating the feed.
NJ: "Are you suggesting it's a realistic possibility?"
LL: "No."2:09pm: The trial is now resuming following its lunch break.
2:17pm: Nicholas Johnson KC continues to cross-examine Lucy Letby in the case of Child G. Letby says it was a "possibility" Child G was overfed by a nursing colleague, but adds: "I don't believe that happened." Mr Johnson says to overfeed Child G twice as much would have taken twice as long. Letby says 45mls of milk feed would take around 15-20 minutes. Letby refers to medical experts Dr Evans and Dr Bohin that overfeeding was a possibility. Mr Johnson describes what Letby had seen, including that Child G's abdomen was "firm and red", with the sight of that and vomit on the floor leaving her "shocked". "That was a clear recollection you had last week, giving evidence?" Letby says that happened at approximately 2.15am. Her nursing note is shown to the court: '[Child G] had large projectile milky vomit at 0215. Continued to vomit++. 45mls milk obtained from NG tube with air++. Abdomen noted to be distended and discoloured. Colour improved few minutes after aspirating tube, remained distended but soft...to go nil by mouth with IV fluids...' Letby says she disagrees with the evidence of Dr Sandie Bohin, saying a pH reading of 4 can be obtained from milk aspirated from the stomach.
2:27pm: A photo of Child G's cot, with circles marking where the vomit fell outside of the cot, is shown to the court. Letby is asked to look at her police interview for Child G. Letby said it was in her cot.
NJ: "This was an extraordinary vomit, the likes of which you had not seen in your career."
LL: "I have, but not in neonates." Letby says it's an "oversight" she had not mentioned the extent of the vomit in police interview. Letby says Child G was "still vomiting" when she went in to see Child G with Ailsa Simpson.
NJ: "You were not there with her, were you?"
LL: "Yes I was." Letby is asked to look at her police interview. She says at the time of the vomit she did not remember where she was, then went into the room where Child G was. Letby is asked why there is no mention of Ailsa Simpson in the interview. Letby says she was describing her own response. The neonatal schedule is shown to the court for Child G. Mr Johnson says Letby deliberately misstated the time at which Child G had her vomit [at 2.15am], and says it was different. Letby disagrees.2:33pm: Mr Johnson refers to Dr Alison Ventress's notes 'Called to r/v [Child G] at 2.35'. He says that is an accurate time, and Letby had misstated the time so Letby's colleague could instead be blamed for overfeeding, and Letby overfed Child G.
Letby: "That's not true." Mr Johnson asks where the air came from before 'Neopuffing'. Letby says she cannot say without looking at the nursing notes. Letby's note: '...45mls milk obtained from NG Tube with air++...' The note does not mention Neopuffing. Letby says that is "an oversight".
Mr Johnson: "The truth is that you injected [Child G] with milk and air, didn't you?"
Letby: "No."2:41pm: Letby is asked to look at her second police interview for Child G. In it, Letby said air had got in through the feeding syringe. She tells the court it had been suggested to her as a possibility. Mr Johnson refers to Child G's 3.15am collapse, with Dr Alison Ventress recalling 'blood-stained fluid coming up'. Letby denies inserting something into Child G's airway and/or causing the deterioration. Dr Ventress and a doctor colleague said '100ml of air/milk' had been aspirated from Child G following the 6.05am desaturation. Letby says she does not recall the 100mls coming out, and asks if it was documented. Dr Alison Ventress's note is shown to the court. It includes '...NG aspirated as abdo appeared v large ~100mls aspirated...'
Letby: "I don't know how the air got there. It's after Neopuffing." She accepts the note as an account of what happened.2:43pm: Letby is shown nursing notes made for the following day shift by a colleague. Letby agrees there are no signs Child G had a build-up of fluid or air from the notes made.
2:45pm: Mr Johnson refers to the second bout of vomiting on September 21, 2015. Letby said she thought she recalled the mother was there as it was during visiting time. Letby had said she did not believe it was an emergency, and did not recall Child G "going blue". Asked if she agrees with Child G's father that Child G was "not the same" after the first deterioration,
Letby replies: "I can't comment on that, nobody knows their babies like the parents do."2:47pm: Mr Johnson asks why Letby was giving Child G the 9.15am feed on September 21.
Letby: "She wasn't awake and she was due her immunisations." Letby says, "feeding wise", she had no concerns with Child G. She said there was an ongoing issue with Child G's low temperature.2:50pm: For that September 21 day shift, the court is shown the rota, and Lucy Letby was the designated nurse for Child G that day in room 4, along with two other babies. Lucy Letby was also responsible for a fourth baby 'rooming in with parents'.
NJ: "Did it annoy you that you were in nursery room 4?"
LL: "Not at all."
Mr Johnson says that Letby, when giving evidence, aspirating can interrupt digestion.
Letby said when fully aspirating, that can happen. She tells the court on this occasion, NGT feeds would be preferable for babies receiving immunisations as they can be quite unwell after them and may need rest.2:57pm: The court is shown a feeding chart for Child G. A 40ml feed of expressed breast milk was given at 9.15am, signed by Letby. After the feed, there were 30ml 'two projectile milk vomits', Letby noted. Child G also had a large bowel motion, 'loose, watery green', and there was a 'review by Drs'. The note is signed by Letby. She says she cannot recall which doctors carried out the review from that note. The 9am reading is recorded on the observation chart for the temperature. Mr Johnson suggests there are two 'dots' in that column recording temperatures. Letby says she cannot recall what the line is below the dot.
NJ: "Did you go back and cook the charts to make it look like [Child G] was declining?"
LL: "No." Letby says both dots are "in the normal range".
Letby: "I haven't misdocumented anything." Two dots are recorded in the 3am column [when Letby was not on shift], and Letby suggests someone else has misdocumented.3:01pm: Letby's notes for that day are shown to the court. They include... 'at 1015 x2 large projectile milky vomits, brief self resolving apnoea and desaturation to 35% with colour loss. NG tube aspirated - 30mls undigested milk discarded. Abdomen distended, soft. Drs asked to review. Temperature remains low, tachycardiac >18bpm since vomit.'
Mr Johnson says it's "not an innocent coincidence" that Child G deteriorated one hour after being fed by Letby.
Letby: "Yes it is."
Letby is asked to look at her defence statement. It included: "I did not shout for help as I did not think this was an emergency." Letby is asked if she sought to minimise what had happened.
LL: "No."
Mr Johnson refers to Dr Peter Fielding's note. It says: "[Child G] had an episode @~10.20 where she had 2 projectile vomits witnessed by nursing staff...nurse called for help." Letby denies 'minimising' events, saying this was a "self-correcting" event for Child G.3:07pm: Letby sent in a text to her work colleague: '...looked rubbish when I took over this morning and then she vomited at 9 and I got her screened' Mr Johnson says that text has two lies in it. Letby accepts she got the time wrong but says she was not asked about Child G's colour. Mr Johnson says Child G was doing well. Mr Johnson shows a nursing colleague's note from the previous night shift and Letby's nursing note from that day shift. "Any suggestion [Child G] was looking 'rubbish'?" Letby says Child G looked 'pale', but didn't use "rubbish", in clinical notes. Letby denies deliberately falsifying times or making up negative observations for Child G. Letby denies "passing off responsibility to other people", as suggested by Mr Johnson.
NJ: "In fact, you are the person causing all these problems."
LL: "No I'm not."3:30pm: The trial is resuming after a short break. Mr Johnson asks Letby to look at her defence statement for the 3.30pm incident for Child G. Letby said she looked round the screen and saw Child G's monitor was off, she was alone, and behind the screen. Mr Johnson asks if that was correct.
Letby: "Yes." The statement adds Letby wanted the matter of Child G being left alone on the procedural trolley behind the screens by a doctor, but a nursing colleague did not want to report this. Letby agrees it was "an innocent coincidence" that she was the only nurse in the room at this time. Mr Johnson said Letby had told in evidence that Letby was preoccupied with other babies in the room she was caring for, while doctors tried to cannulate Child G behind screens "for some time".3:40pm: The court is shown a neonatal schedule for Child G and other babies for September 21. Letby is recorded as having three duties for other babies in the 90 minutes prior to Child G's collapse. One of the three events was for a differently designated nurse's baby in room 2. Letby says that does not mean she was not preoccupied with the babies, and may have been dealing with their families or other duties. Letby is asked about the event and her looking behind the screen, that Child G was 'dusky, blue and not breathing'. Letby is asked if that was true. "Yes." Letby agrees she picked Child G up, put her in a cot and Neopuffed her. She says the Neopuff equipment would not stretch to the trolley. A nursing colleague "froze" and went to get a separate nursing colleague. Letby said, in evidence, she was "very concerned" by what had happened.
Mr Johnson says one thing not mentioned in the defence statement was Letby moving Child G from the trolley to the cot. He asks why Letby had not mentioned that.
Letby says she cannot say.
Mr Johnson says Letby "took advantage of a situation that presented itself".
Letby: "No."3:51pm: Mr Johnson says when the cannulation process was taking place, Letby must have been in the room. Letby says she would not have been there all the time. One of the charts is shown for a baby that Letby was looking after, with the chart requiring readings that took 'about 5 minutes' to make. Letby says she was "in and out of the nursery all day", on activities that did not require being cotside. She says she does not recall "at any point" being told by doctors they had finished with the cannulation process for Child G. Letby says it would have been "up to the doctors" to remove the screens and make sure Child G was safely back in her cot following the cannulation.
3:58pm: Mr Johnson moves on to the case of Child H. Letby says she does recall Child H, due to the chest drains that were put in place. Letby said chest drains had to be couriered from Arrowe Park Hospital, as it was "unacceptable" they didn't have sufficient supplies at the Countess of Chester Hospital. Mr Johnson asks if Letby filled in a Datix form for that. Letby says she does not recall. Letby is asked about the text message she sent to Yvonne Griffiths on September 26, 2015, which said: "Thank you. That's really nice to hear as I gather you are aware of some of the not so positive comments that have been made recently regarding my role which I have found quite upsetting. Our job is a pleasure to do & just hope I do the best for the babies & their family." The court hears this was with regard to Letby and colleague Shelley Tomlins being allocated shifts in room 1, over other nurses who needed the experience. Letby says she cannot recall which nurses, specifically, had been making those comments, but they were band 6 nurses. Letby agrees this message followed events for Child H. Mr Johnson refers to the staffing rota for September 25-26. Letby says it was not the night staff who were making the comments. Mr Johnson asks if it was the day staff, why did they allocate Child H to Letby? Letby replies the comments had come in recent days prior to this.
4:01pm: Letby, in her defence statement, questioned how familiar the doctors were with chest drains. Letby, when questioned on this, says this would be non-consultants. In her defence statement, Letby said she could not recall the specific details of Child H's collapses.
4:08pm: Letby is asked to refer to her defence statement, in which she said her memory for both nights when Child H's collapses "merged into one". Letby added she was also looking after a severely disabled baby. Letby now accepts the disabled baby was born later in the shift. Letby tells the court staffing levels were not a contributory factor in Child H's collapses. Letby said she would "question whether the [chest] drains were securely put in" for Child H, as a potential contributory factor in Child H's collapses.
4:12pm: Letby accepts Child H was born in a good condition, and that she recovered quickly. She tells the court she cannot comment on her interpretation of the security of the chest drains, from her observations.
Thursday 25th May 2023
Cross-examination of Lucy Letby by Nick Johnson KC - Day 5
Children H & IChester Standard Live Reporting
10:31am: The trial is now resuming.
10:41am: Nicholas Johnson KC is continuing to cross-examine Lucy Letby on Child H. Letby is asked if staffing issues contributed to Child H's collapse. She says "no", but believes the "management of the chest drains" was a contributory factor.
LL: "I believe it has been accepted throughout the trial that there were issues with the chest drains". Letby said the location of the chest drains on Child H may have been a factor, and that Child H's pneumothoraces were not treated correctly, due to a lack of experience and "nobody seemed particularly confident" on managing the number of chest drains - she says that was down to "multiple" doctors. Asked who those would be, Letby said that would include Dr [Ravi] Jayaram, Dr [David] Harkness, Dr [John] Gibbs and "Dr [Alison] Ventress, even".10:59am: Letby says she had dealt with chest drains in Liverpool, but not at the Countess of Chester Hospital. She says she did not have much experience, and had a nursing colleague to assist her in the care of Child H. Letby is asked about the time between 8pm and 2am on September 25-26. She says she cannot recall, specifically, the assistance she had from a nursing colleague that night, but she was there 'on and off', and "gave me a lot of verbal advice that night" in the management of Child H's chest drains, and on baptism after the collapse of Child H. Mr Johnson reads from Child H's father's statement. He refers to being at the unit until "about midnight", and was woken up from home "in the early hours". Letby's nursing note is shown to the court. It includes: '...x2 chest drains in situ at start of shift - intermittently swinging. Serous fluid++ accumulating. 2330 Bradycardia and desaturation requiring Neopuff in 100% to recover. 10ml air aspirated from chest drain by Reg Ventress...inserted a 3rd chest drain...' Mr Johnson says Letby misrepresented the time of this event. Letby tells the court she would have got that time from her notes written at the time. An intensive care chart is shown to the court. It includes, for 2200 - '2210 desat...SHO present...serous fluid++ x2 drain' Letby says she cannot recall which SHO was on duty that night. Mr Johnson says the SHO on duty was Jessica Scott, and she has not recorded a note saying she was present for this. Another note 'Brady desat 2330 10ml aspirated from...drain...' Other details are '+clear [in the OP row]' and '+small blood stained [in the Suction ET row]'. Mr Johnson says this is another child producing blood in Letby's care. Letby says this blood has likely come from the ET Tube in the lungs. She denies moving it around to destabilise Child H.
11:04am: Letby accepts that a 52% desaturation is a potentially serious event. She says: "I don't agree" to the suggestion she has "cooked the books" in the nursing notes. She denies falsifying notes for Child H by giving the impression Child H was deteriorating prior to the collapse. Letby is asked why the '52% desaturation' is not in her nursing note. "Not every single thing gets written down...that is an error on my part." Letby says the SHO was present for that earlier desaturation. Letby denies writing in the intensive care chart after Child H's collapse.
NJ: "You're making this up as you go along, aren't you?"
LL: "No."11:08am: Mr Johnson says Child H's father's statement, which was agreed evidence, did not mention a collapse or an SHO being present. Letby denies lying. Dr Alison Ventress records a note for Child H, timed 11.50pm. It begins 'Several episodes of desaturation in past 2 hours...1st one after gas taken...became agitated...' Mr Johnson says Letby told this information to Dr Ventress. Letby says she did not know if she told her this information, she may have been present in the room.
11:12am: Dr Ventress adds: 'Further episodes no change in HR recovered with bagging...[oxygen requirement down] to 30% between episodes'. Letby denies "trying it on" or "falsely creating the impression to Dr Ventress that [Child H] had been having problems for a couple of hours."
LL: "No, I don't agree that it was false." Mr Johnson says the notes (on the observation chart and Letby's nursing notes) don't match. Letby agrees it's an "innocent coincidence" (as said by Mr Johnson).11:17am: An observation chart for Child H is shown for September 25-26. Letby is asked if the results show any concern up to midnight.
Letby: "This [the observations taken] reflects that specific moment in time" and says that chart shows no concerns, with all readings in the normal range. Dr Ventress added in her 11.50pm note: '2nd chest drain advanced back in to 4cm as was almost out. Done prior to chest x-ray'. Mr Johnson says this was Dr Ravi Jayaram's x-ray. Letby is asked why she had not noticed that. Letby says medical staff put drains in and managing them was not part of her nursing role. She accepts she knew chest drains were more secure when stitched in rather than taped in. She says she was checking the chest drains. She denies removing the chest drain to cause a desaturation just after Child H's father left.11:24am: Mr Johnson asks about Letby's error, as mentioned in her evidence, about the timing of the blood transfusion being completed. Letby said on May 15 the '0200 blood transfusion completed' should be 3am. Letby says she has "miswritten" it from looking at the charts. A blood infusion therapy chart is shown, in Letby's writing, which has in the time ended column what appears to be '0205' corrected to '0305'.
NJ: "The same mistake in two different places?" Letby says she "couldn't say with clarity" adjusting the time after she had written her nursing notes.
NJ: "What happened after 0305?"
LL: "I don't recall."
NJ: "Really?...[Child H] had a cardiac arrest." Letby is asked "how on earth" she made the 0205 error.
LL: "Because we're human people, we make mistakes." Letby says the error is "mine" on the nursing notes, but the timings were otherwise accurate. Letby says she cannot remember Child H's father being present. The father recalled "mottling running out of her skin towards her fingers". Letby says she agrees there was mottling on Child H's skin, but not that it was moving.11:27am: A blood gas chart for September 26 is shown to the court for Child H. Letby agrees the reading at 6.44am is a "good" blood gas reading. Mr Johnson says Child H had had a "miraculous recovery".
Letby: "Yes."
NJ: "Were you pleased?"
LL: "Of course I was pleased."
NJ: "Or were you frustrated that you had failed in your attempt to kill her?
LL: "No."11:30am: The second event is being discussed. For the night of September 26-27, Lucy Letby was the designated nurse for two babies in room 2. Nurse Christopher Booth was the designated nurse for Child G in room 2, and Nurse Shelley Tomlins was the designated nurse for Child H in room 1. Elizabeth Marshall is the designated nurse for four babies in room 3, including Child I. The court hears a seriously ill baby was brought into the unit during the night.
11:37am: The court hears Letby, in her evidence to defence on May 15, said she did not have much to do with Child H on the night shift. Letby said she was reliant on medical notes as she did not recall "with any great detail" that night for Child H. Dr Matthew Neame was the registrar that night, with Dr Jessica Scott the night SHO. Letby accepts she had got "confused" in her defence statement between the events of this night and the previous night. She rules out staffing levels as a contribution in Child H's deterioration. She says she cannot comment on medical incompetencies as she was not Child H's designated nurse and was not present for much of the shift, and rules out a doctor or nurse making mistake(s).
11:43am: Letby is asked if she was involved in an event timed 9.15pm for Child H, who had a desaturation and bradycardia. Letby said she did not remember. Dr Neame, in evidence, said "ETT removed by nursing staff" and that nurse was Letby, alone.
LL: "Well I don't have any recollection of that." A text is shown from Letby to a colleague at 9.51pm: "'I've been helping Shelley so least still involved but haven't got the responsibility..." Letby says she "does not agree" she would have removed an ET Tube by herself. The neonatal schedule shown for 9-10pm shows no duties for Child H for which Letby has been named as the nurse for it.12:06pm: The trial is now resuming following a short break and a short legal discussion. Mr Johnson is continuing to cross-examine Lucy Letby on the case of Child H.
12:07pm: Letby is asked about what she had been helping Shelley with, as per her text message - she says she had been helping with Child H. She denies taking an "opportunity" to "sabotage" Child H.
12:10pm: Nurse Shelley Tomlins' note for 9.45pm is shown: The court is shown nurse Tomlin's notes for that shift, which include: '...around 2030 [Child H] had profound desat and brady, air entry no longer heard and capnography negative therefore ETT removed and Drs crashbleeped. New ETT sited...on second attempt...Copious secretions obtained via ETT and orally, blood stained.' 2145 - Desaturation to 40% despite good air entry and positive capnography. ETT suctioned quickly with thick blood-stained secretions noted. [Child H] recovered quickly after...' Letby denies altering Child H's ET Tube to cause bleeding.
12:21pm: Mr Johnson asks if Letby was "bored" with the children she was looking after in room 2 prior to Child H's collapse.
LL: "No." She denies she had "time on her hands". At 12.45am on September 27, Letby is recorded as 'liking' a post on Facebook. At 12.46am, she liked a Facebook photo posted by a colleague. Letby says she may have been on her break at this point. Mr Johnson says Letby was involved in a fluid balance chart for one of her designated babies around that time.
Letby: "Yes, at 1am." Child H's father's statement is read to the court, in which he said "Quite late on [Saturday, September 26]" he went to rest, and was woken up shortly afterwards and to get to Child H's bedside. Letby denies using the time the father was away as an "opportunity" to attack Child H.
LL: "No, I've never attacked any child." Letby says she "couldn't say" if she was covering for Shelley Tomlins at 1am. An observation chart is shown for Child H for September 26-27. Hourly observations are made between 8pm and 4am, except for 1am. Crash call bleep data is made at 1.04am and 1.06am for Child H. Mr Johnson says Dr Neame gave evidence to say when he arrived, Letby was present.
NJ: "Is that right?"
LL: "I can't say, from memory."
NJ: "You were there, weren't you?"
LL: "I can't say exactly where I was, from memory." Letby denies making an "alibi" at 1am for the fluid balance chart for her designated baby.
LL: "That's me giving cares to the baby I was allocated."12:23pm: Nurse Shelley Tomlins' record, written at 3.49am, for the 3.30am desaturation: '0330 - profound desaturation to 60s, again requiring Neopuffing with no known cause for desat....copious amounts of secretions yielded orally, pink tinged. Small amount of ET secretions gained, again pink tinged. Heart rate mainly normal during desat. Recovered slowly.' Letby denies "interfering with [Child H's] ET Tube".
12:25pm: Letby says she is helping Shelley Tomlins after the desaturation.
NJ: "Why is it always you that ends up in nursery room 1?"
LL: "I don't agree it is always me."12:26pm: Mr Johnson moves on to the case of Child I. Letby agrees she remembers Child I "very well". Mr Johnson says this is "another case where you falsified [her records]."
12:32pm: Letby is asked to look at her defence statement. She said Child I's stomach "bloated...regularly" and "all the nursing staff" were aware of it. Letby said "nothing was ever done" about the concerns with Child I's bowel. Letby said she was one of those raising concerns, that she "was not getting the treatment she needed". The defence statement adds Letby did recall one handover, to nurse Bernadette Butterworth, that Child I desaturated and became apnoeic, and she assisted in care thereafter.
12:41pm: Letby, when asked, rules out staffing levels as a problem that led to Child I's deterioration on September 30. For September 30, Letby was looking after Child I and two other babies in room 3 on her long day shift. Letby rules out medical incompetencies or mistakes made by medical staff that led to Child I's collapse on September 30. Letby is asked to look at Child I's medical records from September 26-29, and observations early on Letby's shift on September 30. Letby agrees Child I was stable at this time. A temperature of 36.1C is recorded for Child I at 11am, and the 'hot cot' temperature was turned up. Letby denies by this time she had "fallen out" with medical colleagues Ashleigh Hudson, Melanie Taylor and one other.
12:45pm: The ward round posted a "positive picture" for Child I on September 30. Letby agrees. Child I was due her immunisations, as noted on the ward round. Mr Johnson says this positive picture was similar to Child G, when Child G was about to have her immunisations. Mr Johnson asks what became an obstacle to that. Letby replies it was Child I vomiting and having to be transferred to room 1.
12:54pm: A feeding chart is shown for Child I for September 30. Mum fed and gave cares at 10am. The note is signed by Letby. At 1pm a 35mls feed was given via the NG Tube which had a 5ml aspirate. Letby says the 5ml aspirate "is a very minimal amount". At 4pm a further 35ml feed is given via the NG Tube. On both occasions Child I was asleep. At 4.30pm - 'large vomit + apnoea -> N1' [transfer to nursery 1]. Letby is asked about Child I's mother's routine.
Letby: "Not specifically..." she adds the mother would visit the unit regularly. Mr Johnson suggests Letby knew the family so well through the frequent visits that she got to know their routine when they would be in and out of the unit.
Letby: "I don't agree." Dr Lisa Beebe's note showed she was asked to review Child I due to a low temperature. The note adds: '...mum reports [low] temperature has been happening over past few days'. The note concludes: '...monitor closely, if further concerns for sepsis, screen but appears clinically well at present'. Letby says she does not recall the conversation. She does not recall, as the prosecution suggests, telling the doctor one concern[low temperature] and the mother another [abdomen]. She denies "providing a cover", and says she did "monitor her [Child I] closely", as noted on the doctor's plan.1:08pm: Letby says she first monitored Child I's vital signs at 3pm. She said the concern raised with the doctor was Child I having a low temperature, and she had adjusted that by raising the hot cot temperature. Mr Johnson suggests that "monitor closely" would mean more observations.
Letby: "I disagree." Letby is asked how long the 1pm 35ml feed with thickener, as listed on the chart, would take to administer. She agrees it would take "roughly" 15 minutes. Letby's nursing note, written at 1.36pm is shown to the court: '...3x8 feeds ebm, 2bottles to 1NG Tube. abdomen appears full and slightly distended, soft to touch [Child I] straining++. Bowels have been opened. Mum feels it is more distended to yesterday and that [Child I] is quiet. Appears generally pale...Drs asked to review - to continue with current plan' Letby says: "We monitor all our babies closely" in response to why Dr Beebe had said 'monitor closely' instead of 'do what you normally do'.
Mr Johnson: "This is yet another example of you writing nursing notes for something that didn't happen."
LL: "I don't agree." Letby denies "cooking the notes" to show Child I was deteriorating prior to her collapse.2:06pm: The trial is due to resume at 2.10pm following its lunch break.
2:23pm: The trial is now resuming. Prosecutor Nicholas Johnson KC is continuing to cross-examine Lucy Letby on the case of Child I. An observation chart for Child I is shown for September 30. Hourly observations are made for 10am-1pm, and 3pm to the rest of the day. Letby says there is "no reason" why the 2pm observation is not made. Letby is asked which 'doctors' reviewed Child I at 3pm. Letby names one doctor and believes it was one doctor reviewed. Mr Johnson says there is no medical note in relation to this. Letby denies "making it up". Mr Johnson asks Letby why the 'bottle-bottle-NGT' feed system is interrupted by 'bottle-NGT-NGT'. Letby says the 4pm, 2nd NGT feed was as Child I was asleep. Letby denies "lyingly" recording notes for when Child I had bowel movements during the day. Mr Johnson says a doctor's notes do not note a prior examination. Letby denies making up the examination in her notes. She adds: "Just because it's [not there] doesn't mean it [didn't take place]."
2:26pm: Mr Johnson says Letby is "very keen" to raise doctor's mistakes with the likes of Dr Harkness and Dr Gibbs, but not in this case.
LL: "I don't believe this was noted at the time, my priority was [Child I], not medical notes."
NJ: "You force fed [Child I] didn't you?"
LL: "No, I didn't." Letby says Child I did not wake for that feed, so an NGT feed was given as "standard practice".2:31pm: Mr Johnson says "despite all the positive signs" for Child I, she vomited, just like Child G, and in both cases, Letby was there. Letby says she does not recall if she was there when Child I vomited. A medical report said Child I: "There is splinting of the diaphragm due to bowel distention..." Letby denies "pumping" Child I full of milk or air.
Letby: "I fed [Child I] the normal dose of milk for her feed." A blood gas chart for Child I is shown - the chart had not been noted up by Letby and it was found on a clipboard. It was signed by Bernadette Butterworth for Letby. Letby says the chart was "not hidden - it was there for anyone to see."2:34pm: Mr Johnson talks about the 7.30pm event for Child I. Letby's notes add: 'At 1930 [Child I] became apnoeic, - abdomen distended++ and firm. Bradycardia and desaturation followed, SHO in attendance and registrar crash called....'Air++ aspirated from NG Tube...[Child I] is now very pale and quiet'. Letby denies forcing air into Child I.
2:37pm: Observations for Child I in the remainder of September 30 are shown to the court. Bernadette Butterworth's nursing note: 'During handover [Child I] abdo had become more distended and hard she had become apnoeic and bradycardic and sats had dropped. IPPV given and despite a good seal with Neopuff there was still no chest movement, aspirated NGT air +++ and 2mls of milk obtained, eventually got chest movement and sats and heart rate normalised...'
2:50pm: Mr Johnson talks about the second event for Child I, which was on the night of October 12-13, when Letby said she was standing in the doorway when she could see Child I looked pale, and the lights were turned up. Letby says the lighting was on in that room so Child I could be seen prior to the lights being turned up. Letby is asked to look at her defence statement. She recalls Ashleigh Hudson was "quite inexperienced" to be looking after Child I. Letby said Child I required "very close monitoring", and adds that, "looking back", Ashleigh had stopped monitoring her when she should have been. Asked to explain where that instruction to monitor Child I came from, Letby says it was policy that Child I should have been monitored as she had come off antibiotics some time in the previous 48 hours. Letby adds: "I'm not saying Ashleigh made a mistake." The judge seeks clarification on 'monitoring'. Letby says it includes monitoring observations if a baby is on a monitor, but otherwise involves keeping an eye, regularly, on the baby.
2:57pm: Mr Johnson says there had been at least 48 hours since Child I had gone off antibiotics before the event occurred. Letby is asked in what way Ashleigh Hudson was inexperienced.
LL: "I don't think Ashleigh had a lot of experience in recognising changes in babies, potentially." Letby says the more experience you have, the more you can detect changes, such as changes in colour, in a baby. Letby tells the court she does not recall a reason why she went into room 2 with Ashleigh Hudson. In her defence statement, Letby said as they entered the room, they turned the light up on the light dimmer switch, and she saw Child I looking pale, and they went to assist. Child I was "gasping" and the alarm had not gone off.3:07pm: Letby rules out staffing levels, medical incompetencies or staffing mistakes as a cause of Child I's desaturation on October 12-13. A nursing shift rota is shown for October 12-13, with Lucy Letby in room 1, designated nurse for one baby. Ashleigh Hudson was designated nurse for three babies in room 2, including Child G and Child I. Letby repeats there was no issue with staffing ratios to babies cared for, for that night. Letby agrees with the evidence Ashleigh Hudson said that Child I was doing well - "prospering", and that the level of care had been scaled back. Before the collapse, Child I was in air and on bottle feeds. Letby says she has "no memory" if Ashleigh Hudson, as said in evidence, left room 2 to help colleague Laura Eagles in room 1. Letby says she had a baby in room 1, and cannot recall who was to look after nursery 2. In evidence, she said she was not the nurse called to room 2. She tells she would have remembered having to hand over care of her baby and look after three babies in room 2.
3:17pm: Letby said "very quickly", she had noticed and saw Child I was pale. Letby is asked why she was at room 2. She replies there was "nothing sinister" about that, that she had been in a chat with a colleague.
NJ: "The lights were off, weren't they?"
LL: "I can't say." Letby is asked to look at her police interview. In it, she says she had taken over Child I's care as Ashleigh Hudson had been "quite junior". For the observation of Child I, she replied the lights were off at night, and then they put the lights on, adding she could see Child I and: "I noticed that she was pale in the cot." Letby, asked why she had told the jury the lights were "never off", says the lights are "never off completely", they are turned up. A second police interview has
Letby: "We put the light on - the lights aren't on in the nursery at night." Asked why she did not refer to a dimmer switch in her police interview, Letby says: "I don't know."
NJ: "Are to trying to massage the evidence by [now] saying the lights were on low?"
LL: "No."3:21pm:
NJ: "What effect does going from a bright corridor [looking into] a [dark/dimly lit] room have on your eyesight?"
LL: "I don't know.
NJ: "You really don't know?"
LL: "No."
NJ: "Everybody knows, don't they?" Letby says: "You wouldn't be able to see as well." Mr Johnson says Letby was able to see "straight away" as she had caused Child I's deterioration.
LL: "No."3:35pm: The trial is continuing following a short break.
3:41pm: The photo of the cot, as shown previously, is displayed.
NJ: "Do you agree it is accurate?"
LL: "No...there would be more light visible. The cot would potentially be nearer to the light.
LL: "I think it was nearer to the workbench than that." Mr Johnson asks how big Child I's hands would be - Letby says they would be small. Mr Johnson says Child I would be almost entirely obscured.
LL: "Just her hands and her face."
NJ: "Which would be covered by that tentlike structure."
LL: "Not entirely no." Mr Johnson asks how Letby could spot something Ashleigh Hudson could not, as mentioned from her police interview.
LL: "I had more experience so I knew what I was looking for - at."
NJ: "What do you mean looking 'for'?"
LL: "I don't mean it like that - I'm finding it hard to concentrate."3:44pm: The judge, Mr Justice James Goss, says it "has been a long day" and the trial is adjourned for today.
3:46pm: The next court day scheduled will be for Tuesday, May 30.
Friday 26th May 2023 - no court (planned)
Monday 29th May 2023 - no court (bank holiday)
Tuesday 30th May 2023 - no court (juror absence)
Chester Standard Live Reporting
10:39am: Eleven of the 12 members of the jury come into court. The judge tells them the trial cannot proceed unless all 12 of them are present, and one is not present for "particular personal reasons". "There is obvious uncertainty in relation to your colleague's position", he adds. The jury are urged to turn up tomorrow unless they hear otherwise. The judge tells the jury: "We have had a lot of breaks, and there comes a time where we cannot keep having more and more breaks, as it becomes inappropriate. "Events do occur which are unexpected, and we have had a few during this case."
The court is told that a view will be taken tomorrow on the 12th juror.
Wednesday 31st May 2023 - no court (juror absence)
Thursday 1st June 2023 - no court (juror absence)
Friday 2nd June 2023
Cross-examination of Lucy Letby by Nick Johnson KC - Day 6
Children I, J & KChester Standard Live Reporting
1:00pm: Legal teams, members of the public and the press have entered the courtroom at Manchester crown Court. Lucy Letby has also arrived. The judge, Mr Justice James Goss, has also arrived.
1:01pm: Members of the jury are now coming into court. The trial will now resume, and is expected to hear evidence until around 4pm.
1:04pm: Nicholas Johnson KC, for the prosecution, continues to cross-examine Letby in the case of Child I. He moves on to the third incident, on October 14, 2015. Mr Johnson says Letby does not refer to this incident in her statement. Letby, in her evidence, said she did not recall this night.
1:05pm: Letby rules out staffing levels, medical incompetence or staffing mistakes as a contributory factor in the collapse of Child I for this incident.
1:16pm: The staffing rota for October 13-14, 2015 is shown to the court, with Letby in room 1 as the designated nurse for Child I. Joanne Williams is the designated nurse for two other babies in room 1 that night. Letby is asked to look at her nursing notes for that night. Mr Johnson says Child I was tolerating handling and 'tone appears improved', according to Letby's notes. The notes add: 'At 0500 abdomen noted to be more distended and firmer in appearance with area of discolouration spreading on right-hand side, veins more prominent. Oxygen requirement began to increase, colour became pale...gradually requiring 100% oxygen...blood gases poor as charted. Clear air entry, slightly reduced on left, chest movement reduced...continued to decline. Reintubated at approx 0700 - initially responded well. Abdomen firm and distended. Overall colour pale. Xrays carried out...resuscitation commenced as documented...night and day staff members present' Letby says she cannot recall the discolouration now. She does not recall it moved, but it was spreading by getting larger.
NJ: "Where did you get the time of 5 o'clock from?"
LL: "I don't know. I don't know if it's from paper charts or memory." Mr Johnson says if Letby had seen this, she would have escalated it to a doctor.
LL: "I can't comment on what time the doctor did come." Mr Johnson says almost 24 hours earlier, Child I was found "almost dead", and then this incident happened. He asks what Letby would have done.
LL: "I would have escalated it to someone, senior like a doctor." Mr Johnson shows the doctor's note, which mentions: "Abdomen distended and mottled".
LL: "I can't say specifically what time I asked him to come, the note says he came at 5.55am". Mr Johnson says this would have been an emergency for Child I.
LL: "I don't believe it was an emergency, I believe it showed a decline."
NJ: "You sabotaged [Child I] at about 6 o'clock, didn't you?"
LL: "No."1:24pm: A prescription chart shows Dr Matthew Neame prescribed morphine sulphate for Child I, and the infusion was commenced at 5.50am. A fluid chart shows '0530 abdo distended++' in Letby's writing. Letby says by 6am, the oxygen requirement had gone up to 100% for Child I, from 60% at 5am. Letby had written 'squeaky' for the oxygen level at 5am. Letby tells the court this meant the air entry for Child I was not clear. Letby says squeaky air entry is not an emergency. Mr Johnson says there is also expanding discolouration and a distended abdomen. Letby denies copying the word 'squeaky' for the 5am oxygen column from Dr Neame's 5.55am note.
Letby: "I disagree." Letby says she recalls Dr Neame saying the mottling was unusual; she cannot recall the mottling specifically.1:26pm: A report showed Child I's gaseous distention of the bowel had increased on October 14 since the previous x-ray at October 13. Child I had been on a ventilator and nil by mouth. Letby denies injecting air into Child I.
NJ: "You had inflated [Child I] with air, hadn't you?"
LL: "No."1:28pm: At 7am, Child I had a significant desaturation. Letby's note: 'Reintubated at approx 0700 - initially responded well. Abdomen firm and distended. Overall colour pale. Xrays carried out.'
NJ: "That is because you were sabotaging her, isn't it?"
LL: "No."1:29pm: Letby says she does not remember the 7am desaturation "with any clear detail".
1:34pm: Mr Johnson moves to the final event for Child I, when she died on October 23. Prior to that, Child I had been moved to Arrowe Park Hospital before returning to the Countess of Chester Hospital's neonatal unit. Mr Johnson shows Letby observation charts for Child I from the previous day. Letby accepts Child I's observations were stable, save for one slightly raised respiration rate reading. She agrees Child I was self-ventilating in air at this point. She accepts Child I's abdomen was, the previous day, soft and non-distended.
1:35pm:
NJ: "Would you agree that despite three life-threatening events in the previous three weeks, [Child I] appeared to be in a stable condition?"
LL: "Yes."1:40pm: For the night of October 22-23, Lucy Letby is a designated nurse for a baby in nursery room 2 and one in room 3. Ashleigh Hudson is the designated nurse for Child I in room 1 and one other baby. Mr Johnson tells the court the baby in room 2 went to a hospital in Stoke during that night shift. Letby says there were staffing issues, which were "not ideal", which were a contributory factor in the treatment of Child I following the collapse, in that a doctor had to be called away during the event.
Letby: "Considering what [Child I] had been through, she was a poorly baby, the doctors were not with her at all times...once she deteriorated." Letby adds she believed Ashleigh Hudson was capable of looking after Child I, for Child I's nursing needs at this stage.1:45pm: The neonatal schedule for that night is shown to the court. Letby sent a message on October 22 at 8.47pm to a colleague: '...Unit nice. Transport on way to take my baby back to Stoke. Only 8 babies. Off duty not out. X' Mr Johnson says this refers to the baby he mentioned earlier who was transferred out during that night. The court hears that transfer process, noted as completing at 1am, is not a 'five-minute' process, and takes time and involves family communication.
1:58pm: Child I collapsed at 11.57pm. Letby denies falsifying a note for the Stoke-transfer baby prior to that at 11pm. The court is shown a nursing note by Ashleigh Hudson, which the court heard was timed at 10.57pm. 'Longline removed due to constant occlusions; neonatal nurse Lucy Letby unable to flush, so Paeds Reg Rachel Chang informed.' Dr Chang had written, for the Stoke-transfer baby at 10pm, the baby was safe for transfer. Letby's note for this baby was written at 10.50pm, and completed at 10.52pm. It included a documentation of a longline infusion with a 10% dextrose fluid. Letby has co-signed the document. Mr Johnson says the 'original 2300' reading has been changed to '2400' by Letby. Letby said the '2300' reading was an error and it was changed to '2400' as the correct time. She adds: "The charts are there for everybody to look at."
2:05pm: Letby denies falsifying a fluid balance chart for the Stoke-transfer baby. Mr Johnson asks if Letby recalls what Ashleigh Hudson said for the 11.57pm desaturation. He says Ms Hudson gave evidence to say Child I was crying, making a noise she had not heard before, different to a cry for hunger.
Letby: "I did not hear that cry at that point. When I entered that nursery, she was quiet...and apnoeic." Letby says for this event, it was a case where one of the three nurses on duty that night would have had to come and assist in room 1.2:11pm: Letby says she does not recall Ashleigh Hudson going to call for Child I's parents. Letby says there is an error on the IV chart, and the time has changed.
Mr Johnson: "Three different mistakes on two different babies?" Letby says she does not know who wrote in the different times.
NJ: "How do those sorts of mistakes happen? Letby says when the unit gets busy, "we" can make errors on the paperwork.
NJ: "We? Or you?"
LL: "I don't believe it would have been me - we would both have been there for it."
NJ: "Or is it you altering medical records to put some time between you and serious events for [Child I]?"
LL: "No." Letby adds: "I did not deliberately falsify any paperwork."2:17pm: At 1.06am, Child I was crying again, the court hears. Letby recalls Child I was crying, but cannot recall being there by the cotside first. She accepts she was in the nursery. Mr Johnson asks if Ashleigh Hudson was called over by Letby.
LL: "She might have been in the nursery when I called her, I couldn't say." Letby adds she could have "come in" [as her defence statement says] from the other part of the nursery. Letby says she had her hands in the incubator, "trying to settle [Child I]."
LL: "My assessment of [Child I] at that time was she was hungry and rooting."
NJ: "You had pumped her full of air?
LL: "No."
NJ: "You were doing your best to kill her?"
LL: "No."2:18pm:
Letby: "I have never injected air into any baby."2:25pm:
NJ: "Do you remember interrupting [Child I]'s mother?"
LL: "No." Mr Johnson says Child I's mother, in agreed evidence, recalled Letby was "smiling" and had talked about how Child I had been going on about 'enjoying' her bath. Child I had been bathed as part of the bereavement process following her passing.
NJ: "Why did you say that?"
LL: "It's trying to, in that awful situation - it wasn't meant with any malice. We still talk to them and treat them as if they were alive. It wasn't joking or...malice, it was trying to reflect on a happier memory."
NJ: "How can you say such things?"
LL: "She had her first bath when she was alive and that was what she had enjoyed, not the one when she had passed away."
NJ: "How do you know it was her first bath?"
LL: "Because I was there, we took photographs, it was a big occasion." Mr Johnson asks how many baths Child I had in Arrowe Park - Letby says she cannot say.
NJ: "You were getting a thrill out of the grief and despair in that room, weren't you?
LL: "Absolutely not."2:41pm: The trial has had a short break, and will be resuming shortly with Mr Johnson cross-examining Letby in the case of Child J.
2:51pm: Copies of Letby's defence statement, edited to the relevant parts in the case by agreement, are handed out to members of the jury. Mr Johnson moves to the case of Child J, a baby girl born on October 31, 2015. Letby, in her defence statement, said she had never seen a baby with stomas before at the Countess, and other doctors were "equally unsure about stomas", and the parents were "more proficient" than the Countess staff at dealing with stomas. A handover sheet was taken to Letby's home, the defence statement adds, unintentionally.
2:52pm: The night shift rota for November 26-27 is put up. Two band 4 unit nurses are named in the rota. Child J was in room 4. The designated nurse was Nicola Dennison, a band 4 nurse also looking after one other baby in room 4. Letby was the designated nurse for two babies in room 3 that night. Letby rules out staffing levels as a contributory factor in Child J's collapse, nor medical incompetence, nor staffing mistakes. She says the unit was busy at the time, but was not a contributory factor. She adds she does not know how Child J collapsed.
2:54pm: Letby accepts the evidence from Child J's mother that Child J was well and "about to go home in a day or two".
3:06pm: Letby adds there was an issue with Child J's stoma care, as it had been discussed among the nurses that they had little experience. She adds she does not "want to name names" on any specific nurses' lack of experience. Mr Johnson refers to Nicola Dennison's previous experience with stomas, which she said in evidence she had experience of it. Letby says over the years, she did not recall any other babies with stomas. Mr Johnson says band 4 nurses, as said by Letby in evidence on May 16, should not be involved in stoma bag care, as they would be unfamiliar with the procedure. Letby said: "The unit was very busy and we had to use staff where we could." Letby says she was not referring to Nicola Dennison specifically, but the nursing situation overall. She says there was not an issue over staffing levels at the time of Child J's collapse. Asked to explain a text message she had sent to a colleague Letby tells the court: "Sometimes I felt nurses would take on roles which I didn't think they were trained enough in". The next message adds: "It's shocking really that they are willing to take the responsibility for things that they have no training or experience etc on. Don't think they appreciate the potential difficulties X" Letby agrees she believed it was "potentially dangerous". Mr Johnson says the impression of the court was that band 4 nurses were not qualified in stoma care, and the hospital was 'cutting corners' by assigning such nurses to those tasks. Letby agrees. The court is shown a document about the duties for special care babies [such as Child J], which includes stoma care.
LL: "You need to appreciate the context that the unit was not familiar with stomas."
NJ: "This nurse was familiar with stomas, wasn't she?"
LL: "In her opinion, yes." Mr Johnson says Letby was deliberately creating the impression to the jury that the care for Child J was deficient.
LL: "I do think that. I don't think she had a high standard of care. "I don't think anyone was overly confident in saying 'I know what to do with a stoma'. We were led by the parents..." Mr Johnson asks why Nicola Dennison was not challenged about this.
LL: "I can't answer that."3:10pm: Letby denies not being happy in nursery room 3, or being happier in nursery room 1. Letby accepts the evidence of Nicola Dennison that babies in room 4 should have the light off overnight, as they are due to go home.
3:11pm: Mr Johnson says two pairs of events for child J happened; one pair in room 4, one pair in room 2. The room 4 incidents happened at 3am and 4.57am, and the room 2 incidents happened either side of 7am. Letby accepts this was the case.
3:15pm: The court is shown a night shift staffing rota at the end of the night, in which Child J was in room 2. Letby is asked if she has any memory of the earlier pair of incidents. She says she does not have a recollection. She says from her memory, Child J had a seizure and was moved to room 2. She says she could be mistaken in her memory.
3:21pm: The court is shown an apnoea/brady/fit chart for Child J on November 27, recording events for Child J at 4.40am and 5.03am, recorded by nurse Nicola Dennison, in nursery 4. The desaturations are recorded by Dr Kaliyilil Verghese. Letby recalled when she was called in to room 4, Child J was 'fitting', not desaturating. Letby accepts that by 6.28am, Child J had been moved to room 2, as a text message written by her to a colleague had said that was the case.
3:30pm: Letby says she cannot recall where she was when she sent the 6.28am message, whether she was in room 2 or not. The message added: 'only 5 staff!'
Mr Johnson: "So it was all hands to the pump then?" as twins had been admitted to room 1 as an emergency.
LL: "Yes." Mr Johnson says all staff would have been concentrated in room 1. LL "Not all, but most, yes."
NJ: "You were not involved in that, were you?"
LL: "Not from memory, no." Mr Johnson says the message sent at 6.31am would have meant Letby would not have been in room 1. Letby agrees. Letby says Mary Griffiths would not have been in room 1 as she was not an intensive treatment unit-trained nurse. She denies she would have been the last nurse for room 2. Letby accepts, from looking at the neonatal schedule, she would have been in room 2 when the emergency twins were admitted to room 1.
NJ: "There would have been a lot of distractions...wouldn't there?"
LL: "I don't know what you're implying."
NJ: "The medical staff would have their attention focused on the twins, and any help that could be spared would have gone on the twins.
NJ: "Do you accept that a lot of help was needed?"
LL: "It would be normal practice to get in the consultant when we only had the registrar, yes." Dr John Gibbs arrives at 6.34am, earlier than normal for his shift, to assist.3:31pm: The last message Letby sent to her colleague was 6.49am. The colleague sent three messages which were not replied to in the following minutes.
NJ: "That's because you were in nursery room 2, sabotaging [Child I], weren't you?"
LL: "No, I wasn't."3:35pm: Letby accepts that, on the neonatal schedule, she is not recorded doing anything in the half hour prior to Child J's collapse at 6.56am. Mr Johnson refers to Dr John Gibbs's notes of 'sudden desats (to unrecordable levels) at 6.56 and at 7.24 and bradycardia. Both associated with clenching of hands, stiff limbs, and on second occasion, eyes deviated to left.'
NJ: "This was your doing?"
LL: "No, it wasn't." Letby accepts it was an emergency situation and Dr Gibbs had to be called away from room 1 to Child J in room 2.3:42pm:
NJ: "You took your opportunity, when all the resources at the NNU were concentrated on the twins who had been admitted as an emergency."
LL: "No." Letby accepts evidence had been heard saying there was no known cause for Child J's deterioration. Letby had care of Child J the following night, which the court is shown, from Letby's notes for that night, 'nothing happened'.3:46pm: Mr Johnson moves on to the case of Child K, born on February 17, 2016. Letby said, in her defence statement, she did not recall the events of February 17, and did not recall saying to Dr Ravi Jayaram that Child K had just started deteriorating. She said she had done nothing to interfere with Child K's tube or the alarm. She added the Countess neonatal unit was not capable, given its staffing levels, of looking after a baby of Child K's gestational age. Letby tells the court she has no memory of such a conversation with Dr Jayaram. She says it is "difficult" to dispute Dr Jayaram's recollection of the event as she had no memory of it. She denies she has changed her version of events since starting to give evidence.
3:50pm: Letby is asked if she understands the reason why Child K was born at the Countess.
LL: "Yes." Mr Johnson tells the court it was deemed 'too risky' to transfer Child K and her mother to another hospital at that stage, and that was why Child K was born at the Countess.
LL: "I don't know why more effort was not made to find a bed for her [elsewhere]."
NJ: "You have persistently given the impression that the Countess has taken on babies it [is not able to look after and that is why they collapse]."
LL: "Yes."
NJ: "Is that the reason you said to the jury you didn't understand why [Child K] was born at the Countess?"
LL: "I don't understand why she was born at the Countess."
NJ: "Is it to bolster your defence?"
LL: "No."
LL: "I understand why she was born there but I don't necessarily agree [with the decision to have her born there]."3:53pm: Letby says she does not recall the latter two desaturations for Child K, and does not accept Dr Jayaram's evidence in the first desaturation. Mr Johnson says he will deal with these in a different order than chronologically; he will cross-examine on the second desaturation first.
3:54pm: Letby says she does not know what happened to Child K, so does not cite staffing levels as a contributory factor in Child K's desaturations. She says she feels "potentially" the ET Tubes were not secured for Child K.
4:03pm: The second desaturation occurred at 6.10-6.15am on February 17, 2016. The court hears a note on Child K's birth and assessment was typed up by Letby on a computer from 6.04am-6.10am. The note would have been taken from paper charts taken by the cotside.
NJ: "You were at [Child K's] cotside a minute or two before she desaturated, didn't you?" Letby says she would have got the notes from the cotside "at some point" prior to her typing them up.
Monday 5th June 2023
Cross-examination of Lucy Letby by Nick Johnson KC - Day 7
Children K, F & L - (juror sent home unwell)Chester Standard Live Reporting
10:35am: The trial is expected to resume shortly.
10:37am: The trial is now resuming. The judge, Mr James Goss, informs jurors the court will be sitting no later than 3pm on Wednesday. Nicholas Johnson KC, for the prosecution, is continuing to cross-examine Lucy Letby on Child K.
10:40am: Mr Johnson asks Letby about an ET tube document, which she had entered at 06.10am on February 17, 2016. Child K desaturated at 6.15am. Letby says she has "no memory of being at [Child K's] cotside."
10:41am: Letby agrees Child K had been on morphine and would have been "well sedated"
NJ: "And yet the tube slipped again at 6.15am - just after you had been with her?"
LL: "I can't say that I was physically with her, no." Letby says the notes she would have obtained for Child K were at the end of the bed, and she has no recollection of being physically with Child K at the cotside.10:47am: Mr Johnson asks about the 7.25am-7.30am desaturation. Letby says she has no memory of it. Letby says she cannot recall any intervention regarding Child K at this point. Mr Johnson says one of Letby's colleagues was called to the nursery.
NJ: "What were you doing in nursery room 1 at 7.30am?"
LL: "I can't answer that, I don't have any recollection of it." The neonatal review is shown for February 17, 2016. Letby's duties include tending to her designated baby in room 2 at 7am. Mr Johnson says there was no reason for Letby to be in room 1 at 7.30am. Letby says there can be many reasons. Mr Johnson says Letby was "sabotaging [Child K] yet again, weren't you?"
Letby: "No." Letby says she has no memory of it.10:53am: Letby says she "cannot say" if Child K moved her ET Tube more than once. "I don't have independent memory of the tube slipping." Letby is asked to look at her police interviews for Child K. Within there, Letby said she had believed Child K's tube had slipped at an earlier point. Letby denies dislodging Child K's tube. Asked if she disputes her colleague's recollection of Child K's desaturation, Letby says she cannot recall.
10:59am: Mr Johnson moves to the 3.50am desaturation - the first of the three desaturations for Child K. Letby agrees Joanne Williams was Child K's designated nurse. She agrees Joanne Williams left Child K before the 3.50am desaturation. She accepts that nurse left at 3.47am. Letby says she cannot recall Dr Ravi Jayaram's whereabouts at this point.
11:03am: A note from the transport team at 3.41am is shown to the court: 'Called Dr Jayaram back with the above plan and he was agreeable totally with all the above'. Letby accepts that if this note is accurate, Dr Jayaram would have been around the nursing station at this time. Letby accepts that Joanne Williams would have asked someone to 'babysit' Child K in her temporary absence from the nursery. Asked if she disputes it was her to babysit Child K: "I have no memory of that." Letby says she has no memory of Dr Ravi Jayaram's account of him walking into the unit and seeing her standing over Child K's cotside, or that Child K was desaturating, or that Child K's ET Tube was displaced.
11:13am: Letby denies trying to kill Child K. Letby is shown a copy of her 2019 police interview, specifically police talking through Dr Ravi Jayaram's account of events from the night. That was the evidence he had given in the trial, that he had felt 'uncomfortable' with Letby being in the nursery room 1 and entered, and saw Letby. Letby, in police interview, said she "didn't remember" the event. Mr Johnson suggests Letby is lying. Letby denies this. Letby denied, in police interview, dislodging the tube. Mr Johnson says Letby had earlier said the event "didn't happen".
LL: "I don't believe it did happen, but I have no direct memory of it."11:15am: Letby says it was "standard practice" at the Countess of Chester Hospital's neonatal unit to wait "a few seconds" - "10, 20" to see if a baby self-corrected during a desaturation.
NJ: "30 seconds?"
LL: "I can't say."
NJ: "You are lying, aren't you?"
LL: "No."
NJ: "Because you were trying to kill [Child K]."
LL: "No."11:21am: The nursing notes for Joanne Williams recorded 'large amount blood-stained oral secretions' for Child K. Letby says she did not believe she gave Joanne Williams that information.
NJ: "Did you ever see [Child K's] parents?"
LL: "I can't recall."
NJ: "Did you ever meet them?"
LL: "I can't recall."
NJ: "Then why did you search for them [on Facebook] on April 20, 2018?"
LL: "Because I have thought of babies on the unit over the years, and I do look back at them."
NJ: "You have a very good memory for names?"
LL: "Yes."
NJ: "Her name didn't appear on the handover sheet, did it?"
LL: "I can't say." Mr Johnson says Child K had been born earlier that day, and handed over to the care of Melanie Taylor, and Child K was transferred out of the hospital.
NJ: "How can you remember that name [of Child K]?"
LL: "I can't."
NJ: "Can't or won't?"
LL: "I can't."
NJ: "What was the significance of April 20, 2018?"
LL: "I can't recall."
NJ: "Do you remember the answer you gave to your counsel on May 16?"
LL: "No." Mr Johnson says Letby said you look back on 'all the babies you care for'. Letby says it was taken out of context, and she played a part in Child K's care via the morphine infusion.11:24am: Mr Johnson moves on to the case of Child F, the first of the two babies the prosecution say Letby poisoned with insulin. Child L is the other child allegedly poisoned by Letby. Letby denies she did this. Mr Johnson previously told the court the cases of Child F and Child L would be part of the cross-examination process together. Letby accepts the insulin readings which were shown for Child F - the insulin and insulin c-peptide numbers.
11:32am: Letby says "there may have been some discrepancies" in the blood sugar levels for Child F. Mr Johnson says Prof Hindmarsh had told the court there would be discrepancies between a lab result and that taken from blood gas tests, 'of about 10-15%'. Letby says she does not remember who put up the bag, as she did not recall, but as she had no recollection of it, it would have been her nursing colleague [who cannot be named due to reporting restrictions]. Letby says she co-signed the bag with [colleague].
LL: "To me, the other person who could have [put up the bag] would have been [my nursing colleague]." Letby says: "I can't answer that" to Mr Johnson's suggestion Child F had been targeted with insulin poisoning. Letby says she can accept insulin was given to Child F at some point. She says "if that's the evidence", then the insulin would have been administered via the TPN [nutrition] bag. Letby accepts at the time of her arrest, she did not know or had heard about insulin c-peptide. Mr Johnson says the ratio between insulin and insulin c-peptide from the result had shown insulin had been administered. Letby says the TPN bag could have come from some other area than the neonatal unit.11:37am: The nursing staff rota for August 4-5 is shown to the court. Child F is in room 2, with Letby's colleague the designated nurse. Letby was in room 2 as the designated nurse for another baby. Letby says she cannot say how the insulin got in Child F, so "I don't think I can answer" if staffing levels played a part in the poisoning of Child F. Mr Johnson says Letby was "very keen" to ask police about the TPN bag said to have had insulin in it.
LL: "Because I was being accused of placing insulin in the bag - I thought someone would have checked the fluids."
LL: "I wanted them to check the bag, yes - I thought it would have been standard practice [on the unit]."11:42am: Mr Johnson says Letby had not been questioned about Child F and Child L in 2018, but was questioned about it in the following interviews. In it, Letby asked police about the nutrition bags said to have had insulin in.
NJ: "You knew very well the bags wouldn't have been kept, didn't you?"
LL: "No." Letby had said to police if there had been concerns over the bags, they would have been kept.
NJ: "You knew no concern had been expressed, didn't you?"
LL: "I didn't know no concern had been expressed at the time of this interview, no." Police had asked why Letby had asked about the nutrition bags. Letby had said to police there may "have been an issue with something else." Letby tells the court the issue may have been insulin coming from outside the unit. She says at that point it was not known where the insulin had come from, and it was not known if it was in the bags.11:59am: The trial is resuming after a short break.
12:12pm: Letby says she does not recall there were concerns for Child F's blood sugar level in her police interview in 2019. Mr Johnson says she was aware at the time. Text messages are shown to the court with Letby messaging a colleague about a low blood sugar reading.
NJ: "Had you seen something like this before? Babies having loads of dextrose and still having low blood sugars?"
LL: "Yes."
NJ: "You were trying to [place it as natural causes]."
LL: "I don't think I was trying to provide an explanation." Letby's message: "Wonder if he has an endocrine problem then."
Mr Johnson: "Does that mean natural causes then?"
LL: "Yes." Mr Johnson asks about the security of nutrition bags in the fridge, under lock and key. He says they are not safe from someone with a key who can inject 'a tiny amount of insulin' into the bag.
LL: "The bags are sealed and you would have to break the seal to do that." Mr Johnson asks if that would prevent someone from the previous shift from inserting insulin into the bag.
LL: "I can't say that as I wouldn't put insulin into a TPN bag." Mr Johnson says the prescribed bag must have been 'tampered with' between 4pm on August 4 and 1am on August 5. The replacement bag was a generic one. Mr Johnson describes how the insulin could be administered after the bag has been delivered to the ward. One method is after the cellophane wrap has been removed, to which he says that would mean there would be 'very few candidates' who could have done that.
NJ: "Why would you not put insulin in the bags?"
LL: "Because that would go against [all standard practice]."
NJ: "It is highly dangerous.
LL: "Yes."
NJ: "Life-threatening to a child."
LL: "Yes."
NJ: "Something that would never cross the minds of medical staff?"
LL: "At the time? No."12:14pm: Letby says she "cannot answer" if Child F was deliberately poisoned as she does not know how the insulin got there, who was there, or why.
12:15pm: Mr Johnson asks about the Facebook searches for Child E and Child F's mother carried out in the months after August 4, 2015. Letby says she got on well with the mother at the time, that she thought about Child E often, and wanted to see how Child F was doing.
12:22pm: Mr Johnson moves to the second insulin case, for Child L, who was a twin to Child M. Letby's defence statement said she had done nothing wrong and had not deliberately harmed either twin. Letby agrees this was a case when she challenged doctors if she believed the course of care being given was not correct. Letby said in her defence statement the unit was "exceptionally busy" on April 9, 2016, the day after Child L and Child M had been born. Letby said, at the time, she "could not understand" Child L's insulin levels at the time and "could not understand" why there was not an investigation at the time.
12:23pm: Letby denies 'using' the hypoglycaemic pathway not being followed as an 'opportunity' to attack Child L.
12:24pm: Letby says she accepts someone put insulin into the dextrose solution for Child L, and accepts there would be "no reason" for doing this, and that it would be "highly dangerous".
12:30pm: Letby accepts the blood results 'prove' insulin was placed in the dextrose solution. Prof Hindmarsh had previously given evidence to say insulin had been administered between midnight and 9.30am on April 9.
NJ: "Do you accept that?"
LL: "Yes."12:34pm: Mr Johnson says the insulin administered to Child L was a 'targeted attack' as the dextrose bag had been in place since noon on April 8. "It follows that insulin was administered while the [dextrose] bag was hanging, doesn't it?"
Letby: "I don't know." Mr Johnson talks through the process and repeats that, from evidence, the bag must have been in place when insulin was administered.
LL: "If that's what the expert suggests, yes."
NJ: "It follows that it was a targeted attack?"
LL: "I can't answer that."12:38pm: Mr Johnson says the only two staff members on duty for both days, when Child F and Child L were poisoned with insulin, were Letby and Belinda Williamson [Simcock]. A staffing rota for the April 9 day shift is shown to the court. Child L and Child M are in room 1, with designated nurse Mary Griffith. Letby is designated nurse for two other babies in room 1. Belinda Williamson is the designated nurse for three babies in room 3. Four babies are in room 2 and four babies are in room 4.
12:49pm: The neonatal schedule for April 9 is shown. Mr Johnson says it is to show what Lucy Letby was doing between 9am-9.30am. The schedule shows Letby was a co-signer for medication for one baby in room 2, and giving a feed to her designated baby in room 1. Letby was the co-signer for medication for a room 1 designated baby around 9.10am. Mr Johnson says a series of prescriptions for three different babies at 9.25-9.29am, co-signed by a nursery nurse and Mary Griffith, gave Letby the "opportunity" to administer the insulin for Child L. Letby says: "No, I don't know how the insulin got there." Mr Johnson says it has already been established the insulin was administered on the unit, on the bag that was connected to Child L throughout that time.
NJ: "That's what it's a targeted attack, isn't it?" Letby pauses.
NJ: "What do you say?"
LL: "Not by me it wasn't." Letby says she can "only answer for herself" in relation to the accusation by Mr Johnson that the insulin poisoning for Child F and Child L "can only be you or Belinda Simcock".12:57pm: Mr Johnson says despite the fact the bag was changed at noon on April 9, the insulin kept being administered to Child L, "didn't it?"
Letby: "Yes." Mr Johnson says "we know that" because the blood sample taken to the lab was taken at 3.45pm "contained exogenous insulin".
Letby: "I can't recall." Mr Johnson says Child L was targeted with a second bag of insulin.
Letby: "I'd have to be guided by the evidence - the expert evidence." Mr Johnson says a third bag is hung up at 4.30pm. The hypoglycaemia "continued". Letby agrees. The fourth bag, hung up the following day "when you [Letby] were not working" was put up, and the hypoglycaemia "gradually resolved". Letby agrees.12:58pm: Mr Johnson says the reason for the hypoglycaemia was that someone had poisoned Child L through 'at least two' bags of insulin.
LL: "Yes."
NJ: "And that was you, wasn't it?"
LL: "No."2:16pm: The judge, Mr Justice James Goss, has entered the courtroom. The jury have been sent home as one of the jurors is unwell.
2:19pm: The court is told the trial will not be hearing new evidence in the cross-examination this afternoon or tomorrow (Tuesday).
Tuesday 6th June 2023 - no court (juror unwell)
Wednesday 7th June 2023
Cross-examination of Lucy Letby by Nick Johnson KC - Day 8
Children M & NChester Standard Live Reporting
10:32am: The trial is now resuming, with the 12 members of the jury in attendance. Nicholas Johnson KC is continuing to cross-examine Lucy Letby, turning to the case of Child M. Letby confirms there is nothing she wishes to change in her evidence given in cross-examination so far.
10:36am: Mr Johnson says for Child M, Letby - in her defence statement - said Child M 'was slotted into a space' in nursery room 1 which was 'full'. Child M was 'apnoeic', and it was not known if he had a desaturation. A crash call was put out, and Child M was turned around in an incubator by a nursing colleague, to get him on to a monitor. Letby added she did not notice any skin colour changes in Child M at the time.
10:45am: Letby said in her statement she had written notes on Child M's resuscitation on a paper towel which ended up in her pocket and were taken home with her. Letby tells the court it would have been used to write up [nursing] notes. Letby says Child L and Child M 'stood out' in her mind at the time, as they were the first twins delivered where she was the allocated nurse. Letby agrees Child M was 'not an intensive care baby' and had been doing well. Asked if staffing levels were a contributory factor in Child M's collapse, Letby says the "unit was very stretched" during the April 9 shift. She adds she does not know what caused Child M's collapse. Asked to clarify by Mr Johnson, she says it "was a potential" factor. Letby tells the court Child M had been in a corner unit in a full nursery, and "as nursing and medical staff we were very stretched that day". Staffing "was not at a great level". Letby says she "does not know" what caused Child M's collapse, so rules out a mistake by staff. She says it is "hard to say" if staff competencies were a factor in the collapse.
10:47am: Mr Johnson says Dr Ravi Jayaram observed skin colour changes in Child M at the time of the collapse. He says "because [Child M] was darker skinned, it was more obvious." He said Child M was pale with pink 'blotches' on the torso that would 'appear and disappear'. He said he noted the most 'obvious' patches on the abdomen. "I noted them when I got there at the start of the resuscitation". He added he had only seen that once before, in the case of Child A. Letby says "I did not see anything like that, no".
10:51am: Letby is asked if the lighting was an issue in nursery room 1. Letby had told police in interview the lighting was "poor" in room 1, and she tells the court she has an independent memory of that event. Child M was "in a darker corner of the nursery", Letby tells the court. She added to police: "I do remember his [Child M] colour being harder to assess as he was an Asian baby." Letby tells the court the colour change, if any, was more difficult for her to see.
10:53am: Mr Johnson asks why was it necessary for Child M to be in a corner of room 1 if there were four babies in there for a capacity of four. Letby says there always needs to be an incubator free for emergency admissions in room 1. There were four babies in nursery room 2, three in nursery 3 and four in nursery 4. The court hears the neonatal unit was "at effective capacity".
11:01am: The court is shown a clinical note by Dr Anthony Ukoh, made at 10.25am on April 9. Letby says she does not remember if she had involvement with Child M at this time. Child M was not Letby's designated baby on this day. A neonatal schedule for Letby on April 9 shows a number of duties Letby had for her designated babies in room 1 between 9am-9.11am. Letby says one of the designated babies was "not a low-maintenance baby", with complex cannulation issues, and was on the ward for a long time. Mr Johnson says Letby has an "extraordinary memory" for this baby, seven years on, but not for Child D, who had died.
11:07am: The court is shown a 1.5ml bile-stained aspirate is recorded for Child M, following which Child M was nil by mouth, and the nasogastric tube was put on free drainage. Mr Johnson says at 3.30pm, a 10% dextrose fluid bag is started for Child M. Letby agrees with Mr Johnson there is nothing to suggest insulin was put in this bag. Letby says she cannot recall what Mary Griffith was doing at this time. Mr Johnson suggests this was when Ms Griffith was collecting a blood sample for Child L to be 'podded' and sent to a laboratory for analysis.
11:14am: Letby says she "couldn't say" how long it would take to draw up a 12.5% dextrose solution, which in this case was for Child L, the twin of Child M. Letby agrees it would have been after 3.45pm that that process would have started. Letby denies that it was around 3.45pm that she "sabotaged" Child M. Mr Johnson says the twins' mother said in an agreed evidence statement, she had to be taken back to the unit in a wheelchair, having been alerted by nurse Yvonne Griffiths, and she observed "one of the doctors was pressing [Child M's] chest." Mr Johnson says this is another case where a baby collapsed when the parents were away. Letby says she was with Mary Griffith at the time of Child M's collapse. Letby agrees Child M recovered quickly following the collapse. Letby says she did not see skin discolouration, and it was not discussed at the time.
11:18am: A colleague had previously told the court Child M's blood gas record sheet was disposed of in a confidential waste bin. Asked how it had ended under Letby's bed at home, Letby says she has never taken anything out of the confidential waste bin. Letby says she does not know how many blood gas records she has taken home. She says it has been put in her pocket and taken home with a handover sheet. She says she "probably" put it in her pocket, and put it under her bed. Asked why,
Letby replies: "Because I collect paper". Letby says household bills and bank statements would be shredded as they were 'there and then'. Other sheets such as handover sheets were not thought about.11:24am: Dr Ukoh's records on the resuscitation for Child M are shown to the court. Mr Johnson says the record is "meticulous", including six adrenaline doses. Mr Johnson says the data for the resuscitation efforts is on the paper towel [that Letby took home], which Mr Johnson says he must have had in his hand at some point. Letby agrees. Mr Johnson says that was in his hand at 8.25pm when he wrote up his notes. Letby said she had to stay late that shift for the handover and writing up medical notes for Child M. She denies "waiting an hour and a quarter" to write up those nursing notes or "hanging around" to get the note Dr Ukoh had when writing up the note. Letby denies "rooting around in the bin" for the blood gas record for Child M to take home. She also denies sabotaging Child M.
11:25am: Mr Johnson is now turning to the case of Child N, born on June 2, 2016. Letby, in her defence statement, says she had never encountered a baby with haemophilia before, and no-one on the unit seemed specifically to know how to care for such a baby. She says she does not believe Child N 'collapsed', and it was not accurate to say he had screamed for 30 minutes. She denied causing any harm to him.
11:30am: Letby tells the court she does not believe this event, for Child N, was a collapse which required resuscitation. The court is shown the nursing rota for the night shift of June 2-3. Letby was designated nurse for two babies in room 4. Child N was in room 1 with one other baby - the designated nurse for both babies was Christopher Booth. Letby rules out staffing levels or incompetence as factors in Child N's collapse. Letby agrees Child N collapsed just after Christopher Booth went on his break. Letby denies she was 'bored' or had 'time on her hands' working in nursery 4 that shift. She agrees Child N 'was in good shape' at the start of the shift.
11:54am: The neonatal schedule for June 2-3 is shown, with Letby's duties for her two designated babies from 8.30pm-8.38pm. One of the designated babies received a 50ml NGT feed at 8.30pm as they were asleep. Letby says that feed can take '10-15 minutes or so'. She says she can't put a 'definitive number' on it. Mr Johnson says other estimates for this kinds of feed have been 20 minutes.
Letby: "I really can't say." Mr Johnson says Letby was texting her friends 'right through this shift'. A sequence of messages is shown to the court. The first sent by Letby is at 7.33pm, followed by 7.35pm, 7.58pm, 7.59pm, 8pm ['We have got a baby with haemophilia'], 8pm, 8.01pm, 8.02pm, 8.03pm, 8.04pm [Ah ok I'll have to Google it later lol don't know much about it [haemophilia]], 8.06pm, 8.11pm [Complex condition, yeah 50;50 chance antenatally].
NJ: "That is where you got the answer from, Dr Google?"
LL: "No, '50:50' is something staff would know"
Messages are sent by Letby at 8.26pm [Ffs Mel asking me how to make up 12.5%], Letby said she was "shocked" that a band 6 colleague was asking her how to make up such a solution, when she could have looked for herself.
8.29pm: 'No I've passed her folder but now asking if can run via cannula- she needs to look herself!'
Letby says she was "not happy" with Mel.
Another message is sent from Letby at 8.29pm, and at 8.31pm, and 8.31pm, at 8.32pm, 8.34pm.
Letby is asked how she can feed a baby at 8.30pm when she was also texting.
LL: "You can't."
Letby denies feeding the baby "very quickly" by putting the plunger on the end.
Another message is sent from Letby at 8.38pm [Had strange message from [doctor colleague] earlier...']
Mr Johnson asks if Letby's nursing colleague was implying Letby and the doctor were in a relationship.
Letby says she does not know.
Letby's colleague sent two messages: "Did u? Saying what?"
"Go commando? 😂"
Letby is asked by Mr Johnson if she knows what the implication of 'go commando' means.
LL: "I don't know what was meant, I can't say right now."
NJ: "Do you think this was an army reference, being from Hereford?"
LL: "I don't know."
The messages are sent by Letby at 8.39pm, 8.40pm, 8.41pm, 8.43pm [Do you think he's being odd?], 8.44pm [Shut up!], 8.44pm [I don't flirt with him!].12:03pm: The text message conversation was:
Letby: 'Had strange message from [colleague] earlier....'
Reply: 'Did u? Saying what?'
Letby had replied at 8.39pm: '😂😂😂😂'
LL: 'Asking when I was working next week as wants to talk to me about something, has a favour to ask..?'
Reply: 'Think he likes u too'
Reply: 'Hmm did u not ask what it was?'
LL: 'No just said when I was working and he said wants my opinion on something'
LL: 'Hmm...🤔''
Reply: 'Hmm'
LL: 'Do you think he's being odd?'
Reply: 'Thought as flirty as u'
LL: 'Shut up!'
Reply: 'What?!'
LL: 'I don't flirt with him!'
Reply: 'Ok'
LL: 'Certainly don't fancy him haha just nice guy'
Reply: 'Ok'12:11pm: Mr Johnson says Letby was 'texting non-stop' on the nursery room. Letby says the feed "must have happened at a different time". She says she cannot answer when. She denies 'pushing it through' the feed. Mr Johnson says Child N collapsed at 1am. Christpher Booth 'one episode whilst I was on my break, whereby infant was crying++ and not settling. He became dusky in colour, desaturating to 40s. Responded to facial oxygen within 1-2 minutes. Crying subsided within approximately 30 minutes and colour returned to normal...' Letby tells the court this was not a 'collapse' as facial oxygen was all that was required, not resuscitation.
12:14pm: Mr Johnson says Dr Jennifer Loughnane had a 'look of surprise' in court when she had read her note she had written Child N was 'screaming', as that was unusual. Letby says she does recall that. She denies sabotaging Child N.
12:23pm: Mr Johnson turns to the second set of events for Child N on June 15, when the plan was for Child N to go home that week. Letby agrees he only needed phototherapy at this stage. A feeding chart is shown for Child N, who was being fed mostly expressed breast milk. Child N's mother had visited on the morning of June 14, and in the evening, at 5.15pm. Child N had taken a 60ml bottle feed. Letby agrees with Mr Johnson this was "a very good sign". Mr Johnson suggests Letby did something to destabilise Child N before the end of her day shift.
LL: "No I did not." Letby says it was a "coincidence" Child N was, according to nursing notes that night "very unsettled early part of night", with observations of mottling.12:26pm: Letby is asked about a message sent by a nursing colleague at 5.26am which said 'Baby [N] screened, looks like [s***]'
Letby responded: 'Oh no'
Letby denies she saw this as an opportunity to sabotage Child N during the day shift.
LL: "No, that's not what happened."12:29pm: Letby messaged a doctor colleague at 6.04am on June 15: 'Wonder if I'll find my way back into 1 today then....',
This is in response to his message at 5.53am, which begins: 'What a chaotic 7 hours! Sorry - I may have filled NICU [...] Have a good breakfast 😉 I think your day may be busy.'12:41pm: Swipe data shows that Letby is on the neonatal unit at 7.12am. Child N desaturated three minutes later and was 'crying'. Letby says she does not recall Child N crying. She says, at the time, she was in the doorway, talking to Jennifer Jones-Key - her friend, when the alarm for Child N went off. Letby says it "was very busy" and "a lot of intervention was needed" for Child N after he collapsed. She does not cite staffing levels as a contributing factor for the collapse, or a mistake by medical staff. Letby says she "does not know" if issues with intubating Child N were a factor, and does not know what caused Child N to collapse. She denies "setting up" Child N to collapse overnight.
12:45pm: Letby, in her defence statement, said she had gone to nursery room 3 not to see Child N specifically, but to speak to Jennifer Jones-Key, her friend. She said Child N was 'blue' and 'not breathing'. She shouted for a doctor colleague to assist and Neopuff breathing assistance was applied. Letby is asked about the 'Jennifer and I were talking at the doorway'. Letby says she meant only she was at the doorway, and Jennifer Jones-Key was in the nursery room.
12:48pm: Letby, in a Facebook message to a colleague: 'No repeat today. I've escaped being in 1, back in 3' at 7.12pm. Mr Johnson says Letby had gone in to room 3 as she knew by that point she was designated babies for that room. Letby says she had gone to see her friend. Letby denies sabotaging Child N. Letby agrees it was a "serious event" which happened "within a minute or two" of her entering the room. Mr Johnson says it was "bad luck?"
Letby replies: "Yes."12:59pm: Mr Johnson asks Letby when blood was seen orally on Child N. Letby replies "the only time definitively" she recalled that was at 3pm. she says that is on her memory "sitting here now". Mr Johnson says if she had recorded blood observations at the time, would she accept that now? Letby says she would, although it may have been based on what people had informed her at the time. Mr Johnson says the one who would have informed her would have been the doctor colleague she "loved as a friend". Letby's nursing note: '...infant transferred to nursery 1 on handover. Mottled, desaturating requiring Neopuff and oxygen.' Letby says "both" she and Jennifer Jones-Key had gone over to Child N at the time of desaturation. Mr Johnson says Letby was "hoping to create the impression" on the nursing notes that the problems for Child N happened before the handover.
LL: "No, I disagree." Letby tells the court she had taken over Child N's care from 7.30am.1:01pm: Letby's note, written at 1.53pm-2.10pm adds: 'unable to intubate - fresh blood noted in mouth and yielded via suction ++'. Letby says the 3pm blood observation was the first one she could "definitively remember". Mr Johnson says this note is a 'good hour' before that observation. Letby denies Child N was bleeding from when she first got involved that day.
2:13pm: The trial is now resuming after its lunch break.
2:22pm: Letby says she knows there was blood recorded prior to 3pm. Mr Johnson says the doctor colleague recalled, in evidence, seeing blood before the intubation process at 8am. Benjamin Myers KC, for the defence, rises to say that in cross-examination, the doctor colleague did not rule out the possibility the blood was present after the attempt to intubate. Mr Johnson says there was an attempt to intubate at 8am. Letby agrees. Letby also agrees with the observation there was swelling at the back of Child M's throat. She says she "cannot comment" further on what the doctor colleague saw.
2:24pm: Letby recorded in her notes, written at 1.53pm retrospectively: '...unable to intubate - fresh blood noted in mouth and yielded via suction ++' Mr Johnson says the doctors could not see, for the blood. Letby says she cannot say what doctors observed. Letby agrees that evidence from Professor Sally Kinsey ruled out 'spontaneous haemorrhage' for Child M at this time.
2:35pm: Letby is asked about family communication with Child N's parents. A note by Letby at the time: 'Parents were contacted by S/N Butterworth during intubation. Both mobile phones switched off and no answer on landline. Message left. Call returned shortly after and parents were asked to attend. Have been present since. Both understandably upset...' Agreed evidence said Child N's mother had said Lucy Letby had been in contact with them. Letby says "it's a difference in recollection". Mr Johnson says this is agreed evidence, it's the truth. He says Letby's note "is a lie".
Letby: "no, it's not." The mother recalled Child N 'had a bleed and was unwell', and said Letby had informed the parents of this.
Letby: "No, I disagree."
NJ: "But it's agreed evidence."
LL: "Well, I disagree with it now." Mr Johnson says this is another account from a parent which Letby says is untrue. Mr Johnson says Letby has been 'firing out post-it notes from the dock' during the trial, but had not raised this issue at the time.
LL: "I'm not sure."
NJ: "Is the answer no?"
LL: "It's not something I raised with my legal team."
Letby: "I don't want to comment on whats, ifs and buts." Mr Johnson says Letby interrupted when the mother of Child E and F gave evidence, to say she couldn't hear, and wanted to leave the courtroom when a doctor colleague began to give evidence.
LL: "Yes, because I felt unwell." Mr Johnson says: "No, no..." adding that it was because it was her boyfriend who was giving evidence.
Letby: "That's not fair." Mr Myers rises to say the line of questioning is inappropriate, and asks for the opportunity to consider the issue raised [of a dispute in agreed evidence].2:39pm: Letby adds she did not make the phone call to Child N's parents, and denies making false entries in the paperwork. An intensive care chart is shown for Child N on June 15, saying at 10am '1ml fresh blood'. Letby says she "cannot say" if it was a vomit or aspirate. The note is in Letby's handwriting. Letby is asked what she did about it.
Letby: "I cannot say right now."2:42pm: Mr Johnson asks what would Letby do if fresh blood was observed in Child N's mouth?
LL: "I don't know if it was in the mouth." Letby adds such an observation would have been escalated, but she does not know who to. Mr Johnson says there is no record of it being escalated. Letby agrees there is no "written record", but it may have been verbally escalated. She says 1ml fresh blood is not normal but not a life-threatening event. Mr Johnson says for a baby with haemophilia, it was serious. Letby says it would be a concern, and would be escalated.2:46pm: A doctor in the ward does not record the bleed during the ward round, the court is told. Mr Johnson says Letby has "invented" the blood reading for 10am.
Letby: "I disagree." Mr Johnson suggests it was all designed to give an ongoing impression for a child with haemophilia. Letby disagrees.2:48pm: Letby says it's true that an NG Tube can cause "a small amount" of bleeding in the mouth. Letby says she cannot say if she didn't escalate it [the bleed in Child N] verbally.
2:51pm: A Facebook message from Letby is sent to a doctor colleague at 11.29am on June 15. Small amounts of blood from mouth & 1ml from ng. Looks like pulmonary bleed on Xray. Given factor 8 - wait and see. Apnoeas have improved & gases good, colour & perfusion still not Great. If deteriorates will try to intubate.' The x-ray report ruled out a pulmonary bleed. Letby says this report came some time later. Mr Johnson suggests either there wasn't a problem at all, that Letby was making evidence up, or Letby was causing the problem. Letby disagrees.
2:54pm: Mr Johnson says a statement from the parent of Child N said the collapse was so serious a priest was offered. Mr Johnson says this collapse must have been the one at 2.50pm. Letby noted: 'approx 1450 infant became apnoeic, with desaturation to 44%...fresh blood noted from mouth and 3mls blood aspirated from NG tube...drs crash called...'
NJ: "What had you done to cause this in [Child N]?"
LL: "I hadn't done anything."2:59pm: Letby denies "shoving a foreign object" down Child N's throat.
Letby: "Absolutely not."
NJ: "It's all your work, isn't it?"
LL: "No it's not at all." Letby agrees she was 'agitated' by the need for assistance from Alder Hey, as she had not known a case before of people from another hospital coming in to assist.
NJ: "Do you remember saying 'who are these people?' 'who are these people?'"
"Yes, because I had never experienced who these people were [coming in from a different hospital.] ...It was a completely new experience." Child N later collapsed once more. She denies using the doctors being in a 'huddle' as an 'opportunity' to try and kill Child N again.
Thursday 8th June 2023
Cross-examination of Lucy Letby by Nick Johnson KC - Day 9
Children O, P & QChester Standard Live Reporting
10:14am: The trial is due to resume at 10.30am.
10:41am: Nicholas Johnson KC, for the prosecution, moves to the case of Child O. Letby, in her defence statement, said she did "nothing to hurt [Child O]." She noted a "change in [Child O's] appearance", but it was "not dramatic". He had a deterioration and Letby noted Child O's abdomen was "red and distended". She says she didn't notice a rash on Child O, and no-one mentioned it. She said the abdomen was "very swollen", and there was a struggle to get lines in. Letby tells the court one of the lines had tissued. She said one of the doctors had gone out to smoke a cigarette during the time of Child O's resuscitation, and when that doctor returned, they did not wash their hands.
10:43am: Letby is asked if there is anything she wishes to change in her account of evidence so far. This is a question Mr Johnson asks at the start of most sessions during the cross-examination. Letby says there is nothing.
10:45am: Letby agrees with Mr Johnson it was "big news" to see naturally conceived triplets on the unit, as it was a rare occurrence. Child O and Child P were two of the three triplets. Messages are shown to the court between Letby and Jennifer Jones-Key from June 22. Letby confirms when she is back in, adding: "Yep probably be back in with a bang lol" M Johnson says within 72 hours of that, two of the triplets were dead and Child Q had collapsed.
10:48am: Letby is asked why she was "so interested" in the triplets. Letby tells the court it was "general conversation" between staff colleagues as it was "something unusual on the unit". She accepts that all went well with the birth, and accepts that the triplets had been doing well, with Child O being "fine". Letby accepts that Child O was doing well on the night shift for June 22-23, and had been moved off CPAP on to Optiflo breathing support. Letby accepts Sophie Ellis's description there was 'nothing concerning' about Child O's presentation.
10:56am: Letby is asked to look at an observation chart for Child O for June 22-23. There is a reading which, the court is told, appears to have been changed from '1430' to '1330'. Letby says Child O's temperature is a little unstable in the hours prior to 1.30pm on June 23, but accepts he was otherwise "stable". The court is shown a lab result, that there was no bacterial infection found in a blood sample taken on June 23 for Child O. A feeding chart showed Child O was "tolerating his feeds very well", Mr Johnson says. Letby agrees.
11:05am: Mr Johnson asks Letby where the 'problem' is for Child O's abdomen that she had said was not dealt with, as there is no data to show it. Letby says, after looking at the data, she does not know what the problem was. Mr Johnson says there is no problem shown in the paperwork. Letby says there was "no formal note" made. The court is shown Sophie Ellis's note at 7.32am: Abdo looks full slightly loopy. Appeared uncomfortable after feed....reg Mayberry reviewed. Abdo soft, does not appear in any discomfort on examination. Has had bo. To continue to feed but to monitor.' Letby says the doctor did not formally record it. Letby accepts a review was carried out at 9am and Child O's liver was reviewed, finding no injury. Letby accepts the liver injury happened 'on her watch'. She says she accepts it happened on her shift, but does not know how it happened. She denies it happened on her hand.
11:07am: A shift rota for June 23 is shown. Letby was designated nurse for two of the three triplets in room 2 - Child O and Child P - plus one other baby. The third triplet was in room 1, with Child Q and two other babies. Letby rules out staffing levels as a contributory factor in Child O's collapse or death, or staffing mistakes.
11:17am: Letby says Rebecca Morgan was a student nurse on the unit. She accepts that the student nurse would not always be in room 2, and would sometimes be chatting to parents. Letby says the two triplets she was designated nurse for were in the high-dependency room, and if she left the room for a period of time, she would ask someone to 'keep an eye' on them. A note by Dr Katarzyna Cooke at 9.30am is shown to the court, which included: 'No nursing concerns, observations normal'. Letby says she left the unit at one point to get donor milk for the babies. Letby is shown a series of text messages between herself and a doctor prior to 9.30am. Letby expresses disappointment in the message the doctor will not be on the unit ['Boo']. Letby says she got on well with the doctor. Letby asks if the doctor would be on the unit in the afternoon in the message. She adds: 'My student is glued to me.....' She adds: 'Bit rubbish that you couldn't stay on nnu'. Mr Johnson asks if Letby was 'missing' him. Letby replies this was the first day back from her Ibiza holiday. Letby sent a message at 9.55am: 'I lost my handover sheet - found it in the donor milk freezer!! (clearly I should still be in Ibiza)' Letby is asked if it was a 'busy' morning for her. She says "reasonably, not exceptionally". Letby is asked how she finds the time to text when at work. She says she would not use her phone at the cotside or a clinical area, but would use her phone elsewhere in the unit.
11:24am: A feeding chart for Child O is shown to the court. Letby is recorded as signing for feeds at 10.30am and 12.30pm. She says the writing above is not by her, but by Rebecca Morgan. She says if she has signed, then Rebecca Morgan does not need to sign. Letby denies feeding Child O. She denies overfeeding Child O. Nurse Melanie Taylor, at about 1pm, entered room 2 and said 'he doesn’t look as well now as he did earlier. Do you think we should move him back to [room] 1 to be safe?' Letby declined. She said she doesn't remember being very dismissive. Letby says "That's Mel's opinion" to the evidence that Melanie Taylor had told the jury she felt Letby was 'undermining her authority'. She adds that Melanie Taylor had the right to override that and 'take Child O off her'. Letby denies she had sabotaged Child O, or that this would have meant Child O would have 'escaped her influence'.
11:29am: Letby denies she 'lied' to the doctor colleague about a 'trace aspirate' for Child O at 12.30pm. Mr Johnson says he is mistaken, as a doctor's note records '0 bile' for the 'trace aspirate'. Letby says the 160-170 heart rate for Child O, as recorded by the doctor, is higher than normal, and higher than ideal. Mr Johnson says the abnormal readings start, on the observation chart, 180bpm. Letby had recorded 'tachycardiac' for Child O. Letby tells the court when she reviewed Child O, there was a spike in the heart rate, and in her opinion, Child O was tachycardiac.
11:33am: Mr Johnson says Letby made a 'false, lying entry' in a different chart. A blood gas chart is shown to the court for Child O. Mr Johnson asks where the lying entry is on the chart.
LL: "I don't know." Mr Johnson points to the 'CPAP' note on a column. Letby says Child O had some CPAP pressure. Mr Johnson says Child O had not been on CPAP breathing support for "hours and hours".
NJ: "You were covering for air you had given him, weren't you?"
LL: "No." An x-ray report for Child O is shown, including: 'Moderate gaseous distention of bowel loops throughout the abdomen.' Letby is asked why she wrote CPAP in her notes.
LL: "I can't answer that now, I don't know." Letby says she does not know if Child O might have been on some CPAP pressure via Optiflo. Letby denies 'forgetting to make a false entry on the observation chart'.11:41am: Letby is asked about messages exchanged between her and a doctor when, at 2.30pm, she was recorded as taking observations for Child O. The messages were sent at 2.20pm and 2.23pm. Child O collapsed shortly after 2.40pm. In her defence statement, she said the doctor colleague was on the unit at the time. Swipe data shows Letby has arrived on the neonatal unit from the labour ward at 2.39pm. Letby says she cannot say, definitively, where she was at that time. She denies 'nipping out' of the neonatal unit to make it look like she was elsewhere at the time Child O collapsed.
11:44am: The doctor's note is shown to the court: 'Called to see [Child O] at ~1440 desaturation, bradycardia and mottled...' Letby says she believes she called the doctor to the nursery room. She denies it was to get personal attention; Letby says it was because he was there to assist Child O.
12:09pm: The trial is resuming after a short break. Letby says a 20ml saline bolus was given to Child O in response to a poor blood gas record. She says there was a delay as there was an issue with getting the line for Child O. She says she believes the bolus, which has 'time started: 1440', was in response to Child O's collapse. A doctor's note recorded for the '~1440' collapse: '10ml/kg 0.9% sodium chloride bolus already given.' Letby agrees the two desaturations for Child O that day were "profound" ones. Letby's note: 'Approx 1440 [Child O] had a profound desaturation to 30s followed by bradycardia. Mottled++ and abdomen red and distended. Transferred to nursery 1 and Neopuff ventilation commenced. Perfusion poor' Letby, when questioned, says babies would "frequently desaturate", to this level, and this happened prior to June 2015, and "often".
12:14pm: Letby says the redness to the abdomen on Child O was abnormal, and the description of mottling was normal. Mr Johnson says during the intubation, Dr Stephen Brearey, in evidence on March 15, said Child O had a rash on his chest, on the right side, about 1-2cm in size. He said it was an "unusual" rash that was initially purpuric, and it later disappeared. Letby says: "I don't believe that's what I saw. I saw mottling. If that's what Dr Brearey saw, then if that's what you could take as being true, then yes."
12:20pm: Mr Johnson says when the doctor went to see Child O's parents, and during that time, Child O desaturated again, for the final time. Letby says she does not remember this declining moment, but said she put out a crash call.
LL: "I remember the death, but not this precise moment where he declined and I put out a crash call." Child O was intubated and efforts were made to resuscitate him. Letby says she did not recall seeing the rash disappear. She says she did not see what Dr Brearey and Dr Ravi Jayaram had seen. Letby says she did not pull an NG Tube out of Child O's stomach. An x-ray report for Child O is made at 4.46pm. It record: 'NG Tube in situ with its tip close to the cardia, this should be advanced by 10-15mm.' An earlier x-ray report said the NG Tube was 'in a good position'. Letby says a dislodged tube would still drain, as it would still be in the stomach. Letby says the tube could be moved during the intubation process at 2.40pm.12:24pm: Mr Johnson says Child O's mother, in agreed evidence, said her baby was 'changing colour' with 'prominent veins.' She says she later saw that in Child P. Letby says she didn't see that herself. The father of Child O said 'you could see his different veins - it looked like he had prickly heat, like something oozing through his veins'. Letby says she did not see anything like that. She accepts she saw a red-purply blotchy rash and a red abdomen.
12:28pm: In police interview, Letby said she believed she had done chest compressions and drew up some drugs. Letby says after looking at records, she now believes she was just involved in medications. Mr Johnson suggests Letby is distancing herself from the CPR so it could not be said she caused the liver injury to Child O. Letby denies this. Letby says she "does not know" how Child O got the liver injury. Letby denies injecting air into Child O to cause an air embolus, or inflicting a liver injury on him.
NJ: "These things all happened on your watch, didn't they?"
LL: "Yes." Letby says she disputes an account that Dr Brearey told her not to come in after that shift.
NJ: "Were you bothered by what you witnessed?"
LL: "Of course I was bothered."12:35pm: Messages are shown between Letby and the doctor from 9.14pm on June 23: Doctor: 'Your notes must have taken a long time - Had you documented anything from this morning?'
LL: 'Only a little. Had the other 2 to write on as well and sorting out the ffp etc. Left signing for drugs until tomorrow' A nurse also messaged Letby: 'F***in hell, what happened?'
LL: 'Can't Think straight so took a while'
LL: 'Blew up abdomen think it's sepsis' Letby says it's not a term she uses often, but she had seen it before.
LL: 'Had big tummy overnight but just ballooned after lunch and went from there' Letby tells the court that is what she said, having been reviewed by a doctor and Child O had a loopy bowel. She says she is referring to distention found prior to 8am. LL, at 9.33pm: 'Worry as identical'
Mr Johnson: "Were you setting up a false narrative here?"
Letby: "No, that's not what I'm suggesting at all."
NJ: "You had already set your plan in motion by pumping air into [Child P] before you left."
LL: "No."12:48pm: Letby is asked to look at a Datix form she had written [a form used by staff when issues have been highlighted, such as clinical incidents], on the documentation ['Employees involved' has Letby's name]. The form said 'Infant had a sudden acute collapse requiring resuscitation. Peripheral access lost.' Dr Brearey said the information in the form was 'untrue', and he said he didn't believe at any point IV access was lost. Asked about this, Letby says: "Well, that's Dr Brearey's opinion." The form adds: 'SB [Brearey] wishes amendment to incident form - Patient did not lose peripheral access, intraosseous access required for blood samples only.' Letby says she does not believe her Datix report was untrue at the time.
NJ: "You were very worried that they were on to you, weren't you?"
LL: "No."12:53pm: Mr Johnson turns to the case of Child P, triplet brother of Child O. Letby, in her defence statement, denies hurting Child P. She said she did not recall having an argument with nursing colleague Kathryn Percival-Ward about working in room 1. She said she was in conversation with student nurse Rebecca Morgan when Child P collapsed. She said it was "chaotic" with all the staff arriving to resuscitate, and Child P was too poorly to be transferred to room 1, so was kept in room 2. Child P's stomach was 'red'. She says at some stage she pricked herself with a cannula needle and needed to go to A&E for treatment. While there, she said she fainted, she believed due to stress at the time of the past few days, and had not eaten. She said she had 'forgotten' she had taken a handover sheet home with her.
12:59pm: An examination of Child P at 10am on June 23, 2016 was "unremarkable", the court hears. Letby accepts that. She adds there was nothing of note during the day. Mr Johnson suggests Child P worsened after Child O passed away. Letby agrees. A 6pm feed for Child P is signed by Letby, and she says the writing above is not by her. Dr John Gibbs had reported in his 6pm review for Child P that the baby boy was doing well. A blood sample taken at 6.35pm taken to a lab showed no signs of infection. Letby denies overfeeding Child P 'at some point' between 5pm-8pm on June 23.
2:16pm: The trial is now resuming after its lunch break.
2:22pm: The cross-examination continues in the case of Child P. Letby agrees there were 'no problems' at the time of the handover for Child P on the night of June 23. She recalls the x-ray taken shortly after that handover. The x-ray report said: 'NG tube in satisfactory position...gas-filled bowel loops throughout the abdomen, through to the lower rectum, with no evidence of obstruction and no plain film signs of perforation' Letby denies pumping Child P with air. She agrees this was a deterioration for Child P. Medical expert witness Dr Owen Arthurs had previously told the court this image was "quite unusual" for a baby of that gestation. Letby says she cannot comment how the gas got there, only that she did not put it there.
2:24pm: A 14ml aspirate is recorded for Child P at the time of handover at 8pm.
NJ: "That was your doing, wasn't it?"
LL: "No."
NJ: "On your way home, you were sowing the seeds with your colleagues?" Mr Johnson refers to the 'Worry as identical' text message Letby had sent. "You were feeding a false narrative, trying to divert attention away from your homicidal activities?"
LL: "No."2:32pm: 5ml of air and 2ml of milk is aspirated from Child P at 7am. "How much milk had [Child P] been fed overnight?" Letby said Child P had been fed prior to midnight. She says if the NG Tube is in the stomach, air would come out. Letby disagrees that Child P was well at the morning handover time, as Child P was 'nil by mouth'. A police interview had earlier said Letby saying Child P was stable and well. Mr Johnson suggests Letby is deliberately making the appearance of Child P worse now than at the time she gave her police interview.
LL: "No."2:34pm: The day shift for June 24 is shown to the court. Student nurse Rebecca Morgan is on the rota. Lucy Letby is the designated nurse for Child P in room 2. The other surviving triplet is also in room 2, with designated nurse Christopher Booth. Child Q is in room 1 with two other babies. Three babies are in room 3, and three babies are in room 4.
2:36pm: Letby rules out staffing levels as a contributory factor in Child P's collapse and death. She also rules out staffing mistakes. She says there were "some issues with the chest drain", but "cannot say" how much of an effect that had on Child P.
2:40pm: By 0639, Sophie Ellis’ nursing note recorded that “abdo has been soft and non distended. 25ml of air aspirated by SNP Kate Ward. NGT placed on free drainage”. Mr Johnson says Letby created a false nursing note at 8am to say: "...abdomen full - loops visible, soft to touch." He says that is not the picture from 6.39am. Letby agrees that is not the same as Sophie Ellis' note. Sophie Ellis's note for June 23 for Child O: 'Abdo looks full slightly loopy...abdo soft.' Letby says her observation for Child P that morning was what she saw. She informed a doctor an hour later about the abdomen observation. She denies a suggestion by Mr Johnson that she is lying.
2:48pm: Letby says she escalated the observation to the shift leader. Mr Johnson asks if Letby knew what she was telling her friend, the doctor, at this point. Letby does not recall. The message shown to the court, sent at 8.04am: 'I've got [child] and [Child P], [Child P] has stopped feeds as large asps.' Mr Johnson asks why Letby is lying about having the first child, whose designated nurse was Christopher Booth. Letby says she would have to check the paperwork, as she may have been assisting. Letby's follow-up message, at 8.19am: '...I'm ok, just don't want to be here really. Hoping I may get the new admissions...' Mr Johnson asks why Letby didn't raise it with the doctor colleague who was coming into work. Letby says the doctor was not present in the neonatal unit that day. He went to the children's ward. Letby denies the observation was a 'fabrication' as Dr Anthony Ukoh saw loops as well. She said the context of 'don't want to be here really' was what she had seen earlier with Child O. Mr Johnson refers to Dr Ukoh's note of observation at 9.35am: 'Abdomen moderately distended/bloated; soft'. Mr Johnson says there is no mention of loopy bowels.
Letby: "No." Letby says Dr Ukoh might not have recorded it.
NJ: "Or you have misrecorded it."
LL: "No."2:54pm: Within a few minutes of Dr Ukoh reviewing Child P, Child P collapsed.
NJ: "That has to be your doing, doesn't it?"
LL: "No." Mr Johnson says Rebecca Morgan's evidence was Letby had left the room at the time of collapse. Letby says from her recollection, she was in the room, and is "quite clear" on that. Letby's note for the desaturation: '...[Child P] had an apnoea, brady, desat with mottled appearance requiring facial oxygen and Neopuff for approx 1min. Abdomen becoming distended.' Mr Johnson says the note is deliberately written to make it look like the Neopuffing made the abdomen become more distended. Letby agrees.2:57pm: Dr Ukoh, the court is told, gave evidence to say Child P was in a very different condition between 9.35am and 9.40am. He also said Letby was "very keen" for the doctor colleague to be called. Letby says this was because he had been present for Child O's deterioration. She adds it was one of the other doctors who suggested getting that doctor.
NJ: "Were you trying to attract [the doctor's] attention?"
LL: "No."
NJ: "Did you enjoy being in these crisis situations with [the doctor]?"
LL: "No....[doctor colleague] and I were friends.
NJ: "Something to share?"
LL: "No."3:02pm: Child P desaturated again at 11.30am. He was given adrenaline and he was paralysed with a drug to aid ventilation as he had been 'fighting the ventilator' with his breathing. A note in Letby's handwriting is shown to the court. It details the efforts to resuscitate Child P. It was found at her home. Letby accepts she had put it there.
LL: "I collect paper and that's where it ended up...I have difficulty with throwing anything away, particularly paper.
NJ: "Is there anything comforting in keeping the paper?"
LL: "I keep paper yes, from a variety of different sources." Letby clarifies she does not include bank statements in that. Letby was recorded by a nursing colleague as saying for Child P: "He's not leaving here alive is he?" Letby disputes that. "I don't recall the conversation."3:15pm: Child P's final collapse happened at 3.14pm, just after doctors had reviewed him. Letby says she cannot recall shouting for help, and cannot recall Child P's breathing tube being dislodged.
NJ: "The problem happened just after everybody left, just after you had said 'He's not leaving here alive is he?'"
LL: "I don't agree I said that.
NJ: "Is this another case of bad luck, that is happened just after everybody left?"
LL: "Yes."
NJ: "Did you enjoy making predictions when you knew what was going to happen?"
LL: "No."
NJ: "You were very excited in the aftermath of [Child P's] death?"
LL: "No, I was not." Mr Johnson says a female doctor colleague had said she acted 'in a totally inappropriate way'
LL: "No I didn't." She adds that was what the female doctor colleague had said. Letby says she told colleague Sophie Ellis "out of respect" what had happened. Mr Johnson said Sophie Ellis had been to the races - "why not leave her alone?". Letby said Sophie Ellis had texted her first.
Mr Johnson: "Did you enjoy the drama?"
LL: "No." Letby's response to
Sophie Ellis: 'Just blew tummy up and had apnoeas, downward spiral. Similar to [Child O] x' Mr Johnson said the message were identical to the one for Child O. Letby said that was what happened, his tummy blew up and he had apnoeas.
NJ: "Your portent of doom had fulfilled itself, hadn't it?"
LL: "No."
NJ: "At your hand."
LL: "No."3:30pm: The trial is resuming after a short break. Mr Johnson clarifies from a text message sent to a doctor colleague, Letby did have two designated babies at the start of that shift, one of whom was Child P. He now turns to the case of Child Q. Letby, in her defence statement, said she cannot recall much from the shift given what had happened in the previous days. She said she did not understand why feeding was continued for Child Q when it was not being digested. Letby said Child Q was sick and when she arrived, from the records, she aspirated 'air+++' from Child Q. She says she does not know how that air got there, and she did not cause it. Child Q was not put on a ventilator as there were concerns over NEC. She did not deliberately retain a handover sheet for Child Q. Letby says she would like to amend the statement, to say she was on duty after June 25, 2016.
3:33pm: Medical expert witness Dr Dewi Evans was challenged by the defence on his use of the word 'crashed' for Child Q, saying that was a 'gross exaggeration'. Letby says a more appropriate word for what happened to Child Q would be "deterioration". A doctor colleague had referred to the event, in a message, as an 'acute deterioration'. Letby said that would be accurate. She said the difference would be a crash would require a crash call being put out.
3:37pm: Mr Johnson says Child Q was transferred to nursery room 1.
NJ: "He was in a serious condition after that, wasn't he?
LL: "No I disagree."
NJ: "He needed one-to-one care, didn't he?
LL: "Yes, he was assessed as ITU care." The rota for June 25, 2016, at the beginning of the shift, is shown to the court. Child Q was in room 2, designated nurse Lucy Letby. One other baby is in room 2, with a different designated nurse. Letby was a designated nurse for a baby in room 1. Two other babies are in room 1. Three babies were in room 3 and four babies in room 4. Nurse Mary Griffith had designated babies in rooms 2, 3 and 4. Letby rules out staffing levels or staffing mistakes or medical incompetence as contributory factors for Child Q's collapse.3:40pm: Letby agrees Child Q required some breathing support at birth. She also agrees Child Q "made good progress" after birth, according to Mr Johnson.
3:43pm: Letby says, "other than some temperature issues", the overall condition of Child Q was positive. Child Q was looked after by Samantha O'Brien on the night of June 24-25, and Child Q was being fed 0.5ml of milk every two hours at 3am, 5am and 7am. A blood gas reading at 6.58am was "very good", Mr Johnson says. Letby agrees.
3:45pm: Letby adds there had been a 'slight increase' in the lactate, and the pH reading was slightly lower, but accepts it was a good reading overall. Letby said at the time of Child Q's handover on the morning of June 25: "There were concerns for his abdomen and his feeds." Asked who else had raised these concerns but her, Letby replies she does not know.
3:51pm: Letby had previously told her defence that, due to temperature concerns and aspirates, she wanted Child Q to be reviewed by doctors before feeding at 9am on June 25. The neonatal schedule shows Letby made observations for the designated baby in room 1 at 8.30am. She also co-signed for medication at 8.32-8.34am for a baby in room 3. At 9am, Mary Griffith is doing observations for a baby in room 2. An unsigned entry is made for Letby's designated baby in room 1 at this time. Also at this time, Letby is recorded doing observations for Child Q. Letby says she does not recall doing the observations or being interrupted. Mr Johnson says he uses the word 'interrupted' as swipe data shows Mary Griffith entering the neonatal unit at 9.01am. He suggests Letby pumped Child Q with some clear liquid while Mary Griffith was out. Letby denies this.
3:56pm: Letby is asked why she has only done 'half a job' for the 9am June 25 observation for Child Q.
LL: "I can't explain why I haven't filled the saturations."
NJ: "You were interrupted by Mary Griffith, weren't you?"
LL: "No, I don't know why those weren't filled in."4:00pm: Letby said she left room 2 to go to room 1 as she needed to attend to cares for the other designated baby just after 9am. Mr Johnson says that is a lie. Letby says the baby didn't need a nappy change, but that baby "was an intensive care baby who needed regular attention". Letby agrees she had not filled in the saturation readings, but otherwise 'the job was done' for Child Q's 9am observation.
4:05pm: Letby says she was not present in the room at the time Child Q vomited. She says she cannot recall aspirating air from the NG Tube afterwards, but may have done so. Letby's nursing note: '...mottled++. Neopuff and suction applied....air++ aspirated from NG Tube.' Letby says that information may have been relayed to her. She says the air in Child Q might have come from the Neopuffing process. Letby agrees it could be dangerous if the Neopuffing and suction was done if there was clear liquid in Child Q's system. Letby said Child Q had vomited over his bedding.
4:06pm: Child Q, in a doctor's notes, had “just vomited” and his oxygen saturation dropped to the “low 60s”.
NJ: "There was a concern that [Child Q] had inhaled some liquid, wasn't there?" Letby replies that is a concern any time a baby vomits.4:08pm: The doctor's observations with Child Q continue for 53 minutes.
NJ: "This was no everyday, minor desaturation, was it?" Letby replies it was not serious enough to require an emergency crash call.
NJ: "You pumped him with a clear liquid, didn't you?"
LL: "No."4:10pm: Messages sent to a nursing colleague from 1.13pm are shown to the court: '[Child Q] on CPAP' Minna has taken [other baby] off me so just got him. Almost had a tube earlier but gases improving'. Letby denies the event was 'trivial', saying Child Q had deteriorated but it was not on the same level as some of the other events that have been discussed, and did not need a crash call or resuscitation efforts.
4:15pm: Nurse Amy Davies recorded on June 25, 2016 for the night shift that Child Q had "settled".
NJ: "He became much better, hadn't he?" Letby agrees.
NJ: "A child that was put in your hands in good condition, left your hands in a ventilator in intensive care, but by this time was returning to normality." Letby says by the night shift, Child Q was still on a ventilator and had a poor blood gas record on 6.23pm.
NJ: "You had nearly killed him, hadn't you?"
LL: "No, I hadn't nearly killed him." Letby says she was later concerned she was being blamed for something that did not happen, by leaving the nursery room unattended.
NJ: "The truth is that you pumped him [Child Q] with liquid and air?"
LL: "No."
NJ: "Because you tried to kill him?"
LL: "No, I didn't."
Friday 9th June 2023
Cross-examination of Lucy Letby by Nick Johnson KC - Day 10
What happened next - other matters (Facebook searches, Dr A, social life, notes etc)
Re-examination by Ben Myers KC for the DefenceChester Standard Live Reporting
10:15am: The trial is due to resume at 10.30am.
10:28am: There will be a delay to the start of the trial before the jury this morning. It is now due to begin at 10.55am.
11:03am: The trial is now resuming. Nicholas Johnson KC, for the prosecution, is continuing to cross-examine Lucy Letby. Before that begins, Benjamin Myers KC, for Letby's defence, rises to make a statement. He says Letby was cross-examined on a telephone call it was alleged she had made to Child N's father. Letby had disputed what the court said was agreed evidence. Mr Myers says the dispute was raised by Letby in advance with them, and it was the defence team's mistake to agree that evidence in advance.
11:07am: Mr Johnson says Letby said, in evidence, she found she was not going back to the neonatal unit the day before she went back to work on June 27, 2016. Letby agrees. Letby says at the end of June 2016, she "liked all the doctors" she worked with. Letby says she did not know what the issue was, she had not been informed what was happening. She says she was worried she had "made a mistake" and "was in trouble for something". Asked about the timing of the call, she said she was worried about receiving the call "so late in the day" [after 5pm] in advance of working a night shift. She agrees she was worried it was something serious.
11:09am: Letby agrees this was in the aftermath of Child Q's collapse and Dr John Gibbs making enquiries. She said she was "upset and worried".
LL: "I was upset and I was concerned something was wrong."11:14am: Letby says she was worried about the next day, but not concerned it had gone 'right to the top'.
NJ: "You knew they were on to you, didn't you?"
LL: "No." Letby had messaged a doctor about it: "I can't talk about this now." She writes, 12 minutes later: "Sorry, that was rude. Felt completely overwhelmed & panicked for a minute. "We all worked tirelessly & did everything possible, i don't see how anyone can question that. "Im having a meltdown++ but think that's what I need to do" Letby says she was having a 'dramatic' meltdown.
LL: "It was all happening very last minute and in the evening - it was not normal." She says this is different from work pressures as "this was personal". She denies that people were 'sussing' her.11:16am: A message on Letby's phone at 11.29pm included: "Death datix x 2
Datix - no bicarb, delay in io access
Sign out ffp on meditech & pink chart
[Child O] charts obs
Fluids in sluice
Sign drugs
Sign curosurf out
Traffic light drug compatibility - inotropes, and no policy for panc
Delay in people doing drugs"
Letby said this was documents she had not yet completed for babies she had cared for.11:25am: A message sent by Letby's nursing colleague to Letby: "[doctor] came in chatting to me at the start of last nights shift n I said [baby] needs L.L soon as uvc been in nearly 2wks n he said something about [child O]s already being changed n I said it hadn't n he told me about the open port!" Letby's responded: "I told her about it that night. "Yes because Thought it's a massive infection risk and risk of air embolism, don't know how long it had been like that." A Datix form for the clinical incident is shown to the court - June 30, 2016, 3pm, with the port on one of the lumens noted to not have a bung on the end and was therefore 'open'. Registrar informed. Letby is the reporter of the incident. Mr Johnson says this was a potential case of accidental air embolus which Letby had reported.
NJ: "You had your thinking cap on, didn't you?"
LL: "No." Letby said this was something which needed to be reported.
NJ: "You removed the port and covered it as a clinical incident, didn't you?"
LL: "No."
NJ: "This is an insurance policy - so you could show the hospital was so lax..."
LL: "No."
NJ: "It was to cover for accidental air embolus."
LL: "No."11:26am: Letby is asked about the investigation and Letby being seconded to an office-based role.
Letby messaged: "Hoping to get as much info together as possible -if they have nothing or minimal on me they'll look silly, not Me"
"Did you think attack was the best form of defence?"
"This was me responding what was happening to me."11:29am: Letby's message on August 8: "Tony phoned. He's going to speak to Karen and insist on the review being no later than 1st week of Sept but said he definitely wouldn't advise pushing to get back to unit until it's taken place. Asked about social things and he said it's up to me but would advise not speaking with anyone in case any of them are involved with the review process. Thinks I should keep head down and ride it out and can take further once over. Feel a bit like Im being shoved in a corner and forgotten about by the trust. It's my life and career." Letby said she was feeling isolated and not able to speak to anybody on the unit. Mr Johnson asks if that was really the case. Letby said she spoke to some friends who she was allowed to speak to about the details of the investigation. They were two nursing colleagues and a doctor.
Letby's message: "It's making me feel like I should hide away by saying not speak to anyone and going on for months etc - I haven't done anything wrong."
NJ: "You knew at this stage you were being blamed for the collapses and deaths of these children?"
LL: "No."11:38am: Mr Johnson asks about the 'gang of four' consultants who were 'out to get' Letby. Letby had previously said the four were Dr Ravi Jayaram, Dr John Gibbs, Dr Stephen Brearey and one other doctor, who had apportioned blame to her 'to cover failings at the hospital'. Mr Johnson says he will go through the cases. He says for Child A, staffing levels were a shortcoming in administering a long line. For Child B, nothing, For Child C, nothing. For Child D, the antibiotics being delayed 'may have had an impact on her'. For Child E, the delay in giving him a blood transfusion. For Child F, nothing. For Child G, possibly the colleague had overfed the baby, but that was later retracted. For Child H, the location of the chest drains may have had an influence. For Child I, that Ashleigh Hudson should have put her on a monitor, and that 'potentially' Dr Chang being called away. For Child J, nothing. For Child K, nothing, other than the ET Tube may not have been secured. For Child L, nothing. For Child M, nothing. For Child N, nothing other than it was busy. For Child O, concerns raised by Sophie Ellis were dealt with on the charts. For Child P, an issue with a chest drain. For Child Q, nothing. Letby says she did not know what babies the four consultants were discussing about. "How do the shortcomings count for their conspiracy?" Letby says a lot of the babies were not cared for properly on the unit. Mr Johnson says is it Letby's view that the overall care was not good enough, they pinned the blame on her. Letby agrees.
11:44am: Mr Johnson says Letby has failed to identify, specifically, an issue with staffing levels for each of these cases. Letby says it was raised at times on the unit, in relation to the overall care for babies. Mr Johnson says the point of this case is to determine sabotage for the babies or naturally occurring deficiencies. He says Letby cannot give specifics.
Letby: "No."
Mr Johnson refers to 'sub-optimal care for the babies', from Letby's defence statement.
NJ: "You are raising the point, aren't you?"
LL: "Yes."
NJ: "And you have been given an opportunity to speak about it." Mr Johnson turns to the Facebook searches Letby made for parents of children in the indictment. Three searches are made for parents in quick succession. Mr Johnson asks what the link is. Letby: "They are babies that have died and been seriously unwell." Letby is asked about another series of searches for three parents' names.
LL: "They are babies that had something significant to them and they were on my mind." Letby is asked why she didn't give that answer to the police.
LL: "Because I couldn't recall why I had looked at some of them."
NJ: "Is that a true answer?"
LL: "Yes."
NJ: "You were checking up on your victims."
LL: "No - I look at a variety of [parents]."11:46am:
NJ: "You were a killer who was looking at your victims, weren't you?"
LL: "No." Mr Johnson asks about a series of other searches, and says one of the parents' names has an 'unusual spelling'. Letby is asked to spell that name out in court. She does it incorrectly.
NJ: "You read it [the name of the parent] off a handover sheet, didn't you?"
LL: "No."11:49am: Letby is asked about another series of searches.
Letby: "They were on my mind at the time." One search was made on Christmas Day, for the mother of Child E and Child F.
NJ: "She was the person who caught you in the act?"
LL: "No, [mother of Child E and Child F] and I had a good relationship at the time."12:04pm: The trial resumes after a short break.
12:10pm: Mr Johnson says Letby had given evidence surrounding her suspension from the unit in her first day of giving evidence to the defence. She had said she felt very isolated from my friends and family on the unit, and her mental health had deteriorated.
LL: "We were a very supportive unit - regardless of whether we were personal friends, we were a supportive unit.
LL: "At the time the hospital advised me not to contact anyone on the unit...there were two or three friends I could contact, but [not to contact anyone on the unit]." Letby is asked if that was true. "Yes." And if she abided by that. "Yes." Letby adds that did change as time went on. Letby has a document which she received from the prosecution this morning on her social life. Mr Johnson says it "disproves everything" that Letby had said. Letby disagrees. "You were telling the jury a sob story, that you had been cut off from your family as you called them, on the unit?" Letby disagrees.
NJ: "Were you looking for sympathy?
LL: "Yes, it was a very difficult time."
NJ: "Was it just a mistake?"
LL: "Yes." The document includes photos of Letby's nights out and days out with colleagues, Mr Johnson says. They include a trip to London with a doctor colleague. Letby says that happened once.12:21pm: A 'social timeline' is shown to the court, detailing meetings with the doctor in Harford, Cheshire Oaks (twice) and London between May-June 2017.
LL: I'm near the park next to where you are, let me know where you are finishing up and I'll see you outside
Doctor: Ok will do See you soon ❤️
LL: 🙂 ❤️
Letby denies the doctor was her boyfriend. Letby agrees she had a "very very active social life". Letby says a future date on the Facebook diary, for September 2017, was listed as a trip to London, but they had to cancel as the doctor had a medical appointment. She denies again he was her boyfriend.
NJ: "You have deliberately misled the jury about this background."
LL: "No."
NJ: "You have also deliberately misled them about the circumstances of your arrest, haven't you?"
LL: "No."
Letby says the police knocked on her door at 6am when they arrested her. She says she thought she had a nightie and a tracksuit and trainers. Mr Johnson says Letby was taken away in a blue Lee Cooper leisure suit. Letby says she is not sure. Mr Johnson says video footage can be played of her arrest. Letby agrees she was taken away in that leisure suit. For the 2019 arrest, Letby agrees she was not taken away in her pyjamas.
NJ: "Why did you lie to the jury about this?"
LL: "I don't know." Letby says it was the first arrest when she was taken in her pyjamas.
NJ: "Do you want to watch the video?" Letby does not respond.
NJ: "You are a very calculating woman, aren't you"
LL: "No."
NJ: "You tell lies deliberately."
NJ: "And the reason you tell lies is to get sympathy and attention from people." Mr Johnson says Letby was killing children to get attention.
LL: "I didn't kill the children."
NJ: "You're getting quite a lot of attention now, aren't you?"12:23pm: One of Letby's handwritten notes is shown to the court. It is the one which includes a draft sympathy message for Child O, Child P and another triplet. Mr Johnson asks why a sympathy message has included the name of the surviving triplet as well as the names of Child O and Child P.
NJ: "Was that your objective, to kill all three?
LL: "No."
NJ: "Did that excite you?"
LL: "Absolutely not."12:27pm: The 'I AM EVIL I DID THIS' handwritten note by Letby is shown to the court. Letby is asked about the notes.
NJ: "You had done nothing wrong?"
LL: "No."
NJ: "Why did you think you would not marry and have a family?"
LL: "Because I was in the position that I was in and didn't think it would end."
NJ: "You had a good job working in the patient safety department at the Countess of Chester."
LL: "It wasn't a choice for me."
NJ: "It was still a good job."
LL: "Good as enjoyable?"
NJ: "It was secure, with a secure employer."
LL: "Yes."
NJ: "Pays well?"
LL: "Not as much as nursing."
Letby said there were times when she had good times during the time she was under investigation. Mr Johnson says this includes drinking fizz and days at the races.
Mr Johnson concludes: "You are a murderer."
Letby: "I have not murdered or harmed any child."12:28pm: Benjamin Myers KC rises to ask further questions of Letby. He says Letby has given evidence for 14 court days over the past few weeks.
12:33pm: Mr Myers asks Letby about the increase in documents since giving her defence statement. Letby agrees it was an increase in "thousands of pages" since then, and the increase has continued throughout the trial. Letby agrees the increase in evidence served has come when she and the defence team have been in different parts of the country, with her being in custody.
12:38pm: Mr Myers asks questions in the case of Child E, in relation to Letby's defence statement. In cross-examination, Letby was said not to have made a mention of Child E vomiting in her defence statement, but said it in evidence. Letby tells the court now Child E had vomited. Mr Myers says Letby's nursing note from August 4, 2015, showed Letby recorded a 'large vomit'. Letby says that was not included in the defence statement as she had not included every single detail from all the cases in that statement. The nursing note also includes a 'mucky' slightly bile-stained aspirate was recorded.
12:40pm: In Letby's defence statement, she said she had wanted to work in nursing since being a teenager. Letby is asked about her motive in working at the Countess of Chester Hospital neonatal unit: "To provide the best care possible for them and their families." Letby said she would have looked after "hundreds" of babies during her time at the Countess of Chester Hospital.
BM: "Were you trying to 'get attention' [by attacking babies] in the way it has been put?"
LL: "No." Letby says the Facebook searches were for parents who were on her mind at the time.12:42pm: BM: "Can you recall every baby you cared for?"
LL: "No."
BM: "Is there a reason some babies stand out more?"
Letby says there might have been something about some babies that would stand out in her mind, and some babies would be on the unit longer, and she would have got to know some families more than others.12:43pm: Letby is asked about staffing levels at the unit.
Mr Myers: "Do you know, actually, how every member of staff was affected by staffing pressures?"
LL: "No I don't." Letby adds she does not know if every member of staff was performing their tasks to the level required throughout.
BM: "Can you say at any given point, what the issue of staffing levels were?"
LL: "No."12:51pm: Letby adds from a nursing perspective she can comment on that care, but medical care [from a doctor] is a "different realm". Letby says she can only put a nursing perspective on the issues. Mr Myers asks about Child E and Child L. Letby had said, in evidence, insulin was given to Child E unlawfully, but it was not targeted. She said, from the blood results, Child L was poisoned with insulin, but was not targeted. Letby says for Child L, she accepted the blood results which showed the insulin had come exogenously. Letby says she does not know how the insulin levels of a blood sample are tested. She says she has never worked in a lab for the purposes of such testing. Letby says she accepted the results on the basis of the evidence that is presented in the trial.
12:56pm: Letby, in her defence statement, said she was concerned she was blamed for things she was not responsible for, and was unable to explain how some of the babies had collapsed. The statement added the higher mortality rate had come from the unit taking on more poorly babies. For Child Q, Letby says Dr John Gibbs was asking who was on duty at that time and who the designated nurse was. Letby says, in her statement, Dr Jayaram and Dr Brearey had been "set against her for some time" and did not accept "in good faith" their evidence. Mr Myers asks if Letby had ever accepted the accuracy or honesty Dr Jayaram's recollection of the incident in relation to Child K.
Letby: "No." Letby adds she did not recall clearly what happened at that event. She denied interfering or harming Child K at that time.2:08pm: The trial is now resuming following a lunch break.
2:17pm: Mr Myers continues to ask Lucy Letby questions. He says there is "not a lot further" to go through. He says there were "many times" when the prosecution gave evidence, or parts of evidence, to Letby and the jury. In the case of Child P, he says Child P was the 'worse for wear', and the prosecution said this was similar to the previous night with Child O, which he says was inaccurate. Letby is asked why she agreed with an inaccurate summary of evidence by the prosecution.
LL: "I can't answer that, I don't know." Mr Myers says the prosecution had asserted Lucy Letby had 'fallen out' with Melanie Taylor. Letby denies this was the case at any point. Text messages are shown between Melanie Taylor and Lucy Letby. The exchange is on June 9, 2015, following the death of Child A, and how hard it was going in to back into the unit following such an event. Letby messaged: "I hope you are ok, you were brilliant" and signs off the conversation "Great see you then xx" to which Melanie Taylor replied "Xx". Letby denies she fell out with Melanie Taylor.2:19pm: Letby is asked about the prosecution saying she 'fell over herself' to message Sophie Ellis following the death of Child P. Sophie Ellis had been at the races that day on June 24, 2016.
Sophie Ellis messaged Letby first: "Hey Luce, hope your ok? I heard poor little [Child P] has been sent to Liverpool..."
Letby replied the information was 'too much for a text'.
She added: "Actually you are at the races, sorry I forgot. Don't worry about ringing will txt you tomorrow. X"
Letby tells the court she wanted to leave Sophie Ellis alone as she was at the races.2:21pm: Letby is asked about the 'social folder' she was handed by the prosecution this morning. Mr Myers said the photos showed her 'out on the razz with friends'. Letby had said there were times she enjoyed herself.
Mr Johnson had said: "Yes, you felt like this, because you know you killed and grievously injured these children?"
Letby: "No."
Mr Myers says there was nothing to these events other than going for drinks with friends. Letby agrees.2:29pm: An example is shown of Letby on holiday in Torquay with her dad in July 2016. Another example is of Letby having drinks with university friends in July 14, 2016. Letby says they were the girls she had been with when she was studying nursing. Another example is of a picture of a couple of bottles of Prosecco on July 22, 2016. Letby is asked if she was allowed to drink Prosecco at this time. Letby agrees. Another photo is on August 16, 2016, on a day out in Port Sunlight with her parents who had come to Chester. Letby messaged one of her nursing colleagues - her "best friend", and one she said she was allowed to speak to, about Port Sunlight being 'perfect for a picnic and a stroll'. A photo is taken of Letby at her back garden to her Chester home in August 2016. A WhatsApp message Letby sent in a group of nursing colleagues was: "It's too sad" in reference to Jennifer Jones-Key leaving the unit. Letby says 'around September time' the instructions for Letby not to contact anyone on the nursing unit other than three colleagues had 'changed'. A message on September 22, 2016 to one of the three colleagues - 'All ok with E [Eirian]. Feel bit more positive knowing she's definitely behind me...'
2:32pm: Letby is seen smiling in a number of photos. Mr Myers asks why Letby is smiling in the photos when it was around the time she handwrote notes documenting her problems.
LL: "Because despite what is going on, you have to find some kind of quality of life." December 31, 2016, Letby writes on Facebook: "❤️ I'm not the same person I was when 2016 began; but I am fortunate to have my own home. I've met some incredible people and I have family and friends who have stood by me regardless - Thank you to those who have kept me smiling. Wishing Every Happiness for us all in 2017" Letby says she had changed as a person and had 'lost confidence'2:35pm:
BM: "As far as you understood, were you at least allowed a social life?"
LL: "Yes." Another photo is of Letby at the Kuckoo bar in Chester. A holiday photo is shown of Letby with her father in June 29, 2018 in Torquay. Letby denies killing or harming babies for any reason the prosecution had suggested.
BM: "How content were you before, in life?"
LL: "I had a very happy life."That now completes Lucy Letby's evidence.
2:37pm: The judge tells the jury of the next steps in the trial, which may have further evidence for the defence case. The next listed day for the jury will be next Wednesday (June 14).
Monday 12th June 2023 - no court (planned)
Tuesday 13th June 2023 - no court (planned)
Wednesday 14th June 2023
Defence witness: Plumber Lorenzo MansuttiChester Standard Live Reporting
11:01am: The trial is now resuming.
11:03am: Benjamin Myers KC says to the court there is one witness to give evidence in relation to the sanitation of the hospital.
11:07am: Lorenzo Mansutti, who works at the Countess of Chester Hospital, has had many years of experience in plumbing. He has provided a witness statement. He says the plumbing in the Countess of Chester Hospital's Women's and Children's Building, between 2015-2016, had been built in the 1960s and 1970s, and says there were "issues with the drainage system". He says he had to deal with "various blockages" and the cast-iron piping would crack for "a number of reasons" including age. Asked what would happen if the pipes were blocked, he replies it would come back through the next available point, such as toilets or wash basins. He confirms that would include sewage.
11:11am: He says when alerted to it, it would come through the helpdesk, and it would be rectified "as quickly as possible". He says he would be called out "weekly" to fix problems. He says there was an occasion when they had a blockage in the room next door adjacent to the neonatal unit. He says a colleague attended it, the drainage had backed up and the neonatal nursery room 1 hand wash basin had "foul water" coming out of it. He agrees with Mr Myers that "foul water" would include "human waste...sewage". He says he is unable to confirm exactly when that happened during 2015-2016.
11:15am: Mr Myers says there were Datix forms presented to Mr Mansutti, one dated January 26, 2016. It is a 'non-clinical incident' of a 'flood' type. Nursery 4 was closed at 2.30am 'due to plumbing work/deep cleaning of nursery.' 'Mixer tap was switched on, and sink completely blocked.' 'Floor noted to be completely flooded'. 'Water within sink noted to contain much black debris. Sink still blocked however'. The nursery was 'noted to be flooded again at approximately 4.30am', with the 'floor almost completely flooded again'. Nurse Christopher Booth reported the incident. Mr Mansutti confirms this is an incident different from that which was reported in room 1.
11:24am: A service report of 'blocked drains' is shown to the court. Mr Mansutti says these service reports are "usually" urgent. The report shown to the court is on July 4, 2015. It happened in the maternity wing of the Countess of Chester Hospital, in the central labour suite [CLS], ward 35. He says incidents would be delegated to team members. A second incident is shown reported at August 8, 2015, a 'flood in the CLS' (ward 35), for which Mr Mansutti was called out. Another is on October 2, 2015, for blocked drains in the CLS.
11:28am: Another is on October 6, 2015, in the neonatal unit, to 'investigate flood'. Mr Mansutti says it could be a waste pipe, or rainwater. Another report is on January 26, 2016, a 'leak in the neonatal unit/SCBU'. Another is on February 24, 2016, a 'burst pipe in sluice' in 'ward 35 CLS'. Another is on March 18, 2016, in the neonatal unit, nursery room 2 and the kitchen. There were two 'blocked sinks'. Another is on April 10, 2016, in ward 35 CLS, as 'Sluicemaster and drains blocked'. Mr Mansutti says the Sluicemaster is a bedpan machine.
11:32am: Another report is on June 6, 2016, a 'flood in courtyard' of the neonatal unit. Mr Mansutti says this may have followed a heavy downpour. He does not believe the foul drainage runs that way, so it would more likely be surface water. Another report is on July 5, 2016, in ward 35/CLS, for 'various plumbing jobs in NNU'. Check pall water filters for poor flow' Check that all valves in the ceiling void are fully open - NNU and by theatres...' Leaking sink in Sluiceroom - please check'. Mr Myers asks about the last of these jobs. Mr Mansutti says it is likely a leak in one of the sinks. He says there is not a Sluiceroom in the neonatal unit.
11:37am: Nicholas Johnson KC, for the prosecution, asks Mr Mansutti questions. Mr Mansutti agrees that one of the problems for the flooding was adults 'putting things down sinks'. One incident is somebody 'forcing a wipe towel down a sink'. Mr Mansutti accepts an incident did take place. He says none of the incidents led to no hand washing facilities availability, and there is a system in place. He says there has been 'sewage floods' in the neonatal unit.
He says there was once incident, undated, not on a Datix form, where there was sewage on neonatal unit room 1. He says he has knowledge of it because of "disgust", and work was done on moving sewage pipes away from the unit room in future, "so it couldn't happen again". He says, for his recollection, it was a "one-off". Mr Johnson says half the incidents listed did not take place in the neonatal unit. Mr Mansutti says there would not have been a direct effect on that unit for those days. That completes Mr Mansutti's evidence. It also completes the evidence presented in the Lucy Letby trial.11:38am: The trial judge, Mr Justice James Goss, is now giving preliminary directions to the jury.
11:40am: The trial judge says he has to discuss his directions of law with the prosecution and defence before he can deliver them to the jury. He says those will likely be presented to the jury on Thursday, and the jury will not be present in court 'for very long'.
11:42am: The judge says the week beginning July 3 is when the jury will be expected to go out. He says it is in the "hope and expectation that nothing untoward occurs", as the trial has had delays and it has gone on longer than expected.
11:43am: He also reminds the jurors of their obligations not to discuss the case with anyone, and not to discuss it amongst themselves until they are sent to deliberate.
11:44am: The jury are now sent home for the day.
Thursday 15th June 2023
Instructions to the Jury
Chester Standard article 15-06-2023
Jurors in the trial of murder-accused nurse Lucy Letby have been told to approach the case in a "fair, calm, objective and analytical way".
Letby, 33, is accused of murdering seven babies and trying to murder 10 others during the course of her work on the neonatal unit at the Countess of Chester Hospital.
The defendant, from Hereford, is said to have seriously harmed and killed the babies in various ways, including by injecting air intravenously and administering air and/or milk into the stomach via nasogastric tubes.
She also allegedly added insulin as a poison to intravenous feeds, interfered with breathing tubes and used force to the abdomen.
Some of the babies, the prosecution say, were subjected to repeated attempts to kill them.
On Thursday, June 15, trial judge Mr Justice James Goss gave his first set of directions of law to the jury of eight women and four men ahead of the prosecution and defence delivering their closing speeches at Manchester Crown Court from next week.
He told jurors, who were sworn in last October, they should decide the case solely on the evidence placed before them.
He said: "As I said at the very beginning of the trial, you must not approach the case with any pre-conceived views and you must cast out of your decision-making process any response or approach to the case based on emotion or any feelings of sympathy or antipathy you may have.
"It is instinctive for anyone to react with horror to any allegation of deliberately harming, let alone killing a child – the more so a vulnerable premature baby.
"You will naturally feel sympathy for all the parents in this case, particularly those who have lost a child and the harrowing circumstances of their deaths.
"You must, however, judge the case on all the evidence in the case in a fair, calm, objective and analytical way – applying your knowledge of human behaviour, how people act and react, using your common sense and collective good judgment in your assessment of the evidence and the conclusions to be drawn from it."
Mr Justice Goss told jurors it was not their role to "resolve every conflict in the evidence".
He said: "It would, you may think, be a remarkable and exceptional case in which a jury could say we know everything about what happened in any case and why.
"You are not detectives.
"If you are sure that someone on the unit was deliberately harming a baby or babies, you do not have to be sure of the precise harmful act or acts. In some instances there may have been more than one.
"To find the defendant guilty, however, you must be sure that she deliberately did some harmful act to the baby the subject of the count on the indictment and the act or acts was accompanied by the intent and, in the case of murder, was causative of death."
He told the jury they also did not need to certain of any motive for deliberately harming a baby.
Mr Justice Goss said: "Motives for criminal behaviour are sometimes complex and not always clear. You only have to make decisions on those matters that will enable you to say whether the defendant is guilty or not of the particular charge you are considering.
"Any decision you do make must be based on evidence and not speculation."
Turning to the subject of "circumstantial evidence and the unlikelihood of coincidence", he said this was a case in which the prosecution "substantially, but not wholly" rely upon circumstantial evidence.
Mr Justice Goss went on: "The defendant was the only member of the nursing and clinical staff who was on duty each time that the collapses of all the babies occurred and had associations with them at material times, either being the designated nurse or working in the unit.
"If you are satisfied so that you are sure in the case of any baby that they were deliberately harmed by the defendant then you are entitled to consider how likely it is that other babies in the case who suffered unexpected collapses did so as a result of some unexplained or natural cause rather than as a consequence of some deliberate harmful act by someone.
"If you conclude that this is unlikely then you could, if you think it right, treat the evidence of that event and any others, if any, which you find were a consequence of a deliberate harmful act, as supporting evidence in the cases of other babies and that the defendant was the person responsible.
"When deciding how far, if at all, the evidence in relation to any of the cases supports the case against the defendant on any other or others, you should take into account how similar or dissimilar, in your opinion, the allegations and the circumstances of and surrounding their collapses are.
"The defence say that there are possible causes for many of the collapses other than an intentional harmful act, that the prosecution expert evidence cannot be relied on in terms of providing explanations for many of the collapses and that there is insufficient evidence to lead you to the conclusion that these events were related and were a consequence of any harmful act by the defendant rather than a series of unrelated collapses that, in some cases, ended in death."
When considering the seven counts of murder, Mr Justice Goss told jurors they must be sure Letby deliberately did something to the child that was "more than a minimal cause" of the death.
He said: "The children were all premature and vulnerable, some had mild respiratory distress syndrome of prematurity and some had specific health issues.
"There were also a few cases of delays in the administration of appropriate medicine or other clinical failings. Some of the causes of death were unascertained.
"In the case of each child, without necessarily having to determine the precise cause or causes of their death and for which no natural or known cause was said to be apparent at the time, you must be sure that the act or acts of the defendant, whatever they were, caused the child’s death in that it was more than a minimal cause.
"The defendant says she did nothing inappropriate, let alone harmful to any child. Her case is that the sudden collapses and death were, or may have been, from natural causes or for some unascertained reason or from some failure to provide appropriate care, and they were not attributable to any deliberate harmful act by her."
Letby denies seven counts of murder and 15 counts of attempted murder between June 2015 and June 2016.
Monday 19th June 2023
Prosecution Closing Speech - Day 1
Chester Standard Live Reporting - 19th June 2023
Prosecutor Nicholas Johnson KC says this is "the beginning of the end" of the trial.
Documents are now handed out among members of the jury.
Mr Johnson asks the jury to look at an agreed fact which has been 'crossed through'. He says, in case jurors enquire, it has become "irrelevant". He says it has been a long time since October when he introduced the case. He says the detail given back then is "nothing" compared to what the jury now know about the case.
He says the introduction, evidence and cross-examination has been largely chronologically presented. He says the trial judge is likely to be a chronological presentation too. Mr Johnson says 'drawing together the strands of this case' requires a different approach, and "point out the similarities" and the "evolution" of "Lucy Letby's murderous assaults on these children" and "point out how calculating and devious she has been". "We suggest that Lucy Letby gaslighted staff at the hospital - professional people with many many years of experience." Letby "persuaded" staff the incidents were "just bad luck". The laboratory synthesised insulin found in two babies wasn't "just bad luck", he added.
Mr Johnson says Letby picked Mr Mansutti, a plumber, as a defence witness to pick on incidents "which aren't actually relevant" to the case. He says there may have been one occasion when there was a backed up sink in neonatal room 1, but it did not correlate with any of the incidents heard. If it had, someone would have noted it. NJ: "His evidence isn't going to help you decide in this case. "He was called, we suggest, to bolster the tattered credibility of Lucy Letby - and you might ask yourself why."
Mr Johnson says Child P's injuries, combined with the insulin poisonings, had nothing to do with the plumbing. NJ: "Please do not be distracted." Letby "got away with her campaign of violence for so long" as it was not contemplated that a nurse could do such acts, he adds. Mr Johnson says the "similarities" in these cases "shows who this person was".
Mr Johnson refers to Dr Stephen Brearey's evidence in court. NJ: "Lucy Letby had used ways of killing babies...that didn't leave much of a trace. "Her behaviour persuaded many of her colleagues that most of the collapses were 'normal' - they couldn't see the wood through the trees. "No-one - no-one, was contemplating the possibility of foul play." Mr Johnson says Dr Brearey said, in relation to 'confirmation bias', that senior nursing staff "didn't believe this could be true", but the year was spent "with increasing suspicion with each incident...none of us wanted to believe it either." "Then we stopped to take a step back, to think about it...the unexpected collapses...the unusual rash on a number of occasions, the association with Lucy Letby. "Each time it became more statistically improbable." Mr Johnson says Dr Brearey didn't know about the liver injury or the insulin poisonings at that time. Dr Ravi Jayaram had said it was an "unprecedented" situation - "it seems utterly preposterous, then more and more happens. "It seems easy to see things which aren't there." "We are taught to think about common things, less common things, rare things. We do not generally consider unnatural causes or deliberate things."
Mr Johnson refers to the 'gang of four conspiracy theory'. He says in Letby's defence statement, there is a suggestion that the collapses and deaths were a product of staff shortages, or mistakes, or insufficiently qualified staff. Mr Johnson says Letby said that was a "medical opinion", but the jury have not had any 'medical opinion' to back that up. NJ: "The only things that matter is to concentrate on the issues in this case. Concentrate on the 17 children in this case...and see if there are any shortcomings. "We suggest that was an uncomfortable exercise for Lucy Letby."
Mr Johnson says for Child A, Letby said there were issues with the long line, and "if we agree" it was an air embolus, that Melanie Taylor would have done so. Mr Johnson says Child A did not die of dehydration, and it was not Melanie Taylor who supplied the air embolus. For Child B, nothing. For Child C, nothing.
For Child D, Letby said there was a delay in antibiotics - but Child D did not die from an infection, Mr Johnson says. For Child E, it was delay in response to the bleeding. Mr Johnson asks where did the bleed come from in the first place. For Child F, nothing. For Child G, initial blame with a colleague, but Letby went back on that. For Child H, 'some of the drains were not securely put in', and 'potential incompetence'. Mr Johnson says Letby uses the word 'potential a lot'.
For Child I, nothing on event one or three. For event two, Ashleigh Hudson was blamed for not full monitoring after Child I was taken off antibiotics within 48 hours, but Child I had been off antibiotics for 'much longer'. In the fourth event, 'potential medical staff issues' with doctors being absent may have contributed. For Child J, nothing. For Child K, nothing. For Child L, nothing. For Child M, the 'unit was very stretched' and Child M was not in a proper bed. For Child N, the unit was 'very busy', but Child N was due to go home. For child O, nothing. For child P, concern overnight for Child P's condition - but there was no medical record of this. For Child Q, nothing. Mr Johnson adds: "Do you really think the [gang of four] would say things to get Lucy Letby convicted?" He says: "What did the doctors say that wasn't true?"
Mr Johnson says the 'gang of four' didn't do a very good of scapegoating Lucy Letby, as they missed the insulin evidence - "the best bit of evidence". He says "all the clues point in one direction, don't they? She's sitting in the back of court." He says the four "didn't even know" about the "wildly out of kilter" insulin readings when they "blew the whistle".
"Lucy Letby, we say, put a lot of effort in trying to pull the wool over your eyes." He says Letby spent a lot of time talking about being isolated from her friends. He refers to the 'I AM EVIL I DID THIS' notes - he says "we will come back to them at the end", but says "there are more important things in this case". He says it was established Lucy Letby was "not isolated" and was "still in contact" with people she had "not been allowed to contact". "Even though she knew what we had from our phone, she did repeat the lie. "We went to the spreadsheet and the lie was exposed, wasn't it? "She thought that if she said something often enough...it would be accepted. "We suggest that Lucy Letby was an opportunist - she used their vulnerabilities as camouflage." He says the misperception of the vulnerabilities "gave her away". He says Letby thought Child A and Child B had an inherited blood disorder, and that allowed her the cover to target them. "If she had left it there- she probably would have got away with it."
"Her ignorance of insulin c-peptide...and the ratio [to insulin]...allowed her to poison [Child E and Child L]. "What she didn't know about the disconnection [between the insulin and insulin c-peptide ratio] leaves a biological footprint which leaves foul play. "She would have got away with that - if police hadn't...referred the cases to Dr [Dewi] Evans." He says Letby returned from a holiday in June 2016 and embarked on a "killing spree", with Child O and Child P killed and attempting to murder Child Q. He says Letby put in 'false data sheets' to cover her tracks, and first put in the theory of an air embolus at June 30, 2016.
Mr Johnson says he will look at five cases in one go - twins Child E&F, twins Child L&M, and Child K. He says for E&F and L&M, one twin was poisoned with insulin and the other deliberately administered air. The cases were months apart. "What are the chances of that?" He says Letby "invented" other cases of problems where none existed. With Child K, it was that she was a 'serial tube dislodger', but Child K had been "sedated". For the two poisoned with insulin, they were "deliberately targeted". Mr Johnson says when Letby was "interrupted" for Child E, she 'invented' that Child E really did have a problem.
Mr Johnson refers to Child E and Child F's mother's evidence, given several months ago, for events from July 30, 2015. Mr Johnson says the mother was a "very very important" witness. He says the evidence was that providing milk was a big priority for her twins, as it as the only thing she could do. Child E was crying 'like nothing she had ever heard before' - 'it was horrendous, more of a scream than a cry'. Mr Johnson says screaming was also recorded for Child I and Child N.
Mr Johnson says the mother described Child E's blood around the mouth - 'like a goatee beard'. Letby had said the blood came from the NG Tube and the registrar was 'on his way'. Letby told the mother to go back to the post-natal ward, and had done so by 9.11pm. NJ: "This is a head-on credibility contest between [the mother] and Lucy Letby." "You can be sure Lucy Letby is lying on this - plainly, as any parent will understand, provision of milk and food to any newborn infant is important, and 2100 was [Child E's] feeding time." "Crying like nothing I'd heard before - it was a sound which shouldn't have come from a tiny baby, it was horrendous... "You may think [the mother] would have a very good reason to remember this. "Either she saw blood or didn't - why would she make it up?" If she did see blood at 2100, then Letby's nursing notes are "false", Mr Johnson says.
Dr Sandie Bohin says the NG Tube for Child E had been in place from July 29 to August 3, 2015. Mr Johnson says that was never disputed. He asks why the tube was the cause of the bleed, as said by Letby. NJ: "It was a panicked reaction, told to a mother who knew no better, and it was designed to cover her tracks."
Mr Johnson refers to the '1ml bleed' Letby recorded for Child N. Letby, interviewed on that, had said the tube insertion 'can cause a bleed' - "just a small amount". Mr Johnson says the mother of Child E recorded a small amount of blood at 9pm. He says if that was the case, then Child E was 'producing lots of blood' by 10pm. He says Letby 'falsified' nursing notes for Child E. He says the jury "can be sure" the mother was telling the truth, as the mother rang her husband, and the phone call record "proves that" at 9.11pm, in a call lasting over 4 minutes. He says the father's evidence backs up the mother's evidence on the content of the phone call. "Have [the parents] made that up, to get at Lucy Letby? Are they in on it? Are they a sub-gang of two?"
Mr Johnson says of all the things to see in your life, "you would remember" seeing your son "in terminal decline", as the mother recalled returning later to see efforts to save Child E's life. He says if the parents are telling the truth, then Letby's account is a "lie". He says there is a "fundamental difference" between the mother's "compelling account" and Letby's "lie" in the notes. Dr David Harkness's note for 11pm, Mr Johnson says, coincides with the telephone call from the midwife at 10.52pm to the father of Child E, in a call which lasts over 14 minutes. Letby's family communication note records 'both parents present during the resus.' Mr Johnson says the pieces of the jigsaw 'fit only one way' and the parents' recollection is at odds with Letby's. Mr Johnson says the prosecution say Letby attacked Child E and was interrupted first time, then attacked again. He says of the mother's account: "It's powerful evidence - independent of the medical evidence - that Lucy Letby murdered [Child E]."
Mr Johnson says Dr David Harkness, in evidence, gave a chronological sequence of what happened. He says he accepted he had been on the neonatal unit from 9.30pm. A fluid balance chart for Child E is shown to the court. '15ml fresh blood' is written in the 10pm column, accepted it was written in Letby's handwriting. Mr Johnson says it was signed by Belinda Simcock [Williamson] deliberately so Letby could 'disassociate' herself on the paperwork from the incident, "so it looked" that someone else was there at the time. Letby had said she "assumed" it came after Belinda Simcock's documentation. Mr Johnson refers to a case in Child I, where Letby 'altered the timing' for her designated baby that was due to be transferred to Stoke.
Mr Johnson says Letby needed an "innocent reason" for why Child E's 9pm feed was omitted, and does so by suggesting Dr David Harkness was on the unit earlier in the shift. Dr Harkness had suspected a gastrointestinal bleed for Child E, but all the observations were 'good' and did not point to that. Dr Harkness was "insulted" at the suggestion, in evidence, he was "out of his depth".
NJ: "None of these doctors suspected sabotage - they all looked for a natural cause. "It was not a level playing field - there was no natural cause." Dr Harkness had said something had been "interfering" with Child E's oxygen flow into the bloodstream. He said Letby had been looking "A strange pattern over the tummy area which didn't fit with the poor perfusion - there were these strange kind of purple patches. "There were patches in one area, then in another...it was unusual for a baby [in Child E's condition]."
Dr David Harkness had said he had not seen these patches - "no smaller than 1-2cm", "didn't remain constant", outside of the babies in this case - Child A and Child E. DH: "It was something that was so unusual it's hard to give a clear description". Mr Johnson says this was what a doctor had said. He says Dr Harkness was "traumatised" by what he had seen, in the way Child E had bled in the way he did. He said Letby, by comparison, on the day Child E died, texted "one of those things"; "nothing to see here," Mr Johnson adds. He says Letby was "gaslighting her colleagues".
Mr Johnson says Dr Harkness was not one of the 'gang of four'. He asks the jury if Dr Harkness was lying. He says one of Dr Harkness's colleagues, also a doctor, recalled Dr Harkness was "animated" when describing the discolouration. He says if Dr Harkness is lying, then the doctor colleague is also lying. "How deep does this conspiracy go?" He says Letby had described 'strange discolouration' on Child E, with 'red horizontal banding' around the stomach. Mr Johnson says if Letby agrees there was discolouration on Child E, why was Dr Harkness taken to task for describing it in cross-examination? He suggests it was an attack on Dr Harkness.
"No-one now suggests seriously [Child E] had [gastrointestinal disorder] NEC." A doctor had since expressed regret that they agreed a post-mortem examination was not necessary, Mr Johnson tells the court. A medical expert had excluded the possibility of a congenital blood disorder. Dr Dewi Evans said stress for Child E had been ruled out, and the "graphic" skin discolouration provided by Dr Harkness was 'clear evidence' of air administered into Child E's system. Mr Johnson says there is only one person who could have been responsible for administering air into Child E. He says, for the bleed, "this was no naturally occurring bleed". Dr Sandie Bohin said Child E had been "incredibly stable" prior to the deteriorations. The 16ml aspirate at 9pm "struck" her as "really odd" in that context. She was "at a loss to explain where this had come from". Mr Johnson says this discrepancy is also seen in Child N and Child G - and the similarities are "all down to Lucy Letby's behaviour", he adds, pointing to Letby in the dock.
Dr Bohin had agreed with Dr Evans to say air had been injected. The haemorrhage seen by babies such as Child E on this scale was "vanishingly rare". The purple patches, Dr Bohin said, "didn't fit with any explanation other than air embolus".
Dr Bohin rejected a suggestion that stress in Child E caused excess stomach acid which caused the bleeding, Mr Johnson adds. Mr Johnson says Child E declined within about an hour of Letby coming on duty that night. "What are the chances of that?" Mr Johnson says the point of circumstantial evidence is pointing at the threads of evidence, and the collapses "always happen" when Letby is in the neonatal unit. He adds: "There are no innocent reasons for [Child E's] collapse and death."
He says the level of insulin in Child L was double that found in Child F several months earlier. NJ: "That tells you a lot about intention, doesn't it?" He says for Child A, Letby was interviewed about it and said in the aftermath she had 'asked for the [dextrose] bag to be kept' in June 2015. It was put in a sluice room, and a colleague had confirmed this was done. He says that Letby knew no-one subsequently examined the bag. He says Letby "taunted the police" by repeatedly asking the question if police 'had the bag' [which had insulin in]. "She thought the fact they didn't have the bag would give her a free pass. "But she was wrong, because what she didn't know was insulin c-peptide."
Mr Johnson says experts had given evidence from the laboratory to show results [indicating insulin and insulin c-pep levels] from there were "reliable", and Letby had accepted this in evidence. Mr Johnson said it was ruled out that insulin could have been applied to the nutrition bag in the pharmacy prior to its arrival on the ward. Evidence had been heard by one of the pharmacy team to this effect and it was not challenged.
Mr Johnson says the 'murderer' had to have been working both night shifts for Child F and Child L. "Only three" people were working both shifts. One was a nursery nurse and would not have been in room 1. Another was Belinda Simcock, and the third was Lucy Letby, who 'hung up the bag for Child F'. Child L got "more than one poisoned bag of insulin". Mr Johnson: "These are not random poisonings". He says it's "obvious" who is responsible, as there is only one person who could be responsible.
Mr Johnson shows to the court a "tiny vial of insulin", which had been added by someone who had access to the nutrition bags in the fridge, of which there were "a limited number of candidates". Mr Johnson says "we have heard from all of them" and there is only one candidate left. Mr Johnson says it does not need to be found "how it was done", as the evidence shows "it was done". "Anyone, if they wanted to, could inject 0.6ml of insulin into that bag. "A tiny amount of insulin could have fatal consequences. "What is the state of mind of someone who does that? Is it someone who watches someone freshly born desaturating [for up to half a minute - in the case of Child K]. "Is it a sick person? "This was a targeted attack."
Mr Johnson says "we know from evidence" that insulin is "never put into a TPN bag". The case of Child F had been referred to medical experts as the events for Child E were "suspicious". He says the first contaminated bag was put up for Child F at 12.25am, and Child F vomited less than an hour later. A medical expert said this was a symptom of low blood sugar, as a self-defence mechanism for the body. There was also a 'sudden rise in heart rate' as the body produced adrenaline to combat it. The blood sugar level of 0.8 was a "life-threatening situation for [Child F]."
No other child on the unit was receiving TPN bags that day, in the case of Child F. The turnover of TPN bags was "very low" according to evidence by Yvonne Griffiths. The bag "was only ever going to one child, isn't it?" "It's so sly, isn't it?" Mr Johnson says the insulin-contaminated bag was going to be administered when 'the poisoner' was not on duty, to be administered by "an unsuspecting colleague" - "a member of her 'family'". "What does that tell you about the mindset?" "It shows you a cynical, cold-blooded" planner, Mr Johnson says. The amount of insulin in the two bags was 'about the same', which showed there had been thought put into the preparation. Mr Johnson says Letby "told some interesting lies" about Child F in police interview. "She claimed she hadn't been aware of any concerns about [Child F's] blood sugar." He says Letby otherwise had a very good memory. "You know she is lying [from] the text message[s] she sent to [a nursing colleague]." Police broke the news of insulin c-peptide to Letby in November 2020, Mr Johnson adds. The 'surreptitious' searching of Child E&F's mother on Facebook was "never properly explained." Mr Johnson says Letby was "Cold, calculated, cruel and relentless."
The trial will be resuming shortly after its break for lunch.
Mr Johnson refers to the cases of Child L and Child M, the twins. He says fluids were calculated for Child L by Dr Sudeshna Bhowmik. Letby had recorded 'myself and shift leader A. Davies have discussed this with Reg. Bhowmik as it does not follow the hypoglycaemia pathway'. Amy Davies had not recalled this conversation. Mr Johnson says Letby was "setting up an issue" for Child L. Child L's blood sugar level had improved so monitoring was not required. Nurse Tracey Jones said she didn't change the dextrose bag during her shift. Mr Johnson says for the day shift on April 9, 2016, Mary Griffith was the designated nurse for Child L and Child M, on a "busy shift". Mr Johnson says if people were "very busy", then they might not have the time to monitor what Letby was up to. Mary Griffith was "certainly out of the room" by 9.30am as she was in room 4 administering medication to children in there, Mr Johnson says. He says that means Lucy Letby would have been "alone" with Child L at that time. He says that would be when insulin was put into Child L's dextrose bag, as Prof Hindmarsh, in evidence, said it had to be by 9.30am. A blood sample taken for Child L taken at 10am showed an increase in the amount of dextrose given but a drop in the level of blood sugar - "when the opposite should have been true". Mr Johnson says the "fingerpoint of evidence" is the ratio between insulin and insulin c-peptide later recorded. The 'podding' of the blood sample was delayed due to Child M's collapse, Mr Johnson says, and the timing of the sample taken must be taken from several accounts. He says it "must have been taken about 3.45pm".
The blood sample "would have been treated as urgent" and the nurse said she had been distracted by "an emergency" with Child M, which was timed at 4pm. The blood was put into a vial and envelope and labelled. The request for the blood test was entered at 3.45pm on a 'lab specimen internal inquiry' form at the Countess of Chester Pathology. The form is shown to the court. The process and analysis were "interrupted" by "Lucy Letby's attack on [Child M]," Mr Johnson adds.
An infusion therapy sheet for a 10% dextrose prescription is at 3.40pm. Mr Johnson says this explains why the lab result shows a slightly higher blood sugar reading for Child L than the other readings, and that the blood sample was taken at 3.45pm. Dr John Gibbs said the low blood sugar level should have meant the level of insulin in Child L was also low. He said it had "never occurred to him" that someone was administering insulin to Child L. He said he had never received the lab results for Child L - they went to junior doctors who "didn't appreciate its significance" at the time.
Mr Johnson said scientist Dr Sarah Davies had phoned through the results to the hospital "as they were so unusual". The lab at Liverpool was "performing very well" and Mr Johnson says it can be discounted as a possibility that the lab results were in any way "misleading". He adds "it speaks volumes" that the levels of insulin were double that found for Child E months earlier. "The poisoner, Lucy Letby, upped the dose for [Child L]." He says, for timings, the insulin was put in "after the bag was hung" for Child L.
Mr Johnson says Letby was co-responsible for hanging up the bag for Child L at noon on April 9, and had also co-signed for the previous bag on April 8 at noon. Prof Hindmarsh says the bag was "not poisoned" before midnight on April 8/9, as the blood sugar readings are "following an upward trend" for Child L. Insulin "must have been put in" between midnight at 10am on April 9. Mr Johnson says insulin went into the bag sometime before or at 9.36am, given insulin's half-life of 24 minutes. Mr Johnson says it "had to have been a targeted attack", and is "not a random poisoning". He says "whoever is responsible" must have been on duty between midnight at 9.36am. Mr Johnson says the jury must ask if it could have been a different person. He says "it must have been the same person", and they could "get away with it" as long as "they didn't do it too often". He says Letby came on duty between 7.30am-8am on April 9.
The insulin that poisoned Child L "was put into more than one bag" and all the staff on duty said they were not responsible for that. Mr Johnson says the first poisoning was when the bag was already hanging, and the second one was administered to Child L as well. He says at 9.30am on April 9, Mary Griffith was in room 4. She was not working on the day when Child E was poisoned.
A third bag was being put together for Child L at the time Child M collapsed. "Somebody also spiked that bag," Mr Johnson says. He says it was "spiked" sometime after it was hung up at 4.30pm. Mr Johnson asks if somebody did this to "frame" Lucy Letby, and if she didn't do this, then somebody also targeted Child E, and targeted Lucy Letby to take the blame. "We suggest that is not a reasonable possibility - that is why all the other cases are so important, they are not coincidences."
Mr Johnson moves to Child M, who was "a picture of health" after his birth, and "was doing just fine". "The fact that his twin was poisoned puts his case into sharp relief. "What are the chances of a healthy baby boy collapsing in such an extreme way? The evidence, as you have heard from the doctors, is not very big. "What are the chances of this happening at the same time his brother was poisoned...and [point] you to the identity of the attacker?"
Mr Johnson says "circumstantial evidence" can be "very very powerful", and this is a case where it is. Child M suffered a "profound collapse", from which "he made a miraculous recovery" - "how many times have you heard that before [in this case[?]]" He said this was "entirely out of natural process".
Dr Anthony Ukoh had noted there were issues with aspirates and a slightly distended abdomen for Child M, "but nothing to indicate he was to become seriously unwell". On April 9 at 3.30pm he was put on to 10% dextrose, co-signed by Lucy Letby and Mary Griffith. He did not get a bag with insulin in, Mr Johnson tells the court. Mr Johnson says Mary Griffith was about to take a blood sample for Child L and make up a 12.5% dextrose solution, which would take time. Mr Johnson says Letby would have administered this 10% dextrose infusion for Child M. The parents of Child L and Child M had given evidence to say one of the doctors was "pressing [Child M's] chest" '10 minutes after we had left the boys'. Child M had gone from "fine" to "life-threatening emergency CPR" and the father was left "praying", Mr Johnson says. He says it can be discounted this was all 'unlucky coincidence'.
Mr Johnson refers to a paper towel on the resuscitation notes for Child M "which found its way, under its own steam, to Letby's home". NJ: "It 'quote', "came home with me" - sounds like a dog following home, doesn't it? "Her explanation - I collect paper. "How long has Lucy Letby had to come up with a reason? Here we are now, 7 years later, and her best reason is 'I collect paper'." "Most collectors know what they collect - [it's] absolute nonsense." He adds: "Somebody sabotaged [Child M], didn't they?" The attacks were "almost signature" as Child M deteriorated, and six adrenaline doses were given. "It is a signature of the consequences of many of these attacks." Child M was "at the very edge of life" and the resuscitation "took 30 minutes with no response". 20 minutes is "the usual watershed", according to Dr Ravi Jayaram. Dr Jayaram had the 'difficult conversation' with the parents, but Child M had a "miraculous recovery." Mr Johnson says Dr Jayaram 'wasn't sure what we had done' [to make Child M recover]. Dr Jayaram had noted skin discolouration on Child M, that "flitted around" "appearing and disappearing". Dr Jayaram said: "Because [Child M] was darker skinned, it was more obvious." He added: "I have never seen this before [Child A]." Letby, in interview and cross-examination, had suggested the lighting in room 1 was 'not very good' and that was a possible reason why she could not see what Dr Jayaram had seen. Mr Johnson refers to Child I, when Letby could see in very poor lighting what her condition was.
Dr Jayaram had asked, in cross-examination, if he was being accused of making things up. "What is Lucy Letby's case, if Dr Jayaram is making things up?" Mr Johnson said it had been suggested Dr Jayaram had, in cross-examination, 'added dramatic detail' by mentioning the skin discolouration descriptions but not recording it contemporaneously in notes at the time, and had been accused of 'dramatic detail' when he said a 'shiver had gone down his spine' when he first read about the effects of air embolus. NJ: "We suggest that not only is Letby murdering babies, she is also prepared to trash the reputations of professional people in order to get away with it."
The trial is now resuming after a short break.
Mr Johnson says after the collapse of Child M, the night-shift of April 9/10 happened, and a Countess doctor described there was a plan to remove Child M's ET tube, following an "astonishing" recovery. He was put on to 'bi-pap' within 12 hours, and there was "no cause for concern" for a child who had had "such a devastating collapse". Dr Gibbs had queries NEC and sepsis at the time, but those could be excluded by following evidence. Child M required a dose of caffeine for a slowing breathing rate at the end of the following day. Dr Stavros Stivaros later said Child M had suffered a brain injury. Mr Johnson says this was as a result of the collapse. Mr Johnson says 'a fairly typical picture' in this case is of babies collapsing rapidly and unexpectedly, and recovering just as quickly. Medical expert Dr Dewi Evans said there had been no reason to do blood tests for infection, and subsequent tests ruled that out in any case. Dr Evans and Dr Sandie Bohin had said the cause of the collapse was an air embolus. Mr Johnson says there had been "evolving means of attack" by Letby.
Mr Johnson says there is only one conclusion, as said at the beginning of the trial - "there was a poisoner at work" in the Countess of Chester Hospital's neonatal unit. He says it has not been suggested by Letby or the defence that anyone was responsible for poisoning Child F and Child L. Child F was poisoned with two bags, and Child L was poisoned "with at least two bags", until the 15% dextrose bag was fitted and he began to improve. "Lucy Letby and Belinda [Simcock] were the only ones present when both [Child F and Child L] were poisoned." Mr Johnson says: "You can dismiss the possibility that two murderers were working in the same unit at the same time." Mr Johnson says Letby has 'rowed back' from disputing the accuracy of the insulin readings between her defence statement and giving evidence, and says it will be 'interesting' how the defence get her out 'of that particular creek'.
Mr Johnson moves to the case of Child K. He recalls the evidence heard by Dr Ravi Jayaram that Lucy Letby was "standing over" Child K as the alarm was not sounding and she did nothing. Mr Johnson says Letby had displaced Child K's ET Tube. The Child K case "shines a bright light" for what happened in Child E, Mr Johnson says, when Letby "was almost caught red-handed".
Mr Johnson says nurse Joanne Williams said it was "strange" Child K desaturated two further times, and the second and third incidents saw Child K 'well sedated'. The 6.15am desaturation (the second incident), happened between 6.07am and 23 seconds, and 6.15am, Mr Johnson says. An x-ray, timestamped at 6.07am and 23 seconds, shows Child K's x-ray, with a report the ET Tube was 'in satisfactory position'. By 6.15am, Child K was desaturating, Mr Johnson says. The tube had "gone down her throat" then had to be removed. "How on earth had that happened in a 25-week-old [gestational age] baby who had been on morphine?" Mr Johnson says Letby had no memory of this. He says Letby had been responsible for the admission process for Child K. He says the cross-examination at this time was a "somewhat tortuous process". He relays the cross-examination of this, in which he concluded he got told off for saying they 'danced the dance' in arriving at the point. He says they got there, 'in the end', in that Letby was in room 1 to obtain the medical notes for Child K to input the admission details on the computer, in a record between 6.04am-6.10am on the computer. He says those notes would have to be returned to the cotside in room 1 afterwards.
He says the coincidence between Letby's presence and Child K's desaturation "is not an innocent one". He says the third event for Child K happened at handover, which Mr Johnson says was not the only occasion.
Mr Johnson says once Child K's ET Tube was moved to the correct position, 'she picked up immediately'. Mr Johnson says after nearly being caught red-handed, like in Child E, she 'pressed home her advantage' and tried to create more of a problem for Child K which led her to desaturate again, by moving her ET Tube.
Mr Johnson refers to police interviews with Letby, in which she said Child K's tube had slipped earlier in the shift. Mr Johnson says Letby had, in interview, 'created the impression' of 'innocent tube movement' for Child K.
Mr Johnson says Joanne Williams had left at 3.47am to see Child K's mother, and had left Lucy Letby 'babysitting' room 1, Letby having fed a designated baby. It had been suggested to Dr Jayaram he was 'inventing' an allegation for Lucy Letby, to cover for shortcomings in Child K. "What did Dr Jayaram invent? What was it that was so offensive to their case?" Mr Johnson says Dr Jayaram said Joanne Williams had left and Letby was 'babysitting'. Dr Jayaram was 'suspicious' - "Letby can't say what was on his mind." Dr Jayaram walked into room 1 and saw Letby by the incubator. NJ: "What was Letby's case here?" Mr Johnson says he can't help the jury as Letby was saying one thing and then said another. He says if the jury is confused, then they have to ask why - he says the reason is because Letby won't commit herself. He asks if that is the case, then why? Dr Jayaram said Child K's observations dropped - there was no dispute about that. The alarm was not on, and that was not disputed. He said the cause was a displaced tube - that was not disputed. "Is Dr Jayaram a wicked liar to make up allegations about one of his colleagues?...or is he telling the truth?" Mr Johnson adds: "What lie did Dr Jayaram tell? We suggest it's all smoke and mirrors, that all these doctors are bad, that they tell lies, that they stitch her up."
Mr Johnson says evidence was heard to say a nurse would not leave a baby unattended without checking the tube was secure. Joanne Williams had checked the equipment and made sure the tube was secure, Mr Johnson said. A 'big play' was made of the 'high air leak' on the ventilator. It had been accepted the ventilator was sub-optimal, but said the oxygen saturations were 'optimal'. Mr Johnson says the leak was not having any impact on Child K.
A note was made of 'large blood-stained oral secretions' by Joanne Williams, but she could not confirm she had been present to see that. A doctor had said if he had seen blood stains during reintubation of Child K, he would have noted it and made Dr Jayaram aware of it. Mr Johnson says that note of 'large blood-stained oral secretions' had 'only come from Lucy Letby', and was "entirely typical behaviour by Lucy Letby". He says in Child K's remaining days before she passed away, the ET Tube did not dislodge again. Mr Johnson counts the number of seconds, each one, up to 30, for a 25-week-gestational age baby desaturating, which he says was the sight Letby saw from Child K's cotside. NJ: "It's uncomfortable isn't it? Even talking about it is uncomfortable. "That is why it's attempted murder."
Tuesday 20th June 2023
Prosecution Closing Speech - Day 2
Chester Standard Live Reporting - 20th June 2023
The trial is now resuming. Nicholas Johnson KC is turning to the cases of Child O and Child P.
He says the evidence of Dr Andreas Marnerides is uncontested, that Child O had a significant liver injury. That injury and the "lacerations" in the surface of the liver are "the best evidence you could ever have" of someone "inflicting a violent injury on a small child", he tells the court.
Lucy Letby's 'HELP' post-it note is shown to the court. Mr Johnson says it began with the note to all three triplets: 'Today is your birthday, but you aren't here + I am so sorry for that...I'm sorry that you couldn't have a chance at life... 'I can't do this anymore. I want someone to help me but they can't. What's the point in asking. Hate my life.' Mr Johnson says this note would have been written in June 2017 or June 2018. The note was found in Letby's handbag.
The note shown to the court.
Mr Johnson says Dr John Gibbs had given evidence to say if he had seen Letby 'in the act', he would have reported it to police at the time. He said the deaths of Child O and Child P were a "tipping point" that something was "very wrong" on the neonatal unit. He had been asked, in cross-examination, why he hadn't reported that to the police. He said: "At that stage, I didn't know two children had been poisoned with insulin." "At the time of the events I had never seen before which were unusual and unexpected - that's what raised the concern. "Medicine is not an exact science...just occasionally a patient dies, and [a post-mortem examination does not give an answer]. "But this was happening again and again on our unit. And that cannot be just coincidence or bad luck. There must be a cause. "That's when...one common cause was identified." Mr Johnson tells the jury they have one advantage is they know two children were poisoned with insulin, and knew who hung up the bags.
There had been "no concerns" for Child O or Child P on the shifts prior to the deterioration, Mr Johnson says. Letby had, in evidence, said concerns had been raised by Sophie Ellis and were not dealt with. Mr Johnson says Letby is "trying to persuade" the jury that a problem existed when there was none available.
Dr Huw Mayberry "remembered" Child O and he was "very well" with a "mildly distended abdomen" but all observations within normal limits. Mr Johnson says Letby's 'issue' for Child O did not exist. He says Letby pointed out that Dr Mayberry did not make a note. Mr Johnson says there were two occasions when Letby made up notes for doctors. One was a telephone call in the case of Child E, and another was the 'imaginary examination' of Child I by a doctor. Mr Johnson says Sophie Ellis's notes record that 'Reg Mayberry' was involved in being informed and 'reviewed' on June 23, 2016 for Child O. That was the difference, Mr Johnson explains, as Letby's notes do not attribute any doctor.
Mr Johnson says student nurse Rebecca Morgan was on her first day on the ward, fed Child O, and got a trace aspirate. Shift leader Melanie Taylor said there were no concerns for Child O at the start of the shift. "She did not expect [Child O] to collapse."
An examination of child O's abdomen revealed "no concerns" and this situation was "uncomplicated", and ruled out the possibility of liver haematomas at that stage. Had there been one, Child O would have had symptoms of deteriorating. Mr Johnson said it was accepted by Letby that Child O's liver injury happened during her day shift, and accepted the evidence of Dr Andreas Marnerides.
Mr Johnson says Letby was missing a doctor colleague and had been in a text conversation with him: "Bit rubbish that you couldn't stay on nnu". He said at 10.36am he should be finished on clinic duty in an hour. He then went to observe Child Q on his arrival. He then saw Child O. Letby recorded 'no problems' at 12.30pm. Mr Johnson says it is "obvious" Child O was "deliberately overfed" by Letby at this stage. There was "an issue" at 1.15pm.
Mr Johnson says Child O had been 'supposedly' fed 13ml of milk. By this stage he had vomited and his abdomen was distended. Letby was 'fulfilling two objectives', Mr Johnson says, by 'sabotaging' Child O and 'attracting the attention' of the doctor at the same time. Letby had recorded Child O was 'tachycardiac', which Mr Johnson says was 'an exaggeration'. Samantha O'Brien had said, in agreed evidence, Child O had a distended abdomen but looked otherwise normal. Letby messaged: "Blew up abdomen think it's sepsis" to a nursing colleague at 9.15pm and, for Child P the following day: "Just blew tummy up and had apnoeas, downward spiral. Similar to [Child O]." Mr Johnson says the 1.15pm vomiting by Child O was 'unusual', as observed by a doctor, but Mr Johnson says this is not so much in the context of Child E, Child F, Child G and Child L.
Mr Johnson says Letby made a false reading for Child O at 1.20pm on the blood gas chart. "Even by the standards of mis-recording information, this is right up there." He says the note Child O was put on to CPAP from Optiflo was "a lie", and it had been spotted by Dr Sandie Bohin. Mr Johnson says someone looking at the paperwork, retrospectively, might conclude this note could form an innocent explanation as to why Child O had died. Letby had said in evidence 'he wasn't on the full CPAP machine, he may have been receiving CPAP via Neopuff, I don't know.' A doctor had noted Child O's abdomen was distended. Mr Johnson says this was because Letby had pumped Child O full of air.
Nurse Melanie Taylor had said to Letby 'I don't think he looks as well as he did before', and queried if Child O should be moved to nursery room 1. Letby had said no, to leave Child O in room 2 with his brother. NJ: "Lucy Letby was so insistent, Melanie Taylor felt put out - she felt undermined."
Nurse Melanie Taylor had said to Letby 'I don't think he looks as well as he did before', and queried if Child O should be moved to nursery room 1. Letby had said no, to leave Child O in room 2 with his brother. NJ: "Lucy Letby was so insistent, Melanie Taylor felt put out - she felt undermined."
Nurse Melanie Taylor had said to Letby 'I don't think he looks as well as he did before', and queried if Child O should be moved to nursery room 1. Letby had said no, to leave Child O in room 2 with his brother. NJ: "Lucy Letby was so insistent, Melanie Taylor felt put out - she felt undermined."
Mr Johnson explains Facebook messages were exchanged between Letby and a doctor. Child O collapsed a few minutes after the last message Letby sent. The collapse was a sign for Child O of a cardiac arrest if there had been no intervention by medical staff, the doctor had said in evidence. Professor Arthurs said the gas in Child O's bowel, as shown in an x-ray from that afternoon, was more than there should be. The causes were NEC - which Mr Johnson says had been ruled out - or someone injecting air down the Nasogastric Tube. Mr Johnson says this is "even after a vomit", which would decompress the stomach.
Mr Johnson says the liver injury for Child O had "been inflicted by about this stage", and this was "long before" CPR. A '"small rash" had been seen on Child O's chest, a "purpuric rash - which is very, very rare in a neonatal infant", similar to a sign of meningitis. Dr Stephen Brearey, who had noted it, thought at the time it could have been a sign of sepsis.
Two doctors entered the NNU at 3.53pm and saw Child O 'being bagged by the nurse', and Child O was "very unwell". A female doctor was "shocked by what she saw" as it had been "completely unexpected". The doctors said there had been "good air entry" but Child O's saturation levels "were not improving", Mr Johnson says. Child O was reintubated and cannulated. Dr Brearey was called to help. Child O had been resuscitated. Spontaneous circulation had been re-established - "a miraculous recovery", Mr Johnson tells the court. "But [Child O's] perfusion was not as good as before." Dr Brearey said the rash was "perplexing" and something he had never seen before, Mr Johnson explains. An experienced doctor said the series of collapses were also like nothing she had seen before. Mr Johnson tells the jury: "You know the reason for it, don't you?" Mr Johnson says Child O's mother gave a description of the rash. The father said of Child O: "You could see his veins, all bright blue, changing colour... "You could see something oozing through his veins."
During Child O's resuscitation in his final collapse, a doctor had said efforts were made to decompress Child O's abdomen. In cross-examination it had been suggested this was the cause of the liver injury. Dr Brearey and Dr Marnerides had rejected this, Mr Johnson tells the court. An x-ray was taken of Child O, and Professor Owen Arthurs had explained the bowel gas which was "unusual" and showed an NG Tube in situ and no presence of NEC. Child O and Child P didn't have bowel obstructions, and Prof Arthurs said you are left with injection of air by the NG Tube. Dr Brearey said all triplets had been born in good condition and were "following a healthy path", and these events were "exceptionally unusual", and the type of rash was 'something he had never seen before or since'. NJ: "All natural causes were excluded...even with the benefit of all the years that intervened." Another doctor said it was "incredibly unexpected".
Mr Johnson says Letby took Child O to his death. He says Letby was "sowing the seeds" for Child P the following day. The message sent by Letby to a nursing colleague at 9.33pm on June 23, 2016: "Worry as identical".
A conversation between the doctor and Letby is shown to the court. The doctor said he hoped he was able to help. Letby replied: "Yes you did++" NJ: "Two plusses was the best he was going to get." A Datix form is shown to the court, recorded by Letby, which Mr Johnson says was inaccurate in the 'peripheral access lost' note. Dr Brearey said "it's not correct". Mr Johnson says "it's a lie". He says Letby is trying to invent evidence that peripheral access was lost. If it was, Mr Johnson say, then air could not be injected into the infant. He says if that note was accepted, it would support her case that this was not air embolus. Mr Johnson asks the jury to find why Letby was lying - "to cover up what she had done...we are sure this was air embolus."
Dr Dewi Evans was "taken to task" for changing his opinion while writing his numerous reports in cross-examination, Mr Johnson says, having come up with a number of theories. Mr Johnson says more information came to light during the course of writing his reports between 2017-2019. One was Dr Brearey's note about the purpuric rash 'disappearing'. It was established there had been no mention in medical notes of the rash disappearing, and he was only informed about it by Dr Brearey's witness statement in 2019. Mr Johnson says is the impression by the defence to say Dr Evans "doesn't know what he's talking about?" He says it would be "astonishing" if Dr Evans hadn't changed his mind when handed new information.
Mr Johnson says Dr Evans said in court: "Inevitably, one amends one's opinion as a result." Dr Evans was asked about chest compressions for Child O. He had said he had known no case that chest compressions had resulted in a liver haematoma as seen in the case of Child O. A doctor had said chest compressions were carried out correctly for Child O. Dr Bohin had "spotted that lying entry in the gas chart". She had taken all the evidence into account, including that of Child O's father, of the description of the veins, like 'prickly heat', Mr Johnson tells the court. Mr Johnson said it had been suggested Prof Arthurs had ruled out air embolus as a cause. NJ: "Nothing could be further from the truth." He says Prof Arthurs said the air in the great vessels could be from a number of causes, including air injected, or CPR or trauma. Mr Johnson asks the jury why CPR was required for Child O - he says it was because of air embolus. Prof Arthurs was 'deliberately not doing' what the jury can do, and was treating the cases independently. Prof Arthurs added radiographic evidence of air embolus is "very rare".
Dr Andreas Marnerides' evidence is "compelling and uncontroverted", Mr Johnson says. He says the conclusions were that "significant" force was applied It was "certainly not" an injury formed by CPR. He had never seen, heard of or read of this kind of injury caused by CPR. Mr Johnson says the idea this is the only time this has happened by CPR is "truly fanciful". He says there is no corresponding puncture injury from a needle. The outer surface injury was likely caused after death as there was no 'active circulation' for Child O. There was 'profound gastric and intestinal distention' - i.e. they were 'blown up with air'. Dr Andreas Marnerides concluded it was by injected air and air embolus. Mr Johnson says this case was among the most violent carried out by Letby. He adds: "Of all the offences, all the appalling examples - some of the earliest were less violent but no less devastating." He cites the case of Child E as one of the early, violent examples. He says Letby had "misplaced confidence" following her return from Ibiza "that she could do pretty much what she wanted." He adds: "Frankly, by this stage, she was completely out of control, and was determined to mete out [the same kind of attack to Child P] the very next day."
The trial is resuming after a short break.
Mr Johnson turns to the case of Child P, who was 'doing well'. His case "caused confusion" with several witnesses as to when he came off breathing support, he says. Child P was breathing in air from 6.30am on June 23, 2016 and his antibiotics were stopped, and he was put on expressed breast milk. His observations were 'unremarkable'. A further examination at 6pm was carried out. Dr Gibbs said, following Child O's death: "Oh no, not another one". He said he had become increasingly concerned about the number of incidents on the neonatal unit, and that Letby had been involved in all of them. Child P's abdomen was 'full...mildly distended'. Letby had said the student nurse had fed Child P that evening. Mr Johnson says this was a lie. Child P was "remarkably well - excellent for a triplet baby". Blood tests were taken as a precaution at 6.45pm, showing "no evidence of infection". As a precaution, Child P was put on to antibiotics. Dr Gibbs said the abdominal distention was 'CPAP belly', but he said he had 'misread the chart' - Child P had not had CPAP for two days, and had been taken off Optiflo. "That was not CPAP belly," Mr Johnson tells the court. Mr Johnson says Letby overfed Child P just before she left her shift so she could give the impression this was a child who was deteriorating.
Mr Johnson says what happened here "mirrors" what happened with Child N earlier that month in June 2016. He says Letby did not leave the unit until 9pm that night on June 23. A message sent by Letby to a doctor colleague said she was finishing up notes for Child O. Emphasis had been put on a good blood gas reading for Child P at 8.27pm on June 23 by the defence, Mr Johnson says, but Sophie Ellis gave evidence to say Child P desaturated and had a '14ml part digested milk aspirate' at the 8pm feed. Mr Johnson asks what possible other cause is there other than Letby overfeeding Child P for the baby's last feed before the end of her shift? Mr Johnson says that is why Letby says the last feed was done by the student nurse. Overnight, another large part-digested aspirate was obtained and Child P's were stopped as a precaution. The NG Tube was placed on free drainage. Kathryn Percival-Ward [Calderbank] said Child P was "a well baby" but his abdomen was distended, so she decided to aspirate the stomach. This was recorded at 4am. A further 5mls of air and 2mls of milk were aspirated by Sophie Ellis at 7am. Mr Johnson says the problem Letby had created had been "resolved by proper nursing care" by the two night-shift nurses.
Child P had been, quote, "a little angel overnight", as said in agreed evidence. Letby came on duty, and Child P collapsed shortly afterwards. Mr Johnson says this was Letby at her most malevolent. The 'worry as identical' was "gaslighting at its very best - or worst", as Letby had been laying the lines for what would happen to Child P the next day, Mr Johnson says. "There was nothing wrong with [Child P] at the end of that night shift". Mr Johnson says Letby 'decided to use the template from the day before'. Letby recorded in notes: 'Abdomen full - loops visible, soft to touch.' Mr Johnson says that note wasn't written until 13 hours later, and was a "fabricated note" to give the impression of what had been happening earlier that day for Child P. He says Sophie Ellis recorded for Child O - 'abdo looks full, slightly loopy'. Mr Johnson says this is the equivalent of copying someone's work. He says this observation "happened out of nowhere" for Child P, for a child on free drainage, having been stable. He says if that was observed, Letby would have escalated it immediately, in light of what had happened the previous day. Mr Johnson says instead Letby was texting a doctor colleague at 8.04am. 'I'll be watching them both like a hawk. I’m ok. Don't want to be here really. Hoping I may get the new admissions...' She also mentioned 'I've got [other triplet] and [Child P], [Child P] has stopped feeds as large asps.' Mr Johnson says there is no mention of a loopy bowel for Child P, by Letby to her doctor colleague, as "there is no problem".
At 9.35am on June 24, Dr Anthony Ukoh did a ward round and examined Child P, finding a mildly distended abdomen with bloating. Letby had said looping was visible at this time, and Dr Ukoh had noted this. Mr Johnson says the note was checked and it was not noted. The abdomen was 'soft', he recorded. A consultant doctor noted nothing of concern, other than a distended abdomen. Mr Johnson says there is another case of Letby falsifying notes here. A nursing note by Letby said Child P had been 'Neopuffed for a minute before being examined by Dr Ukoh'. Mr Johnson says it is suggested this is a deliberate mis-recording, minutes before Child P's collapse around 9.40am. He says it is a way of 'covering what she did', by 'pumping [Child P] full of air.' Child P 'crashed', stopped breathing and his heart stopped. He was 'dusky and mottled', according to a witness. A doctor was alerted to Child P in room 2 at 9.50am, it was 'not an emergency, but something he should be called to'. Letby was "not in the room" according to student nurse Rebecca Morgan. Mr Johnson says the jury should consider why that would be the case, as Letby didn't have any designated babies outside of room 2.
Dr Ukoh said Child P "appeared very different" from earlier. He added: "Whoever was doing the Neopuff was very keen on getting [the doctor] in". Mr Johnson says to the jury it's clear who that would be, that Letby wanted this doctor colleague to be present. NJ: "For some reason, she enjoyed these situations, and he was there."
Mr Johnson says the second deterioration happened at 11.30am, and CPR was required. One female doctor said Child P was "vigorous" and fighting the ventilator, something which was unusual as it would not fit the sign of a baby fighting infection. Mr Johnson says Child P was being sabotaged - blood tests excluded infection for Child P. An x-ray at 11.57am showed a pneumothorax and air in the bowel. Just after noon, a female doctor saw several nurses including Letby, and told the people there the transport team would be there soon. The doctor said: "I was thinking out loud" - and, Mr Johnson says, Letby replied "He's not leaving here alive is he?" This is something which was not disputed by the defence, and Letby had said in cross-examination it was said out of concern. In police interview, Letby said she could not remember saying that, Mr Johnson adds.
Letby had agreed in cross-examination it was "not the done thing" to say such a thing, then she had said she couldn't remember saying it. Mr Johnson says it was not disputed she had said it, the question was "Why?" NJ: "She was controlling things - she was enjoying what was going on and happily predicting what was going to happen - she was 'playing god'." The female doctor had said: "Don't say that." in response. The comment was "highly unusual" and "shocking", the female doctor said.
Child P's 12.28pm collapse should be thought in the context of Child K, Mr Johnson says. Two doctors had taken a break when a shout for help happened at this time. When they returned, Lucy Letby was in the room. A doctor said it looked like Child P had "dislodged his ET Tube". Mr Johnson says if the tube was blocked, it had done so in a short period of time, having only been put in hours earlier. Mr Johnson says this collapse happened "at the precise moment" the two doctors had left the room, and Letby was present, and the ET Tube dislodged in Child K, when Letby was present, doing nothing. He says the jury should take that all into account. He says the jury can also take account of Letby's remark "He's not getting out of here alive is he?" made shortly before this collapse. Mr Johnson says the ET Tube was not blocked, Letby had dislodged it. Child P was reintubated and further resuscitation efforts began. Dr Bohin said the pneumothorax was a contributory factor in the collapse of Child P, but not the overall cause.
Dr Stephen Brearey reviewed the circumstances of Child P's death, and regarded the events that day as "exceptional", and could not find a cause. A doctor could not identify any cause as to what had gone on. He thought it 'highly unlikely' the death was complications over the pneumothorax'.
The trial judge, Mr Justice James Goss, says as the day will end a little earlier than usual, this afternoon will be one extended session without a break.
Mr Johnson describes what happened for the final collapse for Child P, after the transport team had arrived. He says despite Child P's situation, there was good air entry and the ET Tube was in a good place. There was "no explanation" for why Child P's condition had changed, according to a doctor.
At 4pm, it was determined the resuscitation attempts were futile. The father said the circumstances for Child P's death were similar to Child O, but could not recall seeing a veiny appearance for Child P (as he had done with Child O). The mother said the third triplet had no problems and was discharged after 11 days. Mr Johnson says that should have been the case with all three. A female consultant said Letby was "animated" and "so excited" asking about a memory box and her behaviour was "inappropriate". In cross-examination, the 'talking enthusiastically' was said that it would 'soften the blow' for the grieving parents who had lost two of the three triplets. NJ: "We suggest that is absurd. Lucy Letby was enjoying the drama, the control, the extremity of grief that she was causing to other people." The father, in the aftermath of Child P's death, was "sobbing" and begged doctors to transfer the third triplet to be taken with the transport team. The female doctor said what had happened was "not normal".
Mr Johnson: "Something was seriously wrong. They just couldn't put their finger on it." The female doctor had said in cross-examination she was not dramatising anything, the situation was dramatic enough as it was. Mr Johnson says nothing was identified medically as the cause of Child P's death. Dr Brearey said the deaths of Child O and Child P caused him great concern. The rash, he had not seen before or since. At the debrief, Dr Brearey asked Letby how she was feeling, and suggested she needed time off, "but she didn't seem upset", and was due to work the next day. Mr Johnson said that caused Dr Brearey "real concern".
Dr Andreas Marnerides did not look at the cases in the context of any other. There was "no natural cause" for Child P's death. He concluded Child P had "excessive air injected into the nasogastric tube". Dr Evans said there was no natural cause, and the cause was air administered. Dr Bohin pointed out a discrepancy between Letby's 'Neopuff' note and it not being mentioned to Dr Ukoh when he examined Child P, Mr Johnson says. Mr Johnson says this is "yet another false example" in the notes, designed to create the impression Child P had an ongoing problem.
Dr Bohin also said Child P had been injected with air, Mr Johnson says. Mr Johnson says if the jury conclude Child O received a liver injury through some inflicted trauma, then Child P's liver injury the following day can be explained by Letby's actions. NJ: "Lucy Letby predicted [Child P's] death when Dr Brearey thought it was under control. How could she have known?" "The number of coincidences here is all too much. [Child O and Child P] were murdered by Lucy Letby."
Mr Johnson says Letby had said she had taken one note/handover sheet home deliberately as it contained information to write up as nursing notes when she returned to work. Mr Johnson says the note only included 'caffeine', so her reason for keeping it was 'a lie'. Mr Johnson says one of the handover sheets contained a name of one of the baby's parents, a difficult to spell name, that she could research on Facebook later. He says Letby's explanations for keeping the handover sheets don't stand up "to any sensible analysis".
Mr Johnson refers to this note. He says the words 'I AM EVIL I DID THIS' should be taken literally. He says the 'anguish', as the defence said was Letby's frame of mind, needs to be taken into context. He says Letby introduced the suggestion she was "isolated" to explain the notes and her behaviour. On the final day of cross-examination, the contents of Letby's phone, diary and photographs "set out her social life" from July 2016- July 2018. Letby "accepted" she had "a very, very active social life" which included "socialising with many of her former colleagues" including "those she had been forbidden from having contact with". She said she was "at least allowed a social life". Mr Johnson says it was "never our suggestion" that she wasn't allowed to have a social life. He says Letby was "deliberately trying to mislead you" and trying to invoke "pity" from the jury. NJ: "We say she is a liar, she lied to you, and the lie is proved by analysis of her social life."
Mr Johnson recaps the seven baby's cases he has dealt with so far, of the total 17. He says if they are all taken into context, the "picture is crystal clear". He says he will take the next cases in chronological order, with twins Child A and Child B.
Mr Johnson says the judge directed that the questions given by counsel are not the evidence, but the answers. He asks if Dr Jayaram and Dr Harkness 'made up' their observations for Child A and Child B to blame Letby. He says before the cases of Child A and Child B, Letby had completed a course on IV lines, which highlighted the dangers of air embolus. Mr Johnson asks if that was a "coincidence".
Mr Johnson says Child A had been doing well and was on hourly observations, and handling well. Child A crashed minutes after Letby came on duty. Mr Johnson says there is no doubt Letby had been involved with Child A's care. He says the evidence was that Lucy Letby was "literally standing over him" at the time of the collapse. He says the circumstances of the collapse are similar to that of Child L and Child M, with Letby "operating in plain sight".
Mr Johnson says despite air going in and out, Child A's saturation levels and heart rate were falling. He says Dr David Harkness described "very unusual patches of skin [discolouration]" which he had "never seen before" and only saw once again with Child E. He described "patches of blue, purple, red and white" that didn't fit with Child A's condition, and the rash "flitting around". He said he was too busy trying to save Child A's life to get a full description. He was criticised in cross-examination for not noting it down. It was suggested by the defence that he had been influenced to apply this description to Child A, and not putting this in his statement. Mr Johnson asks what the implication was - that he didn't see anything? It was suggested discussions had deep-set in his mind. Dr Harkness said he had seen it in Child A and Child E, that made him realise how significant this discolouration was. He was "animated" in the latter case, Mr Johnson says. Dr Ravi Jayaram had said Child A's heart trace showed "no problem" with the baby's heart.
Dr Jayaram had described 'pink patches that appeared mainly on the torso that appeared and disappeared - I had never seen anything like this before,' Mr Johnson says. He had said it "doesn't fit with any disease process I had seen or read about".
Dr Jayaram was 'taken to task' by the defence, Mr Johnson says, as he had not mentioned the discolouration in notes. He said he had not realised the significance of it at the time, and only realised it when later examples came up in other babies. Mr Johnson says the accusation by the defence that Dr Jayaram had made it up is "smoke and mirrors" to distract jurors from the truth. He says there is other evidence, not disputed, to back Dr Jayaram's account. He refers to Letby's July 2018 police interview. Letby had referred to the rash for Child A as a 'rash like' 'reddy-purple' 'more on the side that had his line in - it was his left'. NJ: "How did Lucy Letby remember that? Because it wasn't actually in her notes - just like Dr Jayaram and Dr Harkness." Mr Johnson says Letby referred to it as 'normal mottling' and Child A was 'more pale than mottling'. Mr Johnson says that is "a lie". Mr Johnson says if Letby accepts that as "unusual", it "causes real problems for her defence". He says Letby used the word 'blotchiness' for Child A in police interview. Letby had said 'mottling' and 'blotchiness' were interchangeable.
Mr Johnson says Letby had said in cross-examination, if it was agreed Child A had died of an air embolus, then it would have been administered by colleague Melanie Taylor, and not by her. NJ: "We suggest Lucy Letby was as good as accepting that [Child A] died of an air embolus. "But it doesn't end there." Mr Johnson says Letby's nursing colleague, a friend, came into the unit when Child A collapsed and did CPR for Child A, and noted a 'strange skin discolouration' she had "never seen before". He says the colleague described "blotchiness" - the same word Letby had used in her defence. The colleague was challenged on the description for Child A's skin discolouration, that it might have been mixed with the description for Child B. She said she had not been influenced by what anyone had said. Mr Johnson says the nursing colleague was not accused of making it up. He says it is the defence's case to picture the "doctors are bad".
Dr Rachel Lambie had described 'blotchy' 'purple' marks which would appear and disappear on Child A, Mr Johnson said. She said she had "never seen anything like it before", with "flushes of what looked like bruising underneath" "that would appear for 10 seconds, go, then appear somewhere else", Mr Johnson adds. Mr Johnson says all the other colleagues had proved what Dr Harkness and Dr Jayaram was saying was the truth. He asks the jury if that is the case, then what purpose is the attacks on their integrity? He says the purpose was to deflect the jury from the evidence, to make it about personalities, to destabilise Dr Jayaram "who has been an important witness in many cases", including for Child K. NJ: "Lucy Letby knows how devastating his evidence is in the case of [Child K]." He says it is the defence's case that the nurses are overworked and the doctors are "bad", that there is a "medical conspiracy" involving the "gang of four", and an unnamed police officer 'tipped off' Dr Evans about air embolus.
Mr Johnson says after Letby got home, she advised Melanie Taylor about an administrative note, then searched for the mother of Child A on Facebook.
Mr Johnson turns to the case of Child B. Mr Johnson says "we know that Letby didn't like" being in nursery room 3, and there are "many" text messages sent between Letby and four people over the course of two hours. Five minutes after Child B desaturated around midnight on the June 9-10 shift, Mr Johnson says, Letby turned up in room 1 as she co-signed for medication. No-one signed for the observation readings for Child B at midnight. Letby has signed for a blood gas reading for Child B at 12.16am. Child B had collapsed at 12.30am. The mother of Child A and Child B said it was "a very similar situation to [Child A]", and the consultant asked for pictures to be taken of the mottling as she had "never seen it before". By the time a camera had been sourced, the mottling had disappeared. Dr Lambie had made a note of the discolouration at the time. A nursing colleague said Child B "suddenly looked very ill - like her brother the night before", with the discolouration. Mr Johnson says the colleague had said: "Oh no, not again", and made a note of it, which read "changed rapidly to purple blotchiness with white patches".
Mr Johnson says Letby had used the words a 'rash-like appearance' as it looked like a rash on Child B, and it was "unusual". "Lucy Letby, we suggest, could not keep out of nursery 1. She elbowed her mate...out of the way." Letby signed for a blood gas record for Child B at 12.51am while Child B was being resuscitated, and signed for a 1am observation reading, and co-signed for a morphine administration at 1.10am. NJ: "She was relentless, ladies and gentlemen - she thought she had the cover of antiphospholipid syndrome [for Child B]." Letby searched for Child A and Child B's mother again on Facebook on June 12 and September 2, 2015.
Mr Johnson says the presence of air was the cause of, or the need for, resuscitation. Prof Arthurs says the gas was "not diagnostic" of air embolus, but added it was "the most pragmatic conclusion", Mr Johnson says. He adds the only time he saw that much gas was in the case of Child D. Mr Johnson says medical expert evidence from Dr Andreas Marnerides had shown an air bubble was found in Child A's brain, which was "highly suggestive" of air embolus. He found "no evidence of any natural disease" and "took the view" that the most likely cause was "air embolus". Mr Johnson says the picture is clear, from the witnesses' accounts - including Letby's, that air embolus was the cause of Child A's death, and if that is the case, then Letby was responsible.
Dr Dewi Evans says, for Child A, the baby was "perfectly stable" prior to the collapse. He cited air embolus as the cause, and that conclusion was reached even before Dr Jayaram's account, as Dr Jayaram's description had not been in the notes. He said for Child B, there was nothing that could account for that baby's collapse. He said the rapid appearance and disappearance of the skin discolouration was significant in his conclusion of air embolus.
Wednesday 21st June 2023
Prosecution Closing Speech - Day 3
Chester Standard Live Reporting - 21st June 2023
Nicholas Johnson KC resumes the closing speech for the prosecution, starting with the final part for the case of twins Child A and B. Medical expert Dr Sandie Bohin said Child A had been stable, and the misplaced UVC [line] "had no bearing" on his collapse. She said Child A had received an air embolus. In cross-examination, it was suggested she could not exclude genetic causes for the death of Child A. She replied she did not know of any genetic condition that causes a baby to collapse and die within 24 hours of birth. Mr Johnson says Letby's case "floats the spectre of possibilities" without going into specifics.
Mr Johnson said dehydration was also ruled out as a possible cause of death for Child A. Asked about an 'innocent air embolus' via the catheter, Dr Bohin said she had "never heard of it happening in a neonatal unit" due to the equipment used. For Child B, Dr Bohin had said the baby was "in good shape". She concluded Child B had received an air embolus.
Mr Johnson says the jury has an advantage over medical experts, in that they can look at all the pieces of evidence presented in the case, including Letby's Facebook searches for the parents, her presence on the unit, standing by babies, and there being a "poisoner at work" on the unit, to draw conclusions. "It's the cumulative evidence", Mr Johnson says is key. He says Child A and Child B had similar skin discolourations, and a "concession" from Letby that "if we agree", that Child A died of an air embolus.
Mr Johnson said Lucy Letby "migrated" to room 1 shortly before Child B's collapse, to use the word of Kathryn Percival-Ward.
Mr Johnson turns to the case of Child C. He says Dr John Gibbs first gave evidence on Halloween 2022. He was asked if Child C should have been treated at a tertiary centre. Dr Gibbs replied it depended on what caused Child C's collapse. He denied that in any event it would have been more suitable for Child C to be treated there. Mr Johnson says there has been no evidence presented to suggest the babies in this case would have been better treated at a tertiary unit. [The Countess of Chester Hospital being a Level 2 unit at the time]. Mr Johnson says the jury should ask if there had been any specific shortcomings for the babies in each case. He says the babies would have been better off away from Lucy Letby. He says that may have been what Dr Gibbs meant.
Mr Johnson says Child C, a baby boy, was "born in good condition" and "made good progress" and was "handling well". A nursing family communication note on June 12, for 6.30pm, 'parents spent most of the day with [Child C]...enjoyed kangaroo care most of the afternoon' - Mr Johnson says this was a good sign. Dr Katherine Davies was asked about traces of bile found. She was asked, in evidence, if that was a sign the baby would later collapse. She replied: "Absolutely not." Mr Johnson tells the court she said Child C's abdomen was soft, and if he had an abdominal problem, it would be sore, but he was handling well, and his other observations were stable, which was why he had been out for kangaroo care. By June 13, 2015, Child C was given tiny milk feeds 'to get things moving' in the gut.
"Witness after witness" gave evidence to say the bile aspirates were "very small", and the "black colour" was "altered blood", not bile. Dr Gibbs said the blood had come from inflammation in the stomach, and Child C was given a drug to treat that. Mr Johnson says the jury know, as a fact, from Dr Andreas Marnerides, that Child C did not have a problem with his gut, as there was no sign of infection or sepsis. There was no evidence of Child C having had an obstruction in his bowel. "This is not a case of NEC," he adds.
Nurse Yvonne Griffiths described Child C as an active baby who was "happiest" when receiving kangaroo care, and nurse Sophie Ellis said Child C was "feisty". Mr Johnson says all the treating staff for Child C said he was doing very well - on the three days Letby was not on the unit. He says within a few hours of Letby coming on to the unit, Child C collapsed, and within a few hours of that collapse, died. Mr Johnson said Dr Gibbs could not explain how Child C's heart could have restarted after the collapse, as it did not follow any natural disease process.
Dr Sally Ogden said Child C's abdomen was, on June 13, soft. Mr Johnson says he was "doing well" as observations were normal and he was put on to Optiflo, having gone off CPAP breathing support. Letby's nursing colleague suggested to Letby that the baby in room 3 was more of a priority as that baby had breathing difficulties, than Child C in room 1. "Lucy Letby was not happy about being in nursery room 3," Mr Johnson says. Letby texted colleague Jennifer Jones-Key: "I keep thinking about Mon. Feel like I need to be in 1 to overcome it but [colleague] said no" "Not the vented baby necessarily, I just feel I need to be in 1 to get the image out of my head. Mel said the same and [colleague] let her go. Being in 3 is eating me up, all I can see is him in 1 x" Mr Johnson says the baby who was not vented would be Child C. Mr Johnson says there was no reason for Letby to be in room 1. Letby texted Jennifer Jones-Key: "Yeah I've done couple of meds in 1. I'll be fine X" Mr Johnson says this is something Letby has since revised in her evidence. The neonatal schedule shows Letby being a co-signer for babies in room 3. Mr Johnson says it "stretches the definition" to suggest Mr Johnson says it was "repeatedly" questioned whether Sophie Ellis - "the new girl" as was "up to the mark" to look after Child C. Three nurses dismissed that suggestion. Mr Johnson says in cross-examination that was taken up with Letby. NJ: "The person who had what you wanted wasn't sufficiently qualified for the job?" LL: "No, Sophie wasn't, I think, in the correct position to care for [Child C]." NJ: "Why was that?" LL: "She was recently qualified, she didn't have the skills." LL: "She didn't have experience of premature babies, babies like [Child C]." LL: "I am not saying Sophie caused anything with [Child C], she was just the least experienced. She had very little experience with premature babies." NJ: "So she had something you wanted?" LL: "No." Mr Johnson asks the jury what Sophie Ellis failed to do that a senior nurse would have done. He says there is no evidence of anything, and asks why that suggestion was made to three nurses in cross-examination. He says it is trying to create "something seriously wrong at the hospital" and is "gaslighting" the jury.
Mr Johnson says the series of text messages, and its content in relation to , suggests Letby was not rushed off her feet but had "death on her mind" and sabotaged Child C. Sophie Ellis aspirated Child C's stomach and found a small amount of green bile. There was no air or anything else, Mr Johnson says. She left the room and within a short amount of time, the alarm went off. Upon her return, Letby was standing by Child C, and Letby said words to the effect of: "He's just had a brady/desat". Nurse Melanie Taylor was challenged "repeatedly" on her account of the event. She said she remembered Letby being "at the centre of events". She said she was "surprised how cool and calm" Letby was. Dr Kathrine Davies was 'crash bleeped' to the room. There were no heart sounds or respiration, and this was "very unusual". She said even with the smallest, sickest babies [who had collapsed], there would be some heartbeat, or respiration rate, but with Child C there was "nothing at all". During intubation, Child C's vocal cords were seen by Dr Davies to be swollen. Mr Johnson says that is found in five of the babies' cases, in Child E, Child G, Child H and Child N. "Somebody put something down [Child C's] throat. Who do you think that was?"
Dr Gibbs said if there had been an abdominal obstruction, there would have been 'repeated vomiting'. Child C's parents had given evidence in an agreed statement, when Child C had started breathing after being baptised. "We held him for hours...and he was given another dose of morphine." The 'rally' of survival lasted "a long time", Mr Johnson says. He says during the time with the family, they were interrupted by a nurse the father believed to be Letby. The father recalled the nurse said words to the effect of: "You've said your goodbyes now, do you want to put him in here?" A nursing colleague had told Letby 'more than once' to look after her designated baby, as she had been going 'in and out' of the family room. Mr Johnson asks why Letby had a fascination with that room, and cites her behaviour as noted in the cases of Child I and Child P. "It is not an innocent coincidence." He says Letby, in cross-examination, "could not give a plausible reason" why she kept going into that family room instead of looking after her designated baby that night.
Text messages between Letby and a colleague were exchanged on June 30, 2015: Colleague: "Yeah. There's something odd about that night and the other 3 that went so suddenly." LL: "What do you mean? "Odd that we lost 3 and in different circumstances?" C: I dunno. Were they that different? C: Ignore me. I'm speculating LL: Well Baby C was tiny, obviously compromised in utero. Baby D septic. It's Baby A I can't get my head around C: Was she definitely septic. Did the PM confirm? LL: I don't think the full PM is back yet. Debrief is next week but I’m away. C: When's Baby A's? They were talking of doing a joint one for all 3 as all close together and similar in being full arrests in babies that were essentially stable. Dunno if they are doing tho. LL: Ah not sure but Baby C's is Thursday and Baby D next week LL: No mention of Baby A"
Mr Johnson says Dr Dewi Evans was justifiably criticised for not giving a cause of death for Child C in written evidence, then giving a cause in the witness box. He says if anyone was caught by surprise, he returned to give evidence on 14 more occasions. Mr Johnson says Dr Evans's evidence can be disregarded if there had been any confusion for this case, as Dr Marnerides had given more detailed evidence on this. Dr Bohin excluded the possibility of a bowel obstruction. Dr Marnerides said there was "nothing unusual" about Child C's bowel. He concluded Child C died "with pneumonia not from pneumonia" and the gas in the bowel could not be explained by infection or an abnormality in the bowel. He said "air must have been injected into the nasogastric tube", splinting the diaphragm, which would have compromised Child C's breathing and killed him. He added: "I have never in the past 10 years, come across even a suggestion that 'CPAP belly' would lead to the deterioration of a baby, let alone this gastric distention that would lead to [a baby's death]." Mr Johnson says Child C came off CPAP 12 hours before his collapse, and "did so well" after kangaroo care he was put on to Optiflo, a 'much less invasive method of breathing support, and his NG Tube had been aspirated shortly before his collapse, and no air was found. Dr Marnerides described "massive" gastric distention, using the word "ballooning".
Mr Johnson says Letby's interviews are very important in this case. Letby had said her only involvement with Child C was with his resuscitation. She said she did not remember being the nurse who fed him. She claimed she was not the person who discovered Child C collapsing. She said rough notes on the resuscitation would be transposed into medical notes and then disposed of. She confirmed she had contact with Child C's family when Child C was dying. She would not accept Sophie Ellis's account of her 'standing over' Child C. When asked why she would have been in room 1, Letby said perhaps she was checking the resus trolley, or getting drugs for her baby, or using the computer. Mr Johnson says 'why would you be checking the resus trolley?' and 'why would you use a computer in the dark'? Letby was asked about the text message conversation with Jennifer Jones-Key. NJ: "She claimed, unbelievably, she didn't know what that conversation was about or where she was [when that text conversation took place]. "We say that is incredible, that is not believable." Of the message 'being in 3 is eating me up', Letby accepted she was frustrated she was not in nursery 1. NJ: "She [Letby] accepted she was in room 1 at the time of the collapse, that she was the only staff member there, and she was feeling frustrated and upset." In the 2020 police interview, Letby said she did not remember being involved with Child C's family after Child C's collapse. She said she "wasn't sure" why she had searched for Child C's family on Facebook. She said she "didn't specifically remember what she was thinking" prior to the collapse of Child C.
Mr Johnson says the collapse and death is "inconsistent" with all natural causes, according to the medical evidence. Letby was in her own interview 'angry and frustrated' about not being in room 1. NJ: "She started the interview process by lying about where she was and the reasons for being in room 1" Child C had "massive ballooning of the stomach" and "it's obvious what happened" even without the context of the other cases. NJ: "It's as plain as the nose on your face that Lucy Letby must have injected air down the nasogastric tube [into Child C]. "It was one of her favourite ways of trying to kill children in this case." Mr Johnson says there is a "constellation of coincidences" that can make the jury sure Child C did not die of natural causes and that Lucy Letby killed him.
The trial is now resuming after a short break. Mr Johnson turns to the case of Child D. He says Letby "didn't really remember" the baby girl, as she had said that in police interview. He says the absence from the paperwork of her involvement would "give her plausible deniability". He says "thanks to the hard work of the police", they can put her in the room. He says Letby's interview is undermined by the rota diagram putting her in room 1 on the night shift [with Child D], and for her searching for the parents' names on Facebook. He says Letby could have got the names from the handover sheets - but the handover sheets do not have the parents' names on them. Mr Johnson says this is similar to Child K, when Letby searched for the parents on Facebook 26 months after Child K's time on the neonatal unit. Letby said she could not explain it. Mr Johnson says that is a lie. NJ: "Why won't she tell you the truth?"
Mr Johnson says there is "no doubt" Child D and her mother suffered sub-optimal care, but her progress went "upward" upon her transfer to the neonatal unit. Child D was "stable" with "minimal" oxygen support, and "responding well to treatment". The court had previously heard evidence Child D was on CPAP, "responsive when handled" and her "chest was clear" with "regular respiratory effort". He abdomen was "soft and non-distended". Mr Johnson turns to the night shift on June 21-22, 2015. Mr Johnson says June 21 was Father's Day that year. Child D's designated nurse Caroline Oakley also had a designated baby in room 2. Child D was in room 1. Letby's designated baby in room 3 from the Child C case was now in room 1, again as Letby's designated baby (along with one other baby in room 1). Child D's observations were "all completely normal" according to Caroline Oakley, and she was "breathing beautifully in air", with 100% oxygen saturation - "the highest they can be". Mr Johnson says this couldn't be better for a child with pneumonia.
Dr Andrew Brunton said the plan was for Child D to start receiving milk. Mr Johnson says there were no problems until Caroline Oakley left the room for a break. He cites other cases when this happened of staff members who left and babies collapsed. The alarm went off and when Kathryn Percival-Ward arrived, she found Letby in room 1. She said, in cross-examination, she "couldn't be certain". Mr Johnson says who else could it have been? Who else had children to care for in that room? He says it wasn't any of the other nurses on duty that night - one was looking after babies in room 2, and another was Elizabeth Marshall, a nursery nurse, who said she saw Letby doing chest compressions on Child C in room 1. Kathryn Percival-Ward said the rash on Child D was "something she had never seen before". In cross-examination, she was accused of "adding detail" to the skin discolouration description. Mr Johnson says it was in the original recording she had made to police, a "mosaic, a mottling colour of blotchiness". Caroline Oakley recalled being called back to room 1 by Kathryn Percival-Ward and Lucy Letby.
Mr Johnson had asked Letby, in cross-examination, why she was writing in Child D's chart. Letby said she "could not comment" if she had been in room 1 throughout. The timing on the neonatal schedule, shown to the court, says the note was made at the time of Child D's collapse. Mr Johnson says an observation reading for Child D is timed 1.15am on June 22, written by Caroline Oakley. Those details were "told to her by the girls". Mr Johnson asks who 'of the girls' would have provided those readings. Mr Johnson says Letby did not want the paperwork to attach her to the case of Child D, and that was why she minimised her involvement in police interview. A blood gas chart for Child D at 1.14am is not signed. Letby, in cross-examination, said: "I don't know" when asked if it was in her writing. Letby accepted the elevated '14' on '0114' is in her style of writing. Letby said the lack of a signature was an "error", and said the following entry was also unsigned, and happens "from time to time". Mr Johnson says it's the timing of this absent signature which is "the power of circumstantial evidence".
Mr Johnson says Letby gave an IV infusion to Child D 5 minutes before the baby collapsed. It was signed for by her and Caroline Oakley. Ms Oakley said she couldn't explain the signature as she was on her break. She described the rash on Child D as something she had not seen before in her 20+ years of working with neonates. She described it as: "a deep red brown - different from mottling, different to what I had seen before". Dr Emily Thomas said in agreed evidence that Child D came out in a rash, which faded after treatment. Mr Johnson says the description she provided was "remarkably similar" to that provided by others, but wasn't challenged on it. Dr Brunton said Child D had "developed a rash". In his notes: 'Nurses noted that became extremely mottled +++ 'Also noted to have tracking lesions - dark brown/black across trunk.' Mr Johnson says this explains "I don't remember". He says if Letby had remembered Child D, she would also have to admit it was either her or somebody else in the room with her that gave this description to Dr Brunton. Letby had said, several times: "I don't remember that being discussed at the time." Mr Johnson says it was recorded here.
Dr Brunton said the collapse was " a completely unusual situation I had never seen before", with changes in the skin colour which could not be explained. Dr Elizabeth Newby described two 'bruised areas' on Child D's abdomen, 'like evolving purpura'.
Mr Johnson says the similar descriptions given by the doctors and nurses of the discolouration because the causes of the collapses was the same. Child D's discolouration had gone by 2.35am. Dr Brunton noted the skin discolouration "reappeared" at the second collapse. Mr Johnson: "What are the chances?" At 3.45am, Child D had a third and fatal collapse. Dr Thomas said she was with another baby, when he was alerted by a nurse 'with brown hair' and believed she was the designated nurse for Child D, and believed she had also been the designated nurse for Child A. Dr Thomas said Letby had said: "This is my second baby this has happened to me," and was upset. Mr Johnson says even here, Letby was associating what happened to Child D with what happened to Child A. Dr Brunton had "never seen a baby behave like this" prior or since. Dr Brunton was "struck" by Child D's rapid collapses and recoveries. Mr Johnson says Dr Brunton say, because he didn't know, that the collapses were similar to other children in this case. Mr Johnson says 'it tells you' Child D was sabotaged, and Letby was lying when she said she didn't remember.
Mr Johnson says Letby's interviews were unremarkable, but said of babies' deaths in evidence: "You don't forget things like that, they stay with you. Mr Johnson asks if this is the same case as someone who doesn't remember a baby collapsing three times and dying. He asks if Letby was trying to gain sympathy from the jury. Mr Johnson said Letby said in police interview if the events of Child D upset her: "I honestly can't remember"
Letby said in a message to a colleague on June 22, 2015: '[Child D] collapsed & had full resus. So upsetting for everyone. Parents absolutely distraught, dad screaming'. Mr Johnson says this was on Father's Day. He says Letby, from the text messages, did remember Child D. Prof Owen Arthurs said, in evidence, the minor infection in Child D was improving. He added one of the lines of gas, in the post-mortem examination, was "highly unusual" and had similar findings in Child A and Child O. He said he had 'never seen so much air' [in the great vessels]. Another medical expert, Dr Marnerides, had ruled out sepsis, and concluded Child D was killed by an air embolus. Dr Sandie Bohin said Child D was recovering from pneumonia, and the speed of the collapse was "very unusual and not indicative of infection". She concluded the cause of the collapse was air embolus. Child D's distress and rash description supported her opinion. She rejected the evidence that taking Child D off CPAP caused her death. Dr Dewi Evans viewed the case as one where the air embolus was the "only viable cause" of death. He was cross-examined about the blood gas record for Child D. Mr Johnson says Dr Bohin had given evidence to say that blood gas record was "satisfactory".
The trial is now resuming after its lunch break. Mr Johnson says he is turning to the case of Child G, on three counts of attempted murder.
Child G was the most premature of all the babies, with the lowest birth weight. He says Child G's mother's name is not the easiest to spell - the reason why he mentions that is clear to the jury. Child G had the "grossest misfortune to meet Lucy Letby" when she was transferred to the Countess of Chester Hospital, Mr Johnson says. He refers to Child G's 100th day of life on September 7, 2015, when a banner was up, and a cake had been baked to mark the occasion. He says on that day, she suffered a severe brain injury which has left her dependent on her parents.
Mr Johnson says all the experts agree Child G was in a "very satisfactory position" prior to her collapse. He says "odd coincidences to happen in life - but do you believe in coincidences in this?" Mr Johnson says Letby knew Child G's 100th day, and the premature baby's due date. Mr Johnson says Dr Evans had described Child G's vomit on September 7 was "extraordinary" and nurses had described the extent of the vomit was something they had never seen before. He says there are two choices - that Child G was sabotaged by being overfed, or having tolerated escalating amounts of milk, she then vomited with unprecedented force due to an infection which no staff had ever seen present itself before or since. "Some people say there is a first time for everything" Mr Johnson says, but adds this is "no naturally occurring event" and has been seen in several other babies' cases including Child C, Child J, Child K and Child N.
Mr Johnson says nursing notes showed a 'normal baby, feeding properly' in the hours before Child G's vomit on September 7. At 8pm on September 6, nursing colleagues said Child G was stable and well. A staffing rota for the night is shown for September 6-7 - "a quiet night", and Child G received a full feed from a bottle at 11pm and was "thriving". Mr Johnson says "little babies don't take full feeds from bottles unless they are happy little babies." He says Letby has "massaged the times", as she had done in several other cases. Mr Johnson says the prosecution suggest the vomit was at 2.30am, not 2.15am. Nursing colleague Ailsa Simpson initially said she was with Letby when Child G projectile vomited at 2.15am, and if that was true, Letby could not have been the cause of it. In a subsequent interview, she said she didn't know where the other nurses were. Mr Johnson says Letby's nursing note on September 7 includes: Care given from 0200 to present. [Child G] had large projectile milky vomit at 0215.' Mr Johnson says it's an interesting line that Letby had given care from 2am. He says this note is written six-and-a-half hours later, and the jury should take that with care, especially with Letby, as she "habitually mis-recorded" information. Mr Johnson says Child G wouldn't have tolerated a 45ml milk feed under gravity if the stomach was already containing undigested milk. He says Ailsa Simpson's original account does not correspond with the neonatal review, as Ailsa Simpson fed a different child in room 1 at 2.20am [Child G being in room 2]. That child was "demanding food", Mr Johnson says, and that takes time. Medication was co-signed for Child G at 1.42am by Ailsa Simpson, and another child at 2.13am. Mr Johnson says all this material shows she was busy at this time, and "cannot be accurate" with the 2.15am timing of the event. Dr Alison Ventress recorded Child G was 'called to r/v [Child G] urgently at 2.35am...[Child G] had very large projectile vomit (reaching chair next to cot and canopy)'. Mr Johnson says Dr Ventress was called urgently as Child G suffered a catastrophic brain injury, and the doctor arrived within minutes as they would not wait around. Mr Johnson says Ailsa Simpson was distracted in room 1, her colleague had gone on a break, and that gave Letby "the perfect time" to sabotage Child G, and misrepresent it in the notes.
Mr Johnson says the longer the gap between the feed and vomit, the less likely the feed would be the reason for the vomit. Dr Ventress said Child G's abdomen appeared "purple and distended" upon her return to see Child G after the vomit. A "large watery stool passed", after which Child G's abdomen was "slightly better". Mr Johnson says this was not the situation earlier, when she had taken on a feed by a nursing colleague. Mr Johnson says Child G was force-fed milk and air, injecting by using the plunger in the syringe. He says Letby "took advantage" of taking on Child G's care. Dr Ventress was later called out of theatre to intubate Child G, and noted blood-stained secretions coming from the vocal cords. Dr Stephen Brearey, asked about Child G's deteriorations on the ventilator, said: "I can't explain that - it's unusual for babies to desaturate on ventilators...the fact that Dr Ventress was getting chest movement [from Child G] was perplexing, and I cannot think of a natural cause of why that would happen." Mr Johnson say the truth was it was "an unnatural process" by Letby.
Mr Johnson asks what would cause Child G's throat to bleed, as similar to the cases of child E, Child N, Child O and Child H. He says it was sabotage by Letby. NJ: "It is a signature of many of her attacks on these babies".
After 6am on September 7, 100ml of air/fluid was aspirated from Child G. Mr Johnson says the only source of that was from Lucy Letby, who had caused the baby a "devastating brain injury". After that, Child G's saturation levels improved and she did not have issues with her stomach. Mr Johnson says what was vomited and aspirated was nothing to do with infection. Mr Johnson says Dr Sandie Bohin had been "very stable" prior to the collapse. The pH reading showed Child G's stomach was empty and discounted the possibility of there being undigested milk. If there had been an infection, there would have been 'subtle markers' present in observations. She rejected the suggestion by Letby in interview that Child G swallowed air when vomiting. Dr Bohin said Child G was "extraordinarily premature" and an observation of 'blood-stained secretions was down to the use of a tube on June 14, 2015. Letby, in interview, remembered her colleague was on a break and would not have left Child G alone. Letby suggested the vomit "had not left the cot". Mr Johnson says this is at odds with agreed evidence and and a note made at the time by Dr Ventress. Letby said she had "seen [Child G] vomiting."
Upon Child G's return to the Countess of Chester Hospital [having been transferred to Arrowe Park Hospital for several days], she "had the misfortune", Mr Johnson says, to be in Letby's care on September 21, her due date.
On September 21, Letby was designated nurse for Child G and two other babies in room 4. Letby said in a nursing note that at 10.15am, Child G 'produced two large projectile milky vomits...' Mr Johnson says Child G had been sabotaged again by Letby, shortly after recording 'entirely normal' observations. Child G's abdomen was noted to be 'more distended than usual'. Mr Johnson says Letby "misrepresented" what the situation was when she texted a nursing colleague that night, saying Child G 'looked rubbish when I took over this morning' and she had inherited a problem, which Mr Johnson says "was untrue". Mr Johnson says if Child G did look so bad, she would have referred her to a doctor first before feeding. "It's a lie to divert the suspicion," Mr Johnson adds.
Letby was involved in a text message conversation for the 'looked rubbish...this morning'. Letby added : 'I personally felt it was a big jump considering how sick she was just a week ago. Being in 4 is bad enough & then having NN [nursery nurses] that just don't always know... "Mum said she hasn't been herself for a couple of days" Mr Johnson says it fits Letby's narrative that nursery nurses are 'bad'. He says the "false narrative" "could not be clearer" as Letby also recorded Child G's poor condition in nursing notes written retrospectively.
The trial is now resuming after a short break. Mr Johnson moves to the second incident on September 21, 2015 for Child G. He says this is when Child G was having a cannula inserted behind a screen at about 3.30pm, and there were problems with insertion. Child G was put on to a trolley to carry out the procedure. A nursing colleague said, in evidence, she had contacted police one month prior, to say Letby had not switched off the monitor in this event, and one of the doctors had apologised to her for not putting the monitor back on. Dr Gibbs said if the nursing colleague said it was true, he accepted it was true. Dr David Harkness said the monitor was "definitely not turned off" said they were "so keen to get fluids going again" for Child G, as it had been 6 hours since she last had fluids, and Child G was 'not just left alone'. In cross-examination, it was put to him he had previously said collapses among neonates of Child G's age was quite common. He replied that was his experience in Chester, but his experience in other places since had showed that was not the case, and now refuted the suggestion. Mr Johnson says the nurse was out of the room for Child G, and Letby was in room 4 with Child G. The nursing colleague said Child G was back in the cot, after hearing Lucy Letby shouting for help. Letby had said she moved Child G from the trolley to the cot and Neopuffed her. Mr Johnson says it is not a credible suggestion. Dr Gibbs had said "whatever the position was with the monitor", he would have made sure Child G was stable when he left her, post-cannulation, and would have told someone he had finished with the cannulation. Mr Johnson says if the nursing colleague wasn't in the room, the other person who would have been contacted would have been Letby. Mr Johnson says this is another occasion where Letby had attempted to kill Child G. The nursing colleague said she could not remember a conversation about being cross that Child G had been left alone on a trolley with the monitor off, or that a Datix form should be filled in for that event.
Dr Dewi Evans said the first September 21 incident was all indicative that Child g had been overfed with "potentially catastrophic consequences". Dr Sandie Bohin said it was "basic arithmetic" - two large milky vomits, plus 30mls aspirate, meant Child G was fed much more than she should have been.
Mr Johnson turns to the case of Child H. He refers to a form from the Countess of Chester Hospital to Arrowe Park for transfer, shown to the court, of Child H's deterioration and the chest drains used. The form ends: 'The acute episodes with desaturations and bradycardias do not seem to be directly related to the respiratory problems' Child H's mother said Child H was "like a completely different baby at Arrowe Park". Mr Johnson says Child H had respiratory distress syndrome, which is "not unusual" for a neonatal baby, and was not particularly premature. There were two events where Child H desaturated which were unusual. Cross-examination of Letby said staffing levels did not contribute to the collapse of Child H. She "always had one-to-one nursing care" and the delay in issuing surfactant did not have anything to do with the collapse, Mr Johnson says. Mr Johnson says for the two counts, the tube was not blocked and staff could hear air going in and out of Child H's lungs.
Professor Arthurs, a professor in radiology, "made a significant contribution" to the debate on chest drains, Mr Johnson said. He said chest drains do not normally cause bradycardia or desaturations, and chest drain positions are not examined in detail as they do not cause problems. He said the interpretation of a chest drain position was his area of expertise. He said in his opinion, the chest drains were in the space they were supposed to be. Mr Johnson says the jury don't have to accept his evidence, but there is no evidence to contradict it. Mr Johnson says the first significant collapse happened on September 25-26, 2015. Letby was the designated nurse in room 1. No other babies were in room 1. The father's statement was read out to court. He said he and his wife had spent time in the neonatal unit until September 25. He said he had been there until 'about midnight', had come back to the house, and was awoken by a call needing to go back to the hospital. He said when he got back, "I definitely remember Lucy being there, doing the chest massaging. It was explained to us [Child H] had a collapse. "[Child H] was a very strange colour - I remember the mottling was running out of her skin towards her fingers." Letby, in nursing notes: '...2330 bradycardia and desaturation requiring Neopuff in 100% to recover. 10ml ai[r] aspirated from chest drain by Reg Ventress. Following poor blood gas and 100% oxygen requirement consultant Gibbs attended the unit and inserted a 3rd chest drain' Mr Johnson says 2330 is the time put in by Letby. Dr Ventress recorded '2350 Several episodes of desaturation in past two hours...' Mr Johnson said Letby had told her of 'several' episodes - "where has that come from?" Dr Ventress: '1st one after gas taken (good gas)...'. Mr Johnson says Letby wrote on an intensive care chart a desaturation to 52% at 2210, which does not appear "at all" in the notes. Mr Johnson says there is nothing in the observation charts to suggest there is anything wrong during this period. He says the parent has an uneventful night before he left. The doctor is given a long list of problems, but there is nothing in the nursing record to what Letby told Dr Ventress. Mr Johnson says this was getting other people to record problems for a child when none existed, as was the case for Child E. NJ: "[Child E] hadn't got a problem, until Lucy Letby caused a problem." Dr Ventress had recorded a second chest drain was "almost out". Mr Johnson says moving chest drains was a "very effective way" of sabotaging a child, as would moving an ET Tube.
Mr Johnson says Child H was in "very, very poor shape", and after being in arrest for 22 minutes, the father noted the mottling. Dr Gibbs ruled out all natural causes for Child H. He ruled out involvement of the chest drains. Mr Johnson says the evidence of Prof Arthurs 'puts this all to bed anyway'. For the second event for Child H, Dr Matthew Neame believed Letby was the designated nurse for Child H on that shift, when it was nurse Shelley Tomlins. Mr Johnson says Letby had 'elbowed her colleague aside'. Letby had messaged her colleague that night: 'I've been helping Shelley so least still involved but haven't got the responsibility'. Mr Johnson says this builds Letby's 'plausible deniability'. He says "we know" Letby was supposed to be in nursery room 2, not in room 1 where Child H was. Mr Johnson says it shows the state of mind Letby was in that night, similar to the state of mind for when she killed Child C.
Mr Johnson says this was another case where a child was desaturating "to life-threatening levels" despite good air entry. The ET tube was checked by Shelley Tomlins and there was no blockage. "Mercifully, [Child H] was revived." An x-ray showed there was no issue with the pneumothorax. The father said Child H was ok in the day, then it was 'shortly after' he had gone to get some rest when he had a knock on the door to go and be with Child H at the cotside as she had deteriorated. Mr Johnson says this was "yet another opportunity" for Letby to sabotage a child.
Dr Neame recalled it was Lucy Letby who briefed him on the second collapse for Child H. He recalled he was more concerned by this second collapse. A further collapse occurred at 3.30am despite Child H having 'good air entry', and she was transferred to Arrowe Park, where she recovered quickly. Dr Evans said the pneumothorices were not the cause of the arrests. He ruled out infection as a cause of the collapses, as they were rapid and catastrophic collapses, she was on antibiotics, and a lumbar puncture proved she did not have an infection. He was "at a loss" to explain the collapse, but it was "not one of natural causes". Dr Bohin said there were delays with the surfactant. She said she could find no clinical or mechanical cause for the collapses. She said she had never known a chest drain to cause collapses, or stresses by the baby resulting in a cardiac arrest. Professor Arthurs saw "no problem" with the chest drains. Mr Johnson says the chest drains can be ruled out as a problem. He adds there was no disease or mechanical factor, and it was "undoubtedly" sabotage by Letby. He says both collapses happened "just after" Child H's parents had left, which had "parallels" with other cases, and was a "signature" of Letby's work.
Thursday 22nd June 2023
Prosecution Closing Speech - Day 4
Chester Standard Live Reporting - 22nd June 2023
The trial is now resuming. Mr Johnson says there are four children left to go through - Child I, Child J, Child N and Child Q. He first details the case of Child I.
Mr Johnson says evidence had been heard of Child I, that medics do not worry about self-correcting desaturations. Mr Johnson says having failed to kill Child G and Child H, she turned her attention to Child I, and was designated nurse for two of the four occasions in which she tried to kill the baby girl, and falsified notes along the way. Mr Johnson says it was important to note from the post-mortem evidence that Child I did not have NEC [a gastrointestinal disease].
Mr Johnson says Child I's first collapse was marked with a desaturation to the 30s and had vomited, on September 30. He says the day before, Dr Lucy Beebe had reviewed Child I. She remembered seeing Child I from memory, as the girl became unwell, was shipped out and recovered well, and came back, which she said was unusual, for her short time at the unit. Dr Beebe had said she was shocked and frustrated by Child I's death, as she felt there was something going on which they [the staff] were not aware of. Dr Beebe said the aim for Child I, after the September 29 review, was to continue feeding and growing the baby girl.
The day rota for September 30 had Letby as designated nurse for Child I and two other babies in room 3. Mr Johnson says Letby "did not like" being in room 3. The plan was to give Child I immunisations, as was the case for Child G. He says there was nothing wrong with Child I, who was receiving cares from the mother and a feed. Mr Johnson says Child I produced a small stool at the 10am feed. The 10am feeding chart note is signed by Letby. "The doctors were very happy with [Child I]," Mr Johnson says.
Dr Beebe's note is shown to the court for September 30. Mr Johnson says it is important to note the reason for the review. It was 'asked to review as reduced temperature'. Mr Johnson says Child I was taking full bottles, gaining weight, and Dr Beebe recorded that Child I was handling well. Child I, during the examination, produced a yellow, seedy stool, which indicated good gut health, he tells the court. Dr Beebe said this was not a sign of NEC. Mr Johnson says Child I was "not in distress", the abdomen was the same as yesterday, and the plan was to monitor Child I closely, raise the cot temperature, but Child I appeared clinically well. Mr Johnson asks what was going on at this stage. Child I's mother, in evidence, said Lucy Letby raised the issue with her about Child I's stomach. Mr Johnson says that was not the same reason Letby gave to Dr Beebe. NJ: "So what was going on here?"
Mr Johnson says no concern was expressed to medical staff about Child I's abdomen by Letby. "Why was Lucy Letby expressing concern to [Child I's mother] about the abdomen? Why did Lucy Letby not raise the issue with Dr Beebe?" Mr Johnson says Letby was gaslighting the mother by suggesting a problem with Child I that didn't exist, until she caused the problem.
Mr Johnson says "everything was unremarkable" for Child I until 1pm when she was asleep, and fed via a NGT. The mother said she had gone to meet the family in the canteen at this time. The feed chart shows a 35ml feed for Child I, which Mr Johnson says would take some time - "about 15 minutes", taking until 1.15pm. He says the nursing notes are accurate as they are time-stamped by the computer automatically. The note is written between 1.36pm-1.48pm - it was "at most" 20 minutes after the feed ended. Mr Johnson says the details of the feed and review recorded are not correct. He says the addendum, of a '1500' 'Drs' examination of Child I, is "a complete fabrication". A male doctor's note records examining Child I at 4.30pm. Mr Johnson asks who these doctors were who examined Child I at 3pm. He adds the '3pm note' contains: '[Child I] appeared mottled in colour with distended abdomen and more prominent veins.' Mr Johnson says there is no corresponding doctor's note for this examination of 'mottling'. Letby's note: 'Full monitoring recommenced'. An observation note records this was done from 3pm. Mr Johnson says Dr Beebe had advised it at 11.40am. He asks why did Letby only recommence full monitoring after Child I's mother had left the unit. Mr Johnson says Letby is transposing events, including a note of a yellow seedy stool, from 11.40am to 3pm to an examination - "which never actually happened".
Mr Johnson says it is a "very calculated way" of giving the impression a child who had no problem at all, "had a problem". Child I's mother had a routine for each day, visiting Child I at regular times, and the father would come in from after 5pm. Mr Johnson said the time between 3pm and 5pm was "her window of opportunity" to attack Child I. NJ: "What are the chances of these things happening at precisely this point?" Letby had written: 'Mummy present when reviewed by Drs. Had left unit when [Child I] had large vomit and transferred to nursery 1.' Mr Johnson says Letby had tried to give the impression the Neopuff caused the inflated stomach for Child I. He says "remarkably", Child I improved, and there were 'minimal aspirates'. "Yet another miraculous recovery...all good once Lucy Letby had left." Medical expert Dr Dewi Evans ruled out infection and said the only explanation was a dose of air administered through the NG Tube. Dr Sandie Bohin agreed, and the effect would have been to splint the diaphragm. She discounted the possibility of NEC. Professor Owen Arthurs said the stomach and almost all of the gut had been distended. Mr Johnson says that was from administered air.
The second incident for Child I, on October 13, 2015 at 3.20am, is now detailed by Mr Johnson - the 'see in the dark' incident, he calls it. He says Child I had been progressing well.
The first part of the night shift had Child I being fed normally. Mr Johnson says the second event was much more serious than the first. Before it, Child I had been in a good clinical condition, Mr Johnson says. He says it was expected she was coming up for discharge from the hospital in a couple of weeks. Letby was the designated nurse for a baby in room 1. Nurse Ashleigh Hudson was the designated nurse for Child G, Child I and one other baby in room 2. She left room 2 to tend to another baby in room 1, assisting colleague Laura Eagles, and asked a colleague to monitor Child I - either Caroline Oakley or Lucy Letby. Caroline Oakley had no recollection of being called. Ms Hudson said she had been in room 1, and some milk needed defrosting for Child I's feed, and when she got back, there were no adults in the room. She started to prepare the milk, with her back to Child I. The next thing she remembered was Lucy Letby in the doorway, who pointed out that Child I 'looked pale' - she was 'about 5ft-6ft away' from Child I. She said something along the lines of 'Don't you think [Child I] looks pale?" Ms Hudson said the light in room 2 was low, and the lights were on in the corridor outside room 2. Mr Johnson reminds the jury what Lucy Letby said about this in interview.
Mr Johnson refers to Letby's 2019 police interview, in which she said room 2's light was off, and there was 'an element of light coming from the doorway', and Child I was by the window. Ashleigh Hudson said Child I had a blanket over her, and a 'tent structure' keeping her secure. She said she could not see Child I due to the canopy and the lighting. Mr Johnson says Letby did not have a better view. Ms Hudson said she switched on the light and looked at Child I, who was 'gasping', 'incredibly pale', and in a 'very bad way'. Ms Hudson initially thought the deterioration was so rapid she thought she was too late to save her. She said you "cannot see" a child from the position Lucy Letby was in. Mr Johnson says we have a "head-on credibility conflict", of two accounts who "don't live in the same world". Mr Johnson says in cross-examination, Letby was asked about looking from a brightly lit corridor into a dark room would improve her ability to see. He says her first response was "I don't know". NJ: "She 'conceded' she would not have been able to see, yet she persisted that she could see [Child I]. NJ: "We had a break, we came back, and I asked Lucy what she had said in interview... He says Letby had said "Maybe I spotted something Ashleigh couldn't spot." Mr Johnson had asked Letby: "You don't have better eyesight than Ashleigh, do you?" LL: "No." NJ: "The question is, how would you be able to spot the colouring [of Child I better than Ashleigh Hudson from the same point of view]?" LL: "I had more experience so I knew what I was looking for/at." Mr Johnson adds: "You will remember the way she corrected herself." He says there was a very long pause. He added at the time: "Your answer, you explain it." He said Letby was "finding it difficult to concentrate on all the dates". Mr Johnson said there was nothing about the dates in this context. He says did Letby make an innocent mistake, or did something else slip out, under the pressure of the witness box? He says Letby caused the problem for Child I. He says Child I recovered well.
Mr Johnson says Letby had timed her note, having seen Ashleigh Hudson's nursing note first, so it appeared she saw Child I first. Mr Johnson says it is another case of 'plausible deniability'. Professor Arthurs said Child I's large bowel was distended, and the NG Tube was in the curled up in the oesophagus rather than the stomach. Dr Evans said the only explanation was air administered to Child I via the NG Tube. Mr Johnson says Dr Bohin explained Child I was sabotaged by air administered via the NG Tube and via and IV line. Dr Anne Boothroyd's x-ray report on September 30 recorded: 'There is splinting of the diaphragm due to bowel distention'.
For the third event for Child I, Dr Ravi Jayaram said there were 'no clinical concerns' for Child I before the night of October 13-14. Mr Johnson says evidence was heard to say Child I was "stable". This was the second time Letby was the designated nurse. Mr Johnson says this was the second time she had the opportunity to falsify notes. Dr Matthew Neame's 5.55am note is shown to the court for October 14. Mr Johnson says this is not a retrospectively written note, as it includes a note of a prescription which is timestamped at 5.56am, and an urgent x-ray is timed at 6.05am. He says Letby's addendum note, made at 8.43am, after Child I had desaturated: 'At 0500 abdomen noted to be more distended and firmer in appearance with area of discolouration spreading on right hand side, Veins more prominent' Mr Johnson asks why would Lucy Letby do this? He says to bear in mind what happened the previous night, if these symptoms were shown, then the doctor would be called urgently. He says the absence of a doctor called shows there was no problem at 5am.
Mr Johnson says, from the paper trail, if anyone 'puts two and two together' and thinks there is a problem with Lucy Letby, they are "thrown off the scent". Dr Neame said the mottling was "unusual", which was why he recorded. NJ: "How many times have we heard that in this case?" Mr Johnson says the abdomen was distended. Dr Andreas Marnerides had excluded NEC. Mr Johnson says the only possibility is pushing air in down the NG Tube. Dr Neame said Child I looked uncomfortable when examined and "grimaced". He noted the abdominal distention. Prof Arthurs said, of the x-ray image, the stomach was 'markedly dilated', and the small bowel and the large bowel were also dilated, with 'no symptoms of NEC'. Another image at 8.03am had the stomach decompressed, and a third image the following day showed 'no problems at all'. Dr Neame recorded a further desaturation for Child I at 7am, and the ET Tube was reintubated. It was noted there was 'good air entry' for Child I, but - as Mr Johnson says, in so many other cases for babies in this trial - Child I was desaturating.
Child I had further desaturations on October 14-15, which Mr Johnson said were 'explicable' as there were secretions in the NG Tube. Child I had a 'miraculous recovery' after being transferred to Arrowe Park, and improved, until coming into the "misfortune" of contact with Lucy Letby, he adds. Dr Evans thought Child I's stomach had been injected with air, and air injected into the intravenous system. There was an "astonishing amount of air" in Child I's stomach. Dr Bohin concluded Child I had air administered.
The trial is now resuming after a short break. Mr Johnson turns to the fourth and final event for Child I, on October 22-23, 2015, in which Child I died.
Mr Johnson says Ashleigh Hudson had given evidence to say Child I was "very easy to settle", and although Child I was in nursery room 1, that was as a precaution given her history of episodes. Child I was self-ventilating in air and her saturations "optimal", and she "looked very well", and "pink, well-perfused" and a "soft, non-distended abdomen". Caroline Oakley said in a statement Child I's abdomen was "fine" and "soft, non-distended". Mr Johnson says that is the background to Child I when Lucy Letby came on shift that night.
Letby was designated nurse for a baby in room 2 and a baby in room 3. Ashleigh Hudson was designated nurse for Child I and another baby. Child I was in a "virtually perfect" clinical scenario, Mr Johnson says. He says Letby "got herself involved". Child I gave a 'cry that had not been heard before' - 'loud and relentless', according to Ashleigh Hudson, who interpreted it as "distress". When she was repositioned on her tummy at about midnight, Child I stopped breathing. Resuscitation efforts began and Child I then began to fight the ventilator. Dr John Gibbs was told Child I had had an abnormal cry. He was 'perplexed' at Child I's rapid deterioration and recovery, which would not show a sign of infection. Mr Johnson says Letby falsified paperwork for one of her designated babies at this time - the baby to be transferred to Stoke. Letby recorded a note at 10.50-10.52pm note of a 10% glucose infusion for the 'Stoke baby'. The infusion note is written as starting at '2300', and that writing is changed to '2400'. Mr Johnson says it was changed to give Letby an "alibi" for midnight. Mr Johnson says further times are overwritten/changed on Child I's infusion chart - from 12.15am to 12.25am, and one to a time at 1.25am, which Mr Johnson says puts it out of sequence between '1.28am' and '1.48am' on the chart.
Ashleigh Hudson said she was alerted to Child I at 1.06am by either the alarm going off or Child I crying. She said, in room 1, Letby was already there at Child I's cotside and "had her hands in the incubator". Mr Johnson says Letby had sabotaged Child I, and caused Child I to cry. Mr Johnson says Letby 'put Ashleigh Hudson off' by saying: "She just needs to settle". 'Air++' was aspirated from Child I. Mr Johnson asks how that could have got there other than being forced in by Lucy Letby. Dr Rachel Chang could see air entry and chest movement on Child I, but Child I wasn't recovering. She said Child I's death was "inexplicable". Dr John Gibbs noted mottling on Child I. He said he "could not understand" why Child I had died and referred the case to the coroner. The grieving parents agreed to bathe Child I. Mr Johnson said despite having two designated babies to care for, and Child I not being her designated baby, Letby met the parents. The mother said: "Lucy came back in. She was smiling and kept going on about how she was present at [Child I's] first bath and how much she [Child I] had loved it." "I wish she had just sopped talking. Eventually I think she realised and stopped. It wasn't what we wanted to hear then."
Dr Evans says this was "another" case, in Child I, receiving air administered. He thought the nature of the collapse, the crying, the prolonged resuscitation, and the purple and white discolouration, were all symptoms of air embolus. There was no account of natural disease. Dr Bohin said the cause of death was air embolus - from the unexpected catastrophic collapse, Child I being unsettled and agitated, the 'extremely unusual' crying meaning Child I was in excruciating pain. In cross-examination, Dr Bohin was asked if she had a coherent explanation for an air embolus. Mr Johnson said Dr Bohin's answer, without hesitation, lasted for about 10 minutes. She was asked about Child I's poor weight gain, and Dr Bohin said that did not make her more likely to have a cardiac arrest [as Child I had]. Prof Arthurs said it was 'unusual' to see the amount of dilation in Child I's stomach. He excluded CPAP belly as a cause. He said it was "reasonable to infer" air administered. Dr Marnerides said at the time of Child I's death, she had no acute illnesses or abnormalities in the bowel, other than presence of air. The presence of gas had "no pathological cause". He said the collapses were air administered from the NG Tube. Mr Johnson says Child I's case is a "stark one". He says Letby made repeated efforts to kill Child I, and falsified notes both for Child I and another baby. She 'gave herself away' in the event with Ashleigh Hudson. "Lucy Letby's behaviour in the aftermath [of Child I's death] was bizarre and inappropriate. She revelled in what she had done." "Her voyeuristic tendencies caused her to look up [Child I's mother] on Facebook." "Having killed her [Child I], she wrote a condolence card. It was still on her phone when it was seized by the police."
Mr Johnson details the case of Child J. He says when Letby was giving evidence in this case, she said band 4 nurses [nursery nurses] cannot do intensive care or high dependency babies, or handling of stomas. Letby said the unit was very busy as an explanation why a band 4 nurse was caring for Child J. Mr Johnson says the implication of that exchange was to give that Child J received incompetent care, and staffing levels were compromised. Letby had messaged a colleague on November 19, 2015: "It's shocking really that they are willing to take on the responsibility for things that they have no training or experience etc on. Don't think they appreciate the potential difficulties" Mr Johnson says the jury will remember witnesses had been cross-examined about nursing guidelines. He says the part that was never quoted was the bit about stomas. The care, shown to the court, says special care day nurses can include care of a stoma. Mr Johnson says that whole evidence "was designed to mislead you". "It's the same type of behaviour that Lucy Letby engaged in with her colleagues."
Mr Johnson says Child J had no respiratory difficulties and was being bottle fed, and did not need respiratory support, and was in room 4. Nurse Nicola Dennison said Child J was 'getting ready to go home' with a stoma by November 26, 2015. She wrote in notes that Child J was 'stable'. Child J's mother left at the end of the day, intending to return at 8am the following day, but received an emergency call overnight. Letby was in room 3, designated nurse for two babies that night shift. Nicola Dennison was the designated nurse for Child J and one other baby in room 4.
Child J desaturated at 4.40am on November 27. Mary Griffiths was working in room 2. She said in evidence Child J was a 'joy to look after', and described the first desaturation, which she and Nicola Dennison dealed with. The desaturation was "alarmingly low". Ms Dennison said, after cross-examination, Child J collapsed after her feed. Dr Kalyilil Verghese recorded the shift was busy. Twins had been admitted to room 1 at 6.10am. He said he reviewed Child J once, and all information was given to him by nursing staff. He noted there had been 'two profound desaturations', timed at 5.15am. Child J was moved to nursery 2 when the designated nurse was Mary Griffith. Mr Johnson says Letby was then involved in care of babies in room 2, despite her designated babies being in room 3.
Letby had said, in a text, the unit was 'closed' trying to get someone in. At 6.49am she messaged 'It's all a bit t**s up' Mr Johnson says resources had been diverted to room 1, and this was the "perfect opportunity" for Letby to attack Child J. At 6.56am, Child J collapsed.
Mr Johnson says Child J's saturations dropped, as did Child J's heart rate. Mary Griffith noted '[Child J's] monitor went off at 0650 myself and L Letby attended. Found baby with pale hands and baby very rigid. Sats went to 7 and heart rate to 68. [Child J] Neopuffed with little improvement....Dr Gibbs on unit and called to help. Neopuff continued for 16 mins until sats improved.' Mr Johnson says this was a serious enough incident for the consultant to be called. A glucose bolus was started at 7.20am, which Mr Johnson says was administered by Letby. At 7.40am, according to nursing notes, Child J desaturated again, and her fists were clenched, her eyes were rolling to the left, and Letby got involved again. Dr Gibbs recorded at 7.35am: 'Two seizures' - he said he remembered Mary Griffith and Lucy Letby were there when he arrived. A seizure was 'reasonably long', about '10 minutes'. Mr Johnson says prior to these events, Child J had never had a seizure, and she had not had one since. She "recovered very well" afterwards. He adds blood tests were normal and showed no signs of infection, and a brain scan showed no abnormality, nor in an x-ray. Dr Gibbs said an oxygen drop was the reason for the seizure, but could not find a reason for the oxygen drop. Dr Stephen Brearey said there "was no explanation" for the deteriorations.
Dr Evans said there was no marker of infection for Child J. He said if there had been, the recovery would not have been so quick. He agreed there had been a lack of oxygen, and it had not been an epileptic seizure. Dr Bohin said babies who are ready to go home do not have collapses which require prolonged resuscitation and a quick recovery. Mr Johnson says the cause of collapses "bear all the hallmarks" of an attack by Lucy Letby. He said Child J was "prospering" prior to the attacks, and the attack happened while the unit was distracted by two emergency admissions. He says at that time, when it was 'all hands to the pump', Letby was on her phone. He says Letby stopped texting seven minutes before Child J's collapse. Letby's suggestion that she had little memory of the event is "not realistic", Mr Johnson says, as that night was punctuated by two emergency admissions to the unit. He says Letby "was running with the I don't remember line to avoid answering questions." He says Letby searched for Child J's parents, which is 'inexplicable', other than through an 'unnatural interest in them'.
Mr Johnson moves to the case of Child N. He says Child N was sabotaged by Lucy Letby as he was getting ready to go home. The first incident was "characteristic of Lucy Letby's handiwork", Mr Johnson says. Dr Christopher Booth had gone on a break. Mr Johnson suggests Letby was "in her least favourite room" that day, in nursery 4, with 'only' two babies, and had time on her hands by texting about Melanie Taylor's shortcomings and a male doctor. He says that includes the 'go commando' comment, which he says Letby lied about not knowing its meaning. NJ: "If she's not even prepared to tell you the truth on something so trivial, what is she prepared to tell you the truth about?"
Mr Johnson says Letby's interviews are "very revealing" in relation to the texts in the case of Child N. He refers to the 2020 police interview. Letby was asked if she knew Child N had haemophilia. She replied she didn't know. Mr Johnson says that was a lie, as there was a handover sheet in the 'Morrisons bag' at her home which documented Child N had haemophilia. On June 2, 2016, Letby was recorded caring for two babies in room 4, including giving a feed to one of the babies, a 50ml feed to a baby who was asleep. Mr Johnson says it would take 15-20 minutes. He says the 2030 time could mean any time between 2015-2045. Mr Johnson says the 'keypad on Lucy Letby's phone must have been hot' as Letby was texting constantly at this time. He says it is accepted people do text at work, but giving an NG Tube feed is a two-handed process, and "you can't do that if you're texting at the same time". He says there are 41 text messages in the conversation, and that "cannot be done" if you are giving, "in the proper way", an NG Tube feed. Mr Johnson says Letby was asked about this, how it could be done: LL: "You can't." Mr Johnson had told Letby there was one method of administering a feed quickly. Letby added: "You think I pushed it in?" NJ: "That's what you were doing, wasn't it? LL: "No."
Designated nurse Christopher Booth said, for the incident, he went for a break around 1am on June 3. Sophie Ellis was giving a feed at the time and had only a vague memory of child N, and had a number of designated babies that night. Melanie Taylor was making an entry on a fluid balance chart and had no memory of Child N. Valerie Thomas was a nursery nurse who would not have been in room 1. Mr Johnson says the process of elimination was it was Lucy Letby who was in room 1, as she wasn't recorded doing anything at that time. Dr Jennifer Loughnane noted Child N was 'unsettled' and desaturations had gone to 40%, and he was 'dusky and mottled'. He was "screaming". Mr Johnson says Dr Loughnane sat back in the witness box when reading the word 'screaming'. Mr Johnson says he asked Letby if she remembered Dr Loughnane doing that, and she said she did. Dr Evans said the 30-min crying was unusual, as was the speed of decline. He could think of no naturally occurring or innocent cause. Dr Bohin said the desaturation was 'life-threatening', and there was 'nothing to suggest it was an innocent event', and there 'must have been an inflicted painful stimulus' to cause a life-threatening collapse. Mr Johnson says that same kind of injury was inflicted by Letby on Child O, 20 days later, causing a liver injury. He says this attack happened on a baby who was perfectly well just after the designated nurse had gone on a break.
The trial is now resuming after its lunch break. Mr Johnson is continuing the case of Child N, referring to events on June 15, 2016.
He says the day before, on June 14, Letby was Child N's designated nurse. It was planned for Child N to go home that week. On June 14, notes are shown showing Child N had a 45ml feed at 7.40am. At 8.17am, Letby "complained" she had had to feed Child N - she messaged: 'bottle not done'. Mr Johnson says the 45ml feed took until about 8.15am. Letby had noted Child N was almost 'ready for home'. Child N's mother fed Child Child N at 11.50am. Mr Johnson says Letby noted at 2.20pm: 'mummy visiting this morning, carried out cares and feed...aware that once jaundice treatment discontinued infant will be ready for home...' Mr Johnson says Letby did something to destabilise Child N at the end of her day shift to give the impression of an underlying problem. Jennifer Jones-Key reported that, in the night, Child N was "unsettled". She wrote in nursing notes: "At start of shift, baby nursed in incubator with eye protection in situ...baby very unsettled early part of night." Mr Johnson asks what had happened to unsettle Child N that night. He says it is similar to the case of Child P, just over a week later. Child N started to desaturate at 1am, looking mottled, and it was escalated to Belinda Simcock and Kathryn Percival-Ward. A male doctor reviewed Child N and noted he looked normal. Child N had a number of desaturations and the male reviewing doctor believed it was the beginning of an infection, so ran a test for it. The outcome showed there was no infection, Mr Johnson says. A repeat blood gas test had "reassuring" results. The male doctor said there was no NG Tube in place, and Child N was nil by mouth. A colleague texted Letby at 5.25am: "Baby [N] screened, looks like s**t". Letby almost immediately responded: "Really?!" Mr Johnson says that is the reason Letby went straight to Child N when she went in early. "She saw an opportunity."
Swipe data showed Letby came in "extra early" at 7.12am. Mr Johnson said as soon as she entered, she texted the male doctor: 'I've escaped being in 1, back in 3'. Moments later, Child N collapsed. Mr Johnson said Jennifer Jones-Key said Child N had 'fleeting desaturations' early in the morning. An observation chart "showed no worrying signs at all" at 5am and 7am for Child N, Mr Johnson says, with 100% oxygen saturation levels. Child N had a "big desaturation" at 7.15am. He says Letby knew she had a chance to sabotage Child N as it would be busy. A colleague had texted her: '5 admissions, 1 vent'. Jennifer Jones-Key said she recalled Letby had gone over and noticed Child N was pale. She said Letby had 'just come in to say hello as they were friends'. Mr Johnson says Letby had been texting two colleagues, not Jennifer Jones-Key, the previous day, and continued the texts with a nursing colleague and a doctor colleague up to 7.12am. Mr Johnson says if she was going in to talk to her friend, she would have gone to the nursing colleague who she had been texting and was on duty. Letby, in police interview, said she had 'assumed something had happened for Child N to move because of the observations [on the chart]'. She said she had 'no independent memory' of Child N. The nursing note suggested Child N was desaturating on handover. Mr Johnson says the impression given by the note is she was inheriting the problem of the child already desaturating by the time she came on shift. He says Letby was "trying to avoid an audit trail". Child N's parents were called in urgently, and they saw him being given CPR. The parents recalled Lucy Letby being present. Mr Johnson says Letby made more "misleading notes" after this collapse for Child N.
Letby noted, in family communication at 2.10pm: 'Parents contacted by SN Butterworth during intubation. Both phones switched off and no answer on landline. message left. Call returned shortly after'. Mr Johnson says that note must refer to the 8am intubation done by a male doctor. His note of 'intubation drugs given'. Mr Johnson says it had been said the parents' statements were agreed, but now they are not. Child N's father said Lucy Letby rang him up and gave details. He added, in response to the phone call: "I didn't get the impression he was still unwell." He said a different nurse rang up 10 minutes later, telling him to go to the hospital as soon as possible, and they arrived at 9am. This was on the day Child N was due to go home. Mr Johnson says if Child N had been 'a bit unwell during the night', then he was worse now. He says the parents were told Child N was 'ok now', which was not true. He says the parents 'might just remember the call' to tell them there had been an issue with Child N. He says none of this was dealt with when Letby gave evidence to her own counsel. He says when cross-examined, Letby said she believed there was a note by Bernadette Butterworth on family communication. Mr Johnson says this chapter of evidence is "littered with irreconcilable contradiction". He asks why it was played down to the parents that Child N was unwell. He says that when Letby made the call, she would not have known Jennifer Jones-Key had already recorded Letby had been hands-on with Child N. In police interview, Letby said she "couldn't remember". Mr Johnson says the nursing note was "completely misleading", and suggested S/N Butterworth had been unable to get through to the father of Child N. He says Letby came in early to sabotage Child N. He says if someone looked at the records, it would look like Letby 'had a peripheral role' in Child N's care that day.
A subsequent examination at Alder Hey, of Child N, showed he had no abnormality with his airway. Child N was intubated. The male doctor said upon the intubation attempt, he saw blood. He couldn't see the source of the blood, and said the swelling was "unusual". He said in cross-examination: "It must have been unusual for me to see it." He said, in cross-examination, it was possible the bleed could have been caused by an implement used before the first intubation, but if that was the case, he said he would have noticed blood on the equipment. Dr Brearey said he could not think of a natural cause why Child N had collapsed. At 11.29am, Letby messaged: 'Small amounts of blood from mouth & 1ml from NG. Looks like pulmonary bleed on Xray. Given factor 8 - wait and see...' Mr Johnson says Letby was building a narrative.
When asked about the 1ml fresh blood reading on an intensive care chart at 10am in interview, Letby said she did not remember, and "I don't know what I did". Mr Johnson said if this reading is true, she would have escalated it to a doctor, as a child with haemophilia. He says if it is not true, it is still a point against Letby - why would she make a note?
Mr Johnson says the jury know it wasn't escalated as there weren't any doctor's notes.
Child N's parents came in, and left for a break to get something to eat, and at that point, Child N collapsed. "The power of circumstantial evidence," Mr Johnson says. He adds Letby 'wrote it off as an innocent coincidence'. The next event was at 2.59pm, when doctors were crash bleeped to Child N. He says it is a "repeat" of Child E, with a bleed. Dr Satyanarayana Saladi encountered a "large swelling at the end of the epiglottis" and had never seen it before in a newborn baby. The swelling 'perplexed Dr Gibbs as well'. Dr Brearey was called in by Dr Saladi to help. He said they were worried about pulmonary haemorrhage and full intubation was still required. Mr Johnson says we know now that it was not pulmonary haemorrhage. Mr Johnson says the suggestion Letby first saw blood at this point is "completely unconvincing".
Mr Johnson says the text to a doctor colleague by Letby is made at 11.29am, mentioning 'small amounts of blood from mouth & 1ml from NG.', and another note is on her family communication. Mr Johnson says Letby omitted that in interview. He says the truth is Letby made a damaging admission in interview, and "proves she sabotaged" Child N before the arrival of the doctor. 'Sorry if I was off during intubation, Bernie winds me up faffing etc , I like things to be tidy and calm...' Mr Johnson says Bernadette Butterworth was 'getting on Lucy Letby's nerves that day'. Letby recorded another 1ml of blood at 6pm. When the Alder Hey transport team arrived, a female doctor said Letby was "agitated" and approached the doctor saying "who are these people? Who are these people?" Mr Johnson says this is contradictory to what Letby said in interview, when she said she was 'relieved' the transport team arrived. He says this is all 'part of the gaslighting' on her colleagues. The female doctor felt Letby's behaviour was "out of character" from what she had previously experienced. Dr Gibbs said at 7.40pm he was discussing matters with the transport team when someone called for help for Child N as his saturation levels had dropped. Mr Johnson asks if this was an innocent coincidence when all the doctors were 'distracted', 'in a huddle'.
Mr Johnson says thanks to the skill of the medical team, they were able to bring Child N back following resuscitation efforts. Child N's time in Alder hey was 'uneventful' and he was discharged three days later. Professor Sally Kinsey said the blood seen by the male doctor at 8am could not have been spontaneous - "somebody caused the bleeding", and could not have been seen for the first time hours later by Letby, Mr Johnson says. Mr Johnson says the person who injured Child N was "undoubtedly" Lucy Letby.
Mr Johnson turns to the final case, Child Q, who was "doing just fine until he came into contact with Lucy Letby".
Child Q had a 2ml bile aspirate overnight on June 23-24, and feeds were stopped as a precaution. His bowels were noted to be working. Samantha O'Brien fed Child Q tiny amounts of milk the following night. His respiratory condition was "stable" and was tolerating the feeds. The aspirates were "possibly more than you would expect", but said he was stable and there was 'nothing you wouldn't expect' from the baby boy.
For the day shift of June 25, Child Q's abdomen was noted at the beginning of the shift to be 'soft and non-distended' in a note by Lucy Letby. Letby was in room 2, designated nurse for Child Q, and a child in room 1. Mary Griffith was the designated nurse for the other baby in room 2. Letby and Mary Griffith co-signed for medication for a baby in room 3 at 8.34am. Mary Griffith left the unit shortly after that, and Child Q then collapsed, Mr Johnson tells the court.
The 9am observation chart for Child Q is unfinished - "almost as if she was interrupted by something", and the 9am fluid chart also has gaps, with no initial. Mary Griffith came back on to the unit at 9.01am. Mr Johnson says while Mary Griffith was out, Letby took the opportunity to inject clear liquid and air down Child Q's NG Tube.
In interview, Letby said "repeatedly" at the time of the collapse, she had been in room 1, and gave the full name of the designated baby in there. Mr Johnson says Letby has a good memory for that baby, "but she doesn't remember [Child D]." Mr Johnson adds the reason Letby remembered that baby is the room 1 baby "was her alibi".
In Letby's 2020 police interview, she said she needed to see the room 1 baby as she needed 'cares'. Colleague Minna Lappalainen said cares were needed 'every four hours'. Letby had last given cares for the room 1 baby at 8.30am, and Mr Johnson says the explanation to police of cares is a "hopeless excuse". He adds Letby sabotaged Child Q.
Child Q's alarm sounded, Mary Griffith called for help and Minna Lappalainen arrived to help. Mr Johnson says Letby had noted, at 9.10am, 'air++ aspirated' from Child Q and the baby was 'mottled++'. He says this is something which has been seen before, air which hadn't been seen before the desaturation. Mr Johnson says Minna Lappalainen didn't see the aspiration of the air or the mottling, as she was focused on stabilising on Child Q. He says that is something to consider when the defence mention about differing accounts by doctors and nurses on skin discolourations flitting, coming and going. The discharge note by a male doctor for Child Q 'Profuse vomit with desaturation on morning 25/06/16.' He said he wasn't there, and Mr Johnson says this information must have been given to him by nursing staff. He said Child Q's blood gas before 7am was good, and the one before 10am showed respiratory acidosis. Mr Johnson says this was "no minor desaturation" and took the doctor away from the children's ward. Dr Gibbs said the collapse was "not in keeping" with a baby such as Child Q who was getting tired. Letby had messaged later: "Do I need to be worried about what Dr Gibbs was asking?" Dr Gibbs had said he had a 'heightened concern' on the NNU. Mr Johnson says Letby had a heightened concern at this time that people were on to her.
NJ: "Letby's text messages proved that Dr Gibbs' instinct was absolutely right." He says Child Q had been sabotaged by Letby.
Mr Johnson says if this was a minor collapse, as the defence suggest, why was Dr Gibbs so interested into what had happened? A male doctor noted 'small loops in the bowel' 24 hours after the collapse, and Child Q was transferred to Alder Hey. Mr Johnson says it is all irrelevant to what happened 24 hours earlier. A doctor at Alder Hey said Child Q's abdomen had normalised by June 27 and he was transferred back to Chester. He said it was another case where a child recovered quickly when 'taken out of the orbit of Lucy Letby'.
Professor Stivaros later found evidence of a brain injury in Child Q, which Mr Johnson says proves the collapse was not a minor one. Dr Evans was cross-examined on the 'fluid being injected' as a 'late addition' to his evidence. Mr Johnson says the defence said air being administered via Neopuffed was an explanation for 'air++ aspirated', and the description of the collapse was a 'gross exaggeration' of what had happened. Mr Johnson said such criticism was 'unfair', as Dr Evans had referred to 'profuse' from a male doctor's note on the discharge letter. Mr Johnson adds Child Q suffered a brain injury. Dr Evans said a significant amount of fluid appearing on Child Q did not have a natural cause, and was "suspicious of the volume of air aspirated", although he accepts the air could have been introduced by the Neopuff. Mr Johnson says if that was the case, what caused the collapse in the first place? NJ: "He had no naturally occurring problem at the time to cause that extremity of collapse." Minna Lappalainen noted a 'distinction' between 'mucus' and "Clear fluid+++". Letby recorded: 'Vomited clear fluid nasally and from mouth'. The doctor recorded: 'Profuse vomit with desaturation'. Mr Johnson says the jury can be 'confident' with the 'contemporaneous evidence' that what came out was 'not just mucus'. He says it could not have been milk as Child Q only had 0.5ml of milk each 2 hours. Dr Bohin noted if there was 'clear fluid+++' for Child Q, there was "no innocent explanation" for that. The observation chart showed whatever happened at 9.10am was "an acute event" and it happened in the space of 'minutes'. She added that could not have been from the milk Child Q had earlier. She added if Child Q did have NEC, he recovered too quickly for that.
Mr Johnson says he has 'deliberately not spent a long amount of time' on handover sheets. He says Letby hasn't told the truth on them, as the truth doesn't help her. He says the point is very simple for the notes overall - the notes contain admissions, regarding her 'isolation from friends'. He says it has been categorically proved that was a lie, as shown by her social engagements [in a folder]. He says after Letby left the neonatal unit, she put in a 'lying Datix form', for Letby 'getting her defence in first'. The messages Letby sent 'clearly showed she knew there was going to be an investigation'. The Datix form, timed 3pm on June 30, 2016 is a "devious effort to avoid suspicion."
Mr Johnson lists the common events for the babies in this indictment by categorisation. By ones who collapsed despite having good air entry but saturations were dropping: Child A, C, D, G, H [second event], I [third event and fourth event], M, O [twice], P. By bleeds and/or bleeding in throat: Child C, E, G, H, N, plus 'false note by Letby' in K. Unusual discolouration: Child A, B, D, E, I, M, O, H. Suffered life-threatening collapses out of nowhere then recovered very quickly: Child B, D, H [both collapses], I [events one to three], M, N, O, P. Children who collapsed when designated nurse left or leaving the room: Child C, D, G [first event], I [second event and fourth event], K, N [first event], P [third collapse - when doctors were out of the room], Q [slight variation - when Letby got herself out of the room]. Premature babies screaming/crying uncharacteristically at time of collapse: Child D, E, I, N. Children who collapsed shortly after being visited by their parents: Child B, H, I [first event], M, N, O, P. Children who recovered quickly when taken to other hospitals: Child H, I [after 3rd collapse], N, Q. Mr Johnson says Child K's tube never moved after being transferred out of the Countess. When Letby participated in inappropriate post-death behaviours: Child C, I, O. Poisoned by insulin: F, L. Mr Johnson says if Letby had not sabotaged seven babies, they would all have gone home. The other 10 babies, Letby attempted to murder.
That concludes the prosecution's closing speech.
Contents
- Day 1
- The Prosecution's tactics
- The evidence
- Suboptimal care and the senior doctors
- Medical evidence, theories and burden of proof
- Delays and missing information
- The staff rota and missing events
- The Prosecution's list of similarities
- About Lucy Letby
- The post-it notes and social media
- Medical records and timings
- Text messages & Facebook searches
- Diaries and Handover sheets
- The Expert witnesses
- Dr Dewi Evans
- Dr Sandie Bohin
- Day 2
- Child A
- Child B
- Child C
- Child D
- Child E
- Day 3
- Child F
- Child G
- Child H
- Child I
- Day 4
- Child J
- Child K
- Child L
- Child M
- Child N
- Child O
- Day 5
- Child O cont.
- Child P
- Child q
- Final Section
Monday 26th June 2023
Defence Closing Speech - Day 1
Chester Standard Live Reporting - 26th June 2023
Benjamin Myers KC, for Lucy Letby's defence, begins his closing speech
He says he has been sitting next to the jury for nearly nine months, and can hazard a guess at what they may be thinking - 'five days' [for the expected length of his speech]. He says he is grateful for their presence and the material they have had to listen to, and its 'distressing' content.
The Prosecution's tactics
He says what struck him when listening to the prosecution, was that what Letby has done/not done, said/not said - that 'made her guilty'. He says it's "as if the prosecution have a theory" and no matter what the evidence is, or isn't, is treated as to keep that theory going. He says it "doesn't matter how inconsistent that theory is" and that "different standards are applied to Lucy Letby". "Everything is treated as evidence of her guilt".
He cites examples by the prosecution case - her presence when something happens, or not being present, or just leaving the unit, or just turning up for her work. Her making a note, or not making a note - 'guilty'. He says if she signs for medical records, or signs for others - 'guilty'. A baby in her care doesn't show signs of deteriorations - guilty. A baby does show signs of deteriorations - guilty. He says it is "twisting and turning". She cries when giving evidence - guilty. She doesn't cry when giving evidence, or doesn't cry at the right times - guilty.
He says there is 'not one occasion of Lucy Letby doing one of the harmful acts alleged against her.' Mr Myers: "Not guilty." He says "just about everything became an allegation against Lucy Letby". He says what is really at work is "the presumption of guilt", and the prosecution case is "fuelled" and "riddled" by it.
He says he would ask the jury to look at the "presumption of innocence", which is "like a bucket of cold water over everyone at this point". He says "that's the way it works" - "that someone is innocent until proven guilty", that the jury consider the evidence is "fair and balanced". He says "five days is a lot to listen to" - today and into tomorrow is an overview of the defence case, then he will go through the counts individually in the closing speech. He adds he recognises the "enormity" of what the jury have to go through.
He says the information presented has been a "spaghetti soup" of data and evidence, some of which "carries little weight at all". He says the jury must look at the detail presented. He says it is the jury's views that matter on the evidence.
He says that Letby being drawn into agreeing with things in cross-examination that she could not have known cannot be conclusive. He cites Letby being asked about staffing pressures, or the unit taking on too many babies. He says the jury can draw "common sense conclusions" over all the evidence presented. He says Letby is "in no position to settle the issues" [on the unit]. He adds the issues in the trial being discussed are "harrowing and heartbreaking", and cannot be more serious, and 'nothing he says is to diminish the loss' suffered by parents. He says the defence feel upset and "overwhelming sympathy" for them.
He says the emotional reaction to such serious, upsetting and sensitive charges "is to convict". He says the jury have to be "very careful" on the conclusions reached. He says the prosecution "characterise" Letby, which "they are entitled to do", and he says the jury "must be alert to that". He says the language of 'attack', 'gaslighting', 'sabotage', 'you're enjoying yourself', 'your favourite way of killing', playing god', 'calculating', 'manipulative' was sometimes "on the thinnest of evidence...or no evidence at all". Mr Myers says Letby was in 2015: "She's a 25-year-old band 5 nurse, an excellent one - that's what she was, looking after dozens, if not hundreds of babies...day after day." He says "you saw the real person" in her evidence and cross-examination, that she could "remember pieces of evidence" in the years she has been waiting for her trial: "There's little else to do in prison, isn't there?" She was also "scared, anxious and struggling to hold it all together".
Mr Myers cites "plausible deniability" as "if it was a done deal", "setting up cover". He says the prosecution set up questions and answered them as "Lucy Letby", without referring to evidence. He says the way Letby was dealt with in cross-examination was "bad".
He says Letby has been in prison, and in the dock, surrounded by 'commendable' prison dock officers, "standard measures". He says to 'look how this looks' for her in comparison to the witnesses who have come in. He says this is presented as an "inherent disadvantage".
The Evidence
He says the jury must "get past the emotions" and "look at the evidence". He says there are two possibilities of what happened between June 2015-June 2016. He says one of the possibilities is the result of a medical condition, and a condition of the unit - the clinical fragility of the unit, and failings in care at the unit. He says is the other is a nurse who "decided to kill children" or "tried to kill them" for reasons "which make no sense" and "out of the blue".
He says there was a "marked increase" in the number of babies taken on in the unit during that year. He says it was "too many" babies being admitted to the Countess of Chester Hospital neonatal unit with "too many" high requirements. He says the babies were vulnerable as they were in the neonatal unit. He says what some people have said during the trial in evidence, that the babies were "doing brilliantly" there, "boggles the mind". He says it is "no good brushing aside" the issue of sub-optimal care for the babies.
Mr Myers says "the stand-out point" is "not once is there any evidence" of the acts of harm being done. He says this is "the first time" the defence case has been set out. He says the "suspect account" of Dr Ravi Jayaram "doesn't come close" to an account of an attack in progress, nor does the mother of Child E's account. He says there are 22 counts, and 30 events, over 12 months, and "nothing" in evidence of Letby carrying out an attack. He says that was despite Dr Jayaram saying it was "all eyes on Letby" after Child D. Mr Myers adds the jury can use "circumstantial evidence" to highlight sub-optimal care.
He says: "We are the only people who will stand up for Lucy Letby - no-one else." He says the defence case being at the end of the trial is "not an afterthought", and is "so important". He says the prosecution "are not in any special position" with this - they have brought the evidence, "but it does not mean they are right with this". He says there is a suggestion there has been a "hostile reaction" that Letby has "dared to defend herself" and disagree with the prosecution. He says the prosecution "have gone out of their way" to present some aspects as "smoke and mirrors" and evidence by Letby in cross-examination and her evidence was "gaslighting". He says it is "unjustified" and "unfair". Mr Myers says the jury can judge the staffing competencies. He says the prosecution "don't want you to think" about doctors Ravi Jayaram and David Harkness's inconsistent accounts on skin discolouration, that it was a "stunning omission" for them not to put the skin discolouration in notes or in their reports for inquests. He says that point was only uncovered in cross-examination. He disagrees with the suggestion the defence were "gaslighting" the jury. He says it was "not smoke and mirrors" or "gaslighting". Mr Myers says the unit did face "unusual and increased demand" over the 12 months. He says the trial is not about the NHS, or doctors/nurses in general. He says the defence are entitled to be critical of the neonatal unit. He says there is a suggestion there is an "outrage" the defence have "dared" been critical of it.
Suboptimal care and the senior doctors
Mr Myers says it was accepted by the prosecution there was sub-optimal care in the cases of Child D and Child H, but in the latter they did not give much more detail. He says for Child A, there was a 'four-hour' "delay in fluids", and the "line was placed too close to his heart" and was 'not in the optimal place'. "There is plenty of sub-optimal care knocking about in this unit". He says some of the sub-optimal care is 'more contentious than others'. He says there is a "list" for Child H, including the second chest drain for Child H. 'Poor management of stomas' for Child J, and not moving Child K to a tertiary centre, a failure to have factor 8 ready for Child N, 'mistakes in ventilation' and 'getting the doses of adrenaline wrong' for Child P. Failure to react to 'dark bile aspirates' for Child C for 24 hours. He says Child Q was moved to a tertiary centre after three bilous aspirates. He says that is on top of 'babies not being in the right place'. He says babies like Child G and Child I were "prone to serious problems" and "not always" looked after sufficiently qualified staff. He says 'with one exception', senior consultants refused to accept anything was wrong in the 12 months, except for one doctor who failed to attend an emergency as quick as she should have been in the case of Child E.
Mr Myers says evidence presented on October 25 by Dr Dewi Evans: "One tends not to spread news about the mistakes we make", in reference to doctors. He says that is a piece of evidence 'to keep in mind'. He says that was "one of the many things" that came out of his "relatively lengthy" evidence. He says: "In a way, haven't we seen that in this trial?" He says that in relation to doctors being resistant to criticism. He adds no-one, including Letby, is immune to criticism. He says doctors would come with 'prepared speeches'. He says "don't think the senior doctors came here without motives of their own". He adds: "however you look at it, there was a terrible failing of care" at the unit.
He says senior doctors have 'in various ways' suspected Letby was doing something 'for months and months'. He says those doctors 'said/did nothing to raise the alarm...when nothing prevented them from doing so.' He says if they were right, that failure to do anything right was "staggering". He says whichever way, it was a "terrible failing in care".
Mr Myers: "You will understand the stakes [in this trial] are very high. "We don't say 'doctors bad'. We say for those senior consultants who presided at that unit...Lucy Letby getting the blame matters." He says the prosecution used the expression, the 'gang of four' consultants of Dr Jayaram, Dr Stephen Brearey, Dr John Gibbs and a female doctor [who cannot be named]. He says the doctors 'have an interest in what happens here' and each of them 'had gone out of their way to damage Lucy Letby' in their evidence. He cites an example on pneumothroaxes presented by Dr Gibbs which he says was "unneutral". He says "one way or another" the unit "failed". He says this case is a "prime opportunity" to "hide" bad/poor outcomes.
He says the unit was "noticeably busier" than it had been in previous years, and there was "no change in the staffing levels". He says doctors are "running to and from the neonatal unit" in emergencies. He cites an example in the final collapse of Child I.
He cites Dr Sally Ogden's evidence that June 2015 was a "particularly busy" time at the unit, and that was a combination of factors, including the complexity of the babies' needs, the number of staff, and total unit admissions. He says the increased busyness increases the likelihood of mistakes and the chances of missing developing problems in babies. He says the Countess was designed to look after babies of 27 weeks + (gestational age), and there were babies in this case who would be "far better" cared for at a tertiary centre, and evidence had been heard that for Child K's case, the tertiary centre care could have made a difference.
He says between June 2015-June 2016, the unit was "under a much greater burden". He says during this time, whatever the hospital had to "deal with changed". He says after the Countess neonatal unit became a 'level one unit' after June 2016, two more consultants were added. He says that is indicative of staffing pressures prior.
The trial is now resuming after a short break. Mr Myers continues his closing speech.
Medical evidence, theories and burden of proof
He says the single most important direction in the trial is the burden of proof, which is on the prosecution, and it "never shifts" to the defence. He says the prosecution "have to make you sure", and there are so many areas where the evidence "is not clear".
He says the jury have to be "sure of deliberate harm" and "with the intent to kill", and the jury must assess the "quality of evidence". He says the "medical evidence is the foundation of this case". Mr Myers says Lucy Letby denies all the allegations. He says it must be identified harm being done, and being sure there was an intent to kill at the time. He repeats that Letby denies doing anything like that on any occasion. He says the case is "about an insistent intent to kill". He says that much be considered in the context of Letby 'raising the alarm' for some of the babies, or looking after some of the babies 'before and after their events'.
Mr Myers refers to the theory of air embolus, and if that 'works' each time, why would someone change it up to administering insulin. He says it is 'awful' to think about it, but to go with the prosecution case, he asks why the methods used varied. He says the prosecution referred to levels of insulin were doubled for Child L than for Child F. He says for Child F the level of insulin, from the lab result, was 4,657, whereas for Child L it was 1,099, and the insulin/insulin c-peptide ratio was lower, and 'must be a quarter of the strength'. He says "that was evidence, it was wrong". He says if there was an intent to kill, then the dose wouldn't be a quarter of the strength second time round. He says whatever happened, "that wasn't an intention to kill".
Mr Myers says "various factual allegations" came across Lucy Letby which amounted to 'wholescale document fraud', referred from 'page 34,536 of the evidence', he says, including children not on the indictment - such as 'the Stoke baby'. He asks why witnesses were not cross-examined about such incidents, on 'falsely identifying names' on paperwork, over the months. He says the "prosecution have been looking for things...so they can shore up". He cites a piece of evidence from the case of Child H, a note by Alison Ventress about a chest drain. He says she gave evidence, and she was cross-examined about it, about chest drains moving. He says that was no part of any allegation, and "it came out of nowhere" in cross-examination, "it suddenly became part of an allegation". He refers to a note about blood-stained secretions for Child H, made by Letby. He says the prosecution used that note as an opportunity "to bolster their list" by asking her if she had altered Child H's ET Tube.
Mr Myers says Letby was asked about how long she had been on the phone when feeding a baby not on the indictment, and how long she was spending texting. Letby had said: "You think I pushed it in, didn't you?" Mr Myers said Nicholas Johnson KC, for the prosecution, replied: "I do." Mr Myers asks where had that come from, and "there was no evidential basis" for that. He says it was "an allegation on the hoof". He says no-one suggested that baby had a vomit was unwell. He says that allegation was "made in passing".
Delays and missing information
Mr Myers moves to the issue of 'delay'. He says there is an issue with missing door swipe data between July-October 2015, and allegations are made against Letby during that time, such as during the case of Child I. He says the prosecution had accused Letby of 'making up a note' for September 30, 2015. Mr Myers says the prosecution can make that allegation as the door swipe data is missing for that date. Another note is referred to for October 14, 2015. He says Dr Matthew Neame's note, timed at 5.55am, is used as evidence there was a delay in reporting the issues. Mr Myers says it is their case 5.55am was when the note was written, not the time he attended. He says there is no door swipe data for that day to say when that doctor arrived.
Mr Myers says there is missing post-mortem examination evidence for Child E, which allowed the prosecution to present evidence of 'bleeding from the throat'. He says that allowed the prosecution to provide linked evidence. He says there is no evidence to show it, post-mortem.
The staff rota and missing events
Mr Myers moves to the topic of 'lists'. The 'staff presence' of when staff were on shift during the times of the 25 events for the babies. He says it is a "major part of the prosecution case" that Letby is present "far more often" than other staff. Mr Myers says it "doesn't show fault". He says "one thing that is striking about this chart" is having focused on it in the opening, there has been no reference to it at the end. He says the jury might wonder why that is. Mr Myers says it is "obvious now" that the list isn't complete. It is "missing two or three events" which could be considered "harm events". He points to Child N's case at June 14, 'night', for Child N's second event at 7.15am. Mr Myers says that is correct, and evidence had been heard Child N was unwell that night. He says Dr Sandie Bohin identified that in her evidence. He says Letby wasn't on duty for the night shift. He says the prosecution say Letby 'did something' before she left her shift the previous night - "what, we don't know". He says the point is that Letby 'wouldn't be in that shift' and the note would be blank.
Mr Myers says there is a 'harm event' for Child C, as identified by experts, on June 12, 2015, which is not in the sequence of events, and is not on the list. He says Letby was not on duty at that time. He says the prosecution are "not that bothered" for that one as Letby "wasn't on duty". For Child I, there was a 'harm event' identified which is not included on the chart, and says the table 'doesn't look so good'. He says there was a third 'harm event', not featured on the indictment, for Child G. He says Dr Sandie Bohin had said there were no further projectile vomits. Mr Myers says he referred to a third event happened on October 15, 2015 by Ashleigh Hudson, at 7.20pm...'one vomit, projectile, quite large in size'. Dr Bohin said if she had missed it, she missed it, Mr Myers tells the court. He added that was her attitude. He says there are 'at least two, maybe three events' which happened for the babies when Letby was not on duty. Child C on June 12, 2015; Child I, August 23; and Child N, June 14, 2016, night.
The Prosecution's list of similarities
Mr Myers refers to the 'list of similarities' that Mr Johnson used at the close of his speech. He says the lists are "not similar" and "how on earth" they are supposed to show a pattern of criminal behaviour. He says they are "masses of lists of differences" He says it is "dead right" they are a list of "dissimilarities". He says Child I features on eight of the lists. Child J is on 'none of them'. Child K is on one of the list. Child A and Child B on two, Child N, six, out of '11 similar features'.
He says the alternate reading is that for the babies a list does apply to, the remaining are for which they didn't. He says there is a 'mirror image', that a list which features seven babies, means that 10 babies did not have that similarity, and for one which features three babies, means it didn't happen for 14 babies. "These lists mean nothing...unless it is linked to the harm alleged." He says the list 'presumes a lot', that the defendant is guilty. He cites the list of discolouration features for some of the children, which staff had not seen before or since. He says each discolouration has to deal with individual babies, whether there was sub-optimal care, and on the quality of the evidence featured. He says for Child A, the descriptions given were 'relatively poor'. He says for Child M, one witness saw a discoluration - Dr Ravi Jayaram. He says the basis of Child H's discolouration was a father's account for a description of the fingers. He says the approach of the list is 'prejudged', 'misconceived and unfair', and the evidence is "very variable" and "create a fundamentally unfair situation". Mr Myers says the jury have to be "very careful" to look at a "short-cut" approach.
About Lucy Letby
Mr Myers says he will refer to 'brief looks' at Lucy Letby, the person she was and is, and documents, and the subject of 'experts', this afternoon. He says who Letby is, and was, is at the "heart of this case". He says she had "never been in trouble before". He says the jury will have formed an impression from her giving evidence of a "serious" person. A photo of a noticeboard from her home, taken at the time of her arrest, "is a good snapshot of who she is, and was". The noticeboard includes a photo of Letby smiling. The noticeboard photo isn't conclusive but "isn't unimportant" - "this is the person we were dealing with at that time". He refers to the "commitment" Letby did in training to care for "hundreds and hundreds" of babies. He says it is "important of the type of person she is". He says it makes the allegations "all the more unlikely", and medical professionals had spoken "highly" of Letby. He says nurse Christopher Booth agreed she was 'conscientious and excellent', and it was "not unusual" for her to work overtime. He agreed she was a "hard worker". He agreed she would be "upset" by the events which unfolded, as it was a "harrowing time".
He says it does not automatically make someone a murderer because of their behaviour after a baby has died, that it can be a misjudgment, although that was how it was presented by the prosecution. Mr Myers says Letby was "committed to her work" and evidence showed "how much she wanted to work". He says she was "young, keen, flexible". He cites agreed evidence from one of Letby's nursing colleagues: "I also remember...we had massive staffing issues, where people were coming in and doing extra shifts. It was mainly Lucy [being a band 5 nurse]. Lucy was young, living in halls, saving up to buy a house, single, willing to do extra work shifts..." Mr Myers says that would explain Letby's increased presence on the neonatal unt.
Mr Myers cites evidence from Eirian Powell, ward manager, in which he says she talked about Letby's importance on the unit, and said Letby was an "exceptionally good nurse" and had "known her since she was a student". She said Letby was "very upset" when she was removed from the unit. Mr Myers says that upset was "no act". He says Ms Powell said Letby was "distraught". Ms Powell said Letby was distraught as 'she thought she caused the deaths of the children'. Mr Myers says there is no doubt Letby was "very upset at the time" and this was "genuine distress".
The post-it notes and social media
Mr Myers refers to the 'striking' notes. He says they demonstrate the "anguish caused to Lucy Letby by what was happening". He refers to the 'not good enough' note. He says Letby wrote that not to the court, not to the police, but to herself, plainly "showing how she feels". He says that was "utterly consistent" of Letby being distraught about being taken off the unit. He says Letby wasn't 'pretending to need anti-depressants' for years, and wasn't 'pretending to be suicidal'; "the impact was immense".
He refers to the social media evidence. He asks what did the evidence give a false impression of - "that she dared to have a social life [in those two years before her arrest]?" Mr Myers says Letby, in cross-examination, had agreed she would go to the races, and have 'fizz', and go on family holidays. He says the photos show Letby having a "conventional social life". He says photos like that rarely show what is going on inside. He says there is nothing shown from the social life which runs contrary to the distress she was suffering. He tells the jury: "If you look in the dock [at Lucy Letby], you can see the effect of years of this."
Medical records and timings
Mr Myers refers to the documents, such as the neonatal schedule, which have 'limits to what they show', as they "only show activity". He says they cannot pin down a nurse's time at a precise time, at a particular location. He says the computer-timed prescriptions are not 'definitely precise.' He says the times are often made "retrospectively". The review does not mention how long an activity takes - which can vary, Mr Myers adds. He says the schedule provides a guide to timings, and does not show what somebody is doing when there is no record. He says it shows that nurses may be shown to do more than one activity at a time. He adds many of the events have someone to assist, and says other nurses assist colleagues. He says when that has been the case for Letby, she has been treated in "the most prejudicial way possible".
Text messages & Facebook searches
He refers to the subject of the text messages, which are "normal". She was a "young professional woman with a life", and the messages contain "social activity and banter". He says only when "you start with a presumption of guilt" can be taken as different. He refers to the 'go commando' message. He says a young woman, being cross-examined, being "humiliated" about something 'completely unrelated to what we were talking about', in front of the public, in front of her mum and dad, was inappropriate. He says "You saw me raise to my feet more than once" about the style of questioning, and the comment about 'running out on your boyfriend [doctor colleague]' was inappropriate. He adds the messaging was "unremarkable". He says the basis of Letby being 'bored' was used as the basis of an allegation she went out to kill a baby. He says "others were doing it at work" [text messaging in the workplace]. He cites four work colleagues who did so, and they were "normal...what you might expect". He says there is "work, gossip, there is winning at the Grand National, there is salsa dancing...normal things."
Mr Myers refers to Facebook searches. He says those familiar with social media will look up people for all sorts of reasons at any time of the day or night. He says it may be "no more than a handful of keys". He says the prosecution identified a number of messages, and there were more messages than that, Mr Myers says. He says the jury may agree Letby was a regular user of Facebook, and "rattle through searches". He says the prosecution draw the jury's attention to the searches for parents, in connection with the allegations. He says that would be a pattern in line with the theory. He says some of the parents names of babies on the indictment are missing from the Facebook searches. He says there are no searches for the parents of Child L-Q. He says the searches by Letby also demonstrate an interest for parents of babies not on the indictment. Mr Myers says that is "important", and Letby is seen as somebody who looks up names regularly.
He says of Letby's 2,318 Facebook searches, "only 31" related to parents' names on the indictment. Mr Myers says Letby has not searched for things on 'air embolus', or 'forcing in air', or any 'fascination with what's alleged here'. He says there is no evidence found Letby Googled 'haemophilia' following a conversation between a colleague nd Letby on Child N.
Diaries and Handover Sheets
Mr Myers refers to the 2015 and 2016 diaries found at Letby's home. He says there is nothing in the 2015 diary which is relevant to the indictment. He asks, if the diaries are relevant, why there is no reference to Child A-K in them.
Mr Myers refers to handover sheets. He says it is "not difficult" to see why Letby would have handover sheets in the first place. He says the issue is why she would keep them in such quantities. He adds if that is evidence of her intention to kill. He says Letby's position is she "didn't throw things away". He says Letby had a "habit" of retaining pieces of paper. He says Letby was 'collecting' in the style of 'accumulating', not as in "collecting stamps". Letby had said, in cross-examination, she accumulated the paperwork, not its contents. Mr Myers asks if the jury don't think this accumulation is "random", what is the prosecution's case for them? He says if Letby had handover sheets and only handover sheets relating to babies on the indictment, that would be significant, but a total of 257 handover were found, with 21 relating to babies on the indictment - "less than 10 per cent". He says there are no handover sheets for Child A, C or D.
Mr Myers says for the 21 handover notes relating to babies on the indictment, '9 or 10' do not refer to dates on which events for the babies happened. He says "they don't do what they should do if the prosecution are right".
He says they do show someone who hangs on to paper "compulsively". He refers to the shredder, and what Letby didn't shred. He says if Letby had thought there would be a police investigation - as written on one of her notes - she would have shredded the handover notes.
Expert Witnesses
Mr Myers refers to the subject of 'experts'. He says the prosecution medical evidence is 'central' to their case. He says it is crucial to show the jury that there is no medical cause for the collapses of babies, and that substandard medical performance is ruled out, and that the alleged harmful acts took place.
Mr Myers says experts should be assessed as other witnesses. He says they don't decide the case, and their assistance is needed to explain how the babies collapsed. He says the jurors should take their evidence into account, but "you don't have to accept them". He says there are 'certain features which are important', that the witnesses in their field "must be an expert" and the "expert is an expert on their topic", and that was something, he said, was recognised by Prof Sally Kinsey, an expert in haematology, who "acknowledged frankly" she was "not an expert" on air embolus.
Mr Myers says theories on air embolus were cited by one expert in 'pigs and rabbits', not neonates. He says expert evidence should be 'independent and objective', 'neutral - just stating it as it is', and 'not an advocate for one side or the other'. He asks if Dr Dewi Evans, Dr Sandie Bohin and Dr Andreas Marnerides gave impartial, objective evidence. He says if the experts do not come out to that, it is "game over for their opinion on that topic".
The judge, Mr Justice James Goss, brings the jury's attention to a matter raised in their absence earlier today. He refers to a matter of the chart presented earlier today, to a list of events and which staff were on duty, presented in court on screens. The judge says he and the jury had 24 events listed on their bundle of evidence, whereas the screen had 25 events listed. The 25th event was irrelevant to the point raised by Mr Myers, and was from an earlier version of that document.
The trial is resuming after a short break. Mr Myers continues to give the closing speech.
Dr Dewi Evans
He says, in reference to Child Q, he had omitted a reference from Dr Evans's report on Child Q vomitting. He says he accepts that was a mistake. He says Dr Evans had been criticised "in scathing terms" by a court of appeal judge. He says Dr Evans is the prosecution's 'lead expert', and the prosecution not referring to that criticism in the closing speech is "appalling", and his evidence 'underpins' their case. He says Dr Evans is 'not a neonatologist - and that matters'.
He says Dr Evans hasn't got current clinical practice, and "a good deal of his knowledge is historic" and he is "an expert at being an expert", and "his focus is on that, and not in clinical practice". Mr Myers said Dr Evans had accepted his principal role in recent years was of being an expert, and attended a course on having to 'avoid pitfalls'. Mr Myers: "We say he should have been taking a lot more notes at that course". Dr Evans said he had called himself a medical independent witness, not as an expert, and he had come to assist the court on challenging medicla issues. Mr Myers: "There you have it from the horse's mouth. He is meant to be an expert." "You may think that frank assessment was more revealing than you can imagine." He says Dr Evans' evidence is the starting point for the other experts. "He has led the way on medical opinion."
Mr Myers refers to how Dr Evans came to be involved in the case. Dr Evans said he had been contacted by the National Crime Agency. The court is shown an email from Dr evans: 'Incidentally I've read about the high death rate for babies in Chester, and that the police are investigating. Do they have a paediatric/naeonatal contact? I was involved in neonatal medicine for 30 years, including leading the intensive care set up in Swansea...' Mr Myers says the email concluded 'interested to help. Sounds like my kind of case'. He says Dr Evans 'Did not like' the suggestion he was "touting" for work. Mr Myers says his credibility was affected. He "touted for work on his kind of case" created a "misleading impression". He says Dr Bohin was given a reference and Dr Marnerides has relied "heavily" on Dr Evans's opinions. Mr Myers: "He is a full member of the prosecution team from the very start. He is not neutral. He is not independent in any way."
Mr Myers says he had, in evidence, asked Dr Evans if he had come up with air embolus first. He said he'd had. Mr Myers refers to the chronology. He says doctors including Dr Jayaram were suggesting air embolus from July 2017. Dr Brearey said there were two meetings with police, including one on May 15. At that meeting, Dr Jayaram raised concerns with police about air embolus. Mr Myers says this is before Dr Evans got in contact after that point. Mr Myers says Dr Evans was "very keen to get involved" and "unless they [Dr Evans and the police] met in silence" in July 2017, then Mr Myers says Dr Evans would have been informed about a theory of air embolus after being relayed suspicions by the police.
Mr Myers says Dr Evans was cross-examined "for months" about his 'lack of independence'. He says Dr Bohin "has done the same thing but with rather more subtlety". He refers to agreed facts, of December 5, 2022, of a judge's ruling in a court of appeal, in which there had been a report of Dr Dewi Evans. Included in his reasons for refusal, the judge said: "The report is worthless and shows no support whatsoever for an appeal. “No attempt has been made to engage with the full range of medical information or the powerful contradictory indicators. “Instead the report has the hallmarks of an exercise in ‘working out an explanation’ that exculpates the applicants. “It ends with tendentious and partisan expressions of opinion that are outside Dr Evans’ professional competence and have no place in a reputable expert report. “For all those reasons, no court would have accepted a report of this quality even if it had been produced at the time of the trial.” Mr Myers says those comments are "appalling". He says the language from the judge "resonates very uncomfortably" with the evidence presented in this case. "Those comments paint a disgraceful picture". Mr Myers says those comments were put to Dr Evans. He said Dr Evans the Lord Justice of Appeal had got it wrong. Mr Myers "the worrying thing" is "he wouldn't really accept the criticism at all". Mr Myers says that decision "coincides with the months we have spent complaining about [him]".
Dr Sandie Bohin
Mr Myers says Dr Bohin hasn't 'peer reviewed' Dr Evans, but "supported him as far as she can", and "is every bit as much a part of the prosecution team [as he is]." Mr Myers says Dr Bohin has "worked" to agree where she can. "We do say she has been doing her best to shore up the allegations as far as she can." He says of Dr Andreas Marnerides, a pathologist, "is not a clinician, is not a paediatrician or a neonatologist", which "puts some limits [on his expertise]". He says his expertise is on what happens following a death, not in life. He says Dr Marnerides is "reliant" on the evidence of others, something which he agreed. He says he made a lot of reference to Dr Dewi Evans, and it is "too late in the day" to "insinuate" it is someone else.
Tuesday 27th June 2023
Defence Closing Speech - Day 2
Chester Standard Live Reporting - 27th June 2023
Child A
Benjamin Myers KC is referring to the case of Child A. He says there was sub-optimal care in that case. He says on a neonatal unit, babies "are there for a reason" and many of the babies have "signficant problems" and are "at risk of deterioration"
He says Melanie Taylor was designated nurse for Child A and Child B. They were both intensive care babies. He says the prosecution have relied on nursing guidelines for some of the children, but not on the "fundamental issue" of staffing numbers. He says there "should not have been just one nurse" looking after Child A and Child B. He says if there was one nurse for each, they would be "more confident" the issue of lines and nursing care was resolved. He adds Dr David Harkness was stretched between a number of babies for the shift on June 8, 2015.
The respiration rate chart for Child A is shown, with what Mr Myers says is "escalating up to the point of collapse", and is in a yellow bracket (ie elevated above normal). He says [medical expert] Dr Sandie Bohin would not accept that, saying it was stable. Mr Myers says the defence wonder how much attention was paid to Child A, with Melanie Taylor looking after two babies. Mr Myers says Child A received no fluids for four hours, and Dr Bohin agrees it was "sub-optimal". He says the long line was "in the wrong place" for Child A. He said the records show it was not correctly sited. He refers to an x-ray review on June 8: 'Long line...to be pulled back'. Dr David Harkness put in 9.20pm he was unable to move the long line as he had been called to another patient. Mr Myers says Dr Harkness had a review with colleagues the following day and they agreed it was in a 'perfect place'. Mr Myers cross-examined Dr Bohin on the long line position, which she reported was 'not in the best position'. He says Dr Bohin didn't mention it in her evidence. Mr Myers says the line 'was too close to the heart', and fluids were put down it, and Child A had a fatal collapse within 20 minutes of that. He says Dr Harkness removed the line as soon as the collapse happened.
He says Letby helped a nurse with sterilisation. He asks when was she supposed to have done what she was alleged to have done, and next to Dr Harkness and Melanie Taylor. He says there is "nothing to support" that Letby got a syringe and injected some air. He says "no-one could access" the lines without opening the incubator first.
Letby said it was Melanie Taylor who set up and connected the line and put up the fluids. Melanie Taylor "couldn't remember which way it was". Mr Myers says that is something the prosecution would have "absolutely slated" her is she was the one accused. Mr Myers says another nursing colleague gave "lots of evidence", but "could not remember", in evidence, who connected the line. He says in cross-examination, from her January 2018 police interview, the colleague said: "it appears I was able to say then it was Mel who did it". Mr Myers says on the evidence, there is "no basis" of Letby being guilty of any offence for Child A. He says this account is "firmly based on the experts" who agreed on air embolus.
Mr Myers refers to the 'overarching theory of air embolus'. He says "at the heart of it" are Dr Dewi Evans and Dr Sandie Bohin, 'neither of whom are experts on air embolus'. He says they relied on a research paper written over 30 years ago. He says he asked them the clinical signs of identifying an air embolus. They both said a sudden and unexpected collapse. They said a skin discolouration, and the presence of air in the great vessels. Dr Evans added 'resuscitation is unsuccessful'. Mr Myers not one of those criterium have been applied consistently across the trial, and they have been 'chopped and changed' to suit the evidence, with 'extraordinary contortions' to fit. "My word, it changed", he adds.
Mr Myers says the research paper from 1989 identified 5 out of 53 infants with skin discolouration, and one had a rash, of 'bright pink vessels against a generally cyanosed cutaneous background'. He says it is a very specific description, of one case study. He says as the basis of convicting someone of murders and/or attempted murders it is "tenous in the extreme", but Dr Evans and Dr Bohin have made reference to it. That "meagre" research has "carried into pure guesswork", he adds. Professor Sally Kinsey, a professor of haematology, had also given evidence. She had said in cross-examination, she was not an expert in air embolus. She agreed she hadn't seen it herself, and that air embolus did not feature in her expertise. She said she had given evidence because "she had been asked to". Mr Myers said she had relied upon Dr Evans and Dr Bohin, which he adds was a "big mistake".
Mr Myers says there are many causes of discolouration to a baby, and there isn't a precise description as there is no photograph of any. He says the descriptions vary between the witnesses. He adds sometimes the descriptions have come months or years afterwards, after people have listened to other people's descriptions, and the dangers of recollection being 'contaminated or influenced are obvious'. Mr Myers says 'unexpected collapses' can happen to neonatal babies. He says Child D had pneumonia and was at risk of collapse. He says for 'resuscitations unsuccessful', the proportion of babies who recovered in this case "doesn't make sense". He says the air is 78% nitrogen and "doesn't just go". He says it is "static, it is a blockage", and would be found post-mortem. He says the jury won't find air in the heart, post-mortem, in any of the cases.
Mr Myers says the jury know what an air embolus looks like, from how Professor Owen Arthurs described it, and a radiograph image was supplied with the research article. He says it looks "nothing like" what was shown in this case. He says for Child G, the image looks "nothing like", and the UVC is "misplaced" to the lower liver. A second image for Child G shows the baby 'in life', with an air embolus. He says an air embolus can happen "by accident" in legitimate medical treatment. He says Dr Bohin "reluctantly" accepted that could be the case. He says Dr Evans refused to accept it. Mr Myers says the scientific evidence "falls short" on air embolus in this case, with background research "poor", and the guidance has been applied "inconsistently". He says the evidence "is so poor" it "cannot be used" to back the allegations.
Mr Myers refers back to the case of Child A. He says there was a 'failure to read subtle signs'. He says the "crucial" element is there is no evidence of air embolus. He says the prosecution have gathered witness accounts from this trial of the skin discolourations. He says those recollections can change over the years. He says there is no reference to discolouration in the contemporaneous notes for Child A, which he says is "extraordinary". He says nurses Caroline Bennion and Melanie Taylor didn't note anything remarkable. He cross-examined Dr Harkness on the description, who was "very animated" on the "striking" discolourations and "unexpected deterioration", but did not note it at the time, or in a statement to the coroner. He says the evidence by a nursing colleague noted, in a 2018 police interview, Child A was 'centrally pale', with limbs 'white'. Mr Myers cross-examined her on it, and asked her about 'blotchiness', and where that had come from. She agreed the description was different between police interview and evidence. Dr Jayaram said Child A was 'pale blue', with discolouration 'flitting around'. Mr Myers says the description he gave from the interview was 'very similar' to the one from the research paper. My Myers says the description does not appear in his clinical notes at the time, or in the "lengthy statement" to the coroner. Mr Myers says it is a "remarkable coincidence" that two doctors did not give evidence of discolourations to the coroner in a statement, or note it at the time.
My Myers says there is "no fair or proper basis" for an air embolus for Child A, and sub-optimal care, with the "long line in the wrong place".
Child B
The trial is now resuming following a short break.
Mr Myers refers to the case of Child B. He says Child B's deterioration on June 10 was "relatively brief", and didn't involve her being intubated. He says the defence accept there is no obvious medical condition or obvious evidence of sub-optimal care. He adds the evidence of an injection of air for Child B's deterioration "is so weak" and "unclear". He says: "If it isn't clear, therefore not guilty."
Mr Myers says there can be deteriorations for which the cause cannot be identified. He said there had been a number of attempts to insert a line - five by Dr David Harkness - for Child B, when the guideline was a maximum of three. He says the difficulties of inserting lines can put a baby under stress. He says Dr Evans, in cross-examination, went through all the potential causes. He says it was suggested Letby had moved the nasal prongs, or that Child B had been "smothered" - Mr Myers says there was no evidence of that, and it was 'abandoned'. He says the conclusion was of air embolus. A nursing note by a colleague said the prongs had been moved, and "it was not unusual" for the prongs to be moved out by a baby. On air embolus, Mr Myers says nursery room 1 "is a busy nursery" with staff coming and going. Belinda Simcock [Williamson] said, to police, there are 4 drugs cupboards and a sterile fridge, with keys held by the shift leader or a band 6 nurse. "It was constantly busy - I would liken it to a bus station," she said.
Mr Myers says for this allegation, Letby would have to be close to Child B - "and of course, she is not". He said it was "normal" for her to be assisting a nursing colleague in room 1, in assisting putting up the TPN bag at 12.05am. He says the nursing colleague is "not going to miss that" if air is injected, and it would not take 25 minutes for it to have an effect [when the deterioration takes place]. Mr Myers says at the time of deterioration, Letby was with the nursing colleague and not with Child B. He says the nursing colleague had said she was "keeping a particularly close eye on [Child B]", given the prongs had been dislodged and what had happened to Child A.
Mr Myers says the deterioration was not rapid in this case, and resuscitation was successful. A radiograph was taken 40 minutes after the deterioration. He says 'no-one is suggesting air' is present. He says that is different from the radiograph image for Child G, which was taken at Arrowe Park, where the air was still there. He says for discolouration, there was contemporaneous notes at the time. He says the defence are not disputing these discolouration descriptions at the time. He says none of the descriptions match that from the research paper.
My Myers said a doctor who had been present for Child A and Child B said what she had seen on Child B was something she had "not seen before", Mr Myers tells the court. He says it is accepted the skin discolouration is 'striking', but what happened was 'not air embolus'. He says it is not a particularly nice detail [to point out in comparison to other cases], but there was 'no screaming or distress' for Child B. He says that detail of 'screaming/crying/distress' was 'worked into the theory' by medical experts later in the case.
Mr Myers refers to a text message sent by Letby on June 12: '...They are querying a clotting problem [for Child B].' He says the prosecution said Letby was 'introducing cover' for events that had she had caused, "seizing on comments". Mr Myers refers to a text message conversation on June 10, in which the colleague reported: '[Child A's] prelim report - no gross abnormalities. So now bleeds, clots or line issues.' He says this is something Letby is talking about after being informed about it by another nurse, and is "unremarkable".
Mr Myers refers to a note by a female consultant, and suggests Dr Evans 'grabbed at' an explanation of 'pink and active' to describe a rash on Child B. Dr Bohin, cross-examined on it, had said it was "a mistake". Mr Myers says it was "not an innocent mistake".
Child C
Mr Myers refers to the case of Child C. He says Dr Evans identified no cause for the collapse in his report, but identified air embolus in evidence. He says a number of things are "wrong and unfair" about this case from Letby's perspective. He says if Child C was 1g lighter, he would have been treated at a different hospital. He was very premature, poorly and had pneumonia when he died, and had black bile aspirates in the final 24 hours of life. He says the medical experts refused to acknowledge Child C was more poorly than they said he was. He says Letby is being blamed for something when 'on the evidence she wasn't even in the room when alleged harm was done.'
Mr Myers says there were "failures by the neonatal unit", and he should have gone to a tertiary unit for investigation, and there was no examination by a consultant at an earlier stage, or a sufficiently early response to the black bile aspirates, and there was a "general failure" to document things properly. He says that was "circumstantial evidence" of sub-optimal care.
Mr Myers says the prosecution case was to minimise the problems for Child C. In cross-examination, Letby said she could not recall if Child C had prior issues. Mr Myers says Letby was 'manoeuvred' into saying that was the case, and the defence do not accept Child C had no prior issues. He says one of the notes had been put in the wrong patient's file, which was 'poor record keeping'. "Imagine if it was found Lucy Letby had done that? 'Plausible deniability'."
The note recorded bile on a blanket and black-stained fluid for Child C. He says nurse Yvonne Griffiths hasn't signed for a 9am reading on June 12, and something was entered for noon and not signed. He says bile on a blanket and black fluid is recorded in the nursing note at 6.30pm, but is not noted on the fluid chart. He says a radiograph was taken at 12.36pm. Dr Evans, Dr Bohin and Dr Andreas Marnerides had all regarded the image as a 'suspicious event' of harm. He says Letby was not on duty. Dr Anne Boothroyd recorded 'marked gaseous distention of the stomach'. Mr Myers says the jury should take this as "proof" the experts can "get it wrong". He says if this event happened when Letby was on duty, Letby would be accused of causing it.
Mr Myers says futher bile aspirates recorded are a concern for Child C. Dr Sally Ogden had confirmed that could be serious, Mr Myers tells the court. He says when cross-examined, Dr Ogden said it was "a worrying sign", and agreed it could be a sign of some gut obstruction. Mr Myers says on all the evidence, Child C 'merited closer care and attention than he received'. Dr Gibbs said, in cross-examination, intestinal obstruction 'could be one explanation'. He agreed bilous vomits were a 'red flag' for such an infant.
Mr Myers says Child C's bowels did not open throughout. He says Dr Bohin was 'firmly against' suggestions Child C was not doing well, and that it was not relevant he did not leave intensive treatment unit. He says she had the "gall" to imply that where nurses recorded dark bile, it "could have been blood". BM: "How is that better?...What a thing to say - she wasn't there." He says it is an "extraordinary dismissal" of the evidence of "experienced nurses".
Mr Myers says Dr Bohin, for Child Q, bilous aspirates could indicate gastroenterology problems. He asks why that could not be highlighted as a problem for Child C. Mr Myers says it was a "lack of care" that was a potential factor that led to Child C's collapse. He says Professor Owen Arthurs was asked about the radiograph image for Child C on day three of life on June 12. He says if Child C had not opened bowels, it could be indicative of an obstruction. Mr Myers says Prof Arthurs was not aware the bowels for Child C had not opened, and there was no clinical record they had.
The trial is now resuming following its lunch break.
Mr Myers says, for the case of Child C, he looks at the post-mortem evidence of whether there was a gastrointestinal blockage. He refers to the agreed evidence by the pathologist, Dr Kokai, who conducted the post-mortem examination, who recorded a 'distended colon' for Child C, which was not normal. He says Dr Marnerides refused to accept this evidence, who said the bowel was 'normal'. The stomach contained 'a large amount of air'. Mr Myers says Dr Evans was prepared to accept air being forced down the NG Tube on June 12 - when Letby was not on duty - but 'just came out' with air being forced down the tube, and an air embolus, in evidence for June 13, when he had not mentioned it in his pre-trial reports. Mr Myers says that was "without any evidential basis at all". He says Dr Bohin agreed that pneumonia was a contributory factor for Child C's death. He says the defence's position is that pneumonia made Child C more vulnerable, and Dr Bohin 'refused' to consider a combination of pneumonia and something else - such as an abdominal blockage - caused the collapse. He says Child C was a "very poorly little boy" who "should have been transferred out of [Chester] with the problems he had", and had "sub-optimal care".
Mr Myers says Sophie Ellis "should not have been looking after" Child C, as she was "inexperienced" and put in charge of a "fragile little boy". He says the collapse of Child C follows "the one and only feed" he received. He says Sophie Ellis "didn't see Lucy Letby do anything wrong". Mr Myers says the evidence of Melanie Taylor "contradicts" in court to what she said to police in 2018, "swapping Lucy Letby for Sophie Ellis". He says she was "utterly brazen about this" in cross-examination. He says the account changed so it put Lucy Letby in the room. He says a female nurse colleague said in evidence was consistent with what she told police. She had been dealing with a different baby, in a different room, with Lucy Letby. She said between 10-11pm, she was called to assist Child C. She 'went to nursery 1, where Sophie Ellis and Melanie Taylor were Neopuffing [Child C]'. Mr Myers says Letby is "nowhere near nursery room 1" at the time of the collapse.
Child D
Mr Myers moves to the case of Child D. He says the "evidence is very clear" that Child D was "very unwell" at 12 minutes of age, but she wasn't given antibiotics for four hours, and Child D was born with pneumonia, and required ventilation, and was on it for 11 hours, and there were continuing signs of respiratory difficulties, requiring the use of CPAP. He says after Child D's first collapse, it was discussed what to do, and there woul 'be a low threshold to intervene from a respiratory point of view'. He says after the second collapse, Child D was taken off CPAP, and Child D later collapsed fatally, and post-mortem was found with acute lung damage. He says Child D was "very ill from the outset". He says it is "a very unfortunate decision" after the second collapse that Child D was taken off CPAP after a discussion of a 'low threshold to intervene'.
Mr Myers refers to the pathologist's report for Child D, recording damaged lungs, "continuing respiratory problems". Presence of infection is "not ruled out" following negative microbiology tests, as Child D had been on antibiotics. Mr Myers said despite that, Dr Marnerides "preferred" air embolus as a conclusion. He said he had taken into account clinicians' views of how well Child D was doing. Mr Myers says Child D was not doing well on respiration. He says Dr Bohin had 'revealed' 'distress' was a sign of air embolus, for the first time in the case.
Mr Myers refers to nurse Caroline Oakley's notes of skin discolouration for Child D at the time. He says there is nothing there to identify a discolouration that matches air embolus. He says in cross-examination, she began to give colours such as 'red-brown', and "ended up saying 'I remember an unusual rash'". He says Kathryn Percival-Ward [Calderbank] had said in 2018 police interview that [Child D] changed colour, was mottled, and had seen it before, but...it looked unusual'. He says her memory had developed by the trial, calling it a 'mosaic' and giving a more detailed description with 'oval markings meeting up with each other'. He says "five years later we have a lurid description". He says he is repeating himself by witnesses giving more detailed descriptions five years later. Mr Myers suggests staff had met up in the meantime to 'share recollections', and this 'almost certainly' happened. He says for Dr Bohin, there had been lengthy cross-examination on air embolus, and it went 'increasingly circular' and 'self-feeding'. He says Dr Bohin had said Child D had two non-fatal collapses by referring to research in dogs, pigs and rabbits, and the results were "variable". Mr Myers says those "vague assertions" does not give confidence as to what happened with Child D. He asks why the descriptions of discolourations vary each time, and why Child D was not seen to be in distress before the final collapse [having been in distress prior to an earlier collapse].
Mr Myers says doctors had agreed blood gas test results for Child D had declined - and Caroline Oakley agreed they "were not as good as they had earlier" on June 22, 2015, at 1.14am. He refers to the 3.45am note by Caroline Oakley: '[Child D] desaturated and then became apnoeic. Called SN Letby to help.' He says "yet again" Letby was being held responsible for an event where she did not have responsibility for that baby at that point. He says there is nothing linked to doing any harm. BM: "Again - what is meant to have happened?" He says the jury have to be sure of what.
He says there is "such a blunt point to be made": "We are looking at intentions to kill, from somebody whom the prosecution allege knows what they are doing [as it has already happened by this point, in their view]. "It's not going to take three goes is it? It would be one shot, sudden, and fatal." Mr Myers the suggestion Child D did not die of pneumonia, as opposed to with pneumonia, is "unrealistic". He says the case against Letby is "incoherent".
Child E
The trial is resuming after a short break.
Mr Myers is turning to the case of Child E. He says there is a lot of pressure with all these events, and it is traumatic for the parents of Child E. He says it is important to look at the evidence as objectively as the jurors can. He says the defence will look at the evidence of Child E's mother as 'sensitively' as they can.
He says it is important to note there was no post-mortem examination - "in this, of all cases", and that absence has 'allowed the prosecution to make all sorts of suggestions'. He says doctors failed to deal with a bleed for Child E which was identified or suspected at 10.10pm on August 3. Mr Myers says it was "obvious" a transfusion would be required. He says a further note by Dr David Harkness at 11pm recorded a further gastrointestinal blood loss. He says "even here, no action for a transfusion". He says it was "delayed a further 45 minutes". A female doctor said it was a "serious situation" at 10pm and a "very serious situation" by 11pm, and she agreed she wished she had got there sooner, as it was a medical emergency. He says this is "obviously sub-optimal care".
Mr Myers it may not have been anyone's fault that Child E was at the Countess, but Liverpool Women's was 'full'. He says it is "not extraordinary" that Child E became unwell, and one of the nurses suggested that stress could have caused acidosis and, as a consequence, bleeding. Mr Myers says Dr Bohin would not consider bleeding as a cause of death. He says he knows it is distressing to talk about, and Child E did bleed to death. He says "everybody here could see [Child E] needed a blood transfusion".
Mr Myers refers to the allegation Letby attacked Child E at 9pm. He says Child E's mother's account was she walked in and Letby was not near the incubator at the time. He says the prosecution's statement was a "highly charged" statement. He says "that is the evidence", that Letby was "not causing harm". He says he is sympathetic with Child E's mother. He says the prosecution have "done their best" to turn this "into a binary choice" - that 'either Lucy Letby is lying or [Child E's mother] is lying'. He says the prosecution have done that deliberately. He says the question is what degree of accuracy has each said. BM: "Perhaps can we take the heat out of that?"
Mr Myers recalls Child E's mother's statement. He says there is no basis for what happened here to the bleed later, as Dr Harkness reviewed Child E later and found him to be 'stable'. Mr Myers says the record of Child E's "horrendous" screaming, as recalled by Child E's mother - "cannot be like that". He says the unit would have been "full of people coming and going". He asks "how on earth" would that not raise the concerns of people nearby? He says it is "unrealistic" it can be "in the way she described".
Mr Myers recalls Child E's mother's statement on the 'bleed coming out of the mouth.' A description was made around the mouth and the chin. He says on cross-examination, it was "agreed it was not completely fresh". He says he suggested it could have been aspirate. The mother disagreed. Mr Myers says there is no suggestion by any doctor/nurse of Child E screaming. The neonatal schedule for Child E on August 3 is shown. He says Caroline Oakley is involved in giving medication to Child F at 9.13pm, with Child F 'being near Child E at the time'. Mr Myers says it isn't about lying, it is up to the jury to draw "a fair conclusion". He says no-one else had seen anything that coincides with this.
Mr Myers refers to the phone call at 9.11pm, and the defence say they don't doubt Child E's mother was distressed at that time. The defence suggest the details from the later phone call were moved to the earlier call, something which is not accepted by either parent. Mr Myers says Child E's mother spoke to the midwife, Susan Brooks, which was agreed evidence. The midwife notes: 'Care since 2000hrs...[Child E's mother] asked me to let her know of any contact overnight from NNU as one of the twins- had deteriorated slightly...' Mr Myers says this is the best, and maybe only, independent guide, for the event, and if the situation was more serious, it would have been noted as such.
Mr Myers refers to the expert witnesses' evidence. Dr Evans and Dr Bohin referred to Dr Harkness's description of discolouration as background for 'air embolus'. He says Dr Harkness gave more detailed descriptions in police interview and in evidence than he had in clinical notes, including the 'mobility' of the colours of the discolouration.
He says at the time of the collapse, no-one was seen interfering with Child E, and Dr Harkness said Child E 'collapsed in front of our faces'. He asks where the attack is supposed to have happened. Mr Myers says he is not going to go into detail of Child E's bleed after the collapse, "as it is awful". He says Dr Evans had said, in his third report, an NG tube being forced in was the cause of the bleed. He added that was withdrawn a few weeks before the start of the trial. Dr Evans said it was 'an option worth exploring' that a tube introducer had been used. Mr Myers says Dr Evans had taken up a role of investigator and hunting up ways to find a conviction. Mr Myers says Child E's bleed "ran out of control and he died". He says there is no post-mortem examination, and Letby is getting the blame, and no "realistic opportunity" of air embolus.
Wednesday 28th June 2023
Defence Closing Speech - Day 3
Chester Standard Live Reporting - 28th June 2023
Day 3
The courtroom at Manchester Crown Court is filling up. Lucy Letby has arrived, as has Benjamin Myers KC, who has been delivering the closing speech for the defence the past two days. The trial is now resuming.
Child F
Mr Myers refers to the case of Child F. He discusses the counts of insulin in general - for Child F and Child L. He says the prosecution referred to Letby's 'concessions' of the insulin results. He says the defence reject she has committed an offence for those two counts. He says the jury 'may well accept' the insulin results. He says it is insufficient to say Letby's concessions that the lab results are accurate when she cannot say otherwise. He says the defence can't test the results as they have long since been disposed of. He says the evidence at face value shows how the insulin results were obtained. He says it is not agreed evidence.
He says 'it seems', insulin continued throughout, and Letby 'cannot be held responsible for, realistically'. He says Letby was accused of adding insulin to bags already put up [for Child F], or 'spiking it three times' for Child L. He says these explanations are "contrived and artificial".
Mr Myers says a 'striking' matter that neither Child F or Child L "come close" to exhibiting serious symptoms as a result of high doses of insulin. Child F had a vomit. Child L "only ever seemed to be in good health", other than low blood sugar levels.
He says for Child F, if accurate, received exogenous insulin administered, according to the laboratory result. He says it was 12.25am when a TPN bag is put up for Child F by Letby and a colleague, and that was changed at noon by two other nurses as the cannula line had tissued. He says the lab sample came at a time when Letby was not on duty, and was after the second bag had been put up. Mr Myers says the readings of blood glucose found for Child F and Child L are not that different for their respective days, but the levels of insulin found in the lab sample differ [Child F had a reading of 4,659; Child L had a reading of 1,099]. He says Professor Peter Hindmarsh was asked to describe the signs of high insulin/low blood glucose. He said there was the potential for brain damage in low blood glucose levels. The other symptoms in serious cases include death of brain cells, seizures, coma, and even death. He says "fortunately", "neither of these babies" exhibited the serious symptoms. He says that is surprising if both babies had the high levels of insulin alleged.
Mr Myers says it is "a strange intent to kill" when the person with intent would know a remedy would be available - a solution of dextrose. He says Letby helped administer that dextrose. He says it is "interesting" the proseution did not ask doctors to rule them out of involvement with insulin. He adds he is not making an allegation.
He says there is "no evidence" Letby interfered with any TPN bag. He says the fridge is used by "all nurses" on the unit, and the "risk would be obvious" that someone could be caught interfering with a TPN bag. He says there are "lots of reasons" to show Letby would be noticed if she were to carry the act of administering insulin.
Mr Myers says the defence make the "obvious" explanation that there is nothing to say Letby exclusively was responsible for the insulin being in the bag. He says insulin continued to be given to Child F after Letby had left the unit, via a maintenance bag. He says it is "incredible" that Letby is held responsible for this.
Mr Myers says the evidence is the stock [replacement] bag must have been contaminated with insulin. He asks how can Letby can be responsible for that bag, as no-one could have foreseen it would have been needed? He says the first bag was replaced as the cannula line had tissued. He says it is like "Russian dolls of improbability". He says a TPN bag lasts 48 hours. He says there are a number of stock bags kept, not kept in any particular order. He says there is no evidence no other babies subsequently displayed symptoms of high insulin from the other bags. He says unless Letby had a "Nostradamus-like" ability to read the future, in the event of a targeted attack, a stock bag would not be contaminated with insulin on the off-chance it would be needed, and the bag was the one chosen 'at random' by a colleague.
Mr Myers says Letby believed she had a good relationship with Child E and Child F's mother. He says there is an entry in Letby's diary on Child E - the only entry for any child in the indictment in the 2015 diary. He says there is no entry for Child F. He says the photograph of the sympathy card for Child E's parents, taken by Letby at the hospital, has no relevance. Mr Myers says it was a photo taken while she was at work.
Child G
Mr Myers refers to the case of Child G, for which there are three allegations. He recalls the key events during her care at the Countess of Chester Hospital's neonatal unit in September 2015. Mr Myers says there are many areas to this case which are "upsetting", and the brain injury Child G sustained is "deeply upsetting- heartbreaking". He says whatever emotions that may be felt as a result, that does not establish what Letby is alleged to have done.
Mr Myers says the case against Letby - the allegations - are "weak", and "demonstrate shortcomings in this case". He says it is "shameful" that Letby was being blamed for the monitor being off on one of Child G's incidents, and it was only from one of the nurse's accounts in evidence that showed it was not the case.
Mr Myers says Child G was very premature, and her transport to the Countess of Chester Hospital was delayed as she had an event where she desaturated to 42%. He said there were also events of blood-stained secretions and an event described in the notes at Arrowe Park as a "pulmonary haemhorrhage". He says for 2.15am on September 7, the allegation is Letby force-fed Child G. He says there is no evidence she did so.
The trial is resuming after a short break.
Mr Myers says Dr Evans and Dr Bohin, before the trial, said air and milk had been forced down the NG Tube, and that a colleague of Letby had aspirated Child G's stomach before the 45ml feed [ie the stomach was 'pretty much empty']. He says that was the assumption. He says the assumption was wrong. The nurse said she would have taken enough aspirate to assess the pH level of the stomach, but not enough to empty the stomach. She had said that would have been done with bigger babies who were stable. He says the evidence "all falls apart". He says the nurse said there could have been undigested milk in there. He says this "created a fundamental problem for the experts". He says the defence was critical of how the allegation "morphs", and focused on the description of the pH level. He says the judge, Mr Justice James Goss, asked about that, and the nurse replied the pH level would not give an indication of how much milk was in the stomach. Mr Myers says Dr Evans and Dr Bohin said low pH levels meant acid, and no milk in the stomach, and had "changed their lines of attack". Dr Bohin was "particularly vigorous" about it, saying pH of 4 was "very acidic" and milk would "neutralise" that reading. Mr Myers says the nurse "did not get that wrong". He says in the case of Child P, there can be a low pH reading with a lot of milk in the stomach. He says 14ml of milk was aspirated, and a pH reading of 3, and a later reading gives 20ml aspirate and a pH reading of 3.
Mr Myers says Child G's CRP rating [a test to diagnose conditions which cause inflammation] had risen in the 24 hours after the projectile vomit, from 1 to 218. He says that is a sign Child G was developing an infection. He says what Letby is alleged to have done is "incredibly speculative".
He says there are "vanishing amounts of time" for Letby to have done what she is alleged to have done, given how long the 2am feed takes to be administered and how long Letby had been with colleague Ailsa Simpson before they were both called over for the projectile vomiting incident at 2.15am.
Mr Myers refers to the 6.05am 'profound desaturation' for Child G. 'NG aspirated as abdo appeared v large, ~100mls aspirated'. He says the presumption of guilt is Letby did this. Dr Alison Ventress had said, in cross-examination, this was most likely to be air. He says Dr Stephen Brearey first gave evidence in the trial at this point. He said he "assumed it was fluid". Mr Myers says that is "extraordinary" and there's "no basis" for that.
The note also refers to 'ETT removed at 0610. Thick secretions++ in mouth. Blood clot at end of ETT...Reintubated at 0615'. Mr Myers says Child G was not getting air in due to a blood clot. He says Alison Ventress had agreed in cross-examination the blood clot had interfered with the ETT. Dr Bohin had agreed, in evidence, blood clots can cause a desaturation, when describing a desaturation event for Child G on a different occasion. Mr Myers says there was a failure to ventilate Child G for hours.
Mr Myers refers to the second event for Child G on September 21, 'At 1015 x2 large projectile milky vomits....desaturation to 35% with colour loss. NG Tube aspirated - 30mls undigested milk discarded.' He says if Letby is alleged to have attempted to kill Child G, 'what a thing to put it in a nursing note'. He asks where the 'document fraud', or 'cooking the notes' is. He says it is "an incredibly weak basis" that the only two events of milky vomits on September 7 and September 21 are suspcious. Mr Myers says "we don't know" how much of the 45ml feed at 6am is still in the stomach by the time of the following feed. He says for September 21, Child G recovered quickly, unlike the September 7 event.
Mr Myers says, for the allegation Letby 'cooked the notes', he refers to Child G's temperature reading on the observation chart, that there are 'two dots' on the 9am reading. He says there are multiple dots recorded on other hours on the same chart by other nurses. He adds the dots are both in the 'white' area [ie normal]. He says it is "not a good point".
Mr Myers adds Child G had a further projectile vomit on October 15, when Letby was not on duty. He refers to the third event for Child G, the second on September 21, 2015. He says the prosecution opening in October last year said somebody had switched off the monitor. He says it was the evidence of a nursing colleague who said what did happen. He said the nurse recalled there had been seven attempts to insert a cannula. Mr Myers says that could have caused a desaturation for Child G. Mr Myers said the nurse's "crystal clear evidence" said the doctors left Child G behind screens and the monitor was switched off. He says Dr John Gibbs had said if that was what the nurse had said, then that was what had happened. Dr David Harkness said he could not recall. Mr Myers says it was "very poor treatment" for Child G.
Child H
Mr Myers refers to the case of Child H. He describes the events for Child H, including the insertion of chest drains. He says the evidence reveals "serial, sub-optimal care" and "no evidence" of Letby "doing any wrongdoing at all", but "she gets the blame". Mr Myers says late provision of surfactant would have made the pneumothorax worse for Child H, as Dr Bohin said. He says Dr Bohin also wrote in her report there was an "unacceptable delay" in intubating, and leaving a butterfly needle in the chest was 'sub-optimal practice as it is hazardous'.
He adds there was a delay in inserting the second chest drain, and Child H had not been sedated. He says the issue of the 'moving second chest drain' is "hotly contested". Highlighting the 'sub-optimal care', Mr Myers says there is "a very good reason" why babies got better when transported to a tertiary centre, and it 'wasn't because of Lucy Letby'.
The trial is now resuming following its lunch break.
Mr Myers says it occurs to him they are halfway through the material, and appreciates it is very detailed. He says it is important and necessary to go through the detail. He continues with the case of Child H. He says the defence suggests a 'build-up' of what had gone on, and a poorly positioned chest drain, caused the collapse at 3.15am, after a third chest drain was put in. He said it must have been "a huge stress on a baby".
Mr Myers says the second chest drain "may be another aspect of poor care". He says it was put in the 'wrong position' for Child H by Dr Jayaram. Two x-rays are shown. He says Dr Bohin accepted, in cross-examination, that the position of the chest drain was not in accordance with guidelines. She said the position of the tip was sub-optimal. Mr Myers says the tip also moved around. A number of x-ray images for Child H are shown for the positions of the chest drain tip. He says it is shown to have moved, and says the tips of the other ones had not.
Professor Owen Arthurs was asked, Mr Myers said, about the position of the tip of the needle [from a radiograph image for Child H on September 26, 2015], and whether it was touching the heart. He replied he could not tell - it could be several centimetres away, it could be touching. A doctor wrote for Child H on September 26: 'Possible cause for cardiac arrest could be that a drain is too close to heart and touching pericardium...' A nursing note: 'At 16.21 [Child H] started to desaturate, no air entry heard, ET Tube suctioned and help summoned from colleague. Crash call... 'Second chest drain noted to be in a different position and 'holes' close to chest wall. Further tegerderm applied and chest drain tubing position altered. Both chest drains bubbling ++ during reintubation...' Mr Myers says the chest drain was "not well secured and this can't be blamed" on Letby. He says a desaturation to 56% at 7pm 'should be included in the list of events, but this wouldn't fit as Letby isn't on it'.
Mr Myers says the key event for Child H happens at 3.20am, hours after the parents left before midnight. He refers to the second event, the following night, in which he says Letby has "no opportunity to be involved in this". He says Child H had a 'profound desat' at 2030 and a further 45% desaturation at 2145. He says the 'profound desaturation to 40%' at 0055 is the one Letby is blamed for, "randomly". There is also a desaturation at 0330, which Letby is not linked with. Mr Myers says the desaturation at 12.55am is part of a series Child H had been going through that night. Mr Myers said no cause was identified for the collapse of Child H. He says there were "very serious failings in care".
Child I
Mr Myers refers to the case of Child I, which he says has a lot of detail to it. He says Child I was very small and "fragile" and "capable of deteriorating from almost nothing". He says this was evidence heard from her time in Liverpool. He says nurses would talk of Child I 'having a big tummy', and Dr Bohin agreed there were multiple occasions noted of a distended abdomen. He says Child I regularly presented as "mottled".
Mr Myers refers to an event of 'abdominal distention' on August 23, which experts had agreed was 'consistent of harm', but is not on the sequence of events and Letby was not on duty. He says there is an 18-hour period from September 5-6 where Child I deteriorated from being a well baby, to the point she was transferred to Arrowe Park Hospital. Mr Myers says it shows how quick Child I could deteriorate, and "she was not doing well".
He says, for the first event [that Letby is charged with], the cause of the collapse on September 30 was said by Dr Evans and Dr Bohin to be air down the NG Tube. Mr Myers says this is the event with Letby's note which the prosecution took issue, that there was 'no doctor review', and she was 'lying about a fictional review at 1500'. He says the agreed evidence by Child I's mother said she was changing Child I's nappy when a nurse she later found to be Letby said Child I's stomach appeared swollen. In a second statement by Child I's mother, she said the first time she saw Letby was 3pm, and remembered Letby 'I'll go and get the doctor to come and check her.' The mother said she agreed, and a female doctor went and checked Child I.
Mr Myers says for the 4pm event, Letby calls for the doctors "in good time", and 'that is all'. He says for 7.30pm, nurse Bernadette Butterworth had said Child I's air in the tummy increased from Neopuffing, and that can push the diaphragm up. He says breathing support can cause abdominal distention, and that can be applied from as little as Neopuffing.
He says for the second event of Child I, this event is the 'what could Lucy Letby see or not see?' He says one of the issues in this case, staffing experience levels are a factor. He says Letby had said nurse Ashleigh Hudson was 'quite inexperienced'. He says Child I was on antibiotics up to a few hours before the collapse, not 48 hours as the prosecution had said. He says as there are no heart rate or respiration observations being recorded, it could not be said how stable Child I was before the collapse.
The trial is resuming following a short break.
Mr Myers says Ashleigh Hudson had been away from nursery room 2 'for about 15 minutes', and when she comes back, no-one is in the nursery. He says Letby is in the doorway of 'a small room'. He says there was 'certainly enough light' for nurse Hudson to feed Child I. He says she 'embarked on a lighting reconstruction' five years later, with the lighting level 'made for the purpose of this investigation'. He says the light would be 'so dark' to 'put the milk in the bottle'. He says Nicola Dennison said the babies were arranged so you can look at them. He says the defence case is that is at odds with what Ashleigh Hudson had given.
Mr Myers says Letby had, in cross-examination, said she had more experience what she was 'looking for - at.' He says this was the fifth day of cross-exmanation, when Letby was increasingly tired and finding it difficult to concentrate. He says there is no meaningful difference between the words 'for' and 'at'. He adds room 2 has a window between the corridor and the nursery. He says it is "unrealistic" to say the room was "impossible" to look in and see babies.
Mr Myers asks what evidence there is for air embolus, as there was no NG Tube. He says Dr Bohin relied upon discolouration of sternum. He says extensive CPR took place on Child I after this collapse, and there was bruising as a result. Mr Myers says there is no clear basis as to what have happened, unless someone had used a 'mobile NG Tube in the most improbable of circumstances'.
Mr Myers says abdominal distention is a running theme for Child I, and while that does not mean harm was not done, it does not alone form the basis of an intent to kill. He says: "we keep having incidents where Letby isn't doing anything she shouldn't do". He says the defence are critical of the theory of air down the NG Tube. He says it is a theory that has been done to support the prosecution. He asks how much air is needed, and how long it takes.
He says for the final event, there are two signficant desaturations, one just before midnight, seen by Ashleigh Hudson, who is not sure why. He says there is a similar event at 1.06am the following morning, on October 23, when Child I does not recover and dies at 2.30am. He says the difference with the latter is Lucy Letby is there. He asks what the difference is between the two events. He says Child I was a very poorly baby before this night, and Child I "would have been under terrible stress".
Mr Myers says Dr John Gibbs noted: 'Poor response to second resuscitation might have been to heart being compromised by previous...collapses'. He says the evidence was the abdomen became distended in response to the first collapse, as Ashleigh Hudson had noted the 'abdo soft' at 23.57pm. A radiograph after the collapse showed a distended abdomen. He says Dr Evans and Dr Bohin 'made a lot' of Child I's crying at the time. He says the experts had worked this symptom in during the course of their evidence as a sign of air embolus. He asks whether there was supposed to be an air embolus at 11.57pm, at 1.06am, or both.
Mr Myers asks about the allegation Letby amended a time on a document: "So what?" He asks about the relevance of it. He asks what is meant to establish that it was done deliberately, rather than a mistake.
He refers to the sympathy card Letby had sent for the parents of Child I, a photo of which was taken while she was at work. He says another photo was taken of a card she had sent to some friends. He says it had been heard this was something she did. He said the sympathy card was sent as she could not go to the funeral of Child I. Mr Myers says evidence had been heard by Lucy Beebe saying Letby was 'crying' after the death of Child I, saying: 'Why is it always me?' He says that was a genuine response by her.
Thursday 29th June 2023
Defence Closing Speech - Day 4
Chester Standard Live Reporting - 29th June 2023
Day 4
The trial is due to resume at 10.30am.
Benjamin Myers KC, for Letby's defence, will continue giving the closing speech for a fourth day. He has previously told the jury his speech will last five days.The trial judge, Mr Justice James Goss, says to accommodate timetabling issues, the court will be sitting until 3pm today. To make up for lost time, the lunch break will be shorter than usual, and the court will begin at 10am on Friday.
Child J
Mr Myers refers to the case of Child J, and outlines the events which happened to the baby girl in November 2015, and what is alleged. He says Child J's mother is "a fairly neutral witness on this topic". He says she said she drew comparisons betwen the care at Alder Hey Children's Hospital and the Countess of Chester Hospital, and the latter was 'not favourable'. She says the staff at the Countess relied on them to sort stoma care. She says they were left to "feel unwelcome", and asked about that, she said she felt their concerns "were not treated seriously". She says the staff there "did not have the same confidence and ability" in dealing with stoma bags. Mr Myers says this statement is used as the basis for their argument that the Countess was receiving too many babies with complex needs.
Mr Myers says the mother had said the concerns were met with "pushback". He says nurses, including Nicola Dennison and Mary Griffiths, had said dealing with stoma bags was "unusual", and Dr John Gibbs said it was a "challenge".
He says this case is evidence "beyond doubt" that serious deteriorations can come out of nowhere, as there are two desaturations for Child J, a well baby generally, which are serious and "cannot be blamed on Lucy Letby". Dr Kalyilil Verghese had considered the first was a 'false desaturation'. Mr Myers says Nicola Dennison had given evidence to say the first "serious desaturation" is a real one "which comes out of nowhere", with Child J desaturating to the 30s [of oxygen saturation levels]. He says Dr Stephen Brearey said he could not find a cause for those two desaturations, and agreed they were unexpected. Mr Myers says it is "clear unfairness" that the latter desaturations, when Letby is present, are an allegation of harm, as opposed to the first two desaturations when Letby is not present. He says there is "no evidence" that can be linked for Letby causing harm to Child J.
Mr Myers says the experts do not identify any physical harm for Child J. He says Letby is being left to explain something for which she probably wasn't present for. He says Dr Dewi Evans, when cross-examined, could not rule out infection in his report. He says this is not attempted murder, and the prosecution case is "empty".
Child K
He turns to the case of Child K. He outlines the events and allegation. He says the allegation "illustrates a good deal wrong with this case". He says Child K "should not have been at the Countess of Chester Hospital", but should have been treated at a tertiary unit. He says arrangements were being made post-birth. He says a review carried out at Arrowe Park Hospital said care at the Countess was "sub-optimal". He says the defence acknowledge there is a question whether transporting the mother before birth was possible. He says Child K should have received surfactant.
Mr Myers says Child K was a tiny baby needing complex care. He says Dr James Smith agreed in cross-evidence that an experienced neonatalogist at a tertiary unit would have had more experience than him in looking after babies such as Child K. A mortality review at Arrowe Park Hospital said Child K's death was "avoidable", Mr Myers says. He says surfactant, to allow babies to breathe properly, should have been administered "straight away" to Child K. He says Child K could not breathe without assistance and it was "inevitable" she would need intubation. He says the "air leak" recorded "cannot be ignored". He says staff at the Countess "did not seem concerned". He says the defence acknowledge the oxygen saturation was high. He says a tertiary unit consultant had said the pressure [VTE reading] was "too low" and the oxygen saturation reading was "not consistent" with the air leak and pressure readings.
Mr Myers says the count is Letby "deliberately did nothing to help" when confronted by Dr Ravi Jayaram, and that by implication, she had harmed Child K. He says Letby did not recall what had happened. He says the allegation "relies on the credibility and reliability" of Dr Jayaram. He says the allegation had "morphed" against Letby. He says tubes can dislodge. He says Dr Sandie Bohin agreed tubes can dislodge even if a baby is sedated. He adds nurse Joanne Williams said Child K was an "active baby".
Mr Myers says Dr Jayaram had said Child K was sedated, and that was "a prime basis for blaming" Letby. He says Child K was not sedated until after the tube was dislodged and she was reintubated.
Mr Myers says Letby's presence on the unit allows the prosecution to "say what you like". He says if it is alleged she was 'caught in the act' by Dr Jayaram, she would not have gone back to dislodge the tube twice more the same morning, as is alleged by the prosecution. He says if Dr Jayaram had seen things in the way he told them, he would not have taken his eyes off Letby for the rest of the shift. "He would have been watching her like a hawk". He says the allegation is "not worthy of belief". He asks why Dr Jayaram, if he had seen what he had said, did not contact the police or 'whistleblow', or file a Datix report. He said he did "nothing".
Mr Myers says nurse Joanne Williams recalled Dr Jayaram had asked her what had happened, and who was in the room when the alarms went off. He asks why Dr Jayaram would ask her that if he had been in the room at the time, seeing Letby in there. He refers to a note on the transport team: "Call received from Dr Jayaram baby dislodged the tube and had to be re-intubated".
Child L
Mr Myers refers to the case of Child L. He says it is the second of the two insulin counts, where Child L had low blood sugar for a period of 53 hours, as identified by Professor Peter Hindmarsh. He says the laboratory result, if accurate, shows artificial insulin administered exgoneously.
Mr Myers says Letby was seeing friends, going on holiday, enjoying salsa, a win at the Grand National. He says it is important to keep in mind the person who these allegations are aimed at. He says at this time, her main concern was moving house "and this was on her mind". Text messages are shown to the court showing conversations with Letby about her new home in Chester, having been at hospital residence.
Mr Myers says it is important to consider each count separately. He says it is not accepted Letby has committed this offence. He says there was a delay in getting the sample taken from Child L sorted, and was outside the 30-minute guidance, whether it was taken at noon or 3.45pm. He says the Countess of Chester Hospital Pathology department records the lab specimen report notes it was received at 6.26pm. He says Dr Anthony Ukoh says the sample was taken at noon.
Mr Myers says nurse Mary Griffiths had said there was a delay in podding the blood sample due to what happened with Child M. He says it is a "point of contention" that the delay in processing the sample is "one thing to keep in mind" when processing the results. He says apart from the "apparently" low blood sugar level, there was no ill effect observed on Child L, which he says is "extraordinary". He asks how that is evidence of poisoning. He says the blood sugar level reading in the sample, was 2.8, a "relatively healthy reading". would be inconsistent with the insulin and insulin c-peptide. Professor Hindmarsh said it was a plasma reading, so would give a different blood sugar level reading than a heel prick, and it was said it would be more like '2.4'. He says the heel prick tests showed a blood sugar level reading of 1.6 at noon. The ones at 3pm and 4pm are 1.5. He says it does raise a question on the accuracy of the blood sugar readings.
The trial is resuming after a short break.
Mr Myers says there was one detail he had omitted before the break. He says at 3.40pm, bolus of 10% dextrose was administered for Child L. He says the prosecution says that would account for the higher blood glucose reading. He says the problem of a 1.5 [heel prick] reading at 4pm still remains, as does the 3pm 1.5 reading. He says it is difficult to work out what effect it would have.
He says Letby cannot have interfered with the bags in the way it is alleged. He says the bags are changed during the 53 hours Child L was recorded to have low blood sugar readings, during which five bags were used. He says a number of bag changes took place for which Letby was not involved in. He says the prosecution alleged Letby was 'setting up an issue' of hypoglycaemia for Child L. He says it does not follow as Child L would be a focus on blood sugar levels, and someone with harmful intent would not identify an issue that was going to be detected anyway. He says Letby would be drawing attention to it. He says Child L's designated nurse was recorded on the neonatal schedule as being a co-signer for 9.25am-9.29am prescriptions. He says that is when the electronic prescriptions are inputted. He says Dr Ukoh would also be in room 1 that morning (where Child L and Child M are) as part of his ward round. He says there is no record of him outside of room 1 during the time Letby was alleged by the prosecution to administer insulin in Child L [about 9.30am].
Mr Myers says the theory Letby spiked the various bags with insulin is "contrived and arfiticial", and the mechanics of it are "unrealistic". He asks how Letby could predict to add insulin to the dextrose bags in storage, which would be used for all babies on the unit, only for Child L. He says the theory of 'sticky insulin' is "mixed". He says there is a lot of bag changes over 56 hours. Prof Hindmarsh was cross-examined about it, if the 'sticky insulin' would run out at some point. He said it would. He said over time, additional insulin would be required to maintain the levels [of low blood sugar levels].
Mr Myers says whatever the reason for Letby accumulating paperwork [at home] in the case of Child L, it does not provide sufficient evidence of an intent to harm the baby.
Mr Myers says Letby subsequently cared for Child L after April 9-11, and it is "utterly inconsistent" with someone wanting to target that child to harm or kill them.
Child M
Mr Myers refers to the case of Child M, and outlines the events that took place. He says it was established he was in a corner of room 1 on April 9, which "wasn't ideal" as the unit was busy. He says Letby was "doing nothing" to harm Child M, and had participated in giving antibiotics 15 minutes prior. He says Dr Evans and Dr Sandie Bohin had worked in a theory of how slowly air embolus could take effect. He says that theory is "unbelievable".
Mr Myers said Letby, on April 9, had other babies to look after that day, with their own issues. He refers to a note by Mary Griffith on April 9 for Child M to say there was an underlying problem prior to the 4pm collapse. He says by 3pm, Child M was made nil by mouth, and says it can be argued that was 'not a great direction of travel for him'. He says if it is accepted that the 4pm event is a signficant escalation, it does not show Letby caused harm at that time.
The trial is now resuming after its lunch break.
Mr Myers is continuing to deliver the closing speech in the case of Child M. He says air embolus was the mechanism proposed by medical experts as the reason for collapse. He says Dr Evans and Dr Bohin referred to discolouration. He says the only witness for that was Dr Jayaram. He says the description is not made in the contemporaneous notes, as they were not there for Child A.
Mr Myers says none of the other staff, including Dr Ukoh, give a discolouration description for Child M. He says Child M did make a good recovery, gradually, from the collapse. He says the significant issue is Letby's last contact with Child M is when she is involved with administering antibiotics at 3.45pm, and if air has been administered at that time, he says it would not take 15-16 minutes to have effect. He says air embolus is fast acting. He says the amount of air alleged to be administered in this case is 0.5ml. He says if there was an intention to kill, it would have been larger. He asks how someone would measure 0.5ml or calculate it. He says even a minute quantity would have a quick impact. He says fortunately, neither twin of Child L or Child M appeared to have suffered harm as a consequence. He says the theory of air embolus is "utterly unrealistic" for Child M.
Child N
Mr Myers refers to the case of Child N, for which there are three counts alleged against Lucy Letby. He outlines the events for Child N, who had haemophilia. Mr Myers says Professor Sally Kinsey said Child N was more likely to suffer a bleed from trauma than babies who do not have haemophilia, and the amount of blood would be larger. Prof Kinsey had said the process of instrumentation had the potential to cause bleeding, such as a naso-gastric tube. Mr Myers says the Countess of Chester Hospital did not have Factor 8 for Child N at birth. He says for the first Child N event, for which it is alleged there was trauma and/or an air embolus, he asks if Letby was even there.
Mr Myers refers to Dr Jennifer Loughanne's note for the Child N event - 'asked to see - desat - unsettled - got upset - looked mottled, dusky, sats [down to 40%] [moved to] 100% O2 'On my arrival, 40% O2, screaming'. Mr Myers says it is "plainly not an air embolus", disagreeing with Dr Evans. He says Dr Bohin said it was a painful stimulus. He said there was no sign of injury or blood.
Mr Myers says both experts put "poor opinions" forward. He refers to the first event of June 15, 2016, in the morning, at 7.15am. He says there is no evidence of anyone seeing Letby coming in and causing harm to Child N. He says the prosecution created the narrative Child N was sabotaged in advance the previous night by Letby before she left at the end of her shift. He refers to nurse Jennifer Jones-Key's note for the June 14-15 shift. He says in evidence, Jennifer Jones-Key said Child N first deteriorated at 1am, and remained at that condition through the rest of the night. Mr Myers says that "is an end to the sabotage theory", as Child N became unwell several hours into that night shift.
Mr Myers says Dr Bohin did not accept that from 1am to 7.15am, there had been a gradual process of deterioration. He refers to the 7.15am event. He says Jennifer Jones-Key referred to more desaturations 'from 7am'. He say she remembered being in the nursery, feeding a baby, and Letby came in for her shift, and Letby came into the nursery, the alarm sounds, and Letby walks over. He says there is "no indication or sensible opportunity" for Letby to cause this collapse for Child N. He says it is a continuation of the "mounting problems" for Child N which began at 1am.
Mr Myers says there is a question for when the blood is seen on Child N, before or after intubation. He says it is hard to see that if the attack happened at 7.15am, that blood would only be seen by a doctor at 8.05am. Mr Myers says it would be "reckless" if a doctor embarked on intubation for Child N while seeing there was blood in the way.
Mr Myers refers to the third count for Child N, later in the day at 2.56pm on June 15, 2016. He says the details of the event are clear, and while most of the five or six doctors described swelling, 'only' Dr Satyanarayana Saladi noted blood. He says it is right that a 3ml blood aspirate is collected. He says the defence observe it's surprising, given Child N's haemophilia, there is not more. He says it is "unclear" what the cause of the swelling is, and could be a consequence of what had gone on that morning.
Mr Myers says there are no signs of a wound found on Child N, and he was "well inspected" by doctors. He says at 7.40pm, Child N desaturated when medical personnel arrived to transport him, and he was prepared for theatre as doctors had been unable to intubate. Mr Myers says it was not surprising Child N's condition was poor given the 'long day' he had had. He says a tertiary unit doctor was able to intubate first time successfully after Child N's desaturation. Alder Hey consultant anaesthetist Dr Francis Potter was asked to give evidence. Mr Myers said he had told the court his interest was paediatric intensive care, and he had experience with airway problem resolution. He said the intubation was managed with 'relative ease'. He said Dr Potter had been "surprised" there had been difficulties in intubating Child N as he said the Countess of Chester Hospital team was "pretty competent". He says Dr Bohin "comes to the rescue [of the prosecution]" by not agreeing with the opinion of Dr Potter. He said Dr Bohin said the drugs given to Child N would have reduced the swelling. He said it was a disagreement between the two prosecution witnesses.
Child O
Mr Myers says he will begin the case of Child O in the remaining 10 minutes [to be continued tomorrow]. He outlines the events for Child O. Child O was one of three triplet brothers - Child P being another of the triplets. Mr Myers says he will start with June 22-23, for the night shift with designated nurse Sophie Ellis. The final note 'Abdo looks full slightly loopy. Appeared uncomfortable after feed.Reg Mayberry reviewed. abdo soft, does not appear in any discomfort on examination.' He says an examination took place, but no note was made by Dr Mayberry He asks why Letby is blamed for Child N being unwell at 1am after Letby had finished at 8pm the previous night, whereas for Child O Letby is blamed for Child O being unwell at 1pm when Child O had been unwell at 8am. He asks why there was no record of a doctor's examination after Sophie Ellis had noted a doctor reviewed Child O, when Letby was blamed for noting a doctor review for Child I when there was no record of a doctor's examination.
Friday 30th June 2023
Defence Closing Speech - Day 5
Child O cont.
Mr Myers is on his feet, he's continuing to take the jury back over the evidence for triplet brother Child O.
The court heard he was stable up until 23 June 2016, when he suffered a "remarkable deterioration", he stabilised but later suffered a further fatal collapse. Mr Myers says the explanation of the experts - that there was an assault which resulted in a trauma to the liver and air embolus - is 'confusing'. He invites the jury to consider 'how, where and when' this things happened. He said it's 'very unclear'. Mr Myers says the prosecution has not identified a time or place where these alleged offences took place.
Mr Myers has pulled up the neonatal review - which has been pulled together by police analysts and is a timeline of events - it shows that Child O was given medicines by two other nurses at 14:39. Ms Letby is seen as doing an infusion at 14:40, just before the collapse
Mr Myers notes the door swipe data which shows Ms Letby only arrived at 14:39 on the unit. He drills deeper into the clinical notes which show Child O collapsed at 14:40 and then Ms Letby, on instruction from a doctor, began an infusion in response at 14:40 ie after the event Mr Myers says 'it's important to keep this in mind, the suggestion has been made that at 14:40 somehow Ms Letby was involved in what took place before the collapse, she was not'
Mr Myers picks up on the evidence of an independent pathologist, who reviewed the case. He said the boy suffered an "impact injury" akin to a road traffic collision - which caused bruising on his liver Mr Myers says 'the truth is' we 'don't know' how much force it took to make those bruises. He says the pathologist picked 'graphic examples' but cannot say how 'little force' it would take to cause those injuries in a neonate The barrister says it is a 'possibility' that the bruising was a result of CPR during the failed resuscitation attempts on Child O
Mr Myers is pulling up messages sent between Ms Letby and a doctor who cannot be named on 1 July 2016. They were talking about the events surrounding Child O's collapse The doctor tells Ms Letby that one of his doctor colleagues was 'was upset' as the boy's liver issue 'may have been cause by her chest compressions'. He said he had to reassure the doctor for 20minutes Mr Myers says this 'raises the possibility that injury can be caused by CPR, plainly this was something she was concerned about'. He invites the jury to keep this in mind
Mr Myers notes that the prosecution have made much of Ms Letby's Facebook searches for the parents of Child O. He says 'nothing about those' searches establishes guilt and says 'how is that meant to indicate she had done something to harm' him
Child P
Mr Myers now turns to Child O's triplet brother, Child P. At 09:35 BST on 24 June 2016, a registrar found he was "self-ventilating in air" and stable, but 15 minutes later, he collapsed and required breathing support. He collapsed several more times, before being pronounced dead at 16:00. A medical expert for the prosecution said the collapses were consistent with an "additional amount of air being given to this baby"
Mr Myers says this case is another example of the Crown trying to 'shunt blame Ms Letby's way', he says the management of Child P's care was 'poor'. He notes that the baby had a pneumothorax and a X-ray which would have shown this was delayed Mr Myers says Child P's 'death was in all likelihood a consequence of poor medical procedure' after his 09:40 collapse. He says this case is 'a prime opportunity to hide poor performance and bad outcomes' and blame Ms Letby
A registrar Dr Ukoh recorded that at 09:35 on 24 June that Child P was self-ventilating in air. 15 minutes later, he suffered an acute deterioration at 09:50 hrs. Mr Myers says the Crown's case is that at some point between 09:35 and 09:50 Ms Letby injected the child with air He says 'whatever has happened, there is no opportunity' for Ms Letby to do this and says given the cast of doctors and nurses in the room it is implausible in the extreme
Mr Myers is taking the jury back over medical notes for Child P from the early hours of 24 June. He says they show the 'direction of travel', he says he was nil by mouth at this time. The senior nurse on duty said the child's abdomen appeared distended at 04:00 Mr Myers is going over the evidence for Child P final and fatal collapse when medics were waiting on a transport team from Arrowe Park to take him. A doctor who cannot be named recalled Ms Letby saying 'he's not going to leave here alive is he' The doctor gave a vivid account of how she felt this was inappropriate and that Child P had just had a good gas was okay. But Mr Myers has said the clinical evidence shows Child P had an undiagnosed pneumothorax He also notes that the doctor had said by this stage she was aware of rumours about Ms Letby - but he said 'there’s not even a datix report, not in the notes, no complaint, no issue raised about' what Ms Letby is alleged to have said
Mr Myers says the evidence does show the child was unwell and the doctor, in charge of his care, 'felt out of her depth' - she said in evidence how she was counting down the minutes waiting for the transport team to take him Mr Myers says if Ms Letby did make the remark alleged it may have been out of 'social awkwardness' and does not prove murder He says the allegation here against Ms Letby is 'utterly implausible'. He also cites the fact a senior doctor was seen by the mother of Child P 'googling' how to insert a chest drain - he says that is 'indicative of the level of care at the Countess of Chester'
Child Q
Mr Myers is now on Child Q - the last child on this indictment. He was born in late June 2016 and was "initially stable" after his birth, but jurors heard he deteriorated and needed breathing support shortly after 09:00 on 25 June. The prosecution said Ms Letby injected air and fluid into the boy's stomach via a nasogastric tube. A medical expert for the prosecution said vomit found on Child Q was evidence that liquid had been given to him and his respiratory problems were likely caused by the fluid
Mr Myers says there's 'no evidence of her having done anything at all' to cause Child Q's collapse Mr Myers says the clinical evidence is 'consistent with early stage Necrotising enterocolitis (NEC)' - this is a serious condition that can affect newborn babies Mr Myers says 'what an earth is (Ms Letby) meant to have done, there's no evidence of an attack'
Final section
We're back after a break. Mr Myers is now on the final section of his defence closing speech
Mr Myers thanks the jury for their attention to the evidence. He says it 'isn’t difficult for someone to pick up one item or another and give prominence to one or another depending on which position you're coming from' 'The decision on what evidence is important and where it takes the case is for you', he says He warns of the dangers in this case of 'emotion, suspicion and judging Ms Letby by standards that are not applied to anybody else, unrealistic standards, there's a reliance on the fact she was on the unit as proof for far more than that fact can possibly amount to'
Mr Myers says the consultants who have accused Ms Letby 'are not neutral' he says they are 'deeply involved in what happens, we say at times they have said things deliberately to prejudice Ms Letby's position' He also says the experts - in particular Dr Dewi Evans - are 'highly partisan'
Mr Myers says 'we say there were terrible failings in care on that unit that has nothing to do with Lucy Letby' He notes that 'between June 2015 and June 2016 the neonatal unit at the Countess of Chester took more babies than it would usually care for and took babies with greater care needs' He said 'in that same year there was an increase in the number of deaths and the types of collapses we're looking at in this trial, those two facts are connected we would say' 'What didn’t change was Lucy Letby, she had been a neonatal nurse for years, she was dedicated, she cared for hundreds of babies, she suddenly didn’t change her behaviour in 2015, what changed was the babies on the unit and inability of this unit to cope'
Ms Letby appears to be crying in the dock as Mr Myers continues to wrap up his closing speech.
He says 'it is easy to lose sight of the reality of the person at centre of this' and asks the jury not to focus on the 'picture conjured' by the Crown of the nurse Mr Myers invites the jury to 'apply a presumption of innocence and not a a presumption of guilt, if you do that you will reach the right verdicts, verdicts of not guilt and those are the verdicts we ask you to return'.
That completes the defence closing speech.
Monday 3rd July 2023
Judge's Summing Up - Day 1
Background - Children A, B & CChester Standard Live Reporting
10:26am: The trial is now resuming. The judge, Mr Justice James Goss, is beginning his summing up. He says the prosecution case is there was deliberate harm at the Countess of Chester Hospital neonatal unit, sometimes repeated attempts on the same infants, and some of those babies died. He says after Child O and Child P died, and Child Q collapsed on successive days in June 2016, Lucy Letby was confined to clerical duties.
10:29am: He reminds the jury of the background to the offences alleged on the indictment. He says the Countess of Chester Hospital is, and was, busy. He says the jury are now familiar with the tertiary system of hospitals, with the Countess a level 2 unit, routinely providing care to babies of 27+ weeks gestation. The jury have been provided with a guide, and walkthrough recordings, of the unit. One room, 'room one', the ICU room, had four incubators and two computers plus other pieces of equipment. Room two was the HDU, rooms three and four were special care babies rooms.
10:31am: He says the last evidence heard was from Lorenzo Mansutti, an experienced plumber at the Countess of Chester Hospital. The Women's and Children's building was built in the 1960s and there were issues with the plumbing, and there was an incident between 2015-2016 where the hand basin backed up with foul water. There was another incident where room 4's floor flooded after a back-up sink overflowed. None of the incidents reported happened on the days when the alleged offences took place.
10:34am: Consultant Dr John Gibbs had said in evidence it would have been better if there were more consultants, but refused to say the staffing level at the time compromised the care of neonatal infants. He says every year, up to 2015, the number of deaths at the neonatal unit was within the number to be expected, and less than the national average. Between 2015-2016, the number of deaths "increased significantly", including the number of "unusual" events. The defence said this was a consquence of higher admissions and a higher number of infants with more complex needs.
10:37am: In evidence, Letby was asked about her relationship with other staff. She said she had "no problem or issue" with any of the doctors and had a "normal working relationship" with them "at the time", except for one female doctor she did not get on that well with. She said she "loved one [male] doctor as a friend", but there was no loving relationship between the the two. She later said four doctors had "conspired against her falsely" - Dr Stephen Breary, Dr Ravi Jayaram, Dr John Gibbs and one other.
10:40am: The judge says the evidence given by witnesses behind screens, or from remote locations on videolinks, should not be diminished in any way. He adds their evidence should be judged in the same way as any other witness in the case. He says established BAPM 'gold standard' guidelines had one designated nurse to one ICU baby, one nurse to two HDU babies, and one nurse to four special care babies. He says nursing notes would be written retrospectively on computers. They had an accurate electonic timing of the start and completion of the note.
10:44am: He says nurses were asked about staffing levels. The court had heard from one nurse: "Sometimes there were more babies [on the unit] than there were meant to be". 2015-2016 "was a busy period" with more babies with higher acuity. Staff "were giving up breaks" to provide care. "It was always quite busy," said another nurse. Dr Stephen Breary accepted nursing levels were lower than the gold standard guidelines. He added their levels were similar to other neonatal units, and staffing levels were better than those around Cheshire units. The court heard the other units did not have the mortality levels.
10:48am: The judge says the jury should consider if sub-optimal care was a factor in the collapses of the babies. He says in a few cases, it is accepted there was sub-optimal care. He said Letby accepted herself that sub-optimal care played little or no part in most of the babies' cases. He says [defence barrister] Benjamin Myers KC repeatedly suggested that doctors "had gone out of their way" to "damage" the defendant by blaming her for sub-optimal failures in care. He says she "did nothing to harm any baby". He says it is up to the jury to find who is telling the truth and who is "reliable". He adds he is not going to put a single document up for the jury to look at, as they have all the documents.
10:51am: He says in two cases, two babies received insulin when it was "wholly inappropriate" to do so. Each of them - Child F, Child L - was a twin. He says the prosecution say there is "no doubt" it was added intentionally. He says the prosecution say the chances of more than one person acting in that way [administering insulin] is not realistic. He adds the defence invite the jury to question the samples, and the "lack of harm" caused by the infants if they had been poisoned by insulin. He says the prosecution say the intention was "endangering the lives" of the two babies.
10:55am: The judge says the prosecution referred to a list of reoccurring factors for babies in the case. He says for the defence, they say Letby was a committed, hard-working nurse, and if there was someone intent on harming children, it was not her. The judge now gives the background to Letby, starting as a nurse at the Countess of Chester Hospital in 2012 as a band 5 nurse. The court had heard Letby "always strived to go on every course she could". In March/April 2015, Letby had completed a six-month course - including a placement at Liverpool Women's Hospital - she qualified in the speciality of caring for intensive care babies. She was the only band 5 nurse [along with colleague Bernadette Butterworth] to have that qualification.
11:02am: The judge says Letby has no previous convictions. He says it is entirely for the jury to attach the weight of the defendant's previous character. Letby had said she had cared for hundreds of babies, and that hurting a baby was completely against everything a nurse is. Colleague Christopher Booth "confirmed" she was "conscientious, hard-working, and willing to help", and another colleague said Letby would "remain friends" with the parents of babies on Facebook. Eirian Powell said Letby was "an exceptionally good nurse". Letby had a "passion" for working in the intensive care side, and "staff knew" she enjoyed that side of care. The judge says Letby's health was good, and she did not take time off work in 2015-2016. She was "flexible", living at Ash House [accommodation at the Countess], then at a flat between 2014-2015, then back to Ash House until April 6, 2016, to Westbourne Road, Chester. Letby was "often asked to do more" than the required number of shifts per month. She was "devastated" when taken off clinical duties in 2016. She had "prided herself" on being very competent. Letby registered a grievance in September 2016. It was at that time she learned she was being blamed for the deaths, and that that was "sickening", and her mental health "deteriorated". She was arrested at her home in July 2018. She was interviewed, then moved to Hereford to be with her parents. A search was conducted of her Chester home.
11:06am: The arrest "traumatised" Letby, she said. A defence statement was confirmed by her on February 11, 2022. The judge says some of it differs from the police interviews. He refers to his next legal direction, on the defence statement. He says if the jury find "a material difference" between the two statements, the jury are entitled to ask themselves why. He says the defence say the task was made more difficult by the delays in bringing the case, and the volume of evidence served. He says if the jury are sure there is a 'material difference', and they do not believe the defandant is telling the truth on the reason for those differences, then that should be in support of the prosecution case. He says the jury must not convict on the basis of those changes alone.
11:08am: The judge refers to delays in the case. He says the jury should take into account the passage of time since the events, and the impact that might have on the witnesses and the defendant in recalling them.
11:15am: The judge refers to expert witnesses who have given evidence in the case. He says the jury would expect to hear evidence from experts with relevant expertise. Their role is to be a witness, not an advocate. He says the defence have criticised that evidence, and will come to that when going through the relevant cases. He says the jury are entitled to consider their opinions when coming to conclusions on the case. It is up to them to consider some or all of their evidence. He says their evidence is part of the case, and the jury should not consider it in isolation, and should be considered in the context of expert, clinical and relevant circumstantial evidence. The experts did exclude some reasons for collapses based on their own knowledge and expertise.
11:17am: He says he will turn to the relevant cases. He says the material is dense, and is conscious of the circumstances in which they happened, and does not intend to be insensitive. He reminds the jury of his initial direction for the jury to treat the case on the evidence, not on emotion. He adds he is conscious the jury has already heard nine days of closing speeches.
11:22am: He refers to the case of Child A - the twin of Child B. He recalls the events of their birth and the collapse. Child A's cause of death was "unascertained". The prosecution case is Child A did not die of any natural cause, but instead had air deliberately injected intravenously system with the intention to kill. The defence say Letby did nothing to harm Child A, and raised issues with the long line.
11:35am: The judge details what neonatal unit staff were recorded, and recalled, doing for Child A before the collapse. He says there were issues siting a cannula "as can happen". A long line was later inserted by registrar Dr David Harkness. Nurse Melanie Taylor came on duty. Child A was "stable and satisfactory", and the nurse "had no concerns". She ended her shift at 8pm, and handed over to the defendant, who had come in at 7.27pm. She confirmed a 10% dextrose bag had been prescribed, to be given via the long line. All three babies that night in room 1 required long lines - Child A, Child B and one other. Dr Harkness was unsure if the long line was in the perfect position. He believed it was "imperfect", but good enough to be used. Dr Dewi Evans said the position was not a problem, and there was no evidence of the end of the line puncturing the heart lining. He said if there was, it would show up on a post-mortem examination. Dr Sandie Bohin said it was "not in an optimal position" but "safe to use". Melanie Taylor said she was sitting at the computer in room 1 when Child A started to deteriorate. The alarms sounded, and Melanie Taylor went over, thinking the baby was going to recover. She said Letby was administering Neopuff. She says it "was a bit of a blur". Letby said she was not initially intending to work that night shift, but was "happy to help" after being asked to work. "There was a lot going on", and she said Melanie Taylor, "being the sterile nurse", was administering fluids. Child A's hands and feet were "white" at the time of the desaturation - 'centrally pale and poor perfusion'. An emergency crash call was put out.
11:42am: Dr Rachel Lambie had said Child A 'looked like Child B', pale and blotchy all over. The defence said her original police statement referred to Child A being pale, with white hands. She thought there was a "lot of discussion" over the rashes. She said no-one had told her what to say on them. The defence "draw your attention" to the difference, the judge says. The judge's next legal direction is on differences in evidential statements. He says what a witness says in the witness box is all evidence for consideration. He says where there are, or appear to be, differences in accounts, it is for the jury to decide how different those accounts are, and how important they are. He says if there are important differences, they should consider them, and the explanations given. He says if the jury do not accept their explanations, they should treat the witness' evidence with caution. If the explanations are accepted, then the evidence can be treated as such. He says it is "really no more than a common-sense approach" "to see where the truth lies".
11:48am: Dr Harkness had given a description of the 'blotchy' rash, saying it was only seen again by him in the case of Child E. The defence criticised him for not including the description in medical notes at the time or in notes to the coroner. Dr Ravi Jayaram had said it was "highly unusual" in the way that Child A was deteriorating and his heart rate fell even after intubation. At the time, he noted Child A's pale skin. His explanation for not including the 'pink patches' skin discolouration to the coroner - mentioning it to the police later - was "he had not considered it clinically relevant" at the time. He said it was "a matter of regret" he had not mentioned them. He says he could not explain how Child A collapsed. He said he read a document in a medical paper about skin discolouration in a case of air embolus. He said he had not been influenced by that paper when it came to that explanation.
12:14pm: The trial is resuming after a short break. The judge is continuing the summing up, in the case of Child A. He recalls what Letby had said in police interview, and recalled 'red, purple blotchy markings' on Child A, which she thought were signs of an infection. She believed there was an issue with the long line, and Melanie Taylor had connected the fluids to Child A. Child A's death was not expected or anticipated. She said she thought the bag of fluid was 'not what they thought it was', but they had checked it afterwards. She said she did not keep in touch with the parents, and did not recall what she did with the handover notes. She said she did not know much about air embolisms, and all staff were "meticulous" about precautionary checks to prevent that happening. She denied pushing air through the line. She could not recall using social media to search for the mother of Child A, and when asked to explain searches for the mother on Facebook, said she could not do so. Letby said the fluid bag should be contained and put in the sluice room for checking. She said staffing levels conntributed to the death of Child A, citing difficulties with the long line and Child A's lack of fluids for several hours. She said if air embolus was the cause, Melanie Taylor was responsible. She disagreed with the descriptions of skin discolouration given by a nursing colleague and Dr Harkness. She said searching for the parents was a "common pattern of behaviour" for her.
12:25pm: The judge says Mr Myers "repeatedly expressed his opinions" on the merits of the expert evidence, questioning and challenging them. He says that is his right, but it is up to the jury to determine the reliability of the expert evidence. The judge refers to Prof Owen Arthurs' evidence, who "considered each case on its own merits". Prof Arthurs was provided with radiograph images of Child A. He noted the umbilical catheter was "slightly in the wrong place", and there was "a line of gas in front of the spine" on one of the images, which was "an unusual finding". He said it was "so unusual", he reviewed other cases at Great Ormond Street Hospital, to compare for a similar images. He said such gas would normally only be seen in heavy impacts such as road traffic incidents - this could obviously be discounted. The other usual case would be "overwhelming infection" in organs of the body, such as sepsis, but Child A did not have any such identifiers. He said he had "not seen this much gas" in any baby, other than in the case of Child D. He said it was 'consistent with air administered' to him, but 'not diagnostic' of it. In cross-examination, he said he found no unexplained cases, and accepted this was an observational study, not a controlled study - the judge says for obvious reasons, the latter could not be carried out. 0
12:29pm: Prof Arthurs said radiographic evidence of air embolus was "rare", and in suspected cases, seeing anything on the radiograph was "rare". He said the absence of it on the radiograph did not rule that cause out. He said one of the reasons is the imaging of the event is not important, the main priority is to save the life. An x-ray taken an hour later "wouldn't show anything".
12:41pm: The judge refers to expert witness Dr Andreas Marnerides' evidence. His expertise, the court is told, is on the pathology of conditions on those who had died. He said there was "no evidence of infection" or "any other abnormalities". He said he could see, from his study, "empty structures" of fat or air in Child A - after testing, he ruled out the former. He said he could see evidence of air in the brain when the baby was alive. The findings "could not be taken as absolute proof of air embolus". He said there was "no evidence of any natural cause of death", or any of natural disease. He took the view that Child A's death was of air embolus via injection. 0
12:54pm: The judge refers to Dr Dewi Evans, and his role in providing background evidence for Child A. He said: "On the whole, babies don't suddenly collapse". He said Child A was the fifth case he looked at, and the cause of the collapse was "unusual". He said as he looked at further cases, he noticed a "pattern", as he received more evidence. He said Dr Evans' evidence came for criticism by the defence. He had not been in practice since 2009, and the defence said he had "constructed theories" and "acted as an investigator" and was "biased", " putting himself forward...at the outset". The judge says the prosecution point to a large number of incidents for review with "no apparent reasons for an event or death". They point to Dr Evans' long experience in neonatalogy, and provided "clear evidence" in Child F and Child L that identified two babies on the unit were being poisoned. The prosecution say Dr Evans was not handed other potentially incriminating evidence, such as shift patterns for staff. Dr Evans said Child A was "stable" and "as well as could be expected" before the collapse. Repeated attempts to insert a UVC or long line may have caused upset to Child A, but would not have caused the collapse, he said. The lack of fluids "would not make a material difference". 'Bright pink' skin discolouration would be unusual in a baby's collapse - but skin discolouration is "not diagnostic" of an air embolus alone, Dr Evans said. He denied he had been "influenced" in reaching his conclusion by a 1989 medical paper. He said in Child A's case, there had been colour change, sudden and unexpected collapse, air in various parts of the body, and no explanation for death. He said it was probably an air embolus intravenously.
1:02pm: The judge refers to Dr Sandie Bohin, and her evidence for Child A. He says the defence accused her of lacking independence, and "enthusiastically supported" Dr Evans' evidence. She repeatedly denied this assertions, and said her views were her own. The judge says it is up to the jury to assess the validity of the defence's assertions. Dr Bohin said neither the UVC or long line contributed to Child A's collapse. She said Child A was "so well", that there was consideration to giving him feeds, and babies doing well do not develop pink fluctuating rashes that come and go. She said, excluding other possibilities, air embolus was the "only plausible explanation", and believed air getting in accidentally "was extremely unlikely". Studies on air emboli should be "treated with caution" as they are on adults or animals, she said. In cross-examination, she said she did not know of any genetic condition that would cause a collapse and death within 24 hours of birth.
2:14pm: The trial is resuming following its lunch break. The judge describes Prof Sally Kinsey's evidence, in which she had concluded, from the descriptions by dctors and nurses of skin discolouration, that Child A had had an air embolus. The court had been told of how an air embolus affects the body. She confirmed she had not seen one in her experience, but the descriptions provided were "pretty stark". The judge turns to the case of Child B, and relays the care and events leading up to and the time of her collapse.
2:22pm: A nurse colleague said she had her gloves on, and was drawing up medication, when Child B collapsed at 12.30am. Letby had said Child B was apnoeic [not breathing]. The nurse said Child B 'looked like Child A', with blotchy discolouration; a 'cyanosed appearance' was recorded in the nursing notes. The notes added the colour changed rapidly, to "purple blotches with white patches." Letby said she had accepted being in room 1 at the time of the collapse. She said the colleague had alerted her to Child B's collapse. Child B had a 'dark mottling', a 'general mottling'. Child B was 'more purple' and she did not see what the nursing colleague had seen. Letby had accepted she would have had access to the IV lines prior to the collapses of Child A and Child B, but said she did not do anything with them. Letby, in police interview, said Child B's mottling 'purple, red, rash-like appearance' was more extensive than with Child A, but was "similar". She recalled Child A and Child B's parents being very upset. She said, in a 2019 police interview, she accepted she may have taken blood gas readings prior to the collapse, but did not do anything to harm Child B. In a 2020 police interview, she said she did not know how Child B collapsed.
2:27pm: Dr Rachel Lambie said the most unusual observation for Child B was a 'dusky, pale grey colour - then developing widespread blotches of a purple/red colour - they would flush up, then disappear, then appear elsewhere - they were flitting all over'. It took about 90 minutes for the grey colour to disappear and be replaced by pink, she added. She said this "was a very unusual event" which she had not seen before or since, and Child B recovered quickly. Blood gas results came back as normal. Letby said she had been asked to get a camera to get a photo of Child B, but when she had returned, the discolouration had gone. A female doctor recalled 'purple blotching to the mid-right abdomen and right hand', which she was "puzzled" by. The rash was "so florid" and "so very unusual", she said, and its quick disappearance was not normal.
2:33pm: Dr Evans said Child B was "stable" prior to the collapse, and prone to desaturations. The collapse was either the result of smothering or air embolus. He said if the cause was hypoxia or infection, the effects would stay. He said the fact Child B survived meant it was likely less air was administered, or it was administered more slowly. Dr Bohin said Child B was compromised at birth, but responded very well to resuscitation and breathing support measures. The circumstances of the collapse was "very disturbing" and there were no other warning signs. The disodging of the nasal prongs for Child B had been resolved. She based her air embolus conclusion on 'florid' skin colour changes and ruling out other causes. The defence say it cannot be excluded that Child B's collapse was a natural event.
2:36pm: The judge refers to the case of Child C. He says medical experts found it difficult to conclude the cause of death, but Dr Marnerides said it was air administered into his stomach via the naso-gastric tube. Letby said she did nothing harmful to Child C, and a cause such as a gastrointestinal blockage cannot be excluded, that Child C should have been treated at a tertiary unit, and there was a failure to react to bile aspirates, vomiting, and an overall lack of care.
2:47pm: Child C was "born in good condition" and was 'on the margins' of being treated at the Level 2 Countess of Chester Hospital neonatal unit, the jury is told. The judge recalls the events leading up to Child C's death on the morning of June 14. "Nothing stood out as worrying" for Child C from observations, but there was caution for his care. Prof Arthurs said radiographs for June 12 showed left-sided chest infection, and marked dilation of the bowel. Symptoms of this included CPAP belly, NEC, sepsis or air embolus. Bile was later noted on Child C's blanket on June 13, and 2ml of black-stained fluid was obtained on aspirates. No desaturations were observed. Bile aspirates was a "concern" in neonates, but not that unusual for them, and "not a major cause of concern", the court had heard. Dr Gibbs said the bile for Child C was "a worry", but the aspirates "were not increasing", and "his overall observations were satisfactory". An obstruction would have been found post-mortem.
2:52pm: "Black bile was not normal, but not unknown in premature babies", the court had been told. Dr Sally Ogden said the bilous observations were a "concern", and the x-ray showed a "loopy bowel". Child C was still pink and well perfused and he had "no concerns with breathing" and the abdomen was soft to touch, which was "reassuring". Dr Gibbs had "no particular concerns" about Child C that day on June 13. Babies with [gastrointestinal disease] NEC develop a hardened abdomen, the jury was told.
3:06pm: Messages showed Letby wanted to 'throw myself back in' to the neonatal unit - She said that meant getting back in to looking after babies as that was what she was taught at Liverpool Women's. The messages included Letby saying: "From a confidence point of view, I need to take an ITU baby soon." Sophie Ellis, a band 5 nurse - not intensive care unit trained - was supported by a band 6 nurse that night shift to be the designated nurse for Child C that night in room 1. At the start of the night shift, there was a hope to start Child C on feeds. He was "pink, well perfused, active and alert". At 10.34pm, Letby said she had 'done a couple of meds in 1', and believed Sophie Ellis didn't have the skill in caring for premature babies. Sophie Ellis was alerted to Child C's desaturation. She said she had been alerted to the desaturation by Letby, who had said 'he's just dropped his HR and saturations'. This was something she had not put in the nursing notes, but something she said to police. She said she did not do so at the time as it was ultimately a traumatic event. She said she didn't do anything to Child C, and didn't see anything being done to him. Letby was "stood at the incubator at the far side". A nursing colleague said she believed she saw Melanie Taylor and Sophie Ellis by Child C. Child C was not breathing, "very blotchy", and was not aware if Letby was in the room. Melanie Taylor said in evidence when she approached the incubator, Letby was already there. She said in police interview, she was in room 1 feeding another baby, and was called over by Sophie Ellis, not mentioning Letby. Letby said she had "very little independent memory" of events. She said she had given evidence on Child C's collapse having been "placed" there in the room by Sophie Ellis' account.
3:17pm: The trial is resuming after a short break. The judge says we will finish before 4pm, at the conclusion of the case of Child C. The case of Child D will be referred to tomorrow.
3:27pm: Dr Gibbs said efforts to intubate were unsuccessful due to swollen vocal cords. Sophie Ellis said she got upset at the situation, after Child C's mother arrived, as it was "overwhelming" and she had not been in that kind of situation before. Lucy Letby said to her: "Do you want me to take over?" Sophie Ellis said yes, left room 1 for a short break, then went to look after babies in room 2. Dr Katherine Davis said "even the smallest, sickest babies" would respond to resuscitation, but Child C did not. Dr Gibbs said he could not find anything that would allow to restart long after resuscitation had stopped, and could not understand that from a natural disease process. The mother said, in an agreed statement, she recalled CPR being performed on Child C, and the heart rate had fallen unexpectedly and rapidly. She says she did not grasp the gravity of the situation and was shocked when asked by a nurse if she wanted a priest. She asked if Child C was going to die - the nurse, described to be in her mid 20s, replied "Yes, I think so". The father of Child C said a nurse, who he later believed to be Letby [based on her picture appearing in the newspaper] had said to the parents in the family room 'you've said your goodbyes now, do you want to put him in here?', referring to a basket for Child C. He said Child C's mother said "He's not dead yet", and the nurse then backtracked. Letby had accepted she had made searches for Child C's parents on Facebook 10 hours after, but could not remember doing so, or why. She questioned whether she was the nurse who said the 'you've said your goodbyes...' comment, and did not recall saying it. She said she was very sad for the parents. In evidence, she said she did not recall any specific contact with the parents. She said the search for the parents were as they were 'very much on her mind' at that time, as 'you don't forget' events like those which had happened to Child C.
3:35pm: The nursing colleague recalled asking Letby "more than once" to look after her designated babies that night, and it was not part of her responsibilities to be in the family room, as that was for Melanie Taylor. Dr George Kokai carried out a post-mortem examination for Child C. He noted a distended colon, which Dr Marnerides said was "not an abnormality". He said the potential complication was a twisted colon that would lead to "obvious" symptoms of pain. There was evidence of "acute pneumonia". Dr Marnerides said one could die of pneumonia or with penumonia. He said the former was plausible, but upon hearing further clinical evidence, he reviewed his opinion. He said babies dying of penumonia experience gradual deterioration, which was not the case here. He said he revisited the cause of death, viewing images of a distended stomach, and no evidence of NEC. Prof Arthurs said the small bowel was dilated. Dr Marnerides observed a dilated stomach and bowel, and noted Child C had been off CPAP for over 12 hours. No air had been obtained from aspirates before the collapse. He had never known CPAP belly being the cause of an arrest in a baby in his years of experience. He said, in his opinion, the cause of Child C's collapse was of excessive air administered into the stomach via the naso-gastric tube.
3:44pm: The judge says Dr Evans said the pneumonia infection did not cause Child C's collapse. The cause was "difficult to explain". Initially, he said it was unexplained. He said excessive air in the stomach can cause 'splinting of the diaphragm'. The judge he had not given that conclusion before giving evidence, and it was not advanced in his eight reports. Dr Evans denied he was 'coming up with things now to support an allegation of harm'. Dr Evans said from an academic point of view, air embolus could not be excluded. The judge says Mr Myers was critical of this late conclusion. Dr Bohin had said her conclusion of the 'bubble in the stomach' was if the NGT was not on free drainage, then it could have been accumulation of gas by CPAP. The alternative was the deliberate administration of air via the NGT. She said Child C died with pneumonia, but not because of pneumonia, and that would have made Child C less responsive to resuscitation. In reaction to questions about bowel obstructions, she said Child C would have had a distended abdomen, and normal bowel sounds would not have been heard. The judge said Dr Bohin had added: "There were no clinical indicators of obstruction".
Tuesday 4th July 2023
Judge's Summing Up - Day 2
Children D, E, F & GChester Standard Live Reporting
10:30am: The trial is now resuming.
10:41am: The trial judge turns to the case of Child D. He recalls the baby girl's birth, and that she died 36 hours later on June 22, 2015. The prosecution's case is air was administered intravenously. He says the guideline was for Child D to be given antibiotics at birth, due to the gestational age, and this had not been done. The prosecution said while Child D died with pneumonia, not of pneumonia. The defence said you cannot be sure of that, and the cause could have been infection. Dr Sandie Bohin said Child D should have been screened at birth due to her low temperature, which was a sign of infection. Child D was placed on CPAP. Her heart sounds and capillary refill were normal, abdomen was soft and non-distended, and the chest was clear. The parents were informed it was likely sepsis. Child D stabilised on CPAP.
10:44am: Child D was intubated and ventilated, after showing signs of acidosis. An x-ray showed 'very little abnormal', according to Professor Owen Arthurs. Child D was given the protein surfactant. Child D was weened off the ventilator and extubated. Dr Elizabeth Newby said Child D was a little stiff and hard to handle, and felt there was an element of infection. Dr Bohin said Child D had signs of pneumonia, but was recovering.
10:47am: Child D's mother recalled an event when she arrived on the unit and Letby was 'hovering round [Child D], not doing much, holding a clipboard', and she asked if everything was ok. Letby replied everything was "fine". The mother added: "She just stuck around". The mother said Letby was told to go away, or words to that effect. Child D's father did not recall this event. He recalled he was given a Father's Day card on June 21 by the staff. He said nurses were "friendly and warm" and was made to feel welcome when he went to the unit.
10:51am: Prof Arthurs said a radiograph of Child D from the afternoon of June 21 showed the catheter was in the wrong position, and there was a sign of infection, but nowhere near as prevelent as that seen for Child C. Child D showed 'big improvements' and 'good progress' on June 21 in relation to blood tests and respiratory efforts, although she was 'not stable enough' to have a lumbar puncture. She was 'responding well' and her tone was reasonable. Child D desaturated to the 80s when attempts were made to take her off CPAP. Dr Sarah Rylance was 'happy' with Child D's clinical condition by this stage, 'stable and making good progress'.
11:02am: The judge says shift leader and designated nurse for Child D in room 1 on June 21-22, was Caroline Oakley. Letby was designated nurse for two other babies in room 1. Child D was on 'nasal CPAP in air', with 'satisfactory' gases. The readings for 7.30pm-12.30am were all normal and she was 'happy' with Child D, who was "breathing beautifully in air". Aspirates found had 'minimal importance to them' as Child D was not being fed at this time. Caroline Oakley said she assumed she began an infusion at 1.25am, being the designated nurse, but the writing on the infusion note was not hers. One of the nurses on duty was aware Caroline Oakley had been on her break, and checked Child D, who was fine. While she was at her computer, she was alerted to alarms, and found the monitor was showing Child D was desaturating at 1.30am. She recalled Letby was there. She noted Child D had a rash on her trunk and arms, and was 'not a normal rash' - like a 'mosaic', like 'vessels of blood meeting with each other'. She had not seen anything like it before, she said. She said 'her trunk and legs went a mottling colour, and it was odd'. She discussed it with Dr Andrew Brunton. Child D settled and discolouration 'seemed to disappear and dissipate'. Caroline Oakley said the rash was 'different to mottling' and it was 'an unusual rash'. She "had an episode but responded very quickly". Another senior nurse said she had a limited memory of events. she remembered Child D being stiff and having a rash on her trunk, which was an 'odd, unusual rash'.
11:11am: The judge says at 3am, there was a second event. Caroline Oakley said Child D was crying and desaturating, and the skin was discoloured, but less than before. Dr Brunton recalled Child was agitated and upset, and thought it was something to do with the face mask. He saw skin discolouration, but this was 'not as obvious' as before. A prescribed saline bolus was signed for Child D at 3.20am by Caroline Oakley and Lucy Letby. Nurse Oakley said they were happy with Child D, and she would be provided with expressed breast milk. She said if Child D was unstable, she would not have changed Child D's nappy. Observations were 'fine' by 3.30am. At 3.45am, Child D's monitor was alarming. Caroline Oakley found Child D had stopped breathing and was apnoeic. Dr Emily Thomas heard the call for help. She asked a nurse to put out a crash call for Dr Brunton. He ran when he was crash called. Full resuscitation was carried out on Child D with the assistance of doctors and nurses, including Lucy Letby. There were 'secretions+++' from the nose and mouth. The parents were informed and went to the unit. After 28 minutes of resuscitation attempts, it was decided to stop. At 4.50am, Dr Newby had a discussion with Child D's parents on the 'sudden collapse'. She agreed babies can suddenly collapse, but was "surprised" Child D did. She "did not appear to be a baby in extremis". A nurse had a conversation with Lucy Letby about the drugs administered during resuscitation. Letby asked the nurse how she knew the doses to give. The nurse replied she knew them from her years of experience, and recommended Letby learn them as well.
11:25am: Dr Andreas Marnerides said pneumonia was likely to be present at birth for Child D. Professor Arthurs talked of a 'black line' in front of the spine indicating gas in the great vessels, which was "unusual" in children who had died without an explanation. It was present in "two other children", one of whom was Child A. There was "more air" in Child D than Child A. One explanation was someone was injecting air into the child, and the radiograph images were consistent with, but not diagnostic of, externally administered air to Child D. Dr Marnerides said the presence of air in such a vessel was "significant". He said from a pathology point of view, air embolus could not be proved. He said there was "no other natural disease" that could explain Child D's death. He said in his opinion, Child D died with, not from, pneumonia. He concluded the 'likely explanation' was air embolus. Dr Dewi Evans said the 1.30am episode was "very surprising and unusual" as Child D had been responding to treatment and was "a stable baby". He said Child D had symptoms of early onset pneumonia and had developed that before birth, but was making a recovery. He said he could not think of any events which would end with unsuccessful resuscitation, and the cause was an air embolus. Dr Bohin peer-reviewed Dr Evans' reports and conclusions. She said the striking feature of all events was they were sudden and unexpected, and came with mottling of the skin. She said it was a concern that Child D was crying in the second event. She said although antibiotics were given late, there was nothing, clinically, to suggest Child D was going to collapse. "This was not a picture of a baby with pneumonia severe enough" to collapse. She was "clear" infection did not cause the "sudden" collapse. There were episodes of discolouration which was consistent with the limited recorded events of air embolus. She concluded air had been administered intravenously, causing an air embolus.
11:28am: The judge says Lisa Walker, a band 4 nurse, talked about an event of being in room 3 - a special care unit - where Letby was feeding babies via a naso-gastric tube. The alarm on the portable monitor was going off - the desaturation alarm. Lisa Walker went over to help. Letby stopped the feed and began stimulation for the baby, but was not getting a response. She saw colleague Kate Bissell walking past, and shouted for help as the baby was not picking up. A doctor working on a computer went over to help. The baby was given gentle stimulation and picked up. Lisa Walker said Letby asked her, "quite firmly", why she asked for help. She said Letby was "quite cross" and the band 4 nurse didn't respond. She said Letby's demeanour was that she would have been fine and didn't need any help.
11:32am: Letby, in police interview, denied doing anything deliberately harmful to Child D. She said she could not remember doing Facebook searches for the parents of Child D three days after Child D's death. She said she could not recall why she said Child looked like having 'overwhelming sepsis' or that there was 'an element of fate' in babies. In evidence, Letby said she "didn't really remember" the night shift. She said she would have been caring for her designated babies and assisting colleagues with other babies. She did not remember being called in to room 1 at 1.25am, Child D desaturating at 3am or Child D collapsing at 3.45am.
11:33am: The trial judge refers to the case of twin boys Child E and Child F, dealing with Child E first.
11:39am: Both twins were born "in good condition", the jury is told. Child E died less than six days later. The court had been told Child E was very premature. A doctor agreed Child E was capable of dramatic changes in his condition. The day after Child E was born, the mother went to cuddle Child E, as he was on CPAP. On July 30, the boys were 'progressing really well', and due to a high blood glucose level, Child E was given a low dose of insulin. The twins were 'doing well' and stable on August 1, with time out of his incubator. On the day of August 3, a nurse said the mother was on the unit with long periods of skin-to-skin contact, and Child E could have 'as many cuddles' as he liked. Child E was 'pink and well perfused' with regular circulatory system and a cautious feeding regime. "Everything remained well". Intravenous caffeine was given as prescribed.
11:50am: The trial is now resuming after a short break.
11:56am: The judge says Dr Emily Thomas said she had examined Child E and there were no signs he was unwell, and observations were normal, with a soft, non-distended abdomen and no suspicious aspirates. He was "well and stable". A nurse noted Child E's blood sugar was higher than normal, and his insulin infusion was restarted at a lower dose. Antibiotics were given as prescribed. A doctor said the observations were normal and not a cause for concern, and the high blood sugar level was relatively normal for a neonate and would not lead to the sort of collapse seen hours later.
12:06pm: Child E's mother recalled giving cares to Child E, then going upstairs to provide milk between 7pm-8.30pm, the latter being the time of the night shift handover. Letby was the designated nurse for Child E and Child F in room 1. Letby said the 9pm feed was omitted because of 16ml mucky, bile-stained aspirate, discarded, and the SHO was informed, and told to omit the feed. She said the doctor's name was not always made on nursing notes. She accepted she got '15ml fresh blood' from Child E at 10pm. She denied she had got Belinda Williamson [Simcock] to write in the 10pm entry. Dr Christopher Wood was the on-call SHO and was asked if he recalled receiving a call about an aspirate. He said he didn't recall it, and didn't definitely rule it out. He said if he had received a call, he would make his assessment, and make it in clinical notes, and seek advice from a registrar. Dr David Harkness said it was his recollection that during the review, there was a fresh blood vomit and 14ml aspirate. He says there was a discussion with a doctor about a blood transfusion.
12:18pm: Child E's mother recalled going to see Child E and Child F, at 9pm. Letby was there at the workstation, the mother said. She added child E was crying like nothing before - 'horrendous', and saw 'blood coming out of his mouth'. It was 'not on, or going on to anything else', 'like a dribble pattern - it was blood'. "It was smudged, and didn't look completely dry, it was darker [than normal]." The mother said she was panicking and asked Letby why Child E was bleeding, She said Letby said the NGT had been rubbing at the back of the throat. Letby did not recall saying this. In cross-examination, she said she did not tell the mother and would not tell parents to go away. She accepted that in the interview for Child N, she had said an NGT could cause bleeding. The mother said she accepted what Letby had said, and did as she was told to go back to the post-natal ward as Letby was an authority figure, but she was concerned. She said she made a call to Child E's father. The judge refers to phone call data at 9.11pm. The father said the mother was upset at the time of this call. Midwife Susan Brookes recalled Child E's mother had said to let her know if there were updates overnight from the unit, as one of the twins 'had deteriorated slightly'. She had recalled at 11.30pm the neonatal unit rang to bring Child E's mother to the unit in 30 minutes, as Child E had a bleed. Letby said in police interview, she could not recall the events with Child E's mother, and could not remember any specific bleed. She said the 14ml bleed later, after 10pm, was "very concerning" and, in evidence, that was when she said she first saw bleeding on Child E. The judge says there are "significant conflicts" between Letby's evidence and that of the parents. He says the defence say the mother's evidence is "unreliable" in relation to timings.
12:30pm: The judge says Dr David Harkness noted, at 11.40pm, Child E had a desaturation, with colour changes on the abdomen - "a strange pattern over the tummy which didn't fit with poor perfusion" The legs and upper arms were 'pink in normal colour'. he said the only other time he had seen this was with Child A, and not since. The patches were 1-2cm big, and he carried out an emergency intubation. Letby said there was a 'purple block' on the abdomen for Child E at 11.40pm. She said it was not like Dr Harkness had described. She said she found Child E's death "very traumatic", and filed a Datix form. She said the medical team were late administering a blood transfusion. The defence challenged the decision not to give a blood transfusion earlier. A doctor had said she did not believe the collapse was due to blood loss, and that blood transfusion had its risks. She said she did not believe, "even with hindsight", Child E should have had a blood transfusion at that point. The mother had contact with Letby after Child E died. She said Letby bathed Child E. In Letby's evidence, she said the parents bathed Child E. A doctor said at the time, she believed Child E had died of NEC, and that a post-mortem examination would not tell the parents any more, and would delay their transfer back home. She had said NEC was the most likely cause of the gastro-intestinal bleed. No post-mortem examination was carried out. She completely agreed, that with hindsight, she should have requested a post-mortem examination. She apologised to the parents for not pushing for that, having wanted to avoid further distress for them. Letby said in messaging with Jennifer Jones-Key, in response to the unit being 'on a terrible run', that Child E had a haemhorrhage, and could have happened to anyone. She said the searches for the parents of Child E and Child F more than once on Facebook was part of a normal pattern of behaviour for her, as was taking a picture of the card for the parents. She said it was something for her to remember, as was a photo of her shift pattern.
12:44pm: The judge says Prof Arthurs said there was no evidence on the radiograph image for Child E of an air embolus, but that did not exclude it may have happened. He said there were no features of NEC on the x-ray. Professor Sally Kinsey said Child E did not have a blood clotting problem. Dr Evans said Child E was "incredibly stable", at increased risk of NEC, but suitable treated. He said if a baby had NEC, they would become "gradually unwell" and Child E would not have coped with handling in any way, and have a distended abdomen, along with other observations. He said NEC was not a viable explanation. He said there was a significant haemorrhage and something must have caused this. He noted the 'unusual' discolouration, which prior to this case he had only seen in literature as evidence of an air embolus. He said there must have been some sort of trauma caused by a piece of equipment, such as an introducer. He said there was no "innocent explanation" for it. He said he has never seen an ulcer cause this type of bleed. He said the haemhorrhage was caused by trauma. Dr Bohin says she formed her opinion on the case, and refuted 'going along' with Dr Evans' conclusions. She said the decision not to hold a post-mortem examination was "a poor decision". Dr Bohin said babies with NEC do not go from being well one minute to very unwell the next. The 16ml aspirate before the 9pm feed "struck her" as being odd, and did not match Child E's clinical picture at that point, and was "at a loss" to describe where that had come from. She said the NGT insertion can sometimes cause "very minor bleeding" in a baby, but not a haemhorrhage. The blood vomit was "an extremely unusual feature". Dr Bohin had never seen a baby have a gastric haemhorrhage in this way, the court is told. She believed Child E died of an air embolus.
12:53pm: The judge refers to the case of Child F. On July 31, 2015, Child F was given a dose of insulin to treat high blood sugar levels, and he stabilised. On the day of August 3, other than a minor respiratory issue when Child F was taken off CPAP, all was well, and he was tolerating feeds. The prosecution allege Child F was given insulin via a nutrition bag hung up on August 4-5, and that the next bag hung up at noon on August 5, a stock bag from the fridge, had a similar amount of insulin put in it. The jury is reminded of the relationship between insulin and insulin c-peptide levels, naturally occurring in the body, and the relationship between those two in synthetic insulin. The defence say the proof is on the prosecution, that the jury must be sure that Child F and Child L received synthetic insulin, and that it was Letby who administered that. They ask if Letby was intent on harming Child F, why she did not attack that baby on subsequent shifts.
1:01pm: A new TPN [fluid nutrition] bag was hung at 12.25am on August 5 for Child F. Yvonne Griffiths said the fridge contains stock bags for Babiven and start-up Babiven, and insulin. That fridge was kept locked, with one set of keys, initially in the hands of the shift leader but available on request. There was no system for signing the keys in or out. Child F was the only baby on that night shift of August 4-5 who was receiving TPN.
2:09pm: The trial is now resuming following its lunch break.
2:20pm: The trial judge clarifies a matter from this morning, and says during the cross-examination of Prof Arthurs, it was said that gas could be recirculated in the body in the event of vigorous resuscitation. He continues with the case of Child F. He says a nurse was "really happy" with Child F from 10pm-1am. There was "no way of knowing" who had got the bags out of the fridge. Prof Peter Hindmarsh says the bag administered at 12.25am had insulin in. Dr Harkness attended the unit that night and noted Child F had vomits and tachycardiac, with a heart rate of 200bpm, but otherwise well. Prof Hindmarsh said these were signs of hypoglycaemia. Doses of dextrose and salt water were administered.
2:32pm: Kate Bissell and band 4 nurses said they had never added anything to a TPN bag. Dr Gibbs said the fall in Child F's blood sugar level was 'unexpected'. At 10.30am, a new long line was to be inserted in Child F, as instructed by Dr Satyanarayana Saladi, with the removal of the old one. The fluids were stopped while the line was replaced, and Child F's blood sugar level rose. A new TPN bag, from the stock bags in the fridge - of which there were about five - was hung up at noon. Fluids resumed. Child F's blood sugar levels remained low in the afternoon after dextrose boluses at 3pm and 5pm. The TPN bag was stopped at 7pm.
2:40pm: The judge details how the insulin blood sample was taken to the laboratory in Liverpool and analysed, and the results came back showing an 'undetectable' level of insulin C-Pep compared to a high level of insulin. It was suggested that the sample be referred for further tests, but Child F had recovered by this stage, so the sample was stored for seven days before being disposed of. Prof Hindmarsh said the increased blood sugar readings for Child F during the afternoon were consistent with them following fresh bolus administrations of dextrose. The blood glucose had 'started to rise spontaneously' between 10.30am-noon, Prof Hindmarsh said, during the time the fluids were not being administered. He said the difference between the blood glucose levels on a heel prick and a plasma sample would be about 10-15%. He said the dangers of low blood sugar include confusion, seizures, brain damage and in serious cases, death.
2:52pm: The judge says the court had heard the most likely cause of insulin administration was for it to be administered intravenously. Prof Hindmarsh says the most likely way for this was via an infusion, at a rate of 1.2 units per hour, and calculated that 0.6ml of insulin - a clear fluid - was added. He says the same amount would have been needed to have been added to the stock bag. He concluded that the only explanation was for Child F to have received bags contaminated with insulin. Dr Evans concluded Child F had received exogenous insulin via the TPN bag from before 01.54am to before 7pm. Dr Bohin agreed, and said two bags must have been contaminated with insulin. When interviewed, Letby remembered Child F as the surviving twin of Child E. She agreed her signature was for a TPN bag, and could not remember if she had administered the TPN bag or not. The bags were kept at the top of the fridge, the insulin at the bottom. Letby said medication would not be added to a TPN bag. She agreed the blood sugar level for Child F at 1.54am was "dangerously low", and denied harming Child F or giving him any insulin. Letby, in evidence, said she believed her nursing colleague had hung up the TPN bag. She confirmed she did not know about c-peptide at that time. She knew adding insulin was "life threatening" to a child like Child F. She said Facebook searches for the parents was because the twins were on her mind.
2:59pm: The judge refers to the case of Child G, born in a tertiary unit, and was "very premature", weighing just under 1lb 3oz. She was "at the margins of survival" when born. On August 13, Child G was transferred to the Countess of Chester Hospital, and was "stable". Letby said she remembered Child G, who had "a lot of problems". The prosecution case is Letby deliberately overfed Child G. Dr Stephen Brearey first reviewed Child G on August 22, and the general trend was one of improvement for the baby girl. She was "stable and well", with desaturations self-correcting. The oxygen requirement was "continuing to come down". For September 6-7, the night shift, Child G was the only baby in room 2, and Letby had a baby in room 1.
3:10pm: The prosecution case is after the 2am feed for Child G, administered by a colleague, Letby deliberately injected milk and air afterwards.
3:17pm: September 7, 2015 was Child G's 100th day of life, and a banner was prepared to celebrate that on the unit. Child G was still on nasal prongs and some oxygen, and was "stable". A nurse said she usually completed the chart after the feed. The 2am, 45ml feed was given via an NGT. Letby agreed the readings were good at this time. The nurse said an aspirate was taken from Child G for a pH check, this level being 4. She then went on her break at 2.05am-2.10am. When she returned, she found Child G had deteriorated with a projectile vomit. The deterioration had come as a surprise to her.
3:25pm: Shift leader Ailsa Simpson said she was at the nursing station with Letby when she heard Child G vomit - when they went over, the alarm for Child G went off, and there was "a large amount of milk" fed, and the vomit was on the cot, on the floor and on the chair adjacent to the cot. Respiratory support was given via Neopuffs. Letby had said, in evidence, she had no contact with Child G prior to the vomiting episode. She said she was aware Child G had a lot of ongoing issues, but the observations were good up to that 2am feed. She said she had been with Ailsa Simpson when they heard Child G vomit, and the alarm had gone off. She said when they arrived, no-one else was in there. She said they immediately started to give Child G Neopuffs. She identified a possible problem of the nursing colleague overfeeding Child G, but did not believe that likely. In police interview, Letby said it was a "shock" for three deaths in June-September 2015, and "didn't feel there was anything to need to look into". She said the nursing colleague was on a break when the vomit happened. She said sometimes babies vomit, but did not often projectile vomit. She said when babies vomit, they can taken on air when gasping. She added she was not sure of the cause of air in Child G's abdomen. In a separate police interview, Letby said Child G had either received more than 45ml milk, or had undigested milk from a previous feed. She said it was an oversight from a previous interview that she had not mentioned the vomit going on the floor and the chair by the cot.
3:35pm: Dr Alison Ventress said the vomit had been reported to her. For a description of Child G being in distress, and the abdomen purple and distended, she could not recall if that was something she had seen or was told, and the same went for Child G's watery stool, and a subsequenty improved abdomen. Dr Ventress was then called urgently to theatre. She said by this time, Child G was looking better. She was called out of theatre before 3.30am as Child G was apnoeic and had desaturated, and it took five minutes for the saturations to pick back up. Child G went to room 1, and had a further profound desaturation. At the time of insertion of an ET Tube, blood-stained fluid was noted beneath the vocal cords, which Dr Ventress noted was "unusual". Dr Brearey said he had not seen a projectile vomit in a pre-term baby like Child G. There was a further profound desaturation at 6.05am, and the decision was made to reintubate Child G. 'Thick secretions++' in the mouth and a blood clot in the breathing tube was noted. The NG tube was aspirated and 100ml was aspirated. Dr Ventress said she was not sure it was air, as that was not documented, as it would be noted otherwise. Dr Brearey took the '100ml' reading to be fluid or milk. Letby's case, the judge says, is she did nothing wrong, and did not falsify notes. She accepted air or milk could have been pushed from the feeding syringe into Child G's throat. She denied doing so.
3:53pm: Child G was readmitted to Arrowe Park Hospital on September 8, 2015 with presumed sepsis. She was very unwell on arrival, with severe hypertension. A radiograph, Prof Arthurs said, was not a sign of NEC. The baby girl gradually improved to the point of returning to the Countess of Chester Hospital on September 16. Dr Evans said Child G was compromised by receiving a large volume of milk and air, and this was not unique to babies. He proceeded on the basis the stomach of Child G was empty prior to the 2am feed, and a pH reading of 4 was indicative of an empty stomach. He said babies fed by NGT "do not vomit". He said Child G suffered significant oxygen deprivation which caused irreversible brain damage. He concluded Child G must have had more than 45ml of milk. Challenged on this, he said this was the first case he looked at, and reached his conclusion without looking at any other cases. Dr Bohin said the vomit was "extraordinary", and said it was impossible to say how big Child G's stomach was, but the excess volume of milk would not be much to compromise the lungs. She detailed a number of desaturations and events for Child G in June-July 2015. She concluded that it was "clear" by September 7, Child G was tolerating feeds. A pH reading of 4 was not consistent with there being a large amount of undigested milk in the stomach - she said if there was, the milk would have neutralised the pH reading [to 7]. She concluded Child G's stomach was empty. It was put to Dr Bohin that she was modifying her opinion based on the accounts of the nurse and Dr Evans. She refuted that, and said she based the level of milk on the pH reading, not anything Dr Evans had said. She concluded Child G must have had a large amount of milk and air administered after the 2am feed.
4:01pm: The judge refers to the events on September 21 for Child G, during the day shift, at 10.20am and 3.40pm. Child G was, the court is told, in a "satisfactory" condition. He says there was an event at 10.20am had two projectile vomits and went apnoeic, colour loss, and desaturation to 30%. Letby, the designated nurse, said she remembered the incident, and Child G was due to receive immunisations. The event had happened after a 40ml feed at 10.15am. Child G was being treated as 'a term baby'. Dr Peter Fleming recorded the projectile vomits, and that Child G went apnoeic for '6-10 seconds'. He discussed the case with Dr Rachel Change, and the course was to leave the NGT on free drainage, as the abdomen was distended. Child G was to be transferred to room 1.
4:13pm: Care had been transferred to a nursing colleague on September 21. She said Child G's heart rate was high when she first took over, but had settled by 12.45pm. After the vomits, Child G was 'nil by mouth'. Dr Chang noted Child G was pale and had a feed delayed, and the baby was "not herself". The tummy was "soft and distended" so a screen for sepsis was planned. Child G needed to be cannulated, and this required seven attempts, successful on the seventh attempt by Dr Gibbs, by which time Child G had been without fluids for six hours. A nursing colleague remembered Dr Harkness and Dr Gibbs arriving, and believed Child G was behind screens and on a trolley. She said when the doctors finished the procedure, they would let a nurse know, and the baby would be put in the cot. She next saw Child G when Letby called her for help. She saw Letby providing breathing support for Child G, and the nurse could see Child G was 'a poor colour'. The monitor was switched off. She shouted for nurse Caroline Bennion, and Child G responded to treatment, and was transferred to room 1. Child G was placed in an incubator. Letby, in evidence, said screens were put up for the procedure for Child G. She said it was 'common practice' for nurses to look behind screens, and said she saw Child G behind the screen, alone, on a trolley, blue and not breathing, and the monitor was switched off. She said she was keen to put a Datix form about the incident. She said she did not take it further as the nursing colleague said the situation was in hand. She said in police interview, it was 'bad practice' for the monitor to be switched off and 'somebody had made a mistake' in leaving Child G unattended behind screens on a trolley with the monitor off. She did not remember making numerous searches for Child G's mother on Facebook. She had no comment to make about them. Dr Gibbs accepted the monitor should not have been switched off. He admitted he had no recollection after the cannulation, and accepted it was possible, and said if the nurse said it had happened, then it happened, and he apologised for doing so. Dr Harkness said he did not recall the monitor being detached, and would probably have told a nurse when they were finished. He said it was "possible" Child G was behind a screen unattended. Caroline Bennion recalled Child G needed to be cannulated. Eirian Powell had no recollection of anything untoward clinically being brought to her attention.
4:23pm: The prosecution say Letby was incorrect when she messaged a colleague to say Child G 'looked rubbish' when she took over care for her that morning. Letby accepted she made an error on recalling the timing of the vomit, but said Child G looked pale on handover. Dr Evans said he had 4,000 pages of material for Child G alone, and concluded the episode of projectile vomiting was "life threatening", and said Child G had been given far more milk than intended, more than 40ml. He accepted the events on September 21 were not as serious as those on September 7. Dr Bohin said the "feeds didn't add up" and the events of September 21 were "strikingly similar" to September 7, but the consequences were not as serious for the September 21 event. Prof Arthurs said if a baby had been deliberately overfed, that would not necessarily show up on an x-ray.
5:35pm: That concludes the coverage for today. The trial will continue tomorrow morning with the trial judge summing up in the case of Child H. The Standard will continue to provide live updates from court.
Wednesday 5th July 2023
Judge's Summing Up - Day 3
Children H, I & JChester Standard Live Reporting
10:36am: The trial is due to resume this morning, after a delayed start.
10:46am: The trial is now resuming. Trial judge Mr Justice James Goss will continue his summing up of the case, referring to Child H.
10:52am: Child H was born in good condition on September 22, 2015 at the Countess of Chester Hospital, weighing 2.33kg (5lb 2oz), and was admitted to the neonatal unit. Child H was very unstable into September 24, suffering desaturations, bradycardia and pnemothoraces. Dr Dewi Evans and Dr Sandie Bohin agreed Child H should have had surfactant earlier, and the udge says it is accepted that care was sub-optimal. There was also "an unacceptable delay" in intubation. They said although the pneumothoraces were a complication, and some of the sub-optimal care may have led to later pnemothoraces, none led to the later collapses of Child H on September 26-27, for which neither could find a cause.
10:57am: Child H was later transferred to Arrowe Park Hospital, where she improved, and had no further cardiac arrests. She returned to the Countess of Chester Hospital on September 30. The prosecution say, acknowledging the sub-optimal care and challenges Child H faced, the coincidence of the collapses when Letby was present and being involved in Child H's care, the unexplained collapses, and Letby's interest in the family and other events, that she was responsible, by whatever method, for the collapses by deliberate harm on two occasions. Letby denied harming Child H. She raised the issue of sub-optimal care, issues with the chest drains, and said there was a 'cumulative effect' for Child H which led to her collapses. The defence say an innocent explanation for the collapses cannot be ruled out.
11:05am: The judge details the events for Child H prior to September 26-27, which involved two chest drains being put in place in response to desaturations Child H had. The tip of the second chest drain moved around. In cross-examination, Dr Ravi Jayaram said the second chest drain tip would not come into contact with the heart, and it was "very unlikely" it would come into contact with the sac around the heart, and he had not heard of any event where that had happened. Letby had messaged Sophie Ellis on September 25 saying it was 'pretty bad so far' how busy the unit was. In evidence, she said she had come across chest drains in Liverpool where the drains were stitched in, but not in Chester, and no-one seemed familiar, and a third chest drain had to be obtained from a children's ward.
11:12am: Dr Alison Ventress said the second chest drain on September 25-26 had 'amost fallen out', and Child H's oxygen requirements gradually increased. Dr John Gibbs said "unusually", Child H had developed another tension pneumothorax, and the two chest drains were blocked with serous fluid, and a third chest drain was inserted. Both Dr Gibbs and Dr Jayaram said drains can become blocked. There was then "a marked improvement", the judge tells the court, for Child H. Letby said, in evidence, ruled out staffing levels as an issue, but said there was "potential incompetence" in relation to where the chest drains were located. She recorded at 2210 Child H had a desaturation at the time of the heel prick, and serous fluid++ was recorded on the drains. She added the SHO was informed. There was no note by an SHO. The prosecution say Letby falsified notes, and there was an error on the timing on the blood transfusion note. Letby, in evidence, said these were mistakes, and she was not deliberately fabricating them. She denied sabotaging the drains, and said they had not been stitched in place.
11:26am: At 3.22am on September 26, Child H collapsed, and full resuscitation began. Child H quickly improved and resuscitation was stopped. The cardiac arrest had 'no obvious pneumothorax' and there was no evidence of fluid around the heart, a blood clot, and Child H's temperature was normal. Dr Gibbs concluded the event was caused by hypoxia (lack of oxygen), but the explanation for that was not clear. Child H had chest drains and was deemed 'unstable' for transport, so remained at the Countess of Chester Hospital or September 26-27, when she collapsed at 12.55am on the latter day. Dr Matthew Neame said his recollection was when Child H collapsed, Letby was Neopuffing her, and assumed she was Child H's designated nurse that night [Shelley Tomlins was the designated nurse for Child H that night]. He noted thick secretions blocking the ET Tube. Shelley Tomlins had noted Child H had a 'profound desaturation to 40% despite equal bilateral entry and positive capnography.' Letby, in cross-examination, was referred to text messages of her involvement with Child H that night. She said she had been assisting that night. Child H had another collapse at 3.30am and Dr Neame responded, and believed Letby was present. Child H was reintubated and her oxygen level and heart rate remained low. Dr Satyanarayana Saladi had been called to assist with the resuscitation, and contacted a consultant at Arrowe Park as there was no explanation for the collapse. A blood test revealed a raised result for an infection marker [CRP levels], and Child H was transferred to Arrowe Park.
11:29am: Letby, in police interviews, recalled caring for Child H as she had chest drains in. She did not recall where she was when the first profound desaturation took place. She thought the cause could have been some form of airway problem. She was unable to explain the collapse and denied deliberate harm. She agreed she had searched for Child H's mother on Facebook, but did not know why. Letby, in evidence, denied she was 'bored' on her shift, and said the timing of her messages could have meant she was on a break. She denied having interfered with Child H's tubes on any occasion.
11:36am: Dr Evans said it was unusual for a baby to have three chest drains. He said the deterioration of Child H would have been much more gradual if she had had infection. He said a pneumothorax was a complication of Child H's clinical condition. He said the overall picture for Child H was that she 'improved significantly and quickly' when responding to treatment. Dr Bohin noted the presence of respiratory distress syndrome, and that had surfactant been given earlier, that would have reduced, but not removed, the likelihood of a pneumothorax developing. There was an 'unacceptable delay' in the first intubation, and a needle 'may have punctured lung tissue'. The collapses on September 26 and 27 mirrored each other in having no obvious cause and were not quickly resolved, Dr Bohin had said. She could not identify any cause for these "significant collapses". Prof Owen Arthurs said the radiograph images showed a recurrent pneumothorax. He said there was 'no ideal position' for a chest drain. He said there was movement of the second chest drain. He said they are not known generally to cause bradycardias, particularly in neonates.
11:41am: The judge refers to the case of Child I, born on August 7, 2015 in Liverpool Women's Hospital, before being transferred to the Countess of Chester Hospital on August 18, "where she was expected to improve with no ongoing concerns". Child I died on October 23 in the hospital. The prosecution case is on four occasions, Child I suffered sudden and unexplained episodes, and a consequence of deliberate harm by Letby. They say the final event caused her death, and Letby is responsible for murder. Letby says she did not harm Child I on any occasion, and whatever the causes of her deteriorations, she was not responsible. She said there were periods when Child I desaturated and was being treated for infection, suspected infection and suepcted NEC. The prosecution say for three of the four events, Child I rapidly recovered, and the other desaturations and infections are explicable.
11:49am: The judge refers to an event in late August 2015, when Letby was not on duty, when Child I had a distended abdomen and an NG Tube dislodged. Dr Bohin, in cross-examination, said this decline differed from later events, and Child I had slowly deteriorated due to signs of infection and needed the use of a ventilator. Child I was returned to Liverpool Women's Hospital with suspected NEC. While there, she had a profound bradycardia, with her airway found to have large secretions in the ET Tube. Child I recovered from the episode.
11:56am: The judge refers to the first of the four events, on September 30, when nursing staff were "very happy" with Child I at this point. Lisa Walker carried out a skin patch test on Child I that day, which she would not have done if Child I was not well. On September 30, Letby was the designated nurse for Child I and two other babies in room 3 for the long day. Letby said, in evidence, she did not do anything to cause the event for Child I. Dr David Harkness said in agreed evidence, other than being pale and a slightly enlarged abdomen, there was "nothing to worry about". Dr Elizabeth Newby said they were at a plan of establishing feeds. The judge refers to the target weight gain for babies. Child I was at the lowest percentile end. Dr Newby said Child I's weight was low, and dropped down the percentile guidelines, but there had been numerous events in life when they had been unable to feed Child I due to adominal distension. Dr Bohin said it was "no surprise" Child I's weight was low, and Child I was unable to be fed as she had been ill.
12:09pm: The trial judge says he will not be going beyond 4pm today or tomorrow on his summing up, and apologises to the jury for the late finish yesterday. He says he will confirm timings next week when, it is expected, the jury will go out to consider verdicts.
12:20pm: The judge says Letby had noted, of Child I's abdomen: "mum feels it is more distended to yesterday and that [Child I] is quiet". In evidence, she said Child I waking for feeds was for the 10am feed. At an addendum, Child I was 'reviewed by Drs at 1500 as she was mottled and montoring was recommenced'. There was no corresponding doctor's note. In evidence, Letby said she believed it had been a male doctor, and it was the same name given when she was interviewed by police. She denied force feeding and causing a vomit for Child I. The mother of Child I had, by the time of the desaturation, left the unit and the father was at work. Child I desaturated and had a large vomit at 4.30pm, after a feed recorded by Letby of '35ml via NGT' at 4pm. A doctor had made a note for Child I's event, where Child I had dropped to 30% saturation, but by the time he arrived, Child I was breathing well and was pink, and the chest signs were clear. The abdomen was a little distended. Bernadette Butterworth recalled Child I's heart rate dropping and she desaturated, and required Neopuff. She saw Child I's stomach distending, and milk and 'air+++' aspirated. Letby said she did not know why so much air was aspirated. She said, in evidence, she had not pumped Child I full of air. Dr Harkness saw Child I that night, and Child I was breathing well for herself, and a blood test showed no obvious signs of infection. She did not like being handled. Nurse Ashleigh Hudson noted Child I was stable on October 1.
12:23pm: By October 12, Child I's feeds and weight were up, with feeds given every four hours of about 55ml of milk. At 1.30am on October 13, she took a 55ml bottle feed.
12:31pm: For the second event, the judge says Ashleigh Hudson noted Lucy Letby saying Child I looked quite pale. When the light was turned on, Child I looked very pale, and the monitor was not sounding. Neopuffing was established, heart rate in 50s. Letby wrote her note later, and the judge says she would have been able to see nurse Hudson's note at the time of writing. Letby: 'Child I noted to be pale in cot by myself...SN Hudson present. Apnoea alarm in situ and had not sounded...minimal shallow breaths followed by gasping observed'. Child I was given a blood transfusion. An x-ray showed "marked gaseous distention of bowel loops." A blood test showed no bacterial growth after 5 days. Ashleigh Hudson confirmed she had given Child I a feed at 1.30am, and Child I 'seemed very stable' and her waking for feeds was "really encouraging". She had assisted Laura Eagles with a procedure for about 15 minutes. She would not have left Child I alone if she was unstable, and would have asked a colleague to keep an eye on the baby. The other colleague on duty, Caroline Oakley, has no memory of being asked to do this. In evidence, nurse Hudson said Letby was standing in the doorway, standing 5-6ft away from the cot, the light was switched off, and the corridor light provided some illumination. There was a canopy over the upper part of the cot, and blankets were on Child I. She switched the main light on, and was closer to Child I than the defendant, and could see Child I was pale. She pushed back the canopy and blankets to tend to Child I. The apnoea alarm had "not sounded" and the deterioration was "very surprising".
12:35pm: Letby, when interviewed, remembered the event. She said when she and nurse Hudson went into the nursery room, they put the light on, and saw Child I was pale. She denied injecting air into Child I's stomach. She thought they were at the doorway and had just put on the lights, and the nursery "was never that dark that you would not be able to see the baby". In second interview, she said "maybe I spotted something that Ashleigh wasn't able to spot". She said from her position, she noted Child I was pale. In her evidence, she was asked how she could spot Child I - 'she knew what she was looking for', which she corrected to 'at', the judge says. In evidence, she said she could not recall looing after Child I prior to this event. She recalled herself and nurse Hudson going into room 2 together, and could see Child I's face and hands. Child I was 'gasping and shallow breathing', so the alarms didn't go off. She remembered telling nurse Hudson was 'a little pale'. She said room 2's lights were on a dimmer switch, and it was not as dark as a photo identified by Ashleigh Hudson in evidence.
12:39pm: Dr Elizabeth Newby said she was called to the room. As she arrived, she passed Letby in the corridor. Resuscitation took place on Child I, and it took 12 minutes before signs of life were detected. She said it was "definitely a serious state of affairs". The ETT was seen, by Dr Matthew Neame, to be too far in, and the NGT was also not in the right position. By the following day, Child I was seen by Dr Harkness and assessed to be 'sick but stable'.
12:47pm: The judge refers to the third event for Child I on October 13-14. Child I was in room 1. Dr Neame reviewed Child I, who was 'settled and pink', with breathing 'a bit squeaky' - normal in ventilated babies, the abdomen distended but soft. Letby noted for Child I on October 14: 'At 05:00hrs abdomen noted to be more distended and firmer in appearance with area of discolouration spreading on right hand side. Veins more prominent'. The judge says there are no corresponding medical notes for this. Child I 'grimaced' on Dr Neame palpating the abdomen, which was noted to be mottled and distended. His impression was that the increasing abdominal distention caused the lungs to be "squashed". The increased tenderness and skin discolouration stood out to him. He consulted Dr Jayaram, who was told of the distention, and it was decided to continue with the ventilator settings. After Dr Jayaram consulted Alder Hey Children's Hospital, they said they would contact the Countess of Chester Hospital with a plan in the morning.
12:50pm: Child I had a cardiac arrest at 7am. Shelley Tomlins noted Child I was pale and veiny, with 'slightly greyish discolouration', and Dr Neame thought the swollen abdomen was squashing the lungs. By the time Dr Jayaram arrived, Child I was stable. An x-ray showed no evidence of a pneumothorax. Letby, in evidence, said she did not have any recollection of the shift, other than from the notes. She agreed the signs were initially good for Child I. She said she had not inflated Child I with air or sabotaging her.
12:55pm: Child I 'responded very quickly' to treatment, and stabilised after being transferred to Arrowe Park on October 15. She returned to the Countess of Chester Hospital on October 17.
12:56pm: The judge reminds, and stresses, the jurors of their obligation not to research the case, and not to discuss it among themselves before their deliberation.
2:00pm: The trial is now resuming following the lunch break.
2:08pm: The trial judge is resuming the summing up in the case of Child I, and refers to the fourth and fatal event. Child I was pronounced dead on October 23, at 2.30am. Child I was not an intensive care baby but was in room 1 as a precaution, the court is told. Designated nurse Ashleigh Hudson had agreed Child I was 'settled and stable' the night of October 21-22. The following day, Child I remained nil by mouth, and was unsettled at times - as recorded by Caroline Oakley - but settled with a dummy. Her cares were attended to by Child I's mother. For the night of October 22-23, Ashleigh Hudson was again the designated nurse for Child I. Letby said she did not recall, in evidence, much of the night shift when Child I died. She said staffing levels might have played a part.
2:15pm: The judge says just before midnight, Ashleigh Hudson said Child I became unsettled and had 'very loud crying' - 'relentless', something she had not heard before from her. Child I was put on her tummy and she became quiet, and there were gaps in the breathing. Child I was turned over again and nurse Hudson called for help. Letby said, in evidence, she had not heard Child I 'cry like she had not heard before'. She was 'quiet' and 'apnoeic'. Dr Rachel Chang and Dr Gibbs were called and CPR began on Child I. She was ventilated and recovered - she was pale and mottled (blue) in her trunk. The colour "steadily improved" over five minutes and Child I became pink all over. It was decided to extubate Child I as she was fighting the ventilator - "a good sign". Dr Gibbs was unsure what had caused Child I's rapid deterioration. He said he could not understand what natural disease could have caused it. A 'large stomach bubble' was seen in an x-ray for Child I. Letby, in cross-examination, was asked about a record for one of her designated babies that night [the Stoke baby]. The baby was noted by Dr Chang to be safe for transfer. Letby had noted, between 10.50pm-10.52pm, to commence 10% glucose for transfer. The IV fluid chart showed the start time altered from 11pm to midnight. In response to the allegation of falsifying records, Letby said the 11pm was an error which she had corrected.
2:19pm: Nurse Hudson said Child I was behaving normally prior to the final desaturation. She did not recall how she was alerted. She said when she arrived at Child I, Letby was already there at the incubator, 'with her hands in, with a dummy, trying to settle [Child I]'. Child I's crying was "loud and relentless" and nurse Hudson was concerned Child I was going to collapse. The nurse recalled she said something along the lines of 'She's going to do it again, isn't she?' and that Letby replied: 'She just needs to settle, she just needs to settle'. Child I then collapsed. Dr Chang arrived at 1.12am and was joined by Dr Gibbs in trying to resuscitate Child I, who had 'mottling of purple and white all over'. Efforts to resuscitate were unsuccessful.
2:23pm: Melanie Taylor said they were all devastated, and it was "pure shock", and this was the second death she had been directly involved in. She was never concerned about the treatment/care that babies received. Ashleigh Hudson was supported by Letby. The mother of Child I recalled Letby: 'was smiling and kept going on about how she was present at Child I's first bath and how much Child I had loved it'. Letby had said she was 'trying, in that awful situation', to create a positive memory for the parents.
2:28pm: Letby was asked about a sympathy card she had taken a photo of for Child I's family, on the day of Child I's funeral. She searched for the mother on Facebook on October 2015 and May 2016. Letby said she did not remember if she was present when Child I collapsed, and 'maybe she had gone to her after hearing her crying'. She said the transfer process would have been 'stressful' for Child I, and believed the process was done too quickly. She said it was "upsetting" losing Child I, and said she regularly took pictures of cards she sent. She did not know why she had searched for Child I's mother on Facebook. She recalled settling Child I after crying, but did not know if this was after the first or second collapse.
2:52pm: Prof Arthurs reviewed all the radiographic material. He said lungs were normal prior to the final collapse, and it was quite unusual to see 'massive dilation of the stomach', which could cause splinting of the diaphragm. The post-mortem imaging showed dilation in the bowel, and he said that was present before she died. He said there are not many conditions which cause dilation of all the bowel. He said one of the explanations was air deliberately administered down the NG Tube, and that was his inference. Dr George Kokai carried out a post-mortem examination of Child I. Dr Andreas Marnerides was dependent on the report. Dr Marnerides said Child I did not have NEC. He was "very sceptical" that Child I died of natural causes. He said the collapses were more likely to be excessive air administered to the stomach, via the NGT. The defence say a similar event happened for Child I on August 23, a day when Letby was not on duty. Dr Evans said Child I's weight gain could have been better, and atributed that to her illnesses. He formed the view Child I had received a large volume of air down the NGT. He said it would have had to have been sizeable to cause splinting of the diaphragm. He refuted suggestions he had taken events from September to support a prosecution case, saying at the time of his reports, no-one had been arrested. Dr Bohin said she, too, thought abdominal distention had splinted the diaphragm in the first event. She discounted NEC. Dr Evans said the second event was more serious. He refuted suggestions he had been 'looking for evidence to support the prosecution'. Dr Bohin said she was not sure if an NGT was in place at the time - there was no clinical need for one, but it was practice to keep one in place 'just in case'. She accepted in her report that she said Child I did not have an NGT. She considered air in the vein was a possibility, due to the subsequent discolouration findings. In cross-examination, Dr Bohin was accused of 'backing up' Dr Evans. She refuted that, saying she was independent and had disagreed with Dr Evans on some conclusions. She said she had seen air embolus twice in babies in her career, and explained what the symptoms were, saying the clincial presentation was 'wide and varied'. She agreed there was nothing specific about discolouration that made it diagnostic of air embolus, but it was consistent with air embolus.
3:03pm: Dr Evans said for the third event, he came to the conclusion of a large volume of air administered via an NGT into the stomach. The response to Child I's resuscitation was not what he would expect. In cross-examination, Dr Evans said this was a separate event, not a continuation of an existing event. Dr Bohin concluded it was an air embolus caused by excessive air administration. For the fourth event, Dr Evans said Child I was 'a stable baby' prior to the collapse. He said he thought air was administered, on this occasion, via the blood. He thought the relentless crying, as described, was of a baby in pain and distress, and there was no explanation. In cross-examination, he denied he was 'gonig for whatever mechanism that could support his explanation'. He said if air was injected in the stomach as well, that was something he could not rule out. It was at that point, the judge says, Benjamin Myers KC, for Letby's defence, cross-examined Dr Evans on a family court judgment's report which criticised the medical expert, with "strong views" by Lord Justice Jackson. The defence said the 'inconsistencies' in Dr Evans' evidence undermined his case and the judge's criticism was 'relevant'. The judge says it is up to the jury to consider the evidence, and they know no more about that case - and the judge's summary report - than the agreed evidence which was presented to them.
3:14pm: The trial is resuming after a short break. The judge refers to the case of Child J, born at the Countess of Chester Hospital on October 31, 2015.
3:17pm: After a short time, Child J produced some brown bile, and was transferred to Alder Hey Children's Hospital for surgery. She had a perforated bowel and was fitted with a stoma. She returned to the Countess of Chester Hospital on November 10, and progressed well, moving into nursery room 4 (special care). She had issues with gaining weight, but hospital staff were not overly concerned. Nursery nurse Nicola Dennison said babies with stomas don't tend to grow very well. Child J's mother had stayed with Child J, giving cares, prior to leaving on the night of November 26-27.
3:20pm: Letby was messaging a colleague, prior to this night shift, about how nursery nurses should not be caring for babies with stomas, and there were issues with staffing, saying they would have to send some babies out [to other hospitals]. During the shift, Child J had two sets of sudden and unexpected desaturations, which required resuscitations, and in the latter, there were symptoms of a seizure, something Child J had not had before or since. Dr Bohin said there was no cause for the events. Dr Evans said infection could not be ruled out. The prosecution said Letby did something or things to cause deliberate harm. The defence say in the absence of any identifiable cause, the jury cannot be sure Letby did anything to harm Child J.
3:30pm: Mary Griffith recalled an event at 5-6am when she heard an alarm go off in nursery 4. She saw nurse Dennison had Neopuff on Child J, as she had desaturated. Dr Kalyilil Verghese recalled attending once, at 5.15am. Swipe date showed him entering the unit at 5.03am. He said he was told what had happened, that Child J had two 'profound desaturations', the first to the 30s, the second to the 50s. In the later, Child J was pale and mottled. He said at least one of those events was "significant". Apart from Child J's increased efforts to breathe, Child J had recovered well. Child J was moved to room 2, where Letby was. Letby said it was 'widely talked about' that nursery nurses were doing stomas when they shouldn't. She said it was a very busy time. She said she had no idea these events were happening. Dr Gibbs was on the unit when Child J desaturated again, this time with a falling heart rate. He said he assisted nurses Griffith and Letby. Dr Gibbs noted Child J had desaturations to 'unrecordable levels', the first at 6.56am, the second at 7.24am, plus bradycardia - they were associated with stiff arms, clenching of hands, and on the second occasion the eyes deviated to the left; these were symptoms of seizures. The first took 10 minutes to settle, and the perfusion was poor. The second took five minutes to settle. Both events required ventilation. Dr Gibbs could not explain the desaturations, and Child J had not presented with these symptoms before. He would say there were caused by a drop in oxygen, but the cause of that was not known.
3:38pm: Prof Arthurs reviewed the images for Child J. After the last collapse, the image was unremarkable - it could not assist in an explanation for this event. In polcie interview, Letby recalled Child J as she had a Broviac line and stoma. She thought she only treated Child J after the collapse. She said she had administered medication as Nicola Dennison was a nursery nurse, and not qualified to administer such medications. She accepted searching for Child J's parents, but could not recall doing so. In evidence, she said she was aware of the second pair of events, that she and Mary Griffith heard the alarm, and saw Child J fitting when they arrived. No-one else was present. Child J recovered. Dr Stephen Brearey noted no blood glucose abnormalities to explain the seizures, and there was nothing of concern in blood results. Abdominal x-rays did not raise concerns. He had no concerns, and said it was a "remarkable reovery" for her. He did not understand why Child J had been hypoxic. Letby was the designated nurse for Child J the following night and there were no concerns raised. 0
3:43pm: Dr Evans said the collapses were unexpected, the second pair were more serious, and 'indicative of something wrong with the brain', and indicative of loss of oxygen to the brain, and could not explain any natural process that had caused that hypoxia. Dr Bohin said infection was not responsible for Child J's collapses, and did not come to any major conclusion other than the deteriorations were sudden and unexpected.
3:48pm: The trial judge begins referring to the case of Child K, born at 2.12am on February 17, 2016, weighting 1lb 8oz. She was transferred to the neonatal unit prior to transfer to a tertiary unit - Arrowe Park Hospital, where her condition continued to deteriorate, and the mother agreed, in the "most heartbreaking decision" of her life, to end life support for Child K on February 20. The prosecution say Letby attempted to kill Child K within two hours of her being born, interfering with the breathing tube, causing her to collapse. There were two further collapses and the prosecution allege there was sabotage by Letby, but they are not the subject of charges. There is no expert opinion in Child K's case, and the evidence is circumstantial, the judge says. The prosecution urge the jury to rely on inferences. The defence, the judge says, point to Child K's extreme prematurity, and no 'direct evidence' of harm caused. Child K was given surfactant late, and witness Dr Ravi Jayaram's evidence is "tainted and unreliable". Letby had no recollection of events, but believed the ET Tubes were not secured correctly.
3:52pm: The oxygen saturation of 85% was 'good' for Child K minutes after birth, for a baby of her gestational age, and good enough to attempt intubation. Dr James Smith said if he had seen any evidence of trauma or bleeding, he would have asked a consultant to step in and carry out the procedure. Nurse Joanne Williams said a team would carry out the procedure, and the ET Tube would be secured so the tube does not slip. Child K was transferred to the neonatal unit on a Resuscitaire, with the plan to transfer to a tertiary unit.
3:56pm: Mr Myers referred to a leak on the ventilator in his closing speech. An Alder Hey consultant said the air leak numbers "did not tally" with the high oxygen saturation readings for Child K. Joanne Williams said if Child K was not receiving the oxygen saturation required, the alarms would have gone off. Surfactant was administered, which Dr Smith agreed was "late" by 13 or 18 minutes, but would not have compromised Child K.
4:00pm: The trial judge confirms the jury will not be starting deliberations on Thursday, as he will not have completed his summing up until Monday. He says that will happen 'earlier rather than later' on Monday, July 10. He says the court will resume 10.30am-4pm tomorrow.
Thursday 6th July 2023
Judge's Summing Up - Day 4
Children K, L, M, N, O & PChester Standard Live Reporting
10:28am: The trial is due to resume shortly.
10:31am: The trial judge, Mr Justice James Goss, continues with the summing up in the case of Child K.
10:39am: Joanne Williams was Child K's designated nurse and left the neonatal unit at 3.47am - an hour and a half after Child K was born - to update the parents. She said she would not have left Child K if she was not stable, or had someone to look after her in her absence. Dr Jayaram and nurse Williams were "happy" Child K was "quite stable". Joanne Williams said in cross-examination the morphine infusion for Child K, timed at one chart for 3.30am, could have been at 3.50am. Dr Jayaram said he was aware Letby was alone with Child K, and thought he was being "irrational", but went to check on Child K as a precaution. Dr Ravi Jayaram said he walked in to the nursery room and saw Letby by Child K's incubator, and saw Child K's saturation levels dropping to the 80s. The monitor alarm was not going off. He said: "What's happening?" Letby said something along the lines of: "She's desaturating." Dr Jayaram ascertained the ET Tube was not working as it should, and Child K was ventilated. He said babies usually desaturate after about 30-60 seconds, so the cause of the desaturation would have started before he went into the room. Dr James Smith saw Dr Jayaram on the right side of the incubator as he walked in. He reintubated Child K. The court had heard it was possible for a user to pause the monitor alarm sounds for one minute.
10:48am: Dr Jayaram was challenged about why he had not confronted Letby about her behaviour. He said it was "not appropriate" to raise concerns in medical notes. He said concerns were raised after this incident, and faith was put in senior management, and they were told it was unlikely anything was going on, and to see what happens. He said in hindsight, he wished they had bypassed management. He could not remember the transport team note where he had written 'baby dislodged tube'. He said it was "highly unlikely" Child K had dislodged the ET Tube. He accepted the note Child K had been sedated after the desaturation, but denied altering his account to fit the evidence. He said he had not seen the swipe data for timings. Letby, in interview, said she could only remember Child K because of her size. She did not recall Child K's tube slipping or any collapse. She agreed she thought Joanne Williams would not have left Child K alone if Child K was not stable. She could not remember if the alarm was silent, but agreed it should have sounded if Child K was desaturating. She thought it possible she was seeing if Child K was self-correcting. In evidence, she said she did not have independent memory of Child K other than her being a tiny baby. She said although she had no memory of it, she said she would have waited 10-20 seconds to see if Child K self-corrected, as that was "common practice". Elizabeth Morgan said, in agreed evidence, it was possible for an ET Tube to be dislodged in an unsedated and active baby, and a nurse would not leave the child alone in this situation if the baby was not settled. She said it would be 'good practice' to observe the baby immediately and take corrective action if necessary if a baby of this gestational age had begun to desaturate. She believed it would not be normal practice to 'wait and see', in a child of this gestational age, with the lungs so underdeveloped.
10:53am: At 6.15am and 7.30am, Child K desaturated again, and it was noted the ET Tube had dislodged again in the second event. Letby was on duty. The transport team arrived for Child K, who required several rounds of treatment to stabilise her. She left, having been stabilised, at 12.50pm. The prosecution say Child K was a settled baby who would not dislodge the tube. There was no record of an ET Tube dislodgement at Arrowe Park. Child K died on February 20, 2016. The cause of death was extreme prematurity with severe respiratory distress syndrome.
10:58am: Letby, in further interview, said she had no memory of Child K's ET Tube slipping, and suggested it had not been secured initially. She accepted searching for Child K's mother's name, but could not recall why. In evidence, she said she had nothing to do with the events at 6.15am and 7.25am. she agreed she had no reason to be in room 1 at 7.25am. She said she looked up the name for the mother as "you still think of patients you care for". She said the night was a "busy shift". The judge says the prosecution accept they cannot prove Letby's actions caused Child K's death, but say she attempted to kill her. The judge refers to the case of Child L and Child M, and their birth on April 8, 2016 at the Countess of Chester Hospital.
11:05am: The judge says it is alleged Letby tried to kill Child L by putting insulin into bags of dextrose. Professor Peter Hindmarsh said the hypoglycaemia episode for Child L lasted from April 9-11, and multiple bags had insulin added. He said a 'not noticeable' amount of insulin, 0.1ml, would have been added to the 500ml bag, which would not change the colour. He was of the opinion that two or three bags - depending on how many were hung - had insulin added. He said while 'sticky insulin' would account for some of the hypoglycaemia, over time more insulin would have had to have been added via a bag, he said. Letby worked four long day shifts from April 6-9, and had moved house during that time to Westbourne Road, Chester. She said April 9 was still "fairly busy" on the unit.
11:10am: After birth on April 8, Child L's blood sugar was "a bit low" at 1.9. The court had heard this was normal for premature babies, so he was started on glucose. Reference to hypoglycaemic pathway was mentioned, that milk should be given to infants before an infusion of glucose. Neonatal practitioner Amy Davies said she had "no concerns" for Child L regarding putting him on an alternative pathway. Dr Sudeshna Bhowmik wrote the rate of the glucose infusion. Letby said glucose bags were kept in room 1, and insulin was kept in the equipment room. She could not recall if any of the bags were kept under lock and key. The first bag was 10% dextrose at noon on April 8. Colleague Amy Davies denied administering insulin, saying that would only be given to babies with blood sugar levels over 12, and would be prescribed by a doctor.
11:16am: This was the 60th case Dr Dewi Evans looked at, the court is told, and saw the relation between insulin and insulin c-peptide in the blood plasma laboratory result for Child L. He suggested to police a specialist should be approached to review his findings. Prof Hindmarsh said neonates have higher glucose requitements, and any blood sugar level under 2.4-2.6 is a "cause for concern", so it was appropriate for the initial dextrose infusion. For the night of April 8-9, there were "no concerns" for Child L, and all the blood glucose readings were above 2. No fluid bags were changed during the night shift. For the day shift of April 9, Mary Griffiths was the designated nurse for Child L. She said he was "stable".
11:25am: Prof Hindmarsh says Child L was hypoglycaemic by 10am on April 9 and insulin "must have been added" between midnight and 9.30am. He said it is "fairly easy" to insert insulin into the portal of the bag via a needle. The judge says Prof Hindmarsh says "at least three bags contained insulin" to maintain the low blood sugar levels for Child L. The insulin could have been added to the bags at the same time, he added. He said once it was in the bag, "it would not be known by smell or appearance". The type of insulin used was 'fast-acting', the court was told. Mary Griffiths said it was "quite a shock" the blood glucose levels for Child L dropped after the dextrose was administered. Letby said, in evidence, said she had nothing to do with insulin in the bags, and could not assist with an explanation why the blood sugar level was low. She said she had nothing to do with the bags, prior to changing them. Mary Griffiths could not recall if the bag was changed. A plasma blood sample was taken, but podding was "late", the court had heard, due to the collapse of Child L's twin, Child M. The evidence, the judge says, is the blood sample was taken between noon (when Child L had a 1.6 blood sugar reading) and 3.35pm.
11:31am: The blood sample 'passed all the quality control tests' and 'performance checks' at the Royal Liverpool Hospital. The judge tells the jury: "In short, there is no evidence to doubt the reliability of the test results, you may think." The insulin and the insulin c-peptide results were the 'wrong way around' from what they should have been. Child L's insulin level of 1,099 should have meant an insulin c-peptide of 5,000-10,000, but it was 264. The court had heard said it was therefore synthetic insulin, administered exogenously, and to do so was "dangerous". Clincial biochemist Dr Anna Milan said there was not anything that doubted the accuracy of the results. In cross-examination, she explained in the case of insulin, if the sample had not been treated appropriately, the insulin level would have been even higher, and insulin c-peptide was stable. Prof Hindmarsh said the '1,099' reading was a minimum, not a maximum.
11:42am: Letby, in interview, said the original blood sugar levels for Child L were not a huge surprise for a neonate. She said very prolonged low blood sugar levels can cause brain damage and even death. She said it was not common for babies to be given insulin. She said they had access to the hypoglycaemia pathway on the unit. She said any addition to an infusion bag would be "very rare" and have to be prescribed by a doctor, and would have to be administered via a syringe on the bag port. She replied "That wasn't done by me" to the accusation the bags had been sabotaged. She said an explanation would be insulin would be in one of the bags, and denied responsibility. The prosecution say there is "uncontrovertible evidence" Child L was poisoned with insulin before 10am on April 9, and accounted for 'persistent' low blood sugar levels. They say this happened when Letby was on shift. Blood sugar levels improved on April 11. The prosecution says from the second 15% dextrose bag on that day, Child L was no longer being infused with insulin. Letby said the initial low blood sugar levels for Child L on April 8 showed naturally resolving hypoglycaemia. She accepted only she and Belinda Williamson [Simcock] had been on duty for the Child F and Child L events when the babies first had serious low blood sugar readings. She denied doing anything to harm Child L.
11:58am: The judge refers to the case of Child M, who the court had heard was "not an intensive care baby" but put next to Child L on April 9. At 11am, he had a "small possit", as noted by Mary Griffith, and 1.5ml of bile-stained fluid was aspirated at 12.30pm. Child M was to be 'nil by mouth', a decision made by a registrar.
12:02pm: At 3.45pm, Child M received antibiotics, the prescription by Letby and Mary Griffith, and administered by one of the two nurses. At 4pm, Mary Griffith had been preparing a 12.5% dextrose infusion for Child L. The parents had left a few minutes earlier. Child M collapsed at this time. Letby said: "Yes, it's an event, it needs to be sorted." and the resuscitation call was put out. Dr Jayaram was crash bleeped. A nurse colleague said her role was to draw up the resuscitation drugs. She was shown a piece of paper towel referring to entries on clinical notes, for times and medications administered. She recognised her handwriting of adrenaline made. That note was subsequently recovered from a Morrisons bag in Letby's bedroom at the time of her arrest in July 2018, along with a blood gas record for Child M. The nurse said the practice was to put the note in the confidential waste bin or the clinical waste bin, where it would be incinerated. the judge says it is the prosecution case that Letby recovered the note from the bin afterwards.
12:16pm: Child M was not breathing for himself and required doses of adrenaline in the resuscitation, which lasted under 30 minutes. They reached a point, the judge said, where Child M "might not survive", then Child M suddenly picked up his breathing and heart rate. Dr Jayaram said he saw pink patches/blotches on the abdomen of Child M that moved around. He noticed that He said it was similar to what he had seen with Child A. He first mentioned it in his witness statement. He said his priority at the time was communicating with parents and post-resuscitation care. He said and his colleagues sat down on June 29, 2016 to discuss the findings. Dr Jayaram said someone mentioned air embolus. He researched it in literature, and he shared that research the following day with colleagues. In cross-examination, he said he had not appreciated the clinical significance of the skin discolouration at the time. He rejected the assertion he did not note it at the time because it did not happen, or that omitting it was 'incompetence'. He said at the time, "there were other events going on". He agreed that after Child D had died, Dr Stephen Brearey had carried out an informal review of events at that time, and that Letby was associated with those events. In police interview, Letby denied doing anything to harm Child M. She did not know why Child M desaturated. She said she had been drawing up medications at the time of the collapse. She thought she had taken the paper towel home 'inadvertently', not emptying her pockets. She said the paper towel might have been put to one side. She denied she had kept it to keep a record of the attack. In evidence, she said Child L and Child M stood out as she had been the allocated nurse for when they were delivered. Child M was not in an allocated space on the nursery, she recalled, and maybe things would have been different if he had been in an allocated space. She did not recall seeing any discolouration, did not recall having any description of skin discolouration being mentioned to her, and any discolouration would have been difficult for her to see. Letby said her taking home the notes was an "error" and denied taking them from a confidential waste bin. She added she cared for the twins on subsequent days "quite frequently", during which time there were no adverse incidents.
12:33pm: Paediatric neuroradiologist Dr Stavros Stivaros provided agreed evidence in which he said Child M had shown signs of brain damage, likely caused by the collapse on April 9, 2016. Professor Owen Arthurs viewed radiographic images for Child M and said they could not support or refute an air embolus. Dr Dewi Evans concluded there were no concerns for Child M prior to the collapse, save for one bilous aspirate for which he was put nil by mouth. He did not believe that caused the collapse, as Child M's stomach was empty. He believed a noxious substance or air was administered to Child M's circulation [ie intravenously], and could not explain a natural cause for Child M's rapid recovery, ruling out infection. He said, taking into account Dr Jayaram's description of the skin discolouration, the cause for Child M's collapse was an air embolus. In cross-examination, he accepted there was no imperical research for how air dissipated in the body following a collapse, and based it on physiology, that cardiac massage would dissipate it. He said if the air goes around the abdominal area, it would result in skin discolouration, and if it heads towards the brain, it can cause neurological damage. He said 'very little air' is required to cause collapse. Dr Sandie Bohin said Child M had no markers of infection. She had to find some way to explain how a baby previously well suddenly collapsed, and had prolonged resuscitation for which he almost did not make it, then recovered rapidly. She said the skin discolouration seen by Dr Jayaram was "compatible" with air embolus. She said the actual volume to cause a baby to collapse and die is unknown. She said if it was a small volume, it would "take some minutes" to get to Child M in this case, as he was on a slow infusion. In cross-examination, Dr Bohin accepted most babies die in the case of air embolus, but it was "not inevitable". She could not think of an alternate medical cause from her differential diagnosis. She said the type of cardiac arrest suffered by Child M was "incredibly unusual".
12:36pm: The judge refers to the case of Child N, born on June 2, 2016 at the Countess of Chester Hospital. He says the prosecution case is Child N had three unexpected collapses in June 2016, that are all attributable to inflicted trauma by Letby, and were acts carried out with the intention to murder him. The defence case is Letby did not harm Child N, that there are inconsistencies in the accounts, and the jury cannot be sure Letby intended to murder Child N.
12:39pm: Child N had 'intermittent grunting' and it was recorded at 3.10pm on June 2 that he had a desaturation to 67% for a minute, and was crying, as recorded by nurse Caroline Oakley. He was placed in a hot cot and reviewed by Dr Anthony Ukoh. The nurse said she had no recollection of events other than that in her notes. There was nothing to suggest the naso-gastric tube was moved after it was placed, or that there were difficulties placing it on Child N.
12:46pm: For the night of June 2-3, Christopher Booth was the designated nurse for Child N. Letby had messaged a colleague to say they had a baby with haemophilia, and in evidence, said staff were panicked by this. The prosecution say Letby was messaging a colleague 'constantly' from 8pm while feeding a baby in a nursery which was a two-handed job. She refuted a suggestion, in cross-examination, she had force-fed her designated baby at the time, saying the note of the feed must have happened at a different time. Dr Jennifer Loughanne reviewed Child N and saw he was 'pink and well perfused', and consideration was given to starting enteral feeds. Christopher Booth had no concerns as he went on his break. He handed over care to a nurse when he went on his break at 1am, but cannot remember who. The other colleagues cannot recall caring for Child N. Child N had a deterioration to 40% at 1.05am - "a significant desaturation", and Child N was "screaming", Dr Loughanne had noted. She said she had no direct recollection of that, and said she would not usually have written that word. At 2am, Child N had recovered was settled, and was asleep.
12:48pm: Christopher Booth recorded there had been no further episodes for Child N following that desaturation. The baby remained nil by mouth. The prosecution case is Letby sabotaged Child N in some way to cause the collapse. Letby said she had no memory and did not know Child N had collapsed. She said she did not believe it was a collapse which required resuscitation. She denied using the absence of Christopher Booth as an opportunity to sabotage Child N.
12:56pm: Letby referred to an "active life" in messaging on June 13, planning a holiday. The prosecution say the second and third events for Child N happened on June 15, 2016. There had been no concerns for Child N on June 14 at handover for the night shift, by nurse Jennifer Jones-Key. At 1am, Child N was 'pale, mottled and very veiny', with slight abdominal distention. He was reviewed by a doctor, who observed mottling, a potential sign of sepsis, but was otherwise normal. On further observation, Child N had five minor desaturations which had resolved, and the mottling had gone. Child N's oral feeds were stopped, and he was given antibiotics and glucose. The defence say these were signs of Child N deteriorating. At 7.15am, Child N had another desaturation. The prosecution say Letby, who had arrived early for her day shift, did something to cause the collapse. Letby said she had gone to see Child N as she had had him for the previous day shift. The 'profound desaturation' caused Child N's heart rate to be affected.
12:59pm: A male doctor had been called to attend Child N and recorded a desaturation to 48%. He decided to move Child N to nursery room 1, and attempted to intubate. He saw blood which prevented him from seeing the airway. The back of Child N's throat "looked unusual" with swelling, and he was not sure where the blood was coming from. He made three unsuccessful attempts to intubate, and suction 'did not clear the view enough', and he said he did not want to inflict mechanical trauma. He remembered Letby was helping with the attempted intubation. A chest x-ray confirmed no pulmonary haemhorrhage.
1:59pm: The trial is now resuming, following its lunch break.
2:05pm: The trial judge says Letby, in police interview, she remembered Child N had an 'unusual air way issue', and was 'very difficult to intubate'. She was asked about intensive care charts, and references to blood. She said if the NGT had been inserted forcefully, it could cause about 1ml of blood. She did recall Child N bleeding at the time of intubation, but was not sure why. In her second interview, Letby said she would arrive prior to 7.30am for her day shift. She went to talk to Jennifer Jones-Key, her colleague, on this day. She referred to her colleague's note of Child N being pale and veiny overnight. His condition "deteriorated". In cross-examination, it was put to Letby that observation charts showed nothing deteriorating for Child N. Letby said she was stood at the doorway, and Child N's deterioration happened "within minutes", was "blueish and not breathing". For the intubation, Letby recalled blood being seen, and her interpretation of the note was blood was seen once intubation had been attempted. In the family communication note, Letby wrote parents were contacted, phones were switched off, and message was left. In cross-examination, Letby agreed she had written out the 7.15am incident as she had taken care of Child N from 7.30am. The first time she recalled seeing blood was after the second desaturation at 3pm for Child N.
2:12pm: The judge says there was a dispute over previously agreed evidence on who made a call to Child N's parents. A further desaturation happened at 2.50pm, after the parents left the ward. Dr Huw Mayberry was crash-called to Child N, who had desaturated. He could see vocal cords, but there was a "substantial swelling in the airway", and did not recall seeing any blood. Dr Satyanarayana Saladi recalled seeing blood in the oropharynx and blood in the NG Tube. Child N was later intubated successfully by the Alder Hey transport team. Child N continued to have episodes of apnoea, but they were less serious, and recovered at Alder Hey. Letby noted: 'approx. 14:50 infant became apnoeic, with desaturation to 44%, heart rate 90 bpm. Fresh blood noted from mouth and 3mls blood aspirated from NG tube. Neopuff commenced and Drs crash called...unable to obtain secure airway'. She said after the 3ml aspiration of blood, she had some memory of events, and there was "a sense of panic" on the unit, and it was "chaotic". She said there was no factor 8 left, so some was brought over from Alder Hey. She said Child N was the "focus of the whole unit at that point". She said she was stressed and anxious as they couldn't get an airway.
2:18pm: Professor Sally Kinsey gave evidence on haemophilia, and the purpose of Factor 8. Child N had 'moderate' haemophilia, and would need Factor 8 when it was required, not on a regular basis. She did not see any issue with Child N's blood which caused the collapses. She said a spontaneous bleed could not be explained by haemophilia, as a baby could not damage themselves in the throat, and any instrumentation could "potentially" cause bleeding. A pulmonary haemhorrhage was "not a viable" explanation. The defence do not suggest it was spontaneous bleeding or pulmonary haemhorrhage - they point to when witnesses saw the bleeding. Child N was the 29th case Dr Evans looked at. The event on June 3 was unusual, particularly the screaming and crying. He said something must have been done to him - and this was not an air embolus. For June 15, Dr Evans said the bleed was a consequence of trauma. Dr Bohin said the June 3 desaturation was 'life-threatening' and she had never experienced a baby crying for 30 minutes, or screaming. She said Child N had received a painful stimulus. For June 15, she believed the bleed was a consequence of trauma.
2:24pm: The judge refers to the cases of Child O and Child P, two of three triplets born on June 21, 2016 at the Countess of Chester Hospital. Child O died on June 23, and Child P died on June 24. Child O weighed 2.02kg and was admitted to the neonatal unit. From about 5pm on June 21 and through June 22, there was 'nothing remarkable' about Child O's condition. Letby was on holiday from June 16-22, during which time she had gone to Ibiza. In text messages, Letby enquired with a male doctor about the triplets, and said she felt at home in ITU, and 'the girls' knew she was happy to be in room 1 of the neonatal unit. Child O was moved from room 1 to room 2 during June 22, and had 'a good day' and was 'very stable', the court is told. Overnight on June 22-23, Child O was recorded as having partially digested milk in aspirates, which was 'normal', and a 'stable night', with a full abdomen at 7.30am showing 'no concern'.
2:30pm: Letby accepted that Child O was fine on June 22 and the night of June 22-23. She was the designated nurse for Child O and Child P on June 23, along with another baby, all in room 2. In police interview, Letby said the babies were in the 'high dependency' room and the ratio should have been one nurse to two babies - Letby was the only designated nurse in room 2 for that day, plus supervision of student nurse Rebecca Morgan. In cross-examination, she accepted staffing levels or competencies contributed to the collapse of Child O, and that Child O was not a high dependency baby. Nurse Melanie Taylor confirmed there were no issues for Child O at the beginning of the shift. A doctor noted Child O's abdomen was 'full but not distended, soft, non tender', and he was 'making good progress' at 9.30am. Melanie Taylor said Child O, prior to his collapse, asked Letby if he should be moved to room 1 as he looked unwell. Letby did not agree, and he should stay in 2. Melanie Taylor said she was 'put out' by this. Letby did not recall being dismissive.
2:38pm: Letby recorded feeds for Child O at 10am and noon. A note by a male doctor at 1.15pm recorded a distended abdomen and a vomit after a feed, and ordered an x-ray. Letby noted Child O, reviewed by the registrar 'had vomited (undigested milk) tachycardic and abdomen distended. NG tube placed on free drainage … 10ml/kg saline bolus given as prescribed along with antibiotics. Placed nil by mouth and abdominal x ray performed. Observations returned to normal'. An entry on the blood gas record by Letby said Child O was on CPAP, when he was not. Letby said she meant CPAP via Neopuff. Dr Bohin said she could find no record of Child O being on CPAP for this time. In interview, Letby recalled Child O's abdomen becoming distended and him being intubated. She did not recall who was present when he vomited. Melanie Taylor said Child O collapsed at about 2.40pm. When she went to nursery 2, Letby was already there, and a doctor arrived after. Letby said she discovered the collapse after hearing his monitor alarming, and he had a 'blotchy, purpley-red rash' kind of 'mottling'. She said mottling could be a sign of infection or cold. Child O was moved to nursery 1. The doctor's note of the event was a 'desaturation and bradycardia'. He was 'mottled' and skin looked 'unusual'. Child O was bagged and transferred to room 1. He was intubated at the first attempt and connected to a ventilator. The doctor went to speak to the parents. Letby noted Child O was 'mottled++ with abdomen red...poor perfusion'. She said she did nothing to Child O to introduce air, and said two prescriptions on the neonatal schedule with her co-signature were for after the collapse. The doctor noted a 'very very rare' purpuric rash, and 'good perfusion' and Child O appeared to stabilise. Letby said she did not see the type of discolouration the doctor did.
2:44pm: At 3.51pm, Child O desaturated again, to the 30s. 'Chest movement and air entry observed, minimal improvement.' Doctors were crash-called and Child O was reintubated on the first attempt. He had another desaturation at 4.15pm, and resuscitation efforts were made. There was 'no effective heartbeat' and the abdomen was 'still distended', and the rash had disappeared, which 'perplexed' the doctor, who had not seen that kind of rash before or again. Care was withdrawn and Child O died. Dr brearey said it was "deeply distressing for all involved" as Child o's deterioration "came out of the blue" and they "excluded all natural causes". He later held a debrief at which he said Letby 'did not seem upset'. Letby said she was "shocked and upset" at Child O's death, which was "unexpected", and there was an 'element of delay' when getting a registrar called to the room. She remembered Dr Brearey inserting a drain into Child O's abdomen, which was swollen and red, and she had not seen that procedure before. She said everyone was "completely flat" after Child O died. She said she wanted to save 'every baby in your care...you are not supposed to watch a baby die".
3:06pm: Child O's father described the stomach, swelling up, and 'looked like he had bad prickly heat - like you could see something oozing through his veins'. Letby said she had not seen anything like that. A female doctor was quite upset and very apologetic at Child O's death, and could not explain it. Dr Brearey told the court senior people at the hospital 'could not believe' someone was trying to harm babies. He said there had been a meeting and, when it was put to him about Letby's association with the events, he had said something along the lines of 'it can't be Lucy, not nice Lucy'. He said senior clinicians 'were becoming increasingly concerned' about the deaths. It was his opinion, that there was not an increasing range of acuity of babies being treated, and was wary it was a 'chicken and egg' situation where, because of the unexplained incidents that were happening on the unit, the babies' care needs became more acute. He said he had wanted to escalate the situation properly in the hospital, rather than by going to the police. He said Letby rejected his suggestion to take time off after Child O's death. The Countess of Chester Hospital was redesignated as a Level 1 unit, by its own decision, on July 7, 2016. The number of cot spaces was reduced from 16 to 12, and the gestational age limit was raised from 27 weeks to 32. Dr George Kokai carried out a post-mortem examination. Dr Andreas Marnerides reviewed, and said injuries to the liver were the result of impact trauma. He said during treatment, small bruises could be caused to the surface of the liver, and would not be extensive. He says the liver is not in an area where CPR is applied. He has only seen this kind of injury to the liver before in children, not babies, from accidents involving bicycles. He did not think CPR could produce this extensive injury to the liver, and has never heard of this sort being accepted as such. He also found internal gastric distention, and concluded there had been an air embolus. Prof Arthurs also referred to radiograph images, taken post-mortem. He said the gases were an 'unusual finding'. Dr Evans said the air was "excessive" and could have been administered via the NGT, and the skin discolouration was symptomatic of that. He said the bleed in the liver would also have contributed to the collapse. He could not find any evidence where the air embolus came accidentally. Dr Bohin said the cause was excessive air down the stomach via the NGT, causing an air embolus, and could not see any innocent cause for that. She refuted the accusation from the defence that she was striving to support the case against Letby by supporting Dr Evans. The prosecution say the jury can exclude natural causes, and Letby caused deliberate harm to Child O. The defendant denies wrongdoing, and the defence say it was a natural deterioration, and the liver injury was caused during resuscitation.
3:26pm: The judge refers to the case of Child P, born "in very good health". The triplets had been on CPAP and antiobiotics as a precaution. At 10am on June 23, Dr Kataryna Cooke recorded no concerns. Dr Gibbs recorded Child P had active bowel sounds, and a 'full...mildly distended' abdomen. He said Child P appeared very well, and should continue on NGT feeds, and if there were any concerns, for him to be fed intravenously. There was no suggestion of infection for Child P. Sophie Ellis was the designated nurse for Child P on June 23-24. She had learned that Child O had died on June 23. Child P's observations were in the normal area, and Sophie Ellis recorded a desaturation which resolved, and a low lying heart rate. For feeds, Child P was on two-hourly feeds up to 8pm on June 23, with trace aspirates. At 8pm, Sophie Ellis aspirated 14ml milk aspirates, with a pH of 3. She fed him a further 15ml milk feed, and placed him on his tummy. At the midnight, a further 20ml acidic milk aspirate was taken. Feeds were stopped and Child P was put on 10% dextrose infusions. She said if any of the aspirates were bilous, she would have noted it. The last update on the night shift was 'abdomen soft and non-distended' for Child P.
3:34pm: Nurse Percival-Calderbank had said Letby found working there was 'boring' and she tended to move back to the other nurseries, and colleagues were concerned for her mental health, as those units could be distressing and exhausting. Letby, in evidence, said she never found nursery work 'boring' and did not recall having a conversation with Kathryn Percival-Calderbank to say otherwise. In interview, Letby said she wanted to be designated nurse for Child P that day to provide continuity of care. Full blood tests were ordered for Child P. Dr Ukoh said Child P was to keep an eye on, as he had a distended abdomen. 20 minutes later, at about 9.50am, Child P desaturated. Rebecca Morgan said she recalled all the alarms going off, and she helped Dr Ukoh taking the top of the incubator off. Dr Ukoh said he and Lucy Letby were in the room when Child P collapsed. Letby said she was in the room when Child P collapsed. Arrowe Park provided advice for treatment of Child P. A poor blood gas result showed Child P had respiratory acidosis. He had a poor heart rate and poor perfusion. Child P was sedated and paralysed, which Dr Bohin said was entirely correct.
3:41pm: At 11.30am, Child P desaturated again, and he was given CPR. Spontaneous circulation was restored. A female doctor could not understand what was going on. Upon saying the transport team from Liverpool were arriving to transfer Child P, Letby had said words to the effect of: “he’s not leaving here alive is he?” The female doctor replied "Don't say that" - she thought they were 'winning' at that point. In evidence, Letby said she could potentially have said that at that time, and both she and the female doctor were stressed at that time. Letby said from her recollection, there was no reference to a tube dislodging for Child P. There is no evidence of anyone checking if it was blocked when it was removed. A radiograph image taken at 11.57am had showed a pneumothorax, which was not a tension pneumothorax. A male doctor's recollection from 12.50pm was that it was "very very busy" for Child P, and the plan was to insert a chest drain. There was no apparent cause for what was going on clincially, the judge tells the court.
3:49pm: Letby said she recalled the pneumothorax, and there was a "general decline" for Child P. A miscalculation had been made where the adrenaline doses were higher than they should have been, but a doctor from the transport team had previously told the court they found no sign of Child P being impacted by that. Child P's mother said Child P's stomach looked the same, but not as swollen. The father said the scene in the unit was one of pandemonium. "It was the same again". A female doctor was very apologetic to them, saying they would get to the bottom of what had caused the collapses. The third triplet, who was stable, was taken to Liverpool by the transport team. A female doctor denied she was trying to dramatise anything, in cross-examination. She said the situation was traumatic enough as it was. In evidence, Letby said she had been involved with administering a lot of medication, and did not recall seeing any discolouration. She said there was 'relief' on the unit when the transport team turned up. She said there was discussion if there had been a 'bug' on the unit.
4:01pm: After the deaths of Child O and Child P, the consultants 'insisted' Lucy Letby was removed from the unit, and 'resisted' attempts to bring her back, the court is told. Dr Marnerides said he had no evidence to indicate a natural disease that would account for Child P's death. He thought small haematomas to the liver were potentially the result of CPR, or as a result of prematurity, and did not have enough to say it was an impact injury. He said there was no clinical evidence for a natural cause. He said having considered other accounts, he concluded there was gastric distention caused by excessive air injected into the stomach. Prof Arthurs reviewed radiographic images for Child P. He said the gases shown were 'unusual' for baby who did not have natural diseases. He said it was consistent with air administered. Dr Evans was "at a loss" to explain how Child P had collapsed. He had believed the cause was complications from the pneumothorax. There was no credible natural cause. In cross-examination, he said an experienced or competent nurse or doctor would not cause a liver injury in resuscitations. He said Child P could have collapsed from doses of air administered, and denied shifting his account to fit the evidence. Dr Bohin was concerned about the x-ray for Child P on the night of June 23, and the air present there. Overnight, Child P became intolerant of feeds. She said attention should have been paid to the x-ray, which showed a pneumothorax, earlier. She said the air in Child P's abdomen from the night before was abnormal, and had been introduced at some point or points via the NGT, splinting the diaphragm. She could not think of any natural occurring phenomena that accounted for the subsequent collapses.
4:02pm: The trial judge says the case of Child Q will be referred to on Monday at 10.30am. The jury "will be beginning their deliberations" before the lunch break on Monday. He says he expects that to be after an hour's court sitting. He urges the jurors to bring their refreshments with them on that day.
5:33pm: The trial will not be sittig on Friday. It is expected to resume on Monday, when the jury will retire to consider verdicts. The Standard will continue to provide live updates on Monday.
Monday 10th July 2023
Judge's Summing Up - Day 5
Child Q - Other topics (Notes, Handover sheets, Diaries etc.) - General InstructionsChester Standard Live Reporting
9:02am: Nine months ago to the day, the 12 members of the jury first started hearing evidence in the Lucy Letby trial. Today is expected to see the conclusion to the judge's summing up of the case, after which the jury will retire to consider verdicts on the 22 charges - seven of murder, 15 of attempted murder.
10:17am: Last week, the judge's summing up referred to the cases, chronologically, from Child A to Child P. He told the jury last Thursday afternoon he intends to complete his summing up with the case of Child Q this morning.
10:26am: The courtroom at Manchester Crown Court is filling up with legal teams, members of the public and press, court staff, and Lucy Letby has arrived. The trial is due to resume at 10.30am.
10:31am: The trial judge, Mr Justice James Goss, has entered the courtroom.
10:32am: The 12 members of the jury are now coming into court, and the trial will resume with the judge's closing section of his summing up.
10:36am: Before the judge resumes, the jury is presented with a final selection of documents, which are for reference purposes, to add to their jury bundles.
10:40am: The judge now refers to the case of Child Q, a baby boy born on June 22, 2016 at the Countess of Chester Hospital. He weighed 2,076g at birth, and required breathing support - he was taken to the neonatal unit. There were no signs of infection, the judge says. Three days later, on June 25, Child Q had a profound desaturation and vomit. the prosecution say this was liquid, and possibly air, being forced down the NGT. They say possible mild NEC would not account for the type of desaturation and recovery. The defence say developing NEC cannot be excluded.
10:43am: For June 23-24, Tanya Downes was designated nurse for Child Q. She noted 'coffee ground' style amounts of bile in Child Q. 1.5ml of bile was aspirated at 4am. The nurse recalled Child Q had to be readmitted in July 2016 with gut problems, at the out-of-hours clinic.
10:50am: Child Q was tolerating feeds and there were "intermittent, moderate acidic" aspirates, a sign the milk was being partly digested, by the early hours of June 25. Blood gas readings showed a drop in pH results, and nurse Samantha O'Brien noted, after the doctor's review, was for the current plan of care to be continued. She said Child Q had been stable, and the reviewing doctor had no concerns. Letby, designated nurse for Child Q on the day of June 25, said she was informed Child Q had large aspirates overnight, so he was not in good condition. At about 9.10am, Child Q's alarm sounded, and he desaturated. Nurse Mary Griffith had been giving cares to another baby in the room with Letby and Child Q, with her back to Child Q. Shortly after Letby left the room, Child Q's alarm went off. Nurse Griffith was mid-feed and could not go over immediately, and Minna Lappalainen was called over to Child Q, and began Neopuffing the baby. Nurse Lappalainen recalled the alarm going off and could see Child Q had been sick, with mucus coming out of his mouth. She filled in the apnoea/fit/brady chart, a desat of 68 and brady of 98. "brady 98; desat 68; fit ?; baby found to be very mucousy, clear mucous from nasopharynx oropharynx removed clear fluid +++. O2 via neopuff given post suctioning...NGT used to aspirate stomach by Nurse L Letby"
10:51am: Letby noted: '[0910 Child Q] attended to by SN Lappalainen – he had vomited clear fluid nasally and from mouth, desaturation and bradycardia, mottled ++. Neopuff and suction applied...reg attended. Air++ aspirated from NG Tube'
10:55am: Letby said, in police interview, she had returned to nursery 2 to see Child Q being tended to by nurse Lappalainen. When asked about the air in Child Q's stomach, she said sometimes babies gulp when they vomit, and there could have been a blockage in the bowel. She said she would not have left room 2 if Child Q was not stable. She denied causing Child Q harm, or leaving the room so she had an alibi from the incident. In evidence, she said Child Q had a low temperature, and was concerned about that. She said she arranged with nurses Lappalainen and Griffith for when she went to nursery 1 and was there for a few minutes. For the 9am feed for Child Q, the Oxygen and saturation levels are missing. She said those omissions were "a mistake". She said the baby in room 1 was an intensive care baby, so she could not have left that baby for too long. She said she had no part in giving Neopuff after Child Q needed oxygen. She said she was told air++ had been aspirated from the NG Tube. She said the collapse, relatively, was 'not serious'.
11:03am: A male doctor was called to the unit. He noted as a result of the Neopuffing, Child Q's saturations returned to 100%. The baby was moved to room 1 and pub on CPAP, and given antibiotics as a precaution. He was presumed, at this time, to have sepsis. A blood test could not give a reason for the vomit, the judge says. A chest x-ray showed a 'trace of fluid', and 'no suggestion of a large amount of foreign matter' or a sign of infection. Dr John Gibbs said the collapse did not fit with a baby who was tired. It was decided to intubuate Child Q and put him on a ventilator. A female doctor examined Child Q noted the blood gases were acceptable. Child Q was 'very unsettled at times' but there were no signs of concern, she recalled. She saw a sign of respiratory acidosis, and the ventilator settings were changed. Amy Davies said Child Q was restless at times. On June 26, Child Q showed a loop in the bowel. Arrangements were made to transfer Child Q to Alder Hey Children's Hospital. A consultant there stated in agreed evidence that Child Q had been admitted due to concerns over his deteriorating condition. When assessed, Child Q was stable and his abdomen 'very slightly swollen'. By the night of June 26, he was assessed as 'very stable', with 'subtle signs of NEC', and was taken off the ventilator by June 27. The decision was made to transfer Child Q back to the Countess of Chester Hospital on June 28.
11:18am: The judge says the mother of Child Q said the baby was in and out of hospital about three times a year, and had a weakened immune system, and was diagnosed with developmental delay, and would require appropriate support. Professor Owen Arthurs reviewed radiograph images for Child Q. A single loop of dilated bowel was seen in the first, which was 'slightly normal', and gas in the bowel which had gone to the bowel wall. They were 'signs of NEC', but 'not diagnostic' of NEC. "Things were settling" at the time of the third x-ray, taken at Alder Hey. Dr Dewi Evans and Dr Sandie Bohin had considered the possibility of NEC. Dr Evans said although there were markers of Child Q having infection, from the bile aspirates and 'not really tolerating feeds', it did not explain the 'sudden collapse' at 9.10am, with a 'very significant deterioration', and it was 'not clear how to put it all together'. The suspicion of NEC was 'perfectly reasonable', as was putting Child Q on CPAP. He said Child Q would not have vomitted anything at all, unless 'a lot' of clear fluid had been forced down the NGT, possibly with air as well. He said once Child Q had vomitted, he recovered. He said in relation to the air+++, there was very little Neopuffing taking place. He said when babies vomit, they do not swallow air. In cross-examination, he accepted he had initially concluded Child Q had received air, and not fluid. The air++ was 'noteworthy'. Dr Evans refuted he had 'added' the liquid element to support the case. He said the evidence he had heard from the people looking after Child Q had been "a great help" in forming his opinion. He said the presence of NEC or otherwise could not be discounted, but that would not cause a sudden collapse, and noted the rapid recovery of Child Q, and no further gastro-intestinal problems until his discharge from the Countess hospital in July 2016. Dr Bohin noted the aspirates were 'not uncommon' for Child Q prior to the collapse. She did not know where the fluid+++ came from for Child Q, from the notes. Child Q's intermittent air was unlikely to cause the 'air++' aspirated. She concluded Child Q had been given air down the NG Tube, which had distended the abdomen so much, squashing the lungs, causing mottling. In cross-examination, she agreed 'mucus+++' being aspirated could cause problems with breathing. She said there was not a cause of where the 'mucus+++' would have come from. She refuted the possibility of any baby sucking in air during a vomit. She added aspirates was a sign of NEC, as well as other factors. She said it was not a diagnosis of NEC. She said Child Q 'got better too quickly for it to have been mild NEC'.
11:20am: Letby was enquiring with a male doctor about what Dr Gibbs had been saying about leaving Child Q unattended. The doctor reassured Letby. After Letby was taken off nursing duties, she filed a grievance with the hospital in September 2016. She said that time was emotionally difficult and had left her feeling isolated.
11:22am: The judge says agreed evidence says searches of Letby's home in Chester and Hereford were carried out in 2018 and 2019 respectively. He said there were various papers collected, including 'NOT GOOD ENOUGH' and 'I am a horrible evil person'. The defence says these were notes written by someone who was 'distraught' at what was happening and was being 'unfairly targeted'. The prosecution say the notes are by 'a troubled person' who was 'in part confessing to what she had done'.
11:24am: 257 handover sheets were found at Letby's Chester and Hereford homes, 21 of which in relation to babies in the indictment.
11:29am: In relation to a note filled in on both sides, Letby said she had written it as 'everything had got on top of her', and 'it made her feel guilty and isolated' and 'she was blaming herself'. She thought the police would be involved and she would lose her job. She thought she was being victimised by Dr Ravi Jayaram and Dr Stephen Brearey. She said despite what she had written, she 'had not killed them on purpose'. She said she was 'career focused' and the note 'I AM EVIL I DID THIS' was how the situation had made her feel. She said that year was difficult as there were more babies being admitted to the neonatal unit, with more complex needs such as chest drains and stomas, and staffing levels were 'quite poor at times', and she was doing a lot of additional shifts and overtime, and did not believe there was much support on offer. She said the handover sheets she had taken home in her pocket, were kept 'for no particular reason' and she 'did not know how to dispose of them'.
11:42am: Letby had said 'ideally', handover notes should be put in the confidential waste bin. She said she 'hardly ever looked at them'. In evidence, she confirmed she had bought a shredder, and 'only shredded bank statements', and the handover sheets and notes were 'insignificant'. When asked about Child M's blood gas records, the note taken home was 'an error on her part', and said the sheets had 'no meaning to her'. In a 2019 police interview, she identified a 'support network' of three nurses and a doctor she had after being removed from nursing duties. She had she was 'not really aware' of air embolisms, and could not recall any specific training in that. In her 2020 interview, Letby was asked about the diaries. She said she thought she started documenting names amid concerns of the rising number of babies dying. In evidence, she said she had liked all doctors at the hospital. She said she was worried she was in trouble as she may have made a mistake in the care of Child Q. She accepted, in an email she had written, she was 'having a meltdown++' as noted. In messages to a colleague, she accepted reference had been made to air embolus, and had filed a Datix form on July 1, 2016 in which she cited an open port had a potential risk of air embolus. She denied she was 'covering herself' for a cause of accidental air embolus or 'getting her defence in with friends'. Asked about a series of Facebook searches for parents' names of babies, she had they were for babies who had died or were seriously unwell. She denied she was 'checking up on her victims', but that they were 'on her mind'. She said she could not recall why she had written a sympathy note for all three triplets [Child O, Child P and the surviving triplet], when one of the triplets survived.
11:49am: The judge says the jurors have to be sure of the defendant's guilt, her character, and any inconsistencies between evidence given by the defendant and any witnesses. The judge says if jurors are sure that two babies had insulin administered to them, deliberately, they have to consider whether that was a coincidence, or whether it was done by one person, and if so, who. He says there were 'certain common features' among the cases, that the defendant was on duty for each event. He refers to the note that Nicholas Johnson KC had referred to, which was a list that included five babies had unusual bleeding, eight had discolouration. The defendant said she did not see discolouration or there was no discolouration to be seen. Five babies' collapses happened within moments of a nurse going on break. Four of the babies were 'screaming/crying uncharacteristically'. Four babies recovered after being taken to another hospital. Three cases were where Letby was accused of behaving inappropriately after the baby passed away. The prosecution say these are not unconnected events, and say the insulin, air embolus and post-mortem findings can make the jury sure of Letby's guilt. Letby denies doing any harm, and the searches and keeping of confidential documents had nothing sinister. The handwritten notes were 'a product of despair'. The defence say the jury cannot be sure in any event of Letby's guilt.
11:51am: The judge says a 20-minute process will now commence where jurors will affix their name labels to all the confidential documents they will have for their deliberations, to begin soon. He says there will be a few more things to be said to the jury once this process is completed, before the deliberation process can then begin.
11:54am: The judge says the beginning of the deliberation process is a 'strict procedure', and after the 20-minute break, he has a few words, but 'important words', to say to the jury.
11:55am: The members of the jury are now leaving for a 20-minute break, during which time their name-labelled bundles of documents will be taken to the deliberation room.
12:49pm: The trial will resume shortly - trial judge Mr Justice James Goss has returned to the courtroom.
12:50pm: The 12 members of the jury have now returned to the courtroom.
12:56pm: The judge apologises for the delay, saying the process took longer than anticipated. He says in relation to the lists the prosecution submitted, that the defence say they did not establish patterns, and there were dissimilarities. He says there will be two additions to the evidence bundle for the jurors - they had already been heard in evidence. Benjamin Myers KC says the two additions to the bundle are photographs of Letby's house, and a schedule of social media material which had been served. The judge says an iPad has been linked to a large screen in the room, so evidence for group discussion can be presented on a big screen, for convenience. There will be spare iPads [which contain the evidence stored electronically in the case].
1:00pm: He says the deliberations are confidential to the jury, and there is no disclosure of them to anyone, including any court bailiffs when they are present in the deliberation room. He says the jurors should respect each others' opinions, everyone should be listened to, and no-one should feel pressured, including on time. Deliberation times will be between 10.30am-4pm. At 4pm, the jury will be brought back each day and then sent home. When they are not deliberating, the deliberation room will remain locked. The judge urges jurors to not, under any circumstances, discuss the case with anyone outside of all 12 jurors in the deliberation. They are not allowed to discuss the case with each other in the absence of any juror. Two five-minute 'smoke breaks' will take place during each day, one in the morning and one in the afternoon. For each of those breaks, a bailiff will escort the juror or jurors outside and remain with them. Another bailiff will remain with the jurors inside the deliberation room. A man or woman will be selected as the jury foreman. That person can be changed in advance of a verdict for any reason, the judge advises. Any questions on the case are to be written on a note, not communicated verbally to the court bailiff, for presentation to the court.
1:01pm: He says verdicts should be unanimous on each count. He says if, after a certain length of time, jurors are unable to agree unanimous verdicts, then they will be brought back to court and further directions will be given.
1:02pm: The court ushers are now being sworn as jury bailiffs.
1:03pm: The jury is now being sent out to consider verdicts.
4:01pm: Legal teams, members of the public and press, and Lucy Letby have returned to court, along with the trial judge.
4:03pm: The trial judge informs the jurors they can go home for today, and will resume deliberations at 10.30am. The jurors are urged not to discuss the case with anyone, including each other, until they have returned to the deliberation room tomorrow.